Introduction
Lumbar interbody fusion (LIF) is a standard, widely
accepted surgery in the treatment of degenerative disk disease and
discogenic back pain; it is used when conservative treatments have
failed for ≥6 months (1,2). In 1940, the first successful posterior
(P) LIF was performed (3) and ≥85%
of the 331 patients who underwent this procedure had satisfactory
outcomes (4). However, this
technique has disadvantages, including nerve root compression,
interbody nonunion, and muscle and tissue lesions (4,5).
The transforaminal (T) LIF procedure was first
described by Harms and Jeszenszky (5) as an alternative to PLIF. TLIF provides
access to the disc through a lateral approach following full or
partial removal of the facet and preserving the contralateral joint
(6). Outcomes achieved with TLIF are
similar to those obtained by PLIF (7,8).
Neurologic and vascular damage to the lumbar muscles
have been reported when using the classic open (c-) TLIF approach
(9,10). To minimize muscle damage that occurs
during c-TLIF, a minimally invasive (m-) TLIF procedure was first
described by Foley et al (11), which avoids muscular damage to
achieve fixed fusion (12). The
advantages of transpedicular screws used in m-TLIF have been
described extensively (11,13). A meta-analysis of adverse event data
suggested equivalent rates of surgical complications in patients
undergoing m-TLIF compared with classic open surgery (14). To date, no comparison of m- and
c-TLIF procedures with >5 years follow-up has been described in
the literature (15). The objective
of this study was to compare the clinical effectiveness and
complications of m- and c-TLIF in patients with single-level lumbar
disc herniation disease and ≥5 years of follow-up.
Materials and methods
Patient characteristics
From June 2008 to July 2010, 101 patients (Table I) with single-level lumbar
degeneration were recruited at Tangdu Hospital (Xi'an, China) and
were randomly divided into two groups. Patients in the m-TLIF group
were treated using the Quadrant retractor and Sextant percutaneous
pedicle screw systems (Medtronic Sofamor Danek, Minneapolis, MN,
USA) and patients in c-TLIF were treated using the classical open
procedure (Medtronic Sofamor Danek). Written informed consent was
obtained from all participants prior enrollment. The clinical study
was approved by the Medical Ethics Committee at Tangdu Hospital
(Xi'an, China).
 | Table I.Patient baseline demographics. |
Table I.
Patient baseline demographics.
| Variable | m-TLIF | c-TLIF | P-value |
|---|
| Patients (n) | 52 | 49 |
|
| Lost in
follow-up (n) | 6 | 4 |
|
| Completed
follow-up (n) | 46 | 45 |
|
| Age (years) | 57.3±10.5 | 58.5±10.8 | 0.604 |
| Sex
(male/female) | 26/20 | 27/18 | 0.740 |
| Body mass index | 22.1±5.1 | 23.2±3.4 | 0.350 |
| Location of
disease |
| L2/3 | 4 | 4 | 0.971 |
| L3/4 | 7 | 5 | 0.558 |
| L4/5 | 24 | 27 | 0.452 |
|
L5/S1 | 11 | 9 | 0.648 |
| Follow-up duration
(month) | 62.0±1.66 | 62.3±1.54 | 0.508 |
Patients with the following characteristics were
included: i) Age, 21–60 years; ii) diagnosis, single-level lumbar
disc herniation; iii) X-ray imaging, computed tomography (CT) scan
and magnetic resonance imaging (MRI) results consistently explain
clinical symptoms; and iv) unresponsive to conservative treatment
for ≥6 months prior to surgery. Exclusion criteria were as follows:
i) >1 level lumbar degenerative disease; ii) previous lumbar
surgery; iii) contraindications to surgery or with other diseases,
including tumors or infections; and 5) metal allergies.
Randomization was immediately prior to surgery
through a sealed envelope assigning patients to m- or c-TLIF
groups. Surgeons were informed of the allocation following the
induction of anesthesia. All surgical procedures were performed by
a senior surgeon with assistants. Staff that provided direct
postoperative care was blinded to group assignments and
treatments.
Surgical procedure
Patients were positioned on a radiolucent frame
under general anesthesia. A 3 cm longitudinal incision 3 cm lateral
to the anatomic back midline was performed to insert the m-TLIF
system. A complete facetectomy was performed and the lateral border
of the dura was directly visualized. Following identifying the
traversing and exiting nerve roots, an aggressive full discectomy
was performed (16). Interbody
distractors were used to prepare the disc space. Autologous bone
graft removed from the facet was implanted in the anterior space. A
single cage (PEEK OIC; Stryker Inc., Kalamazoo, MI, USA) was
inserted into the disc space. The side with subjectively worse
radiculopathy received the interbody graft and cage. Following the
removal of the m-TLIF system, the surgeon directly palpated the
pedicle entry point. A cannulated needle was advanced through the
pedicle into the vertebral body under fluoroscopic guidance,
followed by the insertion of a blunt-tipped guide-wire (Stryker
Corporation, Kalamazoo, MI, USA) into the vertebral body. The
cannulated needle was removed and the screw (Stryker Corporation)
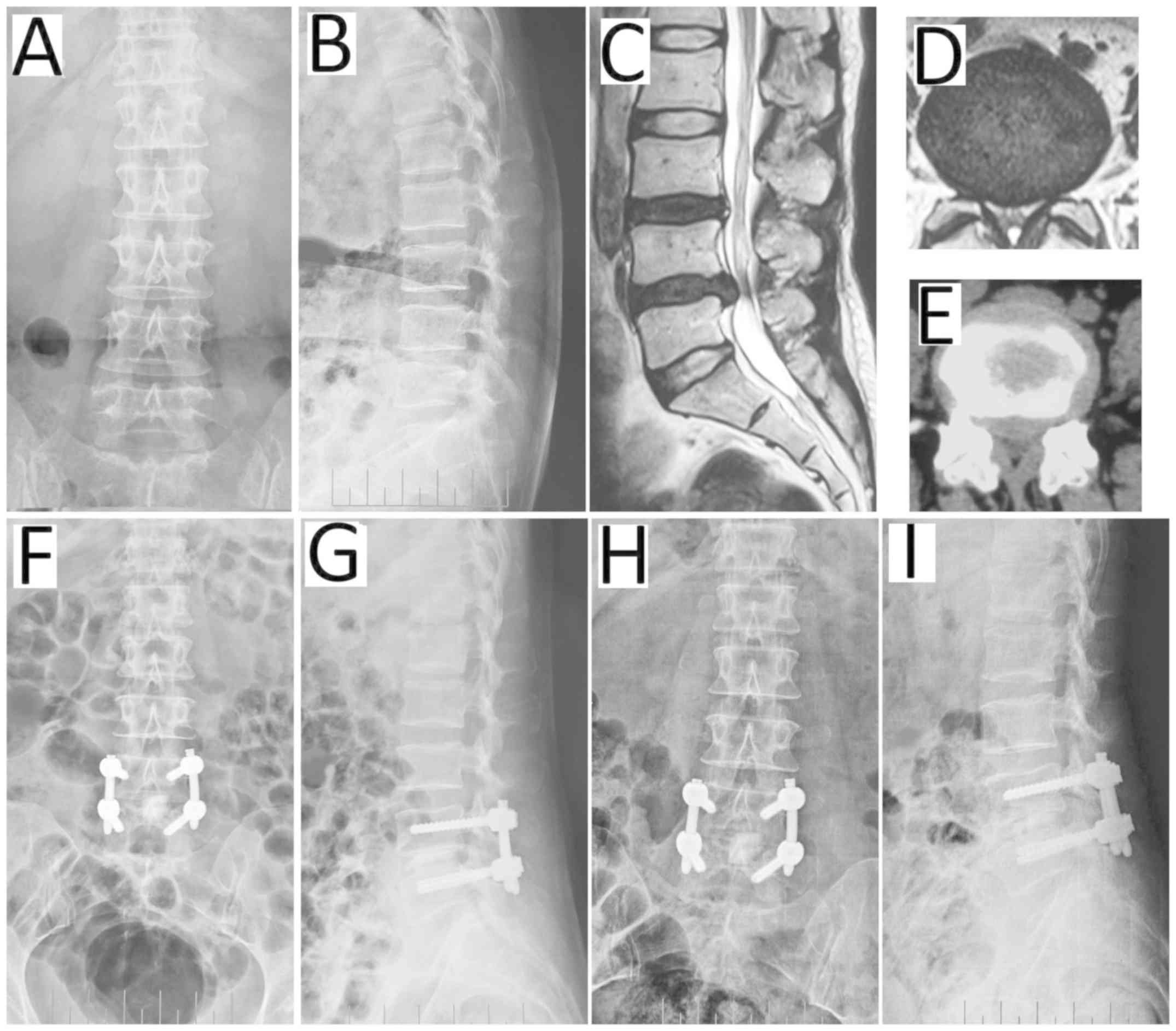
was placed following the guide-wire path. A representative case is
presented in Fig. 1.
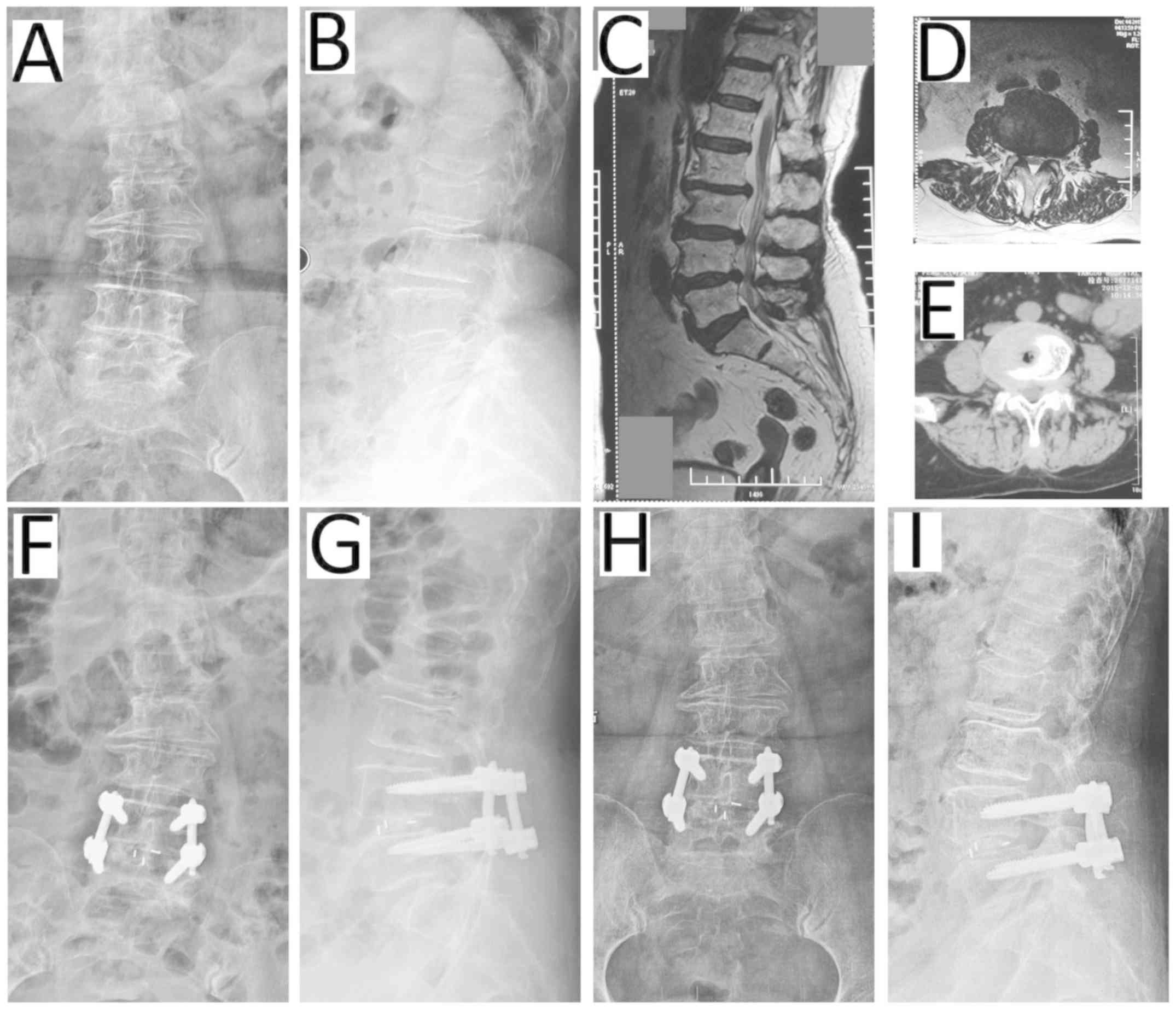
Surgery in the c-TLIF group started with a 12 cm
incision on the anatomic back midline. A mono-portal TLIF with a
unilateral subtotal facetectomy and discectomy was performed from
the symptomatic side. Pedicle screws were placed and facets were
decorticated prior to traversing the processes and implanting the
autologous bone graft that was obtained from the laminectomy and
facetectomy. A representative case is presented in Fig. 2.
Outcome measures and evaluation
The preoperative radiographic evaluation included
anteroposterior, lateral and flexion-extension radiographs, CT and
MRI scans. The prospectively collected data included age, gender,
body mass index (BMI), location of disease, operative time,
intraoperative blood loss and X-ray exposure time. Outcome
measurements included radiographic results, T2 relaxation time on
MRI scans and postoperative complications during follow-up. Back
and leg pain was assessed by the visual analog scores (VAS)
(17,18) collected from the patients at 6
follow-up points (once every 6 months). Preoperative and
postoperative Japanese orthopedic association (JOA) scores
(19,20) were compared between the groups.
Completed union rates (17,19) were determined by an experienced
radiologist using static and dynamic X-rays at 6 follow-up times
post surgery (once every 6 months).
Statistical analysis
Statistical analyses were performed using SPSS 17.0
(SPSS, Inc., Chicago, IL, USA). Continuous data are presented as
the mean ± standard deviation. Student's t-test and χ2
tests were performed to analyze the data. P<0.05 was considered
to indicate a statistically significant difference.
Results
Study participants
A total of 101 patients with single-level lumbar
disc herniation were enrolled in the current study. Following a
random, sealed envelope assignment, 52 patients were treated using
m-TLIF and 49 patients underwent c-TLIF. A total of 10 patients
were lost during follow-up, 6 from the m-TLIF and 4 from the c-TLIF
group.
Baseline characteristic, including age, gender and
BMI, and the levellocation of the lumbar disc herniation were not
significantly different between the groups (P>0.05; Table I). Clinical and radiographic outcomes
were collected and analyzed for ≥5 years. The outcomes were
recorded and evaluated preoperatively and at 7 days and 1, 3, 12,
36 and 60 months post surgery.
Measured outcomes
The mean surgery time was 105.7±16.2 min in the
m-TLIF and 112.7±20.7 min in the c-TLIF group; there was no
significant difference (P=0.077; Table
II). Total intra-operative blood loss was 110.4±27.8 ml in the
m-TLIF group and 119.7±28.5 ml in the c-TLIF group, with no
significant difference between the groups (P=0.115). A significant
difference was observed between the mean X-ray exposure times of
116.2±26.5 and 81.7±25.1 sec in the m- and c-TLIF groups,
respectively (P<0.001). A significant difference was observed in
the MRI T2 relaxation times of the operated level muscles and other
soft tissues between the m- and c-TLIF groups at 3 months post
surgery (45.6±19.2 and 85.5±26.4 sec, respectively; both
P<0.001).
 | Table II.Outcome measurements. |
Table II.
Outcome measurements.
| Measure | m-TLIF | c-TLIF | F | P-value |
|---|
| Surgery duration
(min) | 105.7±16.2 | 112.7±20.7 | 3.196 | 0.077 |
| Intraoperative
blood loss (ml) | 110.4±27.8 | 119.7±28.5 | 2.530 | 0.115 |
| X-ray exposure
timea (sec) | 116.2±26.5 | 81.7±25.1 | 40.842 | <0.001 |
| MRI T2 relaxation
timea (sec) | 45.6±19.2 | 85.5±26.4 | 68.533 | <0.001 |
| VAS
scoreb | 0.348±0.077 | 0.333±0.079 | 0.017 | 0.895 |
| JOA
scoreb | 14.024±0.280 | 13.980±0.283 | 0.012 | 0.912 |
| Reoperation | 2/46 | 3/45 | 0.102 | 0.632 |
| Complete
fusionb | 45/46 | 44/45 | 0.015 | 0.991 |
Secondary surgery
One case in the m-TLIF and two cases in the c-TLIF
group were complicated by transient ipsilateral nerve root palsy
during surgery. Patients were recovered completely at 3 months post
surgery. In the m-TLIF group, 2/46 (4.3%) patients required
reoperation due to adjacent level degeneration at 4 and 5 years
post surgery. In the c-TLIF group, 3/45 (6.7%) patients required
reoperation at 3, 4 or 5 years post surgery. The incidence of
reoperation was not significantly different between the groups
(P=0.632; Table II).
VAS
Preoperative VAS scores were not significantly
different between the treatment groups. Postoperative VAS scores
markedly decreased compared with the preoperative scores in m- and
c-TLIF (data not shown). VAS scores at 7 days post surgery were
significantly lower in the m- compared with the c-TLIF group
(P<0.001; Table III). During
later follow-ups, VAS scores were not significantly different
between the groups (P>0.05).
 | Table III.Correlation of VAS scores in patients
treated with m- or c-TLIF over time. |
Table III.
Correlation of VAS scores in patients
treated with m- or c-TLIF over time.
| Variables | VAS score | F | P-value |
|---|
| Preoperative |
| 0.739 | 0.392 |
|
m-TLIF | 7.050±0.152
(6.748–7.352) |
|
|
|
c-TLIF | 6.864±0.153
(6.559–7.169) |
|
|
| Follow-up at 7 days
post surgery |
| 125.650 | <0.001 |
|
m-TLIF | 3.352±0.135
(3.083–3.621) |
|
|
|
c-TLIF | 5.511±0.137
(5.239–5.783) |
|
|
| Follow-up at 1
month post surgery |
| 3.510 | 0.064 |
|
m-TLIF | 3.117±0.118
(2.883–3.351) |
|
|
|
c-TLIF | 3.431±0.119
(3.195–3.668) |
|
|
| Follow-up at 3
months post surgery |
| 3.857 | 0.053 |
|
m-TLIF | 2.043±0.087
(1.870–2.217) |
|
|
|
c-TLIF | 1.800±0.088
(1.625–1.975) |
|
|
| Follow-up at 12
months post surgery |
| 2.046 | 0.156 |
|
m-TLIF | 1.783±0.118
(1.549–2.017) |
|
|
|
c-TLIF | 2.022±0.119
(1.786–2.259) |
|
|
| Follow-up at 36
months post surgery |
| 0.251 | 0.618 |
|
m-TLIF | 0.587±0.106
(0.375–0.798) |
|
|
|
c-TLIF | 0.511±0.108
(0.297–0.725) |
|
|
| Follow-up at 60
months post surgery |
| 0.017 | 0.895 |
|
m-TLIF | 0.348±0.077
(0.194–0.501) |
|
|
|
c-TLIF | 0.333±0.078
(0.178–0.489) |
|
|
JOA
Preoperative JOA scores were not significantly
different between m- and c-TLIF groups. Postoperative JOA scores
were markedly increased compared to the preoperative scores for m-
and c-TLIF (data not shown). Compared with the c-TLIF group, there
were no significant differences in JOA scores over time for the
m-TLIF group (P>0.05), except at 7 days post surgery (P=0.028;
Table IV).
 | Table IV.Correlation of JOA scores in patients
treated with m- or c-TLIF over time. |
Table IV.
Correlation of JOA scores in patients
treated with m- or c-TLIF over time.
| Variables | JOA score | F | P-value |
|---|
| Preoperative |
| 0.273 | 0.603 |
|
m-TLIF | 11.941±0.202
(11.539–12.343) |
|
|
|
c-TLIF | 11.791±0.204
(11.385–12.197) |
|
|
| Follow-up at 7 days
post surgery |
| 4.997 | 0.028 |
|
m-TLIF | 13.952±0.264
(13.428–14.477) |
|
|
|
c-TLIF | 13.113±0.267
(12.583–13.643) |
|
|
| Follow-up at 1
month post surgery |
|
|
|
|
m-TLIF | 14.154±0.275
(13.609–14.700) | 0.175 | 0.677 |
|
c-TLIF | 13.991±0.278
(13.439–14.543) |
|
|
| Follow-up at 3
months post surgery |
| 0.789 | 0.377 |
|
m-TLIF | 14.135±0.212
(13.713–14.556) |
|
|
|
c-TLIF | 13.867±0.215
(13.440–14.293) |
|
|
| Follow-up at 12
months post surgery |
| 0.016 | 0.901 |
|
m-TLIF | 14.096±0.275
(13.550–14.642) |
|
|
|
c-TLIF | 14.047±0.278
(13.495–14.599) |
|
|
| Follow-up at 36
months post surgery |
| 0.027 | 0.870 |
|
m-TLIF | 13.870±0.251
(13.371–14.368) |
|
|
|
c-TLIF | 13.811±0.254
(13.307–14.315) |
|
|
| Follow-up at 60
months post surgery |
| 0.012 | 0.912 |
|
m-TLIF | 14.024±0.280
(13.468–14.580) |
|
|
|
c-TLIF | 13.980±0.283
(13.417–14.543) |
|
|
Discussion
The m-TLIF procedure was first introduced by Foley
et al (11) to minimize
injury to the paraspinal muscles caused by the classical procedure.
Since then, m-TLIF using the minimal access spinal technologies
(MAST) quadrant retractor was subject of increased research
interest (12,21–23).
Certain surgeons advocate m-TLIF to preserve the muscular and
vascular lumbar structures (21–24).
Consistent with previous investigations, a study reinforced the
concept of minimizing lumbar muscle damage by using a minimal
invasive approach, which resulted in faster and improved short-term
recovery from injury (21) compared
with c-TLIF. Furthermore, it was demonstrated that there is no
clinically relevant difference between mini-open TLIF and c-TLIF
over a 3–4 year follow-up period (22). Research by Wang et al
(23,24) revealed that m-TLIF efficacy and
safety is similar to c-TLIF, when treating primary single-level
lumbar degeneration (23) and for
treating patients in revision, who were previously treated using
open surgery (24). The latter study
further demonstrated that m-TLIF offered several potential
advantages, including smaller incisions, less tissue injury and
quicker recovery. Most studies have consistently reported the
advantages of this approach (25)
and the rate of fusion was not significantly different among the
different approaches (25,26). In conclusion, compared with c-TLIF,
potential benefits of m-TLIF include smaller skin incisions,
decreased soft tissue injury, decreased blood loss, shorter
hospitalization time and earlier returns to work (21–26). The
potential disadvantages of this approach include increased surgery
times and radiation exposure; the procedure is more technically
demanding and more experience is required (27). Accumulated radiation exposure,
particularly to the hands of the surgeons should be monitored
carefully. Furthermore, the cost of m-TLIF is increased compared
with c-TLIF (28). Controversy
remains regarding the selection of m-TLIF vs. c-TLIF. Vogelsang
(29), suggested that the selection
of procedure should be based on the approach that offers superior
individual outcome.
To determine the effectiveness and safety of m-TLIF
over an extended period, a randomized controlled study was
conducted, which compared m- and c-TLIF in patients with
single-level lumbar disc disease. It was demonstrated that there
was no significant difference between these groups with respect to
surgery duration, intraoperative blood loss and intraoperative
complications, including transient ipsilateral nerve root palsy.
These findings were not consistent with the previously reported
results (23,27). One explanation may be the varying
experience levels of the surgeons performing the procedures. In
this controlled study, a total of three patients suffered transient
nerve root palsy. The variant anatomical structure of the nerve
root increased the difficulty of the surgery and accidental injury
to the nerve root caused the palsy. Compared with classical
surgery, TLIF using the MAST quadrant retractor may decrease the
length of hospitalization and result in decreased injury to the
soft tissue, which manifested in a significantly decreased MRI T2
relaxation times in the operated level muscles and other soft
tissues at 3 months post surgery. The X-ray exposure time in the
c-TLIF group was significantly decreased compared with the m-TLIF
group; describing an obvious disadvantage of latter procedure.
There were no significant differences in JOA and VAS scores between
the groups in follow-ups between 1 month and 5 years post surgery.
However, at the 7-day post surgery follow-up, the VAS score of the
m-TLIF group were decreased significantly compared with the c-TLIF
group. m-TLIF was more effective in relieving pain compared with
c-TLIF at early stages post surgery. As the minimally invasive
retractor split the soft tissues and muscles instead of cutting
them, it was possible to minimize the postoperative low back pain
by reducing muscle damage. To gain a clear view during c-TILF
surgery, muscles have to be cut and damaged, leading to an
increased possibility of postoperative backache. Two patients in
the m-TLIF and three in the c-TLIF group required reoperation due
to adjacent level degeneration; the reoperation rate was not
significantly different between the groups. The patients treated
with the same procedure as the first time. The current study
demonstrated that m-TLIF was safe to be considered an alternative
to the c-TLIF procedure.
Despite the benefits, there are certain drawbacks to
overcome prior to achieving effective results. First, manual
experience is required and surgeons must be familiar with the novel
techniques and have to be able to operate in narrow spaces. For
inexperienced surgeons working in a narrow surgical field may lead
to confusion regarding anatomical structures. Limitations regarding
effective decompression are to further be considered. Following the
completion of surgery, symptoms of nerve compression (one case of
transient ipsilateral L5 nerve root palsy) may appear immediately
(30), resulting from a small
hematoma generated in the narrow surgical space. It is therefore
important to control even minimal bleeding.
To achieve a sufficient decompression of the spinal
nerves, an MRI scan must be studied carefully to determine the
extent and scope of the herniation of the nucleus pulposus prior to
surgery. In cases of far lateral disc disease, discectomy and
decompression can be performed to access the midline and
extraforaminal space through only one skin incision (25). Understanding the surrounding
structures is important when moving and positioning the minimally
invasive retractor in the extraforaminal space. To avoid damaging
the nerve root during decompression, it is important to leave the
inner cortical part of the caudal lamina and remove the remaining
portion. The herniated nucleus pulposus is removed in the same
manner as in classical surgery.
To safely place an interbody implant, an adequate
laminectomy and facetectomy may be performed. A single cage was
impacted into the intervertebral space following the complete
removal of the nucleus pulposus through the minimally invasive
retractor. Autograft bones from the laminectomy and facetectomy
were placed in the interspace to augment the fusion. Isaacs et
al (31) concluded that m-TLIF
was safe and resulted in decreased intraoperative blood loss,
postoperative pain, total narcotic use and risk of transfusion.
Pedicle screws can easily be inserted percutaneously via the
minimally invasive retractor systems.
In conclusion, the minimally invasive retractor
system is a safe and effective tool in the treatment of
single-level disc herniation. However, careful attention to the
surgical technique and precise anatomical knowledge are mandatory
skills for surgeons. Further studies and the refinement of surgical
techniques will be required in the future to allow the treatment of
multiple or more extensive lesions using m-TLIF.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
JQ designed the study. HZ, HG and CZ analyzed the
data and wrote the manuscript. SQ, YY and WX collected the data.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Medical Ethics
Committee at Tangdu Hospital (Xi'an, China). Written informed
consent was obtained from all participants prior enrollment.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Atlas SJ, Keller RB, Robson D, Deyo RA and
Singer DE: Surgical and nonsurgical management of lumbar spinal
stenosis: Four-year outcomes from the maine lumbar spine study.
Spine (Phila Pa 1976). 25:556–562. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Atlas SJ, Keller RB, Wu YA, Deyo RA and
Singer DE: Long-term outcomes of surgical and nonsurgical
management of lumbar spinal stenosis: 8 to 10 year results from the
maine lumbar spine study. Spine (Phila Pa 1976). 30:934–936. 2005.
View Article : Google Scholar
|
|
3
|
Cloward RB: History of PLIF: Forty years
of personal experience. Lin PM: Posterior lumbar interbody fusion.
Charles C Thomas. (Springfield). 58–71. 1982.
|
|
4
|
Cloward RB: The treatment of ruptured
lumbar intervertebral discs by vertebral body fusion. I.
Indications, operative technique, after care. J Neurosurg.
10:154–168. 1953. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Harms JG and Jeszenszky D: Die posteriore,
lumbale, interkorporelle fusion in unilateraler transforaminaler
technik. Oper Orthop Traumatol. 10:90–102. 1998.(In German).
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Scheufler KM, Dohmen H and Vougioukas VI:
Percutaneous transforaminal lumbar interbody fusion for the
treatment of degenerative lumbar instability. Neurosurgery 60 (4
Suppl 2). S203–S213. 2007.
|
|
7
|
Liu J, Deng H, Long X, Chen X, Xu R and
Liu Z: A comparative study of perioperative complications between
transforaminal versus posterior lumbar interbody fusion in
degenerative lumbar spondylolisthesis. Eur Spine J. 25:1575–1580.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mehta VA, McGirt MJ, Garcés Ambrossi GL,
Parker SL, Sciubba DM, Bydon A, Wolinsky JP, Gokaslan ZL and Witham
TF: Trans-foraminal versus posterior lumbar interbody fusion:
Comparison of surgical morbidity. Neurol Res. 33:38–42. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pradhan BB, Nassar JA, Delamarter RB and
Wang JC: Single-level lumbar spine fusion: A comparison of anterior
and posterior approaches. J Spinal Disord Tech. 15:355–361. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stevens KJ, Spenciner DB, Griffiths KL,
Kim KD, Zwienenberg-Lee M, Alamin T and Bammer R: Comparison of
minimally invasive and conventional open posterolateral lumbar
fusion using magnetic resonance imaging and retraction pressure
studies. J Spinal Disord Tech. 19:77–86. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Foley KT, Holly LT and Schwender JD:
Minimally invasive lumbar fusion. Spine (Phila Pa 1976). 28 (15
Suppl):S26–S35. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rouben D, Casnellie M and Ferguson M:
Long-term durability of minimal invasive posterior transforaminal
lumbar interbody fusion: A clinical and radiographic follow-up. J
Spinal Disord Tech. 24:288–296. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Eck JC, Hodges S and Humphreys SC:
Minimally invasive lumbar spinal fusion. J Am Acad Orthop Surg.
15:321–329. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Goldstein CL, Macwan K, Sundararajan K and
Rampersaud YR: Perioperative outcomes and adverse events of
minimally invasive versus open posterior lumbar fusion:
Meta-analysis and systematic review. J Neurosurg Spine. 24:416–427.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hackenberg L, Halm H, Bullmann V, Vieth V,
Schneider M and Liljenqvist U: Transforaminal lumbar interbody
fusion: A safe technique with satisfactory three to five year
results. Eur Spine J. 14:551–558. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mummaneni PV and Rodts GE Jr: The
mini-open transforaminal lumbar interbody fusion. Neurosurgery. 57
(4 Suppl):S256–S261. 2005.
|
|
17
|
Arts MP, Wolfs JF, Kuijlen JM and de
Ruiter GC: Minimally invasive surgery versus open surgery in the
treatment of lumbar spondylolisthesis: Study protocol of a
multicentre, randomised controlled trial (MISOS trial). BMJ Open.
7:e0178822017.PubMed/NCBI
|
|
18
|
Franke J, Greiner-Perth R, Boehm H,
Mahlfeld K, Grasshoff H, Allam Y and Awiszus F: Comparison of a
minimally invasive procedure versus standard microscopic discotomy:
A prospective randomised controlled clinical trial. Eur Spine J.
18:992–1000. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Minamide A, Yoshida M, Simpson AK,
Nakagawa Y, Iwasaki H, Tsutsui S, Takami M, Hashizume H, Yukawa Y
and Yamada H: Minimally invasive spinal decompression for
degenerative lumbar spondylolisthesis and stenosis maintains
stability and may avoid the need for fusion. Bone Joint J 100-B.
499–506. 2018. View Article : Google Scholar
|
|
20
|
Tian W, Yan K and Han X, Yu J, Jin P and
Han X: Comparison of the clinical and radiographic results between
cervical artificial disk replacement and anterior cervical fusion:
A 6-year prospective nonrandomized comparative study. Clin Spine
Surg. 30:E578–E586. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rodríguez-Vela J, Lobo-Escolar A,
Joven-Aliaga E, Herrera A, Vicente J, Suñén E, Loste A and Tabuenca
A: Perioperative and short-term advantages of mini-open approach
for lumbar spinal fusion. Eur Spine J. 18:1194–1201. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rodríguez-Vela J, Lobo-Escolar A, Joven E,
Muñoz-Marín J, Herrera A and Velilla J: Clinical outcomes of
minimally invasive versus open approach for one-level
transforaminal lumbar interbody fusion at the 3-to 4-year
follow-up. Eur Spine J. 22:2857–2863. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ
and Liu J: Comparison of one-level minimally invasive and open
transforaminal lumbar interbody fusion in degenerative and isthmic
spondylolisthesis grades 1 and 2. Eur Spine J. 19:1780–1784. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ
and Liu J: Minimally invasive or open transforaminal lumbar
interbody fusion as revision surgery for patients previously
treated by open discectomy and decompression of the lumbar spine.
Eur Spine J. 20:623–628. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Guan J, Bisson EF, Dailey AT, Hood RS and
Schmidt MH: Comparison of clinical outcomes in the national
neurosurgery quality and outcomes database for open versus
minimally invasive transforaminal lumbar interbody fusion. Spine
(Phila Pa 1976). 41:E416–E421. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Seng C, Siddiqui MA, Wong KP, Zhang K, Yeo
W, Tan SB and Yue WM: Five-year outcomes of minimally invasive
versus open transforaminal lumbar interbody fusion: A matched-pair
comparison study. Spine (Phila Pa 1976). 38:2049–2055. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Funao H, Ishii K, Momoshima S, Iwanami A,
Hosogane N, Watanabe K, Nakamura M, Toyama Y and Matsumoto M:
Surgeons' exposure to radiation in single- and multi-level
minimally invasive transforaminal lumbar interbody fusion; a
prospective study. PLoS One. 9:e952332014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Singh K, Nandyala SV, Marquez-Lara A,
Fineberg SJ, Oglesby M, Pelton MA, Andersson GB, Isayeva D, Jegier
BJ and Phillips FM: A perioperative cost analysis comparing
single-level minimally invasive and open transforaminal lumbar
interbody fusion. Spine J. 14:1694–1701. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Vogelsang JP: The translaminar approch in
combination with a tubular retractor system for the treatment of
far cranio-laterally and foraminally extruded lumbar disc
herniations. Zentralbl Neurochir. 68:24–28. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang HL, Lü FZ, Jiang JY, Ma X, Xia XL and
Wang LX: Minimally invasive lumbar interbody fusion via MAST
Quadrant retractor versus open surgery: A prospective randomized
clinical trial. Chin Med J (Engl). 124:3868–3874. 2011.PubMed/NCBI
|
|
31
|
Issacs RE, Podichetty VK, Santiago P,
Sandhu FA, Spears J, Kelly K, Rice L and Fessler RG: Minimally
invasive microendoscopy-assisted transforaminal lumbar interbody
fusion with instrumentation. J Neurosurg Spine. 3:98–105. 2005.
View Article : Google Scholar : PubMed/NCBI
|