Introduction
Osteonecrosis is defined as necrosis of the bone
marrow and trabecular bones due to the lack of sufficient blood
supply (1). The occurrence of
osteonecrosis in patients with systemic lupus erythematosus (SLE)
was first reported in 1960 (2) and
has been frequently reported since, with an incidence ranging from
3 to 30% (3). Many risk factors have
been reported to be involved in the development of osteonecrosis in
patients with SLE, including trauma a history of autoimmune
connective tissue diseases, renal diseases, coagulation disorders,
other hematological disorders, metabolic disorders, infections,
alcohol abuse, smoking and the use of corticosteroids or cytotoxic
drugs (1). Since asymptomatic
osteonecrosis may remain undetected, its true prevalence could be
much higher than reported. The estimation of the overall incidence
rate of osteonecrosis in SLE patients is misleading as patients are
mostly treated with glucocorticoids, which may also result in the
development of osteonecrosis. A previous Meta-analysis demonstrates
a significant increased risk of osteonecrosis in SLE patients with
high disease activity scores (4).
Although osteonecrosis is frequently reported in cases of SLE,
multifocal lesions involving more than three anatomical sites are
unusual (5–16). In the present case report, a case of
multifocal necrosis affecting all limbs of a patient with SLE is
described.
Case report
The patient was a 22-year-old woman diagnosed with
SLE in June 2010 at The Second Hospital Affiliated to Jilin
University and confirmed at the Third Hospital Affiliated to Jilin
University. The diagnosis of SLE was made according to the
following symptoms and laboratory tests: Fever of unknown origin,
malar rash, immunologic disorder and positive antinuclear
antibodies. Following diagnosis, the patient received regular oral
treatment with 12 mg/day methylprednisolone and 200 mg/day
hydroxychloroquine, and the disease was initially well controlled
by monitoring immunologic function via immunity tests including
turbidinetric inhibition immunoassay (including Immunoglobulin
(Ig)G, IgA, IgM, C3 and C4) and assessing the levels of antinuclear
antibodies. The disease is considered to be controlled when serum
levels of immunoglobin and complement return to normal levels.
However, in February 2011, the patient reported bilateral pain and
restricted hip movement, and 4 months later, the patient developed
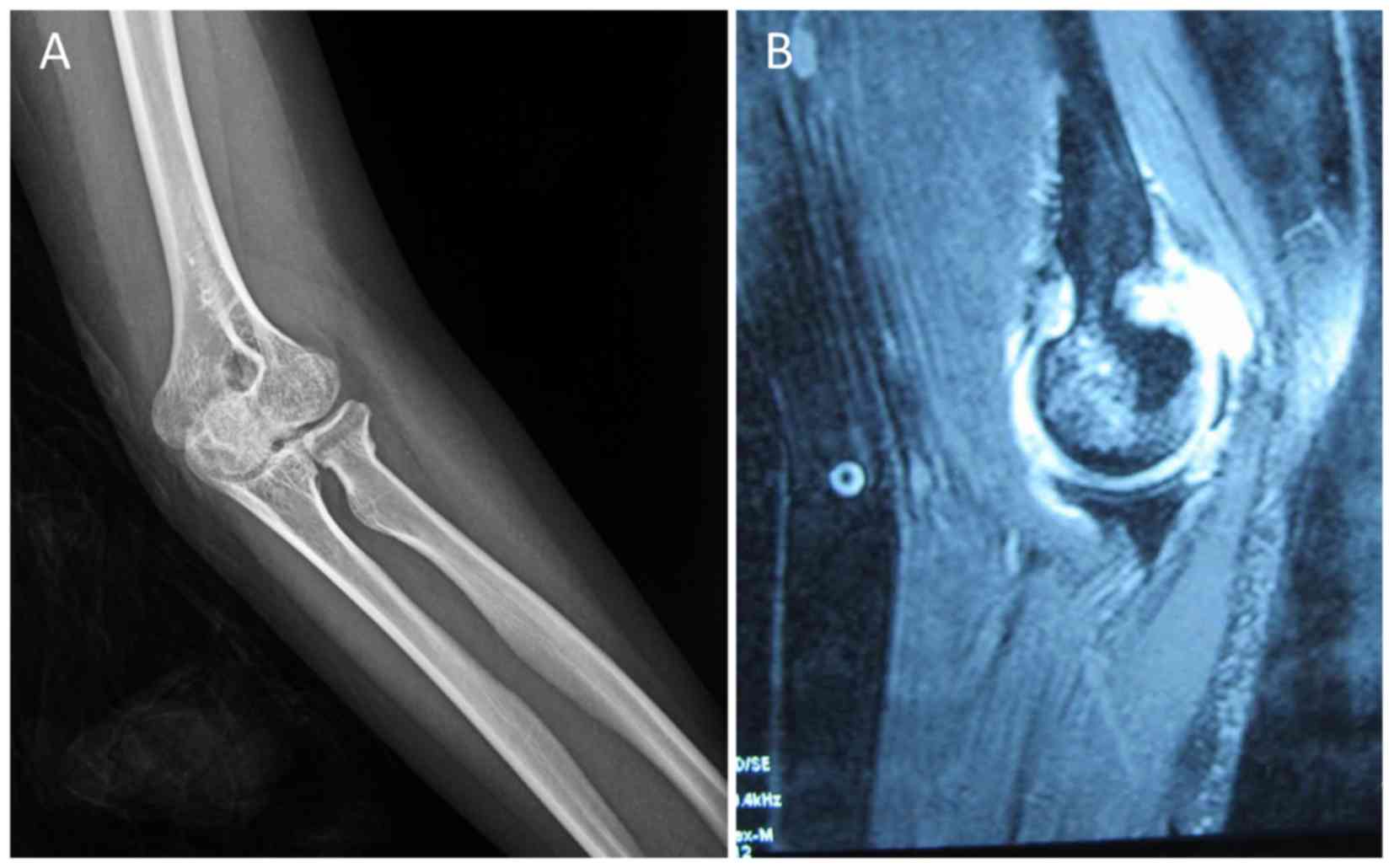
similar symptoms in the elbows. Plain radiographs of the elbows
indicated bilateral osteonecrosis in the distal segments of the
humerus and femoral heads (Fig. 1A).
In February 2012, the patient developed pain in the right knee. Due
to considerable worsening of the symptoms, the patient was
hospitalized on May 29, 2012. On examination, the patient's hip
movement was observed to be severely restricted. For the right and
left hips, the range of movement was 120 and 130° for flexion; 30
and 40° for adduction; 20 and 30° for abduction; and 0° for
extension, pronation and supination, respectively. Furthermore, the
range of movement in the left and right elbows was 35–155° and
25–160°, respectively. Magnetic resonance imaging (MRI) revealed
signs of multifocal osteonecrosis in the distal segments of the
humerus and femoral heads bilaterally, and in the distal segment of
the femur and the proximal segment of the tibia on the right side
of the patient (Fig. 1B). No
evidence of narrowing of the joint space or damage to the joint
surface was observed in the elbows or knee joints. Laboratory tests
of antinuclear antibodies were performed using an indirect
immunofluorescence assay (17),
which revealed that the patient was highly positive for anti-Ro52,
anti-Sjögren's syndrome type A and anti-nuclear
ribonucleoprotein/Sm antibodies. Furthermore, the level of
hypersensitive C-reactive protein was 1.36 mg/l (normal range,
0–3.5 mg/l), the erythrocyte sedimentation rate was mildly elevated
at 38 mm/h, (normal range, 0–15 mm/h) and the serum complement C3
and C4 levels were 1.0 g/l (normal range, 0.9–1.8 g/l) and 0.2 g/l
(normal range, 0.1–0.4 g/l), respectively. On June 4, 2012, the
patient underwent total hip arthroplasty of the right side and
drilling decompression of the right femur and tibia. The surgery
was successful and recovery was uneventful. Thereafter, the
patient's previous treatment was continued, and the patient has
remained stable since the surgery. The patient was followed up
every 6 months at the Department of Rheumatology and Immunology of
the First Hospital of Jilin University (Jilin, China). The
condition of SLE was stable according to the results of immune
tests. Multiple bone infarction and total hip replacement was
monitored at the Department of Bone and Joint Surgery of the First
Hospital of Jilin University (Jilin, China) once a year, with no
apparent pain symptoms being reported during follow-up. The last
follow-up was performed in April 2018. Informed consent was
obtained from the patient for the report of the present case.
Discussion
Osteonecrosis is characterized by the death of bone
marrow and trabecular bone tissue due to disruption of the blood
supply to bone tissues (2). SLE is
the most common rheumatic disease that causes osteonecrosis
(18). Traumatic causes of
osteonecrosis may lead to the displacement of bone fragments,
resulting in impaired blood supply and ischemia of the affected
bone tissue (19). However, when
osteonecrosis occurs due to systemic disease, the pathogenesis
involves disruption of the blood supply to the bone, which leads to
a sequence of events, including localized hyperemia,
demineralization, trabecular thinning and collapse of the bony
architecture (20). Bone infarcts
usually remain clinically asymptomatic and so are frequently only
recognized by characteristic radiographic changes in the later
stages, which include dense, irregular shadows resembling puffs of
smoke in the metaphyso-diaphyseal regions of the long bones
(20). MRI examination is helpful in
such cases since it enables the early detection of bone infarcts;
these are observed as areas of low signal intensity with irregular
margins and dispersed areas of increased signal intensity that
indicate the presence of fat (21).
In the present case, radiographic examination was performed for the
evaluation of the initial symptoms of joint pain. The results
showed a slightly increase in density and osteonecrosis was under
suspicion. Subsequent MRI examination provided definitive
information that helped to establish the diagnosis of
osteonecrosis.
The risk factors implicated in the development of
osteonecrosis in patients with SLE include trauma and a history of
autoimmune connective tissue diseases, renal diseases, coagulation
and other hematological disorders, metabolic disorders, infections,
alcohol abuse, smoking, and the use of corticosteroids and
cytotoxic drugs (1). With regard to
the pathogenesis of multifocal osteonecrosis in SLE, the use of
corticosteroids and cytotoxic drugs is the most relevant factor
(19). The association between
osteonecrosis and the use of corticosteroids is evident from the
observation that the condition is common in patients with SLE who
have been treated with corticosteroids and extremely rare in those
naïve to corticosteroid use (22,23).
Notably, previous studies have shown that the duration, total
cumulative dose and highest daily dose of corticosteroids are
independent factors associated with the occurrence of osteonecrosis
(24–26). In the present case, the development
of multifocal osteonecrosis may be attributed to the administration
of high-dose methylprednisolone for a period of more than 1
year.
The anti-inflammatory and immunosuppressive effects
of corticosteroids are mediated via reductions in the expression of
cytokines and adhesion molecules; inhibition of the migration and
access of leukocytes to the site of inflammation; and disruption of
the functioning of leukocytes, fibroblasts and endothelial cells
(27). In addition, corticosteroids
inhibit osteoblastic activity, leading to decreased bone formation,
loss of bone mineral density and increased risk of fracture
(28). Bone loss begins when
corticosteroid treatment is initiated and peaks at 6 months of
therapy; it decreases when corticosteroid use is discontinued
(28). Loss of bone tissue mainly
occurs in regions with a high content of trabecular tissue, such as
the vertebrae (29). Corticosteroids
may increase the size and number of intramedullary lipocytes; this
raises the pressure within the bone marrow, which results in
vascular compression and reduced perfusion of the bone tissue,
thereby triggering bone ischemia and infarct (30). Evidence supporting this hypothesis
has been obtained from MRI study, which has shown that compared
with healthy controls, patients with SLE have a higher percentage
of bone-marrow fat and exhibit a higher degree of conversion of
hematopoietic marrow into fatty bone marrow (31). The percentage of fatty marrow has
been demonstrated to correlate with the mean daily dose of
corticosteroids and the presence of osteonecrosis (31). Sequential MRI scans of patients with
SLE and osteonecrosis have indicated the presence of extensive
bone-marrow edema (32). This is
further supported by the evident relief of the symptoms of
osteonecrosis following core decompression.
The treatment of osteonecrosis in patients with SLE
is similar to that of osteonecrosis in general, as is the outcome
of the treatment. The main therapeutic approaches for osteonecrosis
are medical management and surgery (22,23).
Small and asymptomatic lesions may heal spontaneously or remain
stable without progressing or causing significant joint damage.
However, symptomatic lesions require a combined approach involving
medical and surgical management. The medical management of
osteonecrosis comprises the administration of analgesics, physical
therapy, and the use of devices to prevent muscle atrophy and allow
non-weight bearing movement (23,32).
Cases in which osteonecrosis affects the femoral heads often
require total hip arthroplasty (22,23), as
in the present case. Another widely used approach in the management
of the early stages of osteonecrosis is core decompression, which
aims to reduce the intramedullary pressure at the osteonecrotic
lesions, thereby improving perfusion of the ischemic bone (33). In the current case, core
decompression was performed for the right femur and tibia, where
the lesions were less severe.
In conclusion, the present case highlights the
importance of conducting a thorough investigation for multifocal
osteonecrosis in patients with SLE and pain in multiple joints. On
the basis of the present case, MRI is suggested to be the
diagnostic modality of choice for osteonecrosis and more
informative than radiography.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
SS acquired the data and wrote the manuscript; QW
analysed and interpreted the data, and revised the manuscript; YG
collected the data, and conceived and supervised the study; XQ and
JL conceived and designed the present study, and revised the
manuscript for important intellectual content. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Informed consent was obtained from the patient for
the report of the present case.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Assouline-Dayan Y, Chang C, Greenspan A,
Shoenfeld Y and Gershwin ME: Pathogenesis and natural history of
osteonecrosis. Semin Arthritis Rheum. 32:94–124. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dubois EL and Cozen L: Avascular (aseptic)
bone necrosis associated with systemic lupus erythematosus. JAMA.
174:966–971. 1960. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Abu-Shakra M, Buskila D and Shoenfeld Y:
Osteonecrosis in patients with SLE. Clin Rev Allergy Immunol.
25:13–24. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang K, Zheng Y, Jia J, Ding J and Wu Z:
Systemic lupus erythematosus patients with high disease activity
are associated with accelerated incidence of osteonecrosis: A
systematic review and meta-analysis. Clin Rheumatol. 37:5–11. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cavallasca JA, Laborde HA, Araujo MB and
Nasswetter GG: Multiple avascular necrosis in a patient with
systemic lupus erythematosus/systemic sclerosis overlap syndrome.
Clin Rheumatol. 24:406–408. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Darlington LG: Osteonecrosis at multiple
sites in a patient with systemic lupus erythematosus. Ann Rheum
Dis. 44:65–66. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fajardo-Hermosillo LD, López-López L,
Nadal A and Vilá LM: Multifocal osteonecrosis in systemic lupus
erythematosus: Case report and review of the literature. BMJ Case
Rep. 2013:bcr20130089802013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fishel B, Caspi D, Eventov I, Avrahami E
and Yaron M: Multiple osteonecrotic lesions in systemic lupus
erythematosus. J Rheumatol. 14:601–604. 1987.PubMed/NCBI
|
|
9
|
García-Miguel J, Calvet-Fontova J,
Maymó-Guarsch J and Carbonell-Abelló J: Multifocal osteonecrosis in
a patient with systemic lupus erythematosus. Med Clin (Barc).
127:2762006.(In Spanish). View
Article : Google Scholar
|
|
10
|
Greenhagen RM, Crim BE, Shinabarger AB and
Burns PR: Bilateral osteonecrosis of the navicular and medial
cuneiform in a patient with systemic lupus erythematosus: A case
report. Foot Ankle Spec. 5:180–184. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Guillaume MP, Brandelet B and Peretz A:
Unusual high frequency of multifocal lesions of osteonecrosis in a
young patient with systemic lupus erythematosus. Br J Rheumatol.
37:1248–1249. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lawal YZ, Ogirima MO, Dahiru IL, Maitama
MI, Ejagwulu FS and Abubakar K: Bilateral osteonecrosis of the
femoral heads in a patient with systemic lupus erythematosus. Ann
Afr Med. 10:64–65. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Outwater E, Oates E and Sarno RC:
Bilateral distal tibial osteonecrosis in systemic lupus
erythematosus. AJR Am J Roentgenol. 152:895–896. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Salesi M, Karimifar M, Mottaghi P,
Sayedbonakdar Z and Karimzadeh H: A case of SLE with bilateral
osteonecrosis of femoral heads and bone infarct in distal of femur.
Rheumatol Int. 30:527–529. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Seymour MW, Mitchell AW and
Mackworth-Young CG: Bilateral calcaneal osteonecrosis in a patient
with systemic lupus erythematosus. Rheumatology (Oxford).
44:5862005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shimizu M, Tokuhisa Y, Ishikawa S, Ueno K,
Yokoyama T and Yachie A: Multiple osteonecrosis in a patient with
juvenile systemic lupus erythematosus. J Clin Rheumatol.
19:1602013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bossuyt X, Frans J, Hendrickx A,
Godefridis G, Westhovens R and Mariën G: Detection of anti-SSA
antibodies by indirect immunofluorescence. Clin Chem. 50:2361–2369.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Abeles M, Urman JD and Rothfield NF:
Aseptic necrosis of bone in systemic lupus erythematosus.
Relationship to corticosteroid therapy. Arch Intern Med.
138:750–754. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Caramaschi P, Biasi D, Dal Forno I and
Adami S: Osteonecrosis in systemic lupus erythematosus: An early,
frequent, and not always symptomatic complication. Autoimmune Dis.
2012:7252492012.PubMed/NCBI
|
|
20
|
Zizic TM: Osteonecrosis. Curr Opin
Rheumatol. 3:481–489. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Halland AM, Klemp P, Botes D, Van Heerden
BB, Loxton A and Scher AT: Avascular necrosis of the hip in
systemic lupus erythematosus: The role of magnetic resonance
imaging. Br J Rheumatol. 32:972–976. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hungerford DS and Zizic TM II: The
treatment of ischemic necrosis of bone in systemic lupus
erythematosus. Medicine (Baltimore). 59:143–148. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ehmke TA, Cherian JJ, Wu ES, Jauregui JJ,
Banerjee S and Mont MA: Treatment of osteonecrosis in systemic
lupus erythematosus: A review. Curr Rheumatol Rep. 16:4412014.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mont MA, Glueck CJ, Pacheco IH, Wang P,
Hungerford DS and Petri M: Risk factors for osteonecrosis in
systemic lupus erythematosus. J Rheumatol. 24:654–662.
1997.PubMed/NCBI
|
|
25
|
Zhu KK, Xu WD, Pan HF, Zhang M, Ni J, Ge
FY and Ye DQ: The risk factors of avascular necrosis in patients
with systemic lupus erythematosus: A meta-analysis. Inflammation.
37:1852–1864. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sayarlioglu M, Yuzbasioglu N, Inanc M,
Kamali S, Cefle A, Karaman O, Onat AM, Avan R, Cetin GY, Gul A, et
al: Risk factors for avascular bone necrosis in patients with
systemic lupus erythematosus. Rheumatol Int. 32:177–182. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zen M, Canova M, Campana C, Bettio S,
Nalotto L, Rampudda M, Ramonda R, Iaccarino L and Doria A: The
kaleidoscope of glucorticoid effects on immune system. Autoimmun
Rev. 10:305–310. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
De Nijs RN: Glucocorticoid-induced
osteoporosis: A review on pathophysiology and treatment options.
Minerva Med. 99:23–43. 2008.PubMed/NCBI
|
|
29
|
Weldon D: The effects of corticosteroids
on bone: Osteonecrosis (avascular necrosis of the bone). Ann
Allergy Asthma Immunol. 103:91–97. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zizic TM, Marcoux C, Hungerford DS,
Dansereau JV and Stevens MB: Corticosteroid therapy associated with
ischemic necrosis of bone in systemic lupus erythematosus. Am J
Med. 79:596–604. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Vande Berg BC, Malghem J, Lecouvet FE,
Devogelaer JP, Maldague B and Houssiau FA: Fat conversion of
femoral marrow in glucocorticoid-treated patients: A
cross-sectional and longitudinal study with magnetic resonance
imaging. Arthritis Rheum. 42:1405–1411. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mont MA and Jones LC: Management of
osteonecrosis in systemic lupus erythematosus. Rheum Dis Clin North
Am. 26279–309. (vi)2000. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Marker DR, Seyler TM, McGrath MS, Delanois
RE, Ulrich SD and Mont MA: Treatment of early stage osteonecrosis
of the femoral head. J Bone Joint Surg Am. 90 (Suppl 4):S175–S187.
2008. View Article : Google Scholar
|