Introduction
Congenital skeletal abnormalities are common
conditions that can generally be surgically corrected in the first
few months of life or during childhood (1). The incidence of congenital cardiac
abnormalities is increased in patients with congenital scoliosis
compared to the general population (1,2).
Therefore, the presence of congenital scoliosis imposes a detailed
echocardiographic assessment (1,2). Atrial
septal defects (ASDs) account for 7–10% of all congenital heart
diseases (CHDs) in children and is found in 13% of patients with
congenital scoliosis (3,4). If untreated, ASDs are associated with a
significant risk for atrial arrhythmias and cardiovascular
morbidity. Closure of hemodynamically significant defects is, thus,
advised (3). Although surgery
continues to be the gold standard therapy, percutaneous ASD closure
has increased in use and has comparable outcomes (3,4).
We present the case of an 11-year-old girl with a
complex chest wall deformity who was scheduled for surgical
correction of severe congenital scoliosis. Preoperative clinical
and echocardiographic evaluation showed the presence of a large
ostium secundum ASD with a significant left-to-right shunt which
required closure prior to orthopedic surgery for the skeletal
disease. Percutaneous implantation of a dedicated device was
preferred over surgical intervention due to the chest deformity and
the pulmonary restrictive disease.
Case report
An 11-year-old girl with complex thoracic skeletal
deformity, congenital scoliosis, and pectus carinatum (Fig. 1A) was referred for cardiovascular
assessment prior to surgical correction of the spinal defect. Her
weight was 15 kg and her height was 109 cm, with a body mass index
of 12.6 kg/m2. Cardiac examination revealed fixed
splitting of the 2nd heart sound, no heart murmurs, a blood
pressure of 120/70 mmHg, and a heart rate of 70 beats/min. Physical
exam was otherwise unremarkable, with the exception of the spinal
deformity. Spirometry revealed severe restrictive pulmonary
dysfunction with a vital capacity at 26% of predicted value.
Routine blood tests were normal, with normal kidney and liver
function.
An electrocardiogram showed sinus rhythm with
‘pulmonary’ P waves and left axis deviation (due to intrathoracic
cardiac orientation) (Fig. 1B). A
transthoracic echocardiogram (TTE) revealed a 14-mm ostium secundum
ASD, left-to-right shunting (Fig.
1C), and a ratio of pulmonary blood flow to systemic blood flow
(Qp/Qs) of 3.18 (Fig. 1D). The right
cardiac chambers were mildly dilated. Estimated pulmonary artery
pressure was normal (25 mmHg). There were no structural changes of
the left cardiac chambers or valves and left ventricular ejection
fraction was normal. A transesophageal echocardiogram (TEE) was
performed; ASD diameter was measured at 14 mm and septal length at
34 mm. The defect was located in the central atrial septum and all
the muscular rims were >5 mm.
Percutaneous treatment of the ASD was the preferred
treatment approach, given the high surgical risk in a cachectic
patient with severe restrictive pulmonary dysfunction. All the
criteria for percutaneous ASD closure were met (3). The Figulla Flex II (Occlutech GmbH,
Jena, Germany) device was chosen, due to its good flexibility and
our previous experience. A 16.5 mm device was considered
appropriate based on TEE assessment.
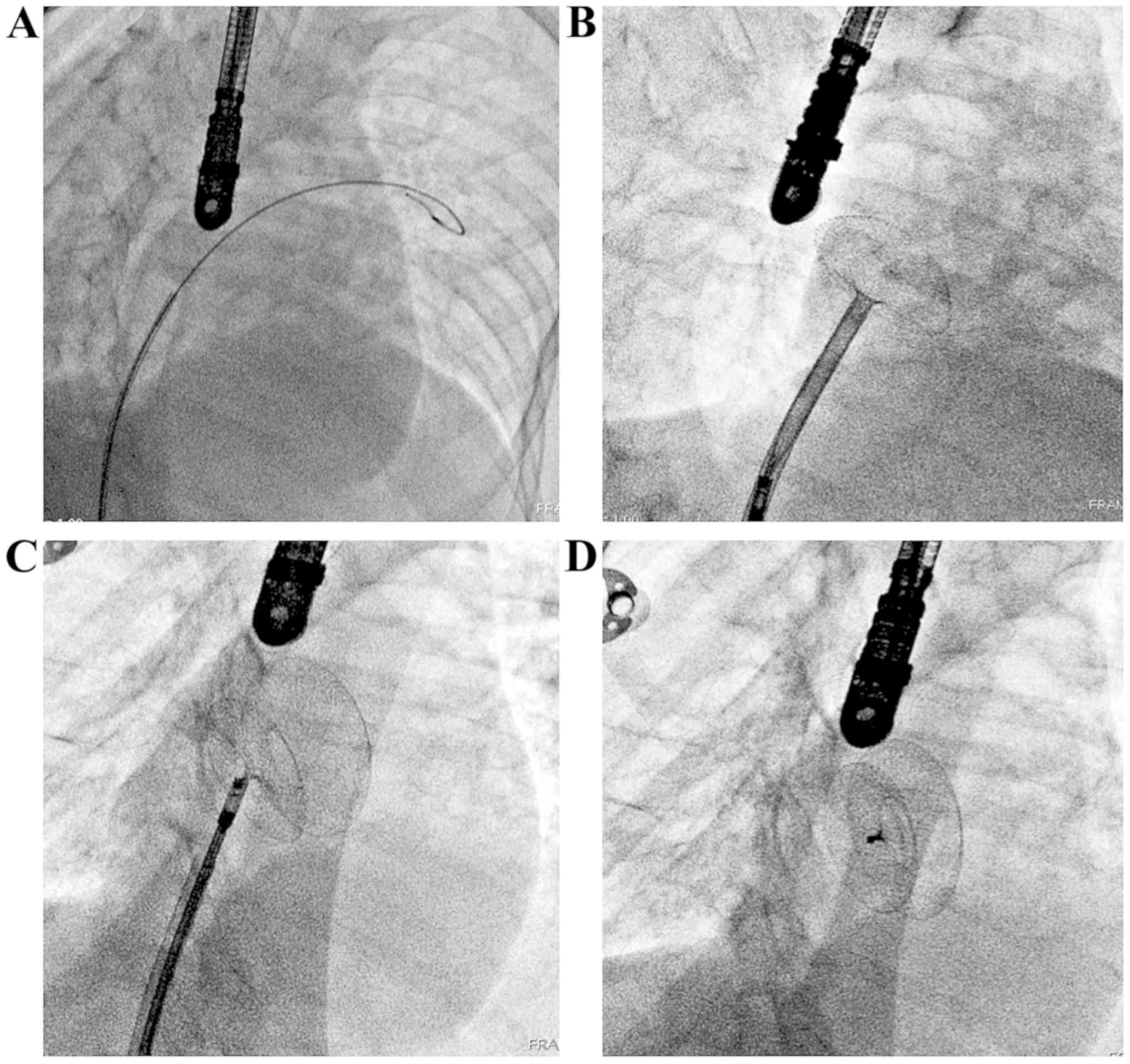
The intervention was performed in the
catheterization laboratory under general anesthesia with
orotracheal intubation and mechanical ventilation. The procedure
was guided by multiplane transesophageal echocardiography. The
right femoral vein was punctured and a 6F sheath was inserted. A 6F
MP1 catheter was advanced via a 0.035 inch, 180 cm long guidewire
through the atrial septal defect into the left atrium and then
further into the left upper pulmonary vein. The standard
antero-posterior angiographic view was modified in order to adjust
for the intrathoracic cardiac orientation secondary to the chest
wall anomaly; therefore, the proper working projection was left
anterior oblique 30° (Fig. 2A). The
0.035-inch guidewire was exchanged for a 0.035 inch 260 cm long
Occlutech stiff guidewire (Fig. 2A)
which allowed for the exchange of the 6F sheath with a long
dedicated introducer-sheath with the tip placed in the left atrium.
The 16.5 mm Figulla Flex II device was advanced through the
introducer sheath and the left disk was released into the left
atrium after gentle clockwise rotation of the introducer-sheath.
The introducer sheath and the device were pulled against the atrial
septum until the apposition of the left disc on the septum was
obtained and then the right disc was released into the right atrium
(Fig. 2B and 2C). After verifying for good stability and
apposition, the device was released (Fig. 2D) with good final procedural results.
Complete exclusion of the ASD and no residual shunting on TEE. The
patient was transferred to the postoperative intensive care unit
where she was extubated. She was soon transferred to the inpatient
unit where she was kept under surveillance for 2 more days. TTE at
discharge showed no residual shunt. The patient was treated with
aspirin 75 mg once daily for 6 months following the procedure.
Surgical correction of the spinal deformity was performed 6 months
after the procedure without complications. The patient was in good
health at 2.5 year follow-up.
Discussion
Our case report describes the association of a major
skeletal birth defect (congenital dextroscoliosis and pectus
carinatum) with one of the most frequent congenital heart diseases
(ostium secundum type ASD). Craniofacial and skeletal abnormalities
are often associated with congenital heart disease (1,2). This
observation has important clinical consequences, as these patients
often require extensive evaluation and carefully selected treatment
strategies.
Although the clinical association between
kyphoscoliosis and congenital heart defects is well recognized
(1,2), few large-scale epidemiological studies
have addressed this issue. In adolescent idiopathic scoliosis, the
prevalence of structural cardiac abnormalities ranges between
3.6–17.5% (5,6). A retrospective cohort of mixed
congenital spinal deformities reports 14.1–26% prevalence of
structural cardiac abnormalities (7,8) in
patients with congenital scoliosis. The authors also report that
congenital kyphosis is more frequently associated with heart
defects. The prevalence of ASD in patients with congenital
scoliosis ranges between 2.5% (7)
and 13% (4); a prevalence of 8.75%
is reported in a study addressing idiopathic scoliosis (6). As a consequence, some experts recommend
routine echocardiographic screening for congenital heart disease in
patients with congenital kyphoscoliosis (1,2,5,8).
To the best of our knowledge, there are only a few
articles in the literature presenting cases of percutaneous ASD
closure in patients with severe congenital scoliosis (9,10). The
chest anatomy of patients with scoliosis imposes technical
difficulties with performing endovascular procedures. The position
of the C-arm needs to be adapted to compensate for the
intrathoracic cardiac orientation. A 30° left anterior oblique
projection was chosen to advance the guidewire in the left superior
pulmonary vein and for the proper positioning of the long
introducer sheath. The introducer sheath needed to be turned
clockwise in order to obtain a good alignment and to minimize the
tension in the device during its release. This ensured that the
device was properly positioned with a minimum risk of slippage of
the left disk into the right atrium during release. After verifying
for correct positioning with TEE and stability check with push-pull
maneuver, the device was safely released and TEE demonstrated
complete closure of the atrial septal device with no residual
shunt.
A comprehensive clinical and echocardiographic
evaluation is needed in patients with skeletal abnormalities in
order to screen for associated congenital heart defects. The
current treatment of choice for most ASDs is percutaneous closure
with dedicated devices. In the case of simultaneous ASD and
kyphoscoliosis, special consideration should be given to the
intrathoracic cardiac orientation. A modified cath lab protocol is
imposed, including adaptation of the angiographic working
projection, the correct alignment of the long introducer-sheath,
and the release time of the occluder device. Percutaneous
techniques can be successfully performed in patients with ASD and
secondary restrictive pulmonary disease, despite challenging
anatomy due to severe chest wall deformity. This approach should,
therefore, be preferred over surgical closure.
Acknowledgements
The authors would like to acknowledge Antonela
Muresan, Department of Anesthesiology, Cardiopediatric Center,
Monza Hospital (Bucharest, Romania), and Dana Constantinescu,
Department of Cardiology, Monza Hospital (Bucharest, Romania), who
were part of the team treating and caring for this patient and
contributed to data collection.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
AL, ARB, EO, DVB and SMB contributed to drafting and
writing the manuscript. AL, EO and SMB were involved in the care of
patient. ARB and DVB contributed to the organization, analysis and
interpretation of data. VCB, ED, and MB were involved in the
critical revision of the manuscript, the organization of data, the
gathering and the image formation. SMB coordinated the group and
the preparation of this manuscript. All authors read and approved
the final version of the manuscript.
Ethics approval and consent to
participate
The need for Ethics approval was waived as this is a
report of clinical practice and does not constitute biomedical
research. Reporting is consistent with all ethical
requirements.
Patient consent for publication
Informed consent was obtained from the patient's
family. All identifying information was removed from this
manuscript.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ASD
|
atrial septal defect
|
|
CHD
|
congenital heart disease
|
|
Qp/Qs
|
pulmonary blood flow to systemic blood
flow ratio
|
|
TEE
|
transesophageal echocardiogram
|
|
TTE
|
transthoracic echocardiogram
|
References
|
1
|
Tikoo A, Kothari MK, Shah K and Nene A:
Current concepts congenital scoliosis. Open Orthop J. 11:337–345.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bozcali E, Ucpunar H, Sevencan A, Balioglu
MB, Albayrak A and Polat V: A retrospective study of congenital
cardiac abnormality associated with scoliosis. Asian Spine J.
10:226–230. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kazmouz S, Kenny D, Cao QL, Kavinsky CJ
and Hijazi ZM: Transcatheter closure of secundum atrial septal
defects. J Invasive Cardiol. 25:257–264. 2013.PubMed/NCBI
|
|
4
|
Vasquez AF and Lasala JM: Atrial septal
defect closure. Cardiol Clin. 31:385–400. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ipp L, Flynn P, Blanco J, Green D,
Boachie-Adjei O, Kozich J, Chan G, Denneen J and Widmann R: The
findings of preoperative cardiac screening studies in adolescent
idiopathic scoliosis. J Pediatr Orthop. 31:764–766. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu L, Xiu P, Li Q, Song Y, Chen R and
Zhou C: Prevalence of cardiac dysfunction and abnormalities in
patients with adolescent idiopathic scoliosis requiring surgery.
Orthopedics. 33:8822010.PubMed/NCBI
|
|
7
|
Liu YT, Guo LL, Tian Z, Zhu WL, Yu B,
Zhang SY and Qiu GX: A retrospective study of congenital scoliosis
and associated cardiac and intraspinal abnormities in a Chinese
population. Eur Spine J. 20:2111–2114. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Basu PS, Elsebaie H and Noordeen MH:
Congenital spinal deformity: A comprehensive assessment at
presentation. Spine. 27:2255–2259. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lanjewar CP, Khothari S and Kerkar PG:
Delivery sheath tear without modification during ASD closure in a
patient with kyphoscoliosis. Catheter Cardiovasc Interv.
69:766–767. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mangovski L, Farkić M and Jovović L:
Transcatheter closure of atrial septal defect in a patient with
Noonan syndrome after corrective surgery. Vojnosanit Pregl.
72:557–560. 2015. View Article : Google Scholar : PubMed/NCBI
|