Introduction
The shape of the radius is important for normal
forearm rotation. A forearm fracture is the third most common
pediatric fracture (1–3), probably because the bones are weaker,
and the gold standard for such fractures remains closed reduction
and casting (2). These fractures are
classified as greenstick, complete, or plastic deformation; 82.5%
of forearm fractures are greenstick fractures (4). Rotational deformity occurs more often
in greenstick fractures than in complete fractures, and the radius
deformities are the direct effect of forearm rotation. Moreover,
the diaphysis has less self-correction ability, and the rotation
transposition is not corrected (2).
Such fractures are treated by correcting the rotational and angular
malalignments simultaneously by reversing the mechanism of injury,
with follow-up radiography at >6 weeks (3). On the other hand, malunion of pediatric
forearm fractures can cause permanent functional disability with
limitation of forearm rotation. In children with functional
disability, corrective osteotomy is indicated when there is
malunion of a fracture in the midshaft of the forearm (5).
In this study, malrotation of the forearm that
resulted in a malunion of a diaphyseal fracture of the radius 3
months after injury is presented. Radius apex angulation was
improved by corrective osteotomy. This study suggests that the
anatomic characteristics of the interosseous membrane affect
forearm greenstick fractures. The interosseous membrane contributes
to forearm stability, especially the central band (CB), which
consists of a thin membranous part and a thick ligamentous part,
that interferes with rotation after a forearm fracture (6,7). Based
on the literature, we suggest that the fixed position of the
forearm is important for the initial treatment of greenstick
fractures, and radius apex angulation of 20° must be corrected by
osteotomy due to loss of rotation. In the present case, follow-up
at 7 years demonstrated full range of wrist and elbow movement and
no adverse symptoms, and no malunion was observed on radiographs of
the forearm.
Case report
A 10-year-old, left hand-dominant, Asian boy fell
from a height of 1 meter playing in the garden. He noticed pain and
swelling around his forearm and presented immediately to a nearby
emergency department. Initial examination showed deformity,
tenderness, and swelling of his left forearm. Full-length forearm
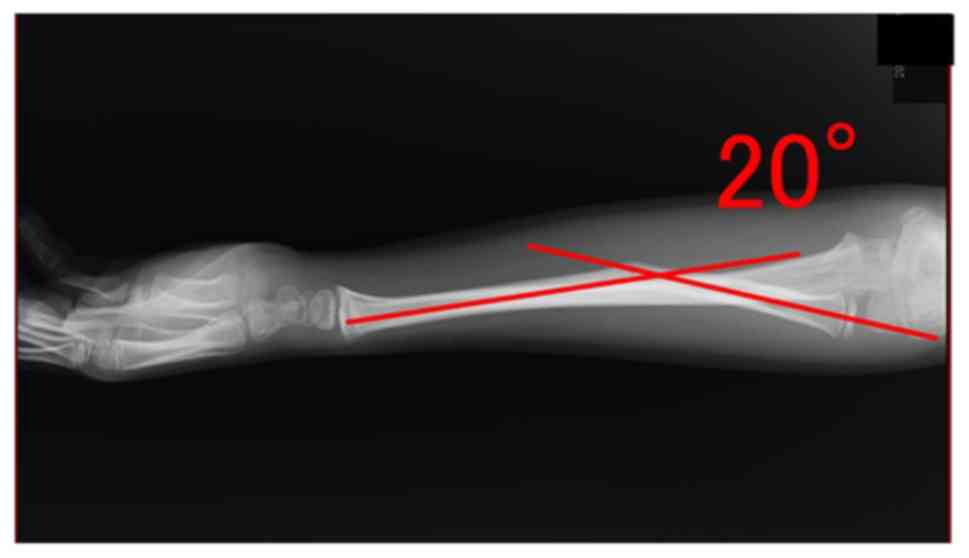
radiographs were performed, confirming an angulated greenstick
fracture of the middle third of the radius (Fig. 1). The radiographic diagnosis was
incomplete fracture of the diaphysis of the left radius. The limb
was fixed by a plaster slab with the forearm in the neutral
position without repositioning. Three weeks after the injury,
follow-up radiographs were taken (Fig.
2). However, after 3 months, loss of supination of the left
forearm appeared, and he presented to our emergency department with
limitation of supination of the left forearm. The left forearm
range was 45° with the forearm in supination and 100° in pronation
(Fig. 3). Range of motion of the
elbow and wrist was unlimited, and there was no tenderness at the
fracture and interosseous membrane. Radiography showed volar
angulation (20°; Fig. 4).
The following day, the injury was treated surgically
under general anesthesia. Written, informed consent was obtained
from the patient and the patient's legal guardian for publication
of this case report and any accompanying images. A copy of the
written consent is available for review by the Editor-in-Chief of
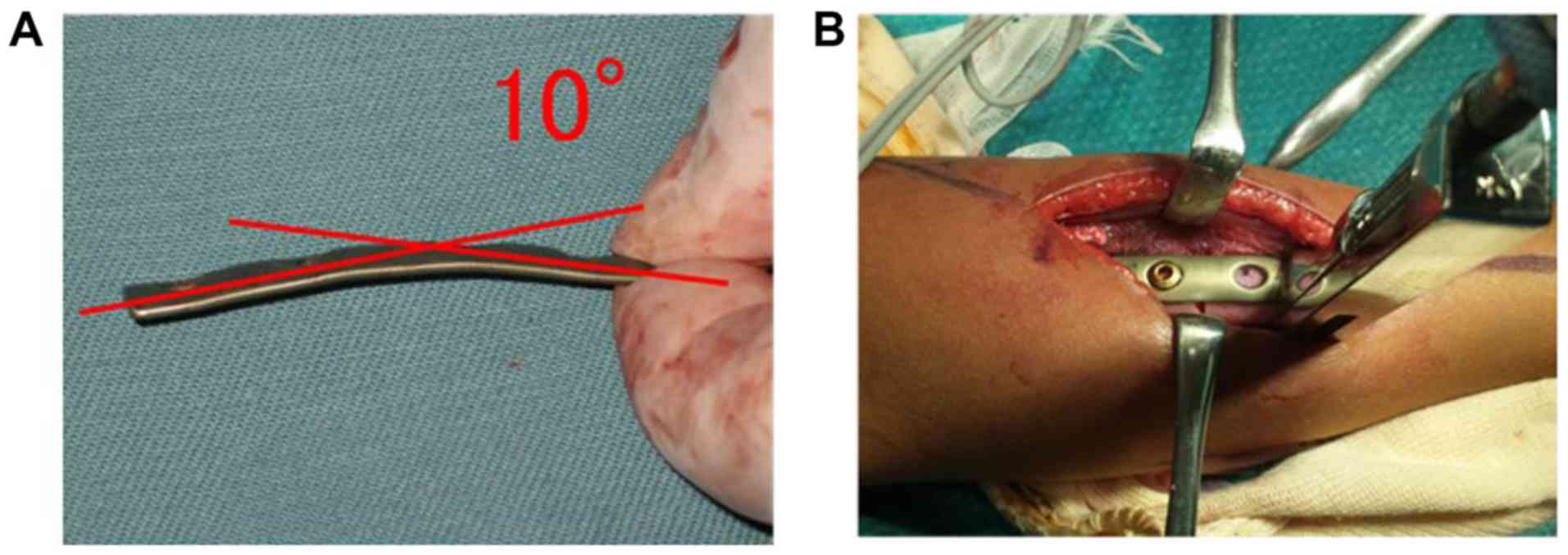
this journal. Open reduction and internal fixation of the radial
shaft fracture were performed using a 1/3 tubular plate with 4
holes with screw diameters of 3.5 mm (standard cortical screws;
Synthes, Paoli, PA) (8,9), which were bent 10° for corrective
fixation (Figs. 5 and 6). Rotation was not corrected; only the
apex angulation was corrected through an anterior approach to the
radius.
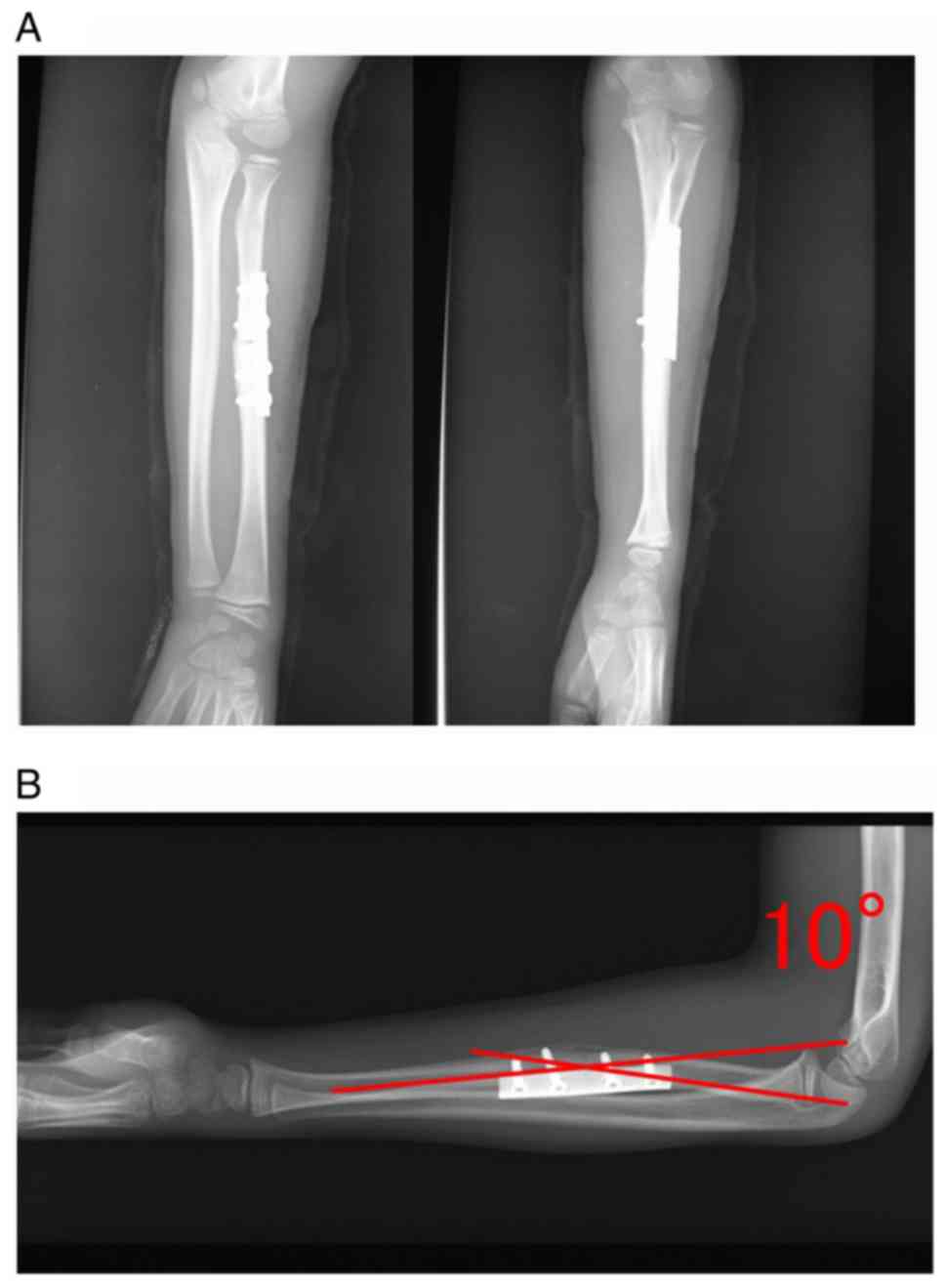
At 12 months, the patient had no pain or limitation
of the elbow and wrist and could carry out his normal day-to-day
activities. The range of motion was 0–130° at the elbow, extension
of 70° and flexion of 80° at the wrist, and supination of 85° and
pronation of 90° at the forearm, although the radius showed a volar
angulation deformity of 10° on radiographic examination (Fig. 7).
The patient had full range of movement of his left
forearm and underwent plate removal from the left radius under
general anesthesia 2 years after the corrective surgery. Moreover,
follow-up at 7 years demonstrated the full range of wrist and elbow
movements and no adverse symptoms. Postoperative radiographs at the
7-year follow-up evaluation (Fig. 8)
demonstrated improved radiographic parameters, including improved
alignment of the hand and elbow.
Discussion
A greenstick fracture is an incomplete fracture in
which the compressive side of the cortex is still intact but
plastically deformed. The incidence of poor results from closed
treatment of such fractures in children greater than 10 years of
age is seriously underestimated (10–12).
Therefore, the fixed position of the forearm is important in the
initial treatment of greenstick fractures, and in a case with
radius apex angulation of 20°, we suggest that osteotomy must be
performed for loss of rotation. The point of this study is that
attention should be paid to the position of fixation in
conservative treatment and that the rotational limitation of the
forearm recovered without correcting the rotation of the radius
with only correction of apex angulation by corrective osteotomy.
Although it has been an issue in the past, this is not well known
in actual clinical practice. In fact, even in this case, a mature
orthopedic surgeon had developed rotational deformation due to the
insufficiency of the fixed position in conservative treatment. We
need to reconfirm it as a warning to orthopedic surgeons including
us. Although fractures in children are neglected, I think it is
crucial in that there are few articles that report cases of
indications for corrective osteotomy of diaphyseal forearm in
children (13). In addition, I think
that it is rare to observe cases up to 7 years after surgery.
It has been previously reported that adequate
remodeling of angulated deformities in children did not occur with
growth, particularly when the diaphyseal forearm was involved in
the fracture, and there was also no correction of rotational
malalignment with growth (14,15).
Permanent functional disability with limitation of forearm rotation
can occur in children with malunion of forearm fractures. A
previous study showed that, for pediatric forearm fractures, the
age of 10 years was the limit for conservative therapy, because
self-correction ability starts to decrease at ≥10 years, and it
then disappears between 12 and 13 years (8). Furthermore, the self-correction ability
of the diaphysis is less, and there is no correction of the
rotational transposition. Forearm diaphysis fractures are
unforgiving, and because diaphyseal bone has less remodeling
capacity, less angulation is acceptable (16). Therefore, when stable fractures or
displaced fractures can be anatomically reduced correctly,
conservative therapy with a long arm cast is the first-choice
therapy. In patients 0 to 8 years of age with fracture angulation
>20° and malrotation >45°, closed reduction is indicated.
Similar studies have reported that sufficient remodeling of
malunion of 20–30° is unlikely after 9 years of age, and that such
cases require correction as soon as soft tissue recovery from the
initial immobilization has occurred (13). Moreover, patients 8 to 14 years of
age with fracture angulation >5° and malrotation >30° require
closed reduction (17). In clinical
practice, the forearm rotation range is 145–170°, and 50%
restriction of excursion is accepted. On the other hand, function
is not impaired with loss of 20–30° of rotation; moreover, loss of
supination presents more problems than loss of pronation (18). A previous study showed that, in
forearm diaphyseal fractures, loss of rotation can occur with
angulation of 15–20° (16).
It has previously been shown that excellent
functional results can be obtained with a corrective osteotomy
technique with few complications. Therefore, corrective osteotomy
should be performed at the earliest opportunity (19). In recent studies,
three-dimensional-planned, patient-specific guides and implants
have been shown to facilitate precise corrective osteotomies of
complex multiplanar forearm deformities, and the preliminary
results have been satisfactory (20–22).
However, another study indicated that, with an accurate
understanding of forearm anatomy and appropriate X-ray views (with
the tuberosity of the radius approximately on the opposite side of
the radial styloid process), the corrective osteotomy procedure can
be simplified and performed with fluoroscopy alone, without the
need for computed tomography (13).
Osteotomy was performed in the present patient only with correction
of apex angulation, based solely on knowledge of the anatomical
structure of the forearm and fluoroscopy.
The radius bent anatomically in our patient, with a
possibility that rotational malalignment occurred at the same time
as the apex deformity, but our concern was about dissection and the
function of the interosseous membrane. A previous study suggested
that rotation caused the apex to remain anterior (23). In addition, when there are angular
deformities of the radius and ulna, tension is produced in the
interosseous membrane, and this tension impairs the radius's
rotation around the mechanical axis of the forearm (24).
Angulation of the apex in this case increased from
10° to 20° due to the interosseous membrane, which consists of a
thin membranous part and a thick ligamentous part, the CB, which
has 2 to 3 times the thickness of the membranous part, is
responsible for 71% of interosseous membrane stiffness, and is the
second principal stabilizer of the radius. The CB contributes to
the stability of the radius (25).
The CB leads to the ulna from approximately 62% of the distal
radius (25). In the present case,
radius fracture lines may have been proximal to the footprint of
the CB band, so that the X-rays indicated horned transformation of
the fracture with the pronated position short arm spica cast and
the distal fragment pulled by a distal CB band. Therefore, the
radius appeared to be pronated through the CB of the interosseous
membrane because this was a greenstick fracture, and the radius
changed onto the palm side, with loss of supination. It seems that
the width of the interosseous membrane is smallest in pronation
(radius and ulna closer) due to an anatomical feature of the
interosseous membrane related to the supination limit; the
interosseous membrane width is greatest in the middle rank (radius
and ulna far) in a neutral or slightly supinated position
(approximately 30°), but the repositioning suggested of forearm
fractures in this position is unstable.
Although the possibility of contracture of the
interosseous membrane was considered in the present case, the
patient complained of loss of supination of the left forearm
without tenderness or induration. In the surgery, pronation became
smoother with osteotomy of the fracture region, and contracture of
the interosseous membrane seemed unlikely. Of note, the rotational
limitation of the forearm recovered without correcting the rotation
of the radius with only correction of apex angulation by the plate
that was bent 10° by corrective osteotomy. Taking into account
previous studies (16,17), it was necessary to correct apex
angulation less than 15°; therefore, including the correction that
would occur by remodeling, it was decided to correct the angle at
10°. This study was similar to and consistent with a previous study
(23).
Thus, apex angulation of pediatric forearm bone
fractures of 20° cannot be permitted, and the deformity must be
reduced at the patient's first visit, if possible. It is also
necessary to consider changing the plan if the forearm deformity is
greater than 20° during conservative treatment.
In conclusion, this case suggests that corrective
osteotomy was needed for loss of supination after a greenstick
fracture of the diaphysis of the radius. In the present patient,
there was rotation due to the CB of the interosseous membrane. In
the initial treatment of greenstick fractures, the fixed position
of the forearm is crucial, and radius apex angulation of 20° must
be corrected by osteotomy due to loss of rotation. This case
indicates that the corrective osteotomy of the radius apex alone,
without rotational correction, with bending of the plate improves
the loss of forearm rotation. Follow-up at 7 years demonstrated the
full range of elbow and wrist movements and no adverse symptoms,
and no malunion was observed on radiographs of the forearm.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JK and NN analyzed and interpreted the data, wrote
the manuscript and organized the figures. JK, AM and KK performed
the surgery. JK, NN and HI designed the study, edited and reviewed
the manuscript and approved the version to be published. All
authors reviewed and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent for the publication of
patient data and accompanying images was obtained.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviation
Abbreviations:
References
|
1
|
Cheng JC, Ng BK, Ying SY and Lam PK: A
10-year study of the changes in the pattern and treatment of 6,493
fractures. J Pediatr Orthop. 19:344–350. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jones K and Weiner DS: The management of
forearm fractures in children: A plea for conservatism. J Pediatr
Orthop. 19:811–815. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vopat ML, Kane PM, Christino MA, Truntzer
J, McClure P, Katarincic J and Vopat BG: Treatment of diaphyseal
forearm fractures in children. Orthop Rev (Pavia). 24:53252014.
|
|
4
|
Alpar EK, Thompson K, Owen R and Taylor
JF: Midshaft fractures of forearm bones in children. Injury.
13:153–158. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Flynn JM, Jones KJ, Garner MR and Goebel
J: Eleven years experience in the operative management of pediatric
forearm fractures. J Pediatr Orthop. 30:313–319. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hotchkiss RN, An KN, Sowa DT, Basta S and
Weiland AJ: An anatomic and mechanical study of the interosseous
membrane of the forearm: Pathomechanics of proximal migration of
the radius. J Hand Surg Am. 14:256–261. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shepard MF, Markolf KL and Dunbar AM:
Effects of radial head excision and distal radial shortening on
load-sharing in cadaver forearms. J Bone Joint Surg Am. 83:92–100.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Price CT: Acceptable alignment of forearm
fractures in children: Open reduction indications. J Pediatr
Orthop. 30:S82–S84. 2010. View Article : Google Scholar
|
|
9
|
Tarmuzi NA, Abdullah S, Osman Z and Das S:
Paediatric forearm fractures: Functional outcome of conservative
treatment. Bratisl Lek Listy. 110:563–568. 2009.PubMed/NCBI
|
|
10
|
Shoemaker SD, Comstock CP, Mubarak SJ,
Wenger DR and Chambers HG: Intramedullary kirschner wire fixation
of open or unstable forearm fractures in children. J Pediatr
Orthop. 19:329–337. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cullen MC, Roy DR, Giza E and Crawford AH:
Complications of intramedullary fixation of pediatric forearm
fractures. J Pediatr Orthop. 18:14–21. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Price CT and Mencio GA: Injuries to the
shafts of the radius and ulnaFractures in Children. Beaty JH and
Kasser JR: 5th. Lippincott Williams & Wilkins; Philadelphia,
PA: pp. 443–482. 2001
|
|
13
|
Price CT and Knapp DR: Osteotomy for
malunited forearm shaft fractures in children. J Pediatr Orthop.
26:193–196. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Creasman C, Zaleske DJ and Ehrlich MG:
Analyzing forearm fractures in children. The more subtle signs of
impending problems. Clin Orthop Relat Res. 40–53. 1984.PubMed/NCBI
|
|
15
|
Daruwalla JS: A study of radioulnar
movements following fractures of the forearm in childrenClin Orthop
Relat Res; pp. 114–120. 1979, PubMed/NCBI
|
|
16
|
Shah AS, Lesniak BP, Wolter TD, Caird MS,
Farley FA and Vander Have KL: Stabilization of adolescent both-bone
forearm fractures: A comparison of intramedullary nailing versus
open reduction and internal fixation. J Orthop Trauma. 24:440–447.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Price CT: Part II: Injuries to the shaft
of the radius and ulnaFractures in Children. Rockwood CA Jr,
Wilkins KE, Beaty JH and Green DP: 4th. Lippincott-Raven;
Philadelphia, PA: pp. 522–524. 1996
|
|
18
|
Patrick J: A study of supination and
pronation, with especial reference to the treatment of forearm
fractures. J Bone Joint Surg Am. 28:737–748. 1946.PubMed/NCBI
|
|
19
|
van Geenen RC and Besselaar PP: Outcome
after corrective osteotomy for malunited fractures of the forearm
sustained in childhood. J Bone Joint Surg Br. 89:236–239. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Byrne AM, Impelmans B, Bertrand V, Van
Haver A and Verstreken F: Corrective osteotomy for malunited
diaphyseal forearm fractures using preoperative 3-dimensional
planning and patient-specific surgical guides and implants. J Hand
Surg Am. 42:836.e1–836.e12. 2017. View Article : Google Scholar
|
|
21
|
Murase T, Oka K, Moritomo H, Goto A,
Yoshikawa H and Sugamoto K: Three-dimensional corrective osteotomy
of malunited fractures of the upper extremity with use of a
computer simulation system. J Bone Joint Surg Am. 90:2375–2389.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jeuken RM, Hendrickx RPM, Schotanus MGM
and Jansen EJ: Near-anatomical correction using a CT-guided
technique of a forearm malunion in a 15-year-old girl: A case
report including surgical technique. Orthop Traumatol Surg Res.
103:783–790. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hensinger RN: Meeting highlights. 1986
Annual Meeting, American Academy of Orthopaedic Surgeons. J Pediatr
Orthop. 6:500–506. 1986. View Article : Google Scholar
|
|
24
|
Graham TJ, Fischer TJ, Hotchkiss RN and
Kleinman WB: Disorders of the forearm axis. Hand Clin. 14:305–316.
1998.PubMed/NCBI
|
|
25
|
Chloros GD, Wiesler ER, Stabile KJ,
Papadonikolakis A, Ruch DS and Kuzma GR: Reconstraction of
essex-lopressti injury of forearm: Technical note. J Hand Surg Am.
33:124–130. 2008. View Article : Google Scholar : PubMed/NCBI
|