Introduction
Hip fracture is the most devastating result of
osteoporosis (1). Hip fracture in
the elderly population, due to its frequent adverse outcomes and
high mortality, has become a major medical and public health
problem (2–5). According to statistics, 5% of men and
10% of women suffer from hip fractures during their lifetime
(6). The mortality rate in the first
year after injury of the hip in elderly patients can reach up to
20% (5,6). According to the manual of the Brazilian
Society of Geriatrics and Gerontology in 2008, approximately 5% of
falls have caused fractures, the most common is a cone fracture.
The incidence of hip fractures is increasing in many countries
(7), so is the risk of subsequent
hip fracture after a fall of elderly people (8). In most cases, fractures have a serious
impact on the patient's physical ability and longevity (9). Both the combined spinal-epidural
anesthesia and the general anesthesia are common anesthesia methods
for hip arthroplasty. Due to the decreased physiological
compensatory capacity and the poor cardiopulmonary function of the
elderly, the risk of surgery and anesthesia increases in elderly
patients. Rashid and his coworkers demonstrated that anesthesia
should be customized for the individual needs of the patient
(10). The choice of anesthesia in
various surgical operations remains controversial (11). Therefore, it is important to choose
an anesthesia method that ensures the efficacy of anesthesia while
reducing the irritation to the patient and improving the safety of
the operation. This study mainly analyzed the effect and clinical
value of the general anesthesia and the combined spinal-epidural
anesthesia in elderly patients undergoing hip arthroplasty.
Patients and methods
General information
One hundred and six elderly patients who received
hip arthroplasty in the department of orthopedics in the Affiliated
Nanhua Hospital, University of South China (Hengyang, China) from
May 2013 to July 2015 were selected as the research subjects and
were divided into the study group (50 patients) and the control
group (56 patients) according to different anesthesia methods. The
study group consisted of 23 males and 27 females, aged from 60 to
87 (72.5±6.8) years who received combined spinal-epidural
anesthesia by ondansetron hydrochloride tablets combined with
spinal-epidural puncture kit, and the control group consisted of 27
males and 29 females, aged from 61 to 88 (75.4±7.2) years who
received general anesthesia by fast-induced endotracheal
intubation. No significant differences existed in terms of sex,
age, BMI and other general data between the two groups (P>0.05).
All the patients and their families signed the informed consent and
cooperated with medical staff to complete relevant medical
treatment. This study was approved by the Ethics Committee of the
Affiliated Nanhua Hospital, University of South China. The general
information is shown in Table I.
 | Table I.Comparison of general data between the
two groups of patients [n (%)]. |
Table I.
Comparison of general data between the
two groups of patients [n (%)].
| Group | Study group
(n=50) | Control group
(n=56) | χ2/t
value | P-value |
|---|
| Sex |
|
| 0.052 | 0.820 |
| Male | 23 | 27 |
|
|
|
Female | 27 | 29 |
|
|
| Age (year) |
|
| 0.149 | 0.700 |
| ≤75 | 25 | 29 |
|
|
| ≥75 | 25 | 27 |
|
|
| BMI
(kg/m2) |
|
| 0.004 | 0.947 |
| ≤22 | 22 | 25 |
|
|
|
>22 | 28 | 31 |
|
|
| Heart rate
(beat·min−1) |
80.64±5.14 |
79.48±4.84 | 1.173 | 0.243 |
| Systolic blood
pressure (mmHg) | 130.24±8.84 | 128.51±8.97 | 0.998 | 0.321 |
| Diastolic blood
pressure (mmHg) |
86.24±5.16 |
86.54±5.24 | 0.296 | 0.768 |
| Drinking
situation |
|
| 0.210 | 0.647 |
| Yes | 21 | 26 |
|
|
| No | 29 | 30 |
|
|
| Smoking
situation |
|
| 0.013 | 0.911 |
| Yes | 20 | 23 |
|
|
| No | 30 | 33 |
|
|
Methods
For patients in both groups, before the anesthesia,
the intravenous access was established on the upper limb of the
patient, and the detection instrument was connected to the patient
to monitor vital signs such as breathing, blood pressure, and heart
rate. Patients in the study group received combined spinal-epidural
anesthesia by ondansetron hydrochloride tablets combined with
spinal-epidural puncture kit, and the specific procedures were as
follows: the patient was placed lying on the uninjured side, with
the L3-4 gap as the puncture point, and then was anesthetized by
the ondansetron hydrochloride tablets combined with spinal-epidural
puncture kit. After the successful puncture, 7.5–10 mg of 0.5%
bupivacaine was injected into the subarachnoid space in 40 sec, and
the epidural tube was placed. For patients whose level of
anesthesia did not reach the 8th thoracic level 16 min after the
drug administration, a total of 7.75 ml of 2% lidocaine was
additionally injected from the epidural tube at two separate times
(6.54 ml for the first time and 1.21 ml for the second time).
Surgery was started after the spinal anesthesia was stabilized, and
2% lidocaine was added intermittently during the operation
according to the situation.
Patients in the control group received general
anesthesia by fast-induced endotracheal intubation, and the
specific methods were as follows: mask oxygenation and endotracheal
intubation were performed on patients with the use of ondansetron
at a dose of 0.1 mg for per kilogram of the patient's weight,
fentanyl at a dose of 2 µg for per kilogram of the patient's
weight, carbazole diazepam at a dose of 0.1 mg for per kilogram of
the patient's weight, etomidate at a dose of 0.2 mg for per
kilogram of the patient's weight. After 3 min of continuous
intubation, the respiration was regulated to a satisfatory state,
and then a constant use of fentanyl combined with propofol
followed, with a 1:2,000 ratio of the two.
Inclusion and exclusion criteria
All research subjects received hip arthroplasty in
the department of orthopedics in the Affiliated Nanhua Hospital,
University of South China. Patients with severe impairment in
mental function or cognitive function were excluded from the study,
so were patients with other cardiovascular diseases, liver
dysfunction, and renal dysfunction, and patients allergic to the
drugs used.
Observation criteria and evaluation
criteria
Comparisons between the two groups were made in
terms of the patient's anesthesia effect, complete block time,
anesthesia onset time, the hemodynamic parameters at different time
points of the patient's surgery, and postoperative adverse
reactions. Evaluation criteria for anesthesia effect: excellent
effect: patients were calm, with great state of muscle relaxation
and no pain symptoms, in no need for adjuvant drugs; good effect:
patients were in fairly good state of muscle relaxation, with
occasional pain and temporary need for adjuvant drugs; poor effect:
patients were not calm, with poor state of muscle relaxation and
pain symptoms, in need for adjuvant drugs.
Statistical methods
The data were analyzed and processed using SPSS 19.6
statistical software [Boyi (Beijing) Information Technology Co.,
Ltd., Beijing, China]. The patient's basic enumeration data was
expressed as a percentage [n (%)] and analyzed by the Chi-square
test. The complete block time, anesthesia onset time, and
hemodynamic parameters were expressed as the mean ± standard
deviation (mean ± SD) and calculated using the t-test, and the
statistical significance was set at P<0.05.
Results
Comparison of anesthetic effects
between the two groups
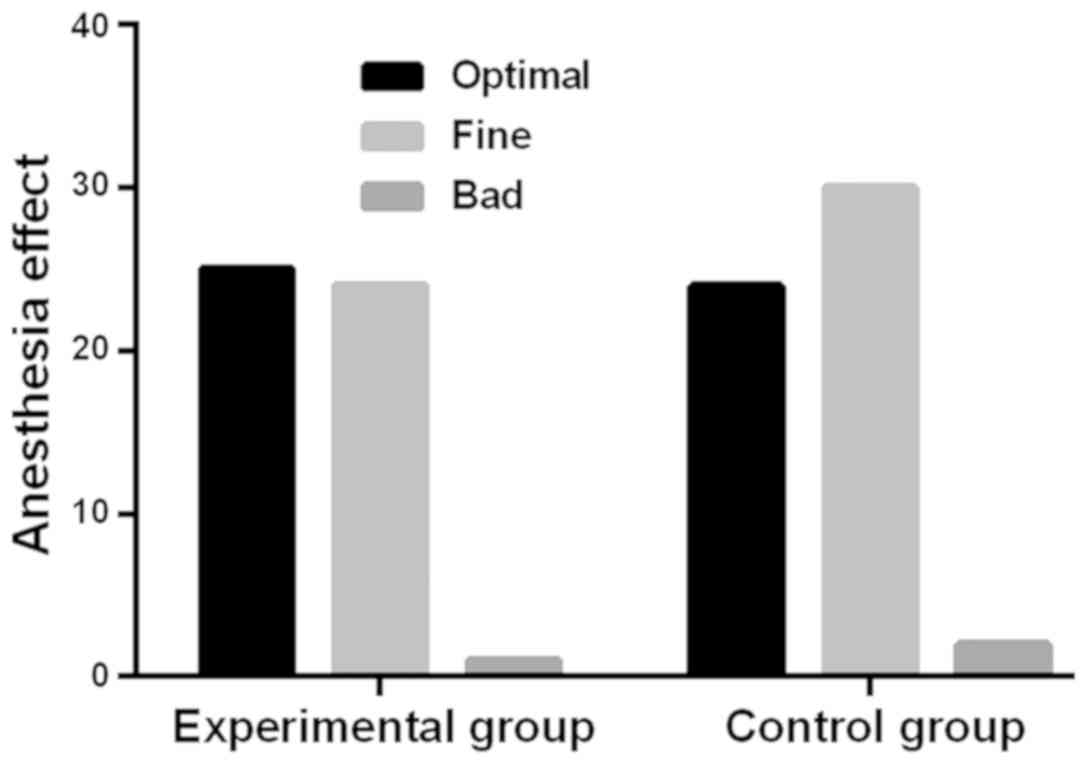
The rate of excellent and good anesthesia effect in
the study group was 98.00%, with 25 patients receiving excellent
effect, 24 patients receiving good effect and 1 patient receiving
poor effect. The rate of excellent and good anesthesia effect in
the control group was 96.43%, with 24 patients receiving excellent
effect, 30 patients receiving good effect and 2 patients receiving
poor effect. The anesthetic effect of the study group was better
than that of the control group, but the difference was not
statistically significant (χ2=0.683, P>0.05)
(Fig. 1).
Comparison of complete block time and
anesthesia onset time
The study group had an onset time of 20.8±4.8 sec
and a complete block time of 8.9±2.8 min, shorter than the onset
time (61.5±17.5 sec) and the complete block time (13.9±2.5 min) in
the control group, and the difference was statistically significant
(P<0.05) (Table II).
 | Table II.Comparison of complete block time and
anesthesia onset time (mean ± SD). |
Table II.
Comparison of complete block time and
anesthesia onset time (mean ± SD).
| Group | Anesthesia onset time
(sec) | Complete block time
(min) |
|---|
| Study group
(n=50) | 20.8±4.8 |
8.9±2.8 |
| Control group
(n=56) | 61.5±17.5 | 13.9±2.5 |
| t value | 15.86 | 10.14 |
| P-value | <0.001 | <0.001 |
Comparison of hemodynamic parameters
at different time points in the operation between the two
groups
The indexes of heart rate, systolic blood pressure,
and diastolic blood pressure before the operation in the study
group were 80.64±5.14, 130.24±8.84 and 86.24±5.16, respectively;
while heart rate, systolic blood pressure, and diastolic blood
pressure before the operation in the control group were 79.48±4.84,
128.51±8.97, and 86.54±5.24, respectively. The differences of the
heart rates, systolic blood pressures, and diastolic blood
pressures before the operation between the two groups were not
statistically significant (P>0.05). The heart rate, systolic
blood pressure, and diastolic blood pressure indexes 20 min after
the start of the operation in the study group were 74.84±4.27 and
123.47±6.74, 83.07±4.23, respectively, greatly higher than the
heart rate (63.17±4.54), the systolic blood pressure (111.27±6.48)
and the diastolic blood pressure (73.64±4.64) 20 min after the
start of the operation in the control group, and the differences
were statistically different (P<0.05). The heart rate, systolic
blood pressure, and diastolic blood pressure indexes 15 min before
the end of the operation in the study group were 76.94±4.61,
126.54±6.87, and 85.84±4.61, respectively, while the heart rate,
systolic blood pressure, and diastolic blood pressure indexes of
the control group 15 min before the end of the operation in the
control group were 68.41±4.61, 115.64±6.51, 77.56±4.81. The heart
rate, systolic blood pressure, and diastolic blood pressure index
15 min before the end of the operation in the study group were
significantly higher than that of the control group, and the
difference was statistically significant (P<0.05) (Table III).
 | Table III.Hemodynamic parameters at different
time points in the operation in the two groups (mean ± SD). |
Table III.
Hemodynamic parameters at different
time points in the operation in the two groups (mean ± SD).
|
| Study group
(n=50) | Control group
(n=56) |
|---|
|
|
|
|
|---|
| Group | Before the
experiment | 20 min after the
start of the operation | 15 min before the end
of the operation | Before the
experiment | 20 min after the
start of the operation | 15 min before the end
of the operation |
|---|
| Heart rate
(beat·min−1) |
80.64±5.14 |
74.84±4.27 |
76.94±4.61 |
79.48±4.84 |
63.17±4.54a |
68.41±4.61a |
| Systolic blood
pressure (mmHg) | 130.24±8.84 | 123.47±6.74 | 126.54±6.87 | 128.51±8.97 |
111.27±6.48a |
115.64±6.51a |
| Diastolic blood
pressure (mmHg) |
86.24±5.16 |
83.07±4.23 |
85.84±4.61 |
86.54±5.24 |
73.64±4.64a |
77.56±4.81a |
Comparison of postoperative adverse
reactions between the two groups
The study group had lower rate of adverse reactions
than the control group, with 1 case of venous thrombosis, 1 case of
pulmonary infection, and 1 case of nausea and vomiting in the study
group, while 7 cases of venous thrombosis, 8 cases of pulmonary
infection, and 8 cases of nausea and vomiting in the control group,
and the difference was statistically significant (P<0.05)
(Table IV).
 | Table IV.Comparison of postoperative adverse
reactions between the two groups [n (%)]. |
Table IV.
Comparison of postoperative adverse
reactions between the two groups [n (%)].
| Group | Venous
thrombosis | Pulmonary
infection | Nausea and
vomiting |
|---|
| Study group
(n=50) | 1 (2.00) | 1 (2.00) | 1 (2.00) |
| Control group
(n=56) | 7 (12.50) | 8 (14.29) | 8 (14.29) |
| χ2
value | 4.174 | 5.132 | 4.174 |
| P-value | 0.041 | 0.024 | 0.041 |
Discussion
Hip fracture is one of the most common injuries in
the elderly, and is associated with complications and mortality
(12–14). Approximately 3 million cases of hip
fractures occur each year in the United States, and this number is
expected to grow with the increase of elderly population (15). According to relevant reports, early
surgery can improve the treatment outcomes, including
hospitalization time, pulmonary function, and the ability to return
to independent life (16,17). Therefore, it is a wise choice to
perform surgical treatment on elderly patients with hip fracture
immediately after admission. However, early surgery is not feasible
for patients with physiological instability and high risk (18). Joint arthroplasty is often considered
a successful treatment beneficial to pain relief and the
improvement of quality of life (19). In addition to the quality of surgical
treatment, a suitable anesthesia method in accordance with the
actual situation of the patient in the specific surgery process is
also very important, which will directly affect the patient's
surgical quality and prognosis. Thus, a carefully selected
anesthesia method according to the situation of the patient is
needed to ensure a good surgical result and prognosis. This study
compared the efficacy and clinical value of the general anesthesia
and the combined spinal-epidural anesthesia in elderly patients
undergoing hip arthroplasty.
This study included 106 elderly patients with hip
arthroplasty in the department of orthopedics in the Affiliated
Nanhua Hospital, University of South China as the research
subjects. Patients in the study group underwent a combined
spinal-epidural anesthesia by ondansetron hydrochloride tablets
combined with spinal-epidural puncture kit, and patients in the
control group received a general anesthesia by fast-induced
endotracheal intubation. First, the anesthetic effects of the study
group and the control group were compared, and the anesthetic
effect of the study group was proved to be better than that of the
control group, but with no statistically significant difference
(P>0.05). No relevant data so far has pointed out whether there
is an improvement in performance of the general anesthesia compared
with the combined spinal-epidural anesthesia or the opposite.
At present, both local anesthesia and general
anesthesia are performed during the operation on the elderly.
However, the final choice of anesthesia comes from the
anesthesiologist's experience and preferences, as well as
discussions with patients and their caregivers (20). Next, this study compared the complete
block time and the anesthesia onset time and found that the onset
time and complete block time of the study group were shorter than
the control group, and the differences were statistically
significant (P<0.05). Studies have shown that (21) local anesthesia is currently selected
during the surgery to shorten the time of possible impact of
anesthesia residues on patients. The direct injection of anesthesia
into the local nerve innervation of the operation area that can
quickly block the generation and transmission of nerve impulses has
a positive effect on shortening the anesthesia time and improving
the safety of surgery. After that, the hemodynamic parameters of
the two groups before the surgery, 20 min after the start of the
operation, and 15 min before the end of the operation were
compared. The results showed that the two groups were not
statistically different in the preoperative heart rate, systolic
blood pressure, and diastolic blood (P>0.05); the heart rate,
systolic blood pressure, and diastolic blood pressure index of the
study group 20 min after the start of the operation were
statistically significantly higher than that of the control group
(P<0.05); the heart rate, systolic blood pressure, and diastolic
blood pressure index of the study group 15 min before the end of
the operation were significantly higher than the control group, and
the difference was statistically significant (P<0.05).
No previous study on the hemodynamics parameters
before and after hip arthroplasty has been reported. Studies have
shown that (22) general anesthesia
makes patients unconscious through the use of various intravenous
and/or inhaled drugs, which causes fewer cerebrovascular accidents
and shorter anesthesia time compared with local anesthesia. Other
studies have shown that (23), the
more adverse reactions of general anesthesia compared with spinal
anesthesia in total hip arthroplasty may be associated with the
increased incidence of intraoperative hypotension aroused by
general anesthesia, which serves as an excellent support for the
view of this study. Finally, comparison of the adverse reactions
between the two groups was performed and revealed fewer adverse
reactions such as venous thrombosis, pulmonary infection, nausea
and vomiting in the study group than in the control group, with a
statistical difference (P<0.05). Patients undergoing hip
arthroplasty are mainly elderly people who usually suffer from
cardiovascular diseases, diabetes and other senile diseases, with a
relatively slow blood flow and hypercoagulable blood due to
long-term bed rest and joint damage before the surgery. Traction of
vessels due to repeated dislocation, restoration and twist of the
limbs during the long operation time may cause damage to the
intima, promote the production of inflammatory cytokines, activate
the exogenous coagulation pathway, and arouse thrombosis. Studies
have proven (24) the marginal
advantage of local anesthesia in the risk of deep vein thrombosis
compared with general anesthesia in patients with hip fracture.
White and his team (25) pointed out
local anesthesia had a better effect than the general anesthesia to
inhibit pulmonary complications, which agrees with the findings of
this study.
In this study, despite every possible effort to
avoid errors caused by human factors, the small number of research
subjects was likely to cause some contingency and deviations in the
results.
In summary, the combined spinal-epidural anesthesia
by ondansetron hydrochloride tablets combined with spinal-epidural
puncture kit had a better anesthesia effect than the general
anesthesia by fast-induced endotracheal intubation. Both anesthesia
methods could maintain a good anesthesia sate, but combined
spinal-epidural anesthesia by ondansetron hydrochloride tablets
combined with spinal-epidural puncture kit could shorten the
complete block time and the anesthesia onset time and have less
impact on the patient's hemodynamic parameters, with a lower
incidence of complications.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HZ and YoW conceived and designed the study. YiW
collected the patient data. HZ and BW analyzed and interpreted the
data regarding the elderly patients undergoing hip arthroplasty. HZ
was a major contributor in writing the manuscript. BW reviewed the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Affiliated Nanhua Hospital, University of South China (Hengyang,
China). Patients who participated in this research had complete
clinical data. Signed informed consents were obtained from the
patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cauley JA: Public health impact of
osteoporosis. J Gerontol A Biol Sci Med Sci. 68:1243–1251. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Haentjens P, Magaziner J, Colón-Emeric CS,
Vanderschueren D, Milisen K, Velkeniers B and Boonen S:
Meta-analysis: Excess mortality after hip fracture among older
women and men. Ann Intern Med. 152:380–390. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Richmond J, Aharonoff GB, Zuckerman JD and
Koval KJ: Mortality risk after hip fracture. J Orthop Trauma.
17:53–56. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bliuc D, Nguyen ND, Milch VE, Nguyen TV,
Eisman JA and Center JR: Mortality risk associated with low-trauma
osteoporotic fracture and subsequent fracture in men and women.
JAMA. 301:513–521. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hung LW, Tseng WJ, Huang GS and Lin J:
High short-term and long-term excess mortality in geriatric
patients after hip fracture: A prospective cohort study in Taiwan.
BMC Musculoskelet Disord. 15:1512014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gullberg B, Johnell O and Kanis JA:
World-wide projections for hip fracture. Osteoporos Int. 7:407–413.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee KH, Ha YC, Lee YK, Kang H and Koo KH:
Frequency, risk factors, and prognosis of prolonged delirium in
elderly patients after hip fracture surgery. Clin Orthop Relat Res.
469:2612–2620. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen XW, Shi JW, Yang PS and Wu ZQ:
Preoperative plasma leptin levels predict delirium in elderly
patients after hip fracture surgery. Peptides. 57:31–35. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Heyes GJ, Tucker A, Marley D and Foster A:
Predictors for readmission up to 1 year following hip fracture.
Arch Trauma Res. 4:e271232015.PubMed/NCBI
|
|
10
|
Rashid RH, Shah AA, Shakoor A and Noordin
S: Hip fracture surgery: Does type of anesthesia matter? BioMed Res
Int. 2013:2523562013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gupta N: Delirium: another factor when
considering type of anesthetic for hip fracture surgery in adults.
BMJ. 349:g48712014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Buecking B, Bohl K, Eschbach D, Bliemel C,
Aigner R, Balzer-Geldsetzer M, Dodel R, Ruchholtz S and Debus F:
Factors influencing the progress of mobilization in hip fracture
patients during the early postsurgical period? - A prospective
observational study. Arch Gerontol Geriatr. 60:457–463. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Caillet P, Klemm S, Ducher M, Aussem A and
Schott AM: Hip fracture in the elderly: A re-analysis of the EPIDOS
study with causal Bayesian networks. PLoS One. 10:e01201252015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cook WL, Schiller C, McAllister MM, Hanson
HM, Brasher PM, Donaldson MG, Macri E, Preto R, Guy P and Ashe MC:
Feasibility of a follow-up hip fracture clinic. J Am Geriatr Soc.
63:598–599. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hawkes D, Baxter J, Bailey C, Holland G,
Ruddlesdin J, Wall A and Wykes P: Improving the care of patients
with a hip fracture: A quality improvement report. BMJ Qual Saf.
24:532–538. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sherrington C, Lord SR and Herbert RD: A
randomized controlled trial of weight-bearing versus
non-weight-bearing exercise for improving physical ability after
usual care for hip fracture. Arch Phys Med Rehabil. 85:710–716.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Boylan MR, Rosenbaum J, Adler A, Naziri Q
and Paulino CB: Hip fracture and the weekend effect: Does weekend
admission affect patient outcomes? Am J Orthop (Belle Mead NJ).
44:458–464. 2015.PubMed/NCBI
|
|
18
|
Clague JE, Craddock E, Andrew G, Horan MA
and Pendleton N: Predictors of outcome following hip fracture.
Admission time predicts length of stay and in-hospital mortality.
Injury. 33:1–6. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rolfson O, Rothwell A, Sedrakyan A, Chenok
KE, Bohm E, Bozic KJ and Garellick G: Use of patient-reported
outcomes in the context of different levels of data. J Bone Joint
Surg Am. 93 (Suppl 3):66–71. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li T, Yeung J, Li J, Zhang Y, Melody T,
Gao Y, Wang Y, Lian Q and Gao F; RAGA-Delirium Investigators, :
Comparison of regional with general anaesthesia on postoperative
delirium (RAGA-delirium) in the older patients undergoing hip
fracture surgery: Study protocol for a multicentre randomised
controlled trial. BMJ Open. 7:e0169372017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
White SM, Moppett IK and Griffiths R:
Outcome by mode of anaesthesia for hip fracture surgery. An
observational audit of 65,535 patients in a national dataset.
Anaesthesia. 69:224–230. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
White SM, Griffiths R, Holloway J and
Shannon A: Anaesthesia for proximal femoral fracture in the UK:
First report from the NHS Hip Fracture Anaesthesia Network.
Anaesthesia. 65:243–248. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Borghi B, Casati A, Iuorio S, Celleno D,
Michael M, Serafini P, Pusceddu A and Fanelli G; Study Group on
Orthopedic Anesthesia of the Italian Society of Anesthesia and
Analgesia, Intensive Care (SIAARTI), : Frequency of hypotension and
bradycardia during general anesthesia, epidural anesthesia, or
integrated epidural-general anesthesia for total hip replacement. J
Clin Anesth. 14:102–106. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Urwin SC, Parker MJ and Griffiths R:
General versus regional anaesthesia for hip fracture surgery: A
meta-analysis of randomized trials. Br J Anaesth. 84:450–455. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
White SM and Griffiths R: Projected
incidence of proximal femoral fracture in England: A report from
the NHS Hip Fracture Anaesthesia Network (HIPFAN). Injury.
42:1230–1233. 2011. View Article : Google Scholar : PubMed/NCBI
|