Introduction
Intra-abdominal pressure (IAP) is normally
atmospheric or sub-atmospheric, and when it exceeds 10
cmH2O, it results in a condition referred to as
intra-abdominal hypertension (IAH) (1). The blood flow to and the perfusion
pressure of organs in the abdominal cavity decrease with increasing
IAP (2). Abdominal compartment
syndrome (ACS) refers to organ dysfunction and ischemia resulting
from IAH, which triggers a systemic inflammatory response by
releasing cytokines, including tumor necrosis factor-α,
interleukin-6 and oxygen free radicals. The inflammatory response
in turn causes capillary leakage leading to bowel edema, thus
further increasing the IAP and resulting in multiple organ
dysfunction syndrome. An IAP of >12 cmH2O is
associated with an increased risk of mortality (3).
The lung is one of the first organs to be damaged
due to IAH, since the increased IAP leads to a decreased lung
volume and lung compliance, and increased airway resistance, which
results in acute respiratory distress syndrome, ultimately
requiring mechanical ventilation support (4).
Pressure-regulated volume control ventilation
(PRVCV) uses the tidal volume as a feedback control for
continuously adjusting the pressure limit (5–7). It
enables satisfactory and stable ventilation at the lowest possible
pressure level, which reduces injury by positive pressure
ventilation and increases safety (8).
Therefore, the objective of the present study was to
determine whether the PRVCV mode has a protective effect on
patients with ACS compared with pressure control ventilation
(PCV).
Materials and methods
Patients and selection
A prospective study was performed, including
consecutive patients hospitalized for >3 days at the intensive
care unit (ICU) between January 2015 and December 2017. In the
current study, 60 patients were enrolled, 20 were excluded, as 18
did not match the inclusion criteria and two refused to be
involved. A total of 40 patients (25 males and 15 females) who
matched the diagnostic criteria and managed according to the
treatment standards for Abdominal Compartment Syndrome (ACS) of the
World Society of the ACS (WSACS) (1), and with the diagnostic criteria for
respiratory failure with a partial pressure of oxygen
(PaO2) of <60 mmHg or a partial pressure of carbon
dioxide (PaCO2) of >50 mmHg, were included.
Pediatric patients, patients with lung diseases,
including acute exacerbation of chronic obstructive pulmonary
disease, severe pneumonia and pulmonary hypertension, and patients
with heart diseases, including congenital heart disease, acute
coronary syndrome and malignant arrhythmia, were excluded. Patients
with severe multiple organ dysfunction, end-stage malignant
carcinoma and immunosuppression conditions were also excluded.
IAH is divided into 4 stages according to the IAP:
Stage I, 12–15 mmHg; stage II, 16–20 mmHg; stage III, 21–25 mmHg;
and stage VI, >25 mmHg. ACS is defined as a sustained IAP at
>20 mmHg, with or without an abdominal perfusion pressure of
<60 mmHg, which is consistent with the definition of organ
dysfunction/failure published in 2013 by the WSACS (1). The IAP was measured every 6 h and
patients were required to have stable hemodynamics for >12 h.
Therefore, their mean arterial pressure (MAP) was maintained at
>60 mmHg by continuous intravenous administration of vasoactive
drugs. In the present study, the sedation score on the
Sedation-Agitation Scale was maintained between 3 and 4 using a
sedative (9). The patients were
randomized into two groups: i) In the PCV group, patients were
ventilated using the PCV mode with an inspiratory pressure of 8–15
mmHg, inspiratory time of 0.8–1.2 sec, inhaled gas oxygen
concentration [fraction of inspired oxygen (FiO2)] of
0.3–0.6 and positive end expiratory pressure (PEEP) of 6–12 mmHg;
and ii) in the PRVCV group, patients were ventilated using the
PRVCV mode with a tidal volume of 5–12 ml/kg, respiratory rate of
12–18 times per minute, upper pressure limit (Pmax) of
35 mmHg, inspiratory:expiratory of 1:2, FiO2 of 0.3–0.6
and PEEP of 6–12 mmHg. Parameters were adjusted based on disease
severity, lung compliance and arterial blood gas (ABG), in order to
maintain an oxygen saturation of 90–95%.
Conventional and active ICU management included
disinfection, fasting, gastrointestinal decompression, abdominal
drainage and correction of any electrolyte imbalances. All patients
required invasive mechanical ventilation; the Dräger Evita 4
ventilator (Drägerwerk AG & Co. KGaA, Lübeck, Germany) was used
for the PCV group and the MAQUET Servo-i ventilator (MAQUET Ltd.,
Tyne & Wear, UK) for the PRVCV group.
Measurement of IAP
The IAP was measured in the urinary bladder by using
a Foley Manometer device with the patient in a supine position
(10). The bladder was first emptied
of intra-vesical urine and then injected with 50 ml saline through
a catheter. Using the symphysis pubis as a zero-reference point,
the end expiration pressure was measured. A measurement protocol
was drafted and performed by experienced staff.
Data collection
ABG parameters, including pH, PaO2,
PaCO2 and oxygenation index
(PaO2/FiO2), were recorded. Respiratory
mechanics indices, including peak inspiratory pressure (PIP), mean
inspiratory pressure (Pmean), pulmonary static
compliance (Cst) and airway resistance (R) were monitored by a
detection system in the ventilator. Hemodynamic values, including
the HR, MAP, central venous pressure (CVP) and extravascular lung
water index (ELWI) were measured by the PiCCO2 system
(Pulsion Co., Glasgow, UK). All data were collected after 6 h of
ventilation and each parameter was measured 3 times.
Statistical analysis
All values are expressed as the mean ± standard
deviation unless otherwise stated and analyzed using SPSS version
19 (IBM Corp., Armonk, NY, USA). Numerical data were compared using
Student's unpaired t-test. Categorical data were analyzed with a
Chi-square test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient characteristics
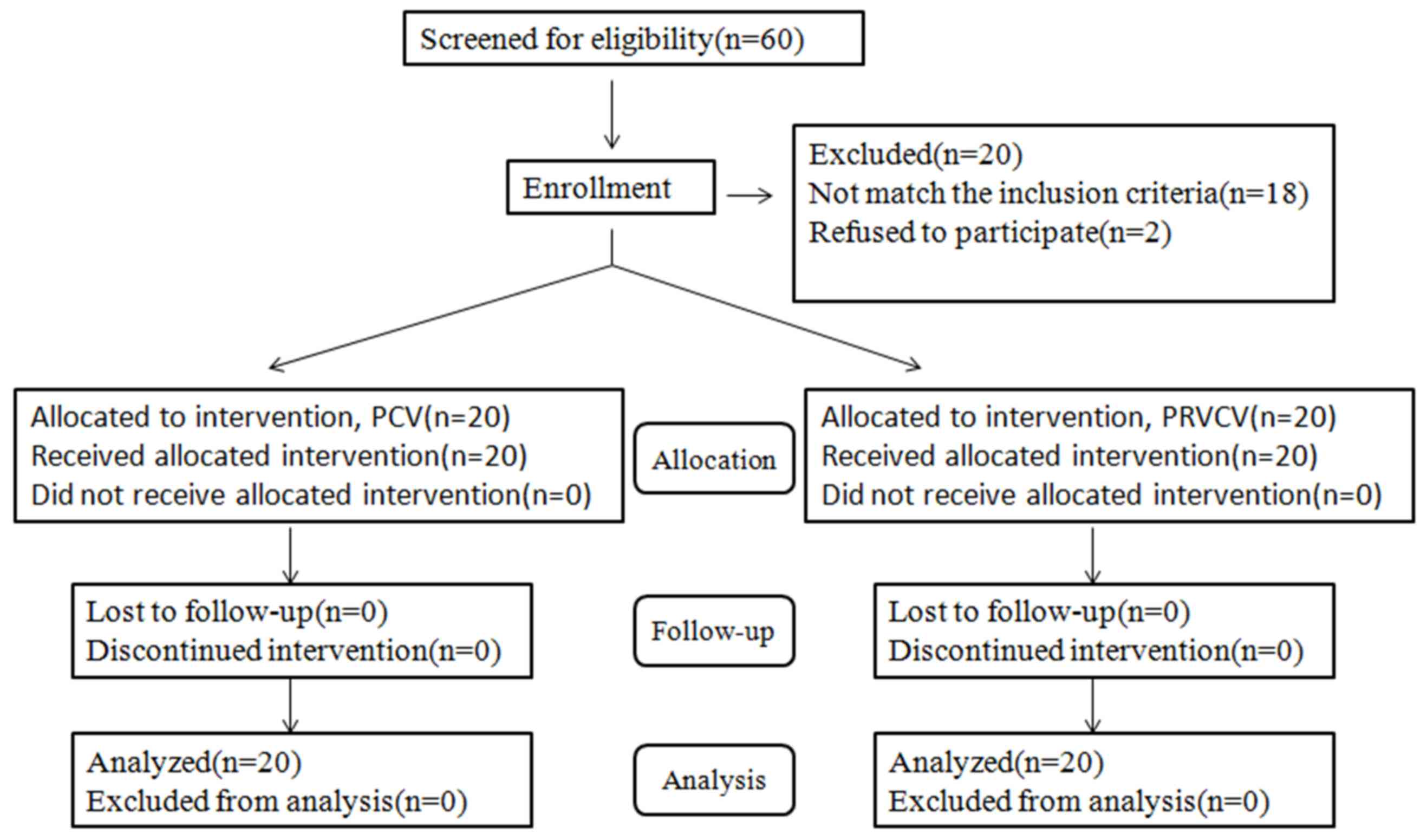
A total of 60 patients were initially screened, of
which 18 did not match the inclusion criteria and 2 refused to
participate. The remaining 40 patients completed the weaning
procedure (Fig. 1). There were no
significant differences between the two groups (n=20 each) in terms
of their clinical characteristics (Table
I).
 | Table I.Baseline characteristics of the study
groups. |
Table I.
Baseline characteristics of the study
groups.
| Characteristic | Normal value | PCV group (n=20) | PRVCV group
(n=20) | P-value |
|---|
| Age (years) |
|
67.05±10.85 |
58.55±15.39 | 0.051 |
| Sex
(M/F) |
| 13/7 | 12/8 | 0.833 |
| Height
(cm) |
| 167.00±6.59 | 166.15±7.05 | 0.696 |
| Weight
(kg) |
|
62.80±5.91 |
63.80±8.05 | 0.657 |
| BMI
(kg/m2) | 18.50–25 |
21.80±2.26 |
21.15±1.66 | 0.307 |
| IAP
(mmHg) | 5–7 |
23.40±2.37 |
24.20±2.86 | 0.341 |
| SOFA | 0 |
17.10±2.10 |
16.75±1.55 | 0.552 |
| pH | 7.35–7.45 |
7.24±0.08 |
7.29±0.09 | 0.071 |
|
PaO2 (mmHg) | 60–90 |
65.40±4.01 |
64.40±3.63 | 0.762 |
|
PaCO2 (mmHg) | 35–45 |
51.00±7.22 |
49.20±3.75 | 0.448 |
|
PaO2/FiO2
(mmHg) | 400–500 |
146.15±16.42 |
148.35±16.10 | 0.788 |
| PIP
(mmHg) |
7–12 |
27.00±4.54 |
26.85±7.23 | 0.917 |
|
Pmean (mmHg) |
4–11 |
14.65±2.60 |
15.30±2.85 | 0.405 |
| Cst
(ml/cmH2O) |
60–100 |
37.35±3.51 |
36.90±4.48 | 0.765 |
| R
(cmH2O/l/sec) | 1–3 |
7.96±1.39 |
8.05±1.43 | 0.829 |
| HR
(beats/min) |
60–100 | 107.70±9.31 |
111.95±13.73 | 0.203 |
| MAP
(mmHg) |
70–105 |
65.90±8.26 |
63.45±7.74 | 0.316 |
| CVP
(mmHg) | 4–9 |
20.90±4.01 |
22.60±4.43 | 0.182 |
| ELWI
(ml/kg) | 3–7 |
12.00±2.07 |
12.05±1.82 | 0.936 |
| Etiology |
|
Intestinal
obstruction/necrosis |
| 6 (30) | 10 (50) | 0.333 |
| Severe
multiple trauma |
| 7 (35) | 4 (20) | 0.480 |
| AP |
| 3 (15) | 2 (10) | 0.999 |
| Septic
shock |
| 1 (5) | 2 (10) | 0.999 |
|
Hepatobiliary disease |
| 3 (15) | 2 (10) | 0.999 |
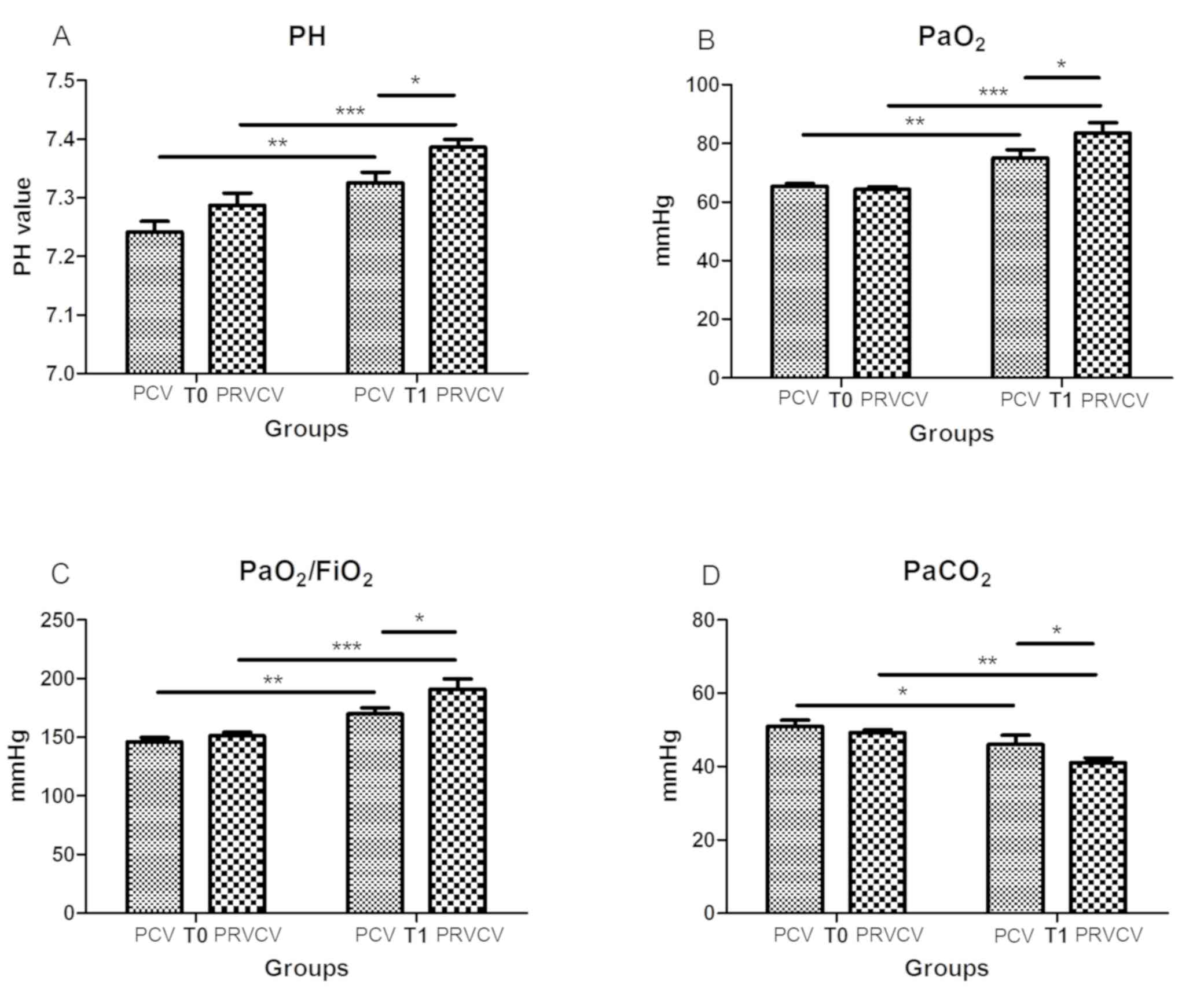
Outcomes regarding ABG parameters
All ABG parameters improved following treatment in
the two groups (all P<0.05). Compared with those obtained using
the PCV mode, significant improvements in pH (7.33±0.81 vs.
7.39±0.57, P=0.017), PaO2 (75.05±12.31 vs. 83.50±15.89
mmHg, P=0.012) and PaO2/FiO2 (169.85±23.53
vs. 190.75±39.72 mmHg, P=0.012), and a significant decrease in
PaCO2 (46.05±11.14 vs. 41.10±5.68 mmHg, P=0.039) were
noted after 6 h of using the PRVCV mode (Fig. 2).
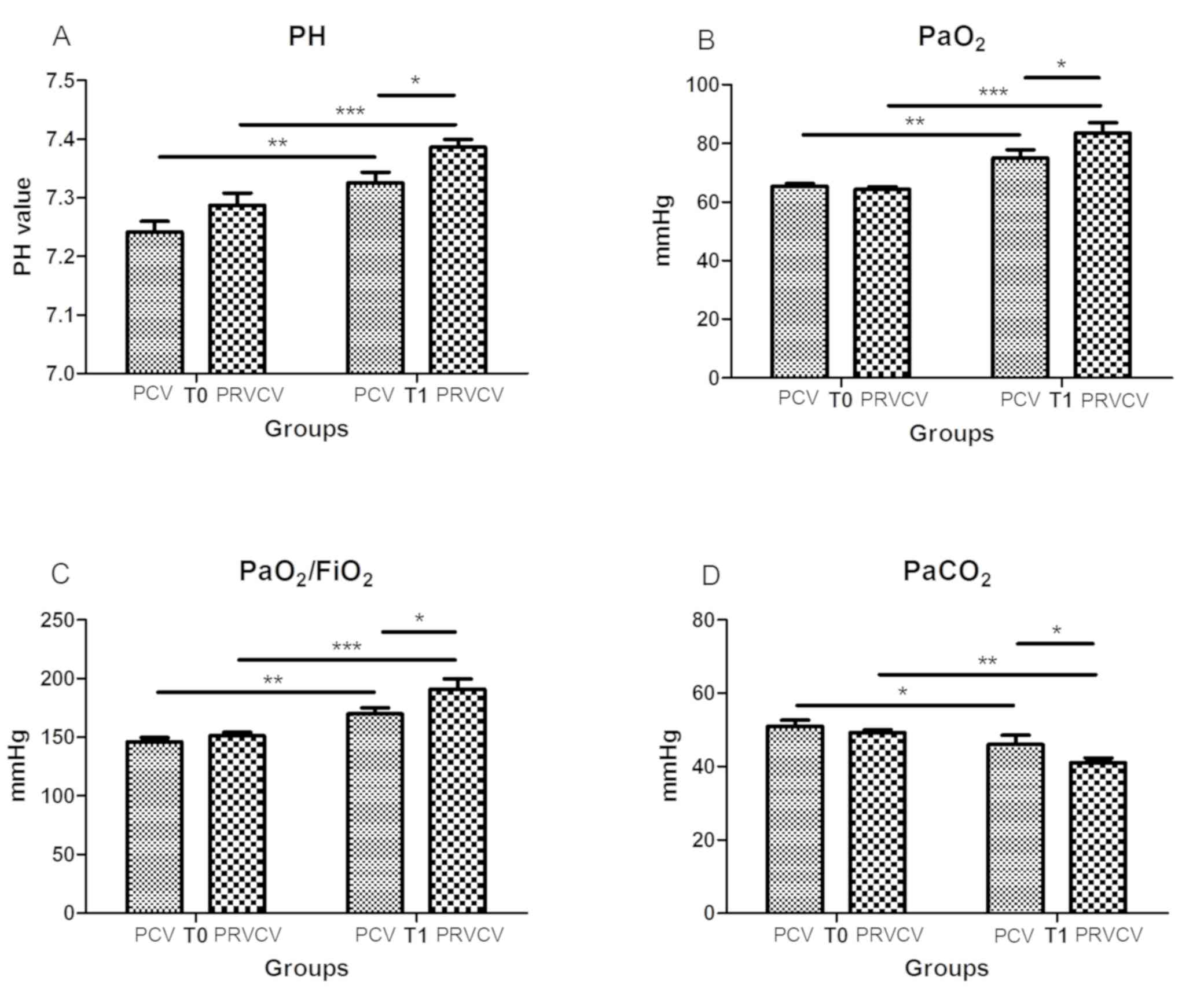 | Figure 2.Differences in arterial blood gas
parameters between the PRVCV and PCV modes. (A) pH, (B)
PaO2, (C) PaO2/FiO2 and (D)
PaCO2. *P<0.05, **P<0.01, ***P<0.001. T0, at
the beginning of mechanical ventilation; T1, 6 h after ventilation;
PCV, pressure control ventilation; PRVCV, pressure-regulated volume
control ventilation; PaO2, partial pressure of
O2; PaCO2, partial pressure of
CO2; FiO2, fraction of inspired
O2. |
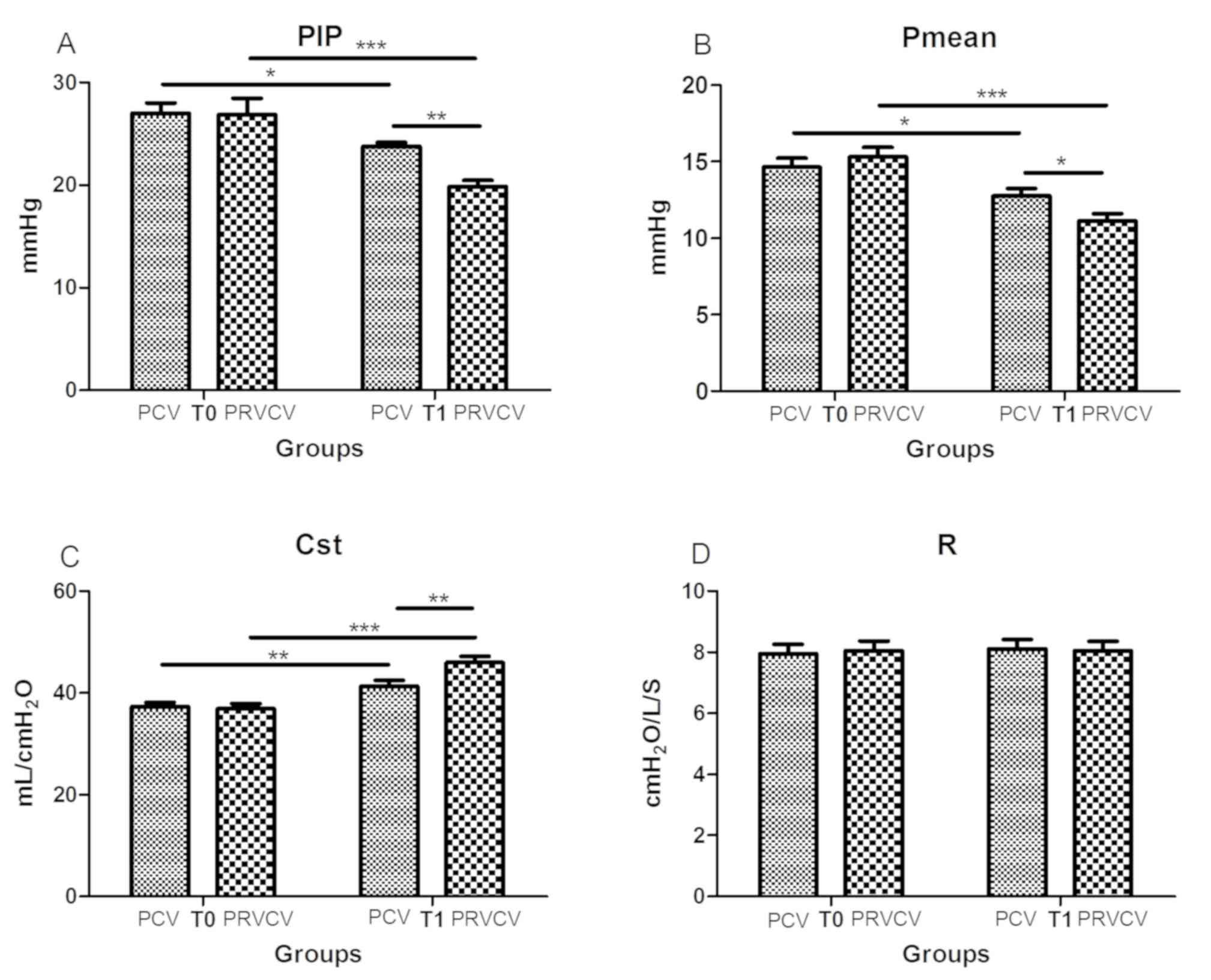
Outcomes regarding respiratory
mechanics
PIP, Pmean and Cst were ameliorated
following treatment (all P<0.05). Compared with those obtained
using the PCV mode, the PRVCV mode achieved a notably reduced PIP
(23.75±1.77 vs. 19.85±2.70 mmHg, P=0.008) and Pmean
(12.75±2.24 vs. 11.15±2.03 mmHg, P=0.043), and an increased Cst
(41.35±4.99 vs. 45.95±5.71 ml/cmH2O, P=0.003). However,
no significant difference was obtained in R (8.11±1.38 vs.
8.06±1.34 cmH2O/l/sec, P>0.05) between the two groups
(Fig. 3).
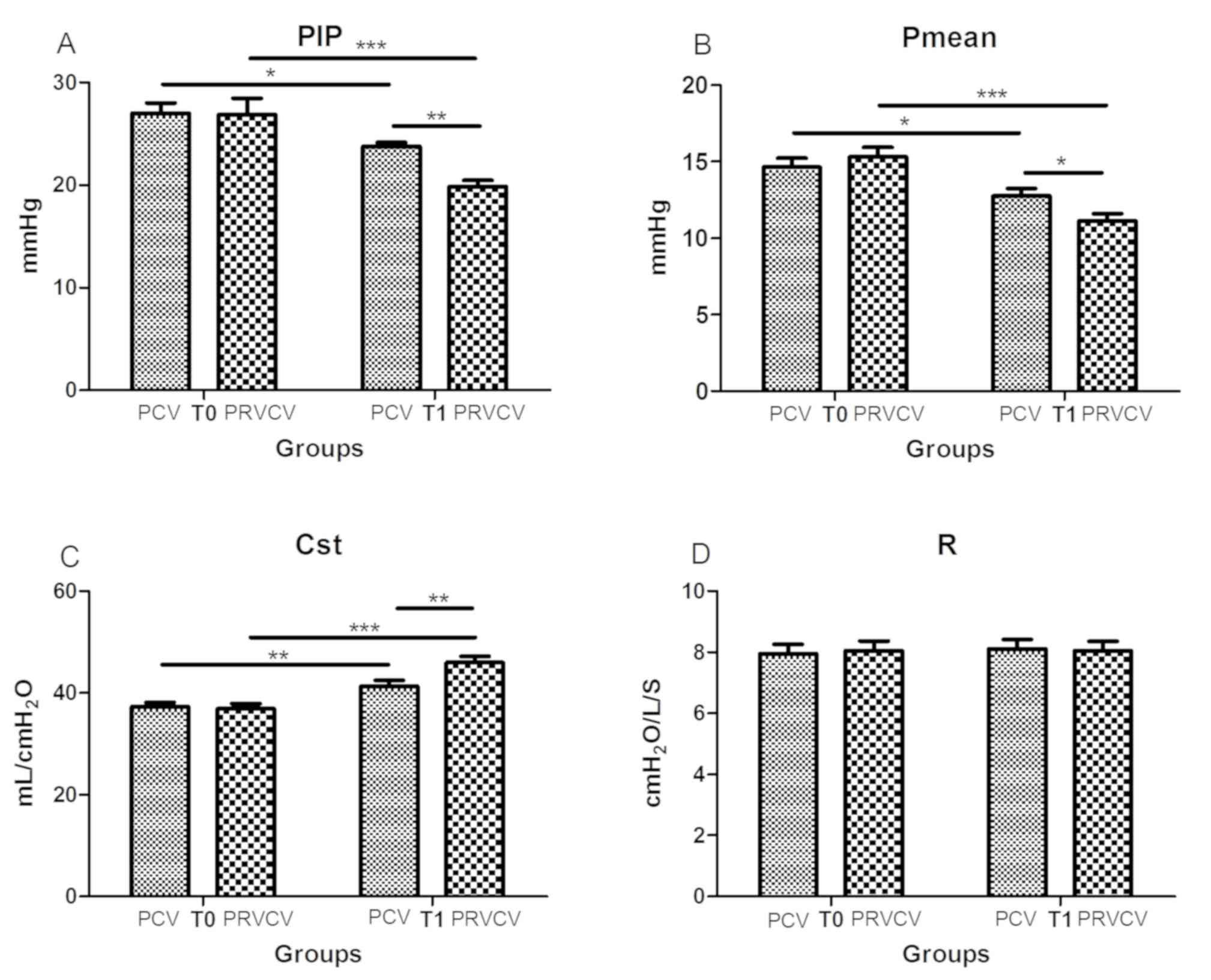 | Figure 3.Differences in respiratory mechanics
(PIP, Pmean, Cst and R) between PRVCV and PCV modes. (A)
PIP, (B) Pmean, (C) Cst and (D) R. There was no
difference between the two groups in R. *P<0.05, **P<0.01,
***P<0.001. T0, at the beginning of mechanical ventilation; T1,
6 h after ventilation; PCV, pressure control ventilation; PRVCV,
pressure-regulated volume control ventilation; PIP, peak
inspiratory pressure; Pmean, mean inspiratory pressure;
Cst, pulmonary static compliance; R, airway resistance. |
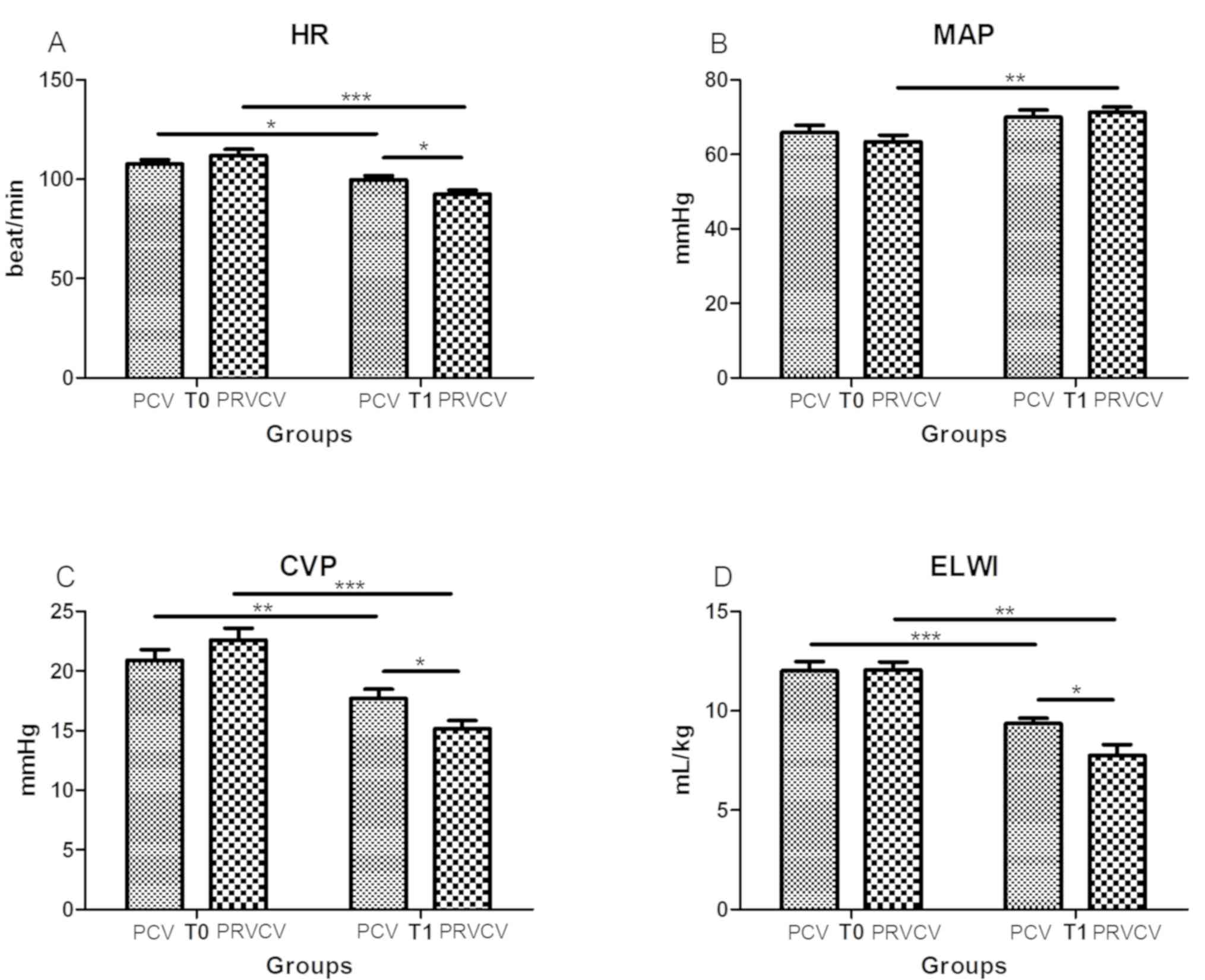
Outcomes of hemodynamics
HR, CVP and ELWI in the PRVCV and PCV groups were
significantly decreased following treatment (all P<0.05), and
MAP in the PRVCV group was significantly increased following
treatment (P<0.01). Compared with those in the PCV group, the
PRVCV group exhibited a significantly decreased CVP (17.70±3.50 vs.
15.15±3.13 mmHg, P=0.037), ELWI (9.35±1.27 vs. 7.75±2.49 ml/kg,
P=0.012) and HR (99.65±9.76 vs. 92.60±8.17 beats/min, P=0.036),
while the MAP was not significantly different (70.00±8.38 vs.
71.30±6.13 mmHg, P=0.594; Fig.
4).
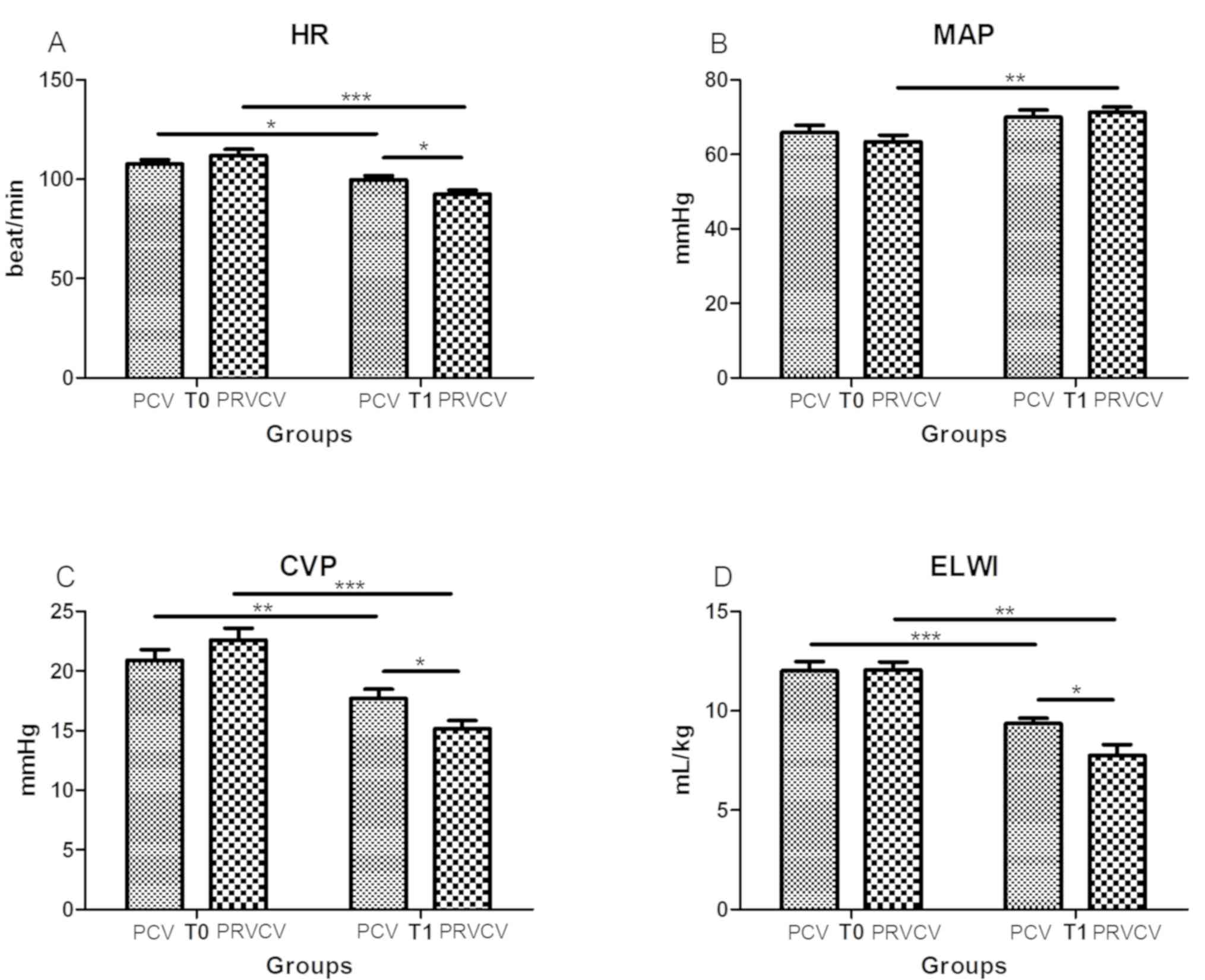 | Figure 4.Differences in hemodynamics between
PRVCV and PCV modes. (A) HR, (B) MAP, (C) CVP and (D) ELWI. No
change was seen in MAP. *P<0.05, **P<0.01, ***P<0.001. T0,
at the beginning of mechanical ventilation; T1, 6 h after
ventilation; PCV, pressure control ventilation; PRVCV,
pressure-regulated volume control ventilation; HR, heart rate; MAP,
mean arterial pressure; CVP, central venous pressure; ELWI,
extravascular lung water index. |
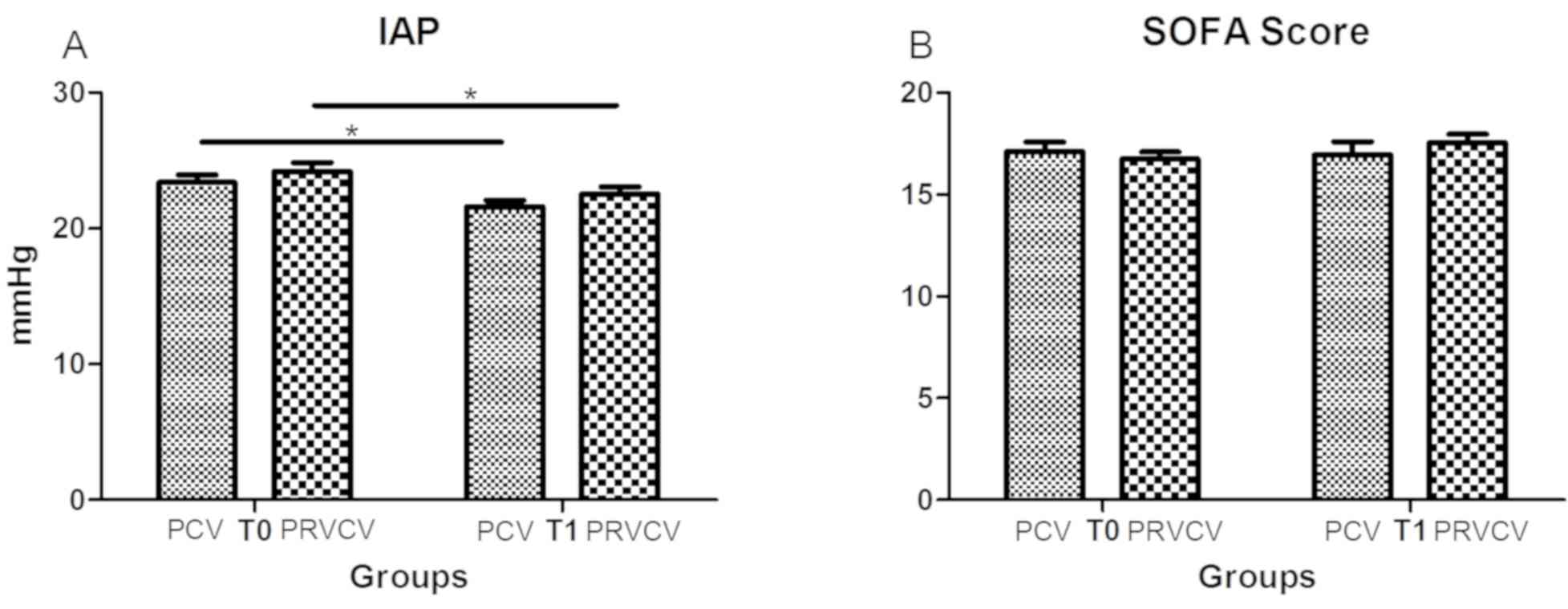
Outcomes regarding IAP and SOFA
scores
No significant differences in IAP (22.55±2.28 vs.
21.60±2.19 mmHg, P=0.222) and SOFA scores (17.55±1.88 vs.
16.95±2.93, P=0.386) were observed between the PRVCV and PCV groups
(Fig. 5). However, the IAP was
reduced in the two groups following treatment (both P<0.05).
Discussion
ACS is a critical condition requiring mechanical
ventilation. In the present study, it was indicated that compared
with those in the PCV group, patients that received PRVCV exhibited
a significant decrease in respiratory parameters, including
PaCO2, airway PIP, Pmean, CVP, HR and ELWI.
In addition, significant improvements in pH, PaO2,
oxygenation index and Cst were achieved by using PRVCV as compared
to PCV. However, no significant differences were observed in R,
MAP, IAP and SOFA scores between the two groups. Thus, PRVCV
provides satisfactory and stable ventilation at the lowest possible
pressure level, which relieves injury by positive pressure
ventilation and increases safety. It is therefore more suitable for
patients with ACS, and may be used as a lung protective
strategy.
ACS refers to organ dysfunction and
ischemia-reperfusion injury resulting from IAH, which may be a
consequence of abdominal trauma, intestinal obstruction or severe
acute pancreatitis (11,12). ACS affects the normal functioning of
the cardiovascular, respiratory and urinary systems. The synergy
between these organ systems further increases the IAP, which
results in a vicious cycle of organ damage and IAH, finally leading
to multiple organ failure (13–15). A
recent multi-center prospective study reported that 32.1% of ICU
patients were diagnosed with IAH and 4.2% with ACS (16). The IAP acts on the diaphragm and
constricts the pulmonary segment, leading to alveolar collapse and
a decreased ventilation to blood flow ratio, which causes
hypoxemia, hypercarbia and ultimately respiratory failure (17,18).
Patients with mechanical ventilation and ACS have a higher risk of
developing IAH than those without ACS (19,20).
Verzilli et al (21) reported that the fluctuation range of
the IAP was lowest when the PEEP was between 6 and 12 mmHg in
patients requiring mechanical ventilation. In the present study,
the PEEP was maintained between 6 to 12 mmHg, since the optimum
PEEP value reduces the extravascular lung water content and
improves chest wall compliance. In PCV mode, the pressure is fixed,
which results in insufficient ventilatory capacity. Similarly, the
ventilatory capacity in the volume control ventilation (VCV) mode
is also fixed, but a lack of pressure control further increases the
risk of pressure-induced injury. Since an excessive tidal volume
results in repeated alveolar folding, the alveolar epithelium and
endothelium are frequently deteriorated in patients with IAH.
PRVCV is a dual-control ventilation mode that avoids
the high peak airway pressures of volume ventilation, as well as
the variation in tidal volume that may occur with pressure
ventilation. The compliance of thorax and lung are calculated
during the first ventilation, followed by the inspiratory pressure
of the preset tidal volume in the next ventilation. The actual
inspiratory pressure is 75% of the expected value, whereas the
actual tidal volume is consistent with the preset value (5–7). The
ventilator continuously monitors compliance and automatically
calculates the association between volume and pressure on the basis
of the preset tidal volume. It regulates the next inspiratory
pressure level according to anterior monitoring, thereby minimizing
the airway pressure. In other words, stable ventilation is provided
at the lowest possible ventilation pressure to minimize the chances
of bariatric injury due to positive pressure ventilation, and
enhance the safety of the treatment. In the present study, the ABG
parameters were distinctly improved in the PRVCV mode compared with
those in the PCV mode. At the same PEEP level, the oxygenation
index was improved and the PaCO2 was significantly
declined with PRVCV as compared with PCV.
A great number of pathophysiological changes occur
due to IAH, including an increase in thoracic pressure and CVP, a
decrease in the returned blood volume and a compensatory increase
in the HR, and finally respiratory failure, which calls for
ventilatory support (22–24). The present study demonstrated that
compared with those obtained by PCV, the PIP, Pmean and
Cst were significant improved, all which is beneficial to the
respiratory system of patients, with PRVCV. The significant
decrease in CVP and ELWI in the PRVCV group may be due to improved
compliance and reduced thoracic pressure. The HR was also lower in
the PRVCV compared with that in the PCV group, partly because the
increased compliance of lung and thorax lead to an augmentation of
the returned blood volume. No significant difference was observed
in MAP, a parameter that is influenced by multiple aspects,
including treatment interventions.
Apart from ABG, significant improvements were also
observed in respiratory mechanics and hemodynamics. However, the
SOFA score was not improved in the present study, due to two
possible reasons: First, the present study only assessed the
respiratory and cardiovascular systems, whereas the SOFA score
encompasses a total of six systems (25,26), and
furthermore, an observation time of 6 h may not have been
sufficient to improve the SOFA score. Therefore, a follow-up
experiment with longer post-ventilation time is required. The
present study was a prospective cohort study with a limited sample
size, which may have affected the difference in outcome this was a
limitation of the study. Additional randomized controlled trials
may be helpful for comparing the two ventilation modes. It may be
concluded that the PRVCV mode combines the advantages of VCV and
PCV, and may provide stable tidal volume at the lowest possible
peak airway pressure and MAP, and is a lung protective mode that
may reduce the risk of barotrauma in patients with IAH or ACS.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from National
Nature Science Foundation of China (grant no. 81500351) and the
Jiangsu Provincial Key Research and Development Program (grant no.
BE2016721).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
BW designed the study and wrote the manuscript. JY,
JJ, XP and SS performed the experiments and analyzed the data. All
authors read and approved the final manuscript.
Ethical approval and consent to
participate
The present study was approved by the Medical
Research Ethical Committee of Jiangsu University (Zhenjiang, China)
and all subjects provided written informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kirkpatrick AW, Roberts DJ, De Waele J,
Jaeschke R, Malbrain ML, De Keulenaer B, Duchesne J, Bjorck M,
Leppaniemi A, Ejike JC, et al: Intra-abdominal hypertension and the
abdominal compartment syndrome: Updated consensus definitions and
clinical practice guidelines from the world society of the
abdominal compartment syndrome. Intensive Care Med. 39:1190–1206.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Arabadzhiev GM, Tzaneva VG and Peeva KG:
Intra-abdominal hypertension in the ICU-a prospective
epidemiological study. Clujul Med. 88:188–195. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Papavramidis TS, Marinis AD, Pliakos I,
Kesisoglou I and Papavramidou N: Abdominal compartment
syndrome-Intra-abdominal hypertension: Defining, diagnosing, and
managing. J Emerg Trauma Shock. 4:279–291. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Smit M, Buddingh KT, Bosma B, Nieuwenhuijs
VB, Hofker HS and Zijlstra JG: Abdominal compartment syndrome and
intra-abdominal ischemia in patients with severe acute
pancreatitis. World J Surg. 40:1454–1461. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aghadavoudi O, Alikiaii B and Sadeghi F:
Comparison of respiratory and hemodynamic stability in patients
with traumatic brain injury ventilated by two ventilator modes:
Pressure regulated volume control versus synchronized intermittent
mechanical ventilation. Adv Biomed Res. 5:1752016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dion JM, McKee C, Tobias JD, Sohner P,
Herz D, Teich S, Rice J, Barry ND and Michalsky M: Ventilation
during laparoscopic-assisted bariatric surgery: Volume-controlled,
pressure-controlled or volume-guaranteed pressure-regulated modes.
Int J Clin Exp Med. 7:2242–2247. 2014.PubMed/NCBI
|
|
7
|
Gruber PC, Gomersall CD, Leung P, Joynt
GM, Ng SK, Ho KM and Underwood MJ: Randomized controlled trial
comparing adaptive-support ventilation with pressure-regulated
volume-controlled ventilation with automode in weaning patients
after cardiac surgery. Anesthesiology. 109:81–87. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Samantaray A and Hemanth N: Comparison of
two ventilation modes in post-cardiac surgical patients. Saudi J
Anaesth. 5:173–178. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Barr J, Kishman CP Jr and Jaeschke R: The
methodological approach used to develop the 2013 pain, agitation,
and delirium clinical practice guidelines for adult ICU patients.
Crit Care Med. 41 (9 Suppl 1):S1–S15. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jaipuria J, Bhandari V, Chawla AS and
Singh M: Intra-abdominal pressure: Time ripe to revise management
guidelines of acute pancreatitis? World J Gastrointest
Pathophysiol. 7:186–198. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hunt L, Frost SA, Hillman K, Newton PJ and
Davidson PM: Management of intra-abdominal hypertension and
abdominal compartment syndrome: A review. J Trauma Manag Outcomes.
8:22014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Prasad GR, Subba Rao JV, Aziz A and Rashmi
TM: The role of routine measurement of intra-abdominal pressure in
preventing abdominal compartment syndrome. J Indian Assoc Pediatr
Surg. 22:134–138. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Atema JJ, van Buijtenen JM, Lamme B and
Boermeester MA: Clinical studies on intra-abdominal hypertension
and abdominal compartment syndrome. J Trauma Acute Care Surg.
76:234–240. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dalfino L, Sicolo A, Paparella D, Mongelli
M, Rubino G and Brienza N: Intra-abdominal hypertension in cardiac
surgery. Interact Cardiovasc Thorac Surg. 17:644–651. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Díaz F, Erranz B, Donoso A, Salomon T and
Cruces P: Influence of tidal volume on pulse pressure variation and
stroke volume variation during experimental intra-abdominal
hypertension. BMC Anesthesiol. 15:1272015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tiwari AR and Pandya JS: Study of the
occurrence of intra-abdominal hypertension and abdominal
compartment syndrome in patients of blunt abdominal trauma and its
correlation with the clinical outcome in the above patients. World
J Emerg Surg. 11:92016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kyoung KH and Hong SK: The duration of
intra-abdominal hypertension strongly predicts outcomes for the
critically ill surgical patients: A prospective observational
study. World J Emerg Surg. 10:222015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Muturi A, Ndaguatha P, Ojuka D and Kibet
A: Prevalence and predictors of intra-abdominal hypertension and
compartment syndrome in surgical patients in critical care units at
Kenyatta National Hospital. BMC Emerg Med. 17:102017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rastogi P, Iyer D, Aneman A and D'Amours
S: Intra-abdominal hypertension and abdominal compartment syndrome:
Pathophysiological and non-operative management. Minerva
Anestesiol. 80:922–932. 2014.PubMed/NCBI
|
|
20
|
Zhao JG, Liao Q, Zhao YP and Hu Y:
Mortality indicators and risk factors for intra-abdominal
hypertension in severe acute pancreatitis. Int Surg. 99:252–257.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Verzilli D, Constantin JM, Sebbane M,
Chanques G, Jung B, Perrigault PF, Malbrain M and Jaber S: Positive
end-expiratory pressure affects the value of intra-abdominal
pressure in acute lung injury/acute respiratory distress syndrome
patients: A pilot study. Crit Care. 14:R1372010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ortiz-Diaz E and Lan CK: Intra-abdominal
hypertension in medical critically ill patients: A narrative
review. Shock. 41:175–180. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shaheen AW, Crandall ML, Nicolson NG,
Smith-Singares E, Merlotti GJ, Jalundhwala Y and Issa NM: Abdominal
compartment syndrome in trauma patients: New insights for
predicting outcomes. J Emerg Trauma Shock. 9:53–57. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kollias S, Stampolidis N, Kourakos P,
Mantzari E, Koupidis S, Tsaousi S, Dimitrouli A, Atiyeh B and
Castana O: Abdominal compartment syndrome (ACS) in a severely
burned patient. Ann Burns Fire Disasters. 28:5–8. 2015.PubMed/NCBI
|
|
25
|
de Freitas GR, da Fonseca-Neto OC,
Pinheiro CL, Araújo LC, Barbosa RE and Alves P: Relationship
between Sequential Organ Failure Assessment (SOFA) and
intra-abdominal pressure in intensive care unit. Arq Bras Cir Dig.
27:256–260. 2014.(In English, Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
26
|
de Grooth HJ, Geenen IL, Girbes AR,
Vincent JL, Parienti JJ and Oudemans-van Straaten HM: SOFA and
mortality endpoints in randomized controlled trials: A systematic
review and meta-regression analysis. Crit Care. 21:382017.
View Article : Google Scholar : PubMed/NCBI
|