Introduction
Force is an innate ability of a body that enables an
individual to modify their body and environment. It is possible to
produce muscle power through effectors muscles. The proper function
of muscles allows for them to efficiently express adequate levels
of strength and forms the basis of health and well-being in
individuals. Furthermore, muscle strength is indispensable for
proper performance in sports and inevitably affects the practice of
any sports disciplines. Numerous studies (1–7) have
identified a significant role of the connective tissue that
surrounds muscles during contraction. Branislav et al
(8), hypothesized that the force
produced by muscle causes a deformation of the surrounding
connective tissue that affects strength. The transmission of muscle
strength is made possible by the contiguous nature of the fascia as
well as its integrity. These features facilitate the transmission
of force, which results in motor activity (7,9–11). Bordoni and Zanier (2) stated that ‘connective tissue can
control the orientation of the muscle fibres, so as to reflect the
vector of the direction of the force, and to make the transition of
the more fluid and ergonomic voltage’.
Fascial tissue alterations may induce various
symptoms that influence the quality of life of the subject
(12–13). In many instances, these symptoms are
debilitating and difficult to detect using conventional diagnostic
tests (14–17). For example, chronic fatigue is a
common symptom (18). Recent studies
have demonstrated that many physiological mechanisms are involved
in the development of muscle pain and fatigue, as the nociceptive
afferents of the fascial system are able to modulate the afferent
response of the central nervous system (18).
In the present study, we examined athletes who play
volleyball, a sport for which strength is needed and jumping is
needed too, this could be mentioned here as strength is needed in
many sports, but jumping is specific to volleyball. Many authors
have examined the concept of training of explosive strength
(19–23) and have concluded that jumping ability
can be a decisive factor in succeeding in volleyball as it
facilitates both attack and in defense (24–27).
Studies by Newton et al (28,29)
demonstrated that performing specific training tasks increases
power and strength of the muscles of the lower limbs, thereby
resulting in improvements in the height achieved during a vertical
jump.
The main goal of the present study was to evaluate
if undergoing specific osteopathic treatment of the lower limb
muscle groups in a sample of volleyball players could improve the
explosive force of the limbs. Our working hypothesis is that
osteopathic treatment, capable to reduce the stiffness of lower
limbs (30), make more efficient
expression of produced explosive force. Simultaneously, the
osteopathic treatment would decrease spasms and tension and release
tissue strain.
To this end, we have developed a protocol of
manipulative techniques with the aim of improving the functionality
of the lower limbs through the normalization of the fascial tissue,
in order to reduce the stiffness and thus to improving the
explosive force.
Materials and methods
Subjects
A total of 120 healthy semiprofessional male
volleyball players were recruited into this study. We excluded
athletes who had one or more of the following: scoliosis,
ligamentous laxity, a history of surgery (e.g., anterior cruciate
ligament reconstruction, deep scars type varicocele, appendectomy),
medication use, previous ligament injuries, or a muscle-tendon with
documented permanent outcomes or fractures.
Of the 120 athletes, only 57 athletes took part in
the present study. The 57 athletes were a mean age 24.18 (±1.75),
high 184.1 cm (1.63), weigh 78.12 kg (±2.25). All 57 athletes
performed three weekly training sessions and participated in a
game. The subjects were fully informed of the purpose of the study
and signed an informed consent document that was prepared according
to the ethical standards laid down in the Declaration of Helsinki.
The present research has been approved by the Ethics Committee of
the Kore University of Enna. We performed a randomized controlled
trial to evaluate whether fascial manipulative treatment was able
to affect lower limb muscle strength. The participants were
randomly divided into two groups: The fascial treatment group
(FTG), which was composed of 30 athletes, and the control group
(CG), which consisted of 27 athletes. Each participant was
convinced to receive the same osteopathic treatment of all other
subjects. In fact, the athletes of CG received only a non-specific
surface massage.
Experimental design
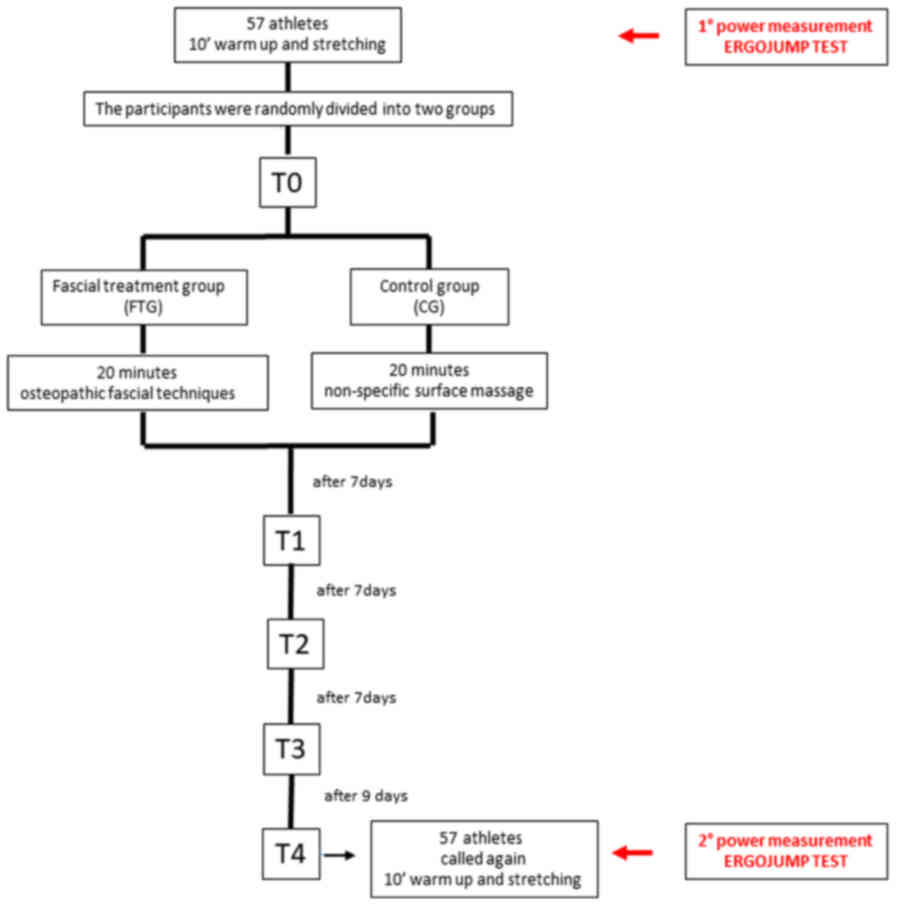
The working protocol included: T0 (Fig. 1): 57 athletes participated in 10 min
of warm up and stretching, before being subjected to the first
battery of tests that assessed the power of the lower limbs. The
sample was then divided into the FTG and CG. The FTG underwent
osteopathic fascial techniques (PFT) and the CG waited in the
locker room, received only a non-specific surface massage. Then,
all subjects underwent a second test to measure the power of the
lower limbs. T1: After seven days, the FTG was subjected to a
second treatment. T2: After seven more days (i.e., after 14 days
from the first treatment), the FTG was subjected to the third
treatment. T3: After seven more days (i.e., after 21 days from the
first treatment), the FTG was subjected to the fourth treatment.
T4: After nine more days (i.e., a month later (30 days)), the first
test was again conducted on both the FTG and CG groups (Fig. 1). The subjects completed a total of
four treatments, with a follow-up measurement performed after 30
days of treatment.
Lower limbs power rating
The evaluation of the power of the lower limbs was
conducted using jumping tests. As described by Bosco et al
(31), these tests involved a
platform that was placed on a rubber-coated contact mat connected
to a digital timer (Ergojump, Globus Inc., Treviso, Italy). The
protocol outlined in Bosco et al (31) and mathematical criteria established
by Bosco et al (31–32), were followed to perform two different
jumping motions: the jump squat jump (SJ) and the counter movement
jump (CMJ) (33).
The increase in flight time (FT) due to the muscle
pre-stretch in CMJ with respect to the jump without pre-stretch in
SJ, has repeatedly been attributed primarily to the release of
elastic energy (34–36). The height of the jump was measured in
centimeters. An expert in physiology and psychobiology who was
blinded to the study groups measured the power of the lower
limbs.
Squatting jump (SJ)
This type of jump allows for the detection of the
explosive force of the extensor muscles of the lower limbs. It is
an easily performable and repeatable test that consists of a
vertical jump at maximum intensity from the starting position,
without making any downward movement (countermovement). The subject
is in a starting position that includes having their feet evenly in
contact with the ground. The knees are bent starting from a
semisquat position with an angle of 90°. The opening angle of the
knee in the first jump is checked with a hands goniometer. The hips
and trunk are vertical to the ground during this type of jump.
Counter movement jump (CMJ)
This type of jump indicates the relief of the
elastic reuse capacity of the extensor muscles of the lower limbs.
It consists of a vertical jump at maximum intensity, starting from
the upright position, that is preceded by counter movement with
bending of the knees up to approximately 90° (muscle
stretch-shortening cycle). The subject then falls with spread knees
and lands on their toes with subsequent cushioning to prevent
injury. The test was performed with the subject's hands on their
hips. The subject begins in the starting position taking (as
described above).
For each of the two sessions, we conducted a
preliminary stage consisting of heating: i) running at a gentle
pace for approximately 10 min on a treadmill; ii) approximately 5
min of stretching and iii) a test jump. After warm-up standards,
all players performed on a contact-time platform (Ergojump R,
Finland) following the test protocol (32).
Protocol of myofascial treatment
The myofascial treatment protocol included the
execution of the below-described techniques. Each osteopathic
technique was performed on a single point for 90 sec and each
technique performed on a single district was administered only once
during the treatment session (37).
The protocol was performed by a physical therapist with 14 years of
experience in technical manipulation and five years of experience
in osteopathic manipulation. The osteopath was not involved in
measurements and was not aware of the values obtained during
measurements.
Superficial dorsal fascia
The fascia that covers the tendons of the long
extensor muscles, the extensor halluces longus and the anterior
peroneus. The top portion of the fascia follows the annular
ligament (upper and lower retinaculum mm extenders), while the
inner and outer edges of fascia are along the foot and is often
confused with the plantar fascia. At this point of the foot, the
therapist places their fingers. With the patient in a supine
position and with the osteopathic practitioner at the side of the
foot, the therapist places one hand cranially to the retinacula of
the ankle and the other hand is placed caudally around the
metatarsal heads (Fig. 2A).
Pedidia fascia
This portion of the superficial fascia splits to
cover the pedidio muscle, the pedidei vessels and nerve, and the
tibialis anterior. The fascia extends to the outer edge of the foot
and is often confused with the superficial fascia. The points of
origin and insertion are the dorsal surface of the cuboid and the
fifth toe, respectively (Fig. 2B).
With the patient in a supine position, the therapist places one
hand below the ankle and the other hand distal to the site of
articulation with the digits. The therapist then performs a helical
pulling movement.
Deep fascia
This portion of the fascia covers the metatarsal
bones and the interosseous muscles. With the patient in a supine
position, the osteopathic clinician sits at the feet of the patient
and locks the last four digits and mobilizes the first metatarsal
using up-and-down motions as well as flexed-and-extended motions.
The therapist carefully tests the margin of the insertion of the
metatarsal head and follows this procedure with the remaining
digits (Fig. 2C).
Plantar fascia of the foot
This portion of the fascia originates from the
anterior portion of the calcaneal tuberosity and extends to the
metatarsal heads. With the patient in a prone position and a bent
leg, the therapist sits to the side that is to be treated. The
therapist then locks the heel bone and performs traction movements
on the plantar fascia using a spiral motion (Fig. 2D).
Outside fascia anterior leg
This fascia follows the aponeurosis of the thigh and
originates from the tuberosity of the tibia, rhyme under the joint
outside of the tibia to the head of the fibula in his front. At
this level, it receives aponeurotic expansions of some of the thigh
muscles, the biceps femoris, sartorius and semitendinosus. From its
deep surface, they are detached different plates, which compose the
muscle sheaths as well as intermuscular septa front and outer. With
the patient in a supine position, the therapist sits with one hand
below the patellar tendon and the other hand on top of the ankle.
The therapist then performs helical movements (Fig. 2E).
Internal fascia posterior leg
This portion of the fascia originates at the
popliteal fossa, part of the tibia, and extends to the heel pulley.
With the patient in a supine position, the therapist places their
hand cranially to the cable below the popliteal tuberosity of the
tibia. They then place the remaining hand distally to the heel and
pull without bending or stretching the foot (Fig. 2F).
Interosseous membrane of the leg
This portion of the fascia includes the
tibia-peroneal interosseous membrane. It is identifiable by its
course, which appears as two beams that intersect. Beams ankle
peroneal: from top to bottom, from the tibia to the fibula, from
the inside to inward. Beams peroneal tibia: The other at the
bottom, from the fibula to the tibia, from outside to inward. This
portion of the fascia also covers the tibia periosteum where the
medial aspect is appreciable any may indicate possibly dysfunction.
With the patient in a supine position, the therapist palpates the
leg for dense areas. The therapist then runs their hand over these
regions to relax them (Fig. 2G).
Condyle shells
This portion of the fascia includes a thickening of
the capsule at the level of each condyle. Through its peripheral
components, the condyle shells ensures the transverse stability of
the knee. This is particularly evident from the inner side where
the shell goes to be confused with the internal lateral ligament.
With the patient in a supine position, the therapist places their
hands in the popliteal area on the inter-condyle shells. The
therapist then tests for tension using small thrusting motions of
the hands (Fig. 2H).
Front thigh superficial fascia
This portion of the fascia includes the inguinal
ligament and extends to the top margin of the patella. With the
patient in a supine position, the therapist sits by the side of the
limb that requires treatment. The therapist then places one hand
cranially on the inguinal ligament under the anterior superior
iliac spine and another hand distally above the knee. The therapist
then pulls using helical movements (Fig.
2I).
Posterior thigh superficial
fascia
This portion of the fascia originates from an
imaginary line formed between the greater trochanter and the
ischial tuberosity. It is part of the popliteal fossa above the
femoral condyles. With the patient in a supine position, the
therapist places one hand cranially and posteriorly to the
trochanter of the femur and the other hand distally on the
inter-condyle shells. The therapist then performs helical movements
(Fig. 2J).
Fascia lata
With the patient in a supine position and with the
therapist standing opposite the TFL that requires treatment, the
therapist places their hands on the muscle belly starting above the
knee and then pull the muscle upward. With the patient in a supine
position, the osteopathic doctor engages the fascia lata with both
hands from the contralateral side and walk along its length
(Fig. 2K).
Fascia lata
The portion of the fascia lata that covers the
iliopsoas muscle was treated differently. With the patient in a
supine position and with the therapist standing by the side of the
muscle to be treated, the therapist places their hand cranially
past the belly of the iliopsoas muscle, while the distal hand
raises and mobilizes the ipsilateral limb, thereby creating tension
in the muscle layer (Fig. 2L).
Technique ‘unrolling leg fascial’
With the patient in a supine position, the therapist
compresses the limb by pulling the foot while one hand is placed at
the knee to aid in mobilization of the entire limb.
Statistical analysis
We performed an ANOVA (Friedman test), which was
followed by Dunn's multiple comparison test. All data are reported
as the mean ± standard deviation and P<0.05 was considered to
indicate a statistically significant difference. Analyses were
performed using GraphPad Prism v.6.0 for Windows (GraphPad
Software, Inc., La Jolla, CA, USA).
Results
The baseline measurements indicated that the sample
was homogeneous relative to strength with the athletes obtaining
average values of 42.49 and 48.54 cm in the SJ test and in the CMJ,
respectively.
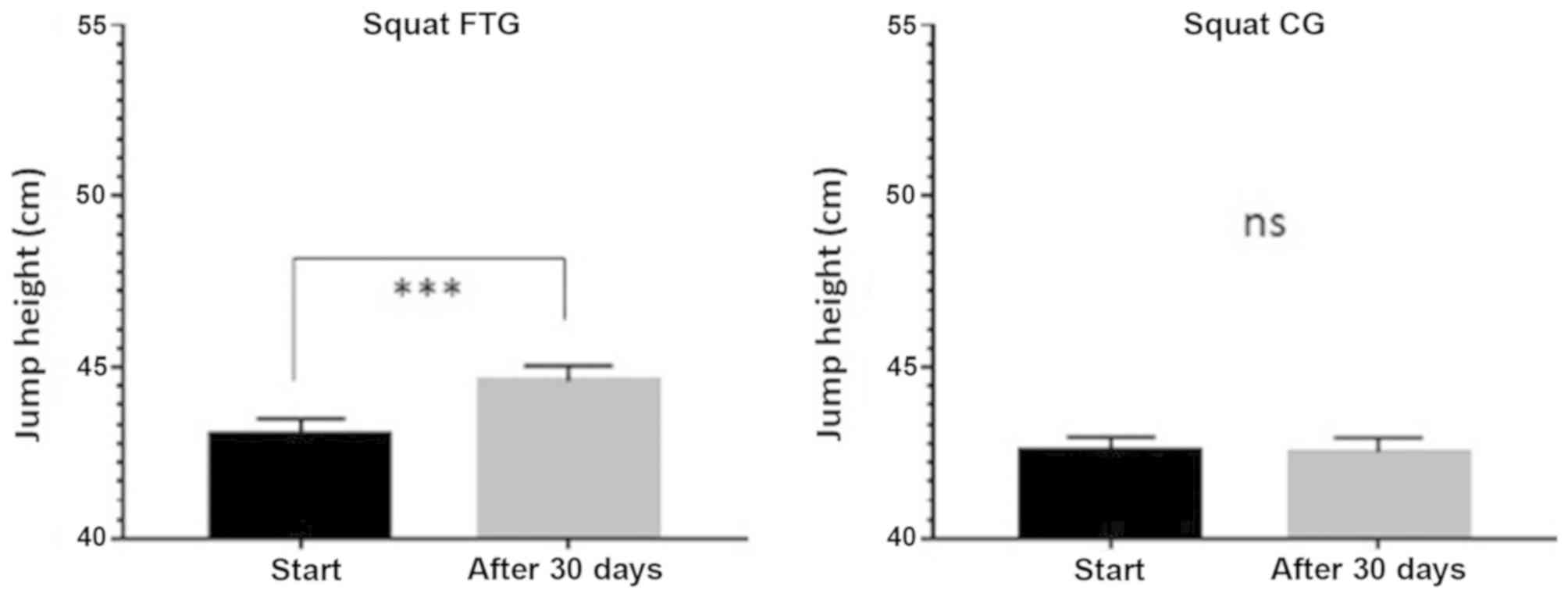
The results obtained during the SJ test are shown in
Fig. 3. The FTG exhibited a
statistically significant improvement in the values obtained before
and after 30 days, with the measurements increasing from 43.08±0.42
cm at baseline to 44.6±0.44 cm after 30 days (P<0.0001).
Conversely, there was no improvement in the CG, with the
measurements increasing from 42.56±0.40 cm at baseline to
42.52±0.41 after 30 days (P<0.56).
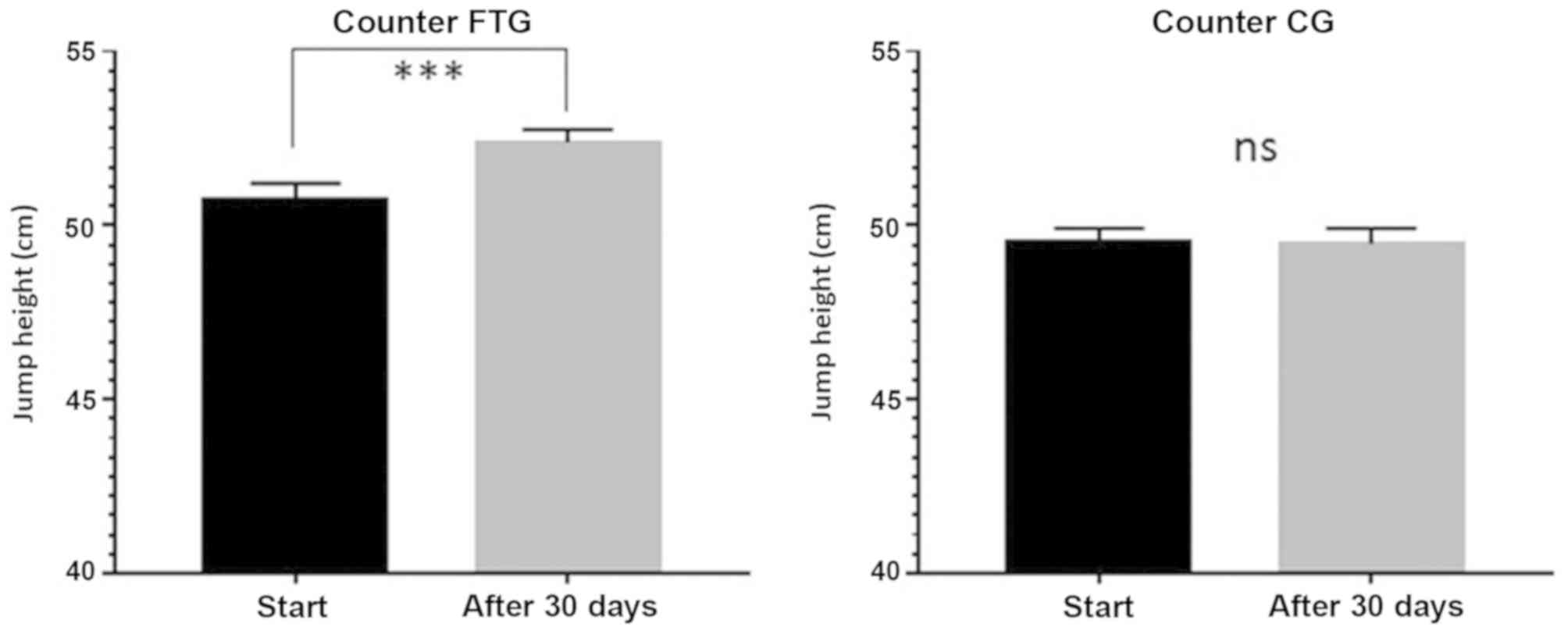
The results obtained in the CMJ test are shown in
Fig. 4. The FTG exhibited a
statistically significant improvement in the values obtained before
and after 30 days, with the measurements increasing from 50.72±0.49
cm at baseline to 52.38±0.37 cm after 30 days (P<0.0001).
Meanwhile, there was no improvement in the CG, with the
measurements increasing from 49.48±0.43 cm at baseline to
49.48±0.44 cm after 30 days (P<0.32).
Discussion
The findings from this research show that that
removing the somatic dysfunction borne by the fascial system of the
lower limbs resulted in an improvement in performance by increasing
the explosive force. These results were in line with the study by
Brown et al (38) as well as
Tozzi et al (39), who
hypothesized that connective tissue has a specific role in both the
generation and transfer of force (40).
From a physiological point of view it could be
suggested the observed improvement in performance could be due, at
least in part, to a significant changes of stiffness of lower
limbs. Stiffness can be defined as ‘the property of a system to
resist an applied stretch’ and can be calculated by dividing the
variation in force by the variation in length (DF/DL) of the system
of interest (41). The concept of
leg-spring stiffness describes an integration of the stiffness of
all structures (muscles, tendons, and ligaments acting across
joints) of lower limb during movement and defines the capability of
those structures to act in unison in a springlike manner (42). The improvements that we observed
indicated that myo-fascial treatment stimulates the fascia, thereby
facilitating the reaction of connection tissue and resulting in
improvements.
Thirty days of treatment led us to hypothesize that
the metabolic activity of the fascia can, over time, restore the
body to optimal biomechanical conditions. We further determined
that correction of the fascial system requires a relatively long
period of time to obtain the best results.
The observed improvement of 2 cm in the measurement
of jump in athletes treated with osteopathic techniques has a
significant clinical relevance as it shows that, with equal
training, the treated group has a better response to the
tone/trophism of lower limbs' musculature.
Osteopathic tests and manipulative techniques
facilitated the troubleshooting and resolution of somatic
dysfunction. It also improved the mechanical function of the
organism. Muscles contract actively to generate force, which they
then transfer by deforming the surrounding connective tissue. This
action influences the application of force by modifying the
magnitude and direction of connective tissue deformation (43–46) and,
therefore, of stiffness. The introduction of a fascial protocol
during athletic training can improve the balance of the bands and,
as a direct result, improve the performance and efficiency of the
musculoskeletal system, thereby reducing the risk of injury. The
strong point of the job is certainly to have put in place a
protocol of techniques that allow to investigate in a sectoral and
specific way the whole fascial system of the lower limb. A weak
point of the work could be the athlete, if you did not perform the
jump properly. In this way, would to may be to perform osteopathic
techniques every two months during an athletic season so as to
maintain the balance of the fascial system and obtain excellent
performance.
The purpose of this study was largely achieved the
sample of volleyball players that has been subjected to osteopathic
treatment of the lower limb muscle groups has shown an improvement
the explosive force of the limbs, while reducing spasms and
tension, releasing tissue strain, and correcting posture. The
strength of the present work is undoubtedly the development of a
detailed and widely reproducible protocol both in term of
techniques and timing. The applicability of this protocol is
twofold: in a clinical field, to recover post-traumatic tissue
damages with residual sore, and in a sports setting to improve
athlete's performances. Future research is required to develop a
new treatment protocol suitable for the upper limbs and trunk.
Acknowledgements
The study was supported and conducted by a
multi-disciplinary team with the collaboration of CSDOI (Centro
Studi Osteopatia Italiano) of Catania, Italy.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AB, CP and CM conceived and designed the
experiments. AB, CP and CM performed the experiments. TR, AB, MCP,
AR, CP, ViP, VaP, DDC and CM analyzed the data. AB and CM wrote the
paper.
Ethics approval and consent to
participate
The paper was approved by the Internal Review Board
of the Research in Psychology at the Kore University of Enna (Enna,
Italy). The subjects signed an informed consent document that was
prepared according to the ethical standards laid down in the
Declaration of Helsinki.
Consent for publication
Written informed consent was provided by all
subjects.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
FTG
|
fascial treatment group
|
|
CG
|
control group
|
|
PFT
|
protocol of osteopathic fascial
techniques
|
|
FT
|
flight time
|
|
SJ
|
squatting jump
|
|
CMJ
|
counter movement jump
|
References
|
1
|
Bordoni B and Zanier E: Skin, fascias, and
scars: Symptoms and systemic connections. J Multidiscip Healthc.
7:11–24. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bordoni B and Zanier E: Cranial nerves
XIII and XIV: Nerves in the shadows. J Multidiscip Healthc.
6:87–91. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Abbott RD, Koptiuch C, Iatridis JC, Howe
AK, Badger GJ and Langevin HM: Stress and matrix-responsive
cytoskeletal remodeling in fibroblasts. J Cell Physiol. 228:50–57.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
van der Wal J: The architecture of the
connective tissue in the musculoskeletal system-an often overlooked
functional parameter as to proprioception in the locomotor
apparatus. Int J Ther Massage Bodywork. 2:9–23. 2009.PubMed/NCBI
|
|
5
|
Stecco A, Gesi M, Stecco C and Stern R:
Fascial components of the myofascial pain syndrome. Curr Pain
Headache Rep. 17:3522013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Buckley CD: Why does chronic inflammation
persist: An unexpected role for fibroblasts. Immunol Lett.
138:12–14. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tozzi P: Selected fascial aspects of
osteopathic practice. J Bodyw Mov Ther. 16:503–519. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Branislav R, Milivoj D, Abella CP, Deval
VC and Siniša K: Effects of combined and classic training on
different isometric rate of force development parameters of leg
extensors in female volleyball players: Discriminative analysis
approach. J Res Med Sci. 18:840–847. 2013.PubMed/NCBI
|
|
9
|
Guimberteau JC, Delage JP, McGrouther DA
and Wong JK: The microvacuolar system: How connective tissue
sliding works. J Hand Surg Eur Vol. 35:614–622. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Turrina A, Martínez-González MA and Stecco
C: The muscular force transmission system: Role of the
intramuscular connective tissue. J Bodyw Mov Ther. 17:95–102. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Purslow PP: Muscle fascia and force
transmission. J Bodyw Mov Ther. 14:411–417. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tozzi P: A unifying neuro-fasciagenic
model of somatic dysfunction-underlying mechanisms and
treatment-part I. J Bodyw Mov Ther. 19:310–326. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tozzi P: A unifying neuro-fasciagenic
model of somatic dysfunction-underlying mechanisms and
treatment-part II. J Bodyw Mov Ther. 19:526–543. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Giacomelli IL, Steidle LJ, Moreira FF,
Meyer IV, Souza RG and Pincelli MP: Hospitalized patients with
COPD: Analysis of prior treatment. J Bras Pneumol. 40:229–237.
2014.(In English, Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Stendardi L, Grazzini M, Gigliotti F,
Lotti P and Scano G: Dyspnea and leg effort during exercise. Respir
Med. 99:933–942. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Savage PA, Shaw AO, Miller MS, VanBuren P,
LeWinter MM, Ades PA and Toth MJ: Effect of resistance training on
physical disability in chronic heart failure. Med Sci Sports Exerc.
43:1379–1386. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Erbs S, Höllriegel R, Linke A, Beck EB,
Adams V, Gielen S, Möbius-Winkler S, Sandri M, Kränkel N, Hambrecht
R and Schuler G: Exercise training in patients with advanced
chronic heart failure (NYHA IIIb) promotes restoration of
peripheral vasomotor function, induction of endogenous
regeneration, and improvement of left ventricular function. Circ
Heart Fail. 3:486–494. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mastaglia FL: The relationship between
muscle pain and fatigue. Neuromuscul Disord. 22 (Suppl
3):S178–S180. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Voelzke M, Stutzig N, Thorhauer HA and
Granacher U: Promoting lower extremity strength in elite volleyball
players: Effects of two combined training methods. J Sci Med Sport.
15:457–462. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Forthomme B, Croisier JL, Ciccarone G,
Crielaard JM and Cloes M: Factors correlated with volleyball spike
velocity. Am J Sport Med. 33:1513–1519. 2005. View Article : Google Scholar
|
|
21
|
Rodriguez-Ruiz D, Quiroga ME, Miralles JA,
Sarmiento S, de Saá Y and García-Manso JM: Study of the technical
and tactical variables determining set win or loss in top-level
European men's volleyball. J Quant Anal Sport. 7:7–15. 2011.
|
|
22
|
Marcelino R, Mesquita I and Afonso J: The
weight of terminal actions in volleyball. Contributions of the
spike, serve and block for the team's rankings in the World League
2005. Int J Perf Anal Sport. 8:1–7. 2008.
|
|
23
|
Fry A, Kraemer WJ, Waseman CA, Conroy BP,
Gordon SE, Hoffman JR and Maresh CM: The effects of an off-season
strength and conditioning program on starters and non-starters in
women's intercollegiate volleyball. J Strength Cond Res. 5:174–181.
1991. View Article : Google Scholar
|
|
24
|
Sheppard JM, Cronin J, Gabbett TJ,
McGuigan MR, Etxebarria N and Newton RU: Relative importance of
strength, power, and anthropometric measures to jump performance of
elite volleyball players. J Strength Cond Res. 22:758–765. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sheppard JM, Gabbett T, Taylor KL, Dorman
J, Lebedew AJ and Borgeaud R: Development of a repeated-effort test
for elite men's volleyball. Int J Sports Physiol Perform.
2:292–304. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sheppard JM and Borgeaud R: Influence of
stature on movement speed and repeated efforts in elite volleyball
players. J Aust Strength Cond. 16:12–24. 2008.
|
|
27
|
Sheppard JM, Dingley AA, Janssen I,
Spratford W, Chapman DW and Newton RU: The effect of assisted
jumping on vertical jump height in high-performance volleyball
players. J Sci Med Sport. 14:85–89. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Newton RU, Kraemer WJ and Häkkinen K:
Effects of ballistic training on preseason preparation of elite
volleyball players. Med Sci Sports Exerc. 31:323–330. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Newton RU, Rogers RA, Volek JS, Häkkinen K
and Kraemer WJ: Four weeks of optimal load ballistic resistance
training at the end of season attenuates declining jump performance
of women volleyball players. J Strength Cond Res. 20:955–961. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Xu Q, Chen B, Wang Y, Wang X, Han D, Ding
D, Zheng Y, Cao Y, Zhan H and Zhou Y: The effectiveness of manual
therapy for relieving pain, stiffness and dysfunction in knee
osteoarthritis: A systematic review and meta-analysis. Pain
Physician. 20:229–243. 2017.PubMed/NCBI
|
|
31
|
Bosco C, Luhtanen P and Komi PV: A simple
method for measurement of mechanical power in jumping. Eur J Appl
Physiol Occup Physiol. 50:273–282. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Komi PV and Bosco C: Utilization of stored
elastic energy in leg extensor muscles by men and women. Med Sci
Sports. 10:261–265. 1978.PubMed/NCBI
|
|
33
|
Baker D: Improving vertical jump
performance through general, special and specific strength
training: A brief review. J Strength Cond Res. 10:131–136. 1996.
View Article : Google Scholar
|
|
34
|
Häkkinen K: Neuromuscular and hormonal
adaptations during strength and power training. A review. J Sports
Med Phys Fitness. 29:9–26. 1989.PubMed/NCBI
|
|
35
|
Lidor R, Hershko Y, Bilkevitz A, Arnon M
and Falk B: Measurement of talent in volleyball: 15-month follow-up
of elite adolescent players. J Sports Med Phys Fitness. 47:159–168.
2007.PubMed/NCBI
|
|
36
|
Marina M, Jemni M and Rodríguez F: Jumping
performance profile of male and female gymnasts. J Sports Med Phys
Fitness. 53:378–386. 2013.PubMed/NCBI
|
|
37
|
Zein-Hammoud M and Standley PR: Modeled
osteopathic manipulative treatments: A review of their in vitro
effects on fibroblast tissue preparations. J Am Osteopath Assoc.
115:490–502. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Brown SH, Carr JA, Ward SR and Lieber RL:
Passive mechanical properties of rat abdominal wall muscles suggest
an important role of the extracellular connective tissue matrix. J
Orthop Res. 30:1321–1326. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Tozzi P, Bongiorno D and Vitturini C: Low
back pain and kidney mobility: Local osteopathic fascial
manipulation decreases pain perception and improves renal mobility.
J Bodyw Mov Ther. 16:381–391. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ćosić V, Day JA, Iogna P and Stecco A:
Fascial manipulation(®) method applied to pubescent
postural hyperkyphosis: A pilot study. J Bodyw Mov Ther.
18:608–615. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Saez Saez de Villarreal E,
González-Badillo JJ and Izquierdo M: Optimal warm-up stimuli of
muscle activation to enhance short and long-term acute jumping
performance. Eur J Appl Physiol. 100:393–401. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Grange RW, Cory CR, Vandenboom R and
Houston ME: Myosin phosphorylation augments force-displacement and
force-velocity relationships of mouse fast muscle. Am J Physiol.
269:C713–C724. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Allen SH: Primary osteoporosis. Methods to
combat bone loss that accompanies aging. Postgrad Med. 93:43–46,
49-50, 53–55. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Willard FH, Vleeming A, Schuenke MD,
Danneels L and Schleip R: The thoracolumbar fascia: Anatomy,
function and clinical considerations. J Anat. 221:507–536. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Lunghi C, Tozzi P and Fusco G: The
biomechanical model in manual therapy: Is there an ongoing crisis
or just the need to revise the underlying concept and application?
J Bodyw Mov Ther. 20:784–799. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Klingler W, Velders M, Hoppe K, Pedro M
and Schleip R: Clinical relevance of fascial tissue and
dysfunctions. Curr Pain Headache Rep. 18:4392014. View Article : Google Scholar : PubMed/NCBI
|