1. Introduction
The rate of psychological co-morbidity of
dermatological disorders in Europe is not known, the patient being
generally treated only dermatologically and in terms of other much
more studied co-morbidities. In other diseases, such as diabetes,
heart disease and asthma, the presence of depression is much more
widely studied than in dermatological diseases.
The World Health Organization's slogan ‘There is no
health without mental health’ highlights the fact that mental
health contributes bidirectionally to physical health (1). On the one hand, mental health can
affect physical health, but also physical health can affect mental
health.
European studies have shown that patients with
eczema, acne, psoriasis and hidradenitis suppurativa pose an
increased risk of depression (2-4).
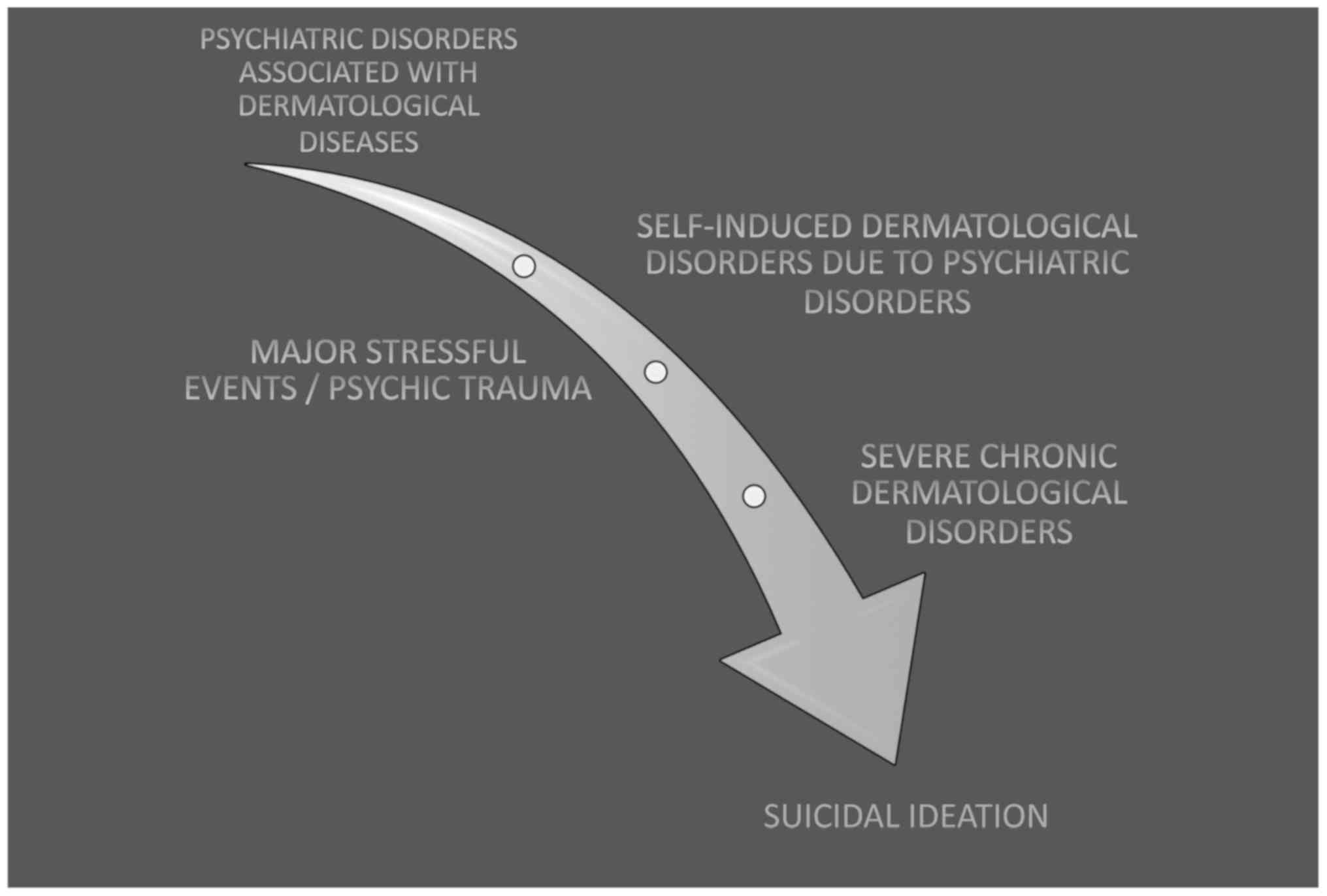
Although a less approached topic, suicide is
encountered even in dermatology. The risk of suicide may be
preexisting, may occur as a complication of skin disorders or can
be triggered by drugs such as interferon. The risk of suicidal
behavior can be an important factor in the general management of
the dermatological patient. Patients at risk should be specifically
asked about suicidal ideation and trends, with immediate
intervention required (5). In
dermatology, the risk of suicide has been described in severe
congestive acne, psoriasis and metastatic melanoma (6). Patients with chronic disease or
potentially fatal or severe pain may be suicidal, and patients with
depression, alcohol dependence, substance abuse, schizophrenia or
personality disorder are particularly at risk (7,8). With
regard to suicidal psycho-dermatological diseases, increased
attention should be paid to the early recognition of a possible
suicide risk (Fig. 1).
2. Suicide in dermatology
Suicide refers to the action of deliberately
terminating one's own life; suicidal behavior can be classified as
suicidal ideation, suicidal plan, and attempted suicide.
Nonsuicidal self-harm refers to deliberate destruction of bodily
tissue without suicidal intent, making it difficult to distinguish
between non-suicidal self-injury and attempted suicide.
Dieris-Hirche et al (9) conducted a study in Germany, showing
that 16% of patients with atopic dermatitis had suicidal ideation,
compared to the control group, of only 1%.
In another study, Dalgard et al (10) observed a significantly higher
prevalence of clinical depression in dermatological disorders,
10.1% vs. control 4.3%, anxiety disorder 17.2% vs. control 11.1%,
and suicidal ideation 12.7% vs. control of 8.3%.
Although many dermatological conditions do not
endanger life, psychiatric disorders that may increase the risk of
suicide should be considered due to the appearance of
dermatological conditions that have a strong impact on the
individual's life.
In patients with dermatological conditions, the
factors associated with suicidal predisposition are psychiatric
disorders, such as body dismorphous disorder, posttraumatic stress
disorder and major depressive disorder. Suicide was associated with
a psychiatric disorder in 90-95% of cases, and depression is a
powerful predictor of suicidal ideation (11).
Certain dermatological symptoms (auto cut,
auto-induced dermatosis) may be a sign of psychiatric disorders
(major depressive disorder, posttraumatic stress disorder,
personality disorder) (12).
Major stressful events and mental trauma can lead to
exacerbation of dermatological conditions, increasing the risk of
suicidal behavior (13).
Chronic severe conditions, such as psoriasis, are
associated with suicidal ideation (independent of psychiatric
comorbidity) (13). Also, pruritus
syndrome correlates with severe depression, increasing the risk of
suicidal behavior (14). Halvorsen
et al (15) followed the
suicidal idea in 4744 adolescents, 21.2% had suicidal ideation
after intense pruritus, compared with 8.4% without pruritus.
Other chronic conditions associated with
dermatological conditions, such as cancer, diabetes, cardiovascular
disease, are alarm signals because patients have cumulative factors
that predispose to suicide (16).
Insomnia (or lack of sleep due to dermatological conditions) is
another important factor to be considered in the suicidal risk
assessment.
Regarding the layout of injuries, permanent or
long-term injuries cause great problems, especially when these
occur in childhood (12). Both
facial and other lesions in the visible body or in the genital
areas greatly affect the quality of life.
Medications used in dermatology, such as
isotretinoin, tumor necrosis factor-α inhibitors, interleukin-17
(IL-17) inhibitors may have suicidal behavior as a side effect. On
the other hand, the medication of psychiatric patients can cause
dermatological conditions (multiforme erythema, severe seborrheic
dermatitis, lithium-induced exacerbation of psoriasis or acne)
(17).
Adalimumab has been associated with suicidal
ideation, attempted suicide and complete suicide (18). Of the biological therapies,
infliximab and adalimumab (tumor necrosis factor-α inhibitors) have
the highest rate of suicidal behavior (19). Ustekinumab (targeting IL-12 and
IL-23), secukinumab (anti-IL-17 agent) and ixekizumab (anti-IL-17
agent) were not associated with increased suicidal behavior.
Brodalumab (an IL-17 receptor subunit A blocker) was initially
banned because of the high rate of suicides following
administration, however, later on it was concluded that there was
lack of data regarding a clear association with suicidal behavior
(20).
Regarding isotretinoin (retinoid), studies are
contradictory. On the one hand, isotretinoin has been associated
with aggression, psychosis, depressive behavior and suicide, on the
other hand it has been associated with a significant improvement in
quality of life and depression (21,22).
Monitoring depressive symptoms and suicidal thoughts in patients
treated with isotretinoin should be observed, if they occur, the
medication should be discontinued and a specialist counselor should
be consulted (if necessary) (23).
There have been reports of depression and suicidal ideation
following the administration of retinitis etretinate and its
metabolite acitretin (24,25).
When doxycycline is administered, it may cause
suicidal behavior and corticosteroids are associated with a wide
range of neuropsychotic effects (26,27).
3. Aspects of suicidal risk assessment in
patients with dermatological diseases
As part of the suicide risk assessment of
dermatological patients, age should be considered. In adolescents
and young adults, the rate of suicide is rising, in middle-aged
people there is a decline, then the rate of suicide increases in
the elderly. The highest suicide rate worldwide is in people over
70 years of age and in the case of adolescents and young adults
suicide is the second leading cause of death after traffic
accidents (28). In the United
States, the assessment of suicidal behavior in the 12-17 age group
showed that 15-29% have suicidal ideation, 12.6-19% suicide plans,
and 7.3-10.6% attempted suicide (11).
Women have suicide attempts 3-4 times more often
than men, but men are more likely to be successful in suicidal
attempts. From another point of view, patients who are unemployed,
lonely, divorced or having a deceased child/husband can have
suicidal behavior.
Suicidal patients usually feel relieved when asked
about suicide. Any threat of suicide is a psychiatric emergency.
The risk of suicide should be considered in all patients with
injuries caused by self-harm. In the case of suicidal thoughts, it
is necessary to find out if there is a suicide plan and the
necessary means. It is also necessary to take into account the
personal or family history of suicidal behavior.
4. Dermatological conditions with increased
risk of suicidal behavior
Psoriasis is a chronic disease, disfiguring, marked
with remissions and exacerbations. Depending on the severity, the
physical appearance may be extremely marked for the patient. In
addition to the numerous comorbidities associated with psoriasis,
there is also major depressive disorder. Of all dermatological
disorders, psoriasis has the highest incidence of suicidal behavior
(28). Gupta et al (29) found the desire for death to be
present in 9.7% of patients with psoriasis studied, and 5.5% had
active suicidal ideation. Another study correlated the severity of
psoriasis with depression and the suicidal ideation was present in
2.5% of patients with moderate psoriasis and 7.2% of patients with
severe psoriasis (30). Numerous
other studies have confirmed both the presence of depression and
suicidal ideation in patients with psoriasis, and their association
with the severity of psoriasis. Along with the increase in
psoriasis severity, increased years of illness, poor treatment
completeness, but also depending on the area of the affected body,
increase the risk of suicidal behavior.
Acne affects mainly adolescents, with a higher
degree of suicidal behavior (31,32).
Acne can be associated with isolation and difficulty in
interpersonal relationships. The presence of scars, the shape and
severity of acne contribute to suicidal behavior. A survey
conducted in New Zealand on 9,567 young people reported the
presence of suicidal ideation in 22.5% and attempted suicide in
5.2%; interviewing only young people with acne, they reported 39.9%
suicidal ideation and 12.9% attempted suicide (33). In women, more than in men, the
presence of acne increases the risk of major depression, with major
depression contributing to the suicide rate (34).
Melanoma is a challenge for both the doctor and the
patient. Lu et al (35), in a
cohort study in Sweden that included 12,669 people, recorded 22
suicides and 136 suicide attempts, with a relative risk of suicidal
behavior after diagnosis of cancer of 1.6 (95% CI, 1.4-1.9).
Atopic dermatitis falls into suicide risk
dermatological diseases. In the spring, exacerbation of atopic
conditions may increase the risk of suicide (36,37).
Halvorsen et al (38)
reported the presence of suicidal ideation in 15.5% of those
studied with dermatitis vs. 9.1% of those who did not have
dermatitis. A study in Japan reported the presence of suicidal
ideation in the case of atopic dermatitis, in the mild form of
0.21%, in the moderate form of 6% and in the severe form of 19.6%,
all three forms having a higher predisposition to female sex
(39). In atopic dermatitis,
pruritus and lack of sleep are correlated with depression. In
addition to the patients with atopic dermatitis, the family also
suffers, and parents of children with atopic dermatitis (depending
on the severity of dermatitis) have thoughts of sacrificing their
child or themselves reported as 0.11% in parents of children with
mild dermatitis, 0.35% in parents of children with moderate
dermatitis, and 3.28% in parents of children with severe dermatitis
(39,40).
Urticaria has a duration of less than 24 h, but
chronic urticaria lasts more than 6 weeks. Urticaria is a traumatic
and stressful event, that can be associated with suicidal behavior.
The suicidal ideation among patients with chronic urticaria was
reported as 6.3-18.8% (41,42).
5. Conclusions
In practice, the psychological or psychiatric
impairment of patients with dermatological conditions should not be
neglected. Dermatological disorders are often associated with
psychiatric disorders, requiring a specific approach to these
patients by the dermatologist, and, if necessary, a
multidisciplinary team need to be formed, including a psychiatrist.
A complex approach is needed to estimate suicidal behavior.
Suicidal behavior may be a psychiatric emergency, in some cases
requiring immediate treatment.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed in the article are
available from the corresponding author on reasonable request.
Authors' contributions
AMAS, AT, DM, SD, LF and GLF collected, analyzed and
interpreted the patient data regarding the risk of suicide in
dermatology. AMAS, OGB, DB and CCD made substantial contributions
to the conception of the study and interpretation of data; also,
they drafted the manuscript and were major contributors in writing
the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Prince M, Patel V, Saxena S, Maj M,
Maselko J, Phillips MR and Rahman A: No health without mental
health. Lancet. 370:859–877. 2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cvetkovski RS, Zachariae R, Jensen H,
Olsen J, Johansen JD and Agner T: Quality of life and depression in
a population of occupational hand eczema patients. Contact Dermat.
54:106–111. 2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Dalgard F, Gieler U, Holm JO, Bjertness E
and Hauser S: Self-esteem and body satisfaction among late
adolescents with acne: Results from a population survey. J Am Acad
Dermatol. 59:746–751. 2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Onderdijk AJ, van der Zee HH, Esmann S,
Lophaven S, Dufour DN, Jemec GB and Boer J: Depression in patients
with hidradenitis suppurativa. J Eur Acad Dermatol Venereol.
27:473–478. 2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Harth W, Hillert A, Hermes B, Seikowski K,
Niemeier V and Freudenmann RW: Suizidalität in der Dermatologie.
Hautarzt. 59:289–296. 2008.(In German).
|
|
6
|
Singh S, Taylor C, Kornmehl H and
Armstrong AW: Psoriasis and suicidality: A systematic review and
meta-analysis. J Am Acad Dermatol. 77:425–440.e2. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Dieris-Hirche J, Gieler U, Petrak F, Milch
W, Te Wildt B, Dieris B and Herpertz S: Suicidal ideation in adult
patients with atopic dermatitis: A German cross-sectional study.
Acta Derm Venereol. 97:1189–1195. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tilea I, Petra D, Voidazan S, Ardeleanu E
and Varga A: Treatment adherence among adult hypertensive patients:
A cross-sectional retrospective study in primary care in Romania.
Patient Prefer Adherence. 12:625–635. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Dieris-Hirche J, Gieler U, Kupfer JP and
Milch WE: Suicidal ideation, anxiety and depression in adult
patients with atopic dermatitis. Hautarzt. 60:641–646. 2009.(In
German). PubMed/NCBI View Article : Google Scholar
|
|
10
|
Dalgard FJ, Gieler U, Tomas-Aragones L,
Lien L, Poot F, Jemec GB, Misery L, Szabo C, Linder D, Sampogna F,
et al: The psychological burden of skin diseases: A cross-sectional
multicenter study among dermatological out-patients in 13 European
countries. J Invest Dermatol. 135:984–991. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Nock MK, Deming CA, Chiu WT, Hwang I,
Angermeyer M, Borges G, Beautrais A, Viana MA, Karam EG, Kawakami
N, et al: Mental disorders, comorbidity, and suicidal
behavior. In: Suicide, Global Perspective from the WHO World Mental
Health Surveys. Nock MK, Borges G and Ono Y (eds). Cambridge
University Press, New York, NY, pp148-163, 2012.
|
|
12
|
Cotterill JA and Cunliffe WJ: Suicide in
dermatological patients. Br J Dermatol. 137:246–250.
1997.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Scott KM, Chiu WT and Hwang I: Chronic
physical conditions and the onset of suicidal behavior. In:
Suicide, Global Perspectives from the WHO World Mental Health
Surveys. Nock MK, Borges G and Ono Y (eds). Cambridge University
Press, New York, NY, pp164-178, 2012.
|
|
14
|
Gupta MA, Gupta AK, Schork NJ and Ellis
CN: Depression modulates pruritus perception: A study of pruritus
in psoriasis, atopic dermatitis, and chronic idiopathic urticaria.
Psychosom Med. 56:36–40. 1994.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Halvorsen JA, Dalgard F, Thoresen M,
Bjertness E and Lien L: Itch and pain in adolescents are associated
with suicidal ideation: A population-based cross-sectional study.
Acta Derm Venereol. 92:543–546. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Nicola P, Ardeleanu E, Gadau C, Dorobantu
M, Darabont R, Tilea I, Varga A, Folescu R, Zamfir AS, Boanca M, et
al: Evaluation of biochemical and clinical parametres of
hypertension with type 2 Diabetes Mellitus. Rev Chim. 69:2402–2406.
2018.
|
|
17
|
Bliss SA and Warnock JK: Psychiatric
medications: Adverse cutaneous drug reactions. Clin Dermatol.
31:101–109. 2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ellard R, Ahmed A, Shah R and Bewley A:
Suicide and depression in a patient with psoriasis receiving
adalimumab: The role of the dermatologist. Clin Exp Dermatol.
39:624–627. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Eshuis EJ, Magnin KM, Stokkers PC,
Bemelman WA and Bartelsman J: Suicide attempt in ulcerative colitis
patient after 4 months of infliximab therapy - a case report. J
Crohn's Colitis. 4:591–593. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Chiricozzi A, Romanelli M, Saraceno R and
Torres T: No meaningful association between suicidal behavior and
the use of IL-17A-neutralizing or IL-17RA-blocking agents. Expert
Opin Drug Saf. 15:1653–1659. 2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gorton HC, Webb RT, Kapur N and Ashcroft
DM: Non-psychotropic medication and risk of suicide or attempted
suicide: A systematic review. BMJ Open. 6(e009074)2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Schrom K, Nagy T and Mostow E: Depression
screening using health questionnaires in patients receiving oral
isotretinoin for acne vulgaris. J Am Acad Dermatol. 75:237–239.
2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Rademaker M: Adverse effects of
isotretinoin: A retrospective review of 1743 patients started on
isotretinoin. Australas J Dermatol. 51:248–253. 2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Henderson CA and Highet AS: Depression
induced by etretinate. BMJ. 298(964)1989.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Arican O, Sasmaz S and Ozbulut O:
Increased suicidal tendency in a case of psoriasis vulgaris under
acitretin treatment. J Eur Acad Dermatol Venereol. 20:464–465.
2006.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Atigari OV, Hogan C and Healy D:
Doxycycline and suicidality. BMJ Case Rep. 2013(pii:
bcr2013200723)2013.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Judd LL, Schettler PJ, Brown ES, Wolkowitz
OM, Sternberg EM, Bender BG, Bulloch K, Cidlowski JA, de Kloet ER,
Fardet L, et al: Adverse consequences of glucocorticoid medication:
Psychological, cognitive, and behavioral effects. Am J Psychiatry.
171:1045–1051. 2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Naghavi M: Global Burden of Disease
Self-Harm Collaborators: Global, regional, and national burden of
suicide mortality 1990 to 2016: systematic analysis for the Global
Burden of Disease Study 2016. BMJ. 364(l94)2019.PubMed/NCBI View
Article : Google Scholar
|
|
29
|
Gupta MA, Schork NJ, Gupta AK, Kirkby S
and Ellis CN: Suicidal ideation in psoriasis. Int J Dermatol.
32:188–190. 1993.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Gupta MA and Gupta AK: Depression and
suicidal ideation in dermatology patients with acne, alopecia
areata, atopic dermatitis and psoriasis. Br J Dermatol.
139:846–850. 1998.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Nock MK, Borges G and Bromet EJ: The
epidemiology of suicide and suicidal behavior. In: Suicide, Global
Perspectives from the WHO World Mental Health Surveys. Nock MK,
Borges G and Ono Y (eds). Cambridge University Press, New York, NY,
pp5-32, 2012.
|
|
32
|
Grigore O, Mihailescu AI, Solomon I, Boda
D and Caruntu C: Role of stress in modulation of skin neurogenic
inflammation. Exp Ther Med. 17:997–1003. 2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Purvis D, Robinson E, Merry S and Watson
P: Acne, anxiety, depression and suicide in teenagers: A
cross-sectional survey of New Zealand secondary school students. J
Paediatr Child Health. 42:793–796. 2006.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Yang YC, Tu HP, Hong CH, Chang WC, Fu HC,
Ho JC, Chang WP, Chuang HY and Lee CH: Female gender and acne
disease are jointly and independently associated with the risk of
major depression and suicide: A national population-based study.
BioMed Res Int. 2014(504279)2014.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Lu D, Fall K, Sparén P, Ye W, Adami HO,
Valdimarsdóttir U and Fang F: Suicide and suicide attempt after a
cancer diagnosis among young individuals. Ann Oncol. 24:3112–3117.
2013.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Timonen M, Viilo K, Hakko H, Särkioja T,
Meyer-Rochow VB, Väisänen E and Räsänen P: Is seasonality of
suicides stronger in victims with hospital-treated atopic
disorders? Psychiatry Res. 126:167–175. 2004.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Solomon I, Ilie MA, Draghici C, Voiculescu
VM, Căruntu C, Boda D and Zurac S: The impact of lifestyle factors
on evolution of atopic dermatitis: An alternative approach. Exp
Ther Med. 17:1078–1084. 2019.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Halvorsen JA, Lien L, Dalgard F, Bjertness
E and Stern RS: Suicidal ideation, mental health problems, and
social function in adolescents with eczema: A population-based
study. J Invest Dermatol. 134:1847–1854. 2014.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Kimata H: Prevalence of suicidal ideation
in patients with atopic dermatitis. Suicide Life Threat Behav.
36:120–124. 2006.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Ilie MA, Caruntu C, Tampa M, Georgescu SR,
Matei C, Negrei C, Ion RM, Constantin C, Neagu M and Boda D:
Capsaicin: Physicochemical properties, cutaneous reactions and
potential applications in painful and inflammatory conditions. Exp
Ther Med. 18:916–925. 2019.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Zachariae R, Zachariae C, Ibsen HH,
Mortensen JT and Wulf HC: Psychological symptoms and quality of
life of dermatology outpatients and hospitalized dermatology
patients. Acta Derm Venereol. 84:205–212. 2004.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Picardi A, Mazzotti E and Pasquini P:
Prevalence and correlates of suicidal ideation among patients with
skin disease. J Am Acad Dermatol. 54:420–426. 2006.PubMed/NCBI View Article : Google Scholar
|