Introduction
Pain is an unavoidable physiological process that
mothers experience during natural childbirth (1). According to the Finnerup pain score
(2), the highest pain level occurs
during delivery. In clinical practice, a vaginal delivery is
preferred, but for patients who cannot tolerate severe pain or who
encounter complications that threaten the mother's or baby's
survival, a cesarean delivery may be performed (3). At present, ~42.35% of deliveries
worldwide are performed by cesarean section, and in certain
developed countries and regions, the cesarean section rate is even
higher (4). Huang et al
(5) indicated that the cesarean
section rate has increased every year since 2010 due to a large
proportion of females being unable to overcome their inner fear of
labor pain during childbirth. However, Mylonas and Friese (6) determined that the average recovery
period from a cesarean section was 3–5 weeks longer than recovery
from a vaginal delivery, and since the neonate does not pass
through the birth canal during the cesarean section, their lungs
and nerve endings are not stimulated. Therefore, cesarean delivery
may affect the newborn's growth and development.
Clinical application of anesthesia during labor and
delivery to reduce the negative impact of pain is common. The most
frequently used method is combined spinal-epidural anesthesia.
Under local anesthesia of the maternal lumbar nerves and below, the
patient's mind remains awake, supporting the normal delivery
process (7).
The most commonly used drug for traditional combined
spinal-epidural anesthesia is levobupivacaine. Levobupivacaine is
safer than bupivacaine and is less toxic to the central nervous
system and heart. However, in recent years, continuous studies have
indicated that females experienced a certain degree of cardiac
dysfunction after the application of levobupivacaine in combined
spinal-epidural anesthesia. Neonatal nerves may also be damaged by
the use of anesthetic drugs used for cesarean section (8). At present, with the increasing cesarean
section rate in clinical practice, research is urgently required in
order to determine how to reduce the impact of anesthetic drugs on
mothers and neonates during cesarean deliveries. There have been
advances in research and medical technology in recent years
(9–11), from which the application of
ropivacaine has evolved. Ropivacaine is a recently developed local
anesthetic drug. It is suitable for anesthesia during maternal
delivery and has little impact on the uterus, placenta and maternal
hemodynamics (12). Kathuria et
al (13) reported that the use
of combined spinal-epidural anesthesia with ropivacaine greatly
reduces adverse reactions in maternal females, and has a better
effect than traditional anesthetic drugs. In 2016, combined
spinal-epidural anesthesia with ropivacaine has been introduced for
application during the delivery process.
In the present study, the use of combined
spinal-epidural anesthesia with ropivacaine for deliveries at our
hospital since 2016 was retrospectively analyzed. The present
analysis aimed to validate that the use of combined spinal-epidural
anesthesia with ropivacaine is beneficial regarding the safety of
mothers and neonates, provide a useful reference for clinical use
and promote the use of ropivacaine in combined spinal-epidural
anesthesia.
Materials and methods
General information
A retrospective analysis of 615 maternal patients
who delivered between April 2016 and March 2017 at Guangzhou Women
and Children's Medical Center (Guangzhou, China) was performed. The
inclusion criteria were as follows: Full-term pregnancy, no
contraindications for intraspinal anesthesia, use of combined
spinal-epidural anesthesia with ropivacaine or levobupivacaine,
vertex presentation of a singleton pregnancy and the availability
of complete medical records. Based on these criteria, 942 patients
were considered for inclusion in the study. The following exclusion
criteria were then applied: Cardiovascular or cerebrovascular
disease (n=78), failure of major organs (n=16), drug allergies
(n=31), severe eclampsia (n=14), tumors (n=33), physical disability
(n=90), family history of disease (n=54) or transfer to another
facility (n=11). Ultimately, 615 patients were included in the
study. All of these patients provided written informed consent. The
patients were divided into two groups based on the drugs used
during delivery: The ropivacaine group (combined spinal-epidural
anesthesia with ropivacaine) included 318 cases and the
levobupivacaine group (combined spinal-epidural anesthesia with
levobupivacaine) included 297 cases. Each procedure was approved by
the Ethics Committee of the Guangzhou Women and Children's Medical
Center (Guangzhou, China) and conformed with the Intrapartum Care:
Care of Healthy Women and Their Babies During Childbirth guidelines
(14) of the National Collaborating
Centre for Women's and Children's Health.
Anesthetic method
The patients underwent dural puncture through the
L2-3 space when the cervix was dilated by 3–4 cm. The catheter was
inserted 3 cm, after which ropivacaine or levobupivacaine was
injected (4 ml each; concentration, 0.125%) with micro-pump. After
10 min, 4 ml ropivacaine or 4 ml levobupivacaine containing 2 µg/ml
sufentanil were again injected, and this was repeated a total of 3
times at 30-min intervals. The amount of controlled analgesia was
set to 4 ml and the time was set to 15 min. After delivery, the
micro-pump was turned off. If the maternal patient was still unable
to give birth normally after anesthesia, a cesarean section was
performed.
Parameters observed
The clinical data collected were age, weight and
gestational age. The onset of analgesia was measured from the
initial injection of the drug to the disappearance of pain in the
patient. A visual analog pain scale (15) was used to assess the maternal
patient's pain at T3, with 0 representing no pain and 10
representing unbearable pain. Systolic blood pressure (SBP),
diastolic blood pressure (DBP) and heart rate (HR) were measured at
pre-analgesia (T1), 30 min after analgesia (T2), at the time of
delivery (T3) and at the time of wound suturing (T4). The cesarean
section rate, neonatal 1- and 5-min Apgar scores (14), and neonatal asphyxia at T4, as well
as the incidence of post-dural puncture headache (PDPH) after
anesthesia was also analyzed in the two groups.
Statistical analysis
SPSS version 22.0 statistical software (IBM Corp.)
was used to analyze and process the data. Enumeration data,
including patient age and analgesia onset time, were expressed as
the mean ± standard deviation, and the t-test was used for
comparisons between the two groups. Measurement data, including
cesarean section and neonatal asphyxia, were expressed as rates.
The Chi-squared test was used for group comparisons.
Repeated-measures analysis of variance with Bonferroni's post-hoc
test was used for comparison among multiple time-points. P<0.05
was considered to indicate a statistically significant
difference.
Results
Comparison of clinical data between
the two groups
As presented in Table
I, there was no significant difference in age, maternal body
weight, gestational age or blood test results between the two
groups (P>0.05). Thus, the two groups were comparable, ensuring
reliable results.
 | Table I.Comparison of clinical data between
two groups of maternal patients. |
Table I.
Comparison of clinical data between
two groups of maternal patients.
| Parameter | Ropivacaine group
(n=318) | Levobupivacine group
(n=297) | t or
χ2 | P-value |
|---|
| Age (years) | 28.53±4.27 | 28.04±5.15 | 1.29 | 0.20 |
| BMI (kg) | 22.16±2.84 | 21.96±3.16 | 0.83 | 0.41 |
| Gestational week | 38.54±2.04 | 38.86±2.59 | 1.71 | 0.09 |
| White blood cell
count (×109/l) | 12.08±5.07 | 12.53±5.24 | 1.08 | 0.28 |
| Red blood cell count
(×1012/l) | 7.88±2.67 | 7.53±3.74 | 1.34 | 0.18 |
| Platelet count
(×109/l) | 124.85±26.53 | 128.17±27.02 | 1.54 | 0.12 |
| Primipara |
|
| 1.28 | 0.26 |
| Yes | 227 (71.38) | 224 (75.42) |
|
|
| No | 91 (28.62) | 73 (24.58) |
|
|
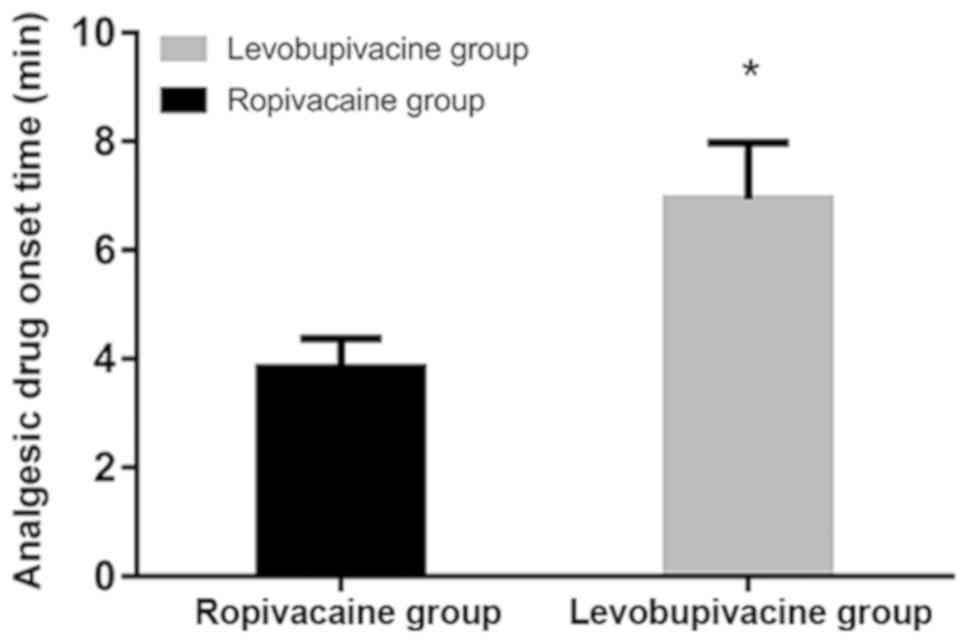
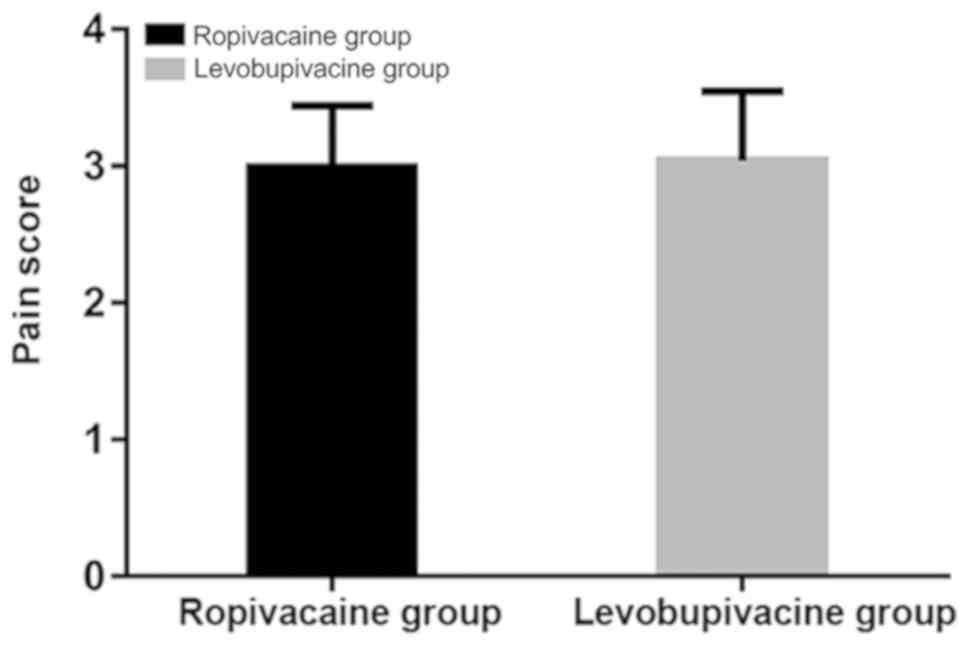
Comparison of analgesia onset time and
pain scores between the two groups
The onset time of analgesia in the ropivacaine group
(3.84±0.54 min) was significantly faster than that in the
levobupivacaine group (6.94±1.04 min; P<0.05). There was no
significant difference in pain scores between the two groups
(P>0.05; Figs. 1 and 2; Table
II).
 | Table II.Onset time and pain score of analgesic
drugs in the two groups. |
Table II.
Onset time and pain score of analgesic
drugs in the two groups.
| Parameter | Ropivacaine group
(n=318) | Levobupivacine group
(n=297) | t | P-value |
|---|
| Onset time (min) | 3.84±0.54 | 6.94±1.04 | 48.83 | <0.01 |
| Pain score at T3 | 2.99±0.45 | 3.04±0.51 | 1.29 | 0.20 |
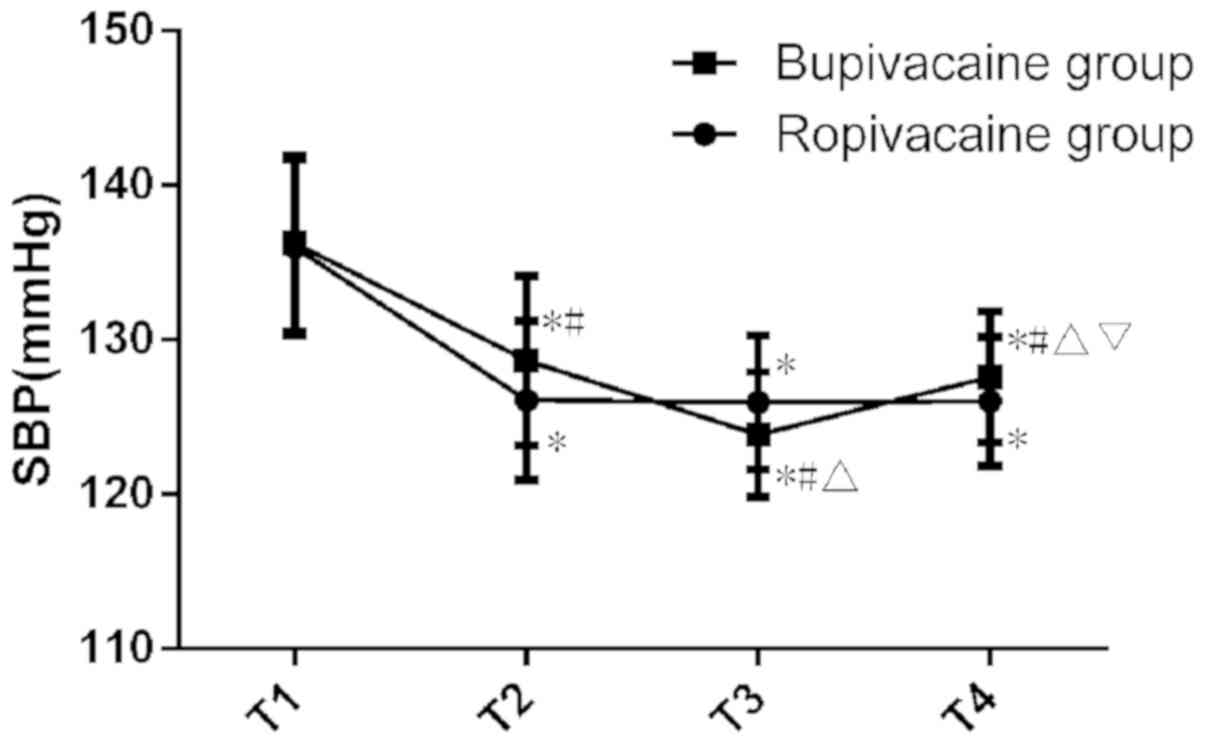
Comparison of vital signs of maternal
patients between the two groups
There was no significant difference in SBP between
the two groups at T1 (P>0.05). The SBP was significantly higher
in the levobupivacaine group compared with that in the ropivacaine
group at T2 and T4 (P<0.05), while the SBP was significantly
lower in the levobupivacaine group compared with that in the
ropivacaine group at T3 (P<0.05). Observation of the trend of
SBP in the two groups indicates that from the start of analgesia,
SBP remained stable in the ropivacaine group from T2 but steadily
decreased in the levobupivacaine group until delivery and then
slightly increased at the time-point of suturing (Fig. 3; Table
III).
 | Table III.Comparison of maternal vital signs
between the two groups at different time-points. |
Table III.
Comparison of maternal vital signs
between the two groups at different time-points.
| Parameter | T1 | T2 | T3 | T4 | F | P-value |
|---|
| SBP (mmHg) |
|
|
|
|
|
|
|
Ropivacaine group | 135.97±5.67 |
126.07±5.17a |
125.94±4.34a |
126.01±4.15a | 334.82 | <0.01 |
|
Levobupivacine group | 136.24±5.72 |
128.64±5.47a,b |
123.86±4.02a–c |
127.59±4.26a–d | 331.34 | <0.01 |
| DBP (mmHg) |
|
|
|
|
|
|
|
Ropivacaine group | 84.92±4.28 | 82.16±5.04 | 84.86±4.42 | 84.37±4.65 | 1.05 | 0.37 |
|
Levobupivacine group | 85.04±4.68 |
84.57±4.52a,b |
87.53±4.88a–c |
79.54±3.83a–d | 166.51 | <0.01 |
| HR (bpm) |
|
|
|
|
|
|
|
Ropivacaine group | 88.64±13.27 |
84.17±12.30a |
80.24±13.86a |
76.34±12.53a | 52.12 | <0.01 |
|
Levobupivacine group | 88.29±14.13 |
82.54±14.86a,b |
89.62±13.42a,b |
92.53±13.65a–d | 26.57 | <0.01 |
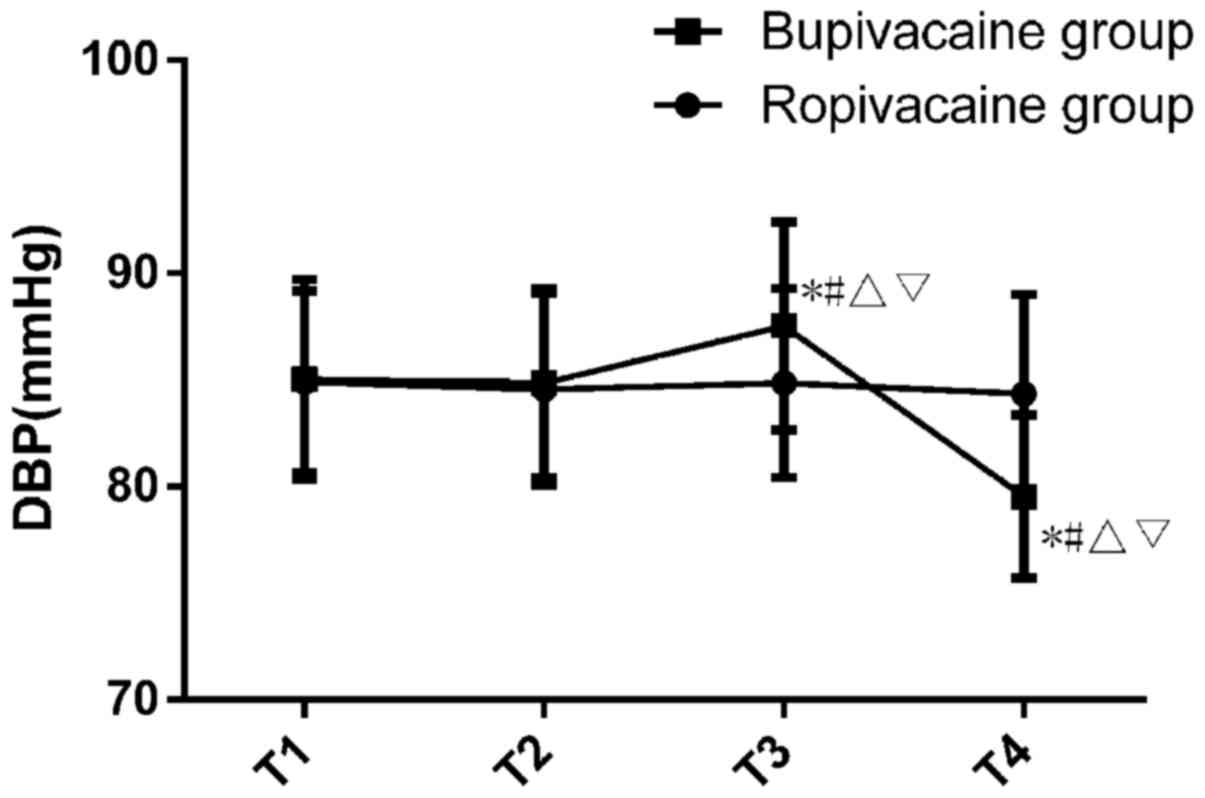
There was no significant difference in DBP between
the two groups at T1 (P>0.05). Regarding the trend of DBP
changes in the two groups, it remained stable in the ropivacaine
group with no significant change, while the DBP in the
levobupivacaine group exhibited more fluctuations (Fig. 4; Table
III).
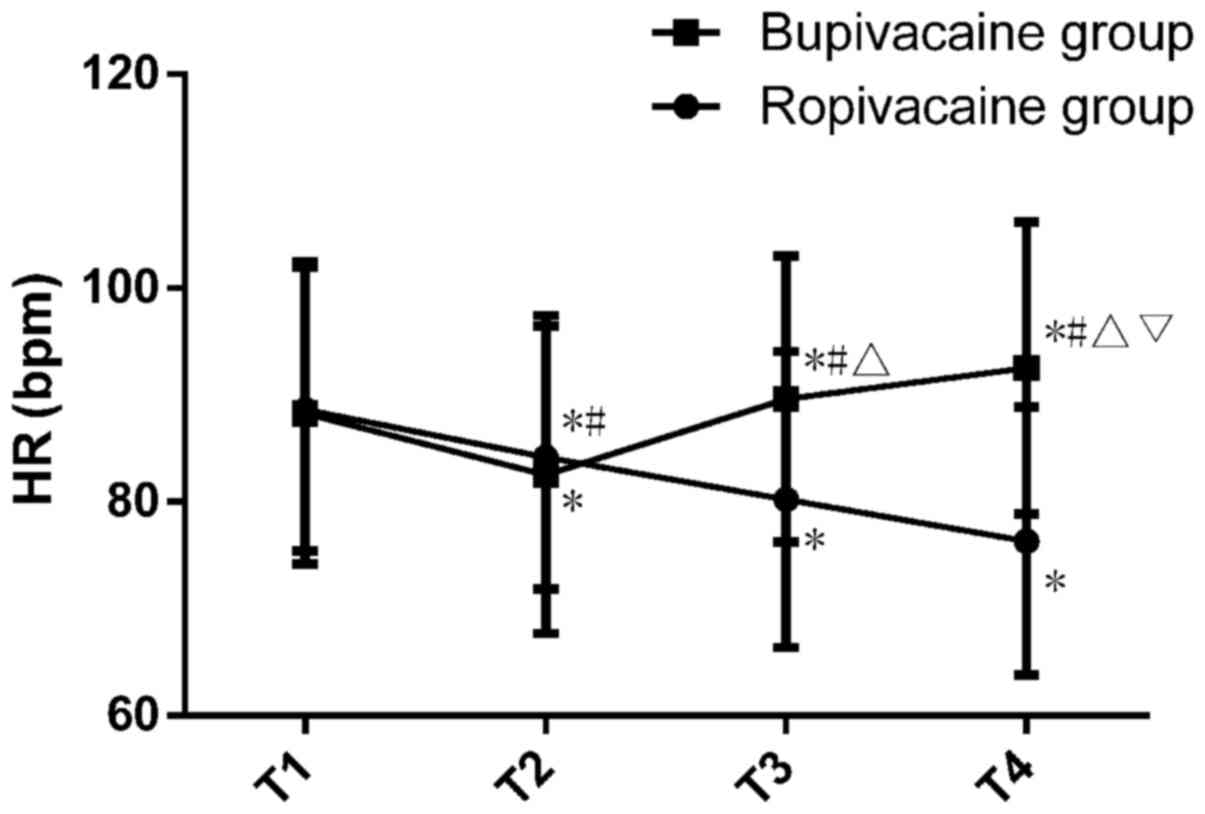
There was no significant difference in HR between
the two groups at T1 (P>0.05). The HR was significantly lower in
the levobupivacaine group compared with that in the ropivacaine
group at T2 (P<0.05), but the HR in the levobupivacaine group
was significantly higher than that in the ropivacaine group at T3
and T4 (P<0.05). Regarding the trend of HR changes in the two
groups, the ropivacaine group maintained a stable downward trend
after analgesia, while in the levobupivacaine group, the HR
increased after the onset of analgesia, while the ropivacaine group
exhibited a steady downward trend (Fig.
5; Table III).
Comparison of delivery method and
neonates
The cesarean section rate was significantly lower in
the ropivacaine group (n=13, 4.09%) compared with that in the
levobupivacaine group (n=68, 22.89%; P<0.01). The neonatal
asphyxia rate was not significantly different between the
ropivacaine group (0.63%) and the levobupivacaine group (1.01%;
P=0.60). There was no significant difference in the 1- and 5-min
Apgar scores between the two groups (P>0.05). The incidence of
PDPH in the ropivacaine group was 17.61%, and that in the
levobupivacaine group was 20.88%; the difference was not
statistically significant (P>0.05; Table IV).
 | Table IV.Comparison of pregnancy outcomes
between the two groups of patients. |
Table IV.
Comparison of pregnancy outcomes
between the two groups of patients.
| Item | Ropivacaine group
(n=318) | Levobupivacine
group (n=297) | χ2 or
t | P-value |
|---|
| Cesarean section
rate | 13 (4.09) | 68 (22.89) | 54.34 | <0.01 |
| Neonatal asphyxia
rate | 2 (0.63) | 3 (1.01) |
0.28 |
0.60 |
| Neonatal Apgar
score |
|
|
|
|
| At 1
min | 9.82±0.42 | 9.78±0.51 |
1.07 |
0.29 |
| At 5
min | 9.12±0.84 | 9.23±0.73 |
1.73 |
0.08 |
| PDPH incidence | 56 (17.61) | 62 (20.88) |
1.06 |
0.30 |
Discussion
During the vaginal delivery process, the fetus
passes through the uterus and narrow vagina, and paroxysmal
contractions and friction from the movement of the fetus stimulate
the mother's nerve endings and produce nerve impulses that pass
from the lumbar plexus to the brain, producing a sense of severe
pain during the delivery process (16,17).
Delivery does not only cause pain for the mother, but is also
associated with negative emotions, including anxiety and fear.
These also affect the vaginal delivery success rate (18,19).
Cesarean section may effectively reduce pain during childbirth, but
this traumatic surgical procedure causes greater damage and
requires a longer recovery time (20). During cesarean sections, major
bleeding may occur, which may cause secondary damage to other
organs in the abdominal cavity, and urinary tract infections or
endometriosis may develop after surgery (21). Furthermore, the fetus does not
experience extrusion through the birth canal or exposure to its
bacteria, resulting in poorer natural immunity than for infants
born vaginally. In clinical practice, vaginal delivery is
recommended if possible (22).
Reduction of pain during labor and vaginal delivery is the focus of
current clinical research. The most common safe and effective
method in clinical practice is to perform combined spinal-epidural
anesthesia during labor and to reduce pain by continuous or
intermittent injection of local anesthetic drugs through an
intraspinal catheter (23).
Furthermore, as anesthetic drugs are frequently accompanied by
adverse reactions during labor, the clinical dosage of combined
spinal-epidural anesthesia requires to be strictly controlled, and
maternal females still experience changes in their contractions
during delivery. At present, ropivacaine and levobupivacaine are
the most common analgesic drugs. However, the value of these two
analgesic drugs for labor and delivery remains controversial.
Therefore, the present study provides a reference for the use of
analgesic drugs during childbirth that may be used in future
clinical trials.
The results of the present retrospective study
indicated that the group receiving combined spinal-epidural
anesthesia with ropivacaine achieved analgesia faster than the
group receiving combined spinal-epidural anesthesia with
levobupivacaine. Compared with levobupivacaine, ropivacaine had a
faster analgesic onset time and was more beneficial, with fewer
side effects for the mother and a reduced rate of cesarean
section.
Through the combined spinal-epidural anesthesia, the
maternal labor pain, fear during childbirth and postpartum fatigue
are greatly reduced, so that the patient may be delivered
naturally. A study by Wang et al (24) indicated that nerve block anesthesia
affects the mother's ability to actively hold her breath and the
pelvic floor muscle tension is reduced, affecting the internal
rotation and head flexion of the fetus. Therefore, the probability
of the fetus becoming transverse or remaining in an
occipitoposterior position is increased. The length of labor is
prolonged and the rate of cesarean section naturally increases. In
the present study, the cesarean section rate was 24.24% in the
levobupivacaine group, which validates the above point of view.
Ropivacaine is less toxic to the heart than levobupivacaine, and it
has a lighter neuromotor block effect (25). Combined spinal-epidural anesthesia
with ropivacaine has a lesser influence on the cervical and vaginal
motor nerves in the lower uterine segment, which decreases the
birth canal resistance. The cervix opens and the fetal head
descends, thus significantly increasing the success rate of vaginal
delivery. In the present study, the cesarean section rate in the
ropivacaine group was only 4.09%. Ropivacaine has strong reactivity
with α1-acid glycoprotein in the human body (26), which may further ensure fetal safety
and reduce the need for surgery. This is also consistent with the
results of Xiao et al (27).
Ropivacaine is a long-acting amide local anesthetic with a stronger
ability to inhibit nerve conduction in pain-sensing fibers, but it
has a lesser effect on the central nervous system and the
cardiovascular system (18).
Therefore, low-concentration medications not only provide effective
analgesia but also affect other system functions to a lesser
extent. In the present study, SBP, DBP and HR all remained stable
after analgesia in the ropivacaine group and were significantly
better than those in the levobupivacaine group. There was no
significant difference in the neonatal asphyxia rate or Apgar
scores between the two groups, and the values were in accordance
with the normal rates and scores, which indicated that neither drug
affected the fetus. Thus, the two drugs have good applicability.
Regarding the incidence of PDPH after anesthesia in the two groups,
there was no significant difference between the ropivacaine group
and the levobupivacaine group, suggesting that there is no
significant difference between the effects of the two anesthetic
drugs on the mother. The two drugs are suitable for anesthesia for
delivery.
In summary, the use of combined spinal-epidural
anesthesia with ropivacaine or levobupivacaine had an excellent
analgesic effect and improved safety for childbirth. However,
compared with levobupivacaine, ropivacaine has a faster effect of
labor analgesia and a lesser impact on maternal vital signs, and
effectively reduced the rate of cesarean section; therefore, it is
worth promoting its clinical use.
However, there were certain limitations to the
present study, including the relatively young population.
Ropivacaine intolerance may occur in mothers >30 years old,
since ropivacaine has toxic effects on the cardiovascular system.
When the blood concentration is too high, cardiac conduction and
myocardial contractility may be inhibited. The bodily functions,
including blood flow, immunity and rehabilitation ability, of older
pregnant females are generally worse than those of the cohort of
the present study. Therefore, longer-term follow-up surveys on the
subjects of the present study will be performed with continuous
refinement and improvement of the assessments and analyses.
Acknowledgements
Not applicable.
Funding
This work was supported by the Science and
Technology Program of Guangzhou, China (grant no.
201709010097).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
QC conceived and designed the study and interpreted
results. WZ and JC contributed to the design of the study and the
interpretation of the experimental results. YL and HT performed
experiments, analyzed data, prepared the figures and drafted the
manuscript. HT edited and revised the manuscript for intellectual
content, grammar and spelling. All authors approved the final
version of the manuscript.
Ethics approval and consent to
participate
Each procedure was approved by the Ethics Committee
of the Guangzhou Women and Children's Medical Center (Guangzhou,
China) and conformed to the Intrapartum Care: Care of Healthy Women
and Their Babies During Childbirth guidelines of the National
Collaborating Centre for Women's and Children's Health. All of
these patients provided written informed consent.
Patients' consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kosinova M, Stourac P, Adamus M, Seidlova
D, Pavlik T, Janku P, Krikava I, Mrozek Z, Prochazka M, Klucka J,
et al: Rocuronium versus suxamethonium for rapid sequence induction
of general anaesthesia for caesarean section: Influence on neonatal
outcomes. Int J Obstet Anesth. 32:4–10. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Finnerup NB, Haroutounian S, Kamerman P,
Baron R, Bennett DL, Bouhassira D, Cruccu G, Freeman R, Hansson P,
Nurmikko T, et al: Neuropathic pain: An updated grading system for
research and clinical practice. Pain. 157:1599–1606. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sevelsted A, Stokholm J, Bønnelykke K and
Bisgaard H: Cesarean section and chronic immune disorders.
Pediatrics. 135:e92–e98. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mueller NT, Whyatt R, Hoepner L, Oberfield
S, Dominguez-Bello MG, Widen E, Hassoun A, Perera F and Rundle A:
Prenatal exposure to antibiotics, cesarean section and risk of
childhood obesity. Int J Obes (Lond). 39:665–670. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Huang L, Chen Q, Zhao Y, Wang W, Fang F
and Bao Y: Is elective cesarean section associated with a higher
risk of asthma? A meta-analysis. J Asthma. 52:16–25. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mylonas I and Friese K: Indications for
and risks of elective cesarean section. Dtsch Arztebl Int.
112:489–495. 2015.PubMed/NCBI
|
|
7
|
McDonnell NJ, Paech MJ, Muchatuta NA,
Hillyard S and Nathan EA: A randomised double-blind trial of
phenylephrine and metaraminol infusions for prevention of
hypotension during spinal and combined spinal-epidural anaesthesia
for elective caesarean section. Anaesthesia. 72:609–617. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kristensen K and Henriksen L: Cesarean
section and disease associated with immune function. J Allergy Clin
Immunol. 137:587–590. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ngan Kee WD, Lee SW, Ng FF, Tan PE and
Khaw KS: Randomized double-blinded comparison of norepinephrine and
phenylephrine for maintenance of blood pressure during spinal
anesthesia for cesarean delivery. Anesthesiology. 122:736–745.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Puri GD, Mathew PJ, Biswas I, Dutta A,
Sood J, Gombar S, Palta S, Tsering M, Gautam PL, Jayant A, et al: A
multicenter evaluation of a closed-loop anesthesia delivery system:
A randomized controlled trial. Anesth Analg. 122:106–114. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li C, Li Y, Wang K and Kong X: Comparative
evaluation of remifentanil and dexmedetomidine in general
anesthesia for cesarean delivery. Med Sci Monit. 21:3806–3813.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Murouchi T, Iwasaki S and Yamakage M:
Quadratus lumborum block: Analgesic effects and chronological
ropivacaine concentrations after laparoscopic surgery. Reg Anesth
Pain Med. 41:146–150. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kathuria S, Gupta S and Dhawan I:
Dexmedetomidine as an adjuvant to ropivacaine in supraclavicular
brachial plexus block. Saudi J Anaesth. 9:148–154. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
National Collaborating Centre for Women's
and Children's Health (UK), . Intrapartum care: Care of healthy
women and their babies during childbirth. London. (RCOG Press).
2007.
|
|
15
|
Tashjian RZ, Hung M, Keener JD, Bowen RC,
McAllister J, Chen W, Ebersole G, Granger EK and Chamberlain AM:
Determining the minimal clinically important difference for the
American Shoulder and Elbow Surgeons score, simple shoulder test,
and visual analog scale (VAS) measuring pain after shoulder
arthroplasty. J Shoulder Elbow Surg. 26:144–148. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dong C, Hu L, Liang F and Zhang S: Effects
of electro-acupuncture on labor pain management. Arch Gynecol
Obstet. 291:531–536. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Makvandi S, Latifnejad Roudsari R, Sadeghi
R and Karimi L: Effect of birth ball on labor pain relief: A
systematic review and meta-analysis. J Obstet Gynaecol Res.
41:1679–1686. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li Y, Hu C, Fan Y, Wang H and Xu H:
Epidural analgesia with amide local anesthetics, bupivacaine, and
ropivacaine in combination with fentanyl for labor pain relief: A
meta-analysis. Med Sci Monit. 21:921–928. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Stourac P, Adamus M, Seidlova D, Pavlik T,
Janku P, Krikava I, Mrozek Z, Prochazka M, Klucka J, Stoudek R, et
al: Low-dose or high-dose rocuronium reversed with neostigmine or
sugammadex for cesarean delivery anesthesia: A randomized
controlled noninferiority trial of time to tracheal intubation and
extubation. Anesth Analg. 122:1536–1545. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ripollés Melchor J, Espinosa Á, Martínez
Hurtado E, Casans Francés R, Navarro Pérez R, Abad Gurumeta A and
Calvo Vecino JM: Colloids versus crystalloids in the prevention of
hypotension induced by spinal anesthesia in elective cesarean
section. A systematic review and meta-analysis. Minerva Anestesiol.
81:1019–1030. 2015.PubMed/NCBI
|
|
21
|
Visser GH: Women are designed to deliver
vaginally and not by cesarean section: An obstetrician's view.
Neonatology. 107:8–13. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Happel-Parkins A and Azim KA: At pains to
consent: A narrative inquiry into women's attempts of natural
childbirth. Women Birth. 29:310–320. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sawhney M, Mehdian H, Kashin B, Ip G, Bent
M, Choy J, McPherson M and Bowry R: Pain after unilateral total
knee arthroplasty: A prospective randomized controlled trial
examining the analgesic effectiveness of a combined adductor canal
peripheral nerve block with periarticular infiltration versus
adductor canal nerve block alone versus periarticular infiltration
alone. Anesth Analg. 122:2040–2046. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wang LZ, Liu X, Zhang YF, Hu XX and Zhang
XM: Addition of fentanyl to the ultrasound-guided transversus
abdominis plane block does not improve analgesia following cesarean
delivery. Exp Ther Med. 11:1441–1446. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jadon A, Dixit S, Kedia SK, Chakraborty S,
Agrawal A and Sinha N: Interscalene brachial plexus block for
shoulder arthroscopic surgery: Prospective randomised controlled
study of effects of 0.5% ropivacaine and 0.5% ropivacaine with
dexamethasone. Indian J Anaesth. 59:171–776. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Song J, Li L, Yu P, Gao T and Liu K:
Preemptive scalp infiltration with 0.5% ropivacaine and 1%
lidocaine reduces postoperative pain after craniotomy. Acta
Neurochir (Wien). 157:993–998. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Xiao F, Xu WP, Zhang YF, Liu L, Liu X and
Wang LZ: The dose-response of intrathecal ropivacaine
co-administered with sufentanil for cesarean delivery under
combined spinal-epidural anesthesia in patients with scarred
uterus. Chin Med J (Engl). 128:2577–2582. 2015. View Article : Google Scholar : PubMed/NCBI
|