Introduction
Fetal hydronephrosis (HY), a type of fetal
malformation, is a common congenital condition (1). It may be determined by prenatal
ultrasound and is characterized by abnormal dilatation of renal
pelvis and calyces, as well as atrophy in renal parenchyma
(2,3). The incidence rate of HY among all
newborns detected by ultrasound is 0.6–5.4% (4). HY is more frequently diagnosed in
fetuses of male gender and those in a unilateral position (5). Studies have demonstrated that
vesicoureteral reflux and tract obstruction, particularly at the
ureteropelvic junction, are the leading causes of HY, while HY
caused by duplex renal system or hydroureteronephrosis is rare
(6,7). HY may be divided into physiological and
pathological types based on the post-partum conditions. HY that may
spontaneously resolve after birth is classified as physiological
HY, while the type that deteriorates and may lead to impaired renal
function is referred to as pathological HY (8).
At present, fetal HY is mainly diagnosed based on
prenatal ultrasound (9). The rate of
clinical detection of HY has been increasing due to the development
of ultrasonic technology and optimization of ultrasonic instruments
(10). However, a dilemma is
emerging with regard to the management of infants diagnosed with
fetal HY (11,12). Society for Fetal Urology (SFU)
grading and anterior-posterior diameter (APD) measurement are two
major ultrasonography-based systems to evaluate HY. The SFU system
consists of five grades (0, I, II, III and IV) according to the
appearance of calices, pelvis and thinning of parenchyma (13). The APD system contains three grades
(mild, moderate and severe) based on the anterior/posterior
diameter of the pelvis (14). The
severity of HY evaluated by ultrasound is closely associated with
the prognosis of the affected pediatric patients. Thus, precise
determination of HY grading is critical for optimal management.
To further investigate the diagnosis and achieve
appropriate management of fetal HY, the present study focused on
the predictive value of the SFU and APD grading systems regarding
the post-partum outcome, and explored their associations with
spontaneous regression of HY and requirement of surgery.
Materials and methods
Subjects
The present study retrospectively analyzed the
ultrasonic data and clinical characteristics of 162 pregnant
females who received antenatal examination and gave birth at the
Second Affiliated Hospital of Wenzhou Medical University (Wenzhou,
China) between January 2014 and December 2017. All of these
subjects fulfilled the inclusion criteria: Singleton pregnancy;
detection of fetal HY by ultrasound; no fetal malformation except
HY; no consanguineous marriage; couples had no genetic disease.
Prenatal ultrasound of these pregnant females at 20–40 gestational
weeks identified 234 fetal kidneys affected by HY, including 72
cases of bilateral HY and 90 of unilateral HY. The protocols of the
present study were approved by the Ethics Committee of the Second
Affiliated Hospital of Wenzhou Medical University (Wenzhou, China)
and written informed consent for the use of ultrasonic data and
clinical characteristics was obtained from each participant.
Imaging
All of the pregnant females underwent assessment of
fetal HY by ultrasonography with an ESAOTE Technos MYLAB 65
(Esaote) every 2–4 weeks prior to delivery. The neonates were
re-examined by ultrasound at 7 days after delivery. The cases still
exhibiting HY were followed up for 12 months, and those patients
with persistent or progressive HY were further diagnosed by other
adjuvant examinations, including intravenous pyelography (IVP),
emission computed tomography (ECT) and magnetic resonance urography
(MRU). An X-ray machine (Siemens AG, Munich, Germany) was used for
IVP, a CT scanner (Siemens AG) was used for ECT, and a nuclear
magnetic resonance detector (Philips NV, Amsterdam, Netherlands)
was used for MRU examination. HY that spontaneously resolves after
birth is referred to as physiological HY, while the type that
becomes deteriorative and may lead to impaired renal function is
called pathological HY. During the follow-up survey, the HY
outcomes and rate of surgery were recorded for further analysis.
The patients were graded using the SFU and APD systems based on
their ultrasound images (15). The
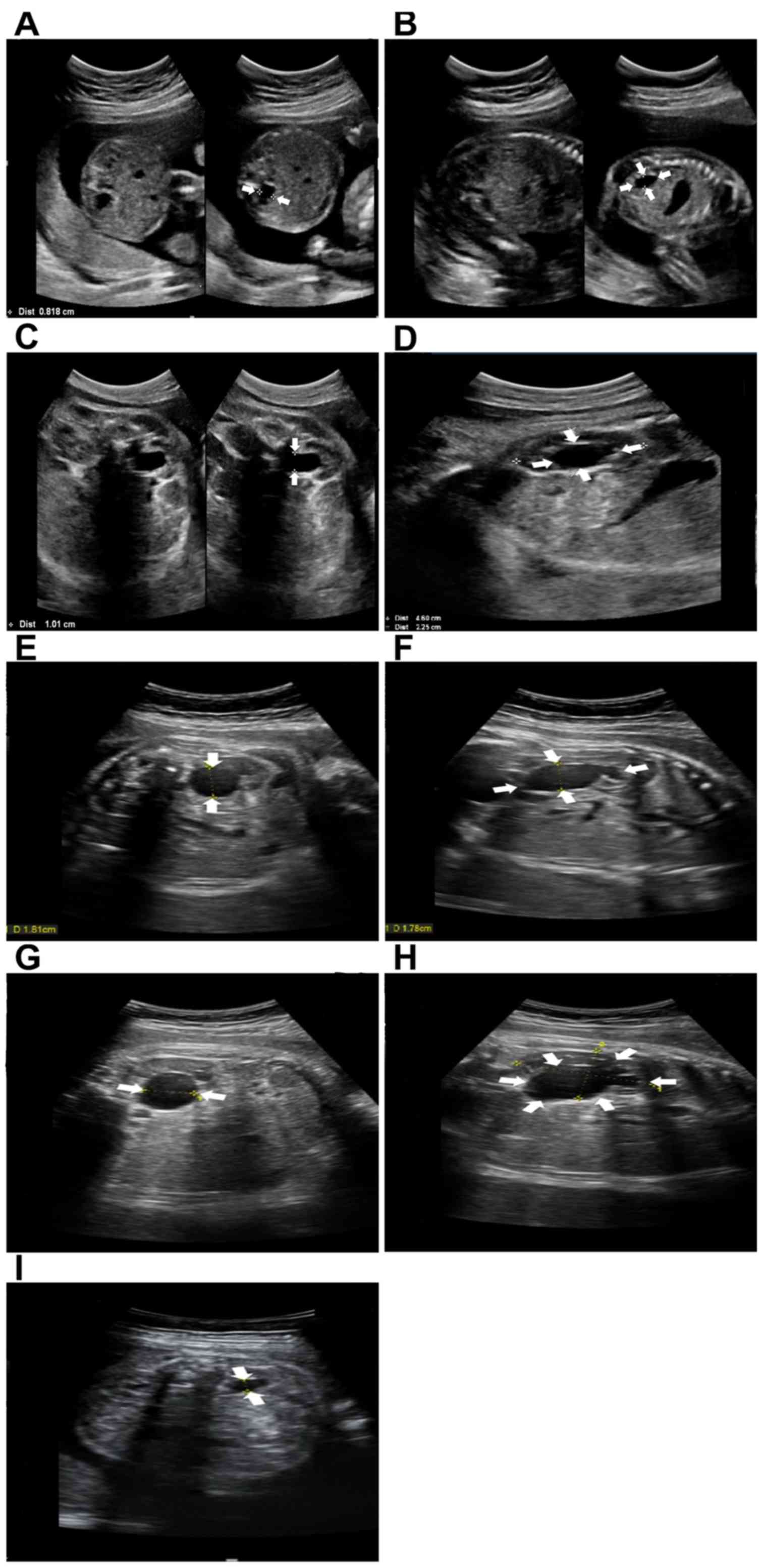
classifications of these two systems are listed in Table I and representative ultrasound images
are provided in Fig. 1.
 | Table I.Classification criteria of SFU and APD
grading systems. |
Table I.
Classification criteria of SFU and APD
grading systems.
| A, SFU grading
system |
|---|
| Grade | Characteristics |
|---|
| 0 | No
hydronephrosis |
| I | Renal pelvis is
slightly separated |
| II | Renal pelvis is
further separated and a single or a few dilated calices may be
visualized |
| III | All calices are
dilated |
| IV | All calices are
dilated and the renal parenchyma over the calices is thinned |
|
| B, APD grading
system |
|
| Grade | Time window/APD
(mm) |
|
| Mild | Second trimester: 4
< APD < 7 |
|
| Third trimester: 7
< APD < 9 |
| Moderate | Second trimester: 7
< APD < 10 |
|
| Third trimester: 9
< APD < 15 |
| Severe | Second trimester: APD
> 10 |
|
| Third trimester: APD
> 15 |
Statistical analysis
All the statistical analyses were performed using
SPSS 20.0 software (IBM Corp.). Continuous variables are expressed
as the mean ± standard deviation. The association between SFU or
APD grades and the clinical characteristics of the patients was
assessed using the Chi-squared test. Univariate and multivariate
logistic regression analysis was performed to examine the
association of clinicopathological parameters, as well as SFU or
APD grading, with the postpartum outcomes, HY regression and
post-partum surgery for fetal HY. Receiver operating characteristic
(ROC) curve analysis was performed to evaluate the predictive value
of SFU and APD grading systems, and the sensitivity and specificity
to distinguish pathological and physiological HY was determined.
The Kaplan-Meier method was applied to analyze the rate of surgery
among the patients with pathological HY and different SFU and APD
grades, and log-rank test was adopted to compare the differences
between curves. P<0.05 was considered to indicate statistical
significance.
Results
Characteristics of the patients and
grading results
The characteristics of the patients are summarized
in Table II. According to the
prenatal ultrasound, a total of 234 kidneys were affected by fetal
HY, including 60 cases with the left and 30 cases with the right
kidney affected, as well as 72 cases with bilateral involvement.
According to the post-partum examination, 217 kidneys (92.7%;
n=146) had physiological HY and 17 kidneys (7.3%; n=16) had
pathological HY.
 | Table II.Characteristics and grading results of
the HY patients. |
Table II.
Characteristics and grading results of
the HY patients.
| Parameters | Nο. of patients (%)
or mean ± SD (range) | Nο. of kidneys
(%) |
|---|
| Gender |
|
Female | 64 (39.5) | 91 (38.9) |
| Male | 98 (60.5) | 143 (61.1) |
| Affected side |
| Left | 60 (37.0) | 60 (25.6) |
|
Right | 30 (18.5) | 30 (12.8) |
|
Bilateral | 72 (44.4) | 144 (61.5) |
| Maternal age
(years) | 29.8±5.2 (20–41) |
|
| Post-partum
outcome |
|
Physiological HY | 146 (90.1) | 217 (92.7) |
|
Pathological HY | 16 (9.9) | 17 (7.3) |
| SFU grade |
| I | 111 (68.5) | 161 (68.8) |
| II | 36 (22.2) | 57 (2.4) |
|
III | 7 (4.3) | 7 (3.0) |
| IV | 8 (4.9) | 9 (3.8) |
| APD grade |
|
Mild | 72 (44.4) | 112 (47.9) |
|
Moderate | 73 (45.1) | 104 (44.4) |
|
Severe | 17 (10.5) | 18 (7.7) |
SFU and APD grading were performed
based on the ultrasound images at 38 gestational weeks
A total of 161 kidneys were scored as SFU grade I,
57 kidneys were SFU grade II, 7 kidneys were SFU grade III and 9
kidneys were SFU grade IV. According to the APD grading system, 112
kidneys were determined as having mild, 104 kidneys as moderate and
18 kidneys as displaying severe HY (Table II).
Association of SFU and APD grades with
the clinicopathological characteristics of the patients
To examine the association of clinical
characteristics with SFU and APD grades, the Chi-squared test was
first adopted, indicating that the patients' gender, affected side
or maternal age were not significantly associated with the SFU or
APD grade (all P>0.05; Table
III). By contrast, the SFU and APD grade were associated with
the post-partum outcome (all P<0.001).
 | Table III.Association of SFU and APD grades
with clinical characteristics of the HY patients. |
Table III.
Association of SFU and APD grades
with clinical characteristics of the HY patients.
|
|
| SFU grade |
| APD grade |
|
|---|
|
|
|
|
|
|
|
|---|
| Features | Affected kidneys
(n=234) | I/II (n=218) | III/IV (n=16) | P-value | Mild/moderate
(n=216) | Severe (n=18) | P-value |
|---|
| Gender |
|
|
| 0.238 |
|
| 0.314 |
|
Female | 91 | 87 | 4 |
| 86 | 5 |
|
|
Male | 143 | 131 | 12 |
| 130 | 13 |
|
| Affected side |
|
|
| 0.290 |
|
| 0.269 |
|
Left | 132 | 125 | 7 |
| 125 | 8 |
|
|
Right | 102 | 93 | 9 |
| 91 | 10 |
|
| Maternal age
(years) |
|
|
| 0.120 |
|
| 0.111 |
|
≤30 | 145 | 138 | 7 |
| 137 | 8 |
|
|
>30 | 89 | 80 | 9 |
| 79 | 10 |
|
| Post-partum
outcome |
|
|
| <0.001 |
|
| <0.001 |
|
Physiological HY | 217 | 213 | 4 |
| 211 | 6 |
|
|
Pathological HY | 17 | 5 | 12 |
| 5 | 12 |
|
SFU and APD grades are independently
associated with the post-partum outcome of fetal HY
Logistic regression analysis was then performed to
assess the influence of clinicopathological features, and the SFU
and APD grading results of the patients on post-partum outcome of
fetal HY (Table IV). The univariate
analysis revealed that an SFU grade of III/IV and severe HY
according to the APD were significantly associated with
pathological HY, which indicated that the pathological HY cases
were more frequently SFU grade III/IV (P<0.001) and had a larger
APD (P<0.001). The multivariate analysis then suggested that the
SFU grade (OR=177.840, 95% CI=16.628–1902.081, P<0.001) and APD
grade (OR=28.209, 95% CI=4.230–196.218, P=0.001) were independently
associated with the occurrence of pathological HY.
 | Table IV.Univariate and multivariate logistic
regression analysis of the association of clinicopathological
features with pathological fetal HY. |
Table IV.
Univariate and multivariate logistic
regression analysis of the association of clinicopathological
features with pathological fetal HY.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Parameters | OR | 95% CI | P-value | OR | 95% CI | P-value |
|---|
| Gender (male vs.
female) | 1.181 | 0.421–3.311 | 0.752 | 0.183 | 0.024–1.404 | 0.102 |
| Affected side (left
vs. right) | 0.899 | 0.330–2.450 | 0.835 | 1.783 | 0.284–11.195 | 0.537 |
| Maternal age
(>30 vs. ≤30 years) | 2.459 | 0.914–6.815 | 0.074 | 2.307 | 0.392–13.567 | 0.355 |
| SFU grade (III/IV
vs. I/II) | 127.800 | 30.351–538.134 | <0.001 | 177.840 |
16.628–1902.081 | <0.001 |
| APD grade (severe
vs. mild/moderate) | 64.472 | 17.859–232.746 | <0.001 | 28.209 | 4.230–196.218 | 0.001 |
Diagnostic accuracy of SFU and APD
grading systems to distinguish pathological from physiological
HY
Considering the close association of the SFU and APD
grading systems with the post-partum outcome of fetal HY, their
diagnostic value was further evaluated to with regard to their
ability to distinguish patients with pathological HY from those
with physiological HY. The sensitivity and specificity of the SFU
grading system was 70.6 and 98.2%, respectively, and the Youden
index (YI) was 0.688 for the discrimination of patients with
pathological HY from the cases of physiological HY. The sensitivity
and specificity of the APD grading system was 70.6 and 97.2%,
respectively, with a YI of 0.678 (Table
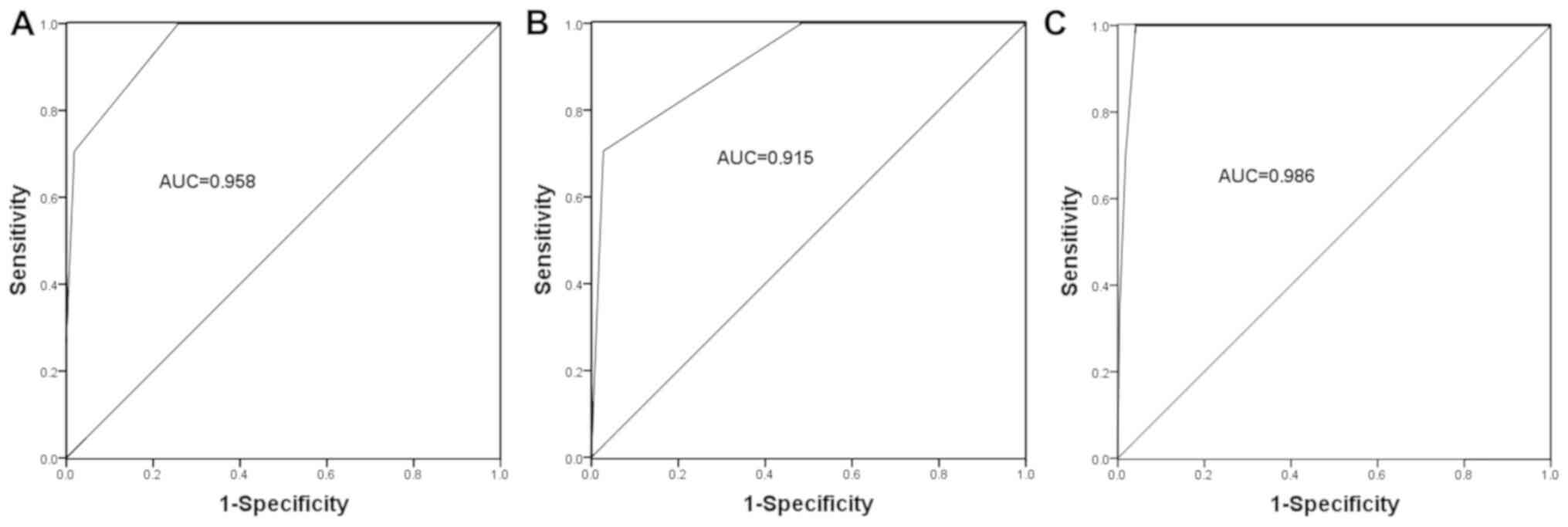
V). In addition, the ROC curves for these two systems were
constructed, and the area under the curve (AUC) was 0.958 for the
SFU grade and 0.915 for the APD grade (Fig. 2). These results indicated that the
SFU and APD grading systems have a relatively high diagnostic
accuracy. Furthermore, we the diagnostic performance of the
combined SFU and APD systems was evaluated, resulting in an AUC of
0.986, a sensitivity of 82.4%, a specificity of 98.6% and a YI of
0.810, suggesting that the combination of the SFU and APD grading
systems has a higher diagnostic value compared with that of these
two systems alone regarding the discrimination of cases of
pathological HY from those of physiological HY.
 | Table V.Diagnostic accuracy of SFU and APD
grading systems to distinguish pathological and physiological
HY. |
Table V.
Diagnostic accuracy of SFU and APD
grading systems to distinguish pathological and physiological
HY.
| Parameters | Physiological
HY | Pathological
HY | Sensitivity | Specificity | YI |
|---|
| SFU grade |
|
| 70.6% | 98.2% | 0.688 |
|
I–II | 213 | 5 |
|
|
|
|
III–IV | 4 | 12 |
|
|
|
| APD grade |
|
| 70.6% | 97.2% | 0.678 |
|
Mild-moderate | 211 | 5 |
|
|
|
|
Severe | 6 | 12 |
|
|
|
| SFU grade + APD
grade |
|
| 82.4% | 98.6% | 0.810 |
| I–II +
Mild-moderate | 214 | 3 |
|
|
|
| III–IV
+ Severe | 3 | 14 |
|
|
|
Influence of SFU and APD grades on HY
regression
The influence of the SFU and APD grades on fetal HY
regression was then assessed. The 234 kidneys affected by HY
included 204 kidneys with spontaneously resolved HY (87.2%) and 30
with persistent HY (12.8%). As presented in Table VI, univariate logistic regression
analysis indicated that an SFU grade of I/II and mild to moderate
HY according to APD grading are associated with HY regression (all
P<0.001), suggesting that those cases with resolution of HY more
frequently had low SFU and APD grades. Furthermore, multivariate
logistic regression analysis revealed that the SFU grade
(OR=24.843, 95% CI=5.471–112.804, P<0.001) and APD grade
(OR=21.301, 95% CI=5.398–84.047, P<0.001) were independently
associated with the occurrence of HY regression.
 | Table VI.Univariate and multivariate logistic
regression analysis of the influence of clinicopathological
features on HY regression. |
Table VI.
Univariate and multivariate logistic
regression analysis of the influence of clinicopathological
features on HY regression.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Parameters | OR | 95% CI | P-value | OR | 95% CI | P-value |
|---|
| Gender (male vs.
female) | 0.948 | 0.433–2.074 | 0.894 | 0.877 | 0.318–2.422 | 0.800 |
| Affected side (left
vs. right) | 1.153 | 0.535–2.488 | 0.716 | 1.085 | 0.389–3.024 | 0.876 |
| Maternal age
(>30 vs. ≤30 years) | 2.810 | 1.281–6.162 | 0.010 | 2.585 | 0.913–7.315 | 0.074 |
| SFU grade (III/IV
vs. I/II) | 51.235 | 13.289–197.531 | <0.001 | 24.843 | 5.471–112.804 | <0.001 |
| APD grade (severe
vs. mild/moderate) | 30.435 | 9.694–95.559 | <0.001 | 21.301 | 5.398–84.047 | <0.001 |
Association of SFU and APD grades with
the rate of surgery
To facilitate optimal management of HY patients,
further analysis focused on the association of SFU and APD grades
with post-partum surgery. Among the 16 patients with pathological
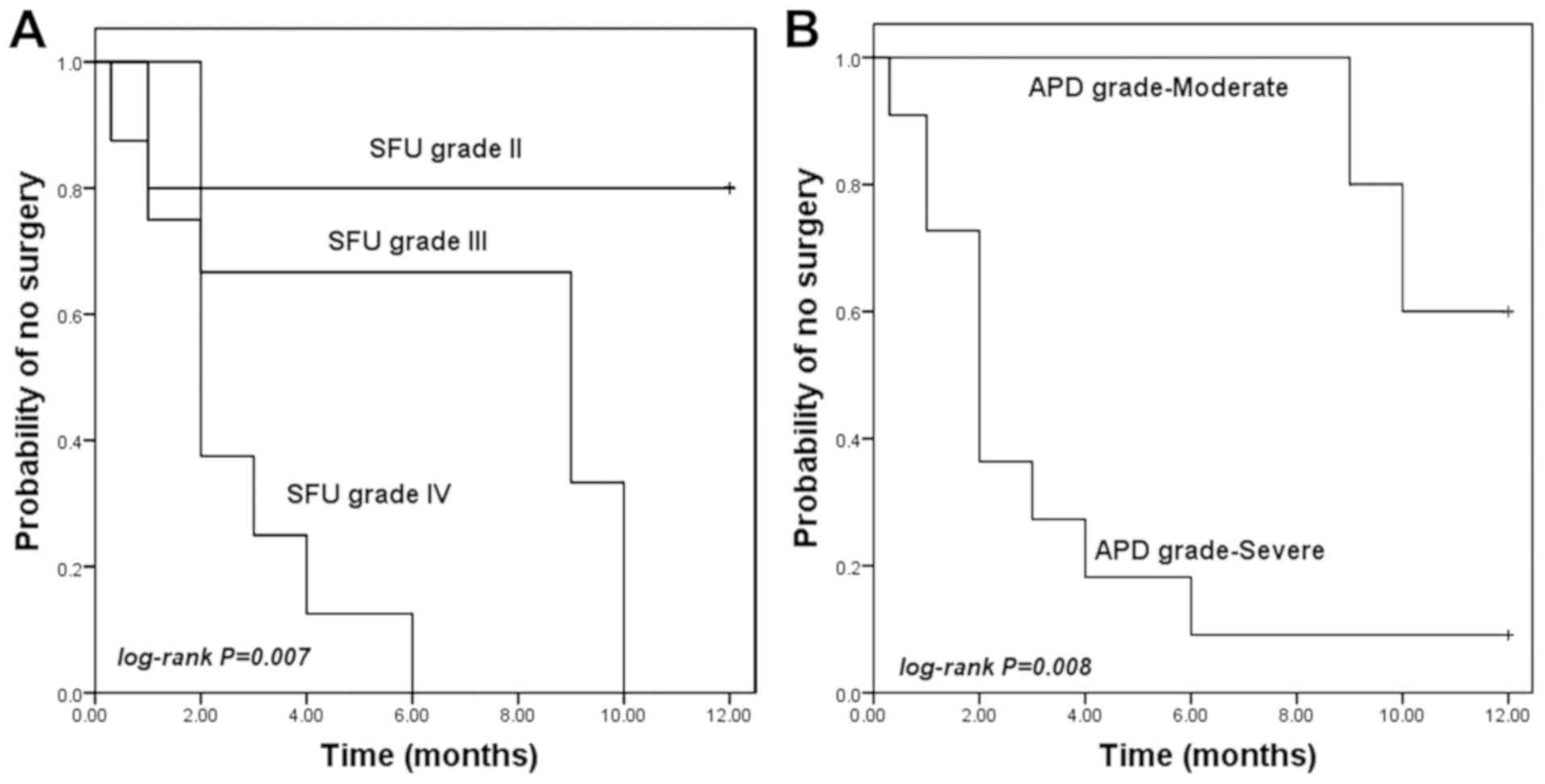
HY, 12 cases received surgery. As presented in Fig. 3, those patients with a high SFU or
APD grade had a higher surgery rate compared with those with a low
SFU (log-rank P=0.007) or APD grade (log-rank P=0.008).
Furthermore, univariate logistic regression analysis suggested that
an SFU grade III/IV and severe HY according to APD grading were
associated with a high surgery rate (all P<0.001). Multivariate
logistic regression analysis further confirmed that the SFU
(OR=55.973, 95% CI=2.202–1422.788, P=0.015) and APD grades
(OR=31.365, 95% CI=1.306–753.495, P=0.034) were independent
indicators for the occurrence of surgery (Table VII).
 | Table VII.Univariate and multivariate logistic
regression analysis of the influence of clinicopathological
features on the requirement of surgery. |
Table VII.
Univariate and multivariate logistic
regression analysis of the influence of clinicopathological
features on the requirement of surgery.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Parameters | OR | 95% CI | P-value | OR | 95% CI | P-value |
|---|
| Gender (male vs.
female) | 1.019 | 0.323–3.218 | 0.974 | 0.833 | 0.067–10.338 | 0.887 |
| Affected side (left
vs. right) | 1.116 | 0.363–3.429 | 0.848 | 1.828 | 0.138–24.212 | 0.647 |
| Maternal age
(>30 vs. ≤30 years) | 2.765 | 0.875–8.737 | 0.083 | 2.265 | 0.212–24.239 | 0.499 |
| SFU grade (III/IV
vs. I/II) | 651.000 |
67.453–6282.911 | <0.001 | 55.973 | 2.202–1422.788 | 0.015 |
| APD grade (severe
vs. mild/moderate) | 430.000 |
47.866–3862.866 | <0.001 | 31.365 | 1.306–753.495 | 0.034 |
Characteristics of the patients
diagnosed with pathological HY
The characteristics of the patients with
pathological HY are summarized in Table VIII. The patients who received
post-partum surgery had a good prognosis, as their HY was resolved
following the surgery. However, the prognosis of the patients
without surgery was unclear due to no available related follow-up
data. The etiological data regarding pathological HY indicated that
stenosis at the ureteropelvic junction was the leading cause of
pathological fetal HY.
 | Table VIII.Characteristics of the patients
diagnosed with pathological hydronephrosis. |
Table VIII.
Characteristics of the patients
diagnosed with pathological hydronephrosis.
| SFU grade | APD grade | Etiology | Surgery | Prognosis after
surgery |
|---|
| IV | Severe | Stenosis at the
left ureteropelvic junction | Yes | Favorable |
| IV | Severe | Obstruction at the
left middle ureter | Yes | Favorable |
| IV | Severe | Stenosis at the
right ureteropelvic junction | Yes | Favorable |
| II | Severe | Stenosis at the
left ureteropelvic junction | Yes | Favorable |
| IV | Severe | Stenosis at the
left ureteropelvic junction | Yes | Favorable |
| IV | Severe | Stenosis at the
left ureteropelvic junction | Yes | Favorable |
| III | Moderate | Stenosis at the end
of left ureter | Yes | Favorable |
| IV | Severe | Stenosis at the
left ureteropelvic junction | Yes | Favorable |
| III | Severe | Stenosis at the
left ureteropelvic junction | Yes | Favorable |
| IV | Severe | Stenosis at the end
of left ureter | Yes | Favorable |
| Left: IV; | Left: Severe; | Posterior urethral
valve | Yes | Favorable |
| Right: IV | Right: Severe |
|
|
|
| III | Moderate | Duplication of
pelvis and ureter with stenosis at the ureter end and
ureterocele | Yes | Favorable |
| II | Severe | Duplication of
pelvis | No | − |
| II | Moderate | − | No | − |
| II | Moderate | Stenosis at the
right ureteropelvic junction | No | − |
| II | Moderate | Stenosis at the
left ureteropelvic junction | No | − |
Discussion
Fetal HY refers to the dilatation and separation of
the fetal renal pelvis system caused by the obstruction of urine
excretion from the kidney (16). It
is generally considered that HY is a temporary clinical
manifestation of fetal urinary system dysfunction (17). In the majority of cases, fetal HY
spontaneously resolves with the increase of gestational weeks or
after birth, and is then defined as physiological HY, while
persistent or aggravated HY are defined as pathological HY.
Woodward and Frank (18) indicated
that reversible HY, which regresses during fetal growth and
development, accounted for ~65% of all fetal HY cases. A total of
162 patients were included in the present study, with 234 kidneys
diagnosed with fetal HY. A total of 16 patients with 17 kidneys
were determined to have pathological fetal HY, accounting for 9.9%
of all HY patients, and the HY in the remaining cases regressed
after birth. Previous studies revealed that pathological HY is
mainly caused by structural abnormalities of the renal pelvis
system and urine reflux (6,19). The present study indicated that 9
patients, accounting for 56.3% of all pathological HY cases, had
stenosis at the ureteropelvic junction, which was the leading cause
of pathological HY in this cohort.
Prenatal ultrasound is a widely used method to
monitor fetal HY. The SFU and APD grading systems are the two most
frequently used standardized systems for the evaluation of HY based
on ultrasound images (20). The
qualitative assessment of HY via the SFU grading system is based on
the degree of pelvicaliectasis and cortical thinning. However, the
determination of certain non-quantitative features is limited by
inter-observer variability (21).
The APD grading system is used to determine the degree of
pelviectasis, which mainly relies on the greatest diameter of the
renal pelvis measured in the ultrasound images (22). To further facilitate the diagnosis
and appropriate management of fetal HY, the present study sought to
investigate the predictive value of SFU and APD grades for the
post-partum outcome, and explore their association with spontaneous
regression of HY and requirement for surgery.
The present study first assessed the association of
the SFU and APD grades with the occurrence of pathological HY. The
results indicated that the kidneys with pathological HY usually had
a high SFU and APD grade, and the grades according to these two
systems were identified as two independent indicators for the
presence of pathological HY. Furthermore, the present study
assessed whether these two systems may be used to distinguish cases
of pathological HY from those with physiological HY. Thus, the YI
was calculated and a ROC analysis was performed, revealing that the
SFU and APD grading systems had a high diagnostic accuracy for
pathological HY. Of note, combination of the SFU and APD grading
systems increased the diagnostic accuracy as compared with that of
each grading system alone. These results suggested that the
combined method provides a reliable predictive tool for the outcome
of fetal HY.
Although the incidence of detected fetal HY has
increased in recent decades, the condition spontaneously resolves
in most cases after birth (23). The
present study performed a 12-month post-partum follow-up, during
which HY was identified to be resolved in 204 kidneys, accounting
for 87.2% of all HY cases. The association of SFU and APD grades
with the occurrence of HY regression was further assessed by
univariate and multivariate linear regression analyses using the
data at 38 gestational weeks. Most of the resolved HY cases had low
SFU or APD grades, and the SFU and APD grading systems were
independently associated with the occurrence of HY regression,
which implied that these two grading systems may be used to predict
post-partum HY regression.
The predominant treatment for persistent fetal HY is
surgery and the prognosis is favorable (24). In spite of the availability of
valuable approaches for outcome evaluation of fetal HY, including
the SFU and APD grading systems (15), controversy remains regarding the
post-partum management on the determination of surgery (25,26). To
date, certain parameters have been identified as indicators for the
requirement of surgery, including ureteropelvic junction
obstruction (27), the renal
parenchyma to hydronephrosis area ratio (28) and cortical transit time (29). The present study also assessed the
association of the SFU and APD grades with the surgery rate. The
Kaplan-Meier curves indicated that those patients with high SFU or
APD grades had a higher surgery rate than those with low SFU or APD
grades. The results of the two grading systems were proved to be
independent predictors for the performance of surgery, indicating
that they may serve as a guide for the decision to perform
surgery.
In conclusion, the majority of cases of fetal HY
spontaneously resolve after birth, and patients with pathological
HY usually have high SFU and APD grades. Stenosis at the
ureteropelvic junction was identified as a leading cause of
pathological HY. The SFU and APD grades may be used as reliable
predictors of the outcome of fetal HY, and may serve as independent
indicators for the occurrence of HY regression and post-partum
surgery.
Acknowledgements
Not applicable.
Funding
This work was supported by the Wenzhou Science and
Technology Project (grant. no. Y20180224).
Availability of data and materials
The datasets used and analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
DZ, YZ and PL designed this study, performed the APD
and SFU grading, analyzed the data and wrote the manuscript. XS,
XC, BY and TL recruited the patients, collected the ultrasound
results and analyzed the clinical data of the patients. YC, MY, LL
and LM analyzed the association of SFU and APD grades with HY
regression and surgery rate. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The protocols of the present study were approved by
the Ethics Committee of the Second Affiliated Hospital of Wenzhou
Medical University (Wenzhou, China) and written informed consent
for the use of ultrasonic data and clinical characteristics was
obtained from each participant.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zampieri N, Zamboni C, Ottolenghi A and
Camoglio FS: Unilateral hydronephrosis due to ureteropelvic
junction obstruction in children: Long term follow-up. Minerva Urol
Nefrol. 61:325–329. 2009.PubMed/NCBI
|
|
2
|
Herndon CD: The role of ultrasound in
predicting surgical intervention for prenatal hydronephrosis. J
Urol. 187:1535–1536. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Plevani C, Locatelli A, Paterlini G,
Ghidini A, Tagliabue P, Pezzullo JC and Vergani P: Fetal
hydronephrosis: Natural history and risk factors for postnatal
surgery. J Perinat Med. 42:385–391. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Delaney C: Antenatal hydronephrosis:
Trends and management. Urol Nurs. 25:173–174, 179-183.
2005.PubMed/NCBI
|
|
5
|
Braga LH, McGrath M, Farrokhyar F,
Jegatheeswaran K and Lorenzo AJ: Society for fetal urology
classification vs urinary tract dilation grading system for
prognostication in prenatal hydronephrosis: A time to resolution
analysis. J Urol. 199:1615–1621. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gordon ZN, McLeod DJ, Ching CB, Herz DB,
Bates DG, Becknell B and Alpert SA: Uroepithelial thickening
improves detection of vesicoureteral reflux in infants with
prenatal hydronephrosis. J Pediatr Urol. 12:257.e1–7. 2016.
View Article : Google Scholar
|
|
7
|
Chevalier RL: Congenital urinary tract
obstruction: The long view. Adv Chronic Kidney Dis. 22:312–319.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhan X, Tao G, Cheng L, Liu F, Li H and
Liu S: Ultrasound score: A new method to differentiate fetal
physiological and pathological hydronephrosis. Eur J Obstet Gynecol
Reprod Biol. 151:26–32. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu DB, Armstrong WR III and Maizels M:
Hydronephrosis: Prenatal and postnatal evaluation and management.
Clin Perinatol. 41:661–678. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Oliveira EA, Oliveira MC and Mak RH:
Evaluation and management of hydronephrosis in the neonate. Curr
Opin Pediatr. 28:195–201. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rao PK and Palmer JS: Prenatal and
postnatal management of hydronephrosis. ScientificWorldJournal.
9:606–614. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Vemulakonda V, Yiee J and Wilcox DT:
Prenatal hydronephrosis: Postnatal evaluation and management. Curr
Urol Rep. 15:4302014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dos Santos J, Parekh RS, Piscione TD,
Hassouna T, Figueroa V, Gonima P, Vargas I, Farhat W and Rosenblum
ND: A new grading system for the management of antenatal
hydronephrosis. Clin J Am Soc Nephrol. 10:1783–1790. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang L, Liu C, Li Y, Sun C and Li X:
Determination of the need for surgical intervention in infants
diagnosed with fetal hydronephrosis in china. Med Sci Monit.
22:4210–4217. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chalmers DJ, Meyers ML, Brodie KE, Palmer
C and Campbell JB: Inter-rater reliability of the APD, SFU and UTD
grading systems in fetal sonography and MRI. J Pediatr Urol.
12:305.e1–305.e5. 2016. View Article : Google Scholar
|
|
16
|
Zee RS, Herbst KW, Kim C, McKenna PH,
Bentley T, Cooper CS and Herndon CD: Urinary tract infections in
children with prenatal hydronephrosis: A risk assessment from the
society for fetal urology hydronephrosis registry. J Pediatr Urol.
12:261.e1–7. 2016. View Article : Google Scholar
|
|
17
|
Renda R: Renal outcome of congenital
anomalies of the kidney and urinary tract system: A single-center
retrospective study. Minerva Urol Nefrol. 70:218–225.
2018.PubMed/NCBI
|
|
18
|
Woodward M and Frank D: Postnatal
management of antenatal Hydronephrosis. BJU Int. 89:149–156. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Anjum M, Moorani KN, Sameen I, Mustufa MA
and Kulsoom S: Functional and structural abnormalities of the
kidney and urinary tract in severely malnourished children-A
hospital based study. Pak J Med Sci. 32:1135–1140. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rianthavorn P and Limwattana S: Diagnostic
accuracy of neonatal kidney ultrasound in children having antenatal
hydronephrosis without ureter and bladder abnormalities. World J
Urol. 33:1645–1650. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Arger PH, Coleman BG, Mintz MC, Snyder HP,
Camardese T, Arenson RL, Gabbe SG and Aquino L: Routine fetal
genitourinary tract screening. Radiology. 156:485–489. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wong DC, Anderson PA, Macken M and Jackson
JR: Congenital hydronephrosis who requires intervention? Can J
Urol. 6:812–818. 1999.PubMed/NCBI
|
|
23
|
Swords KA and Peters CA: Neonatal and
early infancy management of prenatally detected hydronephrosis.
Arch Dis Child Fetal Neonatal Ed. 100:F460–F464. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Al-Mashhadi A, Nevéus T, Stenberg A,
Karanikas B, Persson AE, Carlström M and Wåhlin N: Surgical
treatment reduces blood pressure in children with unilateral
congenital hydronephrosis. J Pediatr Urol. 11:91.e1–6. 2015.
View Article : Google Scholar
|
|
25
|
Gn MZ, Malik A, Hart LA, Mukherjee A and
Reese AC: Hydronephrosis secondary to an ectopic decidual reaction
in the urinary bladder. Urology. 106:e11–e12. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dy GW, Ellison JS, Fu BC, Holt SK, Gore JL
and Merguerian PA: Variable resource utilization in the prenatal
and postnatal management of isolated hydronephrosis. Urology.
108:155–160. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Arora S, Yadav P, Kumar M, Singh SK,
Sureka SK, Mittal V and Ansari MS: Predictors for the need of
surgery in antenatally detected hydronephrosis due to UPJ
obstruction-a prospective multivariate analysis. J Pediatr Urol.
11:248.e1–5. 2015. View Article : Google Scholar
|
|
28
|
Rickard M, Lorenzo AJ and Braga LH: Renal
parenchyma to hydronephrosis area ratio (PHAR) as a predictor of
future surgical intervention for infants with high-grade prenatal
hydronephrosis. Urology. 101:85–89. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Harper L, Bourquard D, Grosos C, Abbo O,
Ferdynus C, Michel JL, Dunand O and Sauvat F: Cortical transit time
as a predictive marker of the need for surgery in children with
pelvi-ureteric junction stenosis: Preliminary study. J Pediatr
Urol. 9:1054–1058. 2013. View Article : Google Scholar : PubMed/NCBI
|