Introduction
Caused by Treponema pallidum (TP), syphilis
is a chronic and infectious disease that may invade multiple organs
(1). At present, the prevention and
cure of syphilis remain a great challenge. In spite of certain
breakthroughs regarding the laboratory cultivation of TP, detection
of its DNA and specific proteins remains difficult in clinical
practice (2). Whether syphilis is
curable or not depends on the rapid plasma reagin (RPR) antibody
test. Serological cure is defined as either a negative RPR or
≥4-fold decrease (2-fold dilution) in titer at 6 months following
therapy (3). Serofast is defined as
either no change in RPR titer or an up to 2-fold decrease (1-fold
dilution) or increase in titer following initial therapy or
retreatment (4,5). Retreatment for syphilis is recommended
by the syphilis treatment guidelines of the USA, UK and China when
additional follow-up cannot be ensured (6–8).
However, the number of retreatments and the treatments'
effectiveness remain controversial. A relatively small number of
studies have been performed to examine the frequency of
retreatments in early syphilis and serofast patients. Seña et
al (5) and Wang et al
(9) re-treated early syphilis
participants who were serofast at 6 months and analyzed the
serological response after retreatment and an additional 6 months
of follow-up. These two studies demonstrated a moderately
incremental benefit of retreatment in serofast early syphilis
patients. It remains unclear whether serofast patients require
further retreatment after the first retreatment.
Over the last 20 years, the incidence of syphilis
has been rapidly increasing in China (10). Syphilis has become one of the three
major infectious diseases in China, which raises the concern of
clinicians. Serofast is frequently observed in patients with early
syphilis (primary, secondary or latent) after treatment (11). This status makes it difficult for
clinicians to judge the curative effects of treatment. Due to the
associated anxiety of affected patients, penicillin is frequently
overused by clinicians in certain hospitals (7). Serofast patients with syphilis receive
penicillin treatments every 3–6 months over 2–3 years. In this
scenario, the treatment of syphilis and the prognosis of patients
require further investigation. In the present study, data of
patients with early syphilis and serofast status after the first
and second retreatment were analyzed in order to contribute to the
determination of the optimal therapeutic schedule.
Materials and methods
Subjects
The present retrospective study considered 1,036
consecutive patients with early syphilis (primary, secondary or
early latent) treated as outpatients at Tianjin Third Central
Hospital (Tianjin, China) between January 2009 and June 2016. A
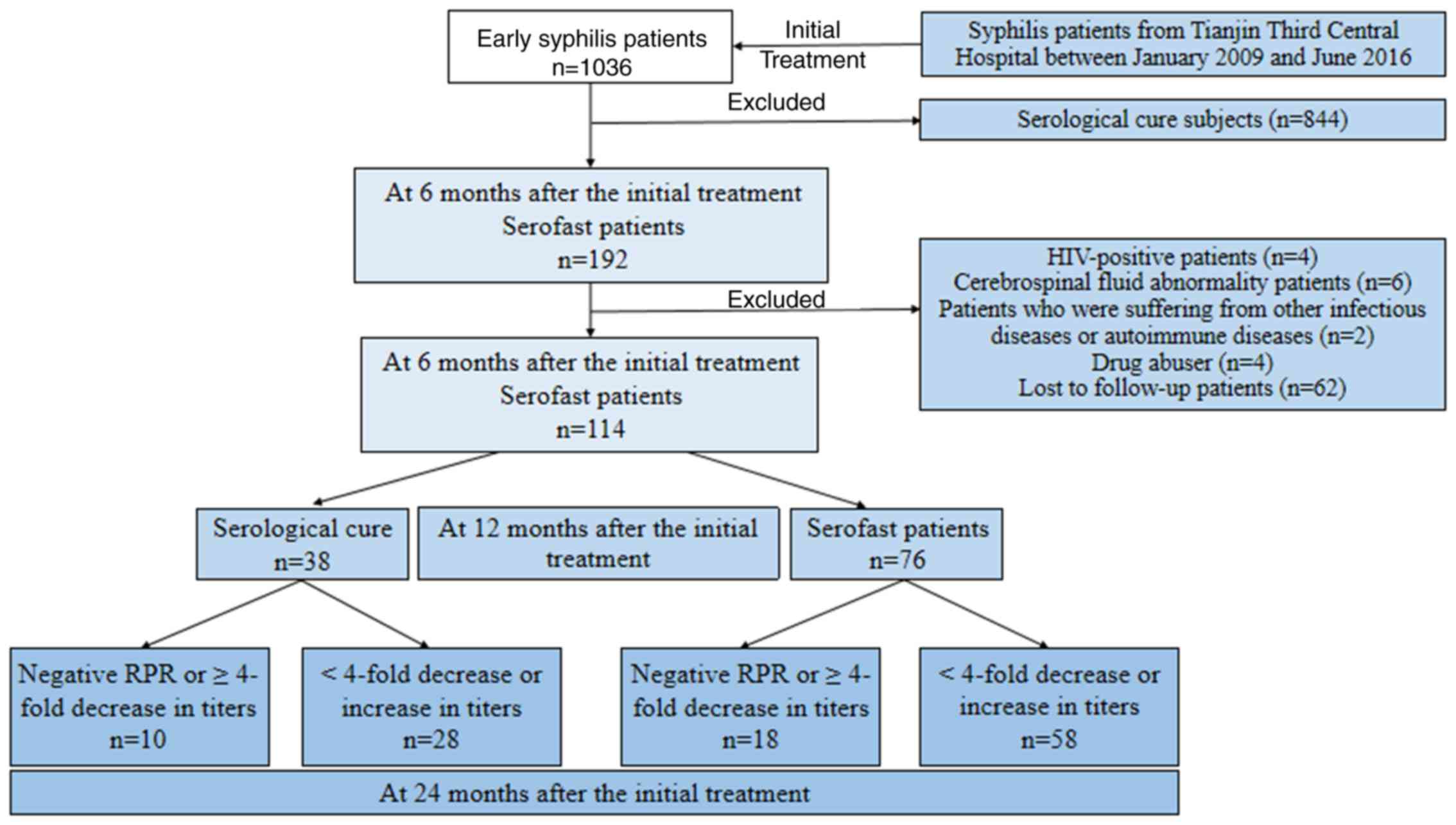
flow chart of the study design is presented in Fig. 1. A total of 114 eligible serofast
patients were included in the present study. All clinical data,
including medical history, process of treatment and results of
laboratory tests recorded by clinicians of the outpatient
department were analyzed. According to the diagnostic criteria of
the China Centers for Disease Control and Prevention (8), early syphilis consists of primary
syphilis, secondary syphilis and early latent syphilis. Primary
syphilis is characterized by more than one chancre and inguinal
lymphadenopathy, as well as laboratory confirmation of TP in
clinical specimens by RPR and particle agglutination assay for
antibody to TP (TPPA), or TP haemagglutination. Secondary syphilis
is characterized by skin rash and lymphadenopathy, and confirmed by
laboratory testing results for syphilis (12). Early latent syphilis is defined as
patients within a year of asymptomatic syphilitic infection
supported by positive laboratory testing results and normal
cerebrospinal fluid (CSF).
All patients with early syphilis have positive
results of serologic examinations (RPR and TPPA). The RPR antibody
test was used to evaluate the curative effect of treatment in the
present study. Serological cure was defined as either a negative
RPR or a ≥4-fold decrease (2-fold dilution) in titer at 6 months
following therapy (3). Serofast is
defined as either no change in RPR titer or a 2-fold decrease
(1-fold dilution) or increase in titer following initial therapy or
retreatment.
The inclusion criterion was serofast early syphilis,
while the exclusion criteria were as follows: i) Tertiary syphilis;
ii) HIV-positive status; iii) CSF abnormality; iv) presence of
other infectious diseases or autoimmune diseases; v) drug abuse;
vi) loss to follow-up. The patients were stratified into different
groups based on retreatment: The 1st retreatment group comprised
patients with early syphilis with a <4-fold decrease (2-fold
dilution) in titer at 6 months following initial therapy; the 2nd
retreatment group included serofast patients after the 1st
retreatment; the control group for the 2nd retreatment group were
patients that had achieved serological cure by 6 months following
the initial therapy.
Treatment
According to the Chinese national guidelines for the
treatment of syphilis, patients with no penicillin allergy received
initial treatment with benzathine penicillin (administered as three
doses of 2.4 million units intramuscularly each at 1-week
intervals; 7.2 million units in total). Alternatives to this
treatment of syphilis were doxycycline 100 mg orally twice daily
for 15 days or procaine penicillin 0.8 million units
intramuscularly daily for 15 days. After the treatment, the serum
RPR titers and clinical symptoms of all patients were reviewed
every 3 months. At baseline (T0) and 6 months after the initial
treatment (T1), the RPR test was performed on patients to evaluate
the curative effect of treatment. Serofast patients were included
in the 1st retreatment group. The RPR test was used to evaluate the
curative effects of treatment at 12 months after initial treatment
(T2). Patients who remained serofast were included in the 2nd
retreatment group. At 24 months after the initial treatment (T3),
the RPR test was used again to evaluate the curative effects.
Statistical analysis
All data were analyzed using SPSS (version 24.0; IBM
Corp.). Prior to analysis, normality of distribution was evaluated
using the Kolmogorov-Smirnov test. Categorical variables were
represented as a percentage and differences between groups were
assessed using the Chi-square test. Continuous variables were
expressed as the median and interquartile range and were compared
using the Mann-Whitney U test. All hypothesis testing was two-sided
and P<0.05 was considered to indicate a statistically
significant difference.
Results
General information
As presented in Fig.
1, a total of 192 patients (18.5%) were serofast at 6 months
after the initial treatment and 114 eligible serofast patients were
included in the present study. A total of 92 serofast patients were
treated with benzathine penicillin and the remaining 22 patients
received an alternative therapy. There were no significant
differences in efficacy between the different treatments. The
median age of the patients was 36 years (range, 36–49) and the
majority were female (60.5%). Primary syphilis accounted for 8.8%
(10/114), secondary syphilis accounted for 14.0% (16/114) and early
latent syphilis accounted for 77.1% (88/114; Table I).
 | Table I.Characteristics and serological
outcomes of serofast patients with early syphilis after the first
retreatment. |
Table I.
Characteristics and serological
outcomes of serofast patients with early syphilis after the first
retreatment.
| A, Sex |
|---|
|
|---|
|
| Overall (n=114) | Serological cure
(n=38) | Serofast (n=76) | P-value |
|---|
| Female | 69 (60.5) | 20 (52.6) | 49 (64.5) | 0.34 |
|
| B, Age |
|
|
| Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
| Median age, years
(IQR) | 36 (23) | 33 (21) | 36 (24) | 0.24 |
|
| C, Syphilis
type |
|
| Syphilis
type | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
| Primary | 10 (8.8) | 5 (13.1) | 5 (6.6) | 0.04 |
| Secondary | 16 (14.0) | 9 (23.7) | 7 (9.2) |
|
| Early latent | 88 (77.2) | 24 (63.2) | 64 (84.2) |
|
|
| D,
Treatment |
|
| Treatment | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
| Benzathine
penicillin | 92 (80.7) | 32 (84.2) | 60 (78.9) | 0.87 |
| Alternatives | 22 (19.3) | 6 (15.8) | 16 (21.1) |
|
|
| E, T0 RPR
titer |
|
| T0 RPR
titer | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
| ≤1:2 | 13 (11.4) | 1 (2.6) | 12 (15.8) | <0.01 |
| 1:4 | 20 (17.5) | 5 (13.2) | 15 (19.7) |
|
| 1:8 | 26 (22.8) | 6 (15.8) | 20 (26.3) |
|
| 1:16 | 34 (29.8) | 13 (34.2) | 21 (27.6) |
|
| 1:32 | 13 (11.4) | 8 (21.1) | 5 (6.6) |
|
| 1:64 | 6
(5.3) | 4 (10.5) | 2 (2.6) |
|
|
1:128 | 2
(1.8) | 1 (2.6) | 1 (1.4) |
|
| Geometric mean titer
(95% CI) | 10 (8,12) | 16 (11,22) | 8 (6,10) | <0.01 |
|
| F, T1 RPR
titer |
|
| T0 RPR
titer | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
|
≤1:2 | 12 (10.5) | 3 (7.9) | 9 (11.8) | <0.01 |
|
1:4 | 21 (18.4) | 1 (2.6) | 20 (26.3) |
|
|
1:8 | 37 (32.5) | 13 (34.2) | 24 (31.6) |
|
|
1:16 | 20 (17.5) | 7 (18.4) | 13 (17.1) |
|
|
1:32 | 18 (15.8) | 10 (26.3) | 8 (10.5) |
|
|
1:64 | 6 (5.3) | 4 (10.6) | 2 (2.7) |
|
|
1:128 | 0 (0) | 0 (0) | 0 (0) |
|
| Geometric mean
titer (95% CI) | 9 (8,11) | 14 (11,19) | 8 (6,9) | <0.01 |
|
| G, T2 RPR
titer |
|
| T0 RPR
titer | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
|
≤1:2 | 26 (22.8) | 15 (39.5) | 11 (14.5) | <0.01 |
|
1:4 | 32 (28.1) | 12 (31.6) | 20 (26.3) |
|
|
1:8 | 32 (28.1) | 8 (21) | 24 (31.6) |
|
|
1:16 | 17 (14.9) | 3 (7.9) | 14 (18.4) |
|
|
1:32 | 5 (4.4) | 0 (0) | 5 (6.6) |
|
|
1:64 | 2 (1.7) | 0 (0) | 2 (2.6) |
|
|
1:128 | 0 (0) | 0 (0) | 0 (0) |
|
| Geometric mean
titer (95% CI) | 6 (4,7) | 3 (2,4) | 7 (6,9) | <0.01 |
Serological outcomes of serofast
patients with early syphilis after the first retreatment
As presented in Table
I, compared with serofast patients, those that achieved
serological cure exhibited no significant difference in sex, age
and initial treatments. However, there were more primary and
secondary cases of syphilis in patients that achieved serological
cure than in serofast patients (13.1 vs. 6.6%, 23.7 vs. 9.2%,
P<0.05). Patients with latent syphilis more frequently achieved
serofast than serological cure (84.2 vs. 63.2%, P<0.05). After
the first retreatment, 17.5% (20/114) of subjects exhibited a
≥4-fold decline in the RPR titers compared with the initial
treatment. However, when the serological response was determined in
comparison with the baseline titers, it was indicated that 33.3% of
patients (38/114) had achieved a serological cure. Significant
differences in RPR titer at T0 (prior to initial treatment), T1 (at
6 months) and T2 (at 12 months) were observed between serofast
patients and those with serological cure (P<0.05).
Serological outcomes in serofast
patients with early syphilis after the second retreatment
The 76/114 patients (66.7%) who remained serofast
after the first retreatment received a second retreatment (Table II). After the second retreatment, a
total of 18 (23.7%) patients had a ≥4-fold decline in RPR titer
from their T2 (at 12 months) RPR titer. The spontaneous RPR titer
change of the 38 patients serologically cured after the first
retreatment were also followed up at 24 months. Of these patients,
26.3% (10/38) exhibited a ≥4-fold decline in RPR titer or negative
status compared to the T2 (at 12 months) RPR titer. There was no
significant difference in RPR titer at T3 (at 24 months) between
the first retreatment and the second retreatment group (Table III).
 | Table II.Characteristics and serological
outcomes of serofast patients with early syphilis after the second
retreatment. |
Table II.
Characteristics and serological
outcomes of serofast patients with early syphilis after the second
retreatment.
| A, Sex |
|---|
|
|---|
|
| Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|---|
| Female | 49 (64.5) | 12 (66.7) | 37 (63.8) | 0.82 |
|
| B, Age |
|
|
| Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
| Median age, years
(IQR) | 36 (24) | 38 (20) | 35 (24) | 0.39 |
|
| C, Syphilis
type |
|
| Syphilis
type | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
|
Primary | 5 (6.6) | 1 (5.6) | 4 (6.9) | <0.01 |
|
Secondary | 7 (9.2) | 2 (11.2) | 5 (8.6) |
|
| Early
latent | 64 (84.2) | 15 (83.2) | 49 (84.5) |
|
|
| D,
Treatment |
|
|
Treatment | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
| Benzathine
penicillin | 61 (80.3) | 15 (83.3) | 46 (79.3) | 0.07 |
| Alternatives | 15 (19.7) | 3
(16.7) | 12 (20.7) |
|
|
| E, T2 RPR
titer |
|
| T2 RPR
titer | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
|
≤1:2 | 11 (14.5) | 1 (5.6) | 10 (17.2) | 0.03 |
|
1:4 | 20 (26.3) | 3 (16.2) | 17 (29.3) |
|
|
1:8 | 24 (31.6) | 5 (27.9) | 19 (32.8) |
|
|
1:16 | 14 (18.4) | 5 (27.9) | 9 (15.5) |
|
|
1:32 | 5 (6.6) | 2 (11.2) | 3 (5.2) |
|
|
1:64 | 2 (2.6) | 2 (11.2) | 0 (0) |
|
|
1:128 | 0 (0) | 0 (0) | 0 (0) |
|
| Geometric mean
titer (95% CI) | 7 (6,9) | 11 (7,17) | 6 (5,8) | 0.04 |
|
| F, T3 RPR
titer |
|
| T3 RPR
titer | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
|
≤1:2 | 18 (23.7) | 7 (38.9) | 11 (18.9) | <0.01 |
|
1:4 | 23 (30.3) | 7(38.9) | 16 (27.6) |
|
|
1:8 | 22 (29.0) | 2 (11.1) | 20 (34.5) |
|
|
1:16 | 11 (14.5) | 2 (11.1) | 9 (15.5) |
|
|
1:32 | 2 (2.5) | 0 (0) | 2 (3.5) |
|
|
1:64 | 0 (0) | 0 (0) | 0 (0) |
|
|
1:128 | 0 (0) | 0 (0) | 0 (0) |
|
| Geometric mean
titer (95% CI) | 5 (4,6) | 3 (2,5) | 6 (5,7) | <0.01 |
 | Table III.Serological outcomes in serofast
patients with early syphilis after two retreatments. |
Table III.
Serological outcomes in serofast
patients with early syphilis after two retreatments.
| Group | Negative RPR or
≥4-fold decrease in titers | <4-fold decrease
or increase in titers | Overall |
|---|
| First
retreatment | 10 (26.3) | 28 (73.7) | 38
(33.3) |
| Second
retreatment | 18 (23.7) | 58 (76.3) | 76
(66.7) |
| Overall | 28 (24.6) | 86 (75.4) | 114 (100) |
After two retreatments, a total of 56 (49.12%)
patients achieved serological cure and the remaining 58 (50.88%)
patients remained serofast (Table
IV). There was no significant difference in sex, age, syphilis
type and therapeutic regimen between the two groups (P>0.05). Of
note, a significant difference in T0 (prior to initial treatment)
RPR titer, T1 (at 6 months) RPR titer and T3 (at 24 months) RPR
titer was seen between serofast patients and serologically cured
patients (P<0.05).
 | Table IV.Characteristics and serological
outcomes of serofast patients with early syphilis after two
retreatments. |
Table IV.
Characteristics and serological
outcomes of serofast patients with early syphilis after two
retreatments.
| A, Sex |
|---|
|
|---|
|
| Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|---|
| Female | 69 (60.5) | 32 (57.1) | 37 (63.8) | 0.47 |
|
| B, Age |
|
|
| Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
| Median age, years
(IQR) | 36 (23) | 37 (22) | 35 (24) | 0.81 |
|
| C, Syphilis
type |
|
| Syphilis
type | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
|
Primary | 10 (8.8) | 6 (10.7) | 4 (6.9) | 0.15 |
|
Secondary | 16 (14) | 11 (19.6) | 5 (8.6) |
|
| Early
latent | 88 (77.2) | 39 (69.7) | 49 (84.5) |
|
|
| D,
Treatment |
|
|
Treatment | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
| Benzathine
penicillin | 92 (80.7) | 46 (82.1) | 46 (79.3) | 0.89 |
| Alternatives | 22 (19.3) | 10 (17.9) | 12 (20.7) |
|
|
| E, T0 RPR
titer |
|
| T0 RPR
titer | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
|
≤1:2 | 13 (11.4) | 1 (1.8) | 12 (20.7) | <0.01 |
|
1:4 | 20 (17.5) | 7 (12.5) | 13 (22.4) |
|
|
1:8 | 26 (22.8) | 10 (17.9) | 16 (27.6) |
|
|
1:16 | 34 (29.8) | 21 (37.5) | 13 (22.4) |
|
|
1:32 | 13 (11.4) | 9 (16.1) | 4 (6.9) |
|
|
1:64 | 6 (5.3) | 6 (10.6) | 0 (0) |
|
|
1:128 | 2 (1.8) | 2 (3.6) | 0 (0) |
|
| Geometric mean
titer (95% CI) | 10 (8,12) | 16 (13,21) | 7 (5,8) | <0.01 |
|
| F, T1 RPR
titer |
|
| T0 RPR
titer | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
|
≤1:2 | 12 (10.5) | 4 (7.2) | 8 (13.8) | <0.01 |
|
1:4 | 21 (18.4) | 2 (3.6) | 19 (32.8) |
|
|
1:8 | 37 (32.5) | 20 (35.7) | 17 (29.3) |
|
|
1:16 | 20 (17.5) | 12 (21.4) | 8 (13.8) |
|
|
1:32 | 18 (15.8) | 12 (21.4) | 6 (10.3) |
|
|
1:64 | 6 (5.3) | 6 (10.7) | 0 (0) |
|
|
1:128 | 0 (0) | 0 (0) | 0 (0) |
|
| Geometric mean
titer (95% CI) | 9 (8,11) | 14 (11,17) | 6 (5,8) | <0.01 |
|
| G, T2 RPR
titer |
|
| T2 RPR
titer | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
|
≤1:2 | 26 (22.8) | 16 (28.6) | 10 (17.2) | 0.19 |
|
1:4 | 32 (28.1) | 15 (26.8) | 17 (29.3) |
|
|
1:8 | 32 (28.1) | 13 (23.2) | 19 (32.8) |
|
|
1:16 | 17 (14.9) | 8 (14.2) | 9 (15.5) |
|
|
1:32 | 5 (4.4) | 2 (3.6) | 3 (5.2) |
|
|
1:64 | 2 (1.7) | 2 (3.6) | 0 (0) |
|
|
1:128 | 0 (0) | 0 (0) | 0 (0) |
|
| Geometric mean
titer (95% CI) | 6 (5,7) | 5 (4,7) | 6 (5,8) | 0.10 |
|
| H, T3 RPR
titer |
|
| T3 RPR
titer | Overall
(n=114) | Serological cure
(n=38) | Serofast
(n=76) | P-value |
|
|
≤1:2 | 40 (35.1) | 29 (51.4) | 11 (9.0) | <0.01 |
|
1:4 | 34 (29.9) | 18 (32.4) | 16 (27.6) |
|
|
1:8 | 26 (22.8) | 6 (10.8) | 20 (34.5) |
|
|
1:16 | 11 (9.6) | 2 (3.6) | 9 (15.5) |
|
|
1:32 | 3 (2.6) | 1 (1.8) | 2 (3.4) |
|
|
1:64 | 0 (0) | 0 (0) | 0 (0) |
|
|
1:128 | 0 (0) | 0 (0) | 0 (0) |
|
| Geometric mean
titer (95% CI) | 4 (3,5) | 3 (2,4) | 6 (5,7) | <0.01 |
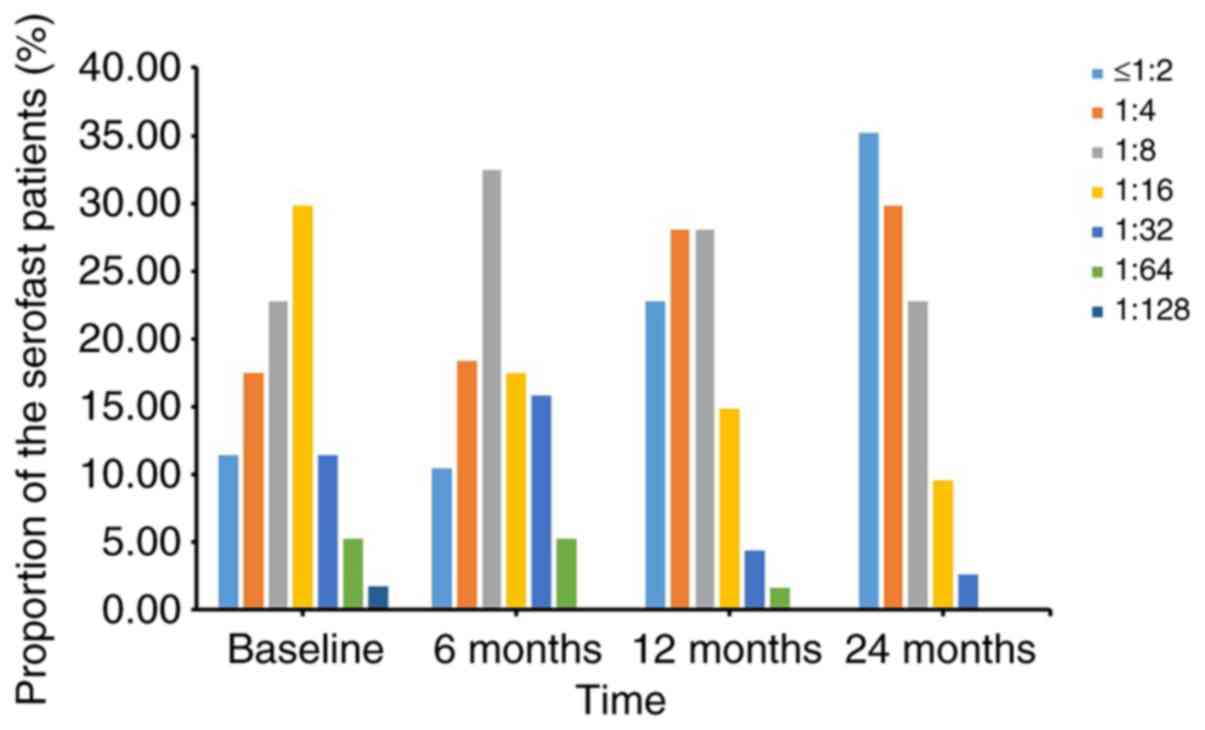
RPR titer at different time-points in
serofast patients
The RPR titers in the serofast patients changed at
varying time-points. All 114 serofast patients were divided into 7
groups according to their initial RPR titer. Fig. 2 presents the proportion of serofast
patients in different RPR titer groups at different time-points.
Serological outcomes of serofast patients with early syphilis and
different RPR titers at different time-points are also provided in
Table V.
 | Table V.Serological outcomes in serofast
patients with early syphilis with different RPR titers. |
Table V.
Serological outcomes in serofast
patients with early syphilis with different RPR titers.
|
| T2 (at 12
months) | T3 (at 24
months) |
|---|
|
|
|
|
|---|
| RPR titer | Negative | ≥4-fold
decrease | 2-fold
decrease | No change or
increase | Negative | ≥4-fold
decrease | 2-fold
decrease | No change or
increase |
|---|
| ≤1:2 | 0 | 0 | 2 | 10 | 0 | 0 | 0 | 12 |
| 1:4 | 0 | 5 | 6 | 9 | 3 | 2 | 3 | 10 |
| 1:8 | 0 | 6 | 8 | 12 | 0 | 5 | 4 | 11 |
| 1:16 | 0 | 14 | 13 | 8 | 0 | 20 | 9 | 5 |
| 1:32 | 0 | 8 | 4 | 1 | 1 | 16 | 2 | 2 |
| 1:64 | 0 | 4 | 1 | 1 | 2 | 5 | 0 | 0 |
| 1:128 | 0 | 1 | 1 | 0 | 0 | 2 | 0 | 0 |
Discussion
After the initial treatment, a total of 114 serofast
patients were included in the present retrospective study. Compared
to the baseline RPR titers, 33.3% patients had achieved serological
cure after the first retreatment with 2.4 million units of
benzathine penicillin weekly for 3 weeks, which was higher than
that in the study by Seña et al (27.50%) (5). There was only 1 dose of benzathine
additionally given to serofast patients in the study by Seña et
al (5). In the study by Wang
et al (9), the serological
cure rate was 48.6%. The baseline titers of patients in Wang's
study were at a high level, which may be the reason for a higher
probability of serological response to therapy (13). Furthermore, the above study had no
blank control group. Therefore, a natural decline in RPR titer
cannot be completely ruled out in certain patients that achieved
serological cure. The serological response of patients who remained
serofast after the first retreatment and received a second
retreatment was also evaluated. Patients that achieved serological
cure after the first retreatment that received no further
retreatment were used as a control for the group with the second
retreatment. At 24 months, 23.7% of patients (18/76) had achieved
serological cure in the second retreatment group. By contrast,
26.3% of patients (10/38) in the control group exhibited a ≥4-fold
decline in RPR titer or negative status. The second retreatment did
not significantly improve the serological cure rate in comparison
to this control. Similarly, the study by Seña et al
demonstrated minimal improvement in serological response among
serofast early syphilis patients re-treated with benzathine
penicillin, although these patients received only one retreatment
(5). In addition, the study by Wang
et al suggested that the incremental benefit of
re-retreatment in serofast patients with early syphilis was
moderate (9).
The present study demonstrated no significant
benefit to multiple retreatment of patients with early syphilis and
serofast. Not pursuing this avenue of treatment may help to avoid
expensive over-treatment of such patients and reduce the financial
burden on patients' families and the health system of governments
(14). A reduction in retreatment
may be beneficial as over-use or abuse of penicillin may lead to
drug resistance, causing future damage to patient health.
Furthermore, the present results may provide insight into the
management of patients with early syphilis with serofast status. It
is difficult for clinicians to assess the biological significance
of the serofast state (15).
Although nontreponemal tests, such as the toluidine red unheated
serum test, the rapid plasma reagin serological test and the
venereal disease research laboratory slide test, are able to
measure IgG and IgM antibodies to TP and potentially to cardiolipin
and lipoidal material released from damaged host cells during
syphilis infection, other illnesses that produce tissue damage may
also lead to positive results (16).
In clinical practice, it is a challenge to manage patients with
syphilis at the serofast stage using the recommended treatments.
Whether there is a persistence of reagin in the circulating blood,
persistent spirochetes foci or progressive lesions in patients with
syphilis following anti-syphilitic therapy remains unclear
(3). The optimal treatment protocol
still requires clarification due to insufficient availability of
data on the serological response to retreatment and long-term
outcomes. In the management of early syphilis at the serofast
stage, the variability of the host response to infection should be
taken into consideration, and possibly other confounding non-TP
inflammatory conditions in the host, including autoimmune diseases,
or other infections when stable non-TP antibody titers prevail
after treatment (17–19). It is necessary to elucidate the
biological basis of serofast and determine whether patients with
early syphilis reaching serofast should undergo continued
serological monitoring and retreatments in future studies.
To the best of our knowledge, the present study
provides the first evaluation of the serological response following
a second retreatment of serofast syphilis. However, there are
certain limitations. First, the data originated from a
retrospectively enrolled cohort, and this retrospective study
design is generally considered inferior to a prospective study
design. Second, a natural decline in RPR titer cannot be completely
ruled out in certain patients with serological cure, as there was
no control in the first retreatment for ethical reasons. Third, the
different characteristic baselines (the RPR titer and syphilis
stage) between the first retreatment group and the second
retreatment group may have been a source of bias. The impact of RPR
titers and syphilis stage on the curative effect of treatment
requires further study. Finally, while the patients with early
syphilis in the present cohort study were recruited
retrospectively, all of the eligible patients were from a single
center and a large number of patients were excluded due to
information loss, and the sample size was relatively small.
In conclusion, the present study suggested that
patients with early syphilis who reached serofast after the first
treatment did not receive any significant benefits after repeated
retreatment. In particular, a second retreatment did not
significantly improve the patients' serological cure rate. A
persistent non-TP serological response after treatment makes it
difficult for clinicians to judge the curative effect of treatment.
In clinical practice, repeated treatments are controversial.
Therefore, in addition to developing a more accurate evaluation
method for remedial effects in patients with syphilis, it may be
required to fully consider the potential benefits and risks before
authorizing repeated retreatments.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YL and SZ designed the study, performed the
investigation and data analysis and wrote the manuscript. QB, SZ
and JW were responsible for data entry. ZW and JL carried out the
RPR test. All of the authors read and approved the manuscript.
Ethics approval and consent to
participate
This study was approved by the Institutional Ethics
Committee of Tianjin Third Central Hospital (Tianjin, China). Data
were extracted from the medical records of the patients in a manner
in which subjects could not be identified; hence, the requirement
for informed consent was waived.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cai SN, Long J, Chen C, Wan G and Lun WH:
Incidence of asymptomatic neurosyphilis in serofast Chinese
syphilis patients. Sci Rep. 7:154562017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Edmondson DG, Hu B and Norris SJ:
Long-term in vitro culture of the syphilis spirochete Treponema
pallidum subsp. pallidum. MBio. 9:e01153–18. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ren RX, Wang LN, Zheng HY and Li J: No
improvement in serological response among serofast latent patients
retreated with benzathine penicillin. Int J STD AIDS. 27:58–62.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kingston M, French P, Higgins S, McQuillan
O, Sukthankar A, Stott C, McBrien B, Tipple C, Turner A, Sullivan
AK, et al: UK national guidelines on the management of syphilis
2015. Int J STD AIDS. 27:421–446. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Seña AC, Wolff M, Behets F, Van Damme K,
Martin DH, Leone P, McNeil L and Hook EW: Response to therapy
following retreatment of serofast early syphilis patients with
benzathine penicillin. Clin Infect Dis. 56:420–422. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Workowski KA and Bolan GA: Sexually
transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep.
64:1–137. 2015.PubMed/NCBI
|
|
7
|
Tuddenham S and Ghanem KG: Emerging trends
and persistent challenges in the management of adult syphilis. BMC
Infect Dis. 15:3512015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
SBTS/MOH, . National Standard of the
People's Republic of China: Diagnostic Criteria and Management of
Syphilis (GB 15974-1995)Standards Press of China; Beijing: 1996
|
|
9
|
Wang ZS, Liu XK and Li J: Serological
response to therapy following retreatment of serofast early
syphilis patients with benzathine penicillin. J Antimicrob
Chemother. 73:1348–1351. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang S, Wu J, Ding C, Cui Y, Zhou Y, Li Y,
Deng M, Wang C, Xu K, Ren J, et al: Epidemiological features of and
changes in incidence of infectious diseases in China in the first
decade after the SARS outbreak: An observational trend study.
Lancet Infect Dis. 17:716–725. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang RL, Wang QQ, Zhang JP and Yang LJ:
Molecular subtyping of Treponema pallidum and associated
factors of serofast status in early syphilis patients: Identified
novel genotype and cytokine marker. PLoS One. 12:e01754772017.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Liang X, Liu T, Yuan C, Wang W and Liang
P: The disappearance of femoral head and neck resulting from
extensive bone defect caused by secondary syphilis: A case report
and literature review. BMC Musculoskelet Disord. 19:2512018.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li J, Wang LN and Zheng HY: Predictors of
serological cure and serofast state after treatment in HIV-negative
patients with early syphilis in China. Sex Transm Infect.
89:692013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen ZQ, Zhang GC, Gong XD, Lin C, Gao X,
Liang GJ, Yue XL, Chen XS and Cohen MS: Syphilis in China: Results
of a national surveillance programme. Lancet. 369:132–138. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sena AC, Zhang XH, Li T, Zheng HP, Yang B,
Yang LG, Salazar JC, Cohen MS, Moody MA, Radolf JD and Tucker JD: A
systematic review of syphilis serological treatment outcomes in
HIV-infected and HIV-uninfected persons: Rethinking the
significance of serological non-responsiveness and the serofast
state after therapy. BMC Infect Dis. 15:4792015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Macfarlane DE, Hare K and Elias-Jones TF:
Evaluation of automated large-scale screening tests for syphilis. J
Clin Pathol. 29:317–321. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Larsen SA, Steiner BM and Rudolph AH:
Laboratory diagnosis and interpretation of tests for syphilis. Clin
Microbiol Rev. 8:1–21. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schultz DR: Antiphospholipid antibodies:
Basic immunology and assays. Semin Arthritis Rheum. 26:724–739.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Augenbraun M, French A, Glesby M,
Sanchez-Keeland L, Young M, Greenblatt R and Sharma A: Hepatitis C
virus infection and biological false-positive syphilis tests. Sex
Transm Infect. 86:97–98. 2010. View Article : Google Scholar : PubMed/NCBI
|