Introduction
Cervical cancer is a common cancer type in females.
Approximately 132,000 novel cases of cervical cancer are reported
each year in China, accounting for 28% of the total number of cases
worldwide. Furthermore, an increasing proportion of females <35
years old have developed cervical cancer in the past 5 years in
China (1). The tumor
microenvironment (comprising tumor cells, nerves and blood
vessels), inflammatory cells and cytokines are closely linked to
the origin and progression of tumors (2). Chen (3)
revealed that nerve fibers and neurotrophins in the tumor
microenvironment are associated with the progression of cervical
cancer and the proportion of new nerves in cervical cancer was
higher than that in the normal cervix (3). In addition, brain-derived neurotrophic
factor (BDNF) and tropomyosin receptor kinase B (TrkB) were
indicated to be widely expressed in cervical cancer. The TrkB
expression level in cervical squamous cell carcinomas (SCC) was
reported to be higher than that in the normal cervix. Furthermore,
TrkB-positive vessels have been observed in foci of SCC (4). BDNF, a cytokine detected in a series of
non-neurogenic tumors, belongs to the neurotrophin family and has
been indicated to be involved in tumor cell proliferation and
invasion (2,5–7); it also
induces perineural invasion (8–10).
The probability of recurrence and metastasis of SCC
at the IB2 stage (also known as bulky-stage SCC) is much higher
than at the early stage of cervical cancer. Furthermore, the
prognosis of IB2-stage SCC is less favorable (11,12).
However, to date, no biomarkers to accurately and effectively
predict the recurrence and metastasis potential of cervical cancer
at the bulky stage have been identified. Of note, the serum level
of SSC antigen (SccA) reportedly is associated with the tumor
grade, size and interstitial infiltration of cervical cancer;
however, it only increased in 65% of patients with cervical cancers
vs. normal volunteers, while serum level of cancer antigen 125
(CA125) was reported to increase in only 15% patients with cervical
adenocarcinoma (13).
The role of the BDNF-TrkB regulatory system in SCC
remains to be fully elucidated. In the present study, it was
hypothesized that the potential for metastasis and recurrence of
IB2-stage SCC is associated with the expression levels of BDNF and
TrkB. Thus, data from clinical trials were retrospectively studied
to investigate whether the expression of BDNF and TrkB, as well as
other associated factors, is associated with the prognosis and
metastasis of IB2-stage SCC. The SiHa cell line is a human
papillomavirus 16-positive cervical cancer cell line, which has the
characteristics of cervical SSC. In order to explore the role of
BDNF in the progression of SCC, a Transwell assay was applied to
evaluate the effect of BDNF on the migration and invasion in SiHa
cells. The aim of the present study was to discover a biomarker
that may serve as a predictor of progression of bulky-stage SCC and
explore whether BDNF and its receptors are involved in the
angiogenesis of SCC.
Materials and methods
Patients
A total of 79 IB2-stage SCC patients treated between
January 2006 and December 2012 at the Department of Obstetrics and
Gynecology of Nanfang Hospital (affiliated to Southern Medical
University, Guangzhou, China) were enrolled in the present study.
The diagnoses of all SCC patients enrolled were performed based on
the post-operative pathological results. The general and clinical
information of the SCC patients was collected, including age, sex,
gestation, parity, Fédération Internationale de Gynécologie et
d'Obstétrique stage, pre-operative hemoglobin level, duration of
operation, type of surgery, complications, lymphovascular space
involvement (LVSI) status, depth of cervical infiltration, uterine
body invasion, parametrical infiltration, pelvic lymph node status
and post-operative therapy. The clinical and pathological data of
the patients were entered into Epidata software 3.1 version (The
EpiData Association) separately by two gynecologists, who revised
the date together, to ensure input errors were minimized. In order
to compare the expression levels of BDNF, TrkB, vascular
endothelial growth factor (VEGF) and CD105 between cervical cancer
tissue and normal cervix tissue, samples of normal comparable
cervix tissue (n=10) were obtained from uterine leiomyoma patients
who underwent a hysterectomy in the same time period as patients in
the cervical cancer cohort at the Department of Obstetrics and
Gynecology of Nanfang Hospital.
Ethics approval and informed
consent
This study was part of a clinical research project
based on a multicenter study of cervical cancer in China. It was
approved by the Ethics Committee of Nanfang Hospital, Southern
Medical University (Guangzhou, China; code: NEEC-2017-135). Written
informed consent for the use of specimens for scientific research
was provided by all patients included in the current study.
Cell culture
SiHa cells purchased from American Type Culture
Collection were provided by the laboratory at Southern Medical
University and incubated with complete Dulbecco's modified Eagle's
medium (DMEM; Gibco; Thermo Fisher Scientific, Inc.) containing 10%
fetal bovine serum (Gibco; Thermo Fisher Scientific, Inc.) and 1%
penicillin-streptomycin (Thermo Fisher Scientific, Inc.) in an
incubator at 37°C with 5% CO2. For stimulation with BDNF
(recombinant human BDNF; cat. no. 450-1; PeproTech EC, Ltd.), the
SiHa cells starved for 12 h and incubated with serum-free DMEM
supplemented with 20, 50 or 100 ng/ml BNDF for 18 h. In another
test to neutralize the effect of BDNF, the SiHa cells were divided
into three groups: The 100 ng/ml BDNF group, the BDNF (100 ng/ml)
plus BDNF antibody (1:500; cat. no. 500-P84; PeproTech) group, and
BDNF (100 ng/ml) plus TrkB inhibitor ANA12 (1 mg/ml; BioVision,
Inc.) group. SiHa cells cultured in DMEM were used as the control
group.
Immunohistochemical staining
The cervical tissue specimens were taken from
surgically cut tissue from the SCC patients and the uterine
leiomyoma patients, embedded in paraffin, cut into 4-µm thick
sections, placed on glass slides and incubated for 10 min in 3%
H2O2 at room temperature to inhibit
endogenous peroxidases. The slides were then incubated with
3,3-diaminobenzidine (DAB) for 10 min, washed with PBS, stained
with 10% hematoxylin, dehydration with gradient ethanol. After
washing with PBS, the samples were blocked by incubation with 5%
goat serum (cat. no. ab 138478; Abcam) at room temperature for 10
min. The primary antibody reaction was performed at 4°C overnight
in 1% goat serum in PBS containing the corresponding antibody [BDNF
(1:500; cat. no. ab203573; Abcam), TrkB (1:500; cat. no. SC-8316;
Santa Cruz Biotechnology, Inc.), VEGF (1:250; cat. no. ab32152;
Abcam), CD105 (1:500; cat. no. ab135528; Abcam) and PBS (as the
negative control)]. After triple washing with PBS, the slides were
incubated with the secondary antibody (Goat Anti-Mouse Anti-Rabbit
IgG/IgM H&L; 1:100; cat. no. ab2891; Abcam) for 30 min at room
temperature.
Average optical density (IOD) and
microvessel density (MVD) evaluation
The images were captured on a Nikon Bx51 camera
(Nikon Corporation). DAB-stained regions of interest were defined
based on their immunohistochemical staining profiles in in a
constant manner. To analyze the immunohistochemically stained
slides, 10 fields of the target slide at a magnification of ×400
were captured and the average integrated optical density (IOD) was
analyzed with Image Pro Plus v6.0 software (Media Cybernetics,
Inc.). Microvessel density (MVD) was determined by immunostaining
for CD105 according to Weidner's method (14). In brief, single brown-stained
endothelial cell or clusters of brown-stained endothelium (with or
without lumen) were counted as individual vessels. The slides were
screened at a magnification of ×100–200 under an upright microscope
to determine the field of the target area containing large number
of positive vessels. Three fields at the magnification of ×400 that
had the highest concentrations of microvessels were selected and
the number of microvessels was counted. The mean value of the three
fields was taken as the mean MVD.
Transwell migration and invasion
assay
The migration and invasion capacity of SiHa cells
were determined using Transwell plates for 24-well plates (6.5 mm;
pore size 8 µm; Corning, Inc.) according to the manufacturer's
protocol. For the cellular migration assay, the pre-treated SiHa
cells were suspended in 600 µl serum-free DMEM at a density of
105 cells/ml and seeded into the upper chambers of
Transwell plates; 100 µl of serum-free DMEM was supplied into the
lower chamber. After 24 h of incubation at 37°C, the migrated tumor
cells on the lower side of the filter were fixed with 4%
paraformaldehyde and stained with crystal violet (Ubio).
For the cellular invasion assay, the procedure was
similar to that described above, except that the inserted filter
was pre-coated with Matrigel (BD Biosciences; diluted at 1:6) and
the plates were incubated for 24 h at 37°C.
The migrated and invaded cells were counted in
triplicate fields of view three times under an Olympus CKX41
inverted microscope (Olympus Corporation) at a magnification of
×100.
Western blot analysis
The treated cells were lysed with
radioimmunoprecipitation assay protein lysis buffer (containing
protease inhibitors) and centrifuged at 12,000 × g or 4 min at 4°C.
The protein concentration of the supernatant was detected with a
bicinchoninic acid assay kit (BioVision). A total of 40 mg of the
total protein samples were loaded onto 12% SDS-PAGE gel, separated
by electrophoresis and transferred onto a polyvinylidene difluoride
membrane (Sigma-Aldrich; Merck KGaA). The membranes were blocked
with Tris-buffered saline containing 5% skimmed milk for 1 h,
incubated with VEGF antibody (1:500; cat. no. 251622; ZEN-Biotech)
overnight at 4°C, triple-washed with Tris-buffered saline
containing Tween-20, reacted with secondary antibody (1:500; cat.
no. 220173; ZEN-Biotech Pvt. Ltd.) at room temperature for 1 h,
triple washed again, and visualized using an enhanced
chemiluminescence detection kit (GE Healthcare). The protein bands
were then exposed to X-ray film (Fujifilm).
Reverse transcription quantitative PCR
(qPCR)
Total RNA was extracted with an RNA Extraction kit
(Promega Corp.), The reaction mix contained 175 µl of RNA
polymerase, 300 nM of primer and 100 ng of RNA. The RNA was
amplified with a starting denaturation for 10 min at 95°C, 95°C for
30 sec, 56°C for 60 sec, and 72°C for 60 sec, and was repeated for
40 cycles. The PCR mixture was prepared with SYBR Green PCR Master
Mix (Toyobo), according to the manufacturer's protocol. 18srRNA
(15) was used as the endogenous
reference gene for qPCR analysis. Each reaction was performed in
triplicate. The results were analyzed using the 2−∆∆Cq
method (16). The primers used for
qPCR were as follows: VEGF forward, 5′-GCAGATTATGCGGATCAAACC-3′ and
reverse, 5′-TTTCGTTTTTGCCCCTTTCC-3′; endogenous reference forward,
5′-CCTGGATACCGCAGCTAGGA-3′; and reverse,
5′-GCGGCGCAATACGAATGCCCC-3′.
Statistical analysis
SPSS v21.0 software (IBM Corp.) was employed for
statistical analysis. Values are expressed as the mean ± the
standard deviation or standard error. A Student's t-test was
applied to evaluate the differences between two groups. Statistical
analysis of multiple groups was performed using one-way analysis of
variance, followed by Dunnett's test. The χ2-square test
was used to analyze categorical variables. The univariate analysis
of the association of factors with survival were performed using
one-way ANOVA and Student's t-test, for categorical
variables and continuous variables respectively. The Cox
proportional hazards model was employed to assess the association
of a variety of factors with survival. Survival curves were plotted
using the Kaplan-Meier method. P<0.05 was considered to indicate
statistical significance.
Results
SCC patients
The average age of the 79 SCC patients was
47.84±8.46 years (range, 24–68 years). The follow-up period after
surgical resection ranged from 1 to 13 years (average, 5.9±2.0
years). During the follow-up, 23 patients died. Additional
information on the cohort is listed in Supplemental Table SI.
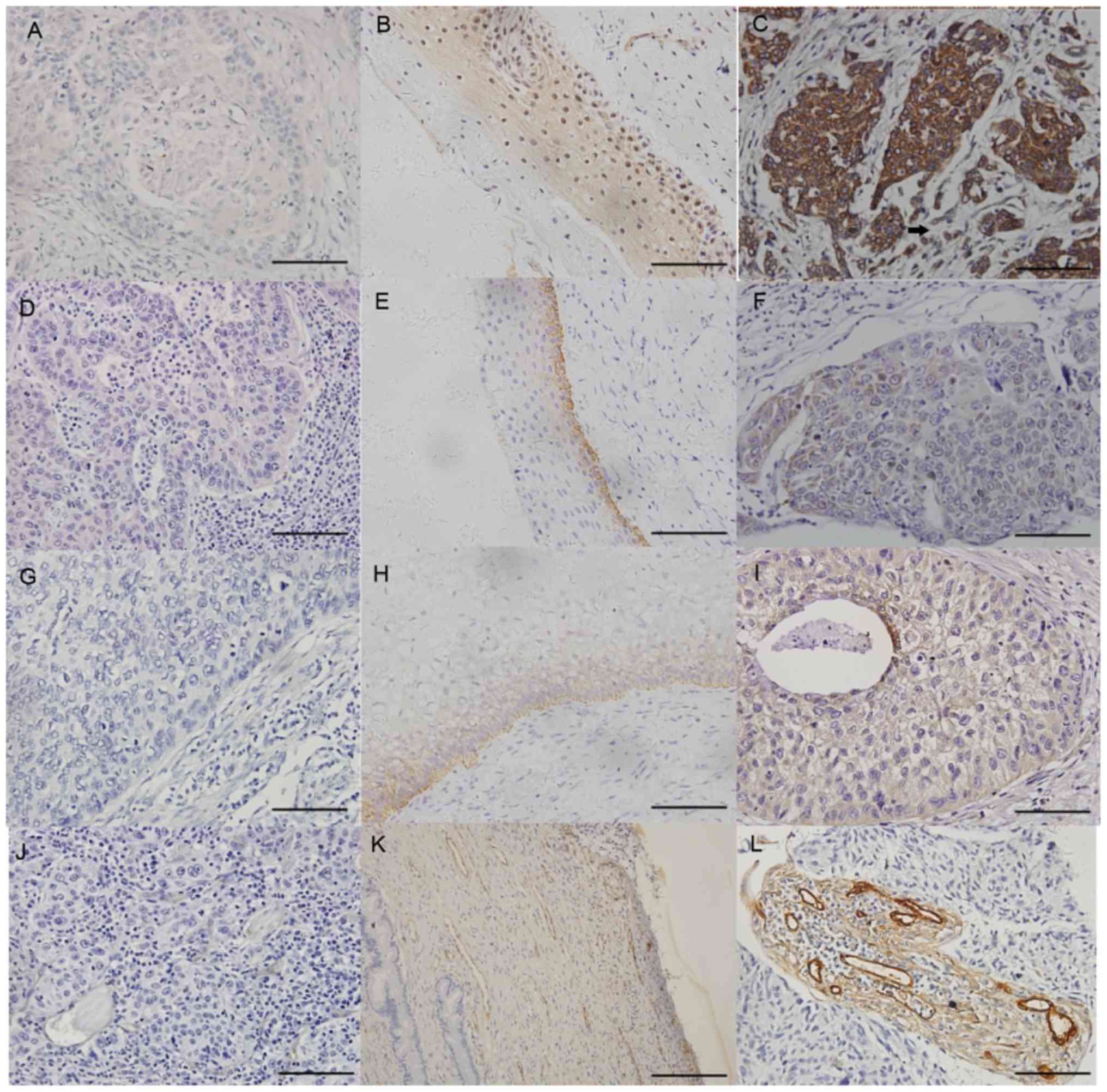
Expression and location of BDNF, TrkB,
VEGF and CD105 in IB2-stage cervical SCC tissue according to
immunochemical staining
The protein expression of BDNF, TrkB, VEGF and CD105
in the cervical cancer tissue specimens and the normal cervix
samples was evaluated by immunochemical staining with the
corresponding antibodies. BDNF, TrkB and VEGF were identified to be
widely expressed in the tumor cells with positive rates of 97.6,
88.2 and 93.0%, respectively. CD105 was located in the capillary
wall with a positive rate of 92.4%. TrkB and VEGF were also
detected in the capillary walls of the cancer specimens (Fig. 1). Furthermore, the expression levels
of BDNF, VEGF and CD105 in SCC tissues were higher than those in
normal cervical tissues (P<0.001, P<0.05 and P<0.05,
respectively). However, the expression levels of TrkB in SCC
tissues and normal tissues were not significantly different
(P>0.05; Table SII).
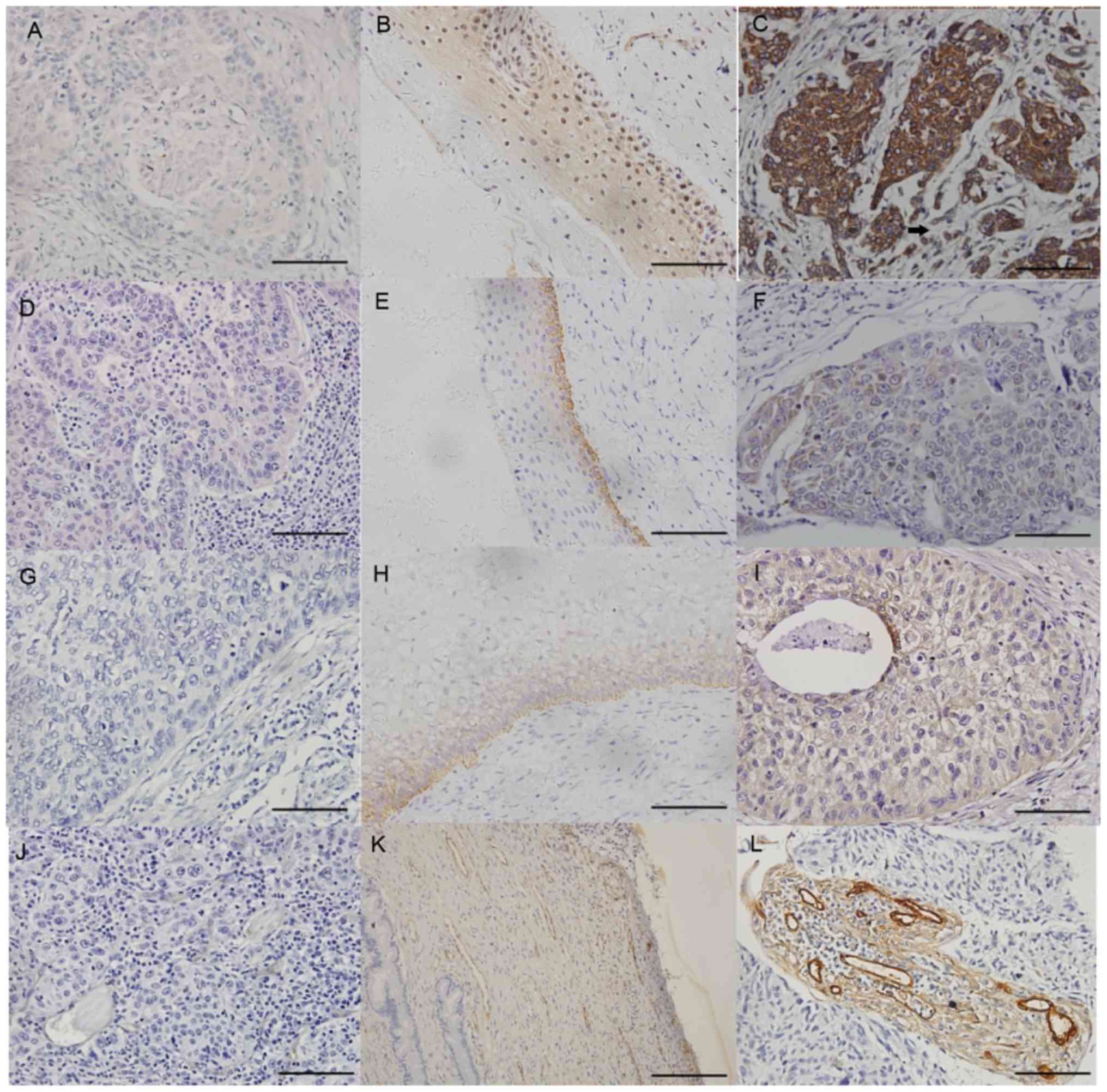 | Figure 1.Immunohistochemical staining for BDNF,
TrkB, VEGF and CD105 in cervical cancer specimens. The expression
of (A-C) BDNF, (D-F) TrkB, (G-I) VEGF and (J-L) CD105 was detected
by immunohistochemical staining in negative controls, normal
cervical epithelium and cervical cancer specimens, respectively,
from left to right. Negative controls were incubated with PBS only
instead of primary antibody. The scale bar was 50 µm in A-I and 100
µm in J-L. The arrow in C indicates negative staining for BDNF in
the cervical cancer stroma. BDNF, brain-derived neurotrophic
factor; TrkB, tropomyosin receptor kinase B; VEGF, vascular
endothelial growth factor. |
Association of the expression of BDNF,
TrkB and VEGF, as well as MVD, with clinicopathological parameters
of the IB2-stage SCC patients
The correlation of the expression levels of BDNF,
TrkB and VEGF, as well as the MVD (CD105 positivity), with various
clinical indexes was statistically analyzed. The expression of BDNF
was significantly correlated with positive LVSI (P<0.001),
pelvic lymph node metastasis (P<0.05) and exogenous gross type
(P<0.05). Furthermore, the expression of VEGF was associated
with larger tumor size (P<0.05) and positive LVSI (P<0.05).
No statistically significant correlation was identified between the
expression of BDNF, TrkB and VEGF, as well as the MVD (estimated by
CD105 stain), and other clinicopathological parameters, including
age and DSI (P>0.05; Tables I and
II).
 | Table I.Analysis of the association between
BDNF and TrkB with clinicopathological indexes of IB2-stage
cervical differentiated squamous cell carcinoma. |
Table I.
Analysis of the association between
BDNF and TrkB with clinicopathological indexes of IB2-stage
cervical differentiated squamous cell carcinoma.
|
| BDNF | TrkB |
|---|
|
|
|
|
|---|
| Characteristic | N | Mean ± SD | P-value | N | Mean ± SD | P-value |
|---|
| Age (year) |
|
|
|
|
|
|
|
≤35 | 5 | 0.06±0.03 | 0.978 | 5 | 0.01±0.01 | 0.068 |
| >35
or ≤50 | 48 | 0.06±0.04 |
| 44 | 0.03±0.03 |
|
|
>50 | 26 | 0.07±0.03 |
| 26 | 0.02±0.02 |
|
| Tumor diameter
(cm) |
|
| 0.209 |
|
| 0.425 |
| >4,
<5 | 40 | 0.06±0.04 |
| 37 | 0.02±0.02 |
|
| ≥5 | 39 | 0.07±0.04 |
| 38 | 0.03±0.03 |
|
| Gross type |
|
| 0.046 |
|
| 0.249 |
|
Exogenous | 63 | 0.07±0.04 |
| 59 | 0.02±0.02 |
|
|
Ulcerative | 11 | 0.05±0.02 |
| 11 | 0.03±0.02 |
|
| DSI |
|
| 0.188 |
|
| 0.441 |
| No | 33 | 0.06±0.03 |
| 31 | 0.03±0.02 |
|
|
Yes | 44 | 0.07±0.04 |
| 42 | 0.02±0.02 |
|
| LVSI |
|
| 0.001 |
|
| 0.256 |
|
Yes | 13 | 0.09±0.04 |
| 11 | 0.04±0.04 |
|
| No | 66 | 0.06±0.03 |
| 64 | 0.02±0.02 |
|
| Pelvic lymph node
metastasis |
|
| 0.010 |
|
| 0.202 |
| No | 56 | 0.06±0.03 |
| 54 | 0.02±0.02 |
|
|
Yes | 23 | 0.08±0.04 |
| 21 | 0.03±0.03 |
|
 | Table II.Analysis of the association of VEGF
and MVD with clinicopathological characteristics of IB2-stage
cervical squamous cell carcinoma. |
Table II.
Analysis of the association of VEGF
and MVD with clinicopathological characteristics of IB2-stage
cervical squamous cell carcinoma.
|
| MVD | VEGF |
|---|
|
|
|
|
|---|
| Characteristic | N | Mean ± SD | P-value | N | Mean ± SD | P-value |
|---|
| Age (year) |
|
|
|
|
|
|
|
≤35 | 7 | 11.76±2.81 | 0.878 | 11 | 0.78±0.05 | 0.567 |
| >35
or ≤50 | 43 | 12.11±2.71 |
| 34 | 0.08±0.03 |
|
|
>50 | 25 | 10.90±2.71 |
| 30 | 0.08±0.01 |
|
| Tumor diameter
(cm) |
|
| 0.463 |
|
| 0.006 |
| >4,
<5 | 37 | 11.84±2.89 |
| 40 | 0.06±0.05 |
|
| ≥5 | 38 | 12.31±2.60 |
| 39 | 0.09±0.06 |
|
| Gross type |
|
| 0.381 |
|
| 0.412 |
|
Exogenous | 59 | 11.79±2.67 |
| 63 | 0.07±0.06 |
|
|
Ulcerative | 11 | 12.57±2.90 |
| 11 | 0.08±0.05 |
|
| DSI |
|
| 0.862 |
|
| 0.852 |
| No | 31 | 11.99±2.86 |
| 33 | 0.07±0.05 |
|
|
Yes | 42 | 12.10±2.60 |
| 44 | 0.07±0.06 |
|
| LVSI |
|
| 0.695 |
|
| 0.005 |
|
Yes | 12 | 12.36±1.83 |
| 13 | 0.11±0.04 |
|
| No | 63 | 12.02±2.88 |
| 66 | 0.06±0.05 |
|
| Pelvic lymph node
metastasis |
|
| 0.403 |
|
| 0.222 |
| No | 54 | 12.24±2.94 |
| 56 | 0.07±0.06 |
|
|
Yes | 21 | 11.65±2.10 |
| 23 | 0.08±0.05 |
|
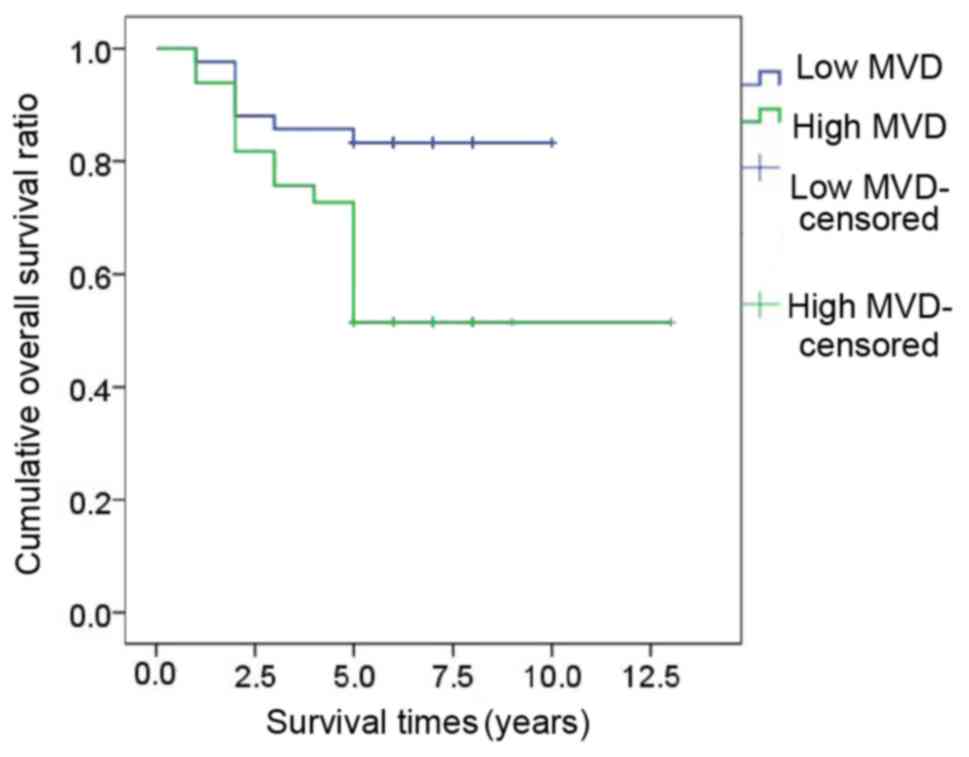
High MVD is an independent predictor
of poor prognosis in IB2-stage SCC patients
Among the 79 SCC patients, 23 patients died as the
consequence of cervical cancer in the follow-up time of 13 years;
the 5-year overall survival (OS) rate of the SCC patients was
70.9%. According to the univariate analysis of the association of
factors with survival, age >35 years, as well as higher
expression of VEGF and MVD were associated with a poorer prognosis
regarding OS (P<0.05; Tables
SIII and SIV). However, Cox
multivariate regression analysis revealed that only high MVD was an
independent prognostic factor for OS (hazard ratio, 2.723; 95% CI:
1.097–6.762; P<0.05; Fig. 2;
Table SV), the expression of BDNF
and VEGF were not independent prognostic factors for OS in SCC
patients (P>0.05).
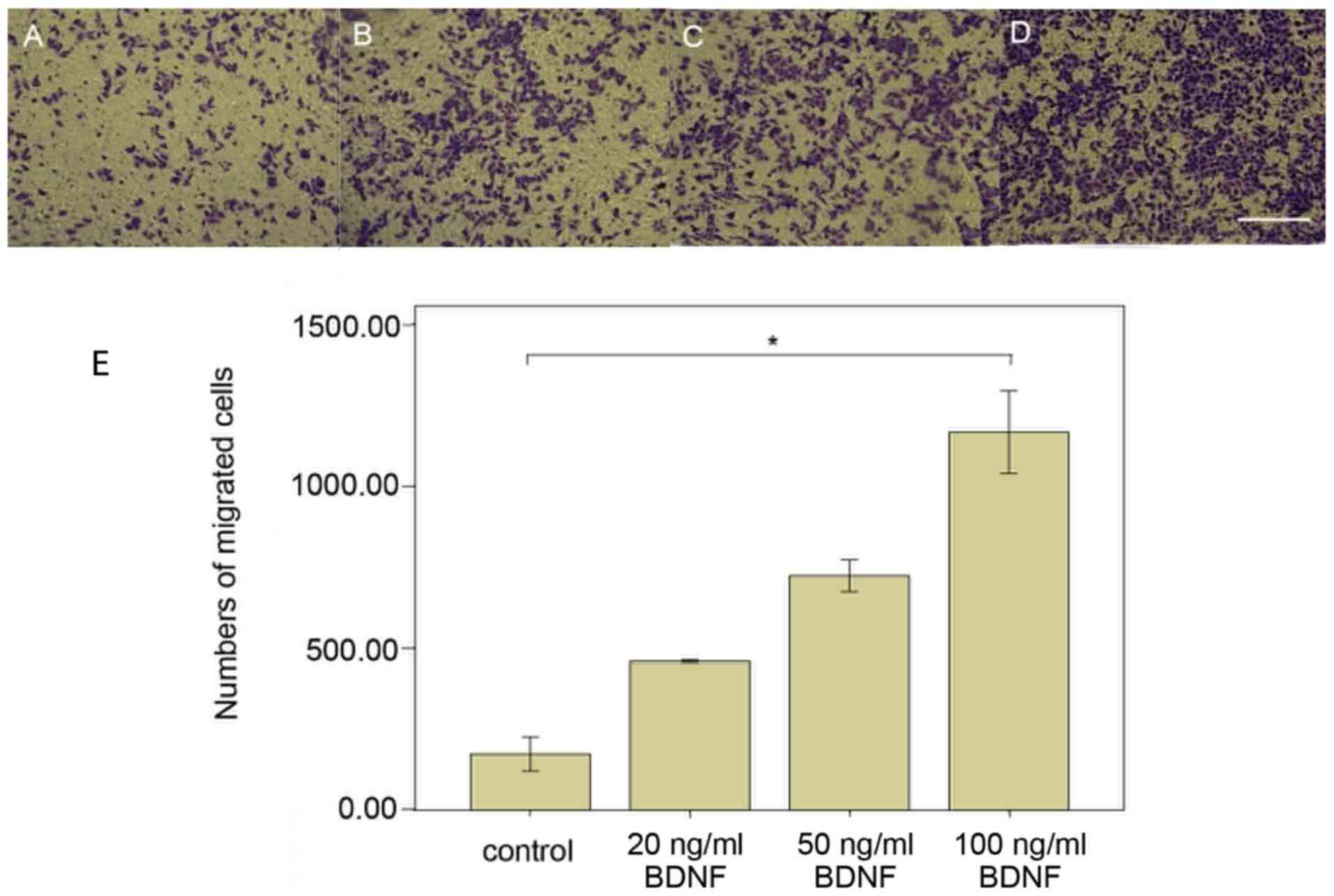
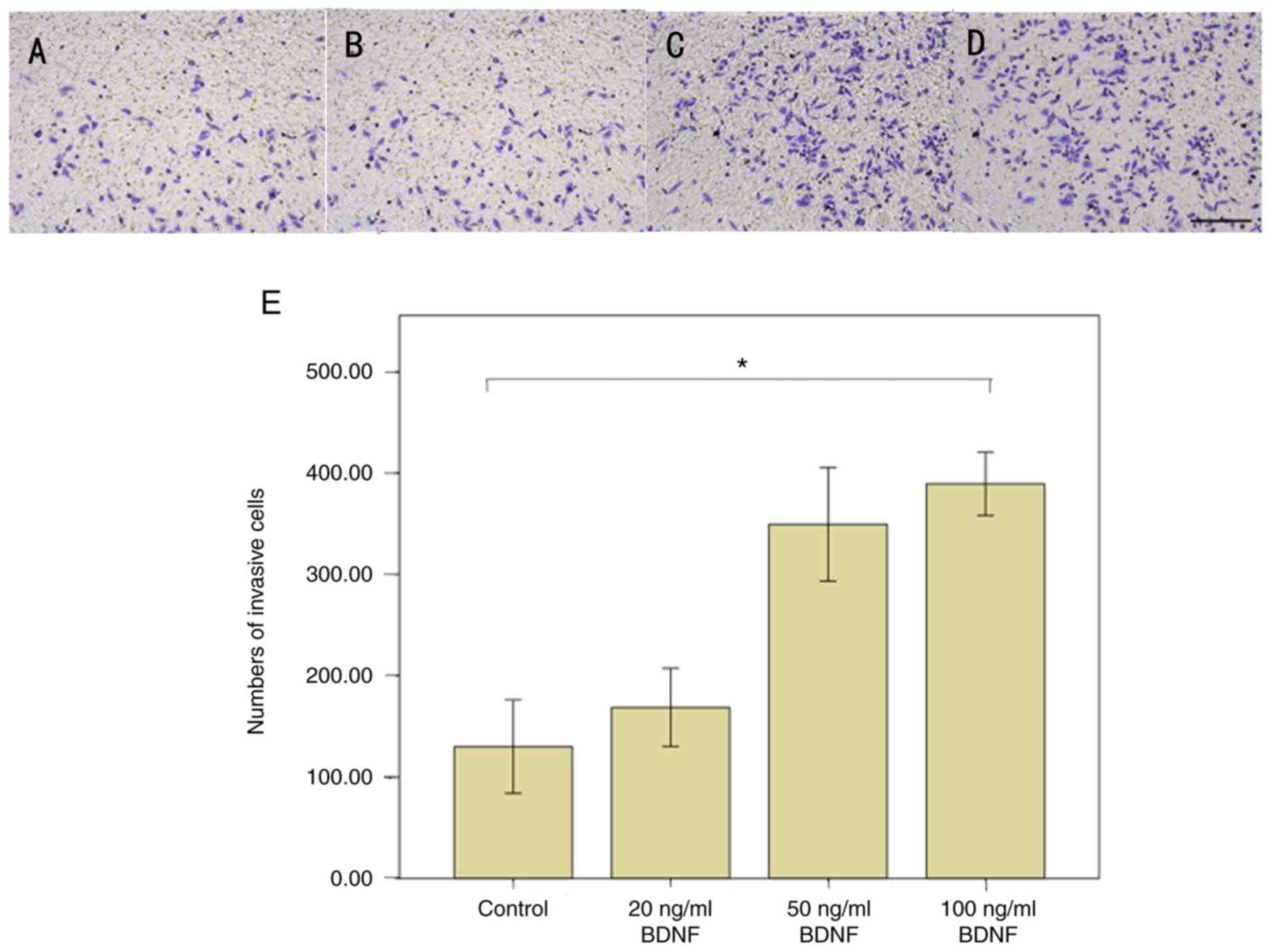
BDNF enhances the cellular migratory
and invasive potential of SiHa cells
The above results indicated that BDNF is closely
linked to the invasive metastatic ability of SCC cells. Therefore,
the effect of BDNF on the cellular migratory and invasive abilities
of the SiHa cell line was assessed by using Transwell assays. The
results indicated that BDNF significantly promoted cellular
migration (Fig. 3) and invasion
(Fig. 4) of SiHa cells in a
dose-dependent manner. The maximal effective dose was 100 ng/ml
BDNF in the two assays among the 20, 50, and 100 ng/ml BDNF groups
(P<0.001).
Effect of BDNF-TrkB pathway on VEGF-A
regulation
It was indicated that exogenous BDNF stimulation of
SiHa cells enhanced VEGF-A protein expression. This response
reached a maximum when the concentration of BDNF was 100 ng/ml
(P<0.05). Furthermore, a similar trend was observed regarding
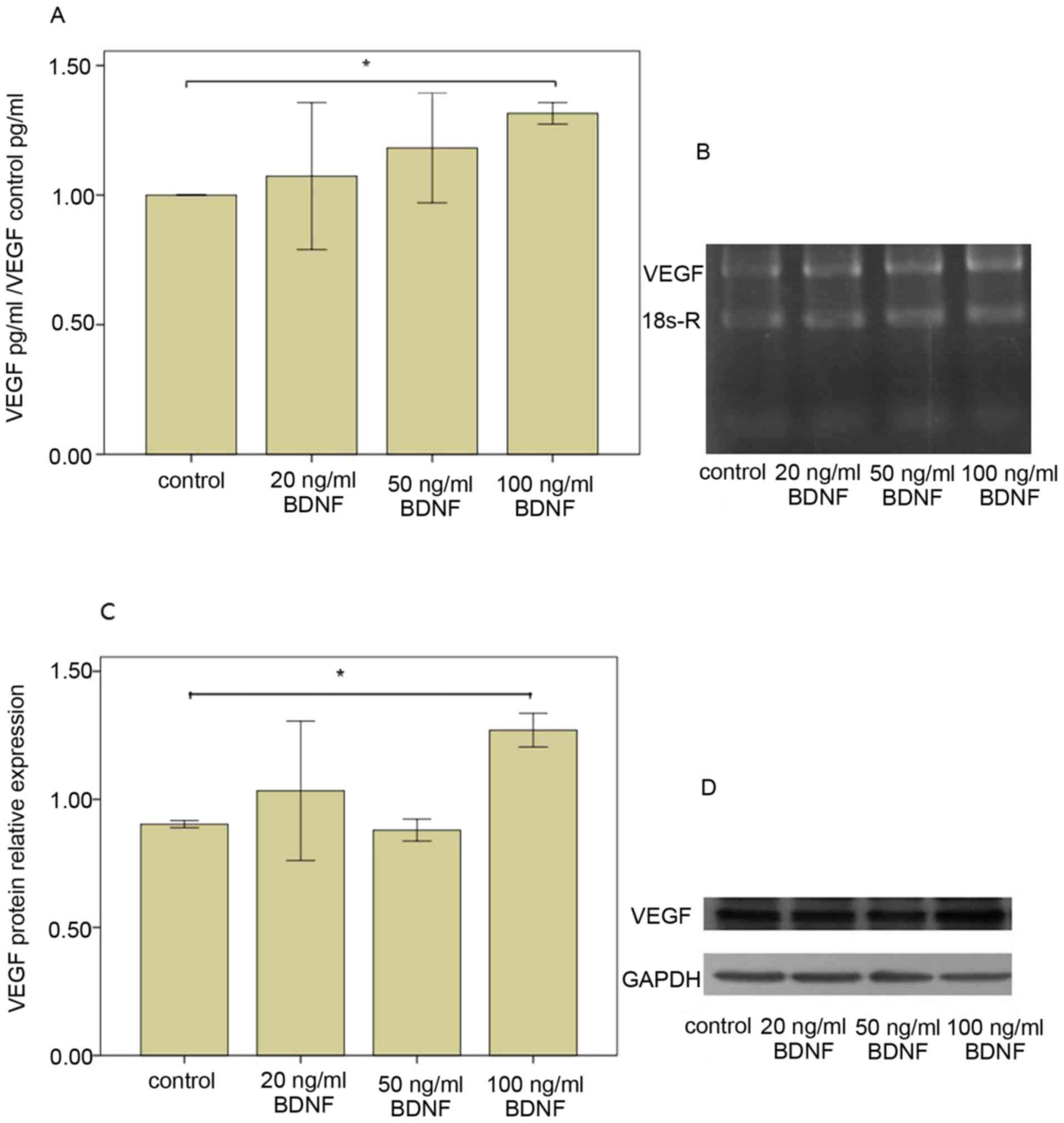
the mRNA expression of VEGF-A (P<0.05; Fig. 5).
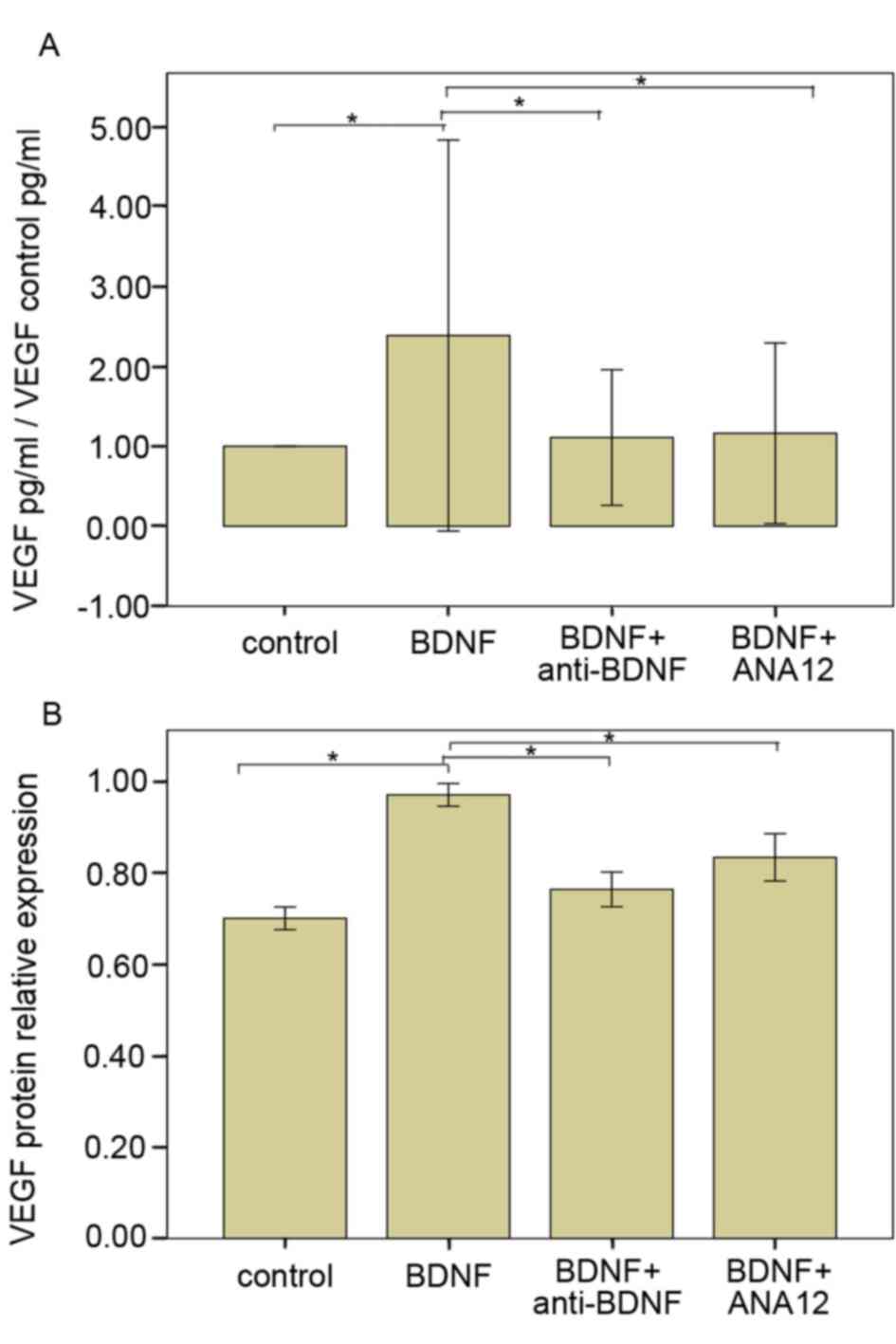
Addition of anti-BDNF antibody or inhibitor of
tyrosine kinase receptor (ANA12, an inhibitor of TrkB receptors)
obviously prevented the BDNF-induced VEGF-A expression in SiHa
cells (P<0.05), indicating that VEGF-A induction by BDNF was
mediated through TrkB receptor binding specifically. Similar
results were obtained from the western blot detection of VEGF-A
(P<0.05; Fig. 6).
Discussion
Pelvic lymph node metastasis is thought to be one of
the most important sources of metastasis in cervical cancer.
According to the National Comprehensive Cancer Network guidelines
from 2015, it is a high-risk factor in cervical cancer patients
(17).
BDNF reportedly promotes VEGF-C expression in
bladder and cervical tumors. VEGF-C was verified to be positively
correlated with pelvic lymph node metastasis in cervical cancer
(18,19). Lin et al (20) reported that upregulation of BDNF is
always accompanied with increased VEGF-C expression. Furthermore,
they indicated that BDNF promoted VEGF-C-associated
lymphangiogenesis via the mitogen-activated protein kinase
kinase/ERK/mTOR signaling pathway, and further induced lymphatic
metastasis. These activities were profoundly inhibited by BDNF
knockdown in vivo.
In the present study, BDNF, TrkB, VEGF and CD105
expression was analyzed in the tumor samples of 79 patients with
IB2-stage SCC of the cervix, and it was revealed that the BDNF
level in cervical cancer samples was significantly associated with
LVSI, pelvic lymph node metastasis. The ability of BDNF to
stimulate aggressive behavior was further verified in vitro
via cellular migration and invasion assays. Macdonald et al
(21) investigated data from a large
database, indicating that positive lymphatic metastasis is a
predictor for poor prognosis in cervical cancer, which is
negatively associated with the number of nodes involved. According
to this previous study, radical hysterectomy and lymphadenectomy is
the classic and standardized type of surgery for certain cervical
cancer patients. However, Ferrandina et al (22) reported that the pelvic lymph node
metastasis rate of locally advanced cervical cancer was only 10.9%,
which means that a large proportion of patients with locally
advanced cervical cancer without lymph node metastasis underwent
unnecessary pelvic lymph node dissection.
The results of the present study indicated that the
expression of BDNF is closely linked to positive LVSI and pelvic
lymph node metastasis, suggesting that BDNF may be an effective
predictor of lymph node metastasis. Furthermore, BDNF may be a
useful indicator to accurately determine the status of lymph node
metastasis prior to surgery and to facilitate the selection of
appropriate candidates for pelvic lymph node dissection.
The results of the present study also revealed that
VEGF expression was associated with tumor size and positive LVSI.
In addition, MVD was an independent prognostic factor for OS of
patients with SCC of the cervix. Indeed, Duff et al
(23) reported a similar correlation
of MVD (CD105-positive cells) or VEGF with cervical cancer. Barbu
et al (24) reported on the
upregulation of VEGF and angiogenesis in cervical adenocarcinomas,
which was mainly distributed at the invasion front and indicated
poor outcome. The results of a mechanistic in vitro
experiment of the present study indicated that exogenous BDNF
acting on SiHa cells enhanced VEGF-A expression, and this induction
may be blocked by BDNF antibodies or an antagonist of its receptor
TrkB (25). Therefore, it may be
speculated that BDNF promotes neovascularization by induction of
VEGF-A expression through binding to its high-affinity receptor
TrkB, which indirectly contributes to the progression of the tumor.
Therefore, most studies have mainly focused on vascular targeting
therapies for cervical cancers, including sunitinib, malate and
sorafenib (26). In 2014, the US
Food and Drug Administration approved bevacizumab for the clinical
treatment of cervical cancer (27).
However, anti-vascular targeted therapies are usually accompanied
by considerable side effects: 40% of cervical cancer patients who
received vascular targeting therapy had complications, including
genitourinary tract spasm and thrombotic disorder, and 2.8% of the
patients died as a result (28). An
experiment using animal pancreatic cancer xenografts in a study by
Zhao et al (29) revealed
that TrkB antagonist significantly reduced the volume of
xenografts. Based on the present results, anti-BDNF-TrkA treatment
combined with anti-VEGF may be a potential strategy for the
clinical treatment of cervical cancers.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This study was supported by key projects of the
National Science & Technology Pillar Program during the Twelfth
Five-year Plan Period (grant no. 2014BAI05B03), the National
Natural Science Foundation of Guangdong, China (grant no.
2015A030311024), the Medical Research Foundation of Guangdong,
China (grant no. A2015063) and the Presidential Foundation of
Nanfang Hospital of Southern Medical University (grant no.
2015C015).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YQ and WL contributed to the study design/planning,
data collection/entry, data analysis/statistics and data
interpretation. YQ contributed to the preparation of the manuscript
and literature analysis/search. MH, WW, SK, LC, BL, ZC, CL, JH and
XC contributed to the data collection/entry. CC and PL contributed
to the study design/planning, data collection/entry, data
interpretation and funds collection. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
This study was part of a retrospective clinical
research project based on a multicenter study of cervical cancer in
China. It was approved by the Ethics Committee of Nanfang Hospital,
Southern Medical University (Guangzhou, China; code:
NEEC-2017-135). Written informed consent for the use of specimens
for scientific research was provided by all patients included in
the current study.
Patients' consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Li S, Hu T, Lv W, Zhou H, Li X, Yang R,
Jia Y, Huang K, Chen Z, Wang S, et al: Changes in prevalence and
clinical characteristics of cervical cancer in the People's
Republic of China: A study of 10,012 cases from a nationwide
working group. Oncologist. 18:1101–1107. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Spencer A, Yu L, Guili V, Reynaud F, Ding
Y, Ma J, Jullien J, Koubi D, Gauthier E, Cluet D, et al: Nerve
growth factor signaling from membrane microdomains to the nucleus:
Differential regulation by caveolins. Int J Mol Sci. 18:E6932017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen CL: Qualitative study on the fine
structure of the cervical cancer. Chin J Pract Gyneco Obstetr.
5:440–444. 2015.(In Chinese).
|
|
4
|
Liu YL: Expression of brain- derived
neurotrophic factor and its low affinity receptor P75 in stage IB1-
IIB cervical squamous cell carcinoma and normal cervical tissues.
Chin J Pract Gyneco Obstetr. 33:200–204. 2017.(In Chinese).
|
|
5
|
Höfner T, Klein C, Eisen C,
Rigo-Watermeier T, Haferkamp A, Trumpp A and Sprick MR: The
influence of prostatic anatomy and neurotrophins on basal prostate
epithelial progenitor cells. Prostate. 76:114–121. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Johnson MD, Stone B, Thibodeau BJ,
Baschnagel AM, Galoforo S, Fortier LE, Ketelsen B, Ahmed S, Kelley
Z, Hana A, et al: The significance of Trk receptors in pancreatic
cancer. Tumour Biol. 39:10104283176922562017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Noh SJ, Kim KM and Jang KY: Individual and
co-expression patterns of nerve growth factor and heme oxygenase-1
predict shorter survival of gastric carcinoma patients. Diagn
Pathol. 12:482017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pundavela J, Roselli S, Faulkner S, Attia
J, Scott RJ, Thorne RF, Forbes JF, Bradshaw RA, Walker MM, Jobling
P and Hondermarck H: Nerve fibers infiltrate the tumor
microenvironment and are associated with nerve growth factor
production and lymph node invasion in breast cancer. Mol Oncol.
9:1626–1635. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Roh J, Muelleman T, Tawfik O and Thomas
SM: Perineural growth in head and neck squamous cell carcinoma: A
review. Oral Oncol. 51:16–23. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sakamoto Y, Kitajima Y, Edakuni G,
Sasatomi E, Mori M, Kitahara K and Miyazaki K: Expression of Trk
tyrosine kinase receptor is a biologic marker for cell
proliferation and perineural invasion of human pancreatic ductal
adenocarcinoma. Oncol Rep. 8:477–484. 2001.PubMed/NCBI
|
|
11
|
Alouini S, Rida K and Mathevet P: Cervical
cancer complicating pregnancy: Implications of laparoscopic
lymphadenectomy. Gynecol Oncol. 108:472–477. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Landoni F, Maneo A, Colombo A, Placa F,
Milani R, Perego P, Favini G, Ferri L and Mangioni C: Randomised
study of radical surgery versus radiotherapy for stage Ib-IIa
cervical cancer. Lancet. 350:535–540. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Scambia G, Benedetti Panici P, Foti E,
Amoroso M, Salerno G, Ferrandina G, Battaglia F, Greggi S, De
Gaetano A and Puglia G: Squamous cell carcinoma antigen: prognostic
significance and role in the monitoring of neoadjuvant chemotherapy
response in cervical cancer. J Clin Oncol. 12:2309–2316. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Weidner N: Chapter 14. Measuring
intratumoral microvessel density. Methods Enzymol. 444:305–323.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mohammadi P, Saidijam M, Kaki A, Etemadi
K, Shabab N and Yadegarazari R: A pilot study of CK19, CK20 and GCC
mRNA in the peripheral blood as a colorectal cancer biomarker
panel. Int J Mol Cell Med. 5:30–36. 2016.PubMed/NCBI
|
|
16
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Koh WJ, Greer BE, Abu-Rustum NR, Apte SM,
Campos SM, Cho KR, Chu C, Cohn D, Crispens MA, Dorigo O, et al:
Cervical cancer, version 2.2015. J Natl Compr Canc Netw.
13:395–404. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dai Y, Tong R, Guo H, Yu T and Wang C:
Association of CXCR4, CCR7, VEGF-C and VEGF-D expression with lymph
node metastasis in patients with cervical cancer. Eur J Obstet
Gynecol Reprod Biol. 214:178–183. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kawamoto M, Onishi H, Ozono K, Yamasaki A,
Imaizumi A, Kamakura S, Nakano K, Oda Y, Sumimoto H and Nakamura M:
Tropomyosin-related kinase B mediated signaling contributes to the
induction of malignant phenotype of gallbladder cancer. Oncotarget.
8:36211–36224. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lin CY, Wang SW, Chen YL, Chou WY, Lin TY,
Chen WC, Yang CY, Liu SC, Hsieh CC, Fong YC, et al: Brain-derived
neurotrophic factor promotes VEGF-C-dependent lymphangiogenesis by
suppressing miR-624-3p in human chondrosarcoma cells. Cell Death
Dis. 8:e29642017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Macdonald OK, Chen J, Dodson M, Lee CM and
Gaffney DK: Prognostic significance of histology and positive lymph
node involvement following radical hysterectomy in carcinoma of the
cervix. Am J Clin Oncol. 32:411–416. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ferrandina G, Distefano M, Mascilini F,
Gallotta V, Chiantera V, Cosentino F, Costantini B, Ercoli A,
Pedone Anchora L, Fanfani F, et al: Could lymphadenectomy be
avoided in locally advanced cervical cancer patients administered
preoperative chemoradiation? A large-scale retrospective study. Eur
J Surg Oncol. 43:2270–2276. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Duff SE, Li C, Garland JM and Kumar S:
CD105 is important for angiogenesis: Evidence and potential
applications. FASEB J. 17:984–992. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Barbu I, Craitoiu S, Simionescu CE,
Dragnei AM and Margaritescu C: CD105 microvessels density, VEGF,
EGFR-1 and c-erbB-2 and their prognostic correlation in different
subtypes of cervical adenocarcinoma. Rom J Morphol Embryol.
54:519–530. 2013.PubMed/NCBI
|
|
25
|
Zhang J, Liu J, Zhu C, He J, Chen J, Liang
Y, Yang F, Wu X and Ma X: Prognostic role of vascular endothelial
growth factor in cervical cancer: A meta-analysis. Oncotarget.
8:24797–24803. 2017.PubMed/NCBI
|
|
26
|
Godoy-Ortiz A, Plata Y, Alcaide J, Galeote
A, Pajares B, Saez E, Alba E and Sánchez-Muñoz A: Bevacizumab for
recurrent, persistent or advanced cervical cancer: Reproducibility
of GOG 240 study results in ‘real world’ patients. Clin Transl
Oncol. 20:922–927. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Penson RT, Huang HQ, Wenzel LB, Monk BJ,
Stockman S, Long HJ III, Ramondetta LM, Landrum LM, Oaknin A, Reid
TJ, et al: Bevacizumab for advanced cervical cancer:
Patient-reported outcomes of a randomised, phase 3 trial (NRG
Oncology-Gynecologic Oncology Group protocol 240). Lancet Oncol.
16:301–311. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sturdza A, Hofmann S, Kranawetter M,
Polterauer S, Grimm C, Krainer M, Kirisits C, Pötter R, Reinthaller
A and Schwameis R: Increased genitourinary fistula rate after
bevacizumab in recurrent cervical cancer patients initially treated
with definitive radiochemotherapy and image-guided adaptive
brachytherapy. Strahlenther Onkol. 193:1056–1065. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhao CM, Hayakawa Y, Kodama Y, Muthupalani
S, Westphalen CB, Andersen GT, Flatberg A, Johannessen H, Friedman
RA, Renz BW, et al: Denervation suppresses gastric tumorigenesis.
Sci Transl Med. 6:250ra1152014. View Article : Google Scholar : PubMed/NCBI
|