Introduction
As the prevalence of hypertension has increased over
the years, an improved understanding of the pharmacology of
antihypertensive agents and the pathophysiology of hypertension has
become indispensable in anesthesia practice. Hypertension is
associated with different etiologies including genetic,
physiological, and environmental factors (1). Patients need treatment with appropriate
antihypertensive agents to achieve their target blood pressure (BP)
that may be possible with monotherapy; some patients may require
two or more agents with different mechanisms of action for
successful outcome (2). The common
drugs of choice are calcium channel blockers (CCBs), angiotensin
receptor blockers (ARBs) or angiotensin converting enzyme
inhibitors (ACEIs), and diuretics. Moreover, data on the decision
to continue or discontinue treatment with ARBs or ACEIs before
noncardiac surgery is inconclusive (3).
The pathophysiological changes following carbon
dioxide (CO2) pneumoperitoneum lead to notable
hemodynamic responses, and the use of preoperative antihypertensive
agents in patients with hypertension affects these responses. This
study noted the effects of preoperative antihypertensive agents on
hemodynamic responses after intraperitoneal CO2
insufflation during laparoscopic surgery. Upon reviewing patients'
medical records, there were three major types of antihypertensive
agents taken by patients undergoing laparoscopic colon surgery:
Monotherapy with ARBs, monotherapy with CCBs, and combination
therapy with ARBs and CCBs. To contribute to the management of
anesthesia in patients with hypertension, a preliminary
retrospective analysis was designed to evaluate the impact of
antihypertensive agents on BP changes following intraperitoneal
CO2 insufflation during laparoscopic colectomy. It was
hypothesized that combination therapy with ARBs and CCBs would not
cause severe fluctuations in BP following intraperitoneal
CO2 insufflation. In addition, preoperative pulse
pressure-an indicator reflecting the blood vessel stiffness
(4) was investigated, and the
relationship between pulse pressure and BP fluctuations after
CO2 insufflation was analyzed. As the age of patients
may be related to the type of antihypertensive agent selected
(5–7), this factor was adjusted with other
potential confounding variables in the final analysis.
Materials and methods
The Institutional Review Board of Keimyung
University Dongsan Hospital (DSMC 2017-08-001) approved this
retrospective study and waived the need for informed consent. The
study was registered at http://cris.nih.go.kr (KCT0002595). The author
retrospectively identified patients who underwent laparoscopic
colon surgery under general anesthesia between January 2014 and
June 2017 via medical records. The inclusion criteria were as
follows: Elective laparoscopic colon surgery; age ≥50 years;
systolic BP <140 mmHg measured at daytime on the day before
surgery and diastolic BP <90 mmHg (8); and American Society of
Anesthesiologists physical status classifications I and II. For
patients with hypertension, additional inclusion criteria were as
follows: On hypertensive medication for at least 1 year following
diagnosis; ≤10 mg/day of the CCB amlodipine; equivalent to ≤80
mg/day of the ARB telmisartan; and systolic BP <140 mmHg
measured at daytime on the day before surgery and diastolic BP
<90 mmHg (8). The exclusion
criteria were as follows: Use of and antihypertensive agent other
than ARBs and CCBs; severe obesity (body mass index [BMI] ≥35
kg/m2); diabetes; heart failure; severe kidney disease;
and pregnancy or lactation.
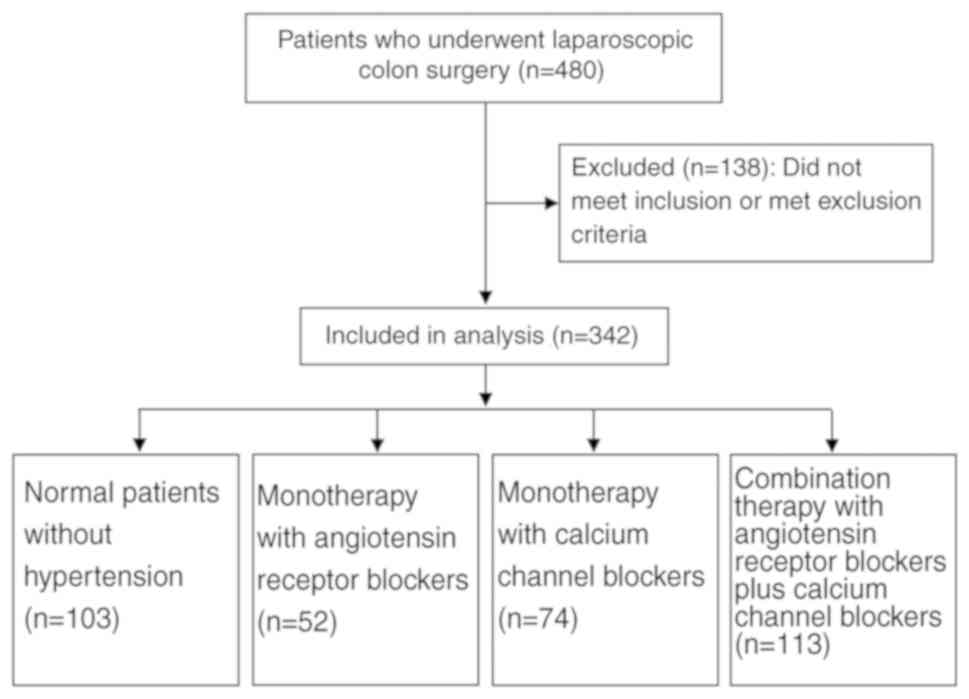
The patients were divided into four groups according
to medication status: Control group without hypertension
(normotensive subjects, group N); and groups of patients receiving
monotherapy with ARBs (group A), monotherapy with CCBs (group C),
and combination therapy with ARBs and CCBs (group AC). All patients
with hypertension continued to take antihypertensive agents until
the morning of surgery.
In all cases, anesthesia care was provided by a team
of anesthesiologists, and a standardized general anesthesia
protocol was followed for all patients. Standard monitoring
included pulse oximetry, electrocardiography, noninvasive BP,
temperature assessment, and capnography. The bladder of the BP cuff
encircled ≥80% of the patient's arm (8). Vital signs were recorded every 5 min or
more frequently, if needed, during anesthesia and post-anesthesia
care unit stay. General anesthesia was induced using intravenous
propofol 2 mg/kg and sufentanil 0.2 mcg/kg. Laryngoscopy and
tracheal intubation were facilitated using intravenous rocuronium
0.6–0.9 mg/kg. During surgery, sevoflurane concentration was
titrated to maintain a bispectral index value between 45 and 60,
and ventilation was adjusted to maintain an end-tidal
CO2 level between 35 and 40 mmHg. The patients were
placed in the Trendelenburg position after induction of anesthesia.
CO2 was insufflated into the peritoneal cavity at a
pressure of 12–15 mmHg.
The baseline BP and baseline pulse pressure were
defined as the average systolic BP and average pulse pressure,
respectively, measured during the daytime at the hospital ward the
day before surgery. CO2 insufflation BP was defined as
the average systolic BP measured within 10 min after
intraperitoneal CO2 insufflation; plateau BP was defined
as the average systolic BP measured within 30–60 min after
intraperitoneal CO2 insufflation. The primary outcome
was the difference between baseline BP and CO2
insufflation BP. The first secondary outcome was the difference
between CO2 insufflation BP and plateau BP. The other
secondary outcomes included incidence of intraoperative
hypotension, use of vasoconstrictor agents, and correlation between
the baseline pulse pressure and degree of BP change. Hypotension
was defined as a 30% decline in systolic BP from baseline values
(9), and the incidence of
intraoperative hypotension was investigated.
Statistical analysis was performed using SPSS 24.0
(IBM Corp., Armonk, NY). Multiple comparison tests for different
drug groups were conducted. Differences in BP were compared using
analysis of covariance (ANCOVA) after adjusting for the effect of
age, sex, height, BMI, and peak airway pressure. Logarithmic
transformation of the differences in BP was performed to normalize
the distributions. Categorical data in the cross-tabulation tables
were compared using Pearson's chi-square or Fisher's exact test
(Fisher's exact test was used in 2×2 contingency tables when the
expected frequency was <5 in any cell). Differences in the
incidence of hypotension among the groups were tested using the
Mantel-Haenszel chi-square test to adjust for confounding factors.
To analyze the correlation between pulse pressure and BP change,
partial correlation coefficients were obtained after adjusting for
confounding factors. P<0.05 was considered to indicate a
statistically significant difference.
Results
Among the 480 assessed patients, 138 were excluded
(Fig. 1). The demographic data of
the 342 remaining patients (Table I)
showed no statistically significant differences among the groups
with respect to sex, height, BMI, and peak inspiratory airway
pressure. Only age was significantly different between group N and
group C, where patients in group C were older on average than those
in group N.
 | Table I.Demographic data, baseline BP and
baseline pulse pressure. |
Table I.
Demographic data, baseline BP and
baseline pulse pressure.
| Characteristic | Group N (n=103) | Group A (n=52) | Group C (n=74) | Group AC (n=113) |
|---|
| Age (years) | 65±9 | 62±7 | 71±6 | 69±7 |
| Sex |
|
|
|
|
| Male | 40 | 21 | 40 | 65 |
|
Female | 63 | 31 | 34 | 48 |
| Height (cm) | 160.6±9.8 | 161.9±5.8 | 161.2±8.2 | 163.1±8.8 |
| BMI
(kg/m2) | 23.7±3.1 | 24.8±2.3 | 24.0±3.1 | 23.3±3.0 |
| Baseline blood
pressure (mmHg) | 122±14 | 121±11 | 124±13 | 118±10 |
| Baseline pulse
pressure (mmHg) | 48±10 | 49±9 | 52±13 | 47±11 |
| Peak airway pressure
(mmHg) | 23±2 | 23±2 | 23±2 | 23±2 |
In the comparison between groups N and A and between
groups N and AC, there was a significant difference in the change
from baseline to CO2 insufflation BP, after adjusting
for confounding factors (age, sex, height, BMI, and peak airway
pressure); the degree of increase from baseline to CO2
insufflation BP was significantly lesser in groups A and AC
(Tables II and III). The comparison between groups C and
A and between groups C and AC also showed less increase in BP from
baseline to CO2 insufflation BP in groups A and AC. The
adjusted confounding factors included age, sex, height, BMI, and
peak inspiratory airway pressure. The ANCOVA showed that only
patient age had a significant effect on the difference in BP. Other
comparisons showed no significant changes in BP. The incidence of
intraoperative hypotension was not significantly different among
the groups after adjusting for confounding factors (Table III).
 | Table II.Intraoperative changes in BP and
incidence of hypotension. |
Table II.
Intraoperative changes in BP and
incidence of hypotension.
| Characteristic | Group N (n=103) | Group A (n=52) | Group C (n=74) | Group AC (n=113) |
|---|
| CO2 BP
(mmHg) | 143±23 | 125±20 | 148±21 | 125±17 |
| Baseline
BP-CO2 BP | −21±24 | −4±18 | −24±23 | −7±19 |
| Plateau BP
(mmHg) | 118±13 | 103±8 | 120±13 | 101±10 |
| CO2
BP-plateau BP | 26±19 | 21±18 | 29±18 | 23±12 |
| Incidence of
hypotension | 43/60 (43.7%) | 25/27 (48.1%) | 39/35 (52.7%) | 60/53 (53.1%) |
 | Table III.Comparison of BP difference and
hypotension incidence. |
Table III.
Comparison of BP difference and
hypotension incidence.
|
| Baseline
BP-CO2 BP | CO2
BP-plateau BP | Incidence of
hypotension |
|---|
| Comparison |
|
|
|
|---|
|
| P-value | Difference (95%
CI) | P-value | Difference (95%
CI) | P-value | OR (95% CI) |
|---|
| Group N vs. A | 0.001 | 17.8 (7.8–27.8) | 0.26 | 5.0 (−3.8–13.7) | 0.75 | 1.2 (0.5–3.0) |
| Group N vs. C | 0.45 | 4.1 (−6.6–14.8) | 0.62 | 2.1 (−6.3–10.4) | 0.66 | 0.8 (0.3–2.1) |
| Group N vs. AC | <0.001 | 18.2 (8.7–27.7) | 0.13 | 5.2 (−1.6–12.0) | 0.61 | 0.7 (0.3–1.9) |
| Group A vs. C | <0.001 | 21.9 (10.3–33.5) | 0.28 | 5.5 (−4.5–15.4) | 0.44 | 0.6 (0.3–1.8) |
| Group A vs. AC | 0.25 | 5.5 (−3.8–14.7) | 0.51 | 2.5 (−5.1–10.1) | 0.39 | 0.6 (0.3–1.7) |
| Group C vs. AC | 0.001 | 17.0 (7.0–27.0) | 0.25 | 4.0 (−2.9–10.9) | 0.79 | 0.8 (0.4–2.2) |
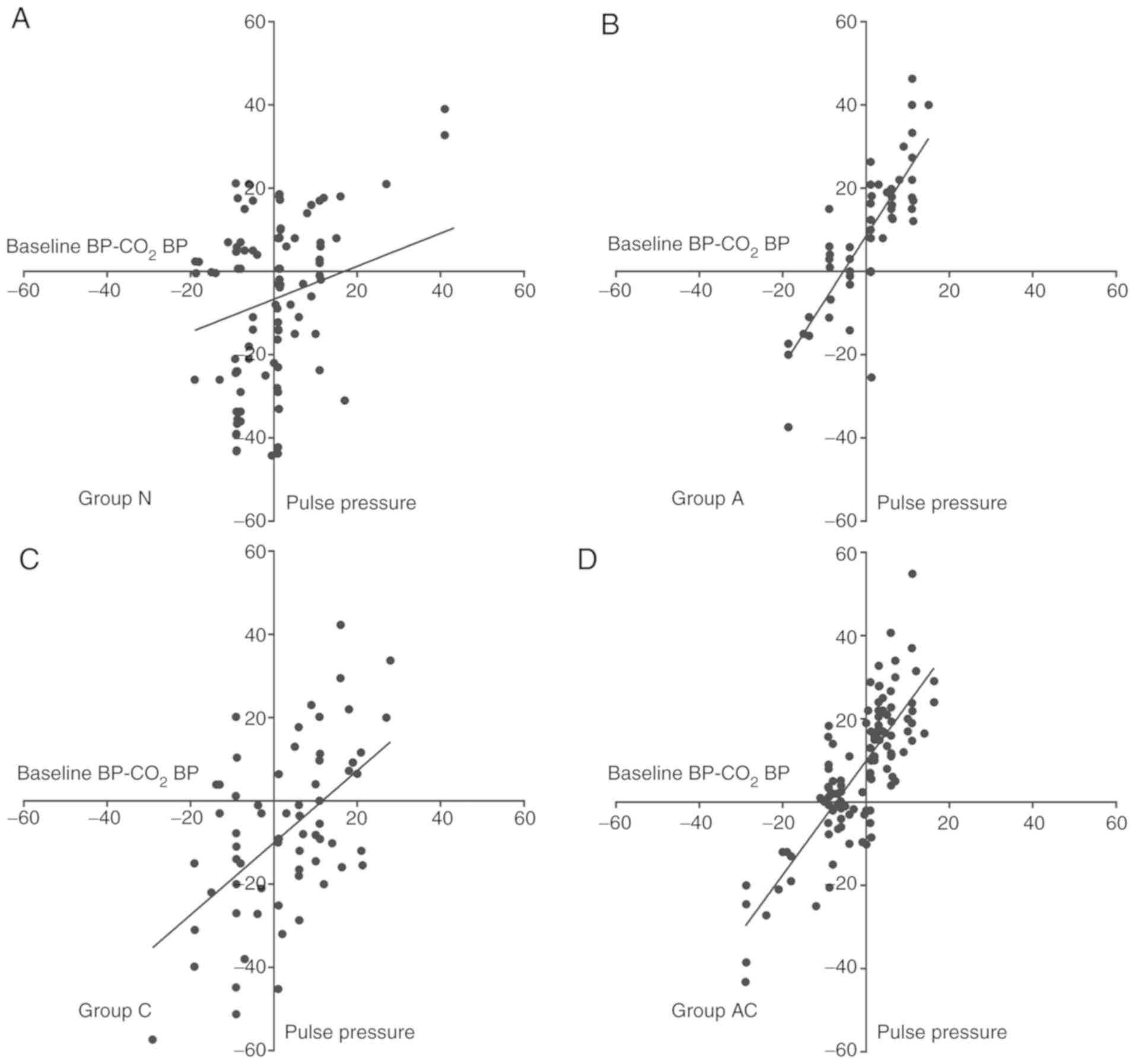
There was a correlation between baseline pulse
pressure and BP increase after CO2 insufflation in all
patients, after adjusting for confounding factors (age, sex,
height, BMI, and peak airway pressure) (Table IV). This correlation ranged from
moderate to strong in patients with hypertension. Groups A and AC
showed a stronger correlation than group C. A partial regression
plot (adjusted for age, sex, height, BMI, and peak airway pressure)
of baseline pulse pressure vs. BP increase after CO2
insufflation is shown in Fig. 2.
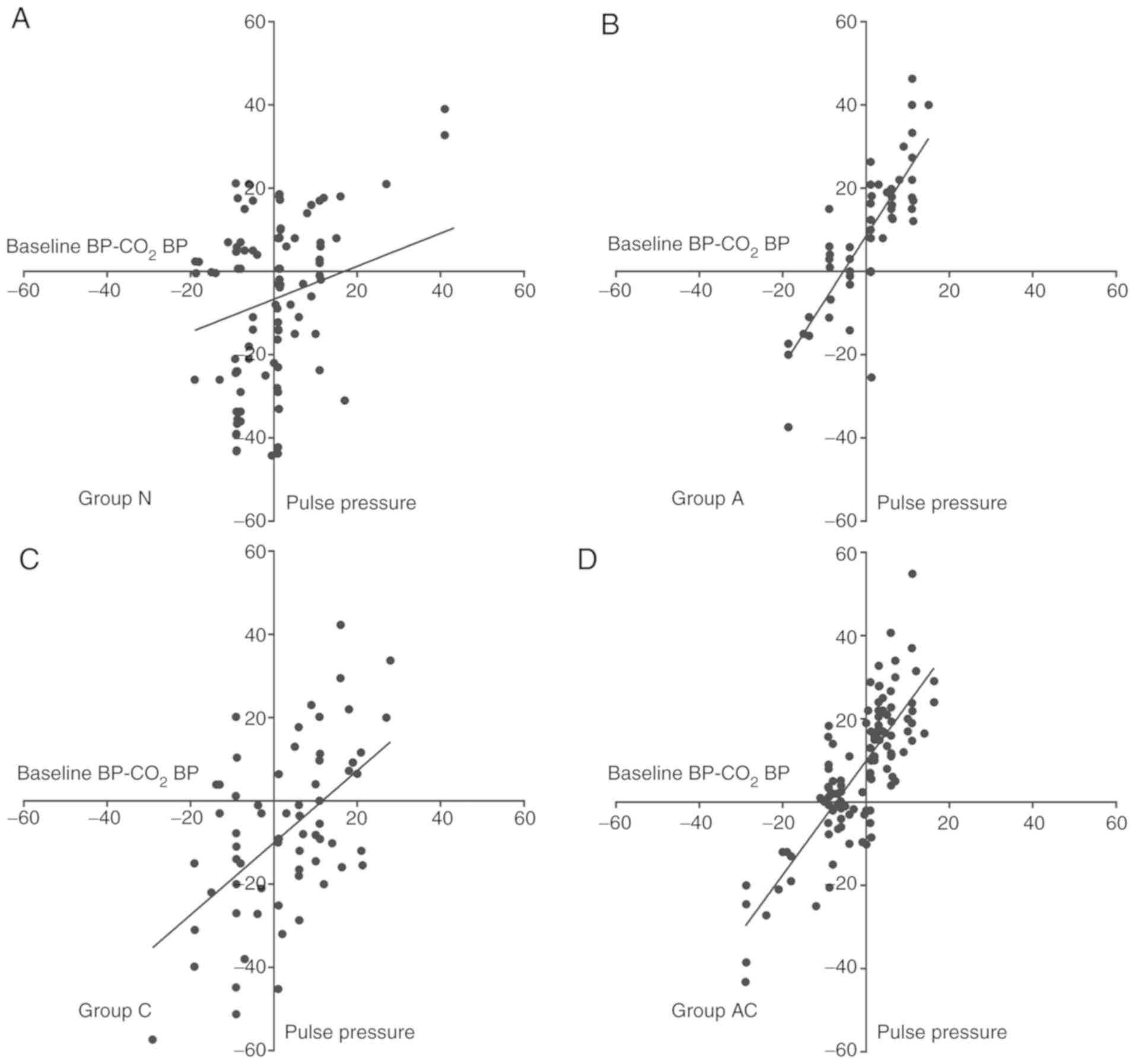 | Figure 2.Partial regression plot. Partial
regression plot (adjusted for age, sex, height, BMI, and peak
airway pressure) of the residuals of baseline pulse pressure and
the residuals of BP change after intraperitoneal CO2
insufflation demonstrates positive linear correlation. The patients
were divided into four groups according to the medication status:
(A) Control group without hypertension (normotensive subjects,
group N) and (B) groups of patients receiving monotherapy with ARBs
(group A), (C) monotherapy with CCBs (group C), and (D) combination
therapy with ARBs and CCBs (group AC). BP, blood pressure; baseline
BP, average systolic BP measured at the hospital ward the day
before surgery; CO2 BP, average systolic BP measured
within 10 min after CO2 insufflation; baseline
BP-CO2 BP, difference between baseline BP and
CO2 BP; BMI, body mass index; ARB, angiotensin receptor
blockers; CCB, calcium channel blockers. |
 | Table IV.Correlation between pulse pressure
and BP change. |
Table IV.
Correlation between pulse pressure
and BP change.
| Characteristic | Group N
(n=103) | Group A (n=52) | Group C (n=74) | Group AC
(n=113) |
|---|
| Baseline
BP-CO2 BP |
|
PCC | 0.31 | 0.73 | 0.54 | 0.83 |
|
P-value | 0.59 | <0.001 | 0.001 | <0.001 |
| CO2
BP-plateau BP |
|
PCC | 0.22 | −0.64 | −0.44 | −0.30 |
|
P-value | 0.19 | 0.11 | 0.06 | 0.06 |
Discussion
In the present study, continuous administration of
ARBs prior to surgery resulted in significantly less increase in BP
after intraperitoneal CO2 insufflation. The correlation
between the preoperative pulse pressure and increase in BP after
intraperitoneal CO2 insufflation was positive and much
stronger upon administration of ARBs compared to monotherapy with
CCBs.
The current perioperative guidelines of the American
College of Cardiology/American Heart Association suggest continuing
the administration of antihypertensive agents prior to noncardiac
surgery (10). Sudden withdrawal of
antihypertensive medication can be associated with significant
rebound hypertension (10,11). Such uncontrolled hypertension is
associated with many complications including myocardial ischemia,
renal failure, and neurologic complications (11,12).
These concepts illustrate the benefits of using antihypertensive
agents prior to surgery.
In the present study, the reason for the significant
decrease in BP fluctuation with administration of ARBs is likely
attributed to the relationship between the antihypertensive
mechanism of the drugs and the mechanism of BP change during
pneumoperitoneum. During pneumoperitoneum in laparoscopic surgery,
increased catecholamine production, plasma renin activity,
antidiuretic hormone production, and systemic vascular resistance
lead to elevated BP (13). This is
in direct contrast to the mechanism by which ARBs lower BP
(14); thus, it can be inferred that
ARBs effectively offset these processes.
Arterial stiffness is one of the major determinants
of increased systolic BP and pulse pressure, especially in patients
aged over 50 years (4,15). Considering that our patients were
older than 50 years, a strong correlation between the pulse
pressure and BP increase during pneumoperitoneum in patients with
hypertension suggests that the severity of arterial stiffness had a
significant effect on BP fluctuation. Interestingly, when compared
to CCB monotherapy, ARB administration showed a stronger
correlation between pulse pressure and BP fluctuation, while the
degree of BP fluctuation was much less. It can be interpreted that
the groups that received ARBs had more severe arterial stiffness or
that ARBs could better control hypertensive factors, other than
arterial stiffness, during intraperitoneal CO2
insufflation.
The retrospective nature of this study led to many
confounding variables. As preoperative factors, BP on the day
before surgery was considered to be an inclusion criterion;
however, the information on the degree of BP control before
admission could not be obtained. Furthermore, the basis for
prescribing each antihypertensive agent in each patient could not
be investigated. As intraoperative factors, first, the depth of
anesthesia and concentration of anesthetic agents were not
controlled. Because intraperitoneal CO2 insufflation was
performed within 15 min of anesthesia induction, the doses of
intravenous and inhalational anesthetic agents used immediately
after anesthesia induction were likely to be similar in terms of
depth of anesthesia and analgesia. Second, the variables
influencing BP and intraperitoneal pressure were not adjusted. All
patients were placed in the Trendelenburg position, but the angles
were not identical. Intraperitoneal CO2 pressure changed
frequently depending on the surgical field. The difference in the
intervention according to the lesion and mesenteric stimulation
could lead to autonomic nervous system reflexes and BP change. To
adjust factors affecting intraoperative pressure, the BP at the
beginning of CO2 insufflation was compared with the mean
BP within 30–60 min after insufflation. This is supported by the
knowledge that hemodynamic changes begin to return to the
pre-insufflation state via compensatory mechanisms approximately 15
min after gas insufflation (16).
Nonetheless, the potential impact of each of these factors remains
a limitation of this study. Third, as all hemodynamic elements were
not analyzed and the entire period of pneumoperitoneum was not
compared, the interpretation of results may not be accurate.
Fourth, the use of vasoactive agents may have affected this
outcome. Despite these uncontrolled confounding factors, the
results of this study of BP changes after intraperitoneal
CO2 insufflation under ARB administration may provide
clues to further studies on antihypertensive agents.
In this study, compared to patients without
hypertension, those with hypertension who were continuously
administered ARBs before surgery had significantly less change in
BP after intraperitoneal CO2 insufflation and no
significant hypotension during surgery. Therapy with ARBs yielded a
stronger correlation between the preoperative pulse pressure and BP
increase following pneumoperitoneum than that with CCB monotherapy;
moreover, the degree of BP fluctuation was also much less with ARB
therapy. This suggests that ARBs as preoperative antihypertensive
agents may play a positive role in managing BP in laparoscopic
surgery. However, larger controlled trials of precise hemodynamic
monitoring in consideration of potential confounding factors are
needed to validate these results. The preliminary data on the
effects of antihypertensive agents on BP during laparoscopic
surgery presented herein lay the foundation for future randomized
controlled trials and are expected to contribute to optimal
preoperative and intraoperative management.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HK designed the study, obtained the data, analyzed
and interpreted the data, and drafted and critically revised the
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Keimyung University Dongsan Hospital (Daegu, South Korea), with a
waiver for the need for informed consent.
Patient consent for publication
Not applicable.
Competing interests
The author declares that they have no competing
interests.
References
|
1
|
Kakar P and Lip GY: Towards understanding
the aetiology and pathophysiology of human hypertension: Where are
we now? J Hum Hypertens. 20:833–836. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gradman AH, Basile JN, Carter BL, Bakris
GL, Materson BJ, Black HR, Izzo JL Jr, Oparil S and Weber MA:
Combination therapy in hypertension. J Am Soc Hypertens. 4:90–98.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
London MJ: Preoperative administration of
angiotensin-converting Enzyme inhibitors or Angiotensin II receptor
blockers: Do we have enough ‘VISION’ to stop it? Anesthesiology.
126:1–3. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Safar ME, Levy BI and Struijker-Boudier H:
Current perspectives on arterial stiffness and pulse pressure in
hypertension and cardiovascular diseases. Circulation.
107:2864–2869. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
James PA, Oparil S, Carter BL, Cushman WC,
Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML,
MacKenzie TD, Ogedegbe O, et al: 2014 evidence-based guideline for
the management of high blood pressure in adults: Report from the
panel members appointed to the Eighth Joint National Committee (JNC
8). JAMA. 311:507–520. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mancia G, Fagard R, Narkiewicz K, Redón J,
Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G,
Dominiczak A, et al: 2013 ESH/ESC Guidelines for the management of
arterial hypertension: The Task Force for the management of
arterial hypertension of the European Society of Hypertension (ESH)
and of the European Society of Cardiology (ESC). J Hypertens.
31:1281–1357. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sever P: New hypertension guidelines from
the National Institute for Health and Clinical Excellence and the
british hypertension society. J Renin Angiotensin Aldosterone Syst.
7:61–63. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Whelton PK, Carey RM, Aronow WS, Casey DE
Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S,
Jamerson KA, Jones DW, et al: 2017
ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the
prevention, detection, evaluation, and management of high blood
pressure in adults: A report of the American College of
Cardiology/American Heart Association Task Force on Clinical
Practice Guidelines. Hypertension. 71:1269–1324. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Meersschaert K, Brun L, Gourdin M, Mouren
S, Bertrand M, Riou B and Coriat P: Terlipressin-ephedrine versus
ephedrine to treat hypotension at the induction of anesthesia in
patients chronically treated with angiotensin converting-enzyme
inhibitors: A prospective, randomized, double-blinded, crossover
study. Anesth Analg. 94:835–840. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fleisher LA, Fleischmann KE, Auerbach AD,
Barnason SA, Beckman JA, Bozkurt B, Davila-Roman VG, Gerhard-Herman
MD, Holly TA, Kane GC, et al: 2014 ACC/AHA guideline on
perioperative cardiovascular evaluation and management of patients
undergoing noncardiac surgery: A report of the American College of
Cardiology/American Heart Association Task Force on Practice
Guidelines. Circulation. 130:2215–2245. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Piccoli GB, Anania P, Biancone L, Mezza E,
Vischi M, Jeantet A, Rabbia C, Savio D, Rossatto D, Gai M, et al:
Hypertensive rebound after angiotensin converting enzyme inhibitor
withdrawal in diabetic patients with chronic renal failure. Nephrol
Dial Transplant. 16:1084–1085. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Malaty J and Malaty IA: Hypertensive
urgency: An important aetiology of rebound hypertension. BMJ Case
Rep. 2014(pii): bcr20142060222014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gerges FJ, Kanazi GE and Jabbour-Khoury
SI: Anesthesia for laparoscopy: A review. J Clin Anesth. 18:67–78.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Burnier M and Brunner H: Angiotensin II
receptor antagonists. Lancet. 355:637–645. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Safar ME: Systolic blood pressure, pulse
pressure and arterial stiffness as cardiovascular risk factors.
Curr Opin Nephrol Hypertens. 10:257–261. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zuckerman RS and Heneghan S: The duration
of hemodynamic depression during laparoscopic cholecystectomy. Surg
Endosc. 16:1233–1236. 2002. View Article : Google Scholar : PubMed/NCBI
|