Introduction
The incidence of Alzheimer's disease (AD) is
increasing rapidly with aging populations worldwide and has given
rise to a series of medical and social-economic problems (1). It has been reported that 44.35 million
people were diagnosed with AD worldwide in 2013, a number which may
increase and to 75.62 million by 2030 and 135.46 million by 2050
(2). Thus, the pathogenesis of AD
and its prevention and treatment is of great importance to medical
research.
AD is a neurodegenerative disease that frequently
occurs in the senior population and is characterized by progressive
dementia (2). AD has also been
demonstrated to be influenced by a variety of factors (3), in which the major manifestation is the
appearance of senile plaques (SP). SP is associated with the
aggregation and accumulation of amyloid-beta (Aβ) peptides in the
cerebral cortex and hippocampus of the human brain (4). Aggregated and accumulated Aβ peptides
have also been reported to induce the abnormal phosphorylation of
tau proteins, leading to neurofibrillary tangle formation, which
serves an important role in AD pathogenesis (5). It is therefore important to determine
novel drug candidates to prevent the development of AD and to treat
patients with AD.
Monochasma savatieri Franch, a member of the
Scrophulariaceae family, is widely distributed through certain
areas of Southern China (6). It is
also a traditional Chinese medicine that is used to treat many
diseases, including the common cold, cough and diarrhea (6). Extracts of Monochasma savatieri
Franch obtained from the Jiangsu province of China was reported
to possess bioactive ingredients for treatment of the
aforementioned diseases (7,8). These extracts were revealed to be
composed of two types of phenylethanoid glycosides (PhGs):
Torenoside B (TB) and Savatiside A (SA) (6).
PhGs exhibit a wide range of bioactivities for the
treatment of disease. For instance, they may be used as
anti-immunomodulatory, anti-oxidative, anti-inflammatory,
anti-bacterial, anti-tumor, and anti-influenza virus agents. They
may also be used as potential drugs for kidney protection and
laxative effect treatments (9).
Previous studies have revealed that PhGs extracts can be used to
treat a variety of coronary artery diseases (7), respiratory infections and pneumonia
(10). In a recent report, PhGs were
demonstrated to influence the structure and function of neurons and
thus, may be used as neuroprotective agents against
H2O2 and Aβ1-42-induced injury in
PC12 cells (11). This observation
is further supported by a dramatic neuroprotective effect exhibited
by Forsythenethosides A and B, two PhGs extracted from Forsythia
suspense, against PC12 cell damage induced by the deprivation
of serum (12).
According to previous studies, PhGs are considered
to be potential drug candidates for the treatment of AD (7,8,10). However, few reports assess the
neuroprotective effect of TB and SA extracted from Monochasma
savatieri Franch, in the treatment of AD as well as the signal
pathways utilized. In the present study, in vitro and in
vivo AD experimental models were constructed and the effects of
TB or SA on these models were assessed. The Aβ fragment 25–35
(Aβ25-35), a short proteolytic fragment of the
full-length Aβ peptide, is known to exhibit neurotoxicity (13). This fragment was utilized as a
substrate for the induction of AD in the cell and small animal
models of the current AD treatment study.
Materials and methods
Materials and ethics statement
SA and TB utilized in the current study were
provided by the Department of Natural Medicine Chemistry, Suzhou
University (Suzhou, China) and Aβ25-35 was obtained from
BIOSS (Beijing, China). MTT was purchased from Sigma-Aldrich (Merck
KGaA, Darmstadt, Germany). Galantamine (Gal) was provided by
J&K Scientific, Ltd. (Beijing, China). The SH-SY5Y cell line
was purchased from the American Type Culture Collection
(ATCC® CRL-2266™; Manassas, VA, USA). All animal
experiments were approved by the Animal Ethics Committee of Soochow
University (Suzhou, China) and all procedures were performed in
strict accordance with the protocols of the Care and Use of
Laboratory Animals and related norms of the animal laboratory of
Soochow University (Suzhou, China).
SH-SY5Y cell culture and treatment
viability
SH-SY5Y cells were cultured in F12/MEM medium
(Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA)
supplemented with 10% fetal bovine serum (Gibco; Thermo Fisher
Scientific, Inc.) in an incubator with 5% CO2 at 37°C.
After cells reached a confluence of 70–80%, they were digested with
0.05% trypsin and transferred to the logarithmic growth phase.
SH-SY5Y cells (1×105 cells/ml) were then inoculated into
the wells of a 96-well plate at a density of 1×104
cells/well and cultured for 24 h at 37°C in an incubator with 5%
CO2.
Cell-cultured wells were subsequently divided into
the Aβ25–35 induced group, the Aβ25–35+SA
treated group, the Aβ25–35+TB treated group and the
blank group (utilized as a control). Cultured cells were pretreated
with 25, 50 and 100 µM of SA or TB, and were induced with 30 µM
Aβ25–35 for 24 h. An MTT assay was then performed to
assess the viability of cells following SA and TB treatments. A
total of 10 µl 5 mg/ml MTT was added into wells and incubated for 4
h at 37°C. The supernatant in the well was removed and 100 µl of
dimethyl sulfoxide (DMSO) was added. The plate was then incubated
for 10 min at room temperature and a fully-automatic microplate
reader was utilized to measure the absorbance at a wavelength of
570 nm [optical density (OD)570 nm]. The wells of the
control group were cultured as aforementioned, except with the same
volume of 1× PBS buffer instead of the assessed PhGs. Cell
viability was calculated using the following formula: Cell
viability rate %=(OD570 nm (experiment group)/OD570
nm (normal group)) ×100%. Measurements for each sample were
performed in triplicate to achieve the deviation.
Assessment of SH-SY5Y morphological
changes
Following the manufacturer's protocol, the Gimesa
assay kit (Nanjing Jiancheng Bioengineering Institute, Nanjing,
China) was utilized for the staining of SH-SY5Y cells with or
without the SA and TB treatments. Stained cells were then rinsed
with water and air dried at room temperature. An inverted optical
microscope (Eclipse TE2000-U; Nikon Corporation, Tokyo, Japan;
magnification, ×400) was used to observe the morphology of SH-SY5Y
cells. Images were obtained using Olympus Image-ProPlus 6.0
(Olympus Corporation, Tokyo, Japan). The morphological changes of
treated SH-SY5Y cells were compared with the control group.
Detection of reactive oxygen species
(ROS)
Suspended cells (1×105 cells/ml; 2 ml)
were seeded in 6-well plates and cultured for 24 h in an incubator
at 37°C with 5% CO2. Wells were grouped into treatment
and control groups as aforementioned. Subsequently, the medium was
removed and cells were washed once with 1× PBS buffer. A
dichlorofluorescin diacetate (DCFH-DA) assay was then performed to
measure the ROS content in cells. Serum-free F12/MEM medium (200
µl) containing 10 µM DCFH-DA (Beyotime Institue of Biotechnology,
Hiamen, China) was added to each well of the 6-well plate. Cells
were then incubated for 10 min at room temperature, washed once
with 1× PBS and digested with 0.05% trypsin to obtain the
suspension. Suspended cells were recovered via centrifugation at
12,000 × g for 15 min at 4°C and washed twice with 1× PBS. Cells
were subsequently suspended in 1× PBS buffer with a final volume of
300 µl. ROS content was measured using a flow cytometer (Beckman
Coulter, Inc., Brea, CA, USA) with an excitation wavelength at 488
nm and emission at 525 nm. Immunofluorescence signals were also
quantified by ImageJ software v1.8.0 (National Institutes of
Health, Bethesda, MD, USA) ROS content in all groups were
obtained.
Detection of Ca2+
concentration
Cell Ca2+ concentration was measured
using the Ca2+ Fluo-3AM (Beyotime Institute of
Biotechnology) staining kit. SH-SY5Y cells were cultured in a
6-well plate as aforementioned. Prior to cell staining, culture
medium was removed from wells and cells were washed once with 1×
PBS buffer. PBS solution (1×; 5 ml) with 5 µM Ca2+
Fluo-3AM was added to each well and incubated for 30 min at 37°C.
PBS solution was removed and wells were washed once with 1× PBS
buffer to remove extra dye. Cells were then digested with 0.05%
trypsin and collected via centrifugation at 12,000 × g for 15 min
at 4°C. Subsequently, cells were suspended in 1× PBS buffer. Upon
excitation at 506 nm, the fluorescence intensity of suspended cells
was measured at 526 nm using a flow cytometer. Fluorescence
intensity was then used to estimate the concentration of
Ca2+.
Quantification detection of
apoptosis
For flow cytometric analysis, Hippocampal neurons
were collected and diluted with PBS. Apoptosis was measured via
flow cytometry using the Annexin V-EGFP/PI Apoptosis Detection kit
(Beyotime Institute of Biotechnology) according to the
manufacturer's protocol. Cell suspensions (100 µl) were added to
100 µl annexin V and 10 µl PI, incubated for 20 min at room
temperature and analyzed using the MUSE cell analyzer (EMD
Millipore, Billerica, MA, USA).
Western blot analysis
Western blotting was utilized to measure the
expression of protein in cells. Proteins were extracted from cells
using a cell lysate (radioimmunoprecipitation assay buffer) and
then determined using a modified Folin-Ciocalteu assay. Samples (20
µg) were then denatured using 10% sodium dodecyl sulfate and then
run on a 12% SDS-PAGE. Subsequently, samples were transferred to a
polyvinylidene difluoride membrane (EMD Millipore) and rinsed with
TRIS-buffered saline with 0.5% Tween-20 for 5 min. Membranes were
immersed in 5% Bovine Serum Albumin (cat. no. 0332; Sangon Biotech
Co., Ltd., Shanghai, China) for 2 h at room temperature, washed
with 1× PBS buffer. Anti-Calnexin (1:500; rabbit polyclonal
antibody; cat. no. 2433; Cell Signaling Technologies, Inc.,
Danvers, MA, USA) and anti-β-actin (mouse monoclonal antibody; cat.
no. 3700; Cell Signaling Technology, Inc.) antibodies were diluted
with PBST (1:5,000), then incubated overnight at 4°C. Membranes
were subsequently washed with TBST buffer for 3×15 min and then
immersed in 1× PBS buffer. Horseradish peroxidase-conjugated sheep
anti-mouse and anti-rabbit antibodies (anti-mouse cat. no. NA931;
anti-rabbit cat. no. NA934V; each, 1:3,000; GE Healthcare, Chicago,
IL, USA) were subsequently added to the solution and incubated for
1 h at 37°C. Samples were kept in the dark to avoid exposure to
light. Membranes were then washed with TBST buffer for 3×10 min.
The density of each protein band was visualized with an ECL
detection kit (Thermo Fisher Scientific, Inc.) and quantified using
SigmaScan-pro V5.01 (SPSS, Inc., Chicago, IL, USA). The results
were used to evaluate the expression of protein in cells.
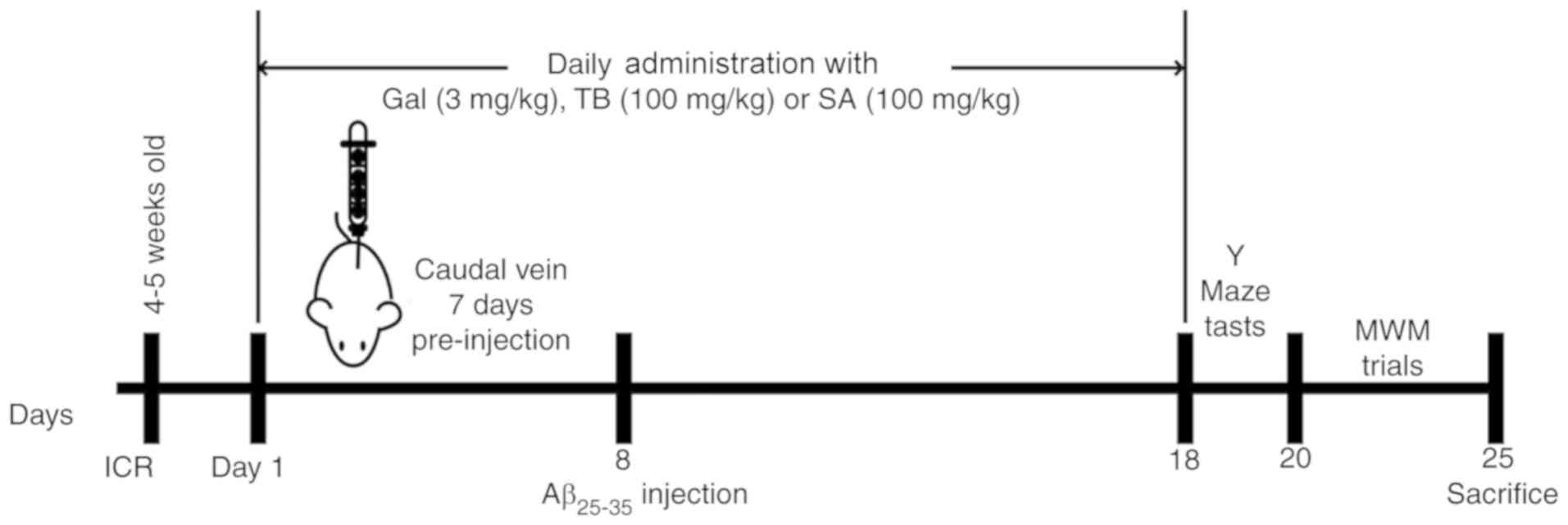
Animal model construction
A total of 15 male Institute of Cancer Research mice
(clean grade; 6–8 weeks; weight, 18–22 g) were obtained from
Shanghai SLAC Laboratory Animal Co., Ltd. (Shanghai, China).
Animals were housed in a quiet laboratory at a controlled
temperature of 22±2°C and a humidity of 50±10% with free access to
food and water, under a 12 h light/dark cycle. Mice were randomly
divided into 5 groups (each, n=3): The blank control, the
Aβ25–35, the Gal + Aβ25–35, the SA +
Aβ25–35 and the TB + Aβ25–35 group.
Mice in the treatment groups were administered a
pre-injection via the caudal vein for 7 consecutive days with the
following agents at various dosages: Gal, 3 mg/kg/d, SA, 100
mg/kg/d and TB, 100 mg/kg/d. Mice of the control group and the
Aβ25–35 group were injected with 10 µl saline. The
experimental procedure was in accordance with a previous study
(14). On the 8th day, following
anesthetization, mice were secured on a stereotaxic instrument. A
10 µl microsyringe was vertically inserted 2.46 mm posterior to the
bregma, at a 2 mm lateral and 2 mm depth under the cortical
surface. Mice in the Aβ25–35 treatment groups were
injected with 3 µl of Aβ25–35 solution (3.4 µg/µl),
while mice in the control group received an equal volume of normal
saline. The injection speed was kept constant at 1 µl/min and was
performed according to the previous study (15). Needles were retained for >5 min
and then slowly withdrawn by 1 mm. According to a previous and to
personal experience, the volume of injection to the hippocampus
does not result in extensive/non-specific neuronal damage (14).
Following surgery, injured mice were kept warm (at
37°C ± 2°C) until their conscious recovery and were then housed
under a constant temperature (22°C ± 2°C). Following 24 h, mice in
the treatment groups were administered intravenous SA, TB or Gal (a
routine drug for the treatment of learning and memory disorder).
Mice in the control and Aβ25–35 induced groups were
injected with 10 µl vehicle (saline). On the 18th day, all mice
participated in behavioral experiments. Histopathological changes
of hippocampal morphology and neuronal ultra-structures, and the
changes of relative biochemical parameters were subsequently
assessed.
Y-maze test
Following the last drug administration, mice were
subjected to the Y-maze test for the assessment of spatial
recognition memory, as previously described (16). The tests were performed for 3
continuous days. The passive avoidance test was performed to assess
short-term learning ability. Following a single training trial,
time latency was measured (consolidation trial). The room in which
tests were performed was kept quiet and dark. The number of correct
responses (scored from 0 to 20) was recorded in the test.
Morris water maze test
The Morris water maze test was performed following a
routine procedure at the Institute of Materia Medica, Chinese
Academy of Medical Sciences and Peking Union Medical College. Mice
were trained to swim 3 times a day for 5 consecutive days, as
described previously (14). Mice
were then placed into a pool of water at a desired start point and
then forced to swim. The recorded latency period was considered to
be the time taken for mice to locate and climb the fixed platform.
If the latency time exceeded 60 sec, mice were led to the platform
and 60 sec was recorded. Mice were subsequently removed from the
platform within 10 sec following arrival and then run to the next
training procedure (probe trial) (17). The data acquisition and analysis were
completed using EthoVision XT7 (Noldus Information Technology BV,
Wageningen, The Netherlands).
H&E and Nissl staining
After the aforementioned behavioral tests were
performed, mice were immediately anesthetized with 400 mg/kg IP 10%
chloral hydrate and then sacrificed via cardiac perfusion with
saline solution, followed by ice-cold 4% paraformaldehyde in 0.1M
phosphate buffer (pH 7.0) as described previously (17). No signs of peritonitis were observed
following anesthetic administration. All mice were sacrificed
following behavioral tests. The brains of three randomly selected
mice from each group were removed and fixed in 4% paraformaldehyde
solution for 24 h at 4°C. Tissues were subsequently embedded in
paraffin and cut into 4 µm thick sections. Samples were stained
with H&E and Nissl dyes as contrast agents via a routine
staining protocol. Histopathological changes in the hippocampal CA1
region were observed using an optical microscope (magnification,
×400). H&E stained brain tissues from an additional three mice
in each group were subsequently stained with hematoxylin solution
for 3 min and NISSL staining with 1% toluidine blue staining
solution for 10 min at room temperature. Samples were then
dehydrated rapidly with 95% alcohol, cleared with xylene and
mounted with the neutral resin. A high-power optical microscope
(magnification, ×400) was used to observe the tissue. Three
randomly selected visual fields were used and the number and rate
of positive cells were counted and calculated from the images.
Transmission electron microscopy
(TEM)
Three other mice were then selected from each group,
anesthetized and sacrificed as aforementioned. The hippocampal
tissues of mice were then obtained. Tissue was fixed with
pre-cooled 2.5% glutaraldehyde solution at 4°C for over 4 h. The
hippocampal CA1 region was subsequently isolated, washed twice with
10 mM PBS buffer and fixed in 1% osmic acid solution at 4°C for 1
h. Fixed tissues were then washed twice with 10 mM PBS buffer and
treated via a routine protocol including dehydration with acetone,
preservation overnight at room temperature in 70% acetone solution
with saturated uranyl acetate (Amresco, LLC, Solon, OH, USA),
dehydrating further with acetone and embedding using the SPURR
embedding kit (TAAB Laboratories Equipment Ltd., UK). The treated
tissue sections were sieved using 200-mesh copper grids, stained
with uranyl acetate for 30 min at room temperature and further
stained with lead nitrate (or lead citrate) at room temperature for
30 min. A H-600 TEM (Hitachi, Ltd., Tokyo, Japan) was used to
obtain high-resolution tissue images.
Maleic dialdehyde (MDA) content and superoxide
dismutase (SOD), glutathione peroxidase (GSH-PX) and
acetylcholinesterase (AChE) activity. MDA content (cat. no. A003-1)
and the enzyme bioactivity of SOD (cat. no. A001-3), GSH-PX (cat.
no. A005) and AChE (cat. no. A024) in murine tissue were determined
to assess the biochemical changes observed following drug
treatment. All measurements were obtained using corresponding
detection kits (Nanjing Jiancheng Bioengineering Institute)
following the manufacturer's protocol.
Statistical analysis
All statistical data were analyzed using SPSS
software v. 17.0 (SPSS Inc., Chicago, IL, USA) and data are
presented as the mean ± standard error of the mean. Differences
between two groups were analyzed via a Student's t-test and among
multiple groups via one-way analysis of variance followed by a
least-significant difference test. P<0.05 was considered
to indicate a statistically significant difference.
Results
In the current study, PhG extracts from
Monochasma savatieri Franch, including TB and SA, were
assessed for their neuroprotective effects as well as their
potential to prevent and treat AD development. Their specific
signaling pathways and medical effects were also assessed. A
detailed flow chart of the in vivo and in vitro
experimental design is presented in Fig.
1. In addition to the biochemical and medical mechanisms
utilized by TB and SA, behavioral and neuroscientific tests were
performed to assess murine spatial learning and memory following
Aβ25-35 induction and subsequent treatment.
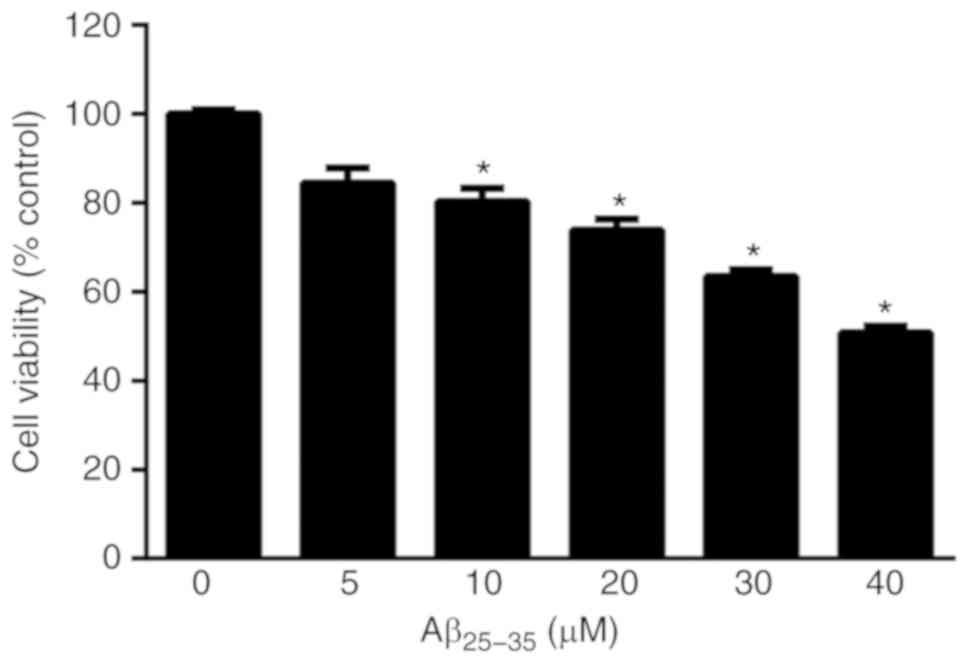
SH-SY5Y cell viability following
Aβ25-35 treatment
SH-SY5Y cells were induced with 0, 5, 10, 20, 30 and
40 µM Aβ25-35. The viability of SH-SY5Y cells was
revealed to decrease with Aβ25-35 (10, 20, 30 and 40
µM), P<0.05; Fig. 2), indicating
marked injury to cells. To avoid an over cytotoxic effect and as
SH-SY5Y cell viability was 63.4%, 30 µM of Aβ25-35 was
selected as the optimal concentration for subsequent
experimentation.
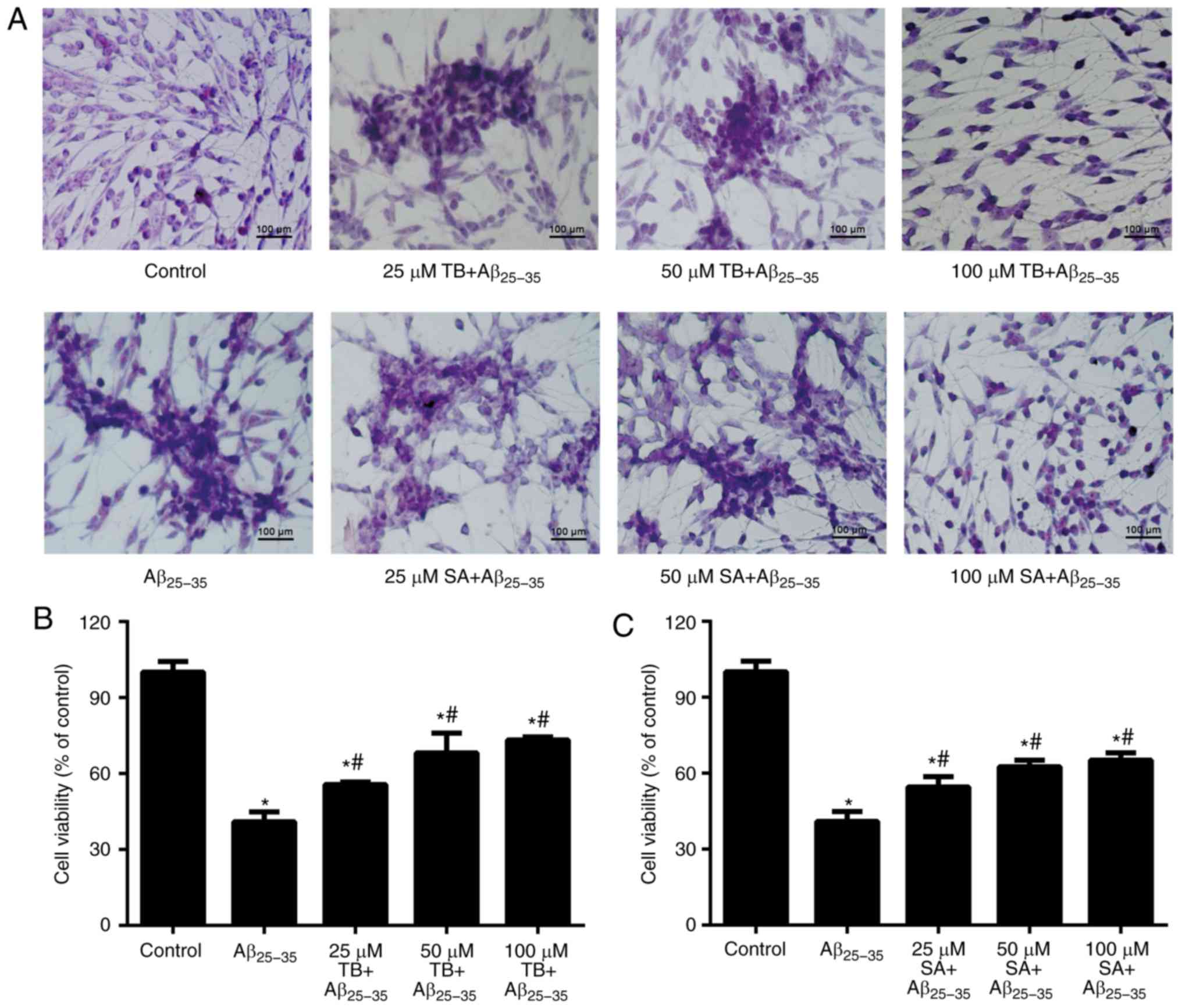
Effect of TB and SA on the morphology
and viability of Aβ25-35-induced SH-SY5Y cells
The morphology of SH-SY5Y cells with or without
treatment are presented in Fig. 3A.
The results demonstrated that cells in the control group were
tightly arranged, exhibiting round and well-stained nuclei.
However, following induction via Aβ25-35, cells
exhibited marked shrinkage, with dark-blue nuclei and a reduced
refractive index following 30 µM of Aβ25-35, indicating
a growth inhibitory effect. However, following treatment with
different concentrations of TB or SA, Aβ25-35-induced
SH-SY5Y cells exhibited a marked restoration of morphology.
An MTT assay was performed to assess cell viability
following treatment. Compared with the cells in the control group,
those induced by Aβ25-35 exhibited a significantly
decreased cell viability (P<0.05; Fig. 3A and B) with an increase of
Aβ25-35 concentration as presented. However, cell
viability increased as TB or SA treatment concentration increased,
indicating that alongside the changes in cell morphology,
Aβ25-35-induced SH-SY5Y cell viability was also
increased in a dose-dependent manner at a TB and SA concentration
range of 25–100 µM (Fig. 3A and
B).
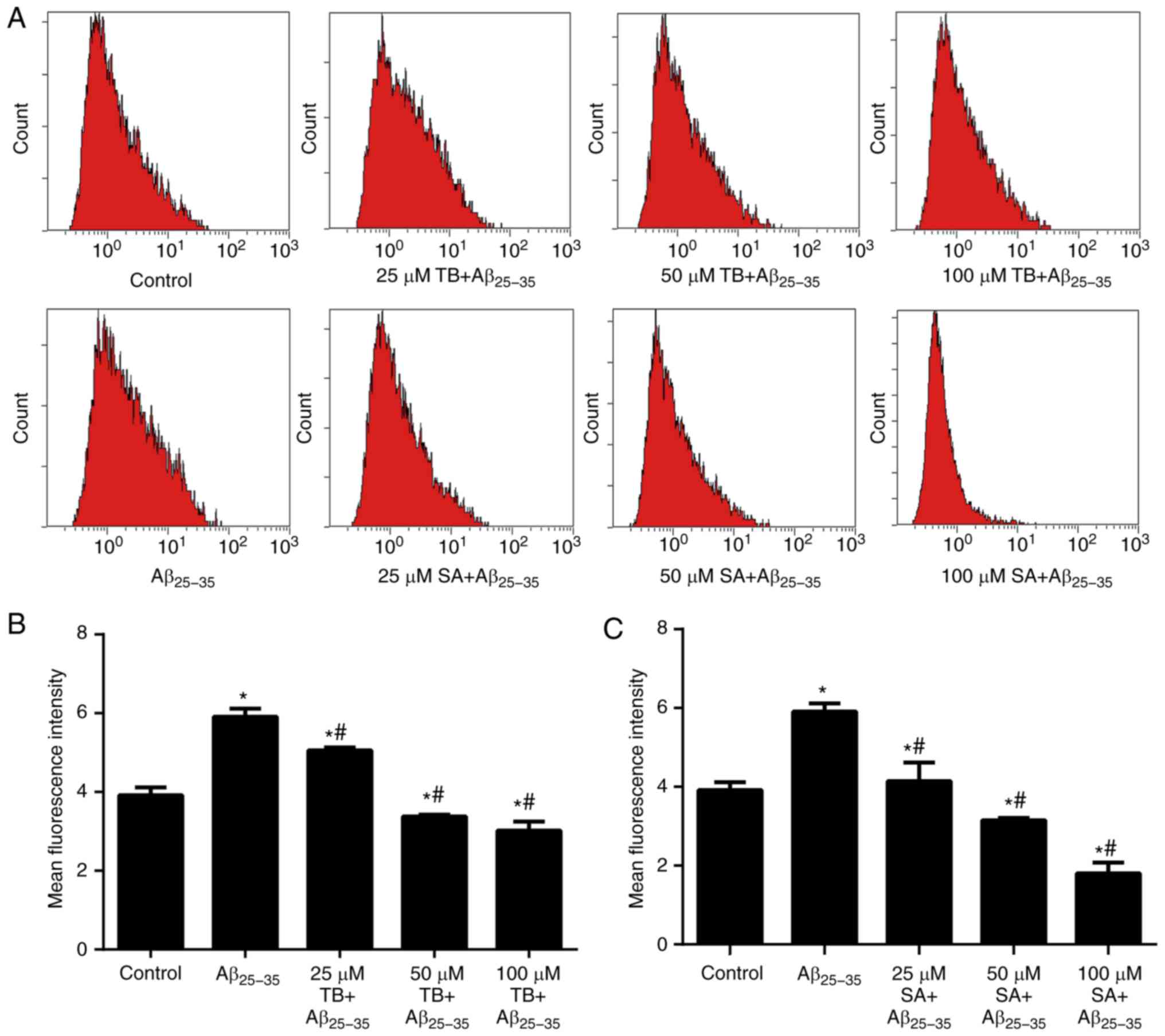
Effect of TB and SA on
Aβ25-35-induced SH-SY5Y cell oxidative stress
A DCFH-DA assay was preformed to assess the levels
of oxidative stress in Aβ25-35-induced SH-SY5Y cells. As
presented in Fig. 4, the mean
fluorescence intensity (MFI) of intracellular ROS in
Aβ25-35-induced SH-SY5Y cells was increased compared
with the control group (P<0.05). In contrast, the MFI value of
Aβ25-35-induced SH-SY5Y cells gradually decreased with
an increase of TB or SA concentration in a dose-dependent manner
(P<0.05), indicating that treatment reduced cell ROS
content.
Furthermore, the MDA content of
Aβ25-35-induced SH-SY5Y cells was markedly elevated
following TB and SA treatment, whereas the enzyme activities of SOD
and GSH-PX were clearly reduced in comparison with control cells.
Thus, oxidative stress parameters were decreased following
treatment with increased TB and SA concentrations. These data with
TB and SA treatments at the different concentrations are presented
in Tables I and II.
 | Table I.Effect of TB concentration on MDA,
SOD and GSH-Px levels in Aβ25-35-induced SH-SY5Y
cells. |
Table I.
Effect of TB concentration on MDA,
SOD and GSH-Px levels in Aβ25-35-induced SH-SY5Y
cells.
| Group | MDA (mmol/mg) | SOD (U/mg) | GSH-Px (U/mg) |
|---|
| Control | 0.94±0.10 | 44.08±0.95 | 56.53±2.61 |
|
Aβ25-35 |
2.23±0.17a |
11.67±0.35b |
21.12±0.28b |
| 25 µM TB +
Aβ25-35 |
1.57±0.41d | 19.75±3.39 | 28.16±1.73 |
| 50 µM TB +
Aβ25-35 |
1.25±0.04d |
30.48±0.40d | 32.88±3.29 |
| 100 µM TB +
Aβ25-35 |
1.07±0.60d |
32.12±2.15c |
37.95±1.29d |
 | Table II.Effect of SA concentration on MDA,
SOD and GSH-PX levels in Aβ25-35-induced SH-SY5Y
cells. |
Table II.
Effect of SA concentration on MDA,
SOD and GSH-PX levels in Aβ25-35-induced SH-SY5Y
cells.
| Group | MDA (mmol/mg) | SOD (U/mg) | GSH-Px (U/mg) |
|---|
| Control | 1.14±0.60 | 37.22±0.4 | 62.00±0.03 |
|
Aβ25-35 |
3.05±0.63a |
9.25±0.15a |
18.77±0.02b |
| 25 µM SA +
Aβ25-35 |
2.10±0.12c |
22.96±0.11c |
25.85±0.03c |
| 50 µM SA +
Aβ25-35 |
1.54±0.14c |
27.45±0.07c |
33.02±0.01c |
| 100 µM SA +
Aβ25-35 |
1.20±0.01d |
29.96±0.06d |
35.27±0.03d |
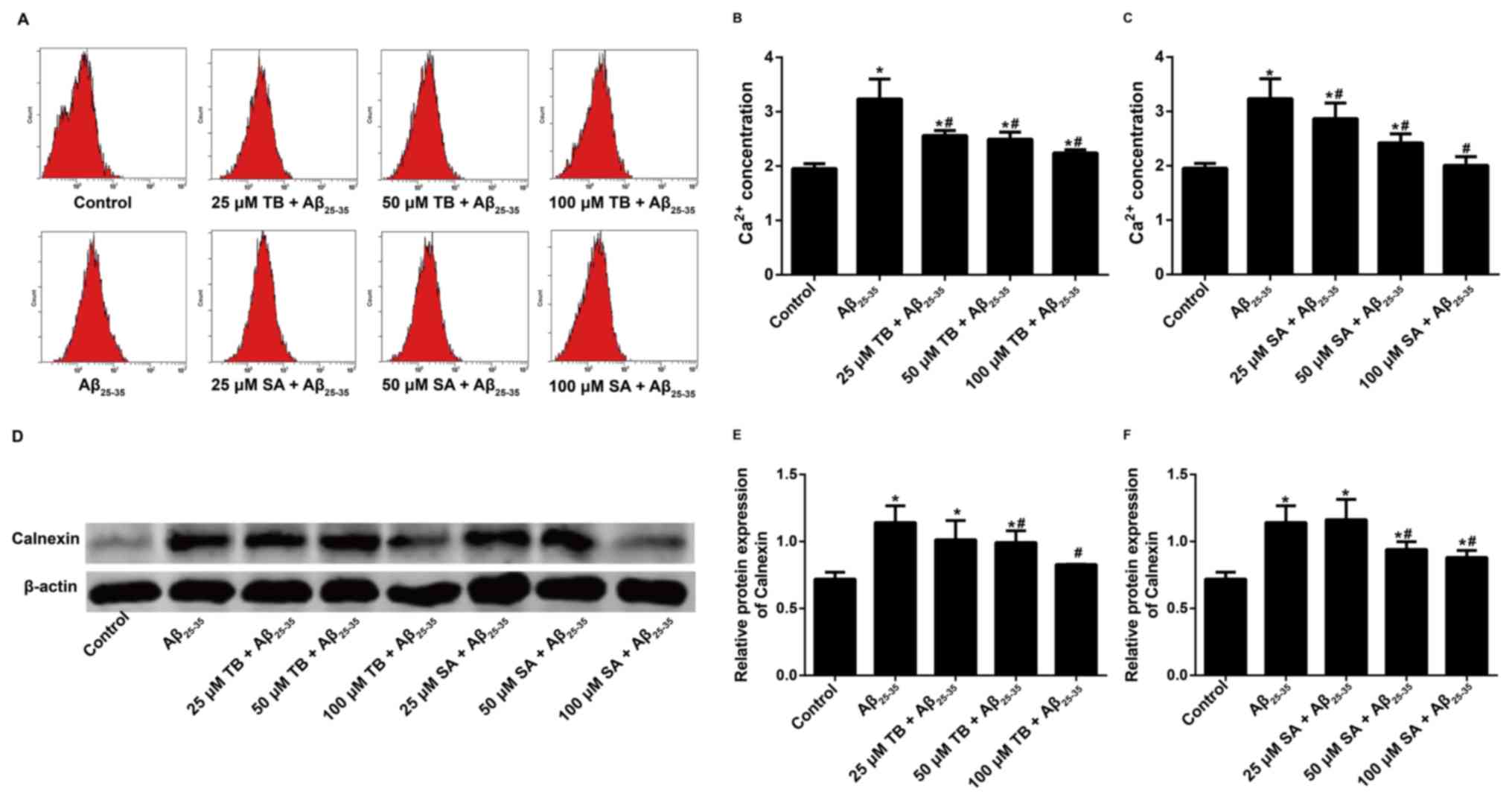
Effect of TB and SA on the
intracellular Ca2+ concentration and calnexin expression
of Aβ25-35-induced SH-SY5Y cells
The intracellular Ca2+ concentration of
Aβ25-35-induced SH-SY5Y cells was measured using the
Fluo-3AM staining method and the MFI of intracellular
Ca2+ was recorded via flow cytometry. The results
demonstrated that the intracellular Ca2+ concentration
of Aβ25-35-induced SH-SY5Y cells decreased following TB
or SA treatment in a dose-dependent manner (Fig. 5A-C). This indicates that TB and SA
treatment may reduce the function of Ca2+ in cells.
The expression of Calnexin was determined following
western blotting. Compared with the control group, Calnexin
expression increased following Aβ25-35-induction in
SH-SY5Y cells. However, TB (50–100 µM) and SA (50–100 µM) treatment
significantly decreased the expression of Calnexin in a dose
dependent manner when compared with Aβ25-35-induced
SH-SY5Y cells (Fig. 5D-F).
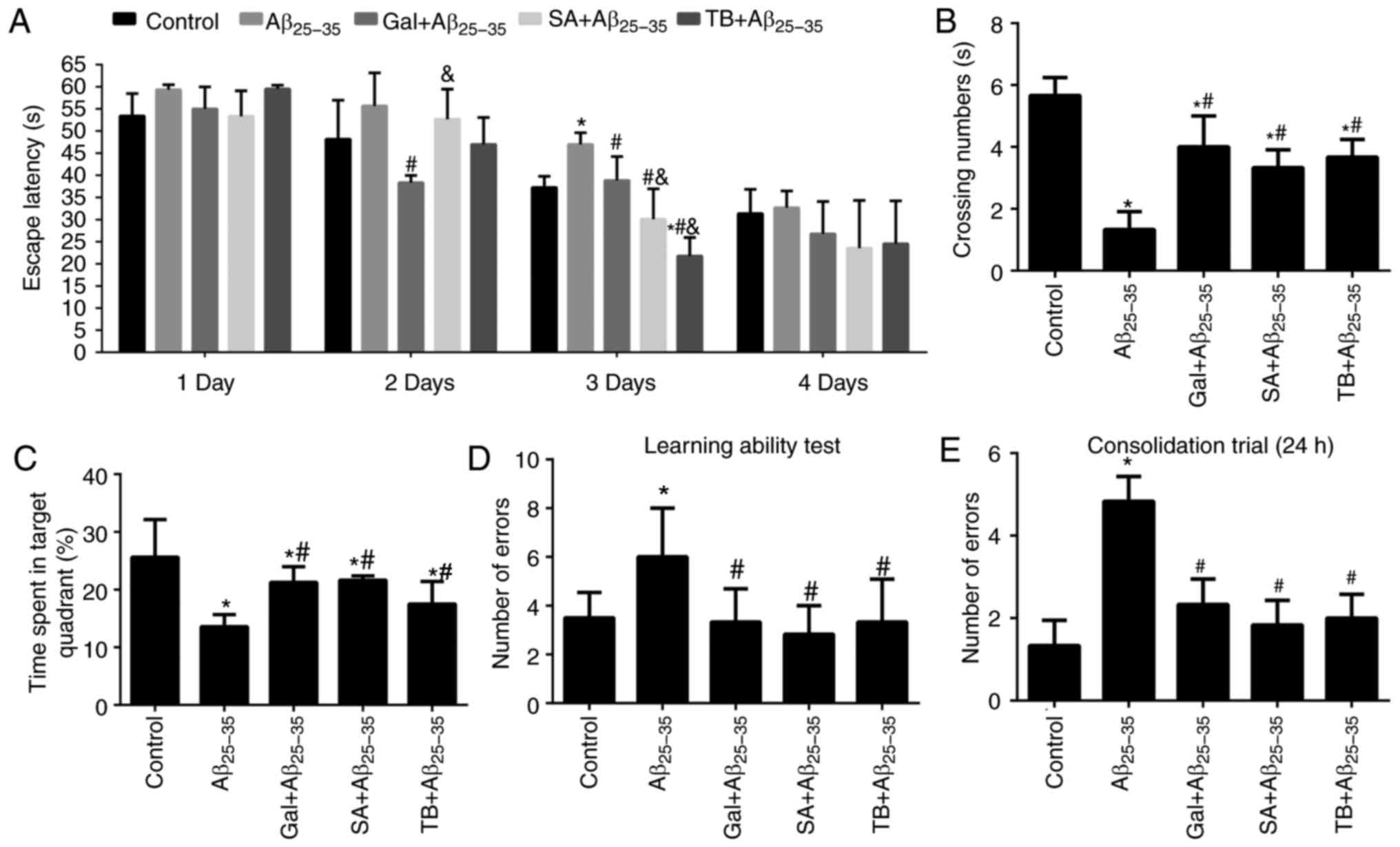
Effect of TB and SA treatment on the
learning and memory of Aβ25-35-induced mice
The Morris water maze test was utilized to assess
the learning and memory of Aβ25–35-induced mice. The
results revealed that the mice induced by Aβ25-35
exhibited markedly prolonged escape latency, markedly decreased
crossing numbers and significantly reduced time spent in the target
quadrant in comparison with mice in the control group on the 3rd
day (P<0.05; Fig. 6A-C). However,
following treatment with SA, TB or Gal, Aβ25-35-induced
mice exhibited a significantly improved non-spatial relational
learning and memory (P<0.05) compared with untreated mice,
indicating that SA and TB served as affective treatments.
In the Y-maze test, following an Aβ25-35
injection to murine hippocampal regions, the spatial recognition
memory of mice was demonstrated to be significantly reduced, as
presented in Fig. 6D-E (P<0.05).
SA and TB compounds were subsequently administered to treat injured
mice. The results revealed an effective improvement on the spatial
recognition memory of Aβ25-35-induced mice (all
P<0.05), which was consistent with the treatment by the Gal.
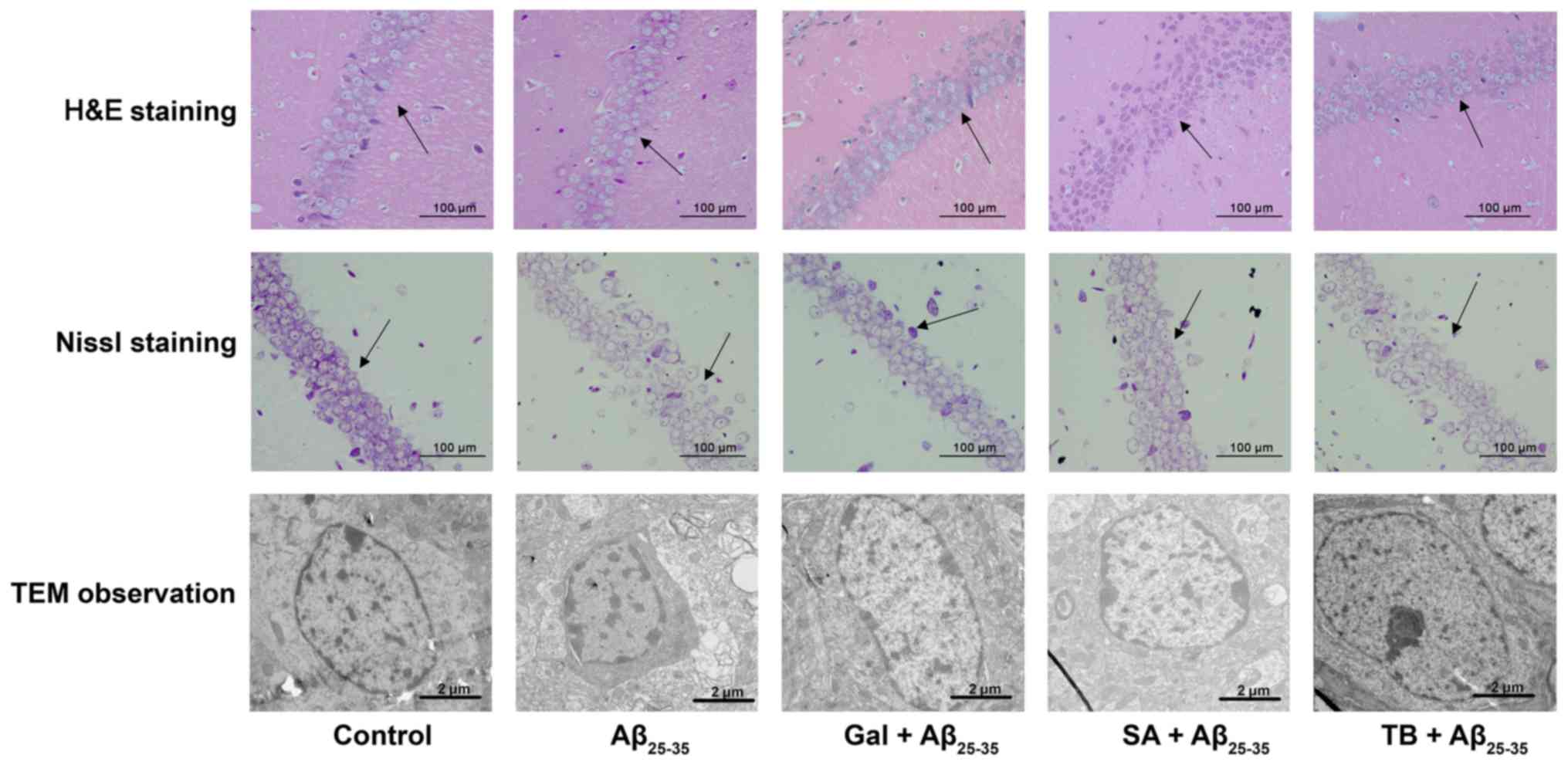
Effect of TB and SA on the
histopathological morphology and neuronal ultrastructure of
Aβ25-35 induced murine hippocampal CA1 regions
H&E staining was performed to monitor neuronal
morphology and pyramidal cells in the hippocampal CA1 region of
mice. The results revealed that mice in the control group exhibited
a normal neuronal morphology, with well-arranged pyramidal cells
(Fig. 7). In contrast,
Aβ25-35-induced mice exhibited a markedly decreased
number of pyramidal cells. The cells were arranged dispersedly in a
disordered manner. However, following SA or TB treatment, the
number of pyramidal cells and the degree of cell edema were
observed to be improved.
The neuronal structure of murine brains was
determined via Nissl staining. The results revealed that the
control group exhibited a complete neuron structure, with clearly
visible nucleoli, lightly stained cytoplasm and a neat arrangement
in the hippocampus. In contrast, the tissues of mice from the
Aβ25-35 group exhibited significant cell shrinkage,
irregular cell morphology, cell membrane shrinkage, pyknotic and
deeply stained nuclei, loosely arranged hippocampal cells,
decreased pyramidal cells and decreased Nissl bodies. Following
treatment with Gal, SA and TB, the pyramidal cells and Nissl bodies
in the hippocampal CA1 region of Aβ25-35-induced mice
were substantially improved, demonstrating treatment efficacy
(Fig. 7).
TEM imaging was utilized to assess the neuronal
structures of mice. It was demonstrated that control group mice had
a normal distribution of neurons, smooth membrane surfaces and
round or oval shape nuclei. However, Aβ25-35-induced
mice exhibited concentrated chromatin in the nuclei of certain
neurons. Following TB and SA treatment, the neuronal structures of
Aβ25-35-induced mice were ameliorated and resumed to
almost normal status, with only very few abnormal nuclear
ultrastructures. This observation was also similar to that of the
Gal+Aβ25–35 group, indicating that TB and SA have a
similar treatment effect to Gal (Fig.
7).
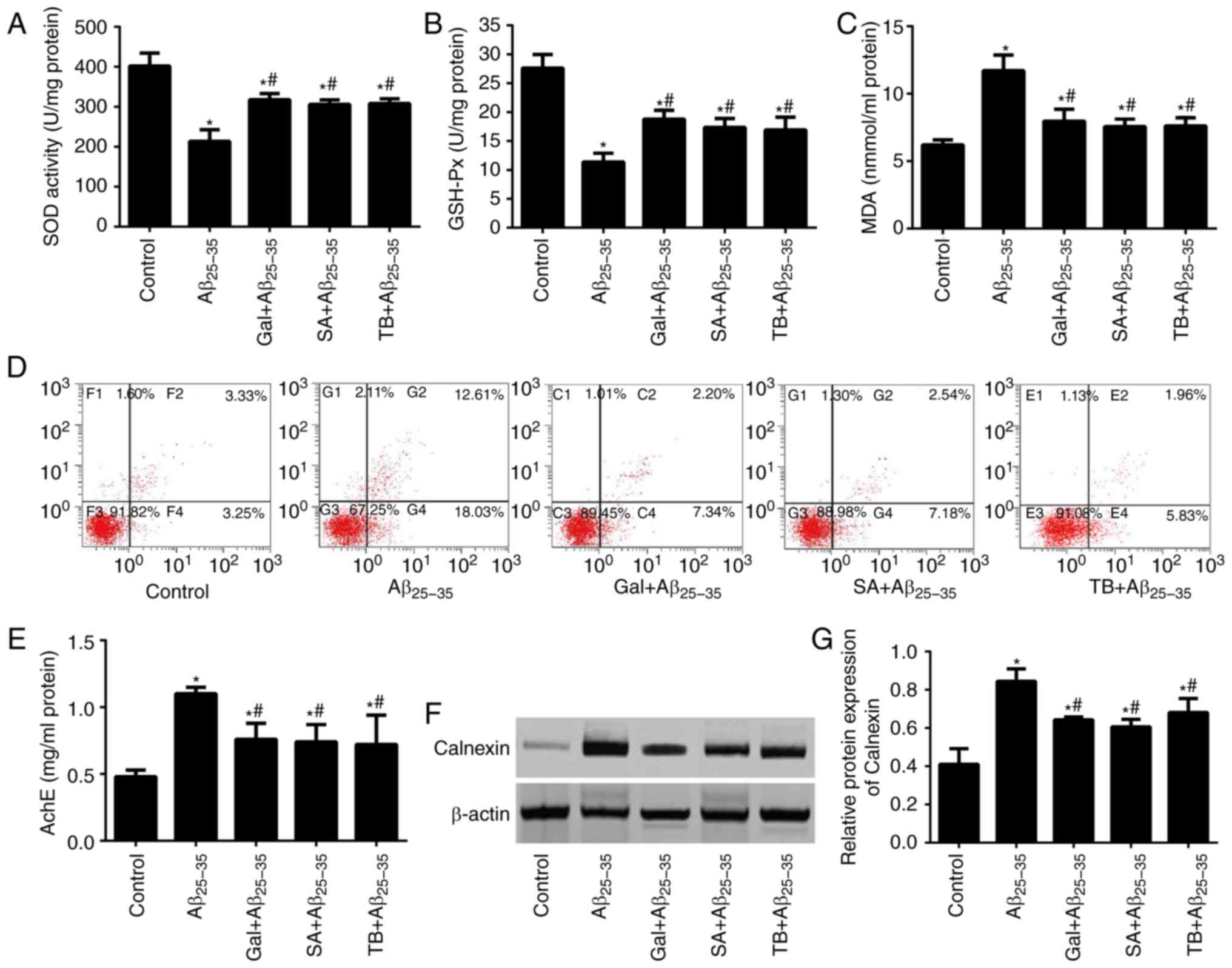
Effects of TB and SA on the oxidative
stress and neuron apoptosis of hippocampal tissues in
Aβ25-35-induced mice
The content of MDA and the activity of SOD and
GSH-Px from Aβ25-35-induced and control mice were
measured (Fig. 8A-D). The results
revealed that the content of MDA in Aβ25-35-induced mice
was significantly higher compared with the control group.
Additionally, the activities of SOD and GSH-Px were significantly
lower in Aβ25-35-induced mice compared with control
mice, indicating the marked aggravation of hippocampal neuron
apoptosis via Aβ25-35-induction (all P<0.05).
Following treatment with SA or TB, oxidative stress in the
hippocampal tissues of Aβ25-35-induced mice was markedly
alleviated, exhibiting a decrease of MDA content, an increase in
SOD and GSH-Px activity and a decrease in the number of apoptotic
neurons (all P<0.05). A similar effect was also observed in
Aβ25-35-induced mice treated with Gal, further
supporting the hypothesis that SA and TB exhibit similar effects to
Gal.
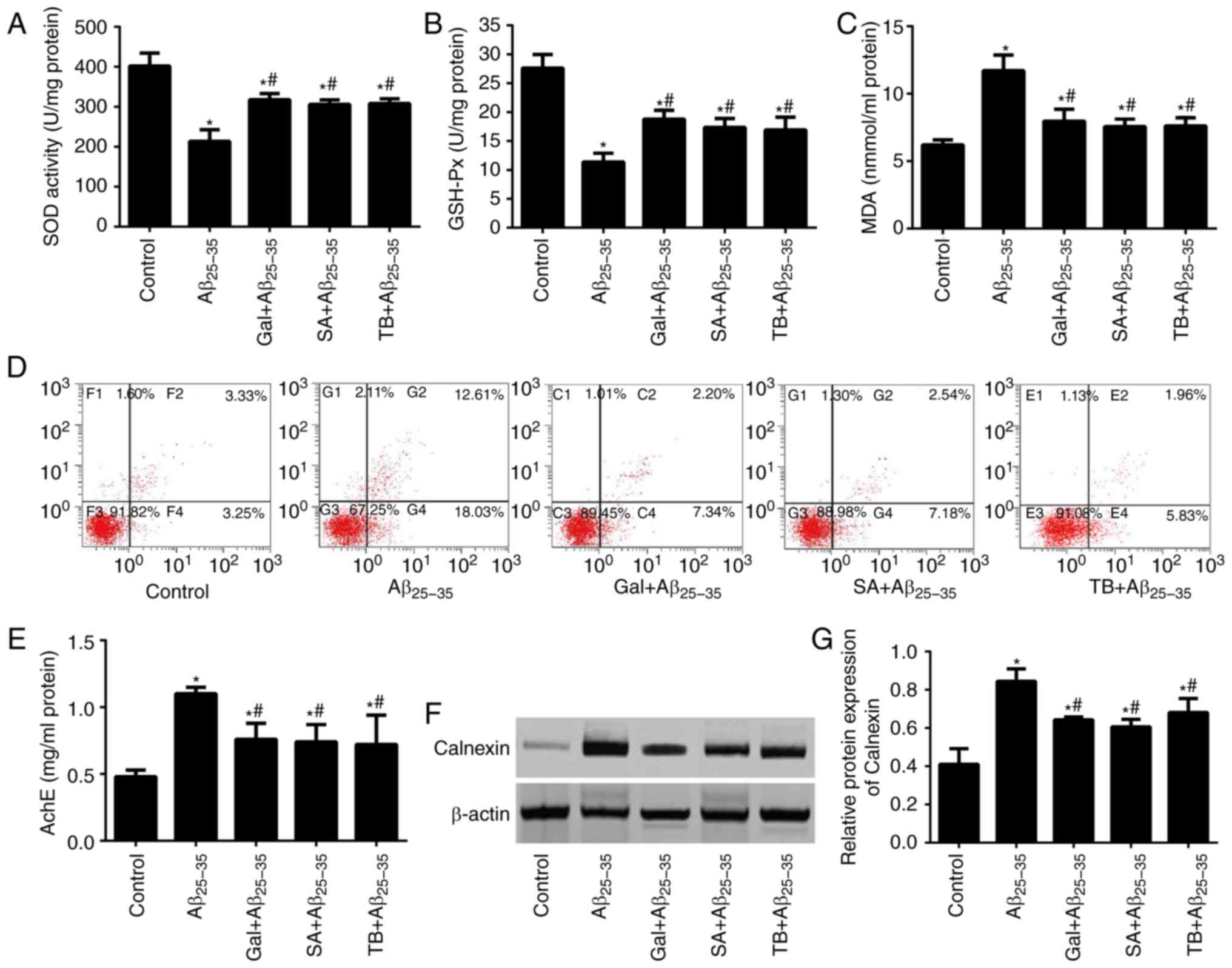 | Figure 8.Effect of TB and SA on oxidative
stress, apoptosis, AchE activity and Calnexin expression of
hippocampal tissues in Aβ25-35-induced mice. Activities
of (A) SOD, (B) GSH-Px and (C) MDA content. (D) Hippocampal neuron
apoptosis was assessed in mice using an Annexin V-EGFP/PI double
staining method. (E) AchE activity in the hippocampal tissues of
mice. The expression of Calnexin in the mice determined via (F)
western blotting and subsequent (G) quantification. *P<0.05 vs.
the control group; #P<0.05 vs. the Aβ25-35
group. TB, torenoside B; SA, savatiside A; AchE,
acetylcholinesterase; Aβ, amyloid-beta; SOD, superoxide dismutase;
GSH-PX, glutathione peroxidase; MDA, maleic dialdehyde. |
Effects of TB and SA on AchE activity
and Calnexin expression in the hippocampal tissues of
Aβ25–35-induced mice
As presented in Fig.
8E, Aβ25-35 induced mice exhibited an increased AchE
activity in their hippocampal tissues compared with the control
group (P<0.05). Following treatment with TB and SA, AchE
activity of the three treated groups were markedly decreased (all
P<0.05). Furthermore, AchE activity in each of the three
treatment groups was not statistically significant when compared,
indicating similar drug effects.
Western blotting was performed to detect the
expression of Calnexin in the hippocampus of mice, the results of
which are presented in Fig. 8F and
G. The results demonstrated that Calnexin expression in
Aβ25-35 induced mice was significantly higher than that
of the control group (P<0.05). Furthermore, following treatment
with TB, SA and GAL, the expression of Calnexin in
Aβ25-35-induced mice markedly decreased (P<0.05),
indicating a significant and similar treatment efficacy of SA, TB
and GAL.
Discussion
Aβ fragments are derived from a family of peptides
that are closely associated with the pathogenesis and development
of AD (13,18). The Aβ25-35 fragment in
particular, exhibits a high cytotoxicity, rapid aggregation and an
enhanced neurotoxicity (13). The
toxic effect of Aβ25-35 on nervous cells has been well
document via in vitro and in vivo experiments
(19,20). In the current study,
Aβ25-35 was used to induce SH-SY5Y cells at different
concentrations. The results revealed a marked decrease in cell
viability with increased Aβ25-35 concentrations, which
is consistent with the results of previous studies (21,22). To
avoid adverse effects following induction, 30 µM of
Aβ25-35 (with a cell viability of 63.4%) was selected
for subsequent cell-based in-vitro experiments.
In accordance with typical protocols for drug
treatment, cells and mice were first induced with
Aβ25-35 and then treated with drugs to determine their
effect on cell injury. The current study assessed the protective
role of PhGs in AD. Thus, cells and mice were treated with PhGs
following induction with Aβ25-35, which is a procedure
that has been utilized in a previous publication (23).
Aβ25-35 is closely associated with the
pathogenesis and progression of many neurodegenerative diseases,
including Parkinson's disease, amyotrophic lateral sclerosis and AD
(24), via a modulating oxidative
stress pathway. Thus, as a product of normal aerobic metabolism,
ROS is considered to maintain a dynamic balance of its production
and clearance under normal circumstances (25). However, an impaired balance of ROS or
antioxidant may contribute to the accumulation of ROS, resulting in
oxidative stress-induced cell injury (26). MDA, a byproduct of free radical lipid
attack, is recognized as a biomarker of lipid peroxidation and
oxidative stress (27,28). In addition, certain enzymes,
including catalase, GSH-Px and SOD, may prevent ROS induced cell
injury via detoxification (29).
The current study determined the content of MDA and
the enzyme activities of GSH-Px and SOD to determine oxidative
stress-induced cell injury following Aβ25-35 treatment,
and the treatment efficacy of antioxidants in the PhGs extracted
from Monochasma savatieri Franch. PhGs are naturally
distributed in dicotyledonous plants and are usually comprised of a
β-glucosamine core with hydroxyl and methoxy subunits substituting
phenyl or cinnamoyl substituent groups via ester or glycosidic
linkages (30,31). Certain PhGs have also been
demonstrated to exert a significant anti-oxidative stress effect
(32). For instance, acteoside,
extracted from Verbascum sinuatum, protects SH-SY5Y cells
against Aβ-induced cell injury by modulating ROS generation and
apoptosis via a signal pathway comprising the B cell lymphoma-2
family, cytochrome-c and caspase-3 (33). Furthermore, Echinacoside, isolated
from Tibetan herb Lagotis brevituba Maxim and Cistanche
tubules, is considered to exert a neuroprotective role in
H2O2-injured PC12 cells by regulating the
mitochondrial apoptotic pathway (34). TB and SA, as two types of PhG
extracted from Monochasma savatieri Franch, were utilized in
the current study to assess their neuroprotective efficacy in in
vitro and in vivo experiments.
SH-SY5Y cell morphology exhibited a large change
following Aβ25-35 induction, but returned to a
relatively normal status following treatment with TB and SA at a
high dose. Meanwhile, a different morphology and cell viability was
observed following TB or SA treatment when compared with
Aβ25-35-induced cells. This may be due to different
solubility of the two compounds. The morphological method provides
an observation on the change of cell shape following treatment and
is only used as a semi-qualitative method, whereas MTT assay is
quantitative. The data obtained from each method exhibits similar
trends and supports the conclusion that TB and SA may serve as
efficient treatments of AD.
Aβ25-35 induced SH-SY5Y cells upregulated
intracellular ROS content and MDA, but downregulated SOD and
GSH-Px. These results indicate that Aβ25-35-induced
oxidative stress may constitute a cause for the cell injury
observed in AD development. This may be due to the binding of Aβ to
the advanced glycation end product cell membrane receptor,
activating nuclear factor (NF)-κB and subsequently generating ROS
(35). An in vitro experiment
was then performed in the present study, in which
Aβ25-35-induced cells were treated with TB and SA
extracts. Gal was also utilized in certain tests as the positive
control. The results revealed that TB and SA treatment
significantly decreased ROS and MDA content, and increased SOD and
GSH-Px in a dose-dependent manner. A previous study also determined
that SA exerts a protective effect against myocardial ischemia
injury (7). The current study
demonstrated that SA and TB compounds may function as antioxidants
and thus prevent AD by eliminating ROS or preventing its
production, and by slowing down or completely inhibiting
degenerative changes in nerve cells. The effect of SA and TB may be
a result of phenolic hydroxyl groups present in their chemical
structure that may lead to anti-oxidative activities, thus
exhibiting free radical removal and oxidative cracking (36).
To further verify the anti-oxidative and
anti-apoptosis properties of TB and SA, the extracts were
administered Aβ25-35-induced mice. It is considered that
the majority of people with AD are older (≥65 years) and as such,
the age of experimental animals is a critical variable in
experimental research (37). The
current study assessed the protective role of PhGs in AD. It has
been revealed that Aβ can be detected in the mice at 2–3 weeks old
and remains at a relatively low level at 4–5 weeks old (38,39).
Thus, to reduce the natural Aβ interference in the brains of mice,
the current study utilized 4–5 weeks old mice to construct AD
models.
According to a previous study, Aβ binds to N-methyl-
D-aspartate receptors, regulating calcium channels and increasing
the number of open channels on the cell surface (40). This phenomenon may increase the
influx of extracellular calcium, triggering the release of
mitochondrial calcium and resulting in the destabilization of
calcium homeostasis and the increased production of ROS (41). However, PhG compounds serve an
essential role in the maintenance of calcium homeostasis. For
instance, echinacoside induces pulmonary artery vasorelaxation in
mice by increasing the number of open NO-cGMP-PKG-BKCa channels and
decreasing intracellular Ca2+ levels (42). In addition, acteoside inhibits the
invasive and migrating capabilities of
phorbol-12-myristate-13-acetate-induced human fibrosarcoma cells by
regulating the Ca2+-dependent calmodulin-dependent
protein kinase/extracellular regulated kinase and Jun
amino-terminal kinase/NF-κB pathways (43). The results of the current study
reveal that TB and SA treatment inhibited the concentration of
intracellular Ca2+ and the expression of Calnexin in
Aβ25-35-induced cells. This observation was also
supported by the results of in-vivo experiments. Thus, it is
suggested that TB and SA compounds may downregulate the expression
of proteins that are associated with the Calnexin transduction
pathway, alleviating the destabilizing state of calcium homeostasis
in neurons, and exerting therapeutic effects in AD.
As determined in the present study, SA (100
mg/kg/d) and TB (100 mg/kg/d) treatment effectively improves the
spatial, non-spatial learning and memory capabilities of
Aβ25-35-injured mice. Furthermore, SA and TB treatment
was revealed to ameliorate the morphology and structure of
pyramidal cells in the hippocampal CA1 region, increase the number
of Nissl bodies and reduce AchE activity in
Aβ25-35-injured mice. As a hydrolase of the central
nervous system, AchE serves a key role in hydrolyzing acetylcholine
(ACh) and terminating the conduction of nerve impulses (44). The results of the current study
demonstrated that SA and TB compounds function as efficient AChE
inhibitors, indicating their potential treatment efficiency.
As a drug to treat mild to moderate confusion in
dementia associated AD, Gal is not curative, but may improve
memory, awareness and the ability to perform daily tasks (45). However, it also exerts side effects
including nausea, vomiting, stomach pain, diarrhea, dizziness, loss
of appetite, weight loss and tiredness (46). In the current study, Gal was utilized
as a positive control in certain tests, the results of which were
compared with the efficacy of TB and SA treatment. Of significance,
the results revealed that TB and SA exhibit a similar effect to Gal
in certain experiments, indicating a high treatment efficacy of TB
and SA. However, the current study did not compare the side effects
of TB and SA to those of Gal. Further study is required to assess
the pharmacokinetics and pharmacodynamics of SA and TB compounds,
as well as their bioavailability.
In the current study, TB and SA compounds exhibited
potential therapeutic effects in the treatment of AD. TB and SA
treatments were revealed to enhance the enzyme activity of SOD and
GSH-Px, reduce the content of ROS and MDA, and downregulate
intracellular Ca2+ concentrations and Calnexin
expression in Aβ25–35-induced SH-SY5Y cells. In
addition, TB or SA treatment administered to
Aβ25-35-induced mice effectively improved their learning
capability and memory, alleviated their oxidative stress in the
hippocampal tissues, significantly decreased the expression of
Calnexin and decreased hippocampal neuron apoptosis. The results
revealed that SA and TB compounds may have a potential for use as
therapeutic drugs to treat AD. However, although the formation of
plaques or tangles in mice may verify the success of animal model
construction, the staining and observation of plaque and tangle
formation were neglected in the experimental design of the current
study to reduce possible interference from multiple staining
protocols and to avoid the complexity and subsequent discussion of
experimental results. This matter should therefore be addressed in
future studies.
Acknowledgements
Not applicable.
Funding
The current study was funded by Jiangsu Science and
Technology Support Program-Social Development Project (grant no.
BE2013631).
Availability of data and materials
All data generated or analyzed during this study
are included in this published article.
Authors' contributions
SJ, SL, XZ, NK, KC, YZ, PP and JF performed the
experiments, analyzed the data and prepared the manuscript. YL, QX
and SY conceived and designed the current study.
Ethics approval and consent to
participate
The current study was approved by the Ethics
Committee of Soochow University (approval no. 201505895).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
PhGs
|
phenylethanoid glycosides
|
|
TB
|
Torenoside B
|
|
SA
|
Savatiside A
|
|
Gal
|
Galantamine
|
|
AD
|
Alzheimer's disease
|
|
ROS
|
reactive oxygen species
|
|
Aβ
|
amyloid-beta
|
|
MDA
|
Maleic dialdehyde
|
|
SOD
|
superoxide dismutase
|
|
GSH-Px
|
glutathione peroxidase
|
|
AchE
|
acetylcholinesterase
|
|
H&E
|
hematoxylin and eosin
|
|
TEM
|
transmission electron microscope
|
References
|
1
|
Feldman HH and Estabrooks CA: The Canadian
dementia challenge: Ensuring optimal care and services for those at
risk or with dementia throughout the country. Can J Public Health.
108:e95–e97. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Josephs K, Whitwell JL, Weigand S, Murray
ME, Tosakulwong N, Liesinger A, Petrucelli L, Senjem M Knopman DS,
Boeve BF, et al: Tdp-43 amplifies memory loss and hippocampal
atrophy in Alzheimer's disease. Alzheimers Dementia. 10:P279–P280.
2014. View Article : Google Scholar
|
|
3
|
Zhang DF, Li J, Wu H, Cui Y, Bi R, Zhou
HJ, Wang HZ, Zhang C, Wang D; Alzheimer's Disease Neuroimaging
Initiative (ADNI), ; et al: CFH Variants affect structural and
functional brain changes and genetic risk of Alzheimer's disease.
Neuropsychopharmacology. 41:1034–1045. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Atwood CS, Martins RN, Smith MA and Perry
G: Senile plaque composition and posttranslational modification of
amyloid-beta peptide and associated proteins. Peptides.
23:1343–1350. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kalra J and Khan A: Reducing Abeta load
and tau phosphorylation: Emerging perspective for treating
Alzheimer's disease. Eur J Pharmacol. 764:571–581. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Li M, Shi MF, Liu YL, Xu QM and Yang SL:
Phenylethanoid glycosides from Monochasma savatieri and
their anticomplement activity through the classical pathway. Planta
Med. 78:1381–1386. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shi M, He W, Liu Y, Li X, Yang S and Xu Q:
Protective effect of total phenylethanoid glycosides from
Monochasma savatieri Franch on myocardial ischemia injury.
Phytomedicine. 20:1251–1255. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu YL, He WJ, Mo L, Shi MF, Zhu YY, Pan
S, Li XR, Xu QM and Yang SL: Antimicrobial, anti-inflammatory
activities and toxicology of phenylethanoid glycosides from
Monochasma savatieri Franch. ex Maxim. J Ethnopharmacol.
149:431–437. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hu XP, Shao MM, Song X, Wu XL, Qi L, Zheng
K, Fan L, Liao CH, Li CY, He J, et al: Anti-influenza virus effects
of crude phenylethanoid glycosides isolated from ligustrum
purpurascens via inducing endogenous interferon-γ. J
Ethnopharmacol. 179:128–136. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang J, Ju B, Yan Y, Xu H, Wu S, Zhu D,
Cao D and Hu J: Neuroprotective effects of phenylethanoid
glycosides in an in vitro model of Alzheimer's disease. Exp
Ther Med. 13:2423–2428. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shao SY, Feng ZM, Yang YN, Jiang JS and
Zhang PC: Forsythenethosides A and B: Two new phenylethanoid
glycosides with a 15-membered ring from Forsythia suspensa.
Org Biomol Chem. 15:7034–7039. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Roura E, Andrés-Lacueva C, Estruch R and
Lamuela-Raventós RM: Total polyphenol intake estimated by a
modified Folin-Ciocalteu assay of urine. Clin Chem. 52:749–752.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kowall NW, McKee AC, Yankner BA and Beal
MF: In vivo neurotoxicity of beta-amyloid [beta(1–40)] and the
beta(25–35) fragment. Neurobiol Aging. 13:537–542. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu YM, Li ZY, Hu H, Xu SP, Chang Q, Liao
YH, Pan RL and Liu XM: Tenuifolin, a secondary saponin from
hydrolysates of polygalasaponins, counteracts the neurotoxicity
induced by Aβ25–35 peptides in vitro and in vivo. Pharmacol Biochem
Behav. 128:14–22. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Guo DK, Zhu Y, Sun HY, Xu XY, Zhang S, Hao
ZB, Wang GH, Mu CC and Ren H: Pharmacological activation of
REV-ERBα represses LPS-induced microglial activation through the
NF-κB pathway. Acta Pharmacol Sin. 40:26–34. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ma MX, Chen YM, He J, Zeng T and Wang JH:
Effects of morphine and its withdrawal on Y-maze spatial
recognition memory in mice. Neuroscience. 147:1059–1065. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mokhtari Z, Baluchnejadmojarad T, Nikbakht
F, Mansouri M and Roghani M: Riluzole ameliorates learning and
memory deficits in Aβ25-35-induced rat model of Alzheimer's disease
and is independent of cholinoceptor activation. Biomed
Pharmacother. 87:135–144. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lai W, Wu J, Zou X, Xie J, Zhang L, Zhao
X, Zhao M, Wang Q and Ji J: Secretome analyses of Aβ(1–42)
stimulated hippocampal astrocytes reveal that CXCL10 is involved in
astrocyte migration. J Proteome Res. 12:832–843. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gerber H, Späth PJ, Perret BA and
Burckhardt JJ: Laboratory workshop on the characterization of
anti-platelet antibodies in immune thrombocytopenic purpura. Blut.
59:61–66. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhi WH, Zeng YY, Lu ZH, Qu WJ, Chen WX and
Chen L and Chen L: Simvastatin exerts antiamnesic effect in
Aβ25-35-injected mice. CNS Neurosci Ther. 20:218–226. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wang K, Zhu L, Zhu X, Zhang K, Huang B,
Zhang J, Zhang Y, Zhu L, Zhou B and Zhou: Protective effect of
paeoniflorin on Aβ25-35-induced SH-SY5Y cell injury by preventing
mitochondrial dysfunction. Cell Mol Neurobiol. 34:227–234. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wei H, Gao Z, Zheng L, Zhang C, Liu Z,
Yang Y, Teng H, Hou L, Yin Y and Zou X: Protective effects of
fucoidan on Aβ25–35 and d-Gal-induced neurotoxicity in PC12 cells
and d-Gal-induced cognitive dysfunction in mice. Mar Drugs.
15(pii): E772017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hashimoto M, Katakura M, Hossain S, Rahman
A, Shimada T and Shido O: Docosahexaenoic acid withstands the
Aβ(25–35)-induced neurotoxicity in SH-SY5Y cells. J Nutr Biochem.
22:22–29. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ganguly G, Chakrabarti S, Chatterjee U and
Saso L: Proteinopathy, oxidative stress and mitochondrial
dysfunction: Cross talk in Alzheimer's disease and Parkinson's
disease. Drug Des Devel Ther. 11:797–810. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Marchi S, Giorgi C, Suski JM, Agnoletto C,
Bononi A, Bonora M, De Marchi E, Missiroli S, Patergnani S, Poletti
F, et al: Mitochondria-ros crosstalk in the control of cell death
and aging. J Signal Transduct. 2012:3296352012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Calingasan NY, Chen J, Kiaei M and Beal
MF: Beta-amyloid 42 accumulation in the lumbar spinal cord motor
neurons of amyotrophic lateral sclerosis patients. Neurobiol Dis.
19:340–347. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Qian X, Cao H, Ma Q, Wang Q, He W, Qin P,
Ji B, Yuan K, Yang F, Liu X, et al: Allopregnanolone attenuates
Aβ25-35-induced neurotoxicity in PC12 cells by reducing oxidative
stress. Int J Clin Exp Med. 8:13610–13615. 2015.PubMed/NCBI
|
|
28
|
Gomes P, Simão S, Silva E, Pinto V, Amaral
JS, Afonso J, Serrão MP, Pinho MJ and Soares-da-Silva P: Aging
increases oxidative stress and renal expression of oxidant and
antioxidant enzymes that are associated with an increased trend in
systolic blood pressure. Oxid Med Cell Longev. 2:138–145. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Buddi R, Lin B, Atilano SR, Zorapapel NC,
Kenney MC and Brown DJ: Evidence of oxidative stress in human
corneal diseases. J Histochem Cytochem. 50:341–351. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Si CL, Shen T, Jiang YY, Wu L, Yu GJ, Ren
XD, Xu GH and Hu WC: Antioxidant properties and neuroprotective
effects of isocampneoside II on hydrogen peroxide-induced oxidative
injury in PC12 cells. Food Chem Toxicol. 59:145–152. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Çaliş İ: Biodiversity of Phenylethanoid
Glycosides. Biodiversity. 137–149. 2002. View Article : Google Scholar
|
|
32
|
Yu P, Hu C, Meehan EJ and Chen L: X-ray
crystal structure and antioxidant activity of salidroside, a
phenylethanoid glycoside. Chem Biodivers. 4:508–513. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wang H, Xu Y, Yan J, Zhao X, Sun X, Zhang
Y, Guo J and Zhu C: Acteoside protects human neuroblastoma SH-SY5Y
cells against beta-amyloid-induced cell injury. Brain Res.
1283:139–147. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kuang R, Sun Y, Yuan W, Lei L and Zheng X:
Protective effects of echinacoside, one of the phenylethanoid
glycosides, on H(2)O(2)-induced cytotoxicity in PC12 cells. Planta
Med. 75:1499–1504. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hsieh HM, Wu WM and Hu ML: Genistein
attenuates D-galactose-induced oxidative damage through decreased
reactive oxygen species and NF-κB binding activity in neuronal PC12
cells. Life Sci. 88:82–88. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yang JH, Hu JP, Rena K and Du NS:
Structure-activity relationships of phenylethanoid glycosides in
plants of Cistanche salsa on antioxidative activity. Zhong Yao Cai.
32:1067–1069. 2009.(In Chinese). PubMed/NCBI
|
|
37
|
Gorina YV, Komleva YK, Lopatina OL,
Volkova VV, Chernykh AI, Shabalova AA, Semenchukov AA,
Olovyannikova RY and Salmina AB: The battery of tests for
behavioral phenotyping of aging animals in the experiment. Adv
Gerontol. 30:49–55. 2017.(In Russian). PubMed/NCBI
|
|
38
|
Kumar DK, Choi SH, Washicosky KJ, Eimer
WA, Tucker S, Ghofrani J, Lefkowitz A, McColl G, Goldstein LE,
Tanzi RE and Moir RD: Amyloid-β peptide protects against microbial
infection in mouse and worm models of Alzheimer's disease. Sci
Transl Med. 8:340ra3722016. View Article : Google Scholar
|
|
39
|
Cummings DM, Liu W, Portelius E, Bayram S,
Yasvoina M, Ho SH, Smits H, Ali SS, Steinberg R, Pegasiou CM, et
al: First effects of rising amyloid-β in transgenic mouse brain:
Synaptic transmission and gene expression. Brain. 138:1992–2004.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Shelat PB, Chalimoniuk M, Wang JH,
Strosznajder JB, Lee JC, Sun AY, Simonyi A and Sun GY: Amyloid beta
peptide and NMDA induce ROS from NADPH oxidase and AA release from
cytosolic phospholipase A2 in cortical neurons. J Neurochemi.
106:45–55. 2008. View Article : Google Scholar
|
|
41
|
Mattson MP, Barger SW, Begley JG and Mark
RJ: Calcium, free radicals, and excitotoxic neuronal death in
primary cell culture. Methods Cell Biol. 46:187–216. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Gai XY, Wei YH, Zhang W, Wuren TN, Wang
YP, Li ZQ, Liu S, Ma L, Lu DX, Zhou Y and Ge RL: Echinacoside
induces rat pulmonary artery vasorelaxation by opening the
NO-cGMP-PKG-BKCa channels and reducing intracellular Ca2+ levels.
Acta Pharmacol Sin. 36:587–596. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Hwang YP, Kim HG, Choi JH, Park BH, Jeong
MH, Jeong TC and Jeong HG: Acteoside inhibits PMA-induced matrix
metalloproteinase-9 expression via CaMK/ERK- and
JNK/NF-κB-dependent signaling. Mol Nutr Food Res. 55 (Suppl
1):S103–S116. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Bencherif M: Pharmaceutical compositions
for the prevention and treatment of central nervous system
disorders. WO. 6468–6480. 2001.
|
|
45
|
Maelicke A, Samochocki M, Jostock R,
Fehrenbacher A, Ludwig J, Albuquerque EX and Zerlin M: Allosteric
sensitization of nicotinic receptors by galantamine, a new
treatment strategy for Alzheimer's disease. Biol Psychiatry.
49:279–288. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Cheung TS, Song TH, Ng TB, Wu FH, Lao LX,
Tang SC, Ho JC, Zhang KY and Sze SC: Therapeutic effects of herbal
chemicals in traditional Chinese medicine on Alzheimer's disease.
Curr Med Chem. 22:2392–2403. 2015. View Article : Google Scholar : PubMed/NCBI
|