Introduction
Osteoarticular tuberculosis (OAT) may cause
significant morbidity and disability if not treated properly. OAT
is frequently difficult to diagnose in the early stage due to the
absence of typical systematic symptoms, physical signs, blood
parameters and radiographic indications (1). Conventional Mycobacterium
tuberculosis (MTB) culture is a gold standard for diagnosis,
but it has a relatively low sensitivity and is time-consuming
(2). Polymerase chain reaction
(PCR)-based genetic analyses are effective for rapidly diagnosing
OAT. However, these methods specifically detect MTB sequences and
are incapable of excluding mixed bacterial and fungal infections
that commonly occur in OAT patients as a result of low immunity and
invasive procedures (3).
Metagenomic next-generation sequencing (mNGS) is a
novel technique for the clinical diagnosis of infectious diseases.
mNGS may accurately detect MTB in sputum specimens from patients
with suspected pulmonary tuberculosis (4). Its ability to identify multiple
pathogens using a single detection method demonstrates its great
potential for uncovering mixed infection. To date, no study has
described the diagnosis of OAT using the mNGS method.
The present study reports on a case of non-specific
progressive swelling and pain in the knee, which was diagnosed as
OAT using mNGS. After surgical treatment and chemotherapy, the
patient demonstrated functional recovery.
Case report
A 64-year-old male presented at the outpatient
department of the First Affiliated Hospital of Fujian Medical
University (Fuzhou, China) in October 2017 with a history of
repeated progressive swelling and pain in the right knee for 1
year. The pain was usually exacerbated after movement. The patient
exhibited other symptoms, including fever or walking instability.
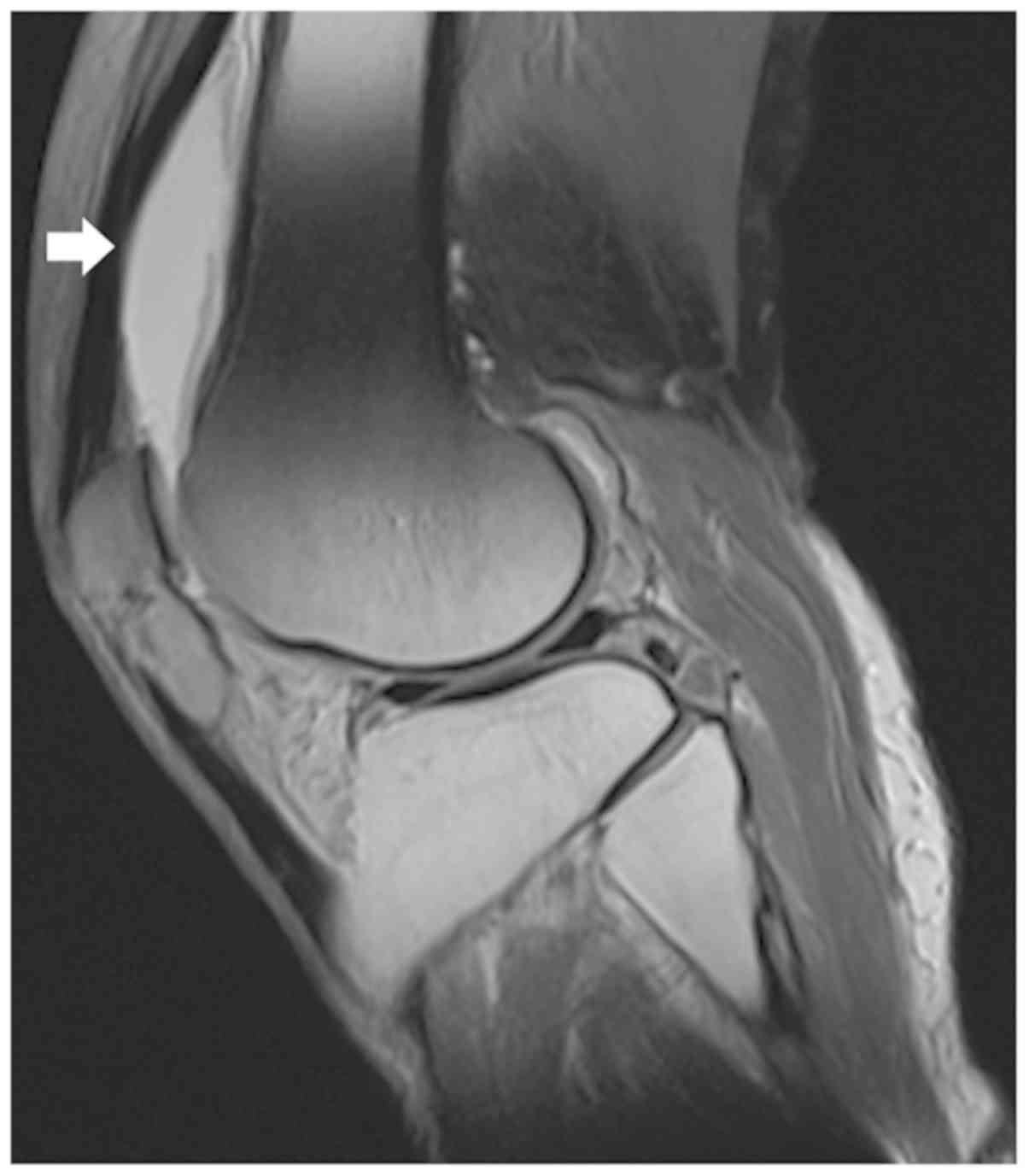
Magnetic resonance imaging scans performed at a local hospital
indicated effusion of the suprapatellar bursa and based on this,
early osteoarthritis was suspected (Fig.
1). Multiple knee aspirations and injections, as well as
anti-microbial therapy, which were performed at a local clinic
(specific details unknown), were ineffective.
The patient's medical history included a right
patella fracture due to a falling accident two years previously.
Good union of the bone was achieved and function of the joint as
regained by the application of a knee brace for 3 months. The
patient denied multiple sexual partners or any recent travel to
endemic areas.
On physical examination, right knee swelling was
noted, with no redness of the local skin or elevated skin
temperature. The patella floating test was positive. The anterior
and posterior drawer tests and the McMurray test were negative. The
range of motion of the knee was restricted to 0–90 degrees. The
right quadriceps muscle exhibited mild atrophy, while lower
extremity limb muscle strength and sensations were normal.
Routine blood and coagulation test results, as well
as liver and kidney function, were normal. Tests for rheumatoid
factor, anti-keratin antibody and anti-cyclic citrullinated peptide
were all negative. The patient's C-reactive protein (CRP) level was
elevated (62.10 mg/l) and the erythrocyte sedimentation rate (ESR)
was 31 mm/h. A T-SPOT.TB assay (Oxford Immunotec) was positive with
the following results: 86/250,000 peripheral blood mononuclear
cells (PBMCs) expressing ESAT-6 (antigen A) and 89/250,000 PBMCs
expressing CFP-10 (antigen B).
A CT scan of the lung was normal. Anterior and
lateral plain images of the right knee indicated that the
tibiofemoral joint space of the right knee was intact and contained
a small number of osteophytes (Fig.
2). Aspiration of the right knee yielded 10 ml red, cloudy
synovial fluid. No uric acid crystals were visible under a
polarizing microscope. The white blood cell (WBC) count of the
synovial fluid was 5895.00 106/l, with 55.4%
polymorphonuclear cells. Acid-fast staining, as well as bacterial
and fungal cultures, were negative, and a rapid MTB culture using
the BACTEC-MGIT960 system (BD Biosciences) was negative within 2
weeks.
At this time-point, the patient's serum CRP levels,
ESR, synovial WBC count and polymorphonuclear cell percentage were
all markedly elevated, and no extra-articular symptoms were
observed. Immune disease indicators were negative; therefore, it
was highly suspected that the patient had a right knee joint
infection. While the cultures were negative, no low-virulence,
difficult-to-grow bacteria or atypical pathogens (mycoplasma, MTB
or nontuberculous mycobacteria) were excluded.
Therefore, the 16s ribosomal (r)RNA PCR method was
used to detect pathogenic microorganisms (5). Ceramic beads were added to 200 µl
synovial fluid to lyse the cell walls. Total DNA was extracted
using the TIANAMP Micro DNA kit (cat. no. DP316; Tiangen Biotech)
following the manufacturer's protocol. Primers targeting the V3-V4
region of 16S rRNA (forward, 5′-CGGCCCAGACTCCTACGGGAGGCAGCA-3′ and
reverse, 5′-GCGTGGACTACCAGGGTATCTAATCC-3′) were used. Real-time PCR
was performed on an ABI 7500 instrument (Applied Biosystems; Thermo
Fisher Scientific, Inc.) using the Takara SYBR Premix Ex Taq kit
(Takara Bio, Inc.). No positive results were detected.
The patient was admitted for open surgery to perform
aggressive debridement (6), during
which adequate tissue samples for microbiological identification
were obtained. The medial parapatellar approach was utilized.
Except for a small cartilage defect on the patella due to a
previous fracture, the surface of the tibiofemoral joint was
smooth. The cruciate ligaments were intact. Extensive swelling and
hyperplastic synovium were observed. The affected synovium was
resected extensively. The synovial fluid and resected synovial
tissue were transported to the laboratory within 30 min for further
pathological and microbiological examination.
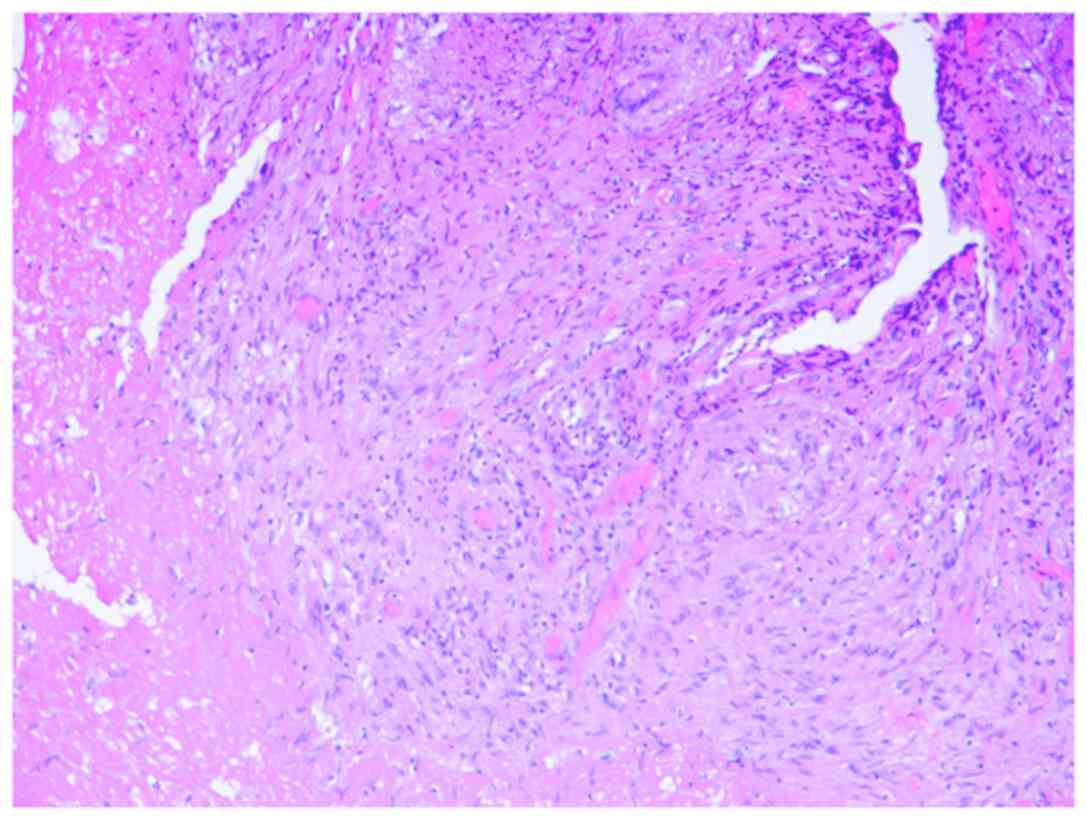
Tissue samples were fixed in 10% neutral formalin
for 8–48 h, dehydrated by 75, 95 and 100% ethanol, embedded in
paraffin and sliced into 4-µm-thick sections. The samples were
stained with hematoxylin for 5–10 min and eosin for 1–3 min at the
room temperature. The sections were observed using an optical
microscope at a magnification of ×300. Histopathological
examination with hematoxylin and eosin revealed an inflammatory
reaction, including massive granuloma with central necrosis,
lymphocytic infiltration, and a small amount of neutrophil
infiltration (Fig. 3). Bacterial and
fungal cultures provided negative results after culturing for 2
weeks.
The mNGS process was utilized to clarify the
pathogenic source. DNA was extracted from synovial fluid collected
intra-operatively through the above-mentioned method. The extracted
DNA was sonicated to generate 200–300 bp fragments. DNA libraries
were constructed according to the standard protocol of the
BGISEQ-500 sequencing platform (BGI-Tianjin). The quantified
libraries were sequenced with the BGISEQ-500 platform.
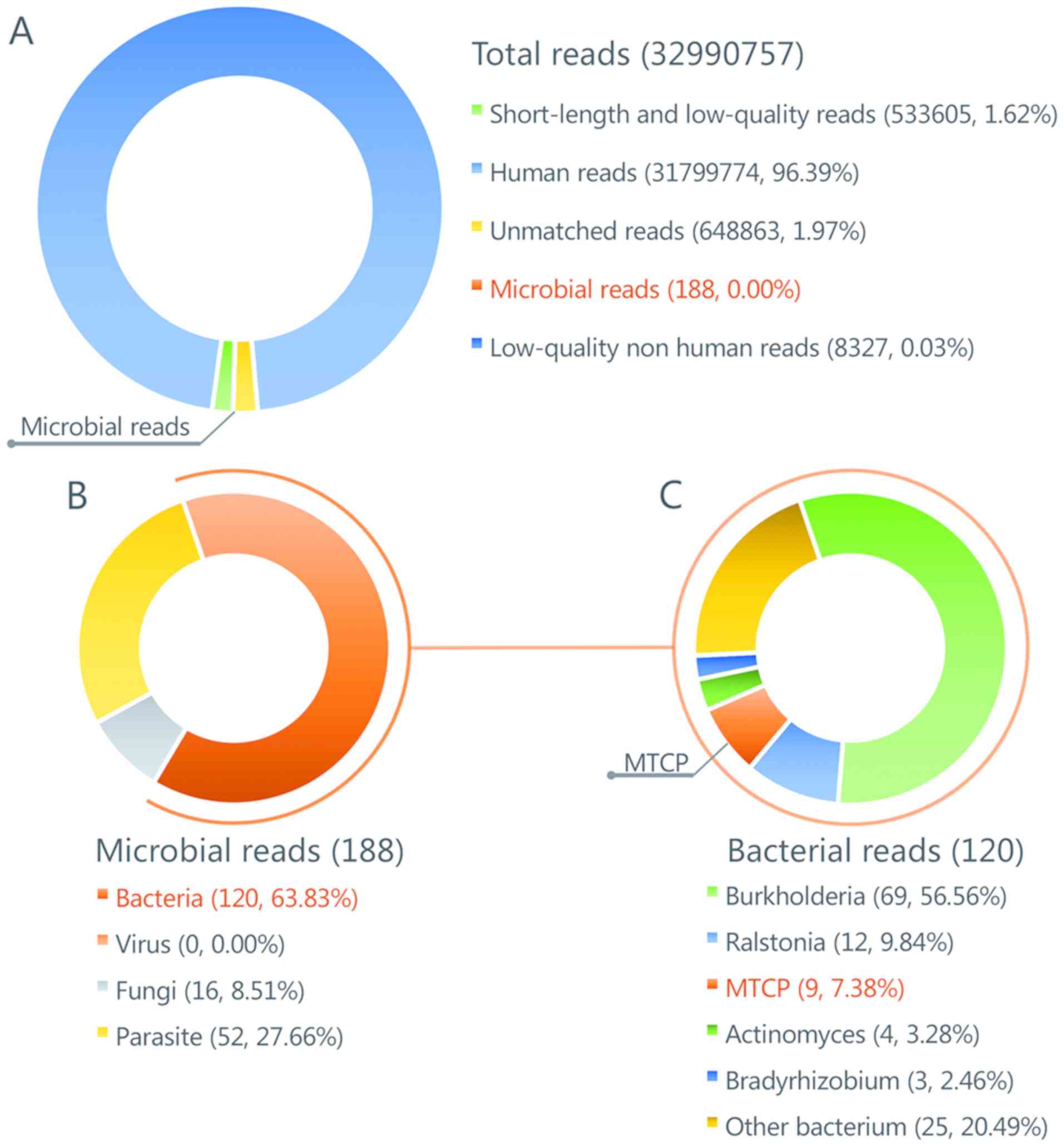
The raw sequencing data were analyzed by a
Bioinformatics pipeline developed by BGI that included the
following steps: i) Clean reads of high-quality sequencing data
were generated by filtering out the short, low-quality and
low-complexity reads. ii) Human host sequences were eliminated by
mapping to the human reference genome (hg19) with Burrows-Wheeler
alignment (http://bio-bwa.sourceforge.net). iii) The remaining
sequencing data were aligned to the Microbial Genome Database (an
in-house database built by BGI, with no plan to publish publicly),
which contains the genomic sequences of 2,700 viruses, 1,494
bacteria, 73 fungi and 48 parasites that are all associated with
human diseases. The reference genomes in the database were
downloaded from the National Center for Biotechnology Information
(https://www.ncbi.nlm.nih.gov/).
The number of microbial reads was 260 (0.000801% of
total clean reads). Burkholderia accounted for the highest number
of microbial reads with 31 (11.92% of the total microbial reads).
This species was observed to be the most common contaminant
according to this sequencing method (data not shown). A total of 6
unique reads (2.31% of the total microbial reads) of the
Mycobacterium tuberculosis complex group (MTCP) were
obtained (Fig. 4). As this had never
been validated as a contaminant in previous experiments and
analyses in the same lab during past 3 months, MTCP was regarded as
the pathogenic organism.
To verify the mNGS test results, the intra-operative
synovial fluid was examined using a variety of validated molecular
diagnostic methods for detecting MTB. i) The results of nested PCR
targeting the IS6110 gene were positive. ii) PCR and hybridization
using the MTB Drug Resistance Detection Array kit (CapitalBio)
indicated no rpoB, katG or inhA mutations, indicating that the
strain is sensitive to rifampicin and isoniazid. iii) Results of
the GeneXpert MTB/RIF test (Cepheid) suggested the presence of MTB
and no resistance to rifampin.
Due to the consistent results of several different
molecular diagnostic methods, the patient was finally diagnosed
with right knee tuberculosis. Anti-tuberculosis treatments included
isoniazid, rifampicin, ethambutol and pyrazinamide, which were
started immediately after the surgery. The patient's incision site
healed within 2 weeks of surgery.
MTB culture of synovial fluid and periprosthetic
tissues on modified Lowenstein-Jensen medium were positive for
tuberculosis at 5 weeks post-operatively. Drug resistance tests
indicated that the strain was sensitive to isoniazid, rifampicin
and ethambutol, but resistant to streptomycin. During the 3 months
of follow-up, the patient reported no fever and fatigue, no
swelling or pain in his knee, and being able to walk without a
cane. The patient's ESR and CRP values returned normal. The patient
is presently undergoing oral anti-tuberculosis chemotherapy,
including isoniazid, rifampicin, ethambutol and pyrazinamide. Until
now, no signs of recurrence of infection have been noted.
Discussion
Approximately 2.2–4.7% of tuberculosis cases affect
the bone and joint systems and are referred to as OAT (7,8). OAT
most frequently occurs in the spine, followed by the knee, hip and
elbow. If not treated properly, OAT may lead to limb and spine
deformities, spinal cord compression and even irreversible
disability (1,2). Early OAT is frequently localized and
may be successfully treated by anti-tuberculosis chemotherapy.
However, OAT is difficult to diagnose in its early stage due to its
lack of acute manifestations of infection. Early OAT is difficult
to differentiate from bacterial or non-tuberculosis mycobacterial
infections, immunological arthritis or spondylitis, and even
degenerative diseases (8). Due to
this difficulty, the treatment is frequently delayed, leading to
poor outcomes. Although MTB culture remains the ‘gold standard’ for
diagnosing OAT, existing methods have numerous drawbacks, including
long culture times (3–8 weeks) and low sensitivity (30–40%)
(9,10).
Molecular diagnostic methods have been applied to
improve the diagnosis of OAT. Primers or probes targeting specific
genes or drug resistance-associated genes of MTB are used for PCR
detection, including fluorescent probe quantitative PCR, GeneXpert
MTB/RIF, loop-mediated isothermal amplification and microarrays.
These methods have advantages over culture, including higher
sensitivity, faster detection and the ability to detect drug
resistance spontaneously. However, the currently available
commercial kits are unable to identify non-MTB bacteria or other
atypical pathogens simultaneously. Clinically, mixed infection is
common in tuberculosis patients due to compromised immunity and
side effects of injections or surgery. Traditional
anti-tuberculosis chemotherapy drugs are frequently ineffective
against bacterial infections, which may lead to failure of
treatment (11–14).
Use of the mNGS method to detect pathogens in
clinical samples has been applied for the diagnosis of meningitis,
bacteremia and orthopedic implant-associated infections (15–17).
Using high-throughput sequencing and subsequent Bioinformatics
processing, mNGS may simultaneously align thousands of sequences of
pathogenic microorganisms, including bacteria, fungi, mycoplasma
and even parasites, to obtain unbiased information on the species
and abundance of all microorganisms in the sample. The mNGS method
has been demonstrated to accurately detect MTB in sputum specimens
from patients with suspected pulmonary tuberculosis (12). However, few studies have described
the diagnosis of OAT using mNGS.
In the present case, MTCP was identified by mNGS of
synovial fluid. The result was successfully verified by other
methods, including culture and PCR. The patient's symptoms were
relieved through surgery and chemotherapy, and inflammatory
biomarker levels returned to normal, which confirmed the
diagnosis.
mNGS is a type of sequencing with no preferences and
allows for identification of microorganisms in an unbiased manner.
The ability of mNGS to identify multiple pathogens with a single
detection method has great potential for uncovering mixed
infections. The case of the present study received multiple
intra-articular injections and therefore had a risk of exogenous
infection. The mNGS results did not indicate the presence of other
pathogenic microorganisms after excluding common background
microorganisms during mNGS procedures (e.g., Burkholderia,
Ralstonia, Actinomyces and Bradyrhizobium) (18,19).
Consequently, only anti-tuberculosis drugs were prescribed. To
date, no signs of recurrence of infection have been noted, which
further verifies the mNGS result. The present study demonstrated
the superiority of mNGS over other molecular diagnostic methods
(17).
In the present study, the number of reads uniquely
aligned to the reference genome of MTCP was insufficient;
therefore, it was impossible to differentiate MTB from MTCP to
obtain resistance-associated information. This may be due to the
small amount of nucleic acid extracted from the MTB in the
specimen. The major causes of this effect may be the low burden of
planktonic bacteria in the synovial fluid, difficulty in lysing the
tenacious cell wall of MTB and interference of overwhelming host
sequences during sequencing. More robust and comprehensive lysis,
removal of human DNA (18) and
utilization of a single-cell whole-genome analysis method may be
adopted to fix these issues (20).
In conclusion, the present case study reported on a
patient with inflammatory pain and swelling of the knee. Using
mNGS, the presence of MTB was detected and mixed infection was
excluded. Culture, specific PCR and GeneXpert MTB/RIF were used to
verify the results. The patient's symptoms were relieved through
surgical treatment and chemotherapy, and functional recovery was
observed. The successful course of diagnosis in the present case
indicates that mNGS has great potential for diagnosing OAT and
excluding mixed bacterial infection in a single assay. This method
provides strong support to guide physicians in selecting the
appropriate pharmacotherapy and surgical treatment.
Acknowledgements
Not applicable.
Funding
The current study was supported by the Fujian
Education and Scientific Research Projects for Young Teachers
(grant no. JAT170241), the National Science Foundation for Young
Scientists of China (grant no. 81702168), and the Natural Science
Foundation of Fujian Province (grant nos. 2018I0006 and
2018Y4003).
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZH and ChoZ analyzed and interpreted the data, wrote
the manuscript and organized the figures. QijW and ML performed the
16 s ribosome RNA gene polymerase chain reaction analysis. QiqW,
DH, KS and WL performed the surgery. BY performed the microbial
culture. ChaZ and WZ designed the study, edited and reviewed the
manuscript, and approved the version to be published. XL, LH and NX
performed the metagenomic next-generation sequencing. All authors
reviewed the final version of the manuscript.
Ethics approval and consent to
participate
This study was approved by the Institutional Review
Board of the First Affiliated Hospital of Fujian Medical University
(Fuzhou, China; process no. 2014-047).
Patient consent for publication
Informed consent for publication of data and images
was obtained from the patient included in the study.
Competing interest
The authors have no competing interests to
declare.
References
|
1
|
Pigrau-Serrallach C and Rodríguez-Pardo D:
Bone and joint tuberculosis. Eur Spine J. 22 (Suppl 4):S556–S566.
2013. View Article : Google Scholar
|
|
2
|
Magnussen A, Dinneen A and Ramesh P:
Osteoarticular tuberculosis: Increasing incidence of a difficult
clinical diagnosis. Br J Gen Pract. 63:385–386. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tarashi S, Fateh A, Mirsaeidi M, Siadat SD
and Vaziri F: Mixed infections in tuberculosis: The missing part in
a puzzle. Tuberculosis (Edinb). 107:168–174. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Brown AC, Bryant JM, Einer-Jensen K,
Holdstock J, Houniet DT, Chan JZ, Depledge DP, Nikolayevskyy V,
Broda A, Stone MJ, et al: Rapid whole-genome sequencing of
mycobacterium tuberculosis isolates directly from clinical
samples. J Clin Microbiol. 53:2230–2237. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Huang Z, Wu Q, Fang X, Li W, Zhang C, Zeng
H, Wang Q, Lin J and Zhang W: Comparison of culture and broad-range
polymerase chain reaction methods for diagnosing periprosthetic
joint infection: Analysis of joint fluid, periprosthetic tissue,
and sonicated fluid. Int Orthop. 42:2035–2040. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bovonratwet P, Nelson SJ, Bellamkonda K,
Ondeck NT, Shultz BN, Medvecky MJ and Grauer JN: Similar 30-day
complications for septic knee arthritis treated with arthrotomy or
arthroscopy: An American college of surgeons National surgical
quality improvement program analysis. Arthroscopy. 34:213–219.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Global tuberculosis report 2017, . World
Health Organization; Geneva: 2017, simplefile:///Users/e.kouneni/Downloads/9789241565516-eng.pdfFebruary
11–2019
|
|
8
|
García-Elorriaga G, Martínez-Elizondo O,
Del Rey-Pineda G and González-Bonilla C: Clinical, radiological and
molecular diagnosis correlation in serum samples from patients with
osteoarticular tuberculosis. Asian Pac J Trop Biomed. 4:581–585.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lakhanpal VP, Tuli SM, Singh H and Sen PC:
The value of histology, culture and guinea pig inoculation
examination in osteo-articular tuberculosis. Acta Orthop Scand.
45:36–42. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen ST, Zhao LP, Dong WJ, Gu YT, Li YX,
Dong LL, Ma YF, Qin SB and Huang HR: The clinical features and
bacteriological characterizations of bone and joint tuberculosis in
China. Sci Rep. 5:110842015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pérez-Osorio AC, Boyle DS, Ingham ZK,
Ostash A, Gautom RK, Colombel C, Houze Y and Leader BT: Rapid
identification of mycobacteria and drug-resistant mycobacterium
tuberculosis by use of a single multiplex PCR and DNA
sequencing. J Clin Microbiol. 50:326–336. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
N'guessan K, Horo K, Coulibaly I, Adegbele
J, Kouame-Adjei N, Seck-Angu H, Guei A, Kouakou J and Dosso M:
Rapid detection of mycobacterium tuberculosis complex in
sputum samples using PURE TB-LAMP assay. Int J Mycobacteriol. 5
(Suppl 1):S164–S165. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bojang AL, Mendy FS, Tientcheu LD, Otu J,
Antonio M, Kampmann B, Agbla S and Sutherland JS: Comparison of
TB-LAMP, GeneXpert MTB/RIF and culture for diagnosis of pulmonary
tuberculosis in The Gambia. J Infect. 72:332–337. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cheng XH, Bian SN, Zhang YQ, Zhang LF, Shi
XC, Yang B, Zhang FC and Liu XQ: Diagnostic value of t-cell
interferon-γ release assays on synovial fluid for articular
tuberculosis: A pilot study. Chin Med J (Engl). 129:1171–1178.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Grumaz S, Stevens P, Grumaz C, Decker SO,
Weigand MA, Hofer S, Brenner T, von Haeseler A and Sohn K:
Next-generation sequencing diagnostics of bacteremia in septic
patients. Genome Med. 8:732016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Guan H, Shen A, Lv X, Yang X, Ren H, Zhao
Y, Zhang Y, Gong Y, Ni P, Wu H, et al: Detection of virus in CSF
from the cases with meningoencephalitis by next-generation
sequencing. J Neurovirol. 22:240–245. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lecuit M and Eloit M: The diagnosis of
infectious diseases by whole genome next generation sequencing: A
new era is opening. Front Cell Infect Microbiol. 4:252014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bukowska-Ośko I, Perlejewski K, Nakamura
S, Motooka D, Stokowy T, Kosińska J, Popiel M, Płoski R, Horban A,
Lipowski D, et al: Sensitivity of next-generation sequencing
metagenomic analysis for detection of RNA and DNA viruses in
cerebrospinal fluid: The confounding effect of background
contamination. Adv Exp Med Biol. 13–Jul;2016.(Epub ahead of print).
View Article : Google Scholar
|
|
19
|
Salter SJ, Cox MJ, Turek EM, Calus ST,
Cookson WO, Moffatt MF, Turner P, Parkhill J, Loman NJ and Walker
AW: Reagent and laboratory contamination can critically impact
sequence-based microbiome analyses. BMC Biol. 12:872014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang L, Ma F, Chapman A, Lu S and Xie XS:
Single-cell whole-genome amplification and sequencing: Methodology
and applications. Annu Rev Genomics Hum Genet. 16:79–102. 2015.
View Article : Google Scholar : PubMed/NCBI
|