Introduction
Chronic venous insufficiency is a disease that
affects up to one third of the population, from young adults to the
elderly (1,2). Some studies (3) showed that if an active diagnostic
system is used, the condition can be seen in ~2/3 of the population
(1,3). There have been several suggested
definitions of this condition in order to encompass both the
classification and the line of treatment (1). Currently, the Comprehensive
Classification System for Chronic Venous Disorders (CEAP) is mostly
accepted by the specialists, even though there are plenty of
proposed improvements (1).
The venous insufficiency treatment of the lower
limbs is according to the stage of the disease. There are
efficiently proven methods such as liquid sclerotherapy and
long-pulsed neodymium ytrium:aluminium garnet laser (Nd:YAG) for
telangiectasias (4,5).
Sclerotherapy of the varicose veins of the lower
limbs is a medical procedure that consists of damaging the blood
wall (endothelium but also some other surrounding structures) by
injecting a certain chemical solution (6,7). This
leads to the sclerosis of the blood vessel, following the
destruction of the endothelium. Despite the fact that the
thrombosis is not the aim of this procedure, this phenomenon
happens in a certain percentage of the vessel that undergo
sclerotherapy (4).
The laser acts on the skin by converting absorbed
light energy in thermal energy that will intensely heat certain
cutaneous compounds called chromophores (5). They have different grades of light
absorption depending on the wavelength. Nd:YAG laser with a
wavelength of 1064 nm, acts mainly on haemoglobin and heats it
suddenly causing the destruction of the blood wall (8). The effect is almost instant, the
destruction of the endothelium and the surrounding structures being
seconded by vascular sclerosis and afterwards by remodelation, same
as in sclerotherapy.
The aim of our study was to evaluate the efficacy
and safety of hypertonic 20% saline/2% lignocaine (HS) versus
polidocanol (POL, 0.5%) versus Nd:YAG laser (LAS) in the treatment
of leg telangiectasias in women.
Patients and methods
During a period of 6 months, between September 2016
and February 2017 we included in this study 285 women (570 legs)
with primary leg telangiectasias and reticular veins
(C1AEpAS1PN) in order
to be treated with sclerotherapy or laser.
The study was conducted in accordance with the World
Medical Association Declaration of Helsinki and was approved by the
Institutional Ethics Committee of the Medical Center Dr. Ianosi
(no. ETIC 6/2016; Craiova, Romania). Informed written consent was
obtained from each patient.
Inclusion criteria aimed for patients over 18 with
primary leg telangiectasias up to 2 mm in diameter
(C1AEpAS1PN) as single
objective sign and those that accepted to enter the study signed
the informed consent form. We used dedicated scales that measured
vessels diameters between 1 and 10 mm.
Exclusion criteria were the following: i) Patients
with symptoms associated with telangiectasias (C1S); ii)
patients with superficial venous reflux assessed with Doppler
ultrasound of the lower limbs; iii) patients with deep venous
thrombosis or post-thrombotic syndrome (ES); iv)
pregnant or breastfeeding patients; and v) patients with neoplasms
or other systemic conditions or under chronic treatment for any
other disease.
The study group was divided in three equal groups of
190 lower limbs each: HS group was treated with hypertonic: 20%
saline/2% lignocaine, POL group with polidocanol: 0.5%
(Aetoxysklerol; Kreussler Inc., Wiesbaden, Germany) and LAS group
with Nd:YAG laser with a wavelength of 1064 nm (StarLux 500;
Palomar Technologies, Carlsbad, CA, USA) platform with a 3 mm spot,
pulse length of 30 msec and fluency between 290 and 350
J/cm2. The patient was included in the study as ‘first
come first served’ principle and each patient received different
treatment on the lower limbs. We randomised the type of the
treatment on each leg. There were two identical sessions at 60-day
interval. Assessment of vessel clearing and complications was
conducted at 60 and 120 days. Investigator's evaluation was made
using before and after photographs of the leg vessels using a
six-point scale: 0, no change; 1, 1–20% cleared; 2, 21–40% cleared;
3, 41–60% cleared; 4, 61–80% cleared; and 5, 81–100% cleared.
Aside from the major objective, comparative
evaluation of the efficacy of the sclerosing treatment (chemical or
thermal), we also followed the rate of the local complications
(burns, hypo- and hyperpigmentation, and thrombosis).
Statistical analysis
The data were introduced into Microsoft Excel for
transversal and longitudinal data statistical analysis. Numerical
variables were expressed as mean ± standard deviation (mean ± SD).
Proportions were always expressed as percentages. The χ2
test was used for determine if there is a significant relationship
between two variables. (significant difference between the expected
frequencies and the observed frequencies in one or more
categories). P<0.05 was considered to indicate a statistically
significant difference.
Statistical analysis of the treatment effects is a
procedure that helps to prove causality hypothesis and is specially
developed for comparing the effect of multiple treatments in
homogeneous group of patients with a given disease. The average
treatment effect was calculated among the treated and potential
outcome mean as measures of treatment effects.
The longitudinal data analysis included calculation
of incidence rates, statistical modelling using longitudinal
regression models and time-to-event analysis. Statistical modelling
used longitudinal regression models, namely random-effects ordered
logistic regression. By accounting for randomness of the treatment
outcome that is inherent to biological systems, the model can
better predict the chance for success of every treatment type,
compared with the usual transversely applied regression models
which ignore the time factor.
The time-to-event analysis (survival analysis) was
performed using the good/very good result as failure variable and
time to event expressed in whole months from the beginning of the
treatment. This produced hazard ratios which can be assimilated to
risk ratios (RR) in the transverse analysis and which can be used
to compare treatment success rates per unit of time, so in the
future the patients can make informed decisions on the type of
treatment outcomes and time required.
Results
Forty-one of 285 patients (82 legs) could not be
followed till the end of the study. Only 244 patients (488 legs)
were evaluated during both visits (after 60 and 120 days). After
the last visit there were 169 legs in the POL group, 154 in HS
group and 165 in LAS group.
There were no deaths or major complications (deep
venous thrombosis, severe burns or ischemic complications)
reported. The minor complications were represented by cutaneous
burns (on 14 legs) and 31 hyperpigmentation with no statistic
correlation.
At the end of all the two sessions of treatment, of
the 488 legs, 123 had a moderate overall result, 360 had good and
very good overall results (4 and 5 on our clearance scale), and 5
had a limited modest results (3 in our scale). Very good results
were encountered in 72 (43.63%) of 165 legs treated with LAS and
good results were encountered in 74 (44.84%) legs. There were very
good results in 19 (11.24%) of 169 legs treated with POL and good
results in 97 (57.39%). Very good results were encountered in 15
(9.74%) of 154 legs treated with HS and good results were
encountered in 83 (53.89%) (Table
II).
 | Table II.Results of the treatments at the
second evaluation - 120 days. |
Table II.
Results of the treatments at the
second evaluation - 120 days.
|
|
|
|
|
|
| χ2 test
(vs. HS) | Multivariate
regression | Treatment effect
analysis | Survival
analysis |
|---|
|
|
|
|
|
|
|
|
|
|
|
|---|
| Treatment | Very good (%) | Good (%) | Moderate (%) | Limited/modest
(%) | Failure (%) | Risk ratio | P-value | Odds ratio | P-value | ATET | PO mean | P-value | Hazard ratio | P-value |
|---|
| Global |
|
LAS | 72 (43.63) | 74 (44.84) | 19 (11.51) | 0 (0) | 0 (0) | 8.09 | <0.001 | 14.72 | <0.001
4.56E-31 | 0.313 | 0.347 | <0.001 | 5.96 | <0.001
1.62E-09 |
|
POL | 19 (11.24) | 97 (57.39) | 50 (29.58) | 3 (1.77) | 0 (0) | 1.16 | 0.122407 | 2.21 | 0.028 | 0.343 | 0.440 | <0.001 | 1.97 | 0.472 |
| HS | 15 (9.74) | 83 (53.89) | 54 (35.06) | 2 (1.29) | 0 (0) | – | – | – | – | – | – | – | 1 | – |
| Diameter <1
mm |
|
LAS | 51 (62.96) | 26 (32.09) | 4 (4.94) | 0 (0) | 0 (0) | 9.72 | <0.001 | 10.34 | <0.001
2.7E-15 | 0.574 | 0.341 | <0.001 | 4.48 | <0.001
6.35E-14 |
|
POL | 4 (4.49) | 43 (48.31) | 39 (43.82) | 3 (3.37) | 0 (0) | 1.65 | 0.21 | 6.98 | <0.001
1.96E-09 | 0.327 | 0.110 | <0.001 | 5.66 | 0.44 |
| HS | 3 (4.54) | 36 (54.54) | 26 (39.39) | 1 (1.52) | 0 (0) | – | – | – | – | – | – | – | 1 | – |
| Diameter >1
mm |
|
LAS | 21 (25) | 48 (57.14) | 15 (17.86) | 0 (0) | 0 (0) | 2.70 | 0.003 | 9.22 | <0.001
2.55E-14 | 0.385 | 0.470 | <0.001 | 3.97 | 0.047 |
|
POL | 15 (18.75) | 54 (67.5) | 11 (13.75) | 0 (0) | 0 (0) | 1.44 | 0.00756 | 2.92 | 0.00457 | 0.370 | 0.281 | 0.041 | 4.96 | 0.486 |
| HS | 12 (13.63) | 47 (53.4) | 28 (31.81) | 1 (1.14) | 0 (0) | – | – | – | – | – | – | – | 1 | – |
Comparing the good and very good results of LAS vs.
HS, it was observed that for telangiectasias under 1 mm occurred in
95.05% of patients treated with LAS vs. 59.08% of patients treated
with HS (RR=9.72, P<0.001). In the case of telangiectasias over
1 mm diameter, good and very good results occurred in 82.14% of
patients treated with LAS vs. 67.03% of patients treated with HS
(RR=2.70; P=0.003). The same comparison between POL vs. HS showed
for telangiectasias under 1 mm diameter, 52.80% of legs treated
with POL vs. 59.08% of legs treated with HS (RR=1.65; P=0.21). For
telangiectasias over 1 mm diameter good and very good results
occurred in 86.25% of legs treated with POL vs. 67.03% of legs
treated with HS (RR=1.44, P=0.00756) (Table II). At the first evaluation (at 60
days) results showed better results for POL vs. HS for
telangiectasias over 1 mm comparing with LAS vs. HS (RR=3.57,
P<0.001 comparing with RR=1.51, P=0.066) (Table I). The same evaluation for
telangiectasias under 1 mm showed a better efficacy for LAS
(RR=1.94, P<0.001 comparing with RR=1.65, P=0.177) (Table I).
 | Table I.Results of the treatments at the first
evaluation - 60 days. |
Table I.
Results of the treatments at the first
evaluation - 60 days.
|
|
|
|
|
|
| χ2 test
(vs. HS) | Multivariate
regression | Treatment effect
analysis | Survival
analysis |
|---|
|
|
|
|
|
|
|
|
|
|
|
|---|
| Treatment | Very good (%) | Good (%) | Moderate (%) | Limited/modest
(%) | Failure (%) | Risk ratio | P-value | Odds ratio | P-value | ATET | PO mean | P-value | Hazard ratio | P-value |
|---|
| Global |
| LAS | 0 (0) | 85 (51.51) | 68 (41.21) | 12 (7.27) | 0 (0) | 4.59 | <0.001 | 14.32 | <0.001
5.41E-30 | 0.102 | 0.251 | <0.001 | 2.13 | 0.017 |
| POL | 0 (0) | 61 (36.09) | 78 (46.15) | 30 (17.75) | 0 (0) | 1.65 | 0.193 | 11.32 | <0.001
6.11E-22 | 0.015 | 0.133 | <0.001 | 1.65 | 0.22 |
| HS | 0 (0) | 43 (27.92) | 85 (55.19) | 26 (16.88) | 0 (0) | – | – | – | – | – | – | – | 1 | – |
| Diameter <1
mm |
| LAS | 0 (0) | 54 (66.67) | 23 (28.39) | 4 (4.94) | 0 (0) | 1.94 | <0.001 | 10.71 | <0.001
6.16E-16 | 0.316 | 0.226 | <0.001 | 3.25 | 0.000127 |
| POL | 0 (0) | 13 (14.60) | 51 (57.30) | 25 (28.09) | 0 (0) | 1.51 | 0.066 | 6.665 | <0.001
7.17E-09 | 0.723 | 0.214 | <0.001 | 1.66 | 0.118683 |
| HS | 0 (0) | 14 (21.21) | 39 (59.09) | 13 (19.7) | 0 (0) | – | – | – | – | – | – | – | 1 | – |
| Diameter >1
mm |
| LAS | 0 (0) | 31 (36.90) | 45 (53.57) | 8 (9.52) | 0 (0) | 1.65 | 0.177 | 8.42 | <0.001
1.02E-12 | 0.727 | 0.079 | <0.001 | 3.44 | 0.02776 |
|
POL | 0 (0) | 48 (60) | 27 (33.75) | 5 (6.25) | 0 (0) | 3.57 | 0.000232 | 8.89 | <0.001
1.73E-13 | 0.585 | 0.165 | <0.001 | 1.51 | 0.182 |
| HS | 0 (0) | 29 (32.95) | 46 (52.27) | 13 (14.77) | 0 (0) | – | – | – | – | – | – | – | 1 | – |
The results of the treatment effect analysis showed
that in the treatment of telangiectasias under 1 mm, LAS treatment
had a higher potential outcome (PO) mean than POL treatment (0.341
vs. 0.110), whereas in telangiectasias over 1 mm, LAS treatment had
also a higher PO mean than the POL treatment (0.470 vs. 0.281)
(Table II).
Multivariate analysis compared the effect of
applying the three types of treatments to the chance of obtaining a
good result (separately for under and over 1 mm telangiectasias).
For telangiectasias under 1 mm LAS treatment had an OR of 10.34
(P<0.001) and POL treatment of 6.98 (P<0.001) vs. HS
treatment comparing with telangiectasias over 1 mm in which LAS had
an OR of 9.22 (P<0.001) and the POL of 2.92 (P<0.00457)
compared to HS treatment (Table
II).
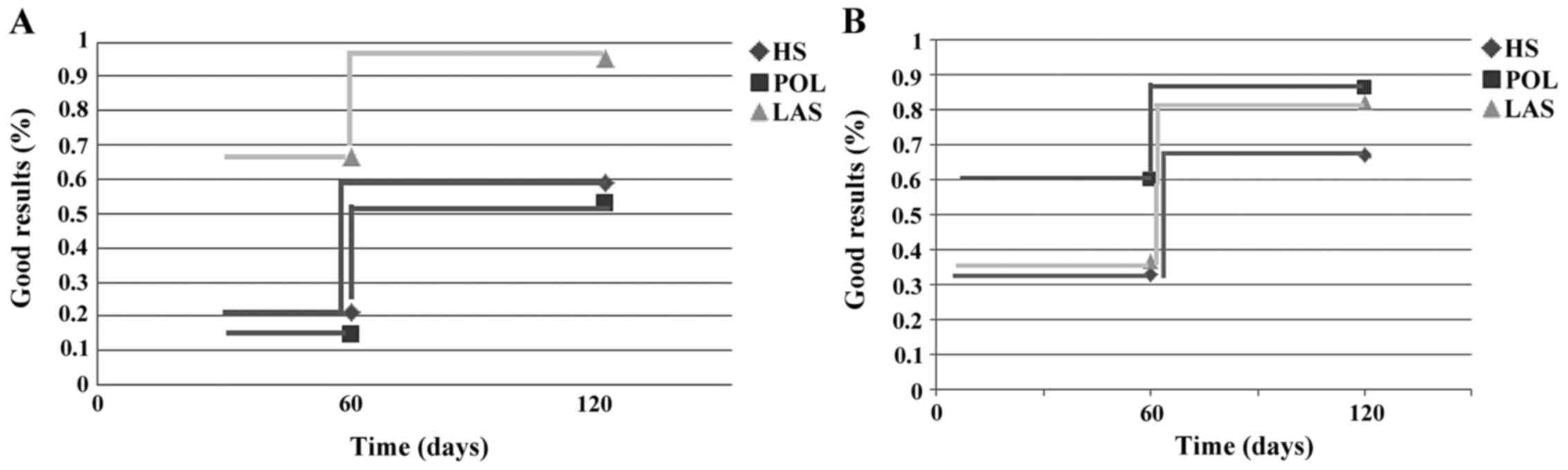
The longitudinal data analysis of the result showed
that, for telangiectasias under 1 mm, the good and very good
results of LAS treatment occurred from the first treatment in 54
legs (66.67%), and after the second in 77 legs (95.05%), while for
the POL treatment the results were 13 (14.60%) and 47 legs
(52.80%). HS treatment achieved good results in 14 legs (21.21%) in
the first treatment and 40 legs after the second session (59.08%)
(Table III).
 | Table III.Longitudinal data analysis for good
and very good results. |
Table III.
Longitudinal data analysis for good
and very good results.
| Treatment | 60 days (%) | 120 days (%) |
|---|
| Diameter <1
mm |
|
LAS | 54 (66.67) | 77 (95.05) |
|
POL | 13 (14.60) | 47 (52.80) |
| HS | 14 (21.21) | 40 (59.08) |
| Diameter >1
mm |
|
LAS | 31 (36.90) | 69 (82.14) |
|
POL | 48 (60.00) | 69 (86.25) |
| HS | 29 (32.95) | 59 (67.03) |
The hazard regression model showed a hazard ratio of
4.48 (P<0.001) for LAS and 5.66 (P=0.44) for POL. For
telangiectasias under 1 mm LAS treatment is clearly superior to POL
treatment, the latter having an insignificant coefficient. For
telangiectasias over 1 mm the good and very good results of LAS
treatment occurred after first session in 31 legs (36.90%), and
after the second in 69 legs (82.14%), while for the POL treatment,
good and very good results occurred in 48 legs (60.00%),
respectively in 69 legs (86.25%). HS treatment achieved good
results in 29 legs (32.95%), respectively in 59 legs (67.03%)
(Table III).
The hazard regression model showed a hazard ratio of
3.97 (P=0.047) for the LAS and 4.96 (P=0.486) for POL vs. HS
treatment. We can conclude, for telangiectasias over 1 mm that a
superiority of POL vs. LAS in terms of achieving good treatment
results could not be demonstrated. Both types of treatments were
well superior to HS treatment (Table
II and Fig. 1).
In our study, for telangiectasias under 1 mm, the
LAS treatment determined a healing rate (telangiectasias
disappearance) of 14.72 times higher than HS (P<0.001), while
the POL treatment produced a healing rate of 11.32 times higher
than HS (P<0.001).
Discussion
According to International Union of Phlebology,
sclerotherapy represent an absolute indication in the treatment of
telangiectasias and reticular veins (5,9,10). If for larger blood vessel, foam
sclerotherapy is more efficient, for telangiectasias liquid
sclerotherapy is the best therapeutic choice (5,10). In
non-occlusive or premature recanalisation of the treated veins it
may require several session of therapy (10). Several substances have been used for
sclerotherapy. The main purpose being the destruction of the venous
wall.
Hypertonic saline solution was the first option for
this method, but nowadays it is used rarely due to discovery of
more effective substances. The polidocanol (Lauromacrogol 400) is a
non-ionic detergent but also with local anaesthetic action
(11). This substance produces a
chemical burn located at the injection site, in the endothelium of
the vessel. The process is due to solubilisation of the lipoprotein
compounds of the venous wall. The results are local inflammatory
reaction followed by fibrosis, processes responsible for a complete
closure of the injected vessel within 6–7 weeks. This way, the
vessel is excluded from the blood circuit, bringing improvement of
the symptoms caused by the varicose veins. Later on, the remodeling
process will generate a good aesthetic outcome according to a
minimal invasive treatment. The maximum accepted dosage is 2
mg/kg/day (5). Currently, there are
available on the market polidocanol ampoules of 0.25, 0,5, 1, 2 and
3%. The substance is administered intravenous, at the venous site,
the concentration of it being chosen directly proportional with the
vessel diameter (10,11). Usually, the treatment of the
telangiectasias and the reticular veins requires low concentrations
of polidocanol, respectively 0.25%, or 0.5%, eventually even 1%,
but in some cases, higher concentrations can be used.
In our study, the group treated with saline solution
was considered the reference group. We noted, similar results to
polidocanol when treating telangiectasias smaller than 1 mm in
diameter but an increased efficacy for polidocanol in case of
larger vessels. The result can be explained by the fact that while
for the very thin vessels, sclerotherapy is slightly inferior to
laser treatment, the difference in efficacy between the 2 methods
is extremely low so both are equivalent. For telangiectasias larger
than 1 mm in diameter, where the best choice is sclerotherapy, the
difference between polidocanol and saline solution is bigger as
seen also in our study.
The current trend in modern medicine is to use when
possible, minimal invasive treatment methods and with speedy
recovery. While laser and intense pulse light became more popular
in acne treatment or in many other skin diseases (12), these methods play the same role in
treatment of telangiectasias of the lower limbs with certain
criteria that limits the usage of sclerotherapy: telangiectasias on
areas that had undergone surgery (telangiectatic matting,
angiogenic flushing), vessel resistant to sclerotherapy, the
impossibility of the catheterisation, needle-phobia and areas with
increased risk of hyperpigmentation (13).
The minimal requirements of a laser used for
treatment of telangiectasias are (13): i) a wavelength that is better
absorbed by the haemoglobin in comparison with the surrounding
chromophores; ii) the capacity for a deep penetration towards the
vascular target; and iii) the capacity to transmit enough energy in
order to be able to destroy the target, but without damaging the
adjacent tissues. Different types of cooling devices have been
developed for the skin surface that allow a higher transmission of
the energy for a pan-endothelial destruction while reducing the
negative effects of the skin. On the other hand, the cooling degree
of the skin depends of the prototype, the lighter ones (Fitzpatrick
I and II) needing more cooling time in comparison to darker skin
(Fitzpatrick V and VI). Furthermore, the cooling systems decrease
the pain, laser treatment being painful.
The 1064 nm wavelength of Nd:YAG laser is
responsible for, on the one hand, an adequate absorption at the
blood vessel levels (where haemoglobin is the main chromophore)
and, on the other hand, a deeper penetration through the skin in
comparison to shorter wavelengths and so being able to penetrate
dermal and subdermal vessels. Moreover, it benefits from a low
absorption of melanin and therefore it is suitable for treating a
large variety of photo types (darker included) with decrease risk
of depigmentation at the treated site. Due to all its features,
Nd:YAG laser represents the best choice for treatment of the
telangiectasias of the lower limbs (14).
We must differentiate the small red telangiectasias,
that are superficial and contain a larger quantity of oxygenated
haemoglobin and the blue-violaceous one, usually thicker, with
lower amount of oxyhaemoglobin. If for the former we need high
fluencies (350–600 J/cm2), short pulse duration (15–30
msec) and small spot size (<2 mm), for the latter larger spot
size (2–6 mm) is recommended, lower fluencies (100–350
J/cm2) and longer duration if the pulse is 30–50 msec
(15). We mentioned above the
characteristics of the light spot we used in our study.
Sclerotherapy associated with laser may result in
better outcome in selected cases. The literature shows numerous
studies regarding the efficacy of different concentrations of
polidocanol in treatment of varicose veins of the lower limbs
(10). In our study we used
hypertone saline solution in a number of cases considered as
reference compared with other methods (5,16,17).
An interesting study assessed Polidocanol 0.5%, 1%,
sodium tetradecyl sulphate (STS) 1% and placebo in treatment of
varicose veins C1 (18). The study
permitted to repeat twice the injections at 3-week interval and
also thrombectomy was accepted for a good aesthetic result. The
efficacy of polidocanol was proven in comparison to placebo (93.6%
at 0.5% vs. 97.4% at 1%) with a slight advantage to STS (96.3%). In
our single-blind study, laser was a variable. We chose not to
perform thrombectomy, in order to maintain equal condition for both
sclerotherapy and laser. Moreover, thrombectomy is rarely used for
telangiectasias treatment.
There are plenty of studies that have assessed
liquid sclerotherapy vs. foam (10,19). The
results are significantly better for foam in varicose veins
(C2), but in telangiectasias treatment the results are
similar, statistically insignificant. In our study we used liquid
form for both polidocanol and saline solution.
Complications are rare for laser and also for
sclerotherapy. We refer to ulcerations that can occur after usage
of both methods to treat telangiectasias. After sclerotherapy,
ulcerations appear following perivascular injection (16). It is mandatory that the physician
makes sure to inject intravascularly because perivascular
penetration of the substance can lead to local necrosis or
ulcerations, mainly in hypoderm reduced areas, near the bone
structures. In most cases, perivascular injection determines local
pain while the correct sclerotherapy, intravascularly, is painless.
During laser treatment, ulcerations can develop due to the tendency
of the physician to retreat the same areas either due to lack of
immediate expected results, or to inappropriate adjustment of the
fluency in the nearby bone areas (13). In our case, the rate of local
complications was minimal and there was no need for complementary
treatment, with spontaneous remission in all the patients. We must
remember that sun protection is critical for a good aesthetic
outcome.
After Nd:YAG laser, pain as short burn can develop
immediately postoperative. Normally, analgesics are not needed. The
immediate aesthetic results are impressive, small vessels
(especially the violaceous ones) disappear completely, being
visible also during the treatment session. Larger blue vessels can
become darker in colour, postoperative but it will fade out in the
following weeks. Sometimes, another laser session is needed on
these vessels but not sooner than 2 months after the first
treatment. Taking this into account, our study encompassed 2
visits, at 2-month interval, for both laser and sclerotherapy.
After laser treatment, the edema is usually minimal
and lasts a few days. Also, erythema is present for 2–3 weeks
depending on the fluency and the sensitivity of the area of the
lower limbs. While compression stocking role after sclerotherapy is
certain, after Nd:YAG laser this is, most of the times, not
recommended. Usually it is advised to apply hydrating creams and
cold compresses during the first days after the treatment. We did
not use compression post sclerotherapy to maintain a balance
between the two methods and due to lack of recommendations for
compression after sclerotherapy of the small vessels (such as
telangiectasias) (10).
Hyperpigmentation after Nd:YAG laser is rare.
Theoretically, hypopigmentation can occur because of the light
absorption by the melanin, but normally the phenomenon is reduced
so the depigmentation risk is also low.
In conclusion, telangiectasias and reticular veins
of the lower extremities can be successfully treated with Nd:YAG
laser or sclerotherapy with polidocanol. Nd:YAG laser is
recommended for treatment of small telangiectasias, less than 1 mm
in diameter, while sclerotherapy with polidocanol is more efficient
as the dimensions of the vessels grow.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GI, SI, MXCP and DN contributed to the conception
and design of the study, acquisition, analysis and interpretation
of the data. CT and DC were responsible for the design, analysis of
the data and critical revision of the study for important
intellectual content. All authors read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
The study was conducted in accordance with the World
Medical Association Declaration of Helsinki and approved by the
Institutional Ethics Committee of the Medical Center Dr. Ianosi
(no. ETIC 6/2016; Craiova, Romania), and informed written consent
was obtained from each patient.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Van der Velden SK, Shadid NH, Nelemans PJ
and Sommer A: How specific are venous symptoms for diagnosis of
chronic venous disease? Phlebology. 29:580–586. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tudoraşcu I, Sfredel V, Riza AL, Miulescu
Dănciulescu R, Ianoşi SL and Dănoiu S: Motor unit changes in normal
aging: A brief review. Rom J Morphol Embryol. 55:1295–1301.
2014.PubMed/NCBI
|
|
3
|
Breu FX and Wollmann JC: Clinical and
technical follow-up after sclerotherapy. Dermatol Surg. 36 Suppl
2:1004–1009. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Heck M, Faulhaber J, Breu FX and Schneider
SW: Foam sclerotherapy. Uses and indications in dermatology and
phlebology. Hautarzt. 63:493–505. 2012.(In German).
|
|
5
|
Perrin M, Eklof B, VAN Rij A, Labropoulos
N, Vasquez M, Nicolaides A, Blattler W, Bouhassira D, Bouskela E,
Carpentier P, et al: Venous symptoms: The SYM Vein Consensus
statement developed under the auspices of the European Venous
Forum. Int Angiol. 35:374–398. 2016.PubMed/NCBI
|
|
6
|
Hamel-Desnos C, Ouvry P, Benigni JP,
Boitelle G, Schadeck M, Desnos P and Allaert FA: Comparison of 1%
and 3% polidocanol foam in ultrasound guided sclerotherapy of the
great saphenous vein: A randomised, double-blind trial with 2 year
follow-up. ‘The 3/1 Study’. Eur J Vasc Endovasc Surg. 34:723–730.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen CH, Chiu CS and Yang CH:
Ultrasound-guided foam sclerotherapy for treating incompetent great
saphenous veins - results of 5 years of analysis and morphologic
evolvement study. Dermatol Surg. 38:851–857. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Prieto V, Zhang P and Sadick NS:
Comparison of a combination diode laser and radiofrequency device
(Polaris) and a long-pulsed 1064-nm Nd:YAG laser (Lyra) on leg
telangiectases. Histologic and immunohistochemical analysis. J
Cosmet Laser Ther. 8:191–195. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Caruntu C, Negrei C, Boda D, Constantin C,
Caruntu A and Neagu M: Biotechnological advances for diagnosis of
peripheral diabetic neuropathy. Rom Biotech Lett. 19:9846–9858.
2014.
|
|
10
|
Breu FX, Guggenbichler S and Wollmann JC:
2nd European Consensus Meeting on foam sclerotherapy 2006,
Tegernsee, Germany. Vasa. 37 Suppl 71:1–29. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Goldman MP, Guex JJ and Weiss RA:
Sclerotherapy. Treatment of Varicose and Telangiectatic Leg Veins.
5th. Saunders; Philadelphia: pp. 1–416. 2011
|
|
12
|
Ianosi S, Neagoe D, Calbureanu M and
Ianosi G: Investigator-blind, placebo-controlled, randomized
comparative study on combined vacuum and intense pulsed light
versus intense pulsed light devices in both comedonal and
papulopustular acne. J Cosmet Laser Ther. 15:248–254. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nijsten T, van den Bos RR, Goldman MP,
Kockaert MA, Proebstle TM, Rabe E, Sadick NS, Weiss RA and Neumann
MH: Minimally invasive techniques in the treatment of saphenous
varicose veins. J Am Acad Dermatol. 60:110–119. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Guex JJ, Schliephake DE, Otto J, Mako S
and Allaert FA: The French polidocanol study on long-term side
effects: A survey covering 3,357 patient years. Dermatol Surg. 36
Suppl 2:993–1003. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sadick NS: Laser treatment of leg veins.
Skin Therapy Lett. 9:6–9. 2004.PubMed/NCBI
|
|
16
|
Rabe E, Breu FX, Cavezzi A, Coleridge
Smith P, Frullini A, Gillet JL, Guex JJ, Hamel-Desnos C, Kern P,
Partsch B, et al: Guideline Group: European guidelines for
sclerotherapy in chronic venous disorders. Phlebology. 29:338–354.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Branisteanu DE, Nichifor M, Dorobat CM,
Branisteanu DC, Petrariu FD, Molodoi AD, Radu DC and Boda D: Use of
textile biomaterials for the topic treatment of chronic venous
disease. Rom Biotechnol Lett. 20:10618–10625. 2015.
|
|
18
|
Rabe E, Schliephake D, Otto J, Breu FX and
Pannier F: Sclerotherapy of telangiectases and reticular veins: A
double-blind, randomized, comparative clinical trial of
polidocanol, sodium tetradecyl sulphate and isotonic saline (EASI
study). Phlebology. 25:124–131. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Uncu H: Sclerotherapy: A study comparing
polidocanol in foam and liquid form. Phlebology. 25:44–49. 2010.
View Article : Google Scholar : PubMed/NCBI
|