Introduction
Central venous catheter (CVC) is frequently used for
temporary or permanent vascular access for hemodialysis, leading to
potential complications, including local injury, hematoma,
pneumothorax, thrombosis, vein stenosis and catheter-associated
infections (1). Central venous
perforation is a rare but serious complication that may lead to
massive hemorrhage, hemorrhagic shock (HS) and even death.
Treatment methods for CVC perforation have varied in the past
decade and have included open surgical repair (2–6) and
endovascular stent grafting repair (7–9). The
present study reports on a case of left brachiocephalic vein (BCV)
perforation into the mediastinum and pleura leading to massive
hemothorax and HS that was successfully treated by coil and glue
embolization of the sinus tract during digital subtraction
angiography (DSA) after effective anti-shock therapy.
Case report
The present study reported a case of left BCV
perforation that was diagnosed at the First Affiliated Hospital of
the University of Science and Technology of China (USTC; Hefei,
China). The present study was approved by the Ethics Committee of
The First Affiliated Hospital of the USTC and informed consent was
also obtained from the patient. A 64-year-old female with a 15-year
history of hypertension underwent left forearm arteriovenous
fistula (AVF) surgery to treat stage-V chronic kidney disease (CKD)
five years previously. One month prior to presentation at our
department on June 8, 2017, the patient had a fistula obstruction
and a local hospital placed a temporary catheter in the patient's
right femoral vein for hemodialysis. However, the inserted catheter
caused occlusion of the right BCV. Review of the patient's medical
history revealed that she received a long-term hemodialysis
catheter (hemosplit 14.5F/23 cm; BARD) via the left internal
jugular vein (LIJV) two days prior to occurrence of HS. LIJV
punctures using the Seldinger technique were performed under local
anesthesia, followed by smooth introduction and positioning of the
guidewires in the left IJV to a level just below the diaphragm.
After dilator and guidewire removal, the catheters were introduced,
followed by removal of the peel-away sheaths. When placing the
catheters, the surgeon felt a marked resistance. Furthermore, the
patient reported mild pain and discomfort in the left chest during
the catheterization process. After the completion of
catheterization, hard venous blood was aspirated. The surgeon
considered the possibility of acute thrombosis. A total of 200,000
units of urokinase were injected into the catheter, revealing
obstructed flow after 20 min. Subsequently, the patient developed
symptoms of palpitations, chest stuffiness and cold sweats.
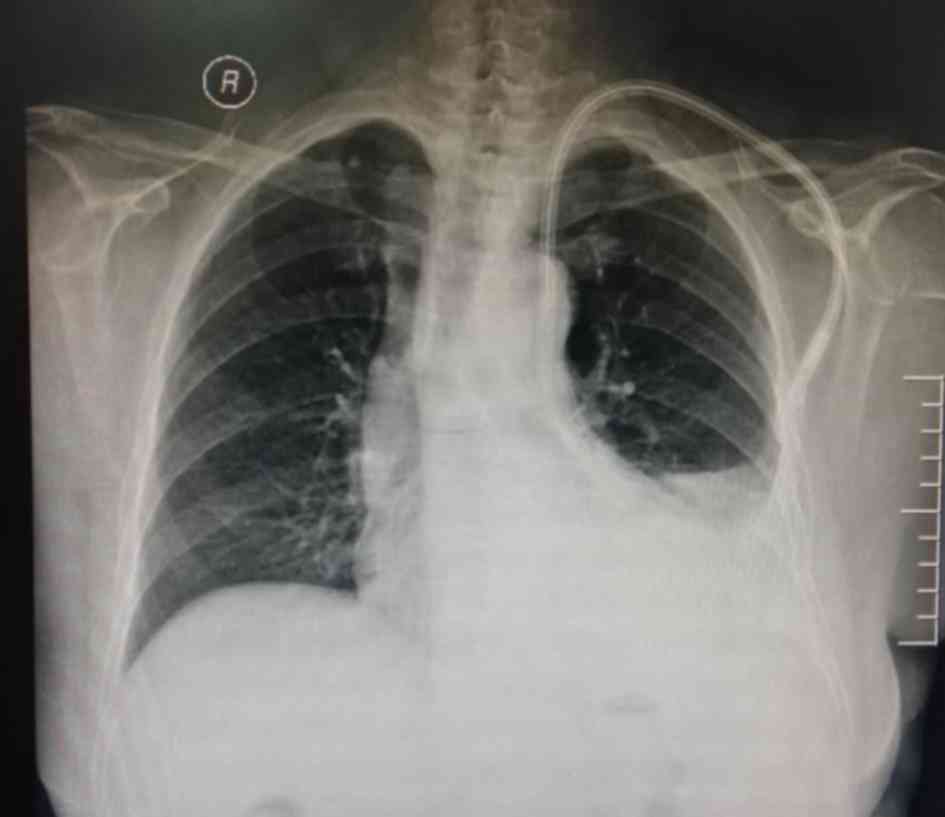
Thoracic anteroposterior radiography at the emergency department
indicated that the body segment of the dialysis catheter was
located on the left side of the mediastinum (Fig. 1). Therefore, the patient was rapidly
transferred to our hospital. Upon admission, general and systemic
examinations were unremarkable except for pectoralgia on the left
side and chest tightness accompanied by asthma or breathing
difficulties/obstruction, an elevated heart rate (115 beats/min)
and hypotension (blood pressure, 82/45 mmHg). Laboratory
investigations revealed a red blood cell count of
1.72×1012/l (normal range: 3.5~5.5×1012/l)
and a hemoglobin level of 59 g/l (normal range: 110–150 g/l). A
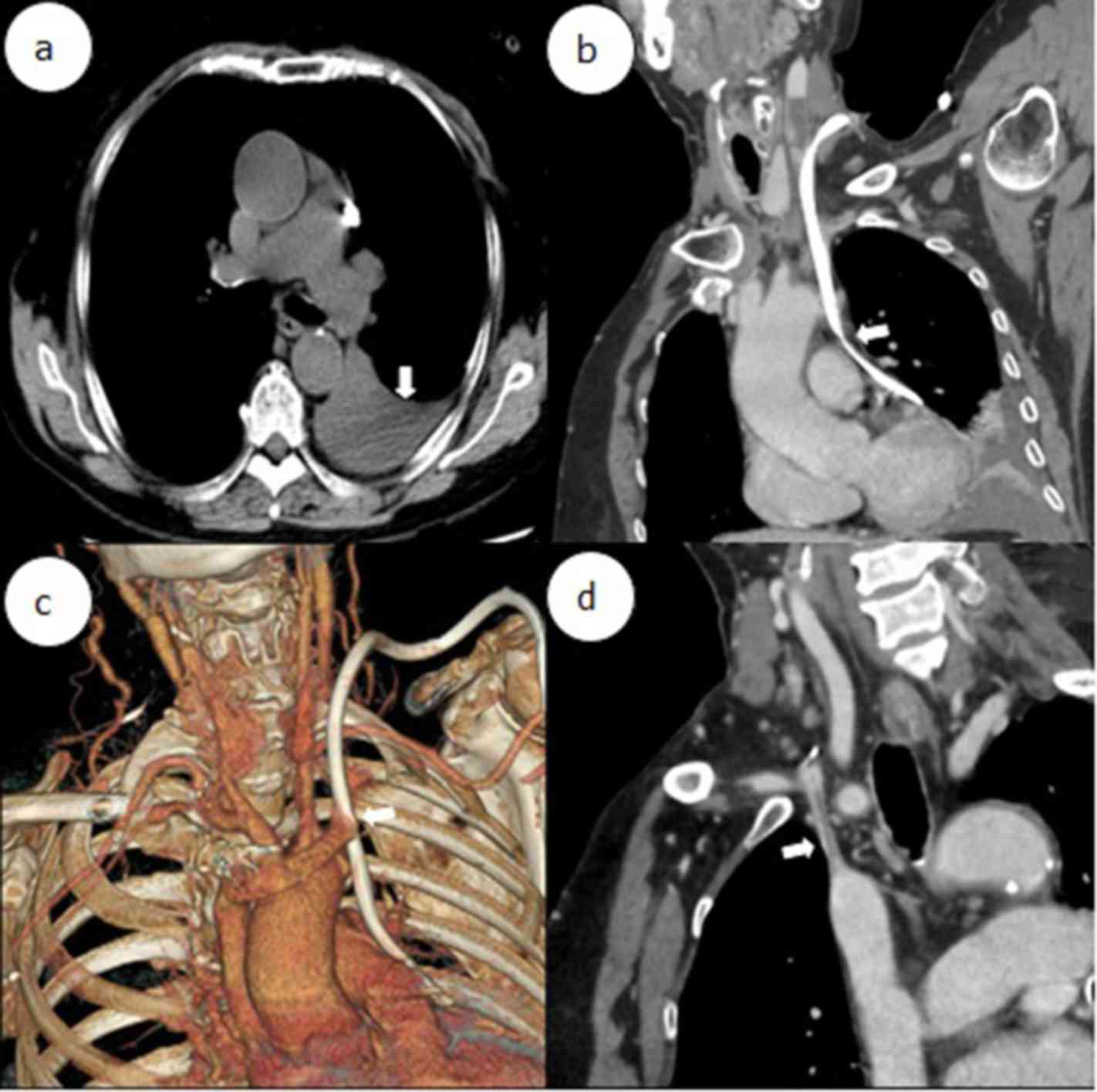
contrast-enhanced chest computed tomography scan revealed that the
left BCV was perforated through the mediastinum and entered the
left thoracic cavity, with the appearance of pleural effusion
(Fig. 2a-d). A pleural puncture was
performed to extract nonclotting blood. According to the above
symptoms, the patient was diagnosed with central venous perforation
and HS. The patient immediately received anti-shock treatment by
fluid infusion and blood transfusion. The patient was given 6 U
total transfused red blood cells and 800 ml fresh frozen plasma.
Subsequently, the patient's blood pressure rose to 90–100/50–60
mmHg and the heart rate was reduced to 100–110 beats/min. However,
there were obvious symptoms of pectoralgia, which was aggravated
when breathing and coughing. Since the patient had evidence of a
bleeding disorder with unstable vital signs, it was decided to
perform intracavitary treatment to repair the damaged blood
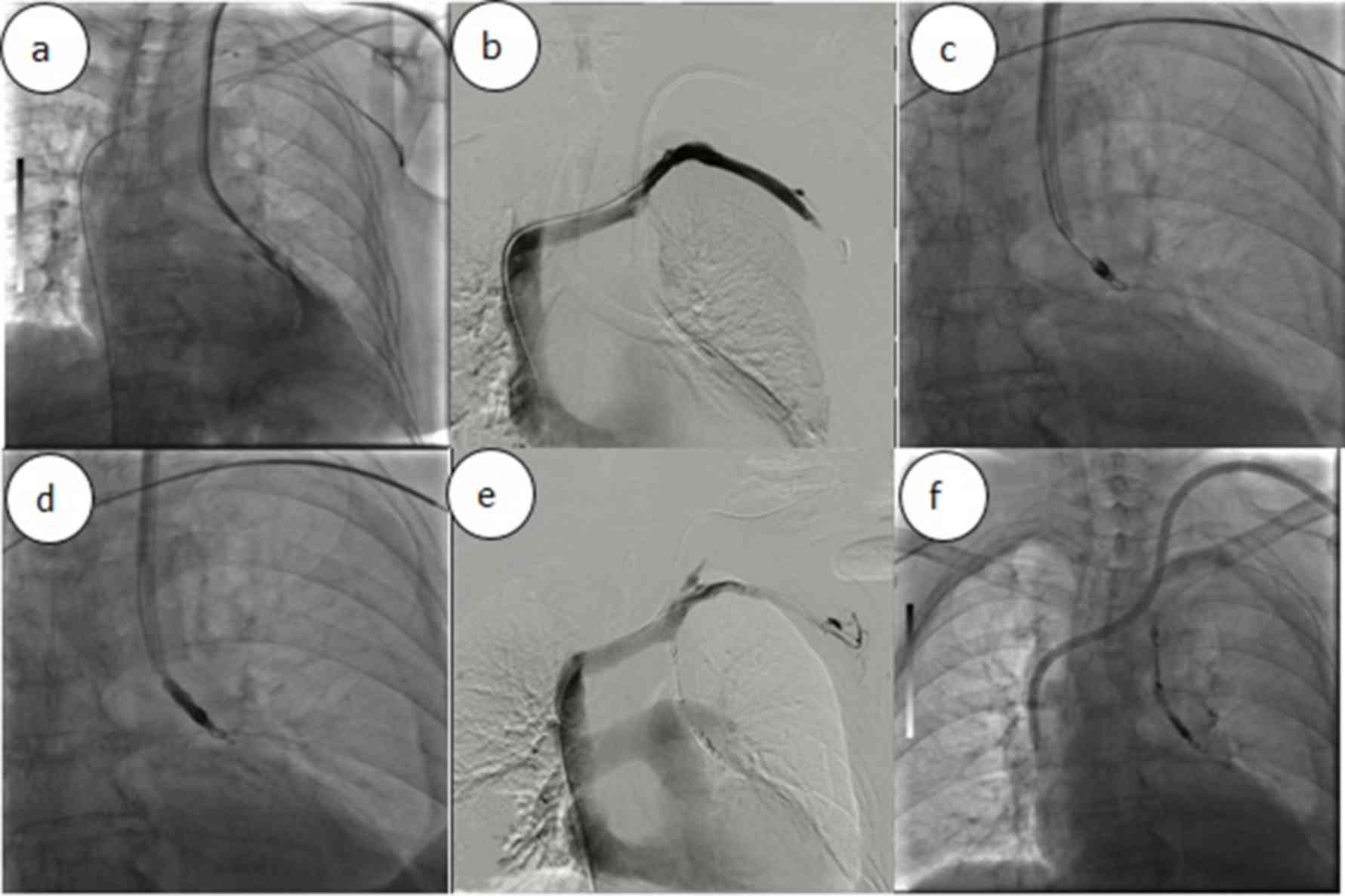
vessels. A total of 10 µl non-ionic contrast medium (Iodixanol; 27
g/100 ml; Amersham Health) was injected into the dialysis catheter,
and X-ray fluoroscopy indicated that the contrast agent entered the
left thoracic cavity through the front of the dialysis catheter and
quickly dispersed (Fig. 3).
A puncture needle was inserted into the left femoral
vein, which was implanted with the 10F catheter sheath. Angiography
revealed that steady blood flow was present in the left subclavian
vein (LSV), cephalic vein and superior vena cava with no obvious
leakage of the contrast agent. A guidewire (RFxPA35263M; 260 cm;
Terumo Corp.) was left in the LSV to seal the sinus groove in the
case of unsuccessful sinus embolization. A 4F catheter (Yashiro;
Terumo Corp.) was inserted into the sinus canal through the artery
end of the original dialysis catheter, followed by a 3F
microcatheter (Progreat; Terumo Corp.). A total of four coils (6×50
mm, Fibered Platinum Coil; Boston Scientific) were then anchored at
the fistula through the catheter. Cyanoacrylates
[n-butyl-2-cyanoacrylate (NBCA)/n-octyl cyanoacrylate; Fuaile] were
mixed with lipiodol (Guerbet) at a proportion of 1:2 and 1.5 ml was
injected under fluoroscopic guidance. The long-term dialysis
catheter was then replaced at the original puncture site under
fluoroscopy and placed in the superior vena cava. Post-operative
blood transfusion, fluid infusion and chest drainage were
continued. The HGB level increased to 103 g/l on the third day
after the operation, and the patient was discharged from the
hospital. The patient was followed up with for one year and she did
not experience any hemorrhage or central venous stenosis.
Discussion
According to the clinical practice guidelines of the
National Kidney Foundation Kidney Disease Outcomes Quality
Initiative, the success rates of autologous and grafted internal
AVFs are 80 and 10%, respectively (1). However, for various practical reasons,
CVC remains the first access for dialysis therapy for most
patients. In China, particularly in underdeveloped areas, a large
number of patients use long-term dialysis catheters as the only
method of vascular access or while waiting for AVF maturation
(10). However, dialysis catheters
are reported to result in complications, including local injury,
hematoma, pneumothorax, thrombosis, venous stenosis and
catheter-associated infection. Central venous perforation is a rare
complication with frequently occurring serious consequences that
even include death. A total of 13 case reports on central venous
perforation caused by dialysis catheterization published between
2007 and 2018 were reviewed (Table
I) (2–9,11–15).
Among them, 8 patients presented with hemothorax and HS (2,3,5,7,8,12–14), and
1 patient died despite rescue after surgery (3).
 | Table I.Previously published cases of central
venous perforation caused by dialysis catheter (n=13). |
Table I.
Previously published cases of central
venous perforation caused by dialysis catheter (n=13).
| First author
(year) | Puncture
approach | Perforation site | Symptoms | Treatment | Outcomes | (Refs.) |
|---|
| Winkes (2016) | LIJV | LBCV mediastinum | Pectoralgia
hemothorax HS | Thoracotomy | Recovery | (2) |
| Iwańczuk (2013) | RIJV | RBCV pleural
cavity | Pectoralgia
hemothorax HS | Thoracotomy | Death | (3) |
| Wong (2016) | RIJV | Precava PA LA | Pectoralgia | Thoracotomy | Recovery | (4) |
| Turkyilmaz
(2017) | LSV | Precava pleural
cavity | Pectoralgia
hemothorax HS | Thoracotomy | Recovery | (5) |
| Kuzniec (2010) | RIJV | Precava | NA | Thoracoscopic
surgery | Recovery | (6) |
| Song (2015) | RIJV | Precava | Pectoralgia
hemothorax HS | EVSGR | Recovery | (7) |
| Azizzadeh (2007) | LSV | Precava | Hemothorax HS | EVSGR | Recovery | (8) |
| Pua (2014) | LIJV | LBCV | NA | EVSGR | Recovery | (9) |
| Zhang (2016) | RIJV | RBCV mediastinum | Hemothorax | Coils | Recovery | (11) |
| Wetzel (2017) | LIJV | LBCV | Hemothorax HS | Conservative
therapy | Recovery | (12) |
| Kabutey (2013) | LSV | LBCV | Hemothorax HS | Conservative
therapy | Recovery | (13) |
| Chao (2010) | RIJV | Precava | Pectoralgia HS | Conservative
therapy | Recovery | (14) |
| Garcarek (2015) | LIJV | LBCV mediastinum | NA | Coils and glue | Recovery | (15) |
Review of the relevant literature and summary of our
experience led to the assumption that the following factors may
increase the risk of central venous perforation caused by dialysis
catheters. First, since the distance from the LIJV to the right
atrium is longer and passes through the left BCV and the superior
vena cava, central venous perforation occurs more frequently with
left intubation (2). Second, obesity
is a risk factor for central venous perforation (16). Wicky et al (17) retrospectively analyzed 11 cases of
severe vascular complications after CVC misplacement, and 7
patients were obese with a body mass index of >30
kg/m2. Third, the experience of the surgeons is an
important factor affecting central venous perforation (2). The procedure was performed by a
primary-hospital kidney physician who had placed <50 long-term
catheter implants.
To reduce the occurrence of central venous
perforation, the following suggestions should be considered. First,
the ‘Fistula First Initiative’ principle should be followed, which
may reduce CVC placement, thrombosis and stenosis. The ‘Fistula
First Initiative’ emphasizes the primacy of the AVF as the desired
vascular access for patients maintained on chronic hemodialysis
(18). Second, the left approach
should be considered unless there is a contraindication regarding
right intubation. Third, if possible, placement of the CVC should
be performed under X-ray guidance. Prior to implantation, vascular
conditions may be clearly confirmed through angiography and the
position of the catheter may be dynamically viewed under
intra-operative fluoroscopy (1).
Finally, if the guide wire inside the long-term dialysis catheter
is more flexible and the expansion tube is more rigid, even if the
guide wire enters smoothly, the rigid expansion tube may break the
guide wire. Therefore, the use of more supportive guide wires
during the left intubation may be a safer choice. Following
placement of the avulsion sheath, the rigid guide wire may be
retained in the upper vena cava and the dialysis catheter may be
placed in the appropriate position through this guide wire. If the
catheter is difficult to maneuver around the turns of blood
vessels, the rigid guide wire may be inserted into the two catheter
cavities to increase the supporting force.
After central venous perforation, the procedure for
dealing with angiorrhexis to prevent further bleeding is a problem
that requires to be considered. As presented in Table I, among the 13 cases reported from
2007 to 2018, 4 cases underwent thoracotomy (2–5), 1 case
underwent thoracoscopic surgery (6),
3 cases received covered stents (7–9), 1 case
received coil embolization (11), 3
cases received conservative treatment (12–14) and
1 case received coil combined with gel embolization (15). Of all of the cases, one patient died
after thoracotomy (3). In the
present case, therapeutic strategies were required to address the
following two important issues. First, due to hemothorax and HS,
extubation and hemostasis were the primary problems. Second, due to
the patient's right BCV occlusion and poor peripheral vascular
conditions, the LIJV channel required to be retained as much as
possible. Catheter insertion from the left side was avoided, as
there was a contraindication of right intubation, and it was
attempted to reduce the risk of complications. Due to the marked
surgical trauma, as well as the patient's complex disease history
and unstable vital signs, surgical treatment was not the preferred
treatment. Although covered stent implantation is an effective
method for the treatment of vascular injury, this method was not
applicable to the present case, since the vascular rupture was
located on the opposite side of the left jugular vein opening,
which would be covered by the stent, causing left jugular vein
reflux disorder (19). Central
venous perforation caused by intubation usually has a clear sinus
tract in which the catheter is located, providing a basis for
endovascular occlusion. To the best of our knowledge, the present
study is the second to report on a case with endovascular
embolization treatment using coils combined with glues. In contrast
to the present case, in the previously reported case, the patient
had less blood loss and stable vital signs (15). The advantages of coils and
cyanoacrylate glue embolization have been noted in various studies.
For instance, Yavuz et al (20) indicated that patients with varicose
veins had significant improvement in venous clinical severity
scores and Aberdeen varicose vein questionnaire scores with no skin
pigmentation, hematoma, paresthesia, deep vein thrombosis or
pulmonary embolism after application of a novel NBCA glue ablation
catheter. A retrospective chart review of the long-term outcomes of
patients treated with the combined injection of coils and
cyanoacrylate glue for bleeding gastric fundal varices demonstrated
that the combination therapy appeared safe and may reduce the risk
of cyanoacrylate embolization (21).
Balloon-protected embolization has been adopted for the
endovascular repair of central vein injuries (22). In the present case, the catheter
passed through the mediastinum and pleura into the thoracic cavity.
It was opted for gradually retracting the dialysis catheter
simultaneously with coil embolization, which not only enhanced the
effect of the coil embolization but also blocked the small broken
blood vessels. This method may achieve hemostasis with good
long-term outcomes.
In summary, vascular perforation is a rare
complication of CVC placement. Combined injection of coils and
cyanoacrylate glue is a minimally invasive, safe and effective
treatment method.
Acknowledgements
Not applicable.
Funding
The current study was funded by Natural Science
Foundation of Anhui Province of China (grant no. 1808085MH254).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
CZ and WL designed the study and drafted the
manuscript. CZ, KL, PW, WR and WL contributed information on the
case and participated in data analysis. All authors approved the
final version of the manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of The First Affiliated Hospital of USTC. The patient
provided consent to participate.
Patient consent for publication
The patient provided written informed consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Group VAW: Clinical practice guidelines
for vascular access. Am J Kidney Dis 48(Suppl 1). 176–247.
2006.
|
|
2
|
Winkes MB, Loos MJ, Scheltinga MR and
Teijink JA: Dialysis catheter placement via the left internal
jugular vein: Risk of brachiocephalic vein perforation. J Vasc
Access. 17:e75–e78. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Iwańczuk W, Guźniczak P and Kasperczak J:
Hemothorax as a complication of subclavian vein cannulation with
haemodialysis catheter-case report. Anaesthesiol Intensive Ther.
45:89–92. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wong K, Marks BA, Qureshi A and Stemm JJ:
Migration of a central venous catheter in a hemodialysis patient
resulted in left atrial perforation and thrombus formation
requiring open heart surgery. A A Case Rep. 7:21–23. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Turkyilmaz A, Karapolat S, Kilic M and
Tekinbas C: The perforation of the superior vena cava secondary to
the left subclavian dialysis catheter. Vasc Endovascular Surg.
51:95–97. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kuzniec S, Natal SR, Werebe Edc C and
Wolosker N: Videothoracoscopic-guided management of a central vein
perforation during hemodialysis catheter placement. J Vasc Surg.
52:1354–1356. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Song D, Yun S, Cho S, Goo DE and Kim YJ:
Latrogenic innominate vein injury by hemodialysis catheter,
successful endovascular repair. J Vasc Access. 16:e4–e5. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Azizzadeh A, Pham MT, Estrera AL, Coogan
SM and Safi HJ: Endovascular repair of an iatrogenic superior vena
caval injury: A case report. J Vasc Surg. 46:569–571. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pua U: Central vein perforation during
tunneled dialysis catheter insertion: Principles of acute
management. Hemodial Int. 18:838–841. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang K, Wang P, Liang X, Lu X and Liu Z:
Epidemiology of haemodialysis catheter complications: A survey of
865 dialysis patients from 14 haemodialysis centres in Henan
province in China. BMJ Open. 5:e0071362015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang W, Liu T, Wang X, Huo Y, Jia Y, Su L
and Liu Y: Hemothorax caused by replacement of hemodialysis
catheter: A case report. Hemodial Int. 20:E7–E10. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wetzel LR, Patel PR and Pesa NL: Central
venous catheter placement in the left internal jugular vein
complicated by perforation of the left brachiocephalic vein and
massive hemothorax: A Case Report. A A Case Rep. 9:16–19. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kabutey NK, Rastogi N and Kim D:
Conservative management of iatrogenic superior vena cava (SVC)
perforation after attempted dialysis catheter placement: Case
report and literature review. Clin Imaging. 37:1138–1141. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chao CS, Chao CT, Chin HK and Chang YP:
Application of positive end-expiratory pressure in a case with
large laceration on the superior vena cava. J Anesth. 24:253–255.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Garcarek J, Wątorek E, Kurcz J, Kusztal M,
Gołebiowski T, Letachowicz K, Letachowicz W, Weyde W and Klinger M:
Endovascular reparation of central vein injury with
balloon-protected embolization. Cardiovasc Intervent Radiol.
38:1057–1059. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mansfield PF, Hohn DC, Fornage BD,
Gregurich MA and Ota DM: Complications and failures of
subclavian-vein catheterization. N Engl J Med. 331:1735–1738. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wicky S, Meuwly JY, Doenz F, Uske A,
Schnyder P and Denys A: Life-threatening vascular complications
after central venous catheter placement. Eur Radiol. 12:901–907.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schinstock CA, Albright RC, Williams AW,
Dillon JJ, Bergstralh EJ, Jenson BM, McCarthy JT and Nath KA:
Outcomes of arteriovenous fistula creation after the fistula first
initiative. Clin J Am Soc Nephrol. 6:1996–2002. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Anaya-Ayala JE, Smolock CJ, Colvard BD,
Naoum JJ, Bismuth J, Lumsden AB, Davies MG and Peden EK: Efficacy
of covered stent placement for central venous occlusive disease in
hemodialysis patients. J Vasc Surg. 54:754–759. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yavuz T, Acar AN, Aydin H and Ekingen E: A
retrospective study of a new n-butyl-2-cyanoacrylate glue ablation
catheter incorporated with application guiding light for the
treatment of venous insufficiency: Twelve-month results. Vascular.
26:547–555. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bhat YM, Weilert F, Fredrick RT, Kane SD,
Shah JN, Hamerski CM and Binmoeller KF: EUS-guided treatment of
gastric fundal varices with combined injection of coils and
cyanoacrylate glue: a large U.S. experience over 6 years (with
video). Gastrointest Endosc. 83:1164–1172. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Vollherbst DF, Otto R, Do TD, von Deimling
A, Kauczor HU, Bendszus M, Sommer CM and Möhlenbruch MA:
Extra-small dual-lumen micro-balloon catheters can improve
endovascular embolization: An experimental in vivo and in vitro
study. J Neurointerv Surg. 10:1092–1096. 2018. View Article : Google Scholar : PubMed/NCBI
|