Introduction
High astigmatism commonly occurs after penetrating
keratoplasty (PKP). Due to the high residual astigmatism after PKP,
patients often fail to obtain a satisfied visual acuity (1). In cases of high astigmatism, spectacles
or contact lens correction may become difficult (2). Several surgical techniques to correct
post-PKP astigmatism have been described. These include astigmatic
keratotomy (AK) (3,4), relaxing incisions (5), corneal wedge resection (6), compression sutures (7), laser in situ keratomileusis
(LASIK) (8) and implantation of
toric intraocular lenses (IOL) (9).
However, these methods have certain limitations. Compression
sutures and LASIK are limited in the range of astigmatism they are
able to correct. Toric IOL implantation is also limited by the
range of the astigmatism correction (10) and not suitable for young patients
without cataracts. With the emergence of femtosecond laser, the
accuracy and safety of the treatment of corneal astigmatism has
increased. The femtosecond laser has been successfully used in
several corneal surgical procedures. Wang et al (11) investigated the efficacy of
femtosecond laser-assisted cataract surgery combined with
femtosecond laser AK to manage pre-operative astigmatism in
cataract surgery and reported a significant decrease in
astigmatism. Buzzonetti et al (12) used femtosecond laser-assisted AK to
correct astigmatism after PKP and reported a decrease in
astigmatism. In order to obtain an augmented effect for reducing
high levels of corneal astigmatism after PKP, certain novel
combined procedures have been designed. Çakır et al
(13) used circular keratotomy
combined with wedge resection to treat high astigmatism after PKP
and reported a significant reduction in astigmatism. Sy et
al (14) performed AK combined
with conductive keratoplasty to treat high astigmatism after PKP
and obtained a satisfactory reduction in astigmatism. AK involves
placing 1 or 2 deep, arcuate corneal incisions perpendicular to the
steep meridian of the astigmatism to flatten the steep corneal
meridian. AK is conventionally used to correct moderate to high
astigmatism (15). However, AK is
also limited in the amount of astigmatism it is able to correct.
Scleral tunnel incisions are able to flatten the corneal curvature
when placed at the steepest astigmatism meridian. Weindler et
al (16) performed a single 6-mm
scleral tunnel incision to correct pre-operative astigmatism by
placing the tunnel incision at the steep meridian during cataract
surgery and reported a reduction in astigmatism from 1.60±0.65 to
0.89±0.61 D. These changes in stromal architecture reduces
astigmatism by placing incisions perpendicular to the steep axis of
astigmatism to flatten the steep corneal meridian, and the
combination of these two treatments is likely to produce a
synergistic effect (15,16).
To the best of our knowledge, no previous study has
evaluated the effects of AK combined with scleral tunnel incisions
to correct high astigmatism after PKP. The present study reported
on the efficacy, predictability and safety of this combined
surgical treatment.
Patients and methods
Patients
All surgeries were performed between January 2014
and March 2017 at the First Affiliated Hospital of Anhui Medical
University (Hefei, China). This study was performed according to
the tenets of the Declaration of Helsinki and was approved by the
Ethics Committee of the First Affiliated Hospital of Anhui Medical
University. Informed consent was obtained from all participants
after explanation of the study and possible consequences. Inclusion
criteria for the present study included, high post-PKP keratometric
astigmatism (>5.0 D), complete removal of sutures at least 6
months prior to the combined procedure and steady ametropia.
Patients with regular astigmatism were included in the study, but
highly irregular patterns of topographic astigmatism were excluded.
General examinations were taken to exclude any systemic and other
eye diseases. The TMS-4 topographic system (Tomey Corp., Nagoya,
Japan) was used to measure the keratometric astigmatism. A total of
8 eyes of 8 patients with high residual keratometric astigmatism
(8.16±3.02 D) after PKP were enrolled in the present study.
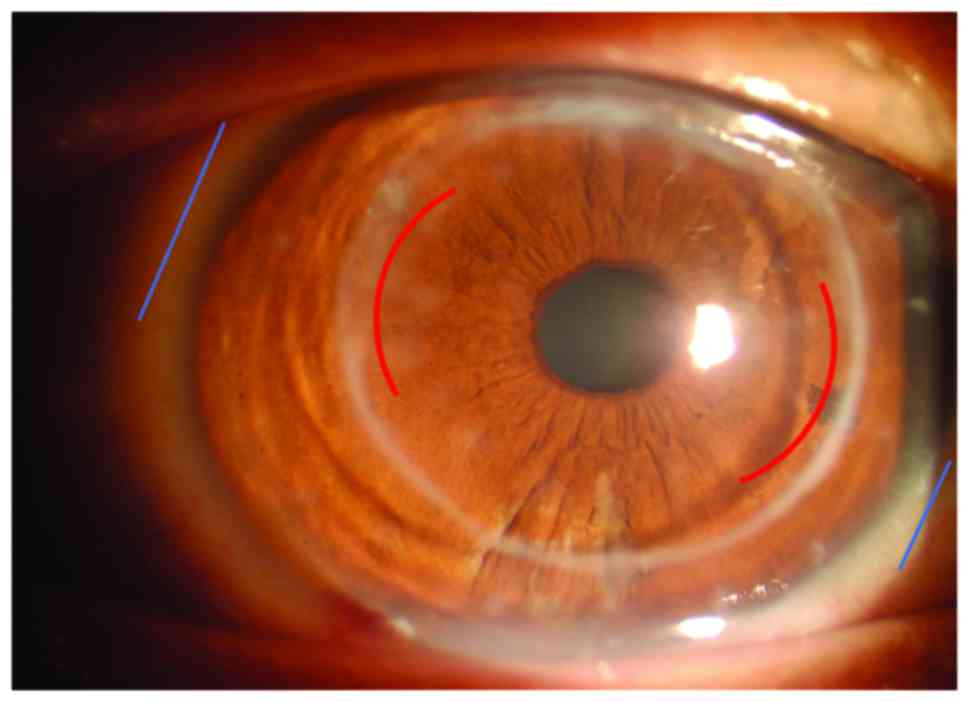
Surgical procedure
Prior to the procedure, the corneal thickness was
measured using a pachymetry map of the Angio optical coherence
tomography (Angio-OCT) system (Optovue Corp., Fremont, CA, USA).
Subsequent to topical anesthesia using 0.5% proparacaine
hydrochloride (Alcaine; Alcon Laboratories, Inc., Fort Worth, TX,
USA), the cornea was marked at the vertical meridian and the
horizontal meridian pre-operatively in the sitting position to
reduce the error induced by cyclotorsion in the lying position. The
steep astigmatism meridian was marked intra-operatively according
to the corneal topography obtained prior to surgery. A pair of
symmetrical arc incisions were created along the steep meridian of
the astigmatism using a guarded diamond blade. The length of the
incisions was determined by the magnitude of the astigmatism and
ranged from 60 to 85° (60–65° for 5–6 D, 65–75° for 7–10 D and 85°
for >10 D of astigmatism). The incisions were placed 0.5 mm
inside the graft-host junction at a depth of ~90% of the corneal
thickness in all cases, and the anterior side-cut angle was set at
90° to the corneal surface. Subsequently, the incisions were opened
using a Sinskey and a pair of symmetrical scleral tunnel incisions
were made 1.5 mm away from the cornea limbus at the steep
astigmatic meridian using a scleral tunnel knife to make 6 mm wide
incisions (Fig. 1). The area was
then cleaned with balanced salt solution. All patients received the
surgery from an experienced operator (RFL). Postoperatively, the
operated eyes were treated with tobramycin and dexamethasone eye
drops and levofloxacin eye drops 4 times daily for 2 weeks.
Patient assessment
Patients were regularly examined after the operation
and the follow-up results at 3 and 6 months after the combined
procedure were recorded. Pre- and post-operative evaluation
included slit lamp examination, refraction, non-contact measurement
of intraocular pressure, logarithm of the minimum angle of
resolution (LogMAR) of uncorrected visual acuity (UCVA) and best
corrected visual acuity (BCVA). Keratometric astigmatism was
measured by corneal topography. Angio-OCT was used to obtain
cross-sectional images of the corneal incisions and assess the
wound healing of these corneal incisions.
Vector analysis
Keratometric astigmatism vectors were evaluated
using the Alpins method, which assesses the effective change in
keratometric astigmatism (17).
Vector parameters analyzed included: The target induced astigmatism
(TIA), defined as the astigmatic correction in magnitude and axis
the operator intended to induce, which is equivalent to the
pre-operative astigmatism; surgically induced astigmatism (SIA),
defined as the amount and axis of astigmatic change actually
induced by surgery; difference vector (DV), defined as the vector
difference of TIA and SIA and reflecting the post-operative
astigmatism; angle of error (AE), which is the angle offset between
SIA and TIA-it is positive if SIA is on an axis counterclockwise to
TIA and negative if SIA is on an axis clockwise to TIA; magnitude
of the error (ME), which is the magnitude difference between SIA
and TIA-it is positive for overcorrection and negative for
undercorrection; correction index, calculated by dividing the SIA
by the TIA-it is ideally 1.0, and >1.0 for overcorrection and
<1.0 for undercorrection; index of success (IOS), calculated by
dividing the DV by the TIA-it is ideally 0.
Statistical analysis
Statistical analysis was performed using SPSS
software (version 17.0; SPSS, Inc., Chicago, IL, USA). Values are
expressed as the mean ± standard deviation. The paired Student
t-test was used to assess the difference between pre-operative and
post-operative values. Pearson correlation analysis was used to
assess the correlation between SIA and TIA. P<0.05 was
considered to indicate a statistically significant difference.
Results
Patient characteristics
The study included 8 patients (3 females and 5 males
aged 21–56 years; mean age, 29.50±11.60 years), who had a history
of high residual astigmatism after PKP. The most common
pre-operative diagnosis was keratoconus in 7 eyes, followed by
infectious corneal scar in 1 eye. The mean interval between PKP and
the surgical treatment was 17±5.5 months. AK and scleral tunnel
incision (case no. 1, male, 22 years old) was performed on the
right eye of a patient to correct high astigmatism after
penetrating keratoplasty (Fig.
1).
Visual acuity and refraction
changes
The mean values for the visual acuity and refraction
changes are presented in Table I.
The mean UCVA at baseline was 0.95±0.24 LogMAR and that at 3 months
post-surgery was 0.61±0.17 LogMAR; this difference was
statistically significant (P<0.05). Prior to surgery, the mean
BCVA was 0.41±0.18 LogMAR and that at 3 months post-surgery was
0.26±0.12 LogMAR; this change was not statistically significant
(P>0.05). The mean magnitude of keratometric astigmatism was
8.16±3.02 D pre-operatively and 2.28±1.07 D at 3 months
postoperatively; the mean difference resembled a reduction by 5.88
D, which was a significant change (P<0.05). The keratometric
astigmatism could not be corrected significantly through the
combined procedure in a patient (case no. 7, female, 56 years old).
The mean subjective astigmatism was 7.68±2.62 D pre-operatively and
2.5±1.24 D at 3 months postoperatively, with a statistically
significant reduction by 5.18 D (P<0.05). The mean spherical
equivalent refraction pre-operatively and at 3 months post-surgery
was 3.65±1.05 and −3.38±0.97 D, respectively, and the difference
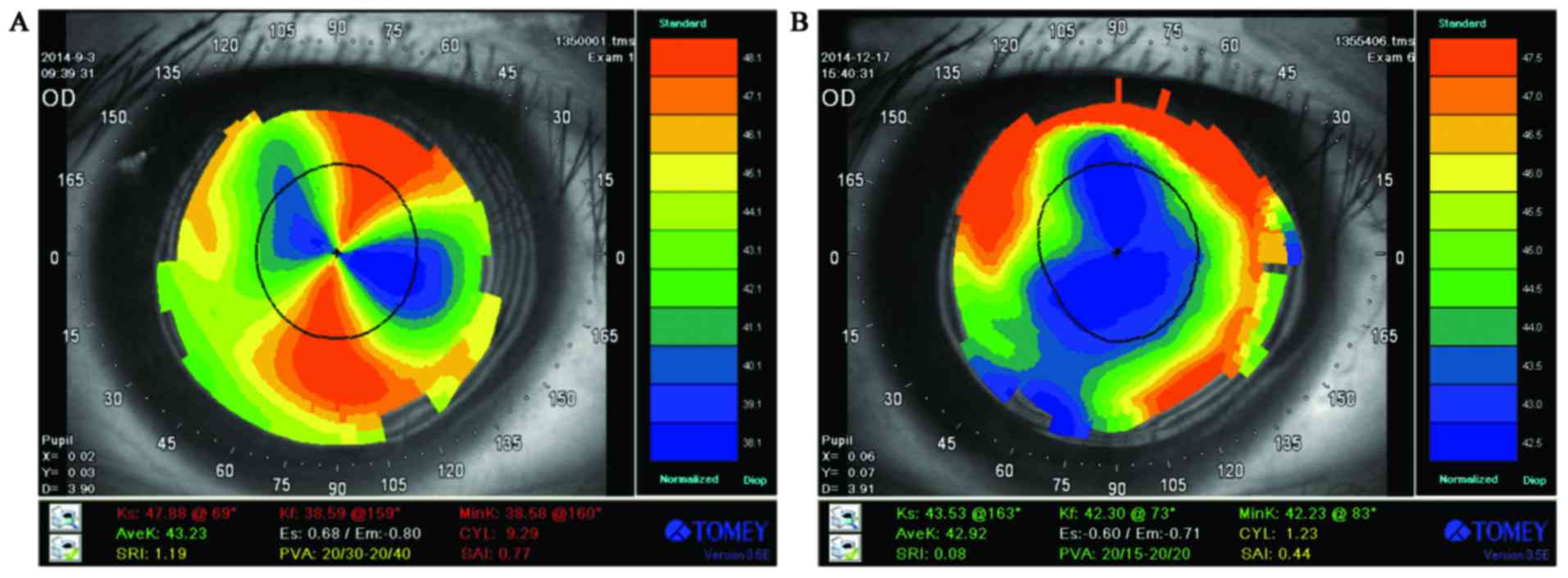
was not statistically significant (P>0.05). The pre-operative
and 3 month post-operative corneal topography in a patient (case
no. 1, male, 22 years old) who had undergone AK combined with
scleral tunnel incisions demonstrated a decrease in keratometric
astigmatism from 9.29 to 1.23 D (Fig.
2).
 | Table I.Visual acuity and keratometric
astigmatism at baseline and 3 months after surgery. |
Table I.
Visual acuity and keratometric
astigmatism at baseline and 3 months after surgery.
|
| Characteristics | Pre-operative | Post-operative |
|---|
|
|
|
|
|
|---|
| Case no. | Age (years) | Sex | UCVA (LogMAR) | BCVA (LogMAR) | KA (D) | Axis (°) | UCVA (LogMAR) | BCVA (LogMAR) | KA (D) | Axis (°) |
|---|
| 1 | 22 | Male | 1.30 | 0.60 | 9.29 | 159 | 0.50 | 0.20 | 1.23 | 73 |
| 2 | 27 | Male | 1.00 | 0.40 | 7.38 | 170 | 0.80 | 0.40 | 3.42 | 166 |
| 3 | 24 | Male | 0.80 | 0.30 | 10.78 | 87 | 0.40 | 0.20 | 2.07 | 15 |
| 4 | 35 | Female | 0.70 | 0.40 | 5.63 | 76 | 0.50 | 0.20 | 2.29 | 166 |
| 5 | 23 | Male | 0.80 | 0.20 | 7.65 | 149 | 0.60 | 0.20 | 2.18 | 118 |
| 6 | 21 | Female | 1.00 | 0.70 | 5.70 | 127 | 0.90 | 0.40 | 2.13 | 117 |
| 7 | 56 | Female | 1.30 | 0.50 | 13.89 | 34 | 0.70 | 0.40 | 4.12 | 24 |
| 8 | 28 | Male | 0.70 | 0.20 | 5.02 | 100 | 0.50 | 0.10 | 0.83 | 129 |
| Mean | 29.50 |
| 0.95 | 0.41 | 8.17 |
| 0.61 | 0.26 | 2.28 |
|
| SD | 11.60 |
| 0.24 | 0.18 | 3.02 |
| 0.17 | 0.12 | 1.07 |
|
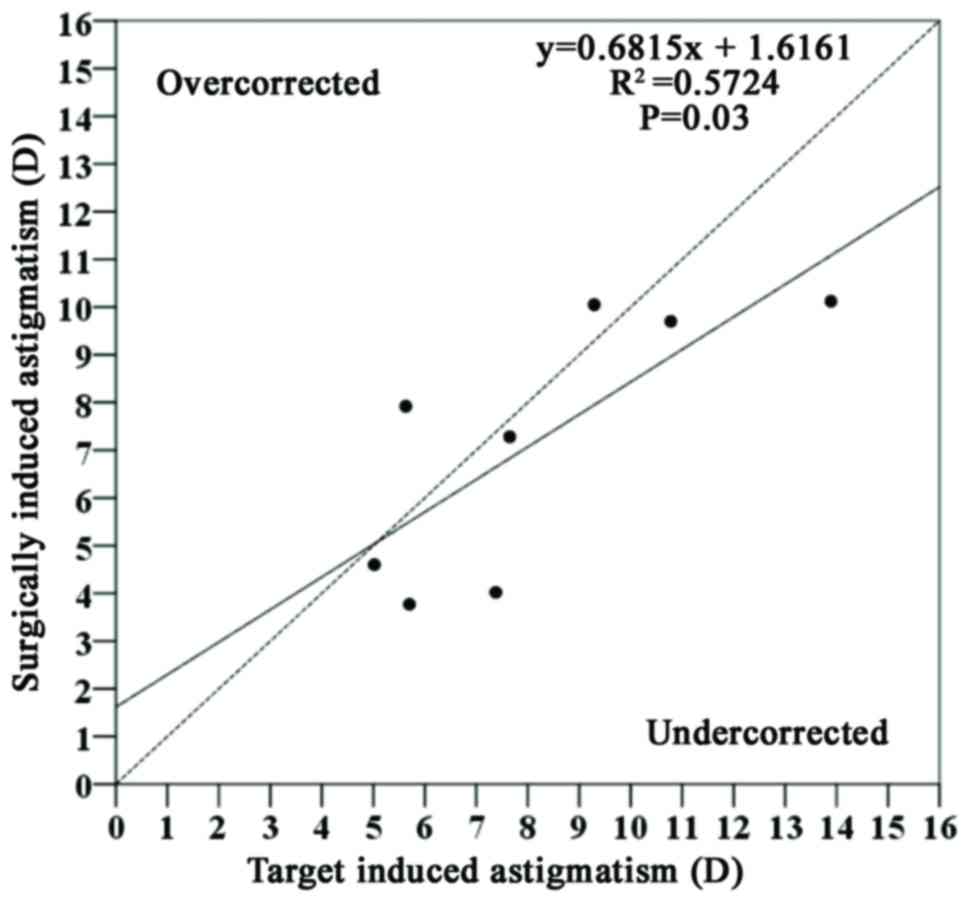
Vector analyses of keratometric
astigmatism
The keratometric vectors were calculated for each
eye (Table II). At 3 months
postoperatively, the mean keratometric vectors were as follows:
TIA, 8.17±3.03; SIA, 7.18±2.73; and DV, 2.28±1.07. The mean AE was
3.5±2.82, indicating no significant systematic bias. The mean ME
was −1.80±1.28, suggesting a tendency for undercorrection. The
correction index was 0.90±0.29, again indicating a slight tendency
for undercorrection. The IOS was 0.29±0.12, suggesting a satisfying
reduction of the original astigmatism. There was a significant
correlation between SIA and the TIA (P<0.05; Fig. 3).
 | Table II.Individual KA assessed using vector
analysis in cases 1–8. |
Table II.
Individual KA assessed using vector
analysis in cases 1–8.
|
| Parameters |
|---|
|
|
|
|---|
| Case no. | TIA (D) | SIA (D) | DV (D) | AE (°) | ME (D) | IOS | Correction
index |
|---|
| 1 | 9.29 | 10.05 | 1.23 | 0 | −1.21 | 0.13 | 1.13 |
| 2 | 7.38 | 4.02 | 3.42 | 2 | 3.36 | 0.46 | 0.54 |
| 3 | 10.78 | 9.70 | 2.07 | 3 | −1.08 | 0.19 | 0.90 |
| 4 | 5.63 | 7.92 | 2.29 | 0 | 2.29 | 0.40 | 1.41 |
| 5 | 7.65 | 7.28 | 2.18 | 8 | −0.37 | 0.28 | 0.95 |
| 6 | 5.70 | 3.77 | 2.13 | 5 | −1.93 | 0.37 | 0.59 |
| 7 | 13.89 | 10.12 | 4.12 | −6 | −3.77 | 0.30 | 0.72 |
| 8 | 5.02 | 4.60 | 0.83 | −5 | −0.42 | 0.17 | 0.92 |
| Mean | 8.16 | 7.18 | 2.28 | 3.5 | −1.80 | 0.29 | 0.90 |
| SD | 3.03 | 2.73 | 1.07 | 2.8 | 1.28 | 0.12 | 0.29 |
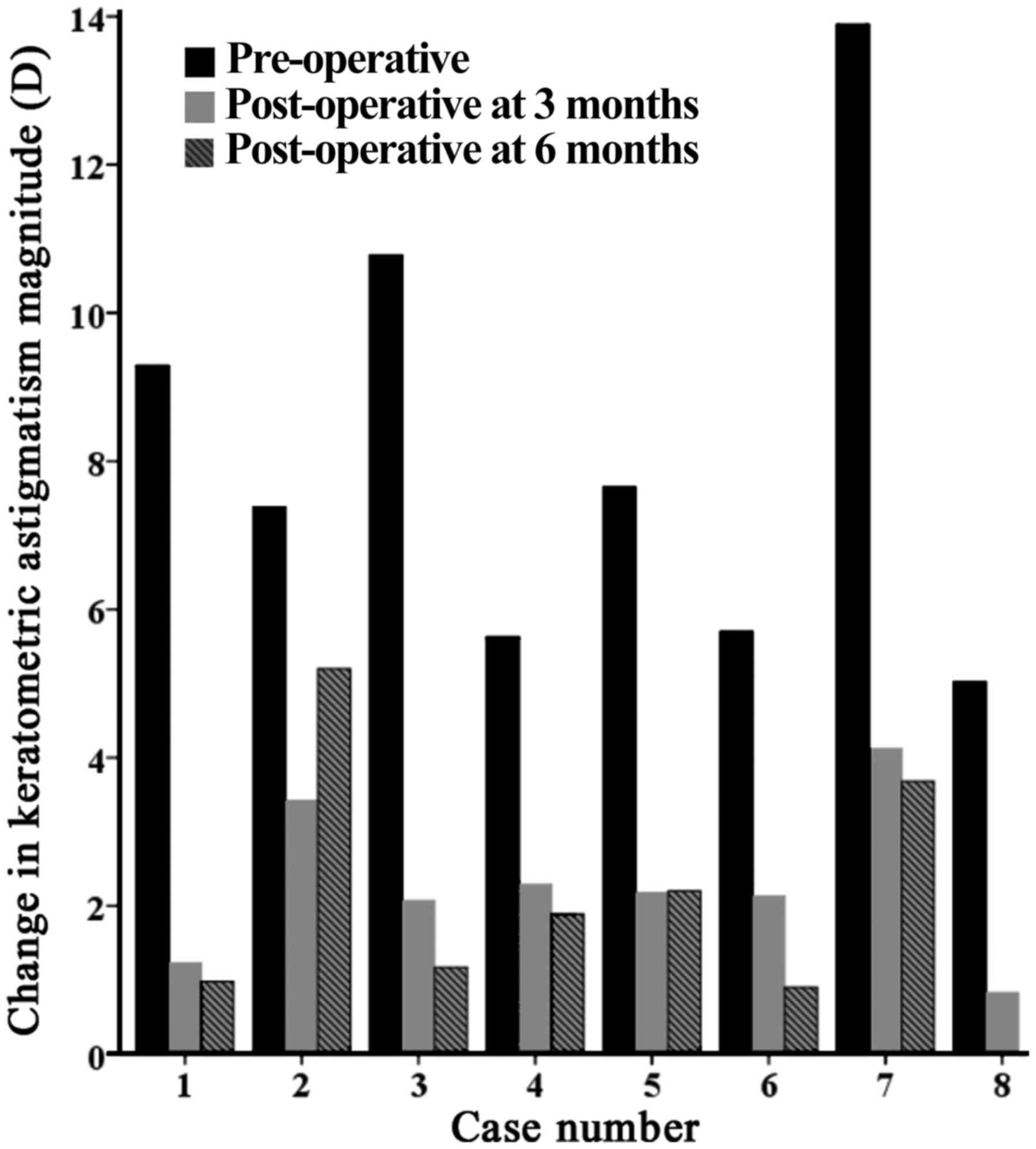
Stability
During the 6-month follow-up after AK combined with
scleral tunnel incisions, the patients retained a stable
keratometric astigmatism. At 3 and 6 months postoperatively, the
mean keratometric astigmatism was 2.28±1.07 and 2.02±1.69 D,
respectively. There was no significant change in keratometric
astigmatism at 3 and 6 months postoperatively (P=0.72; Table III). In addition, a patient (case
no. 8, male, 28 years old) had zero post-operative astigmatism
after 6 months (Fig. 4). The mean
magnitude of SIA was 7.18±2.73 D at 3 months and 7.57±3.37 D at 6
months (P=0.80; Table IV). The mean
difference in SIA magnitude between 3 months and 6 months also
demonstrated no significant trend toward progression or
regression.
 | Table III.Pre-operative and post-operative KA
in cases 1–8. |
Table III.
Pre-operative and post-operative KA
in cases 1–8.
|
| Pre-operative | Post-operative 3
months | Post-operative 6
months |
|
|---|
|
|
|
|
|
|
|---|
| Case no. | KA (D) | KA (D) | KA (D) | P-value |
|---|
| 1 | 9.29 | 1.23 | 0.98 |
|
| 2 | 7.38 | 3.42 | 5.20 |
|
| 3 | 10.78 | 2.07 | 1.17 |
|
| 4 | 5.63 | 2.29 | 1.89 |
|
| 5 | 7.65 | 2.18 | 2.20 |
|
| 6 | 5.70 | 2.13 | 0.90 |
|
| 7 | 13.89 | 4.12 | 3.68 |
|
| 8 | 5.02 | 0.83 | 0.00 |
|
| Mean ± SD | 8.17±3.03 | 2.28±1.07 | 2.00±1.69 | 0.72 |
 | Table IV.Post-operative SIA in cases 1–8. |
Table IV.
Post-operative SIA in cases 1–8.
|
| Post-operative 3
months | Post-operative 6
months |
|
|---|
|
|
|
|
|
|---|
| Case no. | SIA (D) | SIA (D) | P-value |
|---|
| 1 | 10.05 | 9.29 |
|
| 2 | 4.02 | 3.72 |
|
| 3 | 9.70 | 8.86 |
|
| 4 | 7.92 | 7.96 |
|
| 5 | 7.28 | 7.23 |
|
| 6 | 3.77 | 4.70 |
|
| 7 | 10.12 | 14.13 |
|
| 8 | 4.60 | 4.67 |
|
| Mean ± SD | 7.18±2.73 | 7.57±3.37 | 0.80 |
Safety and complications
Patients were reviewed at 1 day, 1 week, 1, 3 and 6
months post-surgery and no severe complications, including
perforation or infectious keratitis, occurred in these patients.
The Angio-OCT clearly displayed the morphology of the keratotomy
incision. The cross-sectional image of the corneal incision (case
no. 2, male, 27 years old), demonstrated no gaping of the wound
(Fig. 5). The incisions were healing
well in all patients.
Discussion
High residual astigmatism after PKP is a common
complication due to various factors. Several studies have attempted
to solve this problem with means including spectacles, AK,
compression sutures, LASIK (8) and
implantation of toric IOL. Although spectacles and contact lenses
may correct refractive errors following PKP, it is difficult to
correct high astigmatism after PKP using these methods (2). Wade et al (18) used a toric intraocular lens to
correct astigmatism in 16 patients with prior PKP and reported a
reduction in astigmatism from 3.34±2.13 to 1.58±1.25 D. However,
toric IOL implantation is also limited by the range of astigmatism
it is able to correct and it increases the risk for graft rejection
after PKP (19).
Compared with other methods to correct astigmatism,
AK has certain advantages, e.g., it is relatively simple and
low-cost, and is commonly performed to correct astigmatism after
PKP (15). Various different
incision nomograms have been used in the AK procedure over the
years (3,4). The most common type of AK involves
creating paired deep, curved corneal incisions at the steep
astigmatism meridian. The fundamental principle of AK is that it
relaxes the corneal tissue, thereby increasing the radius of
curvature and flattening the steep meridian perpendicular to the
incision. AK is also limited regarding the degree of astigmatism it
is able to correct.
Scleral tunnel incisions are also able to flatten
the corneal curvature when being placed at the steepest astigmatism
meridian. Wirbelauer et al (20) used a 7-mm scleral tunnel incision
centered at the steeper meridian to reduce pre-operative oblique
astigmatism in subjects receiving cataract surgery and reported
that a significant mean reduction in astigmatism of 0.58 D
(P<0.01) was achieved only in the group in which the incision
was centered on the steeper meridian. Weindler et al
(16) reported a reduction from 1.6
to 0.89 D in astigmatism after using a scleral tunnel incision on
the steepest meridian in cataract surgery. Heider et al
(21) also reported that the
technique of scleral tunnel incision on a steeper meridian reduced
a pre-existing inverse or oblique astigmatism in cataract
surgery.
Paired AK combined with scleral tunnel incisions is
likely to produce a synergistic action and is expected to have an
augmented effect in reducing high astigmatism after PKP. The effect
of this combined method was evaluated in the present study.
Improvement of the UCVA and BCVA after the combined
procedure was observed in the present study in comparison with the
results of femtosecond laser-assisted AK for the treatment of
high-astigmatism post-PKP reported by Cleary et al (22) and Fadlallah et al (23). In the present study, the mean UCVA
improved from 0.95±0.24 LogMAR pre-operatively to 0.61±0.17 LogMAR
postoperatively (P<0.05). The mean BCVA improved from 0.41±0.18
LogMAR pre-operatively to 0.26±0.12 LogMAR postoperatively
(P>0.05). Although the change was not statistically significant,
there was a trend toward improvement in the post-operative
BCVA.
The mean pre-operative magnitude of keratometric
astigmatism was 8.16±3.02 D, and at 3 months postoperatively, the
mean keratometric astigmatism was 2.28±1.07 D, with a statistically
significant reduction by 5.88 D (P<0.01). The mean pre-operative
subjective astigmatism decreased from 7.68±2.62 to 2.5±1.24 D
(P<0.05). Compared with other current surgical treatments,
including AK alone or LASIK, the combined surgical treatment
produced a greater reduction in astigmatism. Böhringer et al
(24) performed AK alone to correct
keratometric astigmatism and reported a reduction in mean
astigmatism from 9.2 to 5.5 D after AK. Cleary et al
(22) observed a decrease in
keratometric astigmatism from 9.8±2.9 to 4.5±3.2 D after
femtosecond laser-assisted AK. Donnenfeld et al (25) used LASIK to correct astigmatism after
PKP and reported a decrease in astigmatism from 3.64±1.72 D
pre-operatively to 1.29±1.04 D postoperatively. Several combined
surgery methods have been reported for the treatment of high
astigmatism. The reduction in astigmatism achieved using the
combined procedure of the present study is similar to or better
than that achieved by other combined surgery methods. Sy et
al (14) performed AK combined
with conductive keratoplasty to treat high astigmatism and reported
a reduction in astigmatism from 10.25±4.71 to 4.31±2.34 D. Javadi
et al (26) reported a
relatively lesser reduction in astigmatism from 6.8±1.4 to 3.9±1.6
D after augmented relaxing corneal incisions. Of note, the combined
procedure of the present study failed to significantly correct the
keratometric astigmatism in 1 patient (case no. 7, female, 56 years
old), who was the oldest in the study cohort; it may be assumed
that the decline of corneal biomechanics with age is one of the
major reasons. Day and Stevens (27)
reported that the SIA is dependent on the biomechanical properties
of the cornea. In the present study, the change in spherical
equivalent refraction was not statistically significant
(P>0.05).
On the basis of the keratometric data, the
predictability of the new combined procedure was evaluated. Alpin's
method was used in the present study, as the method is able to
comprehensively analyze the changes of astigmatism (17). In the present study, the SIA was
closely correlated with the TIA. The keratometric analysis
indicated an undercorrection of the astigmatism in most cases. The
negative ME values, which are obtained if the magnitude of the SIA
is less than the magnitude of the TIA, also reflected a trend
toward undercorrection. The mean correction index, which was
<1.0 in the present study, also indicated undercorrection. These
outcomes are similar to those obtained by Sy et al (14). The mean AE value was only 3.5±2.82,
indicating no systematic misalignment. The IOS, which is preferably
0, was 0.29±0.12 in the present study, and it testified the
relative predictability of the novel combined method.
The stability profile was also assessed in the
present study. There was no significant change in keratometric
astigmatism between 3 and 6 months post-surgery. The change in the
mean SIA between 3 and 6 months postoperatively also demonstrated
no significant trend toward progression or regression.
The safety of an operation is another important
issue. In the present study, no severe complications, including
secondary glaucoma, infectious keratitis or perforation, were
encountered in any of the patients. In addition, there was no
implantation of epithelium of the cornea in the wounds. The
Angio-OCT images demonstrated that there was no gaping in the
wounds and incisions were healing well in all patients. It is
therefore indicated that the treatment of AK combined with scleral
tunnel incisions may be a safe method to reduce high astigmatism
after PKP.
Based on previous studies, the effect of AK is
affected by three factors: The length of the incision arc, the
depth of the incision and the position of the incision. Increasing
the length of the incision arc may yield better results. Kumar
et al (28) performed
intralase-enabled AK to correct high astigmatism after PKP. The
depth of the incision was set at 90% and it was placed 0.50 mm
inside the graft. The length of the incision arc was determined by
the magnitude of the astigmatism: 40–60° for up to 6 D, 65–75° for
6–10 D and 90° for >10 D of astigmatism. They obtained a
reduction in astigmatism by 64%. Fares et al (29) also applied a varied incision depth
according to the magnitude of astigmatism to correct astigmatism
after PKP and reported a satisfactory reduction in astigmatism.
Increasing the depth of the incision is another option. Akura et
al (30) reported a method of AK
termed full-arc, depth-dependent AK (FDAK). They chose an arcuate
incision of 90° in length with an optical zone of 7.0 mm and varied
the incision depth between 40 and 75% to treat astigmatism; the
outcomes demonstrated that FDAK may be an effective and safe method
to correct astigmatism. In addition, incision nomograms may also be
affected by changes in optical zone size, with a small optical zone
having a greater effect. However, as the cornea becomes thin near
its center, the difficulty of the surgery is increased. Based on
previous studies, the use of the following incision nomogram may be
proposed: All incisions should be placed at 7.0 mm into the optical
zone and have a depth of 90% of the cornea. The Arc length should
range from 60 to 85°, with 60–65° for 5–6 D, 65–75° for 7–10 D and
85° for >10 D of astigmatism (28–30).
In conclusion, AK combined with scleral tunnel
incisions is an effective, relatively predictable and safe method
to reduce high astigmatism after PKP. The limitations of the
present study include the small number of subjects and the limited
follow-up time. An increase of sample size and long-term
observation are required to further examine the efficacy of the
combined procedure. In addition, further studies are required to
improve the incision nomograms for improving the predictability of
this combined procedure.
Acknowledgements
Not applicable.
Funding
The project was supported by the Science Foundation
of Anhui Medical University (grant no. 2017kj25).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
Z-YG designed the study and performed patient
examinations; M-JY and K-KJ collected and analyzed the data; Z-YG
and R-FL prepared the manuscript; R-FL performed the surgeries and
supervised the project. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the First Affiliated Hospital of Anhui Medical
University (reference no. Quick-PJ 2013-11-17). Informed consent
was obtained from all participants.
Patient consent for publication
Patients provided written informed consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Williams KA, Roder D, Esterman A,
Muehlberg SM and Coster DJ: Factors predictive of corneal graft
survival. Report from the Australian Corneal Graft Registry.
Ophthalmology. 99:403–414. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bochmann F and Schipper I: Correction of
post-keratoplasty astigmatism with keratotomies in the host cornea.
J Cataract Refract Surg. 32:923–928. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nubile M, Carpineto P, Lanzini M, Calienno
R, Agnifili L, Ciancaglini M and Mastropasqua L: Femtosecond laser
arcuate keratotomy for the correction of high astigmatism after
keratoplasty. Ophthalmology. 116:1083–1092. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kim BK, Mun SJ, Lee DG, Kim JR, Kim HS and
Chung YT: Full-thickness astigmatic keratotomy combined with
small-incision lenticule extraction to treat high-level and mixed
astigmatism. Cornea. 34:1582–1587. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fronterrè A and Portesani GP: Relaxing
incisions for postkeratoplasty astigmatism. Cornea. 10:305–311.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ezra DG, Hay-Smith G, Mearza A and Falcon
MG: Corneal wedge excision in the treatment of high astigmatism
after penetrating keratoplasty. Cornea. 26:819–825. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chang SM, Su CY and Lin CP: Correction of
astigmatism after penetrating keratoplasty by relaxing incision
with compression suture: A comparison between the guiding effect of
photokeratoscope and of computer-assisted videokeratography.
Cornea. 22:393–398. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Arenas E and Maglione A: Laser in situ
keratomileusis for astigmatism and myopia after penetrating
keratoplasty. J Refract Surg. 13:27–32. 1997.PubMed/NCBI
|
|
9
|
de Sanctis U, Eandi C and Grignolo F:
Phacoemulsification and customized toric intraocular lens
implantation in eyes with cataract and high astigmatism after
penetrating keratoplasty. J Cataract Refract Surg. 37:781–785.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Akcay L, Kaplan AT, Kandemir B, Gunaydin
NT and Dogan OK: Toric intraocular Collamer lens for high myopic
astigmatism after penetrating keratoplasty. J Cataract Refract
Surg. 35:2161–2163. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang J, Zhao J, Xu J and Zhang J:
Evaluation of the effectiveness of combined femtosecond
laser-assisted cataract surgery and femtosecond laser astigmatic
keratotomy in improving post-operative visual outcomes. BMC
Ophthalmol. 18:1612018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Buzzonetti L, Petrocelli G, Laborante A,
Mazzilli E, Gaspari M and Valente P: Arcuate keratotomy for high
postoperative keratoplasty astigmatism performed with the intralase
femtosecond laser. J Refract Surg. 25:709–714. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Çakır H, Genç S and Güler E: Circular
keratotomy combined with wedge resection in the management of high
astigmatism after penetrating keratoplasty. Eye Contact Lens.
25–June;2018.(Epub ahead of print). View Article : Google Scholar
|
|
14
|
Sy ME, Kovoor TA, Tannan A, Choi D, Deng
SX, Danesh J and Hamilton DR: Combined astigmatic keratotomy and
conductive keratoplasty to correct high corneal astigmatism. J
Cataract Refract Surg. 41:1050–1056. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wilkins MR, Mehta JS and Larkin DF:
Standardized arcuate keratotomy for postkeratoplasty astigmatism. J
Cataract Refract Surg. 31:297–301. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Weindler J, Pesch C, Hille K and Ruprecht
KW: Lateral corneoscleral 6-mm-incision for reduction of
against-the-rule astigmatism. Eur J Implant Ref Surg. 7:244–246.
1995. View Article : Google Scholar
|
|
17
|
Bachernegg A, Rückl T, Strohmaier C, Jell
G, Grabner G and Dexl AK: Vector analysis, rotational stability,
and visual outcome after implantation of a new aspheric toric IOL.
J Refract Surg. 31:513–520. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wade M, Steinert RF, Garg S, Farid M and
Gaster R: Results of toric intraocular lenses for post-penetrating
keratoplasty astigmatism. Ophthalmology. 121:771–777. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Iovieno A, Guglielmetti S, Capuano V,
Allan BD and Maurino V: Correction of postkeratoplasty ametropia in
keratoconus patients using a toric implantable Collamer lens. Eur J
Ophthalmol. 23:361–367. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wirbelauer C, Anders N, Pham DT and
Wollensak J: Effect of incision location on preoperative oblique
astigmatism after scleral tunnel incision. J Cataract Refract Surg.
23:365–371. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Heider W, Müller M, Schalnus R and Kaiser
P: Corneal topography after cataract surgery with tunnel incision
on a steeper meridian in inverse and oblique astigmatism.
Ophthalmologe. 94:16–19. 1997.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cleary C, Tang M, Ahmed H, Fox M and Huang
D: Beveled femtosecond laser astigmatic keratotomy for the
treatment of high astigmatism post-penetrating keratoplasty.
Cornea. 32:54–62. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fadlallah A, Mehanna C, Saragoussi JJ,
Chelala E, Amari B and Legeais JM: Safety and efficacy of
femtosecond laser-assisted arcuate keratotomy to treat irregular
astigmatism after penetrating keratoplasty. J Cataract Refract
Surg. 41:1168–1175. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Böhringer D, Dineva N, Maier P, Birnbaum
F, Kirschkamp T, Reinhard T and Eberwein P: Long-term follow-up of
astigmatic keratotomy for corneal astigmatism after penetrating
keratoplasty. Acta Ophthalmol. 94:e607–e611. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Donnenfeld ED, Kornstein HS, Amin A,
Speaker MD, Seedor JA, Sforza PD, Landrio LM and Perry HD: Laser in
situ keratomileusis for correction of myopia and astigmatism after
penetrating keratoplasty. Ophthalmology. 106:1966–1975. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Javadi MA, Feizi S, Yazdani S, Sharifi A
and Sajjadi H: Outcomes of augmented relaxing incisions for
postpenetrating keratoplasty astigmatism in keratoconus. Cornea.
28:280–284. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Day AC and Stevens JD: Predictors of
femtosecond laser intrastromal astigmatic keratotomy efficacy for
astigmatism management in cataract surgery. J Cataract Refract
Surg. 42:251–257. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kumar NL, Kaiserman I, Shehadeh-Mashor R,
Sansanayudh W, Ritenour R and Rootman DS: IntraLase-enabled
astigmatic keratotomy for post-keratoplasty astigmatism: on-axis
vector analysis. Ophthalmology. 117(1228–1235): e12010.
|
|
29
|
Fares U, Mokashi AA, Al-Aqaba MA, Otri AM,
Miri A and Dua HS: Management of postkeratoplasty astigmatism by
paired arcuate incisions with compression sutures. Br J Ophthalmol.
97:438–443. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Akura J, Matsuura K, Hatta S, Kaneda S and
Kadonosono K: Clinical application of full-arc, depth-dependent,
astigmatic keratotomy. Cornea. 20:839–843. 2001. View Article : Google Scholar : PubMed/NCBI
|