Introduction
Spontaneous intracerebral hemorrhage (ICH) is a type
of neurosurgical emergency, which is particularly common in East
Asia due to ethnic backgrounds and eating habits (1–3).
Thalamic hemorrhage (TH) accounts for ~30% of all cases of ICH
(4,5). TH is frequently accompanied by
intraventricular hemorrhage (IVH), which is associated with high
mortality and morbidity rates due to a high incidence of
complications, including obstructive hydrocephalus, hypothalamic
storm or hyperthermia. In recent years, an increasing number of
studies have demonstrated that evacuation of hematoma in the
ventricle is associated with a better prognosis (1–3,5,6). The
major aim of surgery is to evacuate the hematoma maximally, while
minimizing injury to normal brain tissues. Therefore, it is
necessary to use a navigation tool to precisely devise the
trajectory of surgery. In a previous study, our group demonstrated
the feasibility of hematoma evacuation using a Kocher's point
approach under the assistance of smartphone navigation and 3D
Slicer image reconstruction (7). The
aim of the present study was to investigate the efficacy of
endoscopic surgery via a Kocher's point approach for IVH caused by
TH, in comparison with external ventricular drainage (EVD).
Materials and methods
Patients
A contemporary, non-randomized, controlled design
was adopted for the present study. From January 2016 to August
2017, 64 patients diagnosed with TH were treated at the Departments
of Neurosurgery and Neuro-Intensive Care Unit (NICU), Central
Hospital of Jinzhou (Jinzhou, China). Patients with IVH caused by
TH who had a Glasgow Coma Scale (GCS) score (8) of ≤12 were indicated for surgery.
Finally, 40 patients were included in the study and were allocated
to an EVD group or an endoscopic surgery group. As the patients
were in comas, the decision of what treatment the patient would
receive was made by the legally authorized representative. The
inclusion criteria were as follows: i) Hypertensive TH with IVH
confirmed by computed tomography (CT) scan; ii) hematoma volume ≥25
ml (7,9,10); iii)
patient age ≤75 years; iv) 4≤GCS≤12; v) written informed consent
provided by the patient's legally authorized representative. The
exclusion criteria were as follows: i) Secondary hemorrhage caused
by trauma, aneurysms, vascular malformations or tumor; ii)
multifocal bleeding with the exception of extension of TH to
another location; iii) brainstem failure indicated by bilateral
mydriasis, decerebrate rigidity and unstable vital signs; iv)
severe dysfunction of the heart, liver or kidney; v) mortality
within 3 days (7). The present study
was approved by Ethics Committee of Central Hospital of Jinzhou
(Jinzhou, China) and was performed in conformity to the Declaration
of Helsinki. All patient's legally authorized representative
provided written informed consent prior to enrolment in the present
study.
Surgery
In the EVD group, standard EVD was performed on
patients under local anesthesia and intravenous sedation (11). No intraventricular injection of
thrombolytics (e.g. urokinase) or aspiration were performed during
the surgical procedure. At 6 h after EVD, 20,000 units of urokinase
were injected through the catheter to dissolve the residual
hematoma and facilitate drainage. The drainage bottle was then
opened but elevated to the height of 27 cm H2O for 2 h
to allow for drug and hematoma interaction. This prevented high
intracranial pressure and undetected obstructive hydrocephalus.
After 2 h, the drainage bottle was reduced to 15 cm H2O
for drainage. Injection of urokinase was performed twice a day for
3–5 days. Patients with ventricular blood received continuous
drainage at 15 cm H2O until there was no further
reduction in cerebrospinal fluid (CSF) blood content. The EVD
catheter was then elevated to the height of 27 cm H2O.
The catheter was removed if the drainage volume was <50 ml over
the next 24 h. Patients were considered as having failed catheter
‘elevation’ if they developed hydrocephalus or their consciousness
deteriorated.
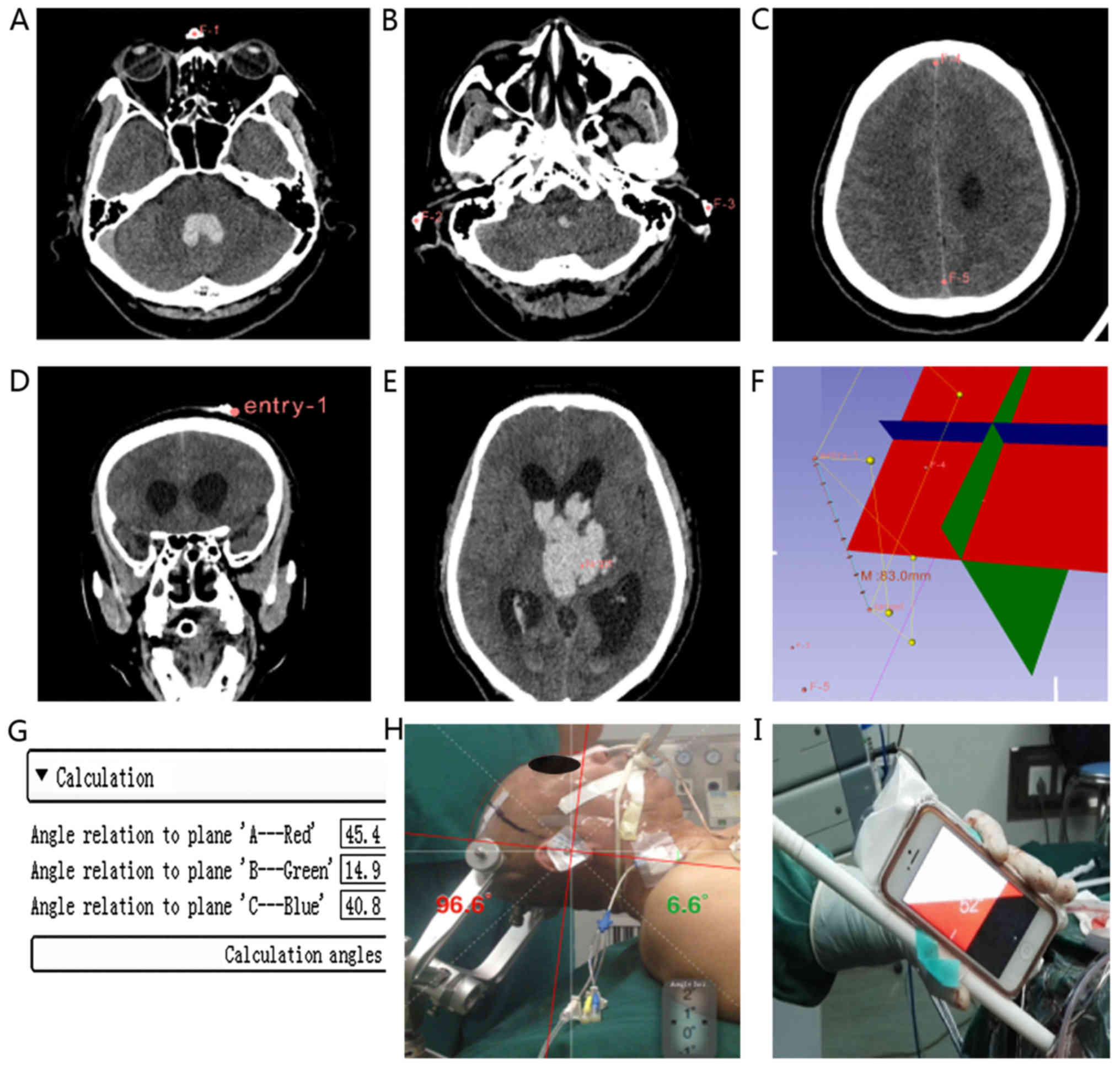
In the endoscopic surgery group, smartphone-assisted
navigation was used (Fig. 1). First,
four fiducial markers (electrode pads) were attached to the
patient's head at the following locations: Nasion (F-1), external
auditory canal on both sides (F-2, F-3) and entry point (Kocher's
point). The fiducial F-1, F-2 and F-3 were marked to define the
first reference plane. The reference fiducials F-4 and F-5 were
indicated on the midline of the CT image, usually on the cerebral
falx. Using these two fiducials, the second reference plane was
then defined and the third reference plane was automatically
generated. The entry point was 1 cm anterior to the coronal suture
and 2.5 cm lateral to the midline. This was named Kocher's point
and selected for endoscopic port insertion. The target point was
the bottom of the thalamic hematoma rather than the IVH hematoma,
and was marked to define the trajectory. After removing the
hematoma of the thalamus, the ventricle was entered through the
crevasse. Using the GyroGuide software extension for 3D Slicer
(http://download.slicer.org), the angle
between the trajectory and each of the three reference planes was
automatically calculated. The endoscopic surgery procedure was
performed under general anesthesia with the patient in the supine
position. A contra-lateral EVD was performed first if the Graeb
score of the contra-lateral ventricle was ≥2. Second, a 4-cm
incision was made at Kocher's point. A Burr hole was drilled and a
2.5-cm bone flap was milled off. A transcortical puncture was made
with an 18-mm rigid plastic rod. A relatively big diameter was able
to reduce the frequency of adjustment of the sheath and support the
evacuation of hematoma. According to the smartphone-assisted
navigation, the puncture depth was the distance between Kocher's
point and the target, which was calculated using the 3D Slicer
software (7,12,13).
When the target was reached, a transparent sheath was placed along
the rod. The rod was then removed and the sheath was fixed by a
retractor 0° endoscope (Neuroendoscope; Aesculap, Inc.) and a
suction tube was inserted through this transparent sheath, allowing
for the removal of hematomas. A slim bipolar cauterizer was used to
cauterize the vessel when bleeding. When all procedures were
completed, a drainage tube was left in the ventricle in accordance
with the hematoma evacuation rate. The EVD procedure after
endoscopic surgery was the same as that performed in the EVD group.
No urokinase was administered during this procedure. Permanent
ventriculo-peritoneal (VP) shunt surgery was performed if patients
were diagnosed with hydrocephalus 3 weeks after surgery and total
protein in the CSF was <0.45 g/l.
Outcome evaluation
The pre-operative characteristics recorded included
the pre-operative GCS score, age, ICH volume and severity of IVH. A
simplified equation was used to estimate the volume of hematoma:
1/2A × B × C, where A is the maximum width measured, B is the
length and Cis the height (14). The
Graeb score was used to evaluate the severity of IVH, which is the
sum of the score in each ventricle; 4 is the maximum score in each
lateral ventricle and 2 is the maximum score in the third and
fourth ventricles (15). The
modified Rankin Scale (mRS) (16)
was used to evaluate the prognosis of patients. The mRS includes
seven grades: 0, no symptoms; 1, no significant disability; 2,
slight disability; 3, moderate disability; 4, moderately severe
disability; 5, severe disability; and 6, death. All patients were
followed up at 180 days after ictus using the mRS by telephone or
at the clinic. A favorable outcome was defined as a 180-day mRS
score ≤3, whereas an unfavorable outcome was defined as a 180-day
mRS score >3.
Statistical analysis
All statistical analyses were performed using SPSS
19.0 (IBM Corp.). An unpaired t-test or χ2 test was used
for comparison between groups, as appropriate. Normally distributed
data are expressed as the mean ± standard deviation and were
compared using an unpaired t-test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Patient characteristics
From January 2016 to August 2017, 64 patients
diagnosed with TH were treated at the Departments of Neurosurgery
and NICU, Central Hospital of Jinzhou (Jinzhou, China). Patients
with IVH caused by TH who had a GCS ≤12 were indicated for surgery.
Finally, 40 patients were included in the present study, with 20
patients allocated to the EVD group and 20 to the endoscopic
surgery group. The clinical characteristics of the patients in each
group are presented in Table I. The
average age of the patients was 59.9±8.7 (42–73) years in the EVD
group and 61.0±8.5 (48–70) years in the endoscopic group
(P>0.05). The mean pre-operative GCS score was 7.7±1.7 (5–10)
for the EVD group and 7.4±2.3 (4–10) for
the endoscopic group (P>0.05). In the EVD group, the mean
hematoma volume was 34.8 ml, and in the endoscopic group, it was
35.2 ml (P>0.05). The baseline data, including age, GCS,
hematoma volume and Graeb score, were not significantly different
between the endoscopic group and the EVD group.
 | Table I.Clinical data of the patients with
intraventricular hemorrhage caused by thalamic hemorrhage. |
Table I.
Clinical data of the patients with
intraventricular hemorrhage caused by thalamic hemorrhage.
| Parameter | EVD (n=20) | Endoscopic
(n=20) | P-values |
|---|
| Age (years) | 59.9±8.7 | 61.0±8.5 | 0.64 |
| Initial GCS | 7.7±1.7 (5–10) | 7.4±2.3 (4–10) | 0.64 |
| ICH volume (ml) | 34.8±8.4 (25–50) | 35.2±7.4 (25–50) | 0.88 |
| Graeb score | 7.5±2.2 (4–10) | 7. 4±2.3 (4–10) | 0.95 |
Clinical outcomes
The clinical outcomes are presented in Table II. The length of NICU stay was
6.4±4.4 days in the endoscopic surgery group and 8.4±4.6 days in
the EVD group; this difference was not statistically significant
(P>0.05). The 30-day and 90-day mortality rates were 5 and 15%
in the endoscopic surgery group, and 10 and 20% in the EVD group,
respectively. However, statistical analysis demonstrated no
significant difference due to an insufficient number of cases
(P>0.05). The mean mRS score was 3.7±1.2 in the endoscopic
surgery group and 4.2±1.4 in the EVD group (P>0.05). The VP
shunt rates were 50.0% in the EVD group and 15.0% in the endoscopic
surgery group. Patients in the EVD group had a significantly higher
VP shunt rate (P=0.02; odds ratio, 5.7) compared with those in the
endoscopic surgery group. Endoscopic surgery significantly reduced
permanent shunt dependency for IVH caused by TH compared with EVD
alone. No secondary infections were observed in any of the 40
patients.
 | Table II.Clinical outcomes of patients with
intraventricular hemorrhage caused by thalamic hemorrhage. |
Table II.
Clinical outcomes of patients with
intraventricular hemorrhage caused by thalamic hemorrhage.
| Parameter | EVD (n=20) | Endoscopic
(n=20) | P-value | Odds ratio (95%
CI) |
|---|
| Length of NICU
stay | 8.4±4.6 | 6.4±4.4 | 0.17 | ND |
| 30-day mortality
rate | 2 (10%) | 1 (5%) | 0.55 | ND |
| 90-day mortality
rate | 4 (20%) | 3 (15%) | 0.68 | ND |
| Postoperative
GCS | 10.2±3.4 | 11.3±3.3 | 0.31 | ND |
| Modified rankin
scale | 4.2±1.4 | 3.7±1.2 | 0.76 | ND |
| VP shunt rate | 10 (50%) | 5 (15%) | 0.02 | 5.7
(1.27–25.53) |
Case report
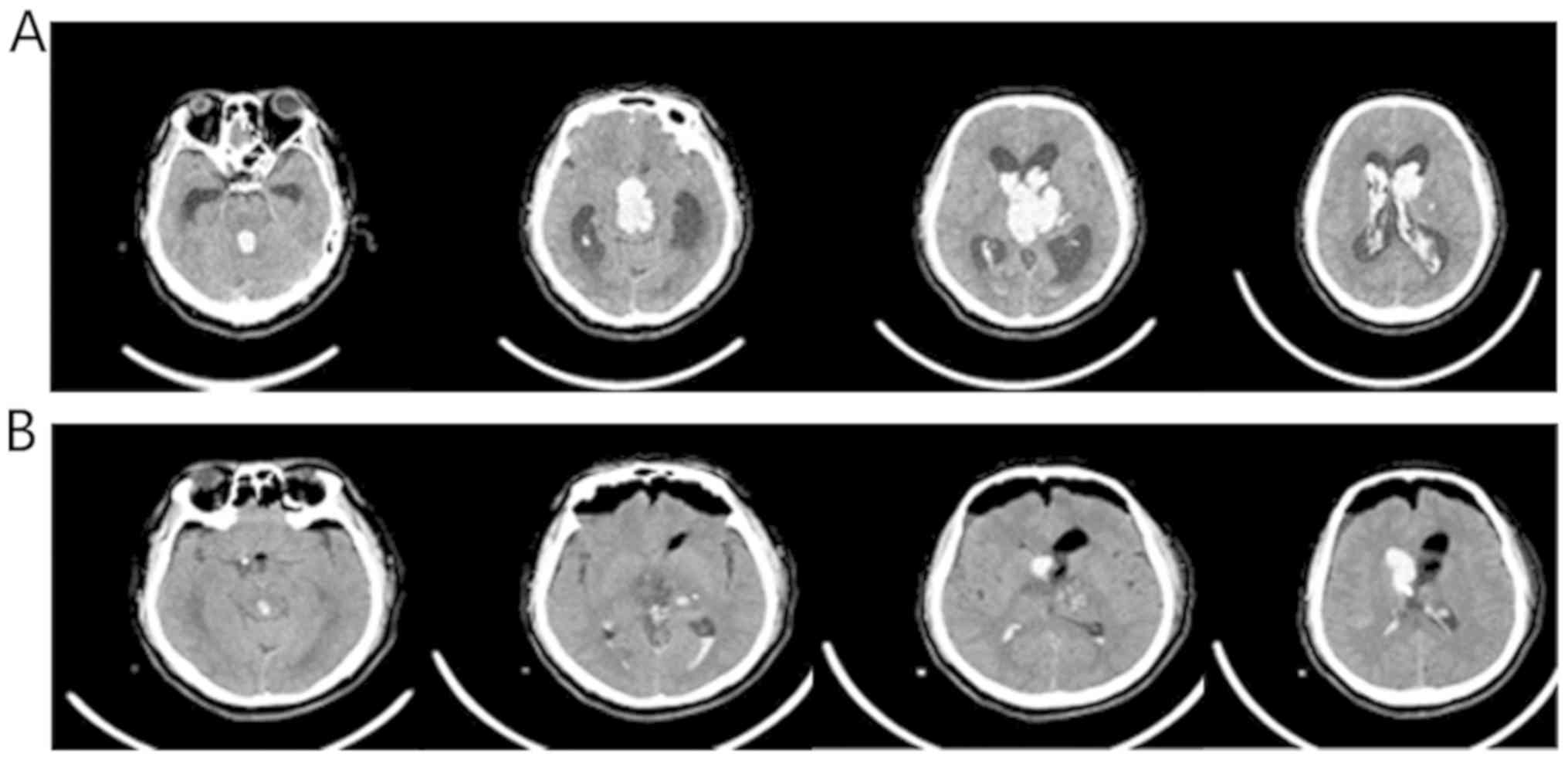
A 58-year-old man was transferred to our hospital
due to sudden loss of consciousness and vomiting several times. In
the emergency room, the patient was in a severe coma (GCS score,
6). A CT scan illustrated left-sided TH with rupture into the
bilateral ventricles and the 3rd and 4th ventricles. The patient
also presented with acute hydrocephalus (Fig. 2). The volume of the hematoma was
estimated to be 40 ml according to a simplified equation (12). The patient underwent a contra-lateral
EVD and endoscopic surgery to evacuate the thalamic hematoma. A
post-operative CT scan demonstrated complete removal of the
thalamic hematoma, including hematoma of the left-side lateral
ventricle and the 3rd ventricle (Fig.
2). The right-side ventricular drainage was kept for 5 days
after surgery. Intraventricular injection of 20,000 units of
urokinase twice a day was applied for 4 days. The patient regained
consciousness 2 weeks later and was sent to a rehabilitation
center. At 3 months, the patient's mRS score was 3 (Video S1).
Discussion
Our group previously reported a procedure performed
on 8 patients by Kocher's point approach using 3D Slicer software
and handheld smartphone-assisted navigation (7), among whom only 1 patient required VP
shunt surgery. To further demonstrate the feasibility and efficacy
of this surgical approach, 40 patients were assigned to an EVD
group or an endoscopic surgery group in a non-randomized fashion
for the present study. There were no significant differences
between the two treatment groups with regard to their 30- or 90-day
mortality rate or mRS score at 6 months after the onset of TH. As
compared with EVD alone, smartphone-assisted endoscopic surgery via
Kocher's point was safe and feasible, and significantly reduced
dependency on permanent shunt due to hydrocephalus. In general,
there are four types of TH according to the anatomical location of
the hemorrhage: Posterior-lateral, anterior-lateral, medial and
dorsal (17). The first two types of
hemorrhage may easily rupture into the trigone of the lateral
ventricle. This may obstruct normal CSF flow and result in acute
hydrocephalus. For ICH, removal of the hematoma is the most
important step. This does not only reduce the hematoma volume and
edema formation, which leads to reduction in intracranial pressure,
but also reduces neurotoxic edema that is caused by increased
thrombin and blood degradation products (18). Therefore, it is beneficial to remove
the hematoma as soon as possible so as to reduce secondary injuries
of ICH, particularly for severe TH accompanied with IVH.
Severe IVH has a high mortality and morbidity rate
due to multiple complications, including obstructive hydrocephalus,
hypothalamic storm and hyperthermia. A previous study identified
that EVD surgery was able to relieve hydrocephalus, but not to
prevent shunt-dependent hydrocephalus, as IVH disrupted CSF
circulation (16). IVH is a negative
prognostic factor in ICH and permanent shunt dependency is present
in a substantial proportion of patients (6,19).
Strategies to prevent permanent shunting are increasingly
important, as shunt malfunction and other shunt-associated
complications occur frequently and are associated with increased
morbidity (6). In the present study,
13 out of 40 patients with IVH caused by TH required VP shunt
surgery. The overall VP shunt rate was 32.5%, but only 15% of
patients in the endoscopic surgery group required VP shunt surgery,
whereas 50% of those in the EVD group required shunt surgery. The
EVD group had a significantly higher VP shunt rate (P=0.02; odds
ratio, 5.7). No endoscopic third ventriculostomy (ETV) was
performed in the present study and the possible reason may be that
endoscopic surgery was able to evacuate the hematoma while
protecting the unaffected areas of the brain.
There are numerous strategies to prevent
hydrocephalus (6,20,21).
Huttner et al (20) reported
that using temporary lumbar drainage was able to reduce VP shunt
rates after ICH. In a study published ten years later, the same
group recommended lumbar drainage for treating IVH and reducing VP
shunt rates (21). Oertel et
al (22) explored the value of
ETV in the treatment of patients who had suffered IVH with
obstructive hydrocephalus. They reported that in the ETV group,
which consisted of 33 patients, only two patients who suffered from
IVH (2/33, 5.9%) required VP shunt surgery. Therefore, it was
proposed that ETV is a safe treatment for IVH-associated
obstructive hydrocephalus. Compared with the EVD group, ETV had a
lower risk of infection and a low VP shunt rate.
Obaid et al (23) performed a retrospective analysis of
78 consecutive patients who underwent ETV at their institution.
They identified 17 consecutive patients who underwent ETV for
obstructive hydrocephalus associated with IVH. None of the patients
who suffered from IVH and underwent ETV required VP shunt surgery.
To treat primary TH and reduce secondary injury of TH and IVH,
certain studies have used minimally invasive surgery to mobilize
sedentary blood and enhance CSF clearance through intraventricular
fibrinolysis (IVF) (5,24,25).
Chen et al (5) performed
stereotactic aspiration with subsequent thrombolysis for moderate
TH. They concluded that IVF is safe and feasible for
post-hemorrhagic hydrocephalus and may markedly reduce the
requirement for shunt surgery.
In the present study, endoscopic surgery was
performed via Kocher's point by smartphone-assisted navigation to
evacuate hematomas of TH and IVH. First, this approach is a
modification of the EVD approach and suitable for a minimally
invasive strategy. Second, smartphone-assisted navigation was used
to ensure the transparent sheath arrived precisely at the target,
which reduced unnecessary surgery-induced injury. Modern navigation
systems are helpful but expensive. A low-cost solution to locate
the hematoma or brain lesion and navigate the surgery under the
assistance of augmented reality would be beneficial. The accuracy
of smartphone navigation is fine and acceptable (3). Third, the hematoma was removed
aggressively by neuroendoscopy, including TH and IVH. During the
endoscopic surgery, only the IVH and soft TH were removed, while
the hard hematoma was left in the hematoma cavity as described by
Chen et al (6). Compared with
other approaches, the Kocher's point approach allowed for improved
evacuation of hematomas, as the whole lateral ventricle was visible
under neuroendoscopy. In the present study, the third ventricular
hematoma was evacuated through the foramen of Monro and ETV was
possible when required, even though none of the patients of the
present study underwent an ETV procedure. Finally, a drainage tube
was left in the ventricle to evacuate the bloody CSF and perform
IVF to hasten the resolution of IVH. No urokinase was administered
during the endoscopic procedure to avoid rebleeding.
Intra-ventricular injection of a thrombolytic (20,000 units of
urokinase, twice a day) was performed 6 h after surgery. The
urokinase was injected through the catheter to dissolve the
residual hematoma and facilitate drainage, and then the drainage
bottle was opened but elevated to the height of 27 cm
H2O for 2 h to allow for drug and hematoma interaction.
This avoided high intracranial pressure and undetected obstructive
hydrocephalus. No secondary infections were observed among the 40
patients in the present study.
The present study demonstrated that endoscopic
surgery lowered the shunt-dependent hydrocephalus rate from 50 to
15% in IVH caused by TH compared with the EVD group. Endoscopic
surgery is able to remove primary hematoma and intraventricular
blood quickly, and may rapidly reverse ventricular dilatation and
reduce intracranial pressure. Developing hydrocephalus may be
prevented by removing primary and IVH hematomas and reversing
ventricle dilatation. After surgery, urokinase was used to dissolve
the residual hematoma and facilitate drainage to enhance CSF
clearance, as the volume of intraventricular blood is a key
prognostic factor associated with poor outcome in patients with IVH
(26). All of these procedures
helped to reduce the requirement for VP shunt surgery, and a better
prognosis was obtained according to the outcomes. Compared with
Chen et al (6), a lower VP
shunt rate was achieved in the present study, which is likely due
the patients receiving IVF.
In the present study, the Graeb scores of the
endoscopic group were similar to those in the EVD group, but the VP
shunt rate was lower (P=0.02). The 30-day mortality rate was 5% in
the endoscopic surgery group and 10% in the EVD group, while the
90-day mortality rate was 15% in the endoscopic surgery group and
20% in the EVD group. However, no statistically significant
difference was obtained due to the insufficient sample size. The
mortality rate was lower compared with that reported by Steinke
et al (27) and Chen et
al (5). This demonstrated that
the present endoscopic and successive procedure was able to remove
IVH faster, reduce ventricular dilatation and re-equilibrate CSF
circulation, avoiding persistent hydrocephalus and the requirement
for VP shunt surgery, and resulting in a lower mortality rate
compared with that obtained in other studies.
Although certain studies have demonstrated that
endoscopic surgery offers a better surgical outcome compared with
EVD in IVH therapy (28), no
significant difference in mortality rates, post-operative GCS
scores at 2 weeks and mRS scores at 6 months were obtained between
the endoscopic surgery and the EVD group of the present study.
These outcomes are similar to those of Chen et al (5). The present study addressed certain
limitations of Chen et al (5), but certain limitations still exist. The
present study had a non-randomized design and a relatively small
sample size; therefore, a randomized study with a larger number of
patients is warranted.
In conclusion, the present study demonstrated that
endoscopic surgery significantly lowered the rate of VP shunt
surgery and may shorten the stay at the NICU in patients with IVH
resulting from TH compared with traditional EVD.
Smartphone-assisted endoscopic surgery via Kocher's point is
feasible and safe, and significantly reduces permanent shunt
dependency for IVH caused by TH.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This study was supported by Scientific Technology
Research Projects of Jinzhou (grant no. 16B1G37) and the Chinese
National Key Research and Development Plan (grant no.
2018YFC1312602).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XG and XX are co-first authors. XG, XX, XY and XC
designed drafted the manuscript. DL and YZ collected the data. XG,
XX, YZ and YX statistically analyzed the data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The current study was approved by the Ethics
Committee of Central Hospital of Jinzhou (Jinzhou, China). Written
informed consent was obtained from each patient's legally
authorized representative.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Xu X, Chen X, Li F, Zheng X, Wang Q, Sun
G, Zhang J and Xu B: Effectiveness of endoscopic surgery for
supratentorial hypertensive intracerebral hemorrhage: A comparison
with craniotomy. J Neurosurg. 128:553–559. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ma L, Hou Y, Zhu R and Chen X: Endoscopic
evacuation of basal ganglia hematoma: Surgical technique, outcome,
and learning curve. World Neurosurg. 101:57–68. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hou Y, Ma L, Zhu R and Chen X:
iPhone-assisted augmented reality localization of basal ganglia
hypertensive hematoma. World Neurosurg. 94:480–492. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nomura S, Ishihara H, Yoneda H, Shirao S,
Shinoyama M and Suzuki M: Neuroendoscopic evacuation of
intraventricular hematoma associated with thalamic hemorrhage to
shorten the duration of external ventricular drainage. Surg Neurol
Int. 1(pii): 432010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen M, Wang Q, Zhu W, Yin Q, Ma M, Fan X,
Li Y, Ni G, Liu C, Liu W, et al: Stereotactic aspiration plus
subsequent thrombolysis for moderate thalamic hemorrhage. World
Neurosurg. 77:122–129. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen CC, Liu CL, Tung YN, Lee HC, Chuang
HC, Lin SZ and Cho DY: Endoscopic surgery for intraventricular
hemorrhage (IVH) caused by thalamic hemorrhage: Comparisons of
endoscopic surgery and external ventricular drainage (EVD) surgery.
World Neurosurg. 75:264–268. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ge X, Chen X, Sun J and Li D: Endoscopic
surgery via kocher point approach by simply navigation to treat
Intraventricular Hemorrhage (IVH) Caused by Thalamic Hemorrhage.
Chin J Nerv Ment Dis. 43:176–179. 2017.
|
|
8
|
Teasdale G and Jennett B: Assessment of
coma and impaired consciousness. A practical scale. Lancet.
2:81–84. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Auer LM, Deinsberger W, Niederkorn K, Gell
G, Kleinert R, Schneider G, Holzer P, Bone G, Mokry M, Körner E, et
al: Endoscopic surgery versus medical treatment for spontaneous
intracerebral hematoma: A randomized study. J Neurosurg.
70:530–535. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Teernstra OP, Evers SM, Lodder J, Leffers
P, Franke CL and Blaauw G; Multicenter randomized controlled trial
(SICHPA), : Stereotactic treatment of intracerebral hematoma by
means of a plasminogen activator: A multicenter randomized
controlled trial (SICHPA). Stroke. 34:968–974. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dey M, Jaffe J, Stadnik A and Awad IA:
External ventricular drainage for intraventricular hemorrhage. Curr
Neurol Neurosci Rep. 12:24–33. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fedorov A, Beichel R, Kalpathy-Cramer J,
Finet J, Fillion-Robin JC, Pujol S, Bauer C, Jennings D, Fennessy
F, Sonka M, et al: 3D Slicer as an image computing platform for the
quantitative imaging network. Magn Reson Imaging. 30:1323–1341.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen X, Xu BN and Yu XG: iPod
touch-assisted instrumentation of the spine: Is it accurate and
reliable? Neurosurgery. 6:E734–E736. 2014. View Article : Google Scholar
|
|
14
|
Kothari RU, Brott T, Broderick JP, Barsan
WG, Sauerbeck LR, Zuccarello M and Khoury J: The ABCs of measuring
intracerebral hemorrhage volumes. Stroke. 27:1304–1305. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Graeb DA, Robertson WD, Lapointe JS,
Nugent RA and Harrison PB: Computed tomographic diagnosis of
intraventricular hemorrhage. Etiology and prognosis. Radiology.
143:91–96. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gupta VP, Garton ALA, Sisti JA, Christophe
BR, Lord AS, Lewis AK, Frey HP, Claassen J and Connolly ES Jr:
Prognosticating functional outcome after intracerebral hemorrhage:
The ICHOP score. World Neurosurg. 101:577–583. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kumral E, Kocaer T, Ertubey NO and Kumral
K: Thalamic hemorrhage. A prospective study of 100 patients.
Stroke. 26:964–970. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang WZ, Jiang B, Liu HM, Li D, Lu CZ,
Zhao YD and Sander JW: Minimally invasive craniopuncture therapy
vs. conservative treatment for spontaneous intracerebral
hemorrhage: Results from a randomized clinical trial in China. Int
J Stroke. 4:11–16. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Miller C, Tsivgoulis G and Nakaji P:
Predictors of ventriculoperitoneal shunting after spontaneous
intraparenchymal hemorrhage. Neurocrit Care. 8:235–240. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huttner HB, Nagel S, Tognoni E, Köhrmann
M, Jüttler E, Orakcioglu B, Schellinger PD, Schwab S and Bardutzky
J: Intracerebral hemorrhage with severe ventricular involvement:
Lumbar drainage for communicating hydrocephalus. Stroke.
38:183–187. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Huttner HB and Kuramatsu JB: Current
treatment concepts in intracerebral hemorrhage. Med Klin
Intensivmed Notfmed. 112:695–702. 2017.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Oertel JM, Mondorf Y, Baldauf J, Schroeder
HW and Gaab MR: Endoscopic third ventriculostomy for obstructive
hydrocephalus due to intracranial hemorrhage with intraventricular
extension. J Neurosurg. 111:1119–1126. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Obaid S, Weil AG, Rahme R and Bojanowski
MW: Endoscopic third ventriculostomy for obstructive hydrocephalus
due to intraventricular hemorrhage. J Neurol Surg A Cent Eur
Neurosurg. 76:99–111. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Morgan T, Awad I, Keyl P, Lane K and
Hanley D: Preliminary report of the clot lysis evaluating
accelerated resolution of intraventricular hemorrhage (CLEAR-IVH)
clinical trial. Acta Neurochir Suppl. 105:217–220. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Morgan T, Zuccarello M, Narayan R, Keyl P,
Lane K and Hanley D: Preliminary findings of the minimally-invasive
surgery plus rtPA for intracerebral hemorrhage evacuation (MISTIE)
clinical trial. Acta Neurochir Suppl. 105:147–151. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Nishikawa T, Ueba T, Kajiwara M, Miyamatsu
N and Yamashita K: A priority treatment of the intraventricular
hemorrhage (IVH) should be performed in the patients suffering
intracerebral hemorrhage with large IVH. Clin Neurol Neurosurg.
111:450–453. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Steinke W, Sacco RL, Mohr JP, Foulkes MA,
Tatemichi TK, Wolf PA, Price TR and Hier DB: Thalamic stroke.
Presentation and prognosis of infarcts and hemorrhages. Arch
Neurol. 49:703–710. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhang Z, Li X, Liu Y, Shao Y, Xu S and
Yang Y: Application of neuroendoscopy in the treatment of
intraventricular hemorrhage. Cerebrovasc Dis. 24:91–96. 2007.
View Article : Google Scholar : PubMed/NCBI
|