Introduction
Osteoporosis is a common orthopedic disease
clinically, which is closely related to the age and sex of patients
(1). According to the investigation
and study by Wong and McGirt (2), it
was found that the incidence rate of osteoporosis is on the
increase annually. Osteoporosis treatment constitutes an increasing
financial burden. Osteoporosis is a disease caused by a variety of
reasons. The pathological characteristics of patients' bone tissue
are bone mass reduction and bone tissue degeneration (3). Femoral neck fracture is the most common
part of osteoporotic fracture clinically. Due to the decrease of
bone mineral density and the degeneration of bone tissue, patients
are prone to fracture under mild impact (4). At present, the elderly population in
China is continuously increasing, and statistics show that the
number of elderly >65 years of age in China has reached 138
million (5). The increasing number
of the elderly leads to an increase in the number of patients with
osteoporosis, which not only brings great pain to the patients
after fracture, but also increases the economic burden (6). Therefore, a good treatment plan is the
key to improve the patients' condition.
Since the clinical onset characteristics of
osteoporosis are not obvious and are relatively hidden, most
patients are diagnosed with osteoporosis only after fracture
(7). The study found that patients
who do not receive timely treatment will affect the prognosis and
even endanger the lives of patients (8). At present, the clinical treatment plan
for osteoporotic femoral neck fracture patients is mainly total hip
replacement, which relieves pain by changing the joint structure of
the patients, thus achieving the effect of improving the prognosis
and quality of life of the patients (9). However, recent findings have shown that
some patients suffer from bone loss and osteolysis due to
osteoporosis after surgery, which has an impact on the stability of
the prosthesis after replacement, shortens the service life of the
prosthesis, and leads to the failure of clinical treatment to meet
expectations (10). Alendronate
sodium, as a bone metabolism regulator, can inhibit bone absorption
and improve bone mineral density, and it is widely used in clinical
practice (11). There are few
reports on the combined use of alendronate sodium and hip
replacement in the treatment of osteoporotic femoral neck fracture.
During metabolism, osteoblasts secrete bone alkaline phosphatase
(BALP), which regulates the hydrolysis of phosphate and
pyrophosphate and promotes bone formation and bone mineralization
(12); human type I collagen
C-terminal peptide (CTX-1) can specifically reflect the
decomposition of type I collagen in bone tissue (13). Previous studies have shown that CTX-1
and BALP are involved in the process of osteoporosis (14).
Therefore, this study explores the improvement of
hip replacement combined with alendronate sodium on the condition
of patients and the risk factors affecting the efficacy of
patients, providing references for clinicians' treatment.
Materials and methods
Clinical data of patients
From July 2015 to October 2017, in Affiliated Xuzhou
Hospital of Jiangsu University (Jiangsu, China), 140 patients who
underwent hip replacement due to femoral neck fracture were
collected, of which 61 patients were treated with hip replacement
as the control group and 79 patients were treated with hip
replacement combined with alendronate sodium as the observation
group. This study was approved by the Medical Ethics Committee of
Affiliated Xuzhou Hospital of Jiangsu University. Inclusion
criteria were as follows: Garden index can be used for evaluation
with a grade ≥III, Singh index can be used for evaluation with a
Singh index between IV and VI. Patients were diagnosed as femoral
neck bone fracture through imaging examination. The clinical data
were complete and signed written informed consents were obtained
from the patients and/or guardians. Patients were admitted to
hospital for treatment within 24 h after injury with indications
for hip replacement surgery. Exclusion criteria were as follows:
Patients combined with tumor, cognitive dysfunction of patients
could not be evaluated. In addition, patients with congenital
heart, liver and kidney defects, patients with surgical
contraindications, patients who were allergic to this drug
therapy.
Main reagents and drugs
CTX–I, BALP, ELISA kit (China Shanghai Enzyme-Linked
Organisms, ml028171, ml058531), alendronate sodium tablets
(Yangzijiang Pharmaceutical Group Shanghai Heini Pharmaceutical
Co., Ltd.; SFDA approval no. H20065637), calcitriol pills [Roche
Pharma (Switzerland) Ltd.], SFDA approval no. J20150011), Caltrate
D tablet (Wyeth Pharmaceutical Co., Ltd.; SFDA approval no.
H10950029).
Treatment plan
Patients from both groups received total hip
replacement surgery (12). After the
surgery, patients from both groups were treated with conventional
drugs as follows: Caltrate D tablets were chewed after meals, 1
day/time, 1 tablet/time; calcitriol pills were taken orally on an
empty stomach 30 min before eating in the morning, 1 day/time, 2
tablets/time. On this basis, patients in the control group took
alendronate sodium tablets 1 day/time, 10 mg/time, 30 min before
eating in the morning. Patients took the medicine continuously for
3 months.
Detection of CTX–I and BALP
expressions
Peripheral venous blood (5 ml) of patients before
and 3 months after treatment was collected, kept still for 30 min,
and centrifuged at 2,680 × g for 10 min, at 4°C. Serum was
collected, and the expression of CTX–I and BALP was detected by
ELISA kit. The detection methods were as follows: Bank wells,
standard wells and sample wells to be detected were respectively
arranged. Standard substance (50 µl) was accurately added to the
enzyme-labeled coating plate, 40 µl of sample diluent was added to
the sample well to be tested, and then 10 µl of sample to be tested
was added. The sample was added to the bottom of the well of the
enzyme-labeled plate without touching the wall of the well, and it
was gently agitated and mixed. After sealing the plate with sealing
plate membrane, it was incubated at 37°C for 30 min. The sealing
film was removed, the liquid was discarded, and then it was
spin-dried. Each well was filled with washing liquid, left to stand
for 30 sec, and then discarded. The process was repeated five
times, and then it was patted dry. Enzyme-labeled reagent (50 µl)
was added to each well, except for blank wells. After sealing the
plate with sealing plate membrane, it was incubated at 37°C for 30
min. The sealing film was removed, the liquid was discarded and
spin-dried. Each well was filled with washing liquid, left to stand
for 30 sec, and then discarded. Again the process was repeated five
times, and then it was patted dry. Firstly, 50 µl of developer A
was added to each well. Then, 50 µl of developer B was added to
each well. They were mixed with gentle shaking and developed color
at 37°C in the dark for 15 min. Then, 50 µl of stop solution was
added to each well to stop the reaction. The absorbance (OD value)
of each well was measured in sequence at zero and 450 nm wavelength
of blank wells. The determination was carried out within 15 min
after the termination liquid was added.
Observation indicators
Main observation indicators were as follows: Harris
score was used to compare the clinical efficacy of patients after
treatment. Harris score (15) had a
total score of 100 points. The higher the score was, the more
significant the improvement of hip joint function was. The score of
100–90 was considered as excellent, 89–80 was considered as good,
79–70 was considered as general and <70 was considered as poor.
Excellent rate = (excellent+good)/total number × 100%.
Secondary observation indicators were as follows:
The expression changes of CTX–I and BALP before and after treatment
in the two groups were compared, and the correlation between CTX–I,
BALP and Harris score was analyzed. According to the clinical
efficacy of the patients, they were divided into the significant
effect group and poor effect group, and the risk factors affecting
the efficacy of the patients were analyzed, and the receiver
operating curve (ROC) of risk factors for efficacy diagnosis was
drawn.
Statistical methods
SPSS 20.0 software was used to analyze the collected
data in this study, GraphPad Prism 7 software was used to draw
relevant images, K-S was used to analyze the data distribution, and
the measurement data were expressed by usage rate (%). Chi-square
test was used, expressed as χ2. Non-parametric test was
used for grade data, expressed as Z. Means ± SD was used for
measurement data, and t-test was used for data conforming to normal
distribution. Paired t-test was used for intra-group comparison
before and after treatment, independent sample t-test was used for
inter-group comparison, expressed by t. Rank sum test was used for
data that did not conform to the positive distribution, expressed
by z. Multi-factor logsitic regression was used for analysis of
risk factors affecting the efficacy of patients. ROC curve was used
for analysis of clinical value of significant risk factors.
Spearman's correlation test was used for analysis of correlation
between CTX–I, BALP and Harris score after treatment. And when
P<0.05, there were statistical differences.
Results
Clinical data of patients
The comparison of clinical data of patients from the
two groups showed that there was no statistical difference in
factors including sex, age, admission time, BMI, previous medical
history, smoking history, history of alcoholism, and place of
residence of patients in the control group (P>0.05) (Table I).
 | Table I.Clinical data of patients [n%]. |
Table I.
Clinical data of patients [n%].
| Factor | Observation group
(n=79) | Control group
(n=61) | χ2/t
value | P-value |
|---|
| Sex |
|
| 0.464 | 0.496 |
| Male | 33 (41.77) | 29 (47.54) |
|
|
|
Female | 46 (58.23) | 32 (52.46) |
|
|
| Age (years) | 64.8±4.90 | 65.8±6.25 | 1.221 | 0.224 |
| Admission time
(h) | 4.51±1.35 | 4.77±1.69 | 1.012 | 0.313 |
| BMI
(kg/m2) | 21.74±1.77 | 21.97±1.61 | 0.793 | 0.429 |
| Previous medical
history |
|
Hypertension | 40 (50.63) | 27 (44.26) | 0.560 | 0.454 |
|
Diabetes | 25 (31.65) | 16 (26.23) | 0.488 | 0.485 |
| Smoking history |
|
| 0.329 | 0.566 |
| Yes | 35 (44.30) | 30 (49.18) |
|
|
| No | 44 (55.70) | 31 (50.82) |
|
|
| History of
alcoholism |
|
| 0.271 | 0.603 |
| Yes | 10 (12.66) | 6 (9.84) |
|
|
| No | 69 (87.34) | 55 (90.16) |
|
|
| Place of
residence |
|
| 0.800 | 0.371 |
| City | 50 (63.29) | 43 (70.49) |
|
|
|
Countryside | 29 (36.71) | 18 (29.51) |
|
|
Clinical efficacy of patients
Comparing the clinical efficacy of patients from the
two groups after treatment, it was found that the control group had
15 excellent cases, 18 good cases, 18 general cases, and 10 poor
cases. The observation group had 25 excellent cases, 35 good cases,
10 general cases, and 9 poor cases. In terms of the single clinical
efficacy, there was no difference in the other efficacy grades
except for good (P>0.05). The rank sum test analysis showed that
there were significant differences in the clinical efficacy of the
two groups (P<0.05). Comparing the excellent and good rates of
patients from the two groups, it was found that the excellent and
good rates of the observation group were significantly higher than
those of the control group (P<0.05), as shown in Table II.
 | Table II.Clinical efficacy of patients
[n(%)]. |
Table II.
Clinical efficacy of patients
[n(%)].
| Group | Excellent | Good | General | Poor | Excellent rate | Z value | P-value |
|---|
| Control group
(n=61) | 15 (24.59) | 18 (29.51) | 18 (29.51) | 10 (16.39) | 33 (54.10) |
|
|
|
|
|
|
|
|
| −2.015 | 0.044 |
| Observation group
(n=79) | 25 (31.65) | 35 (44.30) | 10 (12.66) | 9 (11.39) | 60 (75.95) |
|
|
| χ2
value | 0.840 | 3.203 | 6.108 | 0.734 | 7.370 |
|
|
| P-value | 0.360 | 0.074 | 0.014 | 0.392 | 0.007 |
|
|
Changes of CTX–I and BALP of patients
before and after treatment
Comparing expressions of CTX–I and BALP in serum of
patients from the two groups before and after treatment, it was
found that there was no difference in expressions of CTX–I and BALP
between the two groups before treatment (P>0.05). After
treatment, the expression of BALP in serum of patients from the
observation group was obviously higher than that from the control
group, and the expression of CTX–I was lower than that of the
control group. Differences in expressions of CTX–I and BALP in the
observation group were obviously greater than those in the control
group (P<0.05). More details are shown in Tables III and IV and Fig.
1.
 | Table III.Changes of CTX–I of patients before
and after treatment. |
Table III.
Changes of CTX–I of patients before
and after treatment.
|
| CTX–I (µg/ml) |
|
|
|
|---|
|
|
|
|
|
|
|---|
| Group | Before
treatment | After
treatment | t value | P-value | Variation
difference |
|---|
| Control group
(n=61) | 0.53±0.21 | 0.35±0.12 |
5.902 | <0.001 | 0.18±0.14 |
| Observation group
(n=79) | 0.54±0.22 | 0.24±0.08 | 12.192 | <0.001 | 0.30±0.20 |
| t value | 0.288 |
6.339 |
|
|
3.990 |
| P-value | 0.774 | <0.001 |
|
| <0.001 |
 | Table IV.Changes of BALP of patients before
and after treatment. |
Table IV.
Changes of BALP of patients before
and after treatment.
|
| BALP (U/l) |
|
|
|
|---|
|
|
|
|
|
|
|---|
| Group | Before
treatment | After
treatment | t value | P-value | Variation
difference |
|---|
| Control group
(n=61) | 36.04±1.87 | 50.57±1.68 | −46.728 | <0.001 | −14.53±2.43 |
| Observation group
(n=79) | 36.27±1.71 | 60.70±1.90 | −83.230 | <0.001 | −24.43±2.61 |
| t value | 0.751 | 32.928 |
|
| 22.928 |
| P-value | 0.454 | <0.001 |
|
| <0.001 |
Relationship of expressions of CTX–I
and BALP with clinical efficacy of patients after treatment
The Spearman correlation test was used to analyze
the relationship between the CTX–I and BALP expressions in serum of
patients from the two groups after treatment and the clinical
efficacy of the patients. It was found that the CTX–I expression
was negatively correlated with the clinical efficacy of the
patients after treatment, that is, the expression gradually
decreased with the improvement of the clinical efficacy; while the
BALP expression was positively correlated with the clinical
efficacy of patients after treatment, that is, the expression
gradually increased with the good clinical efficacy (rCTX–I=−0.801,
PCTX–I<0.001; rBALP=0.563, PBALP<0.001) (data not shown).
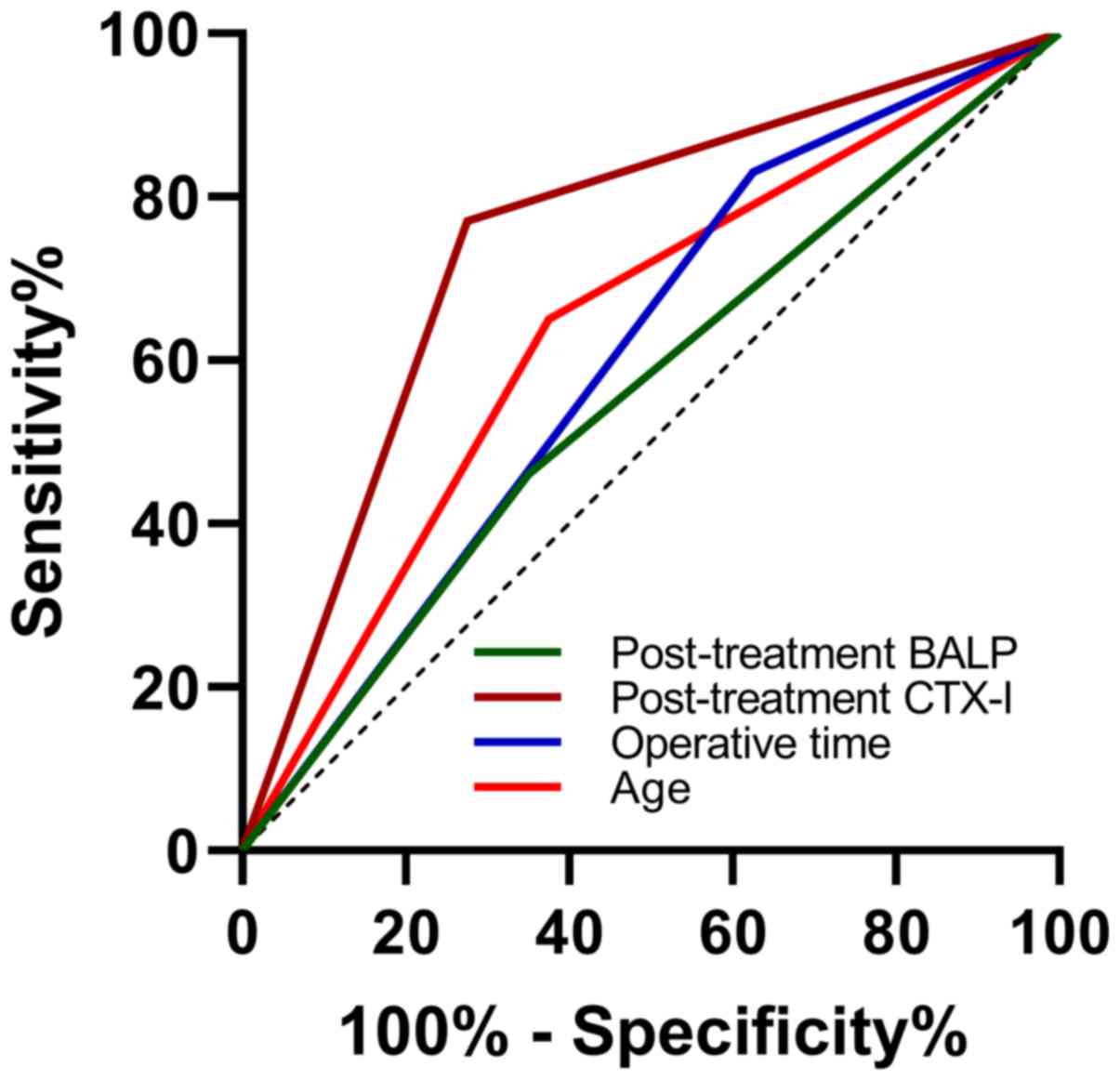
Analysis of risk factors affecting
efficacy
According to the clinical efficacy of patients after
treatment, patients with excellent efficacy were divided into
groups with significant efficacy, patients with good efficacy,
general efficacy and poor efficacy were divided into groups with
poor efficacy. Single factor analysis of the collected clinical
data of patients showed that there were differences between the two
groups (P<0.05) in age, time of operation, CTX–I after treatment
and BALP after treatment that were risk factors affecting the
prognosis of patients, while the other indexes had no differences
(P>0.05), and the indexes with differences were assigned.
Furthermore, multi-factor logstic regression was used and LR method
was selected for analysis. It was found that age, time of
operation, CTX–I after treatment and BALP after treatment were
independent risk factors affecting the efficacy of patients. ROC
curve analysis showed that age, time of operation, CTX–I after
treatment, and area under BALP curve after treatment were 0.638,
0.603, 0.748, 0.555, among which there was no difference between
time of operation and area under BALP curve after treatment and 0.5
(P>0.05), while there were significant differences between age
and CTX–I after treatment and 0.5 (P<0.05) (detailed in Tables V–VIII).
 | Table V.Single factor analysis of clinical
data. |
Table V.
Single factor analysis of clinical
data.
| Factor | Significantly
effective group (n=40) | Less effective
group (n=100) | χ2/t
value | P-value |
|---|
| Sex |
|
| 2.605 |
0.107 |
| Male | 22
(55.00) | 40
(40.00) |
|
|
| Female | 18
(45.00) | 60
(60.00) |
|
|
| Age (years) |
|
| 8.823 |
0.003 |
| ≥65 | 15
(37.50) | 65
(65.00) |
|
|
| <65 | 25
(62.50) | 35
(35.00) |
|
|
| Admission time
(h) |
4.15±1.44 |
4.65±1.71 | 1.631 |
0.105 |
| BMI
(kg/m2) |
21.54±1.57 |
21.80±1.88 | 0.773 |
0.441 |
| Previous medical
history |
|
Hypertension | 20
(50.00) | 47
(47.00) | 0.320 |
0.572 |
|
Diabetes | 8
(20.00) | 33
(33.00) | 2.332 |
0.127 |
| Smoking
history |
|
| 1.795 | 0.180 |
|
Yes | 15
(37.50) | 50
(50.00) |
|
|
| No | 25
(62.50) | 50
(50.00) |
|
|
| History of
alcoholism |
|
| 0.706 |
0.401 |
|
Yes | 6
(15.00) | 10
(10.00) |
|
|
| No | 34
(85.00) | 90
(90.00) |
|
|
| Place of
residence |
|
| 0.388 |
0.534 |
|
City | 25
(62.50) | 68
(68.00) |
|
|
|
Countryside | 15
(37.50) | 32
(32.00) |
|
|
| Time of operation
(min) |
40.13±7.10 |
54.36±9.92 | 8.258 | <0.001 |
| Intraoperative
hemorrhage (ml) | 301.54±66.88 | 310.55±101.70 | 0.517 |
0.606 |
| CTX–I (µg/ml) after
treatment |
0.20±0.11 |
0.33±0.11 | 6.317 | <0.001 |
| BALP (U/l) after
treatment |
58.57±5.16 |
55.38±5.18 | 3.301 |
0.001 |
 | Table VIII.ROC parameters of each index of risk
factors. |
Table VIII.
ROC parameters of each index of risk
factors.
| Parameter | Age | Time of
operation | CTX–I after
treatment | BALP after
treatment |
|---|
| AUC | 0.638 | 0.603 | 0.748 | 0.555 |
| 95% CI | 0.535–0.740 | 0.494–0.711 | 0.654–0.841 | 0.450–0.660 |
| Standard
deviation | 0.053 | 0.055 | 0.048 | 0.053 |
| P-value | 0.011 | 0.059 | <0.001 | 0.310 |
| Specificity | 62.50% | 37.50% | 72.50% | 65.00% |
| Sensitivity | 65.00% | 83.00% | 77.00% | 46.00% |
| Youden index | 27.50% | 21.00% | 49.50% | 11.00% |
| Cut-off | ≥65 years old | <45 min | ≥0.20 µg/ml | <55.00 U/l |
Discussion
With the continuous development of society, people's
living standards and quality of life have been continuously
improved, and most developed countries are prone to population
aging (16). Some surveys and
statistics show that 12% of the world's population are >60 years
old, and the metabolism and immune function of people gradually
decline with age (17,18). Hip fracture is a kind of femoral neck
fracture which is more common clinically, in which the incidence
rate of the elderly is significantly higher than that of the young,
and the elderly are prone to fracture when falling and twisting due
to physical mobility inconvenience (19,20). At
present, there are reduction and internal fixation and total hip
replacement for the treatment of femoral neck fracture clinically.
Compared with reduction and internal fixation, total hip
replacement, although the time of operation is long and the trauma
is relatively large, can carry out weight-bearing training and
corresponding recovery exercise in early postoperative patients,
which can rapidly improve the quality of life of patients (21). However, recent findings have shown
that patients are prone to bone loss and osteolysis after total hip
replacement, which leads to prosthesis loosening and affects the
postoperative quality of life of patients to some extent (19). For this reason, some scholars said
that patients after total hip replacement can combine drug
intervention to improve this phenomenon.
Caltrate D tablets and calcitriol pills are commonly
used clinically as basic anti-osteoporosis drugs (22). In this study, we added alendronate
sodium tablets on the basis of patients' basic drugs. Alendronate
sodium tablets are the third generation of anti-osteoporosis
diphosphate drugs widely used clinically, are potent osteoclast
inhibitors, have high affinity with bone surface, and have little
effect on bone mineralization (23).
Previous studies have shown that alendronate tablets can improve
bone morphology and clinical vertebral body fractures, and can also
reduce the recurrence rate of fractures (24). Through combined treatment, we found
that the clinical efficacy of patients in the observation group was
significantly improved compared with that in the control group, and
the excellent and good rate of patients in the observation group
was significantly higher than that in the control group, which
suggested that the addition of alendronate sodium tablets on the
basis of conventional treatment could further improve the clinical
efficacy of patients. At present, the clinical evaluation indexes
of the efficacy after hip replacement are mainly judged according
to Harris and Charnley scores (25).
Although the accuracy of these scores has been verified clinically,
subjective bias still exists to some extent, while the serological
index results are relatively objective. In this study, we also
detected CTX–I and BALP in serum of patients. CTX–I and BALP are
markers of reactive bone metabolism, in which BALP changes through
the secretion of bone cells, which can reflect the maturation and
activity of osteoblasts, and the expression will obviously increase
when bone diseases occur, while the differential expression of
CTX–I can reflect bone loss (26).
We found that the CTX–I and BALP expressions of patients in the
control group and the observation group had obvious changes after
treatment. The CTX–I expression of patients in the observation
group was significantly lower than that of patients in the control
group, while the BALP expression was opposite to that of patients
in the observation group. This shows that the combined alendronate
sodium tablets can promote the maturation of osteoblasts of
patients and inhibit the generation of osteoclasts, thus achieving
the effect of accelerating the postoperative recovery of patients.
In the study of Zhang et al (27), it was found that the high level of
CTX–I was one of the risk factors for hip fracture in patients.
However, this study significantly reduced the expression of CTX–I
in patients after treatment, possibly by inhibiting the formation
of osteoclasts. Furthermore, we further analyzed the correlation
between CTX–I and BALP and the clinical efficacy of patients, and
found that the expression of CTX–I was negatively correlated with
the clinical efficacy after treatment, while the expression of BALP
was positively correlated with the clinical efficacy, which
suggested that we could become an evaluation index of the efficacy
of patients by observing expressions of CTX–I and BALP after
treatment.
At the end of the study, we analyzed the factors
that affect the efficacy of patients. We found that age, time of
operation, CTX–I after treatment and BALP after treatment were
independent risk factors that affect the efficacy of patients.
Furthermore, we found that age and CTX–I after treatment had
certain predictive value for the clinical efficacy of patients
through ROC curve analysis. Due to the improvement of quality of
life and the gradual increase of the elderly population, the study
found that China has entered an aging society initially, and the
elderly have reduced their tolerance to surgery due to the
reduction of their metabolism, thus affecting the clinical efficacy
of patients (28). CTX–I, as a
marker of osteoclast formation, its increased expression indicates
the increase of osteoclasts. The increase of osteoclasts is easy to
cause bone loss and osteolysis in patients, which is not conducive
to the improvement of patients' condition (29). Therefore, patients should choose
treatment according to their own conditions before surgery, pay
close attention to the expression of CTX–I in patients after
surgery, and take drugs in time, so as to accelerate the recovery
of patients after surgery.
However, there are still some limitations in this
study. Firstly, in this study, we only carried out the death of
patients after 3 months of clinical efficacy, and did not carry out
long-term follow-up and detection. Secondly, in this study, we only
detected the expressions of CTX–I and BALP, and did not detect
other bone metabolism indicators. Whether there are better
prognostic observation indicators is unclear. Therefore, we will
increase our follow-up time and detection index in future
researches to supplement our research results.
In conclusion, hip replacement combined with
alendronate sodium can effectively improve the clinical efficacy of
patients, and age, time of operation, CTX–I after treatment and
BALP after treatment are found to be independent risk factors
affecting the postoperative efficacy of patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XO and YZD wrote the manuscript and were also
involved in the conception of the study. LY and FX interpreted and
analyzed the patient data. XY, PS and SMT designed the study and
performed the experiment. QC and YQX were responsible for the
analysis and discussion of the data. XO wrote the manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the Affiliated Xuzhou Hospital of Jiangsu University (Jiangsu,
China). Patients who participated in this research had complete
clinical data. Signed written informed consents were obtained from
the patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Koevska V, Nikolikj-Dimitrova E, Mitrevska
B, Gjeracaroska-Savevska C, Gocevska M and Kalcovska B: Effect of
exercises on quality of life in patients with postmenopausal
osteoporosis - randomized trial. Open Access Maced J Med Sci.
7:1160–1165. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wong CC and McGirt MJ: Vertebral
compression fractures: A review of current management and
multimodal therapy. J Multidiscip Healthc. 6:205–214.
2013.PubMed/NCBI
|
|
3
|
Morabito N, Catalano A, Gaudio A, Morini
E, Bruno LM, Basile G, Tsiantouli E, Bellone F, Agostino RM,
Piraino B, et al: Effects of strontium ranelate on bone mass and
bone turnover in women with thalassemia major-related osteoporosis.
J Bone Miner Metab. 34:540–546. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Florschutz AV, Langford JR, Haidukewych GJ
and Koval KJ: Femoral neck fractures: Current management. J Orthop
Trauma. 29:121–129. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rizzoli R: Postmenopausal osteoporosis:
Assessment and management. Best Pract Res Clin Endocrinol Metab.
32:739–757. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Swart E, Roulette P, Leas D, Bozic KJ and
Karunakar M: ORIF or arthroplasty for displaced femoral neck
fractures in patients younger than 65 years old: An economic
decision analysis. J Bone Joint Surg Am. 99:65–75. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhao YR, Wei X, Jiang JJ, Zhang YL, Wang
SQ and Xie YM: Systemic review of Jintiange capsules in treatment
of postmenopausal osteoporosis. Zhongguo Zhong Yao Za Zhi.
44:186–192. 2019.(In Chinese). PubMed/NCBI
|
|
8
|
Nijmeijer WS, Folbert EC, Vermeer M,
Slaets JP and Hegeman JH: Prediction of early mortality following
hip fracture surgery in frail elderly: The Almelo Hip Fracture
Score (AHFS). Injury. 47:2138–2143. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Le Manach Y, Collins G, Bhandari M,
Bessissow A, Boddaert J, Khiami F, Chaudhry H, De Beer J, Riou B,
Landais P, et al: Outcomes after hip fracture surgery compared with
elective total hip replacement. JAMA. 314:1159–1166. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Salemyr M, Muren O, Ahl T, Bodén H, Eisler
T, Stark A and Sköldenberg O: Lower periprosthetic bone loss and
good fixation of an ultra-short stem compared to a conventional
stem in uncemented total hip arthroplasty. Acta Orthop. 86:659–666.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yuan F, Peng W, Yang C and Zheng J:
Teriparatide versus bisphosphonates for treatment of postmenopausal
osteoporosis: A meta-analysis. Int J Surg. 66:1–11. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Siller AF and Whyte MP: Alkaline
phosphatase: Discovery and naming of our favorite enzyme. J Bone
Miner Res. 33:362–364. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yang C, Ren J, Li B, Jin C, Ma C, Cheng C,
Sun Y and Shi X: Identification of gene biomarkers in patients with
postmenopausal osteoporosis. Mol Med Rep. 19:1065–1073.
2019.PubMed/NCBI
|
|
14
|
Zhang C, Wang Y, Zhang CL and Wu HR:
Prioritization of candidate metabolites for postmenopausal
osteoporosis using multi-omics composite network. Exp Ther Med.
17:3155–3161. 2019.PubMed/NCBI
|
|
15
|
Kalairajah Y, Azurza K, Hulme C, Molloy S
and Drabu KJ: Health outcome measures in the evaluation of total
hip arthroplasties - a comparison between the Harris hip score and
the Oxford hip score. J Arthroplasty. 20:1037–1041. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fehlings MG, Tetreault L, Nater A, Choma
T, Harrop J, Mroz T, Santaguida C and Smith JS: The aging of the
global population: The changing epidemiology of disease and spinal
disorders. Neurosurgery. 77 (Suppl 4):S1–S5. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gorsky M and Sirrs C: World health by
place: The politics of international health system metrics, 1924-c.
2010. J Glob Hist. 12:361–385. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Giefing-Kröll C, Berger P, Lepperdinger G
and Grubeck-Loebenstein B: How sex and age affect immune responses,
susceptibility to infections, and response to vaccination. Aging
Cell. 14:309–321. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Peeters CM, Visser E, Van de Ree CL,
Gosens T, Den Oudsten BL and De Vries J: Quality of life after hip
fracture in the elderly: A systematic literature review. Injury.
47:1369–1382. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bliuc D, Nguyen ND, Alarkawi D, Nguyen TV,
Eisman JA and Center JR: Accelerated bone loss and increased
post-fracture mortality in elderly women and men. Osteoporos Int.
26:1331–1339. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mahmoud SS, Pearse EO, Smith TO and Hing
CB: Outcomes of total hip arthroplasty, as a salvage procedure,
following failed internal fixation of intracapsular fractures of
the femoral neck: A systematic review and meta-analysis. Bone Joint
J. 98-B:452–460. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhang BL, Wang F, Tian MB, Yin WL, You XY,
Li D, Ma LG and Xing LQ: Articular capsule repair in initial
artificial hip replacement via anterolateral approach to the hip
joint. J Biol Regul Homeost Agents. 30:441–447. 2016.PubMed/NCBI
|
|
23
|
Lhamo Y, Chugh PK and Tripathi CD: Vitamin
D supplements in the Indian market. Indian J Pharm Sci. 78:41–47.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang Y, Chen X, Tang Y, Lu Y, Guo L,
Zhong D and Zhang YF: Bioequivalence of generic alendronate sodium
tablets (70 mg) to Fosamax® tablets (70 mg) in fasting,
healthy volunteers: A randomized, open-label, three-way,
reference-replicated crossover study. Drug Des Devel Ther.
11:2109–2119. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Black DM, Cummings SR, Karpf DB, Cauley
JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, et al:
Randomised trial of effect of alendronate on risk of fracture in
women with existing vertebral fractures. Lancet. 348:1535–1541.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hozack WJ, Rothman RH, Booth RE Jr,
Balderston RA, Cohn JC and Pickens GT: Survivorship analysis of
1,041 Charnley total hip arthroplasties. J Arthroplasty. 5:41–47.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhang YP, Ao S, Liu Y, Wang Y, Jia YM,
Zhang H and Leng H: Identification of hub genes associated with
postmenopausal osteoporosis by Gibbs sampling method. Exp Ther Med.
17:2675–2681. 2019.PubMed/NCBI
|
|
28
|
Dai Z, Wang R, Ang LW, Yuan JM and Koh WP:
Bone turnover biomarkers and risk of osteoporotic hip fracture in
an Asian population. Bone. 83:171–177. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lizaur-Utrilla A, Serna-Berna R,
Lopez-Prats FA and Gil-Guillen V: Early rehospitalization after hip
fracture in elderly patients: Risk factors and prognosis. Arch
Orthop Trauma Surg. 135:1663–1667. 2015. View Article : Google Scholar : PubMed/NCBI
|