Introduction
Breast cancer (BC) is the most commonly diagnosed
cancer and the second leading cause of cancer-associated mortality
among women worldwide (1). In 2017,
~252,710 new cases of invasive BC and 40,610 BC-associated
mortalities occurred among females in the US (2). In China, an estimated 272,400 new cases
and 70,700 BC-associated mortalities were reported in 2015
(3). The current primary treatment
strategy for BC is surgical resection followed by hormonal therapy,
chemotherapy, radiotherapy and/or biological therapy (4). Although recent advances in early
diagnosis and targeted therapies in BC have been achieved, the
molecular mechanism of BC progression remains poorly understood and
the prognosis of patients with advanced BC remains low. It is
therefore important to identify novel biomarkers associated with
clinical prognosis that are also involved in the progression of
BC.
The homeobox (HOX) gene family encodes
homeodomain-containing transcription factors that participate in
various physiological processes, which include embryonic
development, cell proliferation and differentiation (5). In vertebrates, the HOX gene family
contains 39 Hox genes, which are organized into four
different chromosome clusters, each containing 9–11 genes (5,6). As a
member of the HOX gene family, HOXA1 was previously reported to be
involved in tumor progression and prognosis in certain types of
human cancer (7–9). Yuan et al (7) reported that elevated HOXA1 expression
levels enhance cell proliferation and poor prognosis in gastric
cancer. In addition, Wang et al (8) demonstrated that HOXA1 is upregulated in
prostate cancer and knockdown of HOXA1 suppresses the growth,
invasion and migration of prostate cancer cells. Furthermore, Zha
et al (9) reported that HOXA1
overexpression correlates with poor prognosis in patients with
hepatocellular carcinoma. However, whether HOXA1 is associated with
the prognosis of patients with BC remains unknown.
In the current study, the expression of HOXA1 in BC
tissue and adjacent non-cancerous tissue samples from patients with
BC was examined. The prognosis of patients with BC with high and
low HOXA1 mRNA expression levels was assessed. In addition, the
association between HOXA1 expression and clinicopathological
features of patients with BC was examined. Furthermore, the effect
of HOXA1 expression on BC cell proliferation, apoptosis and cell
cycle distribution was assessed. The present study demonstrated
that HOXA1 was upregulated in BC. HOXA1 overexpression was
associated with a poor prognosis and advanced clinicopathological
features in patients with BC. In addition, knockdown of HOXA1
significantly inhibited cell proliferation by enhancing cell
apoptosis and cell cycle arrest in BC cells, which was accompanied
with the aberrant expression of cell cycle and apoptosis-associated
proteins, cyclin D1, B-cell lymphoma 2 (Bcl-2) and Bcl-2-like
protein 4. The current study demonstrated that HOXA1 may act as a
novel marker in BC prognosis and a potential therapeutic target for
the treatment of BC.
Materials and methods
Tissue collection
BC tissue and adjacent non-cancerous tissue samples
were collected from 45 female patients (age range, 40–72 years) who
underwent surgical resection between January 2007 and December 2012
at Dalian Central Hospital Affiliated to Dalian Medical University
(Dalian, China). Following surgery, fresh tissue samples were
frozen in liquid nitrogen and stored at −80°C until further use.
All samples were evaluated and subject to histological diagnosis
according to the World Health Organization criteria by two
pathologists (10). All patients had
regular follow-ups (1–60 months; median follow-up time, 52.4
months) following surgical resection and overall survival was
recorded. The clinicopathological features of each patient,
including age, tumor size, tumor, node and metastasis (TNM) stage
and lymph node metastasis, as well as biological parameters,
including estrogen receptor (ER), progesterone receptor (PR) and
human epidermal growth factor receptor (HER)-2 status were recorded
(Table I). The current study was
conducted according to the World Medical Association Declaration of
Helsinki and approved by the Ethics Committee of Dalian Central
Hospital Affiliated to Dalian Medical University. Written informed
consent was obtained from each patient prior to surgery.
 | Table I.Association between HOXA1 expression
and clinicopathological features of female patients with BC. |
Table I.
Association between HOXA1 expression
and clinicopathological features of female patients with BC.
|
|
| HOXA1 expression |
|
|---|
|
|
|
|
|
|---|
| Clinicopathological
features | Cases (n) | Low (n=22) | High (n=23) | P-value |
|---|
| Age (years) |
| ≤50 | 18 | 8 | 10 | 0.626 |
|
>50 | 27 | 14 | 13 |
|
| Tumor size (cm) |
| ≤3 | 17 | 10 | 7 | 0.299 |
|
>3 | 28 | 12 | 16 |
|
| ER status |
|
Negative | 20 | 11 | 9 | 0.463 |
|
Positive | 25 | 11 | 14 |
|
| PR status |
|
Negative | 19 | 11 | 8 | 0.302 |
|
Positive | 26 | 11 | 15 |
|
| HER2 status |
|
Negative | 18 | 10 | 8 | 0.465 |
|
Positive | 27 | 12 | 15 |
|
| Lymph node
status |
|
Negative | 25 | 16 | 9 | 0.023a |
|
Positive | 20 | 6 | 14 |
|
| TNM stage |
| I–II | 26 | 17 | 9 | 0.01a |
| III | 19 | 5 | 14 |
|
Cell culture
Human BC cell lines BT549, T47D, MDA-MB-231 and MCF7
as well as the human breast epithelial cell line MCF-10A were
obtained from the Cell Culture Collection of the Chinese Academy of
Sciences (Shanghai, China). The four BC cell lines were cultured in
Dulbecco's modified Eagle's medium (DMEM) supplemented with 10%
fetal bovine serum (FBS) and 100 U/ml penicillin/streptomycin
mixture (all Gibco; Thermo Fisher Scientific, Inc., Waltham, MA,
USA). MCF-10A cells were cultured in RPMI-1640 medium supplemented
with 10% FBS and 100 U/ml penicillin/streptomycin mixture (both
Gibco; Thermo Fisher Scientific, Inc.). Cells were maintained at
37°C in a humidified incubator with 5% CO2.
Cell transfection
Cells were seeded into six-well plates at 30–40%
confluence and following a 12 h incubation, cells were transfected
with small interfering RNA (siRNA) targeting HOXA1 (si-HOXA1) or
scrambled negative control siRNA (si-NC) using
Lipofectamine® 2000 (Invitrogen; Thermo Fisher
Scientific, Inc.), according to the manufacturer's protocol.
si-HOXA1 (5′-CAACAAGUACCUUACACGA-3′) and si-NC
(5′-UUCUCCGAACGUGUCACGUTT-3′) were purchased from Shanghai
GenePharma Co. Ltd. (Shanghai, China). Following 48 h of
transfection, cells were harvested and transfection efficiency was
detected by reverse transcription-quantitative polymerase chain
reaction (RT-qPCR) and western blot analysis prior to functional
assays.
RNA extraction and RT-qPCR
Total RNA was extracted from tissue samples or cells
using TRIzol® reagent (Invitrogen; Thermo Fisher
Scientific, Inc.). Total RNA was reverse transcribed into cDNA
using a PrimeScript™ RT-PCR kit (Takara Bio, Inc., Otsu, Japan) for
15 min at 37°C and terminated by heating the samples at 85°C for 5
sec. HOXA1 expression was detected by qPCR, which was performed
using SYBR-Green PCR Master mix (Applied Biosystems; Thermo Fisher
Scientific, Inc.) on the 7300 Real-Time PCR system (Applied
Biosystems; Thermo Fisher Scientific, Inc.). The following primer
pairs were used for qPCR: HOXA1 forward, 5′-CGGCTTCCTGTGCTAAGTCT-3′
and reverse, 5′-TTCATTGTGCCATCCATCAC-3′; and β-actin forward,
5′-TTAGTTGCGTTACACCCTTTC-3′ and reverse, 5′-ACCTTCACCGTTCCAGTTT-3′.
The reaction conditions for PCR were as follows: 95°C for 3 min and
40 cycles of 95°C for 30 sec and 60°C for 30 sec. HOXA1 mRNA levels
were quantified using the 2−ΔΔCq method (11) and normalized to the internal control
β-actin. RT-qPCR was repeated three times.
Western blot analysis
Total protein was extracted from tissue samples or
cells using radioimmunoprecipitation assay buffer (Pierce; Thermo
Fisher Scientific, Inc.) supplemented with protease inhibitor
(78438; 1:100; Thermo Fisher Scientific, Inc.). Total protein was
quantified using a bicinchoninic acid assay and equal amount of
protein (30 µg per lane) was separated via SDS-PAGE on a 10% gel.
Separated proteins were transferred to polyvinylidene fluoride
membranes and blocked with 5% non-fat milk at room temperature for
1 h. Membranes were washed three times and incubated with primary
antibodies against HOXA1 (ab230513; 1:1,000), β-actin (ab8227;
1:2,000), cyclin D1 (ab40754; 1:2,000; all Abcam, Cambridge, UK),
B-cell lymphoma 2 (cat. no. 4223, 1:1,000) and Bcl-2-like protein 4
(Bax; cat. no. 2774, 1:1,000; both Cell Signaling Technology, Inc.,
Danvers, MA, USA) overnight at 4°C. Following primary incubation,
membranes were incubated with horseradish peroxidase-conjugated
secondary antibodies [horseradish peroxidase (HRP) conjugated goat
anti-mouse immunoglobulin G (IgG); sc-2005 and goat anti-rabbit
IgG-HRP; sc-2004; 1:5,000; Santa Cruz Biotechnology, Santa Cruz,
CA, USA] for 2 h at room temperature. Protein bands were visualized
using the enhanced chemiluminescence detection system (Pierce;
Thermo Fisher Scientific, Inc.) with an ECL kit (EMD Millipore,
Billerica, MA, USA). Protein expression was quantified using
β-actin as an internal control. Relative protein expression was
analyzed using ImageJ software 1.4 (National Institutes of Health,
Bethesda, MD, USA). Each experiment was performed in
triplicate.
Cell proliferation
To examine the effect of HOXA1 on BC cell
proliferation, MDA-MB-231 and MCF7 BC cell lines were transfected
with si-HOXA1 and cell proliferation was assessed using the MTT
assay. Briefly, transfected cells were seeded into 96-well plates
at 3×103 cells/well and cultured at 37°C. Following
incubation for 24, 48, 72 and 96 h, 100 µl full DMEM medium
containing 0.5 mg/ml MTT (Sigma-Aldrich; Merck KGaA, Darmstadt,
Germany) was added into each well and incubated for a further 4 h
at 37°C. Subsequently, the medium was removed and 150 µl dimethyl
sulfoxide (Sigma-Aldrich; Merck KGaA) was added to dissolve the
formazan crystals. The absorbance was measured at 490 nm using a
microplate reader (Molecular Devices, USA). Each experiment was
performed in triplicate.
Cell cycle analysis
Cell cycle distribution was determined by propidium
iodide (PI) staining. Following 48 h transfection with si-NC or
si-HOXA1, MDA-MB-231 and MCF7 cells were seeded into 6-cm dishes at
a confluence of 30% and incubated for 48 h. Cells were subsequently
collected and fixed with 70% ethanol overnight at 4°C. Cells were
washed twice with cold PBS and stained with PI (Sigma-Aldrich;
Merck KGaA) for 30 min at room temperature in the dark. The
proportion of cells in each phase was analyzed using a BD FACS
Calibur Flow Cytometer (BD Biosciences, San Jose, CA, USA) and the
data were analyzed using SPSS software (version 18.0; SPSS, Inc.,
Chicago, IL, USA). Each experiment was performed in triplicate.
Apoptosis assay
Cell apoptosis was analyzed by using the Annexin
V-fluorescein isothiocyanate (FITC) Apoptosis Detection kit (BD
Pharmingen; BD Biosciences, San Jose, CA, USA). Following 48 h
transfection with si-NC or si-HOXA1, cells were collected via
centrifugation at a speed of 50 × g for 5 min at room temperature
and resuspended in 200 µl binding buffer. Cells were subsequently
stained with 5 µl Annexin V-FITC and 5 µl PI together for 15 min at
room temperature in the dark. Apoptotic cells were detected using a
BD FACSCalibur Flow cytometer (BD Biosciences) and the rate of
apoptosis was analyzed using SPSS software (version 18.0; SPSS,
Inc.). Each experiment was performed in triplicate.
Statistical analysis
Data are presented as the mean ± standard deviation
of three replicates. Statistical analyses were performed using SPSS
software (version 18.0; SPSS, Inc., Chicago, IL, USA) and GraphPad
Prism software (version 6.0; GraphPad Software, La Jolla, CA, USA).
Expression levels of HOXA1 mRNA in BC tissue and adjacent
non-cancerous tissue samples were compared using the Wilcoxon
signed-rank nonparametric test. Student's t-test was used to
analyze differences between two groups. Tukey's analysis following
one-way analysis of variance was used to analyze differences among
multiple groups. The association between HOXA1 expression and
clinicopathological features of patients with BC was analyzed using
the Chi-square test. The overall survival of patients was
calculated using the Kaplan-Meier method, and the differences
between survival curves were examined using the log-rank test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
HOXA1 upregulation is associated with
poor prognosis in patients with BC
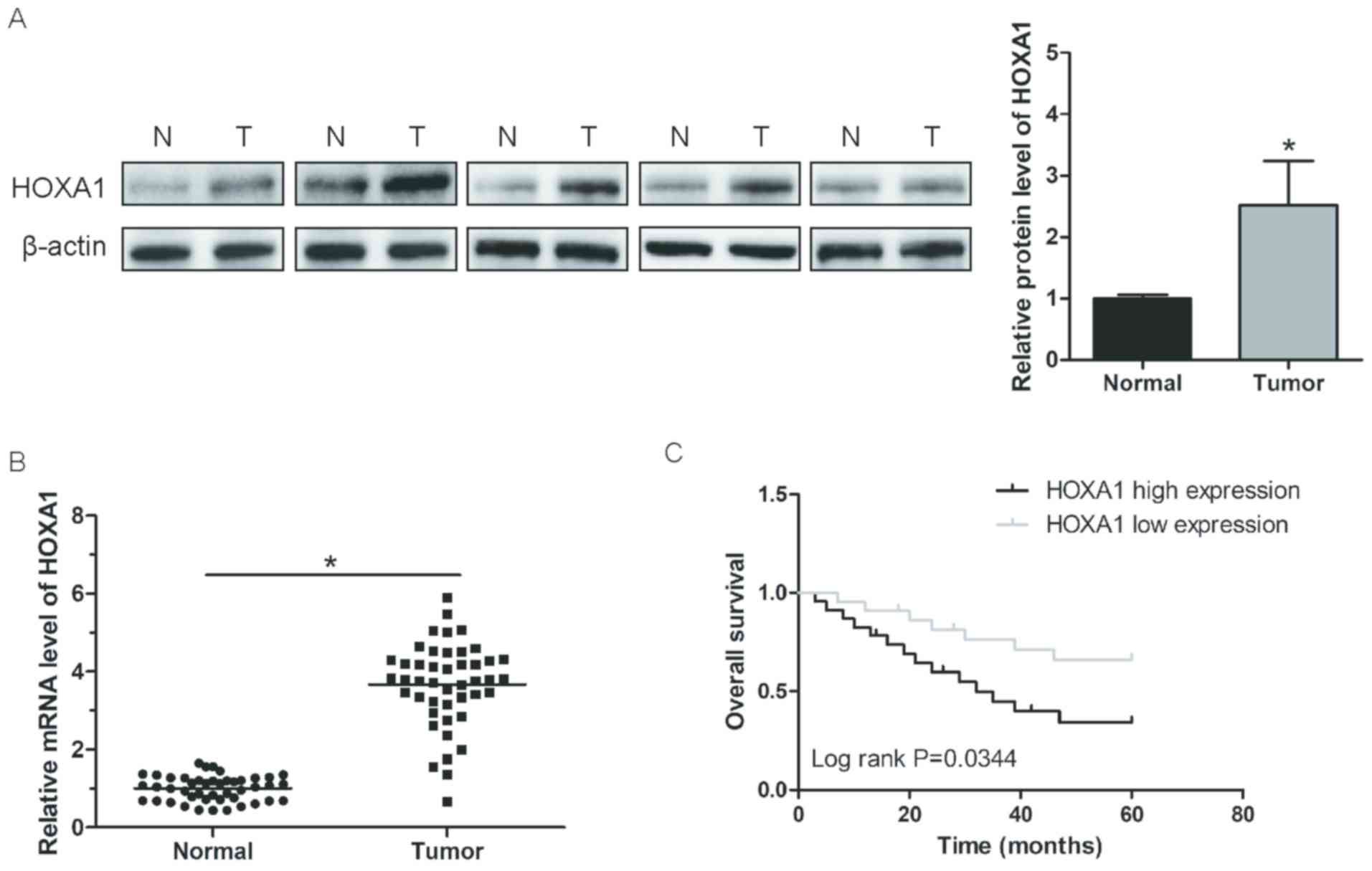
To investigate the expression of HOXA1 in BC, the
relative HOXA1 protein expression in BC tissue and adjacent
non-cancerous tissue samples from patients with BC was determined
by western blot analysis. HOXA1 protein expression was
significantly increased in BC tissue compared with adjacent
non-cancerous tissue samples (P<0.05; Fig. 1A). In addition, the relative HOXA1
mRNA expression levels in BC tissue and adjacent non-cancerous
tissues from patients with BC were determined by RT-qPCR. HOXA1
mRNA expression levels were significantly increased in BC tissue
compared with adjacent non-cancerous tissue samples (P<0.05;
Fig. 1B). Patients with BC were
divided into two groups: High (n=23) and low (n=22) HOXA1
expression based on the median mRNA expression level of HOXA1
(3.782 relative to β-actin) detected in BC tissue samples from
patients with BC. To determine the effect of HOXA1 expression level
on the survival of patients with BC, survival curves were plotted
using the Kaplan-Meier method and the differences between survival
curves were examined using the log-rank test. The overall survival
of patients in the high HOXA1 expression group was significantly
decreased compared with patients with BC in the low HOXA1
expression group (P=0.0344; Fig.
1C). These results suggested that HOXA1 was upregulated in
patients with BC and HOXA1 upregulation may be associated with poor
prognosis.
HOXA1 upregulation is associated with
tumor progression in BC
The association between HOXA1 expression and
clinicopathological features of patients with BC was examined
(Table I). The mRNA expression level
of HOXA1 was significantly associated with lymph node metastasis
(P=0.023) and TNM staging (P=0.01); however, no association with
age, tumor size, and ER, PR or HER2 status was identified
(P>0.05). These results suggested that HOXA1 upregulation may be
associated with tumor progression in BC.
HOXA1 siRNA effectively silences HOXA1
gene expression in BC cells
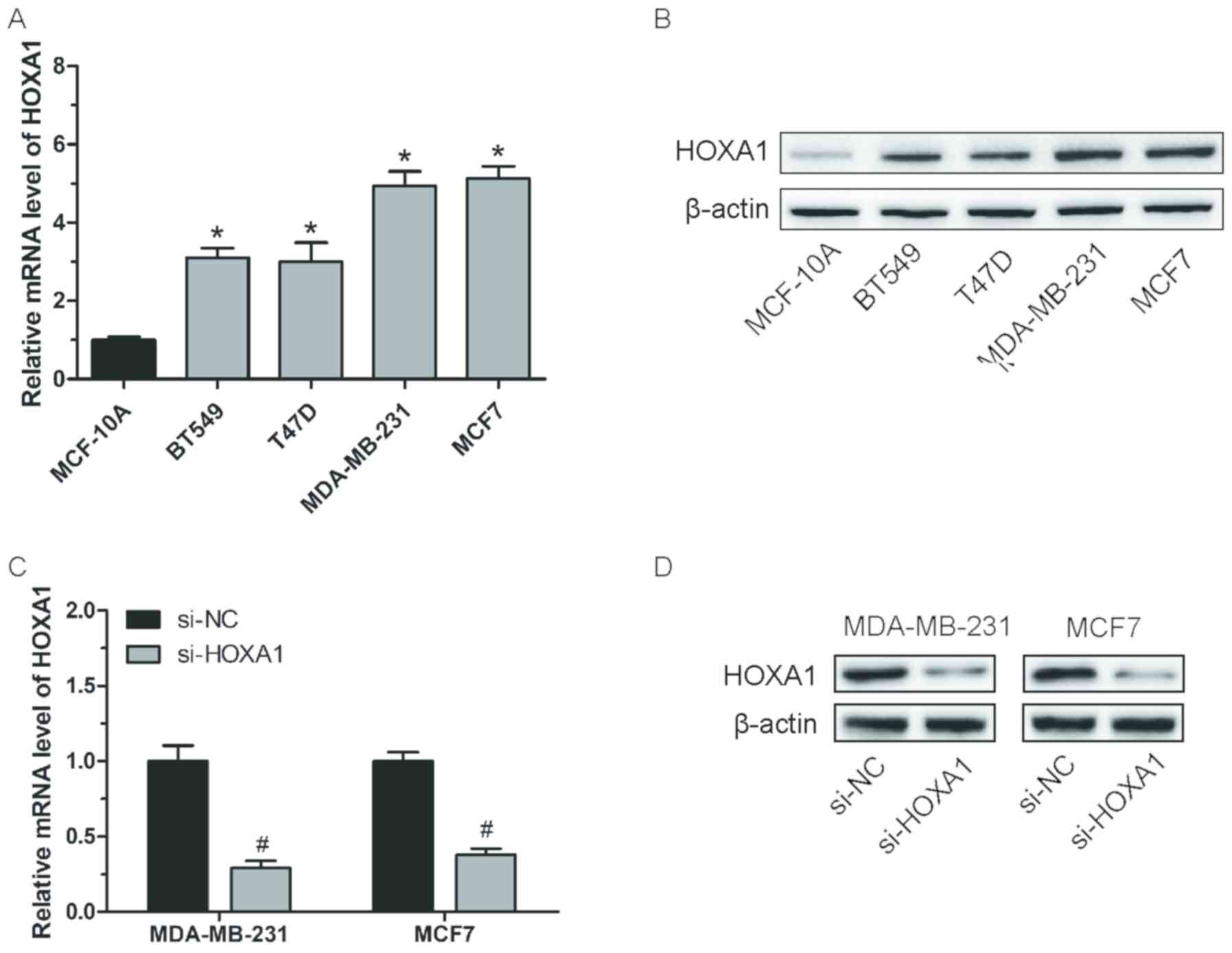
To further confirm HOXA1 overexpression in BC, the
mRNA and protein expression levels were determined in BC cell lines
BT549, T47D, MDA-MB-231 and MCF7 and the normal breast epithelial
cell line MCF-10A. HOXA1 mRNA expression levels were significantly
increased in BC cell lines compared with MCF-10A (P<0.05;
Fig. 2A and B). Similarly, western
blot analysis revealed that HOXA1 protein expression levels were
increased in BC cell lines compared with MCF-10A (Fig. 2B). To investigate the functional role
of HOXA1 in BC progression, BC cell lines MDA-MB-231 and MCF7 were
transfected with si-HOXA1 or si-NC and transfection efficiency was
confirmed by RT-qPCR and western blot analysis. The results
demonstrated that si-HOXA1 significantly downregulated HOXA1 mRNA
(P<0.05) and markedly reduced protein expression in BC cell
lines compared with the si-NC control (Fig. 2C and D).
Knockdown of HOXA1 inhibits BC cell
proliferation
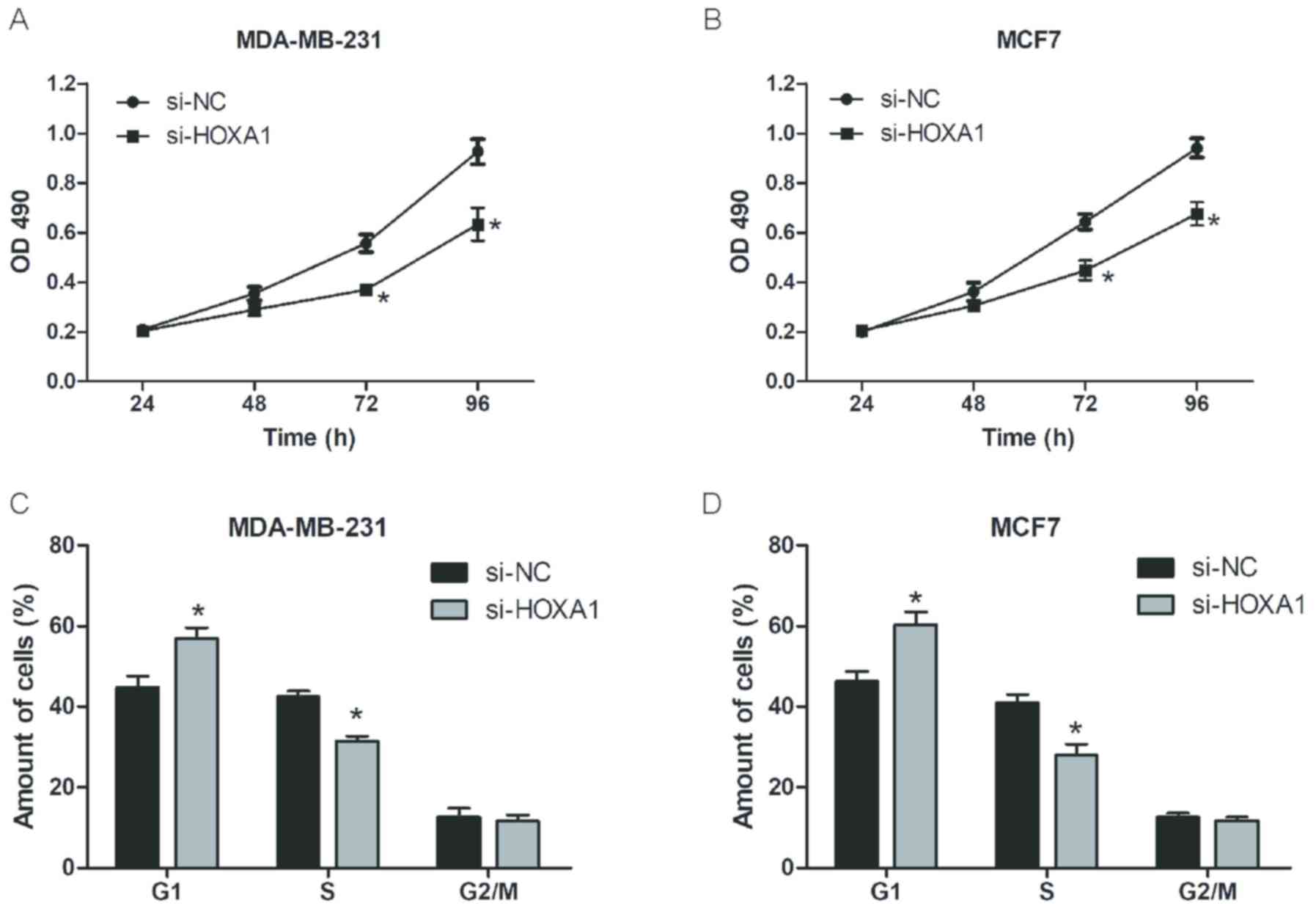
MTT assays were performed to investigate the effect
of HOXA1 knockdown on cell proliferation in BC cell lines
MDA-MB-231 and MCF7. Knockdown of HOXA1 significantly inhibited BC
cell proliferation compared with si-NC at ≥72 h (P<0.05;
Fig. 3A and B). In addition, PI
staining was used to assess cell cycle distribution using flow
cytometry in BC cell lines MDA-MB-231 and MCF7 following
transfection with si-HOXA1 or si-NC. The percentage of cells in G1
phase was significantly increased, whilst those in S phase were
significantly decreased in BC cells following HOXA1 knockdown
(P<0.05; Fig. 3C and D). These
results suggested that knockdown of HOXA1 may inhibit BC cell
proliferation partly by suppressing cell cycle progression.
Knockdown of HOXA1 promotes BC cell
apoptosis
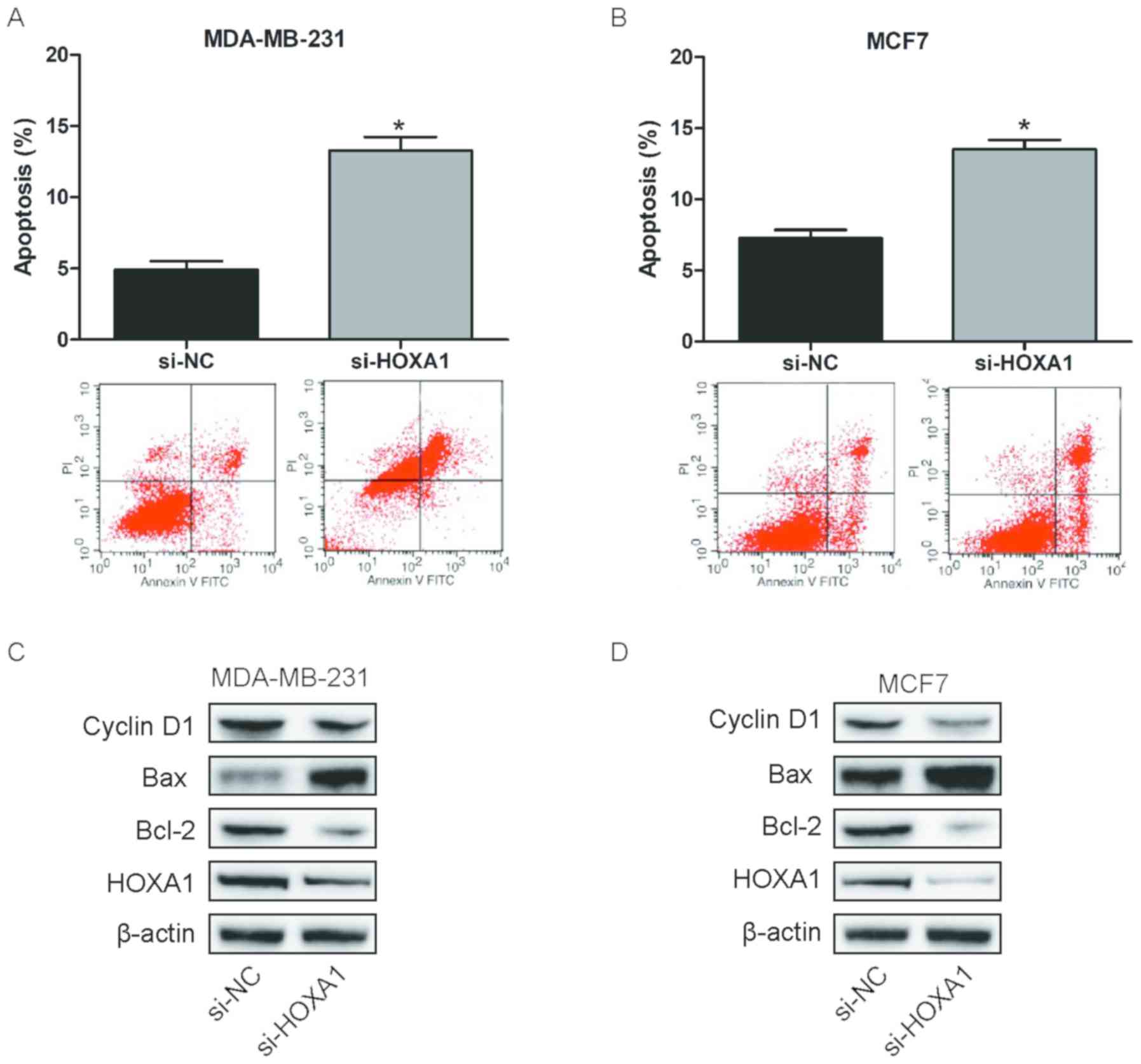
Cell apoptosis was analyzed in BC cell lines
MDA-MB-231 and MCF7 following transfection with si-HOXA1 or si-NC.
Flow cytometry revealed that knockdown of HOXA1 significantly
enhanced BC cell apoptosis (P<0.05; Fig. 4A and B). In addition, western blot
analysis was used to determine the expression level of cell cycle
and apoptosis-associated proteins cyclin D1, Bax and Bcl-2
following transfection with si-HOXA1 or si-NC. The protein
expression levels of cyclin D1 and Bcl-2 markedly decreased, whilst
the levels of Bax markedly increased in BC cells following HOXA1
knockdown (Fig. 4C and D). Taken
together, these results suggested that knockdown of HOXA1 may
inhibit BC cell proliferation partly by inducing cell
apoptosis.
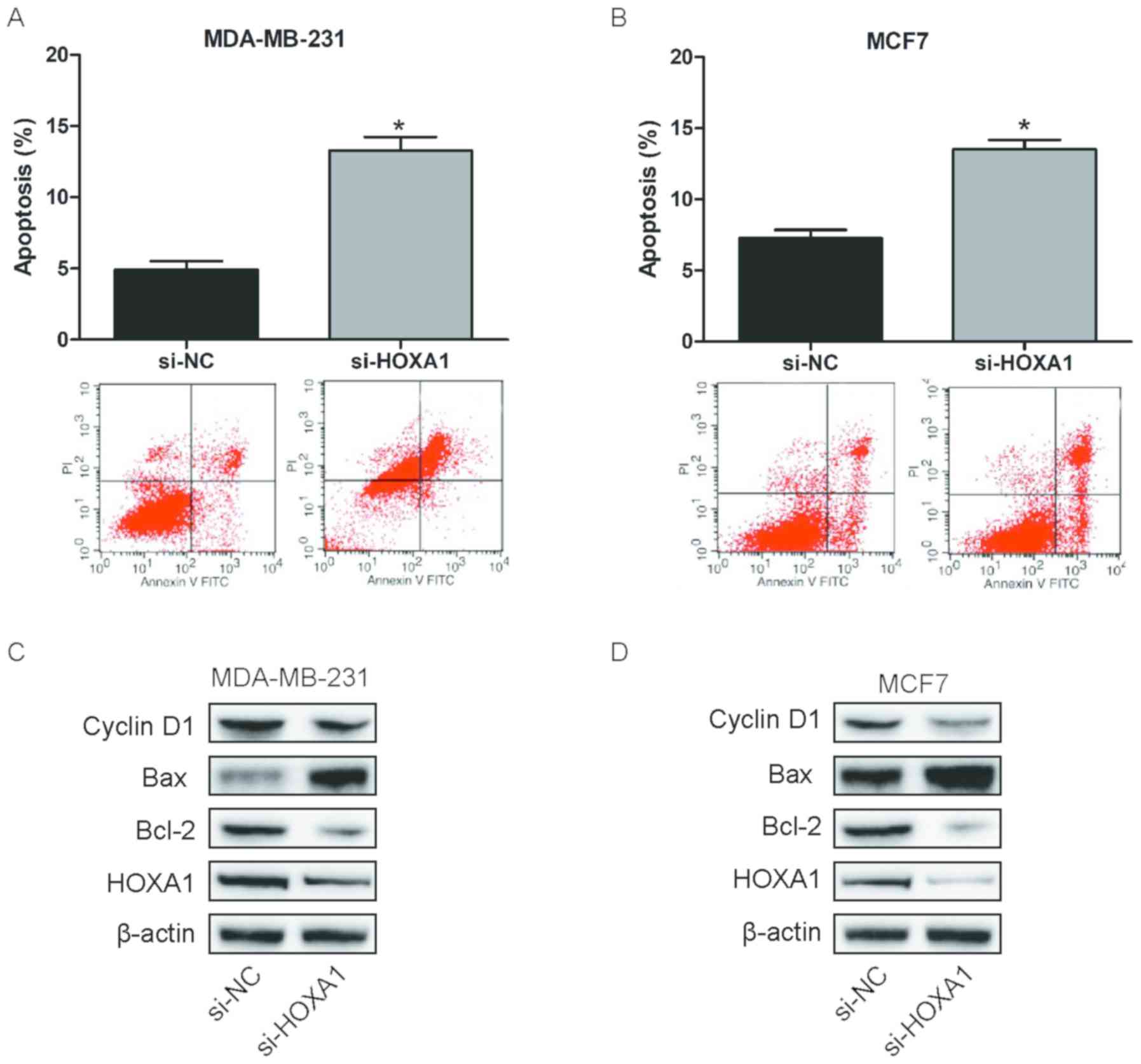 | Figure 4.Knockdown of HOXA1 promotes BC cell
apoptosis. Cell apoptosis was analyzed in (A) MDA-MB-231 and (B)
MCF7 BC cell lines by flow cytometry following transfection with
si-HOXA1. Relative protein expression of cyclin D1, Bax and Bcl-2
was determined by western blot analysis in (C) MDA-MB-231 and (D)
MCF7 BC cell lines following transfection with si-HOXA1. Data are
presented as the mean ± standard deviation. *P<0.05 vs. si-NC.
HOXA1, homeobox A1; BC, breast cancer; si, small interfering RNA;
NC, negative; si-HOXA1, siRNA targeting HOXA1; Bcl-2, B-cell
lymphoma 2; Bax, Bcl-2-like protein 4; PI, propidium iodide; FITC,
fluorescein isothiocyanate. |
Discussion
BC is the most common malignancy among females
worldwide and as the incidence of BC has been increasing over the
past years, it is considered to be a serious health risk (12,13).
Thus, a better understanding of the molecular mechanisms involved
in BC initiation and progression as well as validation of novel
prognostic biomarkers may have a potential clinical significance
for patients with BC. Previous studies demonstrated that several
HOX genes, including HOXA5, HOXB9 and HOXC8 were aberrantly
expressed in BC and served roles in tumor progression in BC
(14–16). Additionally, HOXA1 is involved in the
development and prognosis of several types of human cancer,
including gastric cancer, prostate cancer and hepatocellular
carcinoma (7–9). However, the clinical significance of
HOXA1 in BC remains unknown.
In the current study, the mRNA and protein
expression levels of HOXA1 in BC tissue and adjacent non-cancerous
tissue samples were determined via RT-qPCR and western blot
analysis, respectively. The results demonstrated that both HOXA1
mRNA and protein expression levels were significantly upregulated
in BC tissue compared with non-cancerous tissue samples from
patients with BC. Survival analysis indicated that patients with
high HOXA1 expression had a significantly poorer overall survival
compared with patients with low HOXA1 expression. In addition, the
association between HOXA1 expression and clinicopathological
features of patients with BC was examined and HOXA1 expression was
associated with lymph node metastasis and TNM staging. No
association with age, tumor size and ER, PR or HER2 status was
identified. Taken together, these results suggested that HOXA1
upregulation may be associated with poor prognosis and tumor
progression in BC.
To investigate the biological function of HOXA1 in
BC, BC cell lines MDA-MB-231 and MCF7 were transfected with
si-HOXA1 or si-NC. Knockdown of HOXA1 significantly inhibited cell
proliferation and induced apoptosis and cell cycle arrest in BC
cells. Furthermore, the expression of cell cycle and
apoptosis-associated proteins, cyclin D1, Bax and Bcl-2 were
examined. Western blot analysis revealed that the protein
expression levels of cyclin D1 and Bcl-2 decreased, whilst the
level of Bax increased following knockdown of HOXA1 in BC cells.
Together, these results suggest that HOXA1 may be involved in the
development of BC.
The underlying mechanism of HOXA1 in BC progression
was not investigated in the current study and remains unclear. A
recent study demonstrated that HOXA1 activates nuclear factor
(NF)-κB and operates upstream of the NF-κB inhibitor, IκB to
modulate the tumor necrosis factor-α/NF-κB signaling pathway
(17). In addition, a previous study
reported that HOXA1 regulates tumor progression in gastric cancer
via cyclin D1 (7). Furthermore,
previous studies demonstrated that in different types of cancer,
HOXA1 is regulated by several microRNAs (miR), including miR-99a,
miR-30c and miR-100 (18–20). Therefore, further studies are
required to investigate the underlying mechanism of HOXA1 in
BC.
In conclusion, the current study demonstrated that
HOXA1 mRNA and protein expression levels were significantly
upregulated in BC. In addition, HOXA1 overexpression was associated
with poor prognosis and tumor progression in BC. Furthermore,
knockdown of HOXA1 significantly inhibited cell proliferation by
inducing apoptosis and cell cycle arrest in BC cells. Together,
these findings suggested that HOXA1 may serve as a novel prognostic
marker and a potential therapeutic target in BC.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JintL designed the current study. JintL and JinqL
performed the experiments. JinqL and XL collected and analyzed the
data. JintL and XL wrote and revised the manuscript.
Ethics approval and consent to
participate
The current study was approved by the Ethics
Committee of Dalian Central Hospital Affiliated to Dalian Medical
University. Written informed consent was obtained from each
patient.
Patient consent for publication
Patients provided written informed consent for the
publication of any associated data from their samples.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
DeSantis CE, Ma J, Goding Sauer A, Newman
LA and Jemal A: Breast cancer statistics, 2017, racial disparity in
mortality by state. CA Cancer J Clin. 67:439–448. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Qin C, Zhao Y, Gong C and Yang Z:
MicroRNA-154/ADAM9 axis inhibits the proliferation, migration and
invasion of breast cancer cells. Oncol Lett. 14:6969–6975.
2017.PubMed/NCBI
|
|
5
|
Gehring WJ and Hiromi Y: Homeotic genes
and the homeobox. Annu Rev Genet. 20:147–173. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Scott MP: Vertebrate homeobox gene
nomenclature. Cell. 71:551–553. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yuan C, Zhu X, Han Y, Song C, Liu C, Lu S,
Zhang M, Yu F, Peng Z and Zhou C: Elevated HOXA1 expression
correlates with accelerated tumor cell proliferation and poor
prognosis in gastric cancer partly via cyclin D1. J Exp Clin Cancer
Res. 35:152016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wang H, Liu G, Shen D, Ye H, Huang J, Jiao
L and Sun Y: HOXA1 enhances the cell proliferation, invasion and
metastasis of prostate cancer cells. Oncol Rep. 34:1203–1210. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zha TZ, Hu BS, Yu HF, Tan YF, Zhang Y and
Zhang K: Overexpression of HOXA1 correlates with poor prognosis in
patients with hepatocellular carcinoma. Tumour Biol. 33:2125–2134.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Leong AS and Zhuang Z: The changing role
of pathology in breast cancer diagnosis and treatment.
Pathobiology. 78:99–114. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Li Y, Lv M, Song Z, Lou Z, Wang R and
Zhuang M: Long non-coding RNA NNT-AS1 affects progression of breast
cancer through miR-142-3p/ZEB1 axis. Biomed Pharmacother.
103:939–946. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li P, Dong J, Zhou X, Sun W, Huang H, Chen
T, Ye B, Zheng Z and Lu M: Expression patterns of microRNA-329 and
its clinical performance in diagnosis and prognosis of breast
cancer. Onco Targets Ther. 10:5711–5718. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Teo WW, Merino VF, Cho S, Korangath P,
Liang X, Wu RC, Neumann NM, Ewald AJ and Sukumar S: HOXA5
determines cell fate transition and impedes tumor initiation and
progression in breast cancer through regulation of E-cadherin and
CD24. Oncogene. 35:5539–5551. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hayashida T, Takahashi F, Chiba N,
Brachtel E, Takahashi M, Godin-Heymann N, Gross KW, Vivanco Md,
Wijendran V, Shioda T, et al: HOXB9, a gene overexpressed in breast
cancer, promotes tumorigenicity and lung metastasis. Proc Natl Acad
Sci USA. 107:1100–1105. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang Y, Yang C, Zhang M, Liu H, Gong C,
Zhang J, Xu S, Zou J, Kai Y and Li Y: Interleukin enhancer-binding
factor 3 and HOXC8 co-activate cadherin 11 transcription to promote
breast cancer cells proliferation and migration. Oncotarget.
8:107477–107491. 2017.PubMed/NCBI
|
|
17
|
Taminiau A, Draime A, Tys J, Lambert B,
Vandeputte J, Nguyen N, Renard P, Geerts D and Rezsöhazy R: HOXA1
binds RBCK1/HOIL-1 and TRAF2 and modulates the TNF/NF-κB pathway in
a transcription-independent manner. Nucleic Acids Res.
44:7331–7349. 2016.PubMed/NCBI
|
|
18
|
Wang JG, Tang WP, Liao MC, Liu YP and Ai
XH: MiR-99a suppresses cell invasion and metastasis in
nasopharyngeal carcinoma through targeting HOXA1. Onco Targets
Ther. 10:753–761. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ni LY, Zhao JD, Lu YH, Li W, Li BL, Wang
XC and Meng QG: MicroRNA-30c suppressed giant-cell tumor of bone
cell metastasis and growth via targeting HOXA1. Eur Rev Med
Pharmacol Sci. 21:4819–4827. 2017.PubMed/NCBI
|
|
20
|
Xiao F, Bai Y, Chen Z, Li Y, Luo L, Huang
J, Yang J, Liao H and Guo L: Downregulation of HOXA1 gene affects
small cell lung cancer cell survival and chemoresistance under the
regulation of miR-100. Eur J Cancer. 50:1541–1554. 2014. View Article : Google Scholar : PubMed/NCBI
|