Introduction
As the most common disease of the digestive system,
cholelithiasis and the formation of gallbladder polyps have a high
incidence (1). Open cholecystectomy
and laparoscopic cholecystectomy are classic methods for the
treatment of cholelithiasis and gallbladder polyps and have been
widely used in clinical practice. After cholecystectomy, however,
certain patients are prone to dyspepsia, reflux esophagitis,
gastritis and post-cholecystectomy syndrome, which has raised
concern among clinicians (1).
Furthermore, studies have indicated that after cholecystectomy, the
incidence of colon cancer, pancreatic cancer, esophageal squamous
carcinoma and hepatocellular carcinoma was increased (2–5).
However, with increasing knowledge on gallbladder physiology, the
significance of the gallbladder is being increasingly recognized.
The gallbladder is not only an important component of the human
digestive system but also an immune organ: The gallbladder is able
to secrete mucus and IgA antibodies and participate in the
construction of the biliary immune defense system (6,7).
Therefore, certain clinicians recommend that patients undergo
cholecystolithotomy with preservation of the gallbladder, which is
able to treat cholelithiasis whilst preserving the function of the
gallbladder (8). Furthermore,
certain patients refuse to undergo open or laparoscopic
cholecystectomy due to this causing surgical scars on the abdominal
wall. It is thought that these scars have negative effects on their
physical or mental wellbeing (9).
With the rapid development of endoscopic technology,
cholecystolithotomy with preservation of the gallbladder and no
surgical scars is possible.
Case report
A 45-year-old male patient presented at the
Affiliated Hospital of Nanjing Medical University of Traditional
Chinese Medicine (Nanjing, China) in May, 2018 and requested the
removal of his cholecystic polyps and cholecystolithiasis which had
been diagnosed earlier in the outpatient department of the hospital
with preservation of the gallbladder. Over the past 2 years, the
patient had experienced frequent abdominal pain and fever.
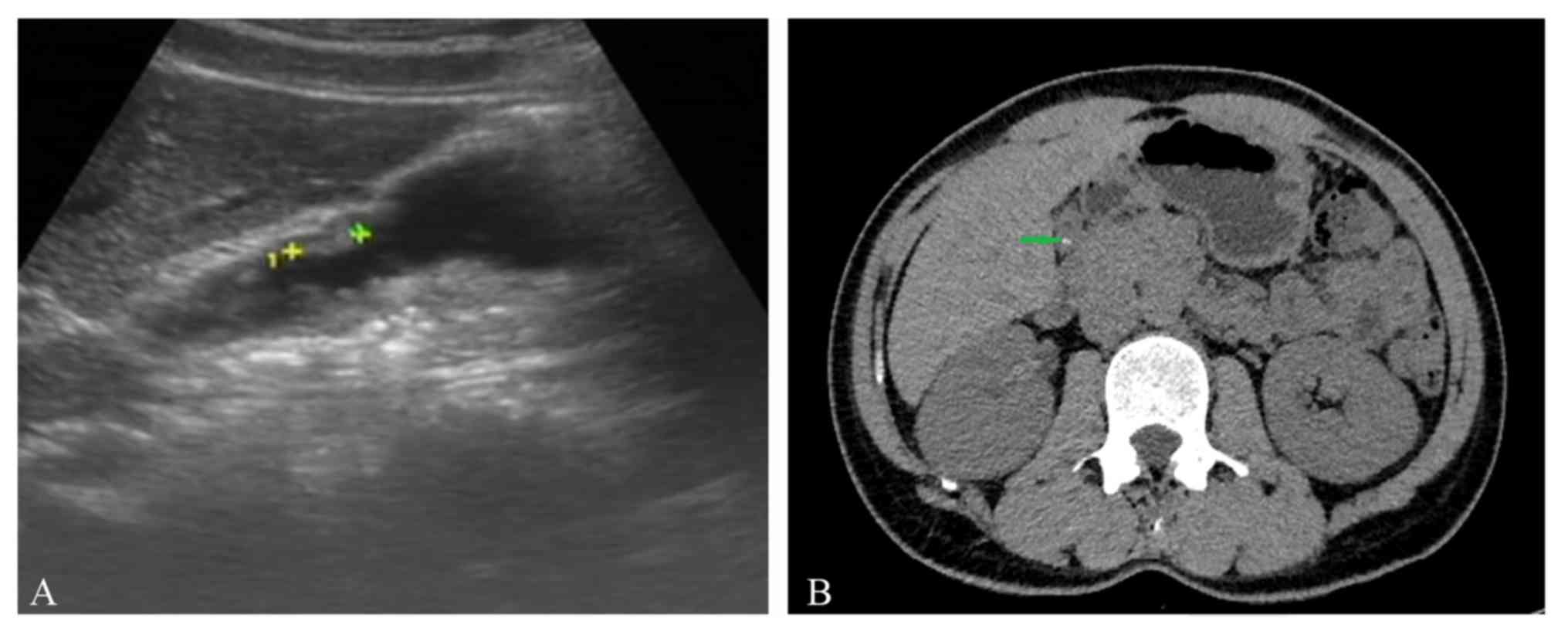
Cholecystic polyps and gallstones were observed by pre-operative
abdominal ultrasonography (Fig. 1A)
and abdominal CT (Fig. 1B). It was
estimated that the maximum diameter of cholecystic polyps was 1.2
cm and that of the biggest stone was 0.8 cm. The pre-operative
gallbladder ejection function was deemed good according to
gallbladder contraction function test under abdominal ultrasound.
Following consultation of relevant literature and discussion with
certain endoscopy experts, it was decided that transgastric
endoscopic gallbladder polypectomy and cholecystolithiasis was
feasible in this patient (10–12). The
present study reports on the successful use of flexible
transgastric endoscopy in gallbladder polypectomy and treating
cholecystolithiasis, which appears to be a promising novel surgical
option for patients wishing to retain their gallbladder and
functions without scarring on the abdominal wall. Prior to the
operation, written informed consent was obtained from the patient
and the operation was approved by written the Ethics Committee of
Affiliated Hospital of Nanjing University of Chinese Medicine
(Nanjing, China).
A second-generation cephalosporin was
prophylactically administered to prevent infection at 30 min prior
to surgery. With the assistance of a transparent cap, an endoscopic
full-thickness incision was made on the posterior antrum of the
stomach near the small curved side by using a hook knife (Olympus
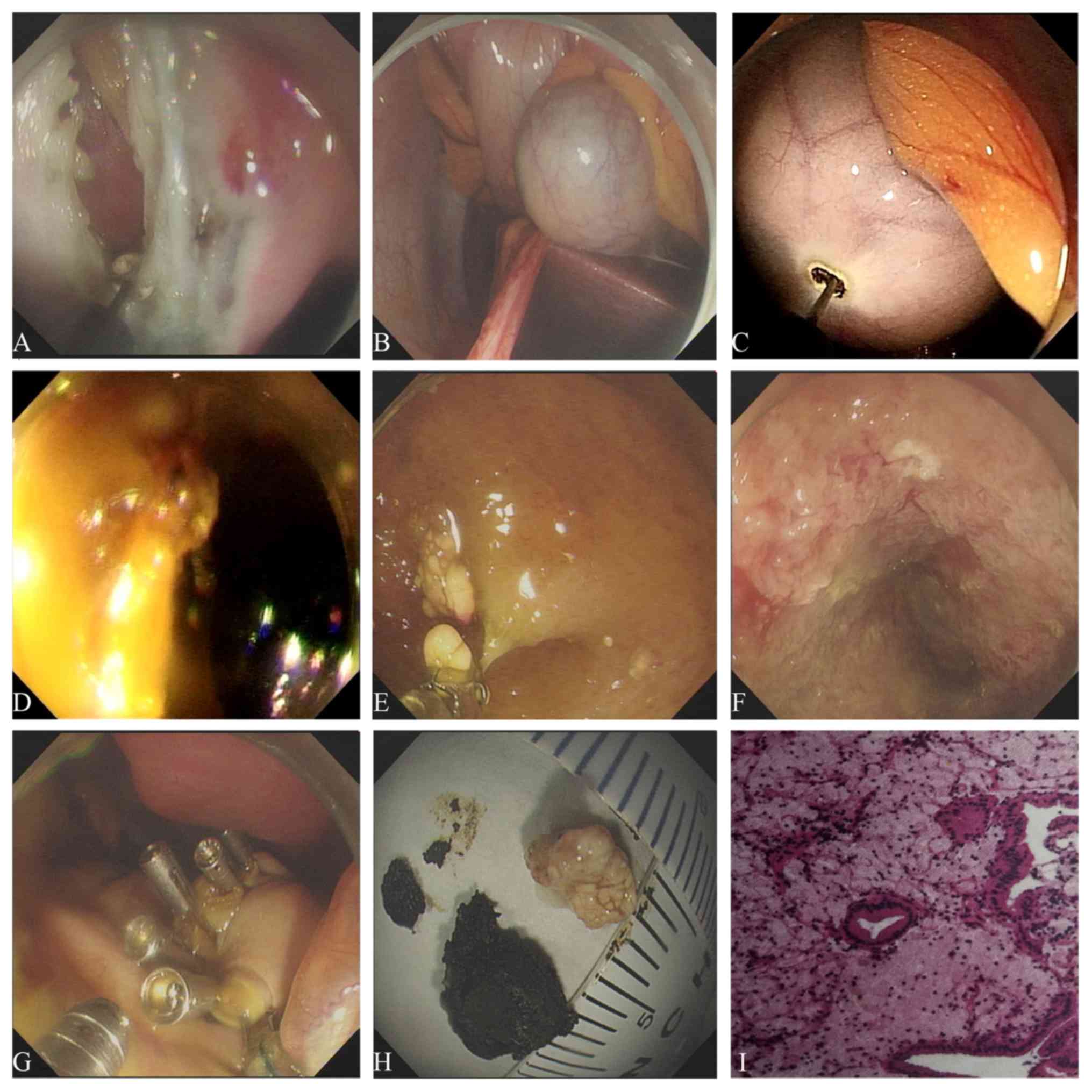
Corp.) and an IT2 knife (Olympus Corp.). After
full-thickness dissection, the omentum present in the abdominal
cavity was separated layer by layer (Fig. 2A). The gallbladder exhibited mild
edema (Fig. 2B). A small incision
was opened at the junction of the gallbladder by using the hook
knife. With the same tool, the window was extended to allow the
endoscope to enter the gallbladder (Fig.
2C). An endoclip with endoloop was used to pull the gallbladder
so that the endoscope was able to enter the gallbladder easily.
During this procedure, the bile overflowing from the gallbladder
into the abdominal cavity was cleaned up. After rinsing the inner
wall of the gallbladder with aseptic saline repeatedly, three
gallstones were removed (Fig. 2D).
The cholecystic polyps were resected from the gallbladder by snare
traction and assistance of hot biopsy forceps (Fig. 2E and F). After local hemostasis, the
endoscope was retracted from the gallbladder and four endoclips
(Micro-Tech) were used to clip the gallbladder incision. The
endoscope was withdrawn from the stomach and the incision was
closed with endoclips (Micro-Tech) (Fig.
2G). The operation time was 120 min and no bleeding was
observed during surgery. Two sediment-like stones and two larger
polyps were successfully removed. The maximum diameter of the
extracted gallstones was 1.5 cm and that of the cholecystic polyps
was 0.5 cm (Fig. 2H).
The pathologic diagnosis of the cholecystic polyps
was cholesterol polyp (Fig. 2I). The
patient recovered without any incident and discharged by the
hospital in 2 days. During the three-month follow-up after the
endoscopy operation, the patient had no specific discomfort and no
gallstones and polyps were observed by transabdominal
ultrasound.
Discussion
With the rapid development of endoscopic technology,
novel approaches for treating cholecystic polyps and gallstones are
becoming available. Natural Orifice Transluminal Endoscopic Surgery
(NOTES) is an improvement in surgical interventions and has been
widely used in the clinic. In 2007, Marescaux et al
(13) reported on the use of
transvaginal endoscopic cholecystectomy for the first time. In
2015, Liu et al (14)
performed the first NOTES cholecystolithotomy with gallbladder
preservation by flexible endoscopy through a rectal approach.
However, due to the presence of intestinal bacteria, it may easily
cause contamination through incisions and abdominal infection. In
2018, Schwaitzberg et al (15) reported on transgastric endoscopy
cholecystectomy performed in 4 cases. To the best of our knowledge,
endoscopic cholecystic polypectomy and cholecystolithiasis in
clinical patients has not been previously described. The present
study reports on the successful use of endoscopy gallbladder
polypectomy and cholecystolithiasis with a transgastric approach by
flexible endoscopy, which appears to be a promising novel surgical
option for patients wishing to retain their gallbladder and its
functions with no scar on the abdominal wall.
In the case of the present study, the patient had
suffered from recurrent low fever and abdominal pain for a long
time. Gallstones and cholecystic polyps were identified in the
pre-operative examination. These are two indications for surgical
treatment. Furthermore, the patient did not wish to have any
surgical scars on his abdominal wall. Hence, transgastric
endoscopic gallbladder polypectomy and cholecystolithiasis was
performed. This type of surgery was a huge challenge for
endoscopists. Firstly, the snare or forceps polypectomy should
completely remove the pathological tissue and avoid gallbladder
perforation. This technique was translated from the removal of
colon polyps using endoscopy. Submucosal injection in the
gallbladder wall and electrocoagulation technology may avoid
gallbladder perforation and reduce bleeding (16). Furthermore, the gallbladder and
stomach wounds generated by this operation must be treated with
caution. In the approach reported in the present study, intensive
endoclips and a full set of endoloop successfully solved this
problem. In terms of post-operative recovery, these strategies
achieved desirable outcomes. Initially, the prevention of abdominal
scarring rendered it more feasible for patients to undergo surgery.
This type of operation preserved gallbladder function, reduced
postoperative complications such as dyspepsia caused by removal of
the gallbladder and enhanced postoperative recovery. However, prior
to its eventual application in clinical routine, two questions
regarding the method require to be addressed, including the
possibility of intra-abdominal infection caused by the endoclips
which is left in the abdominal cavity following surgery, whereas
the other is anastomotic fistula due to poor closure. At our
institution, continuous efforts will be made to further develop and
eventually include this procedure in clinical routine as soon as
possible.
In conclusion, the present study provided the novel
technique of transgastric endoscopy gallbladder polypectomy and
cholecystolithiasis, an innovative method that should be of
interest for interventional endoscopists and may expand the current
endoscopic repertoire. With its constant improvement, this method
may increasingly become an option for certain patients.
Acknowledgements
The authors would like to thank Professor Hailin
Jin, Professor Jun Xiao, Professor Qide Zhang, Professor Yuhong
Zhou, Dr Dapeng Wu, Miss Lu Ze, Miss Wenxia Gu and Miss Jie Su from
The Gastroenterology Endoscopy Center, Affiliated Hospital of
Nanjing University of Chinese Medicine, Jiangsu Province Hospital
of Chinese Medicine (Jiangsu, China). Professor Hailin Jin was the
second assistant of this operation. Professor Jun Xiao, Professor
Qide Zhang and Professor Yuhong Zhou participated in the
formulation of the surgical plan. Dr Dapeng Wu and Miss Jie Su were
responsible for the perioperative treatment of this patient. Miss
Lu Ze and Miss Wenxia Gu were the surgical nurses of this
operation.
Funding
The present study was supported by the second batch
of scientific research special projects for the construction of the
National TCM Clinical Research Base in 2015 (grant no.
JDZX2015086), an innovation fund of the Jiangsu Province Hospital
of Chinese Medicine (grant no. Y2018CX57) and the Jiangsu Province
‘333 Project’ Training Fund (grant no. BRA2017551).
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
YL was the first assistant during the operation and
wrote the manuscript. SH was the endoscopy surgeon of this
operation and approved the final version of the manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Approval was obtained from the Medical Ethics
Committee of Affiliated Hospital of Nanjing University of Chinese
Medicine (No. 2018NL-094-0; Jiangsu Province Hospital of Chinese
Medicine; Nanjing, China).
Patient consent for publication
The patient provided written informed consent for
the publication of data and images.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
EUS
|
endoscopic ultrasound
|
|
NOTES
|
Natural Orifice Transluminal
Endoscopic Surgery
|
References
|
1
|
Saxena P and Khashab MA: New NOTES
clinical training and program development. Gastrointest Endosc Clin
N Am. 26:385–400. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Saliba F, Lakehal M, Pageaux GP, Roche B,
Vanlemmens C, Duvoux C, Dumortier J, Salamé E, Calmus Y and
Maugendre D; Diapason Study Group, : Risk factors for new-onset
diabetes mellitus following liver transplantation and impact of
hepatitis C infection: An observational multicenter study. Liver
Transpl. 13:136–144. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lin G, Zeng Z, Wang X, Wu Z, Wang J, Wang
C, Sun Q, Chen Y and Quan H: Cholecystectomy and risk of pancreatic
cancer: A meta-analysis of observational studies. Cancer Causes
Control. 23:59–67. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lagergren J and Mattsson F:
Cholecystectomy as a risk factor for oesophageal adenocarcinoma. Br
J Surg. 98:1133–1137. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lagergren J, Mattsson F, El-Serag H and
Nordenstedt H: Increased risk of hepatocellular carcinoma after
cholecystectomy. Br J Cancer. 105:154–156. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Maurer KJ, Carey MC and Fox JG: Roles of
infection, inflammation, and the immune system in cholesterol
gallstone formation. Gastroenterology. 136:425–440. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Martelli MG and Lee JY: Parasitic
infection of the gallbladder: Cystoisospora belli infection as a
cause of chronic abdominal pain and acalculous cholecystitis. J
Miss State Med Assoc. 57:174–176. 2016.PubMed/NCBI
|
|
8
|
Soltes M and Radoňak J: A risk score to
predict the difficulty of elective laparoscopic cholecystectomy.
Wideochir Inne Tech Maloinwazyjne. 9:608–612. 2014.PubMed/NCBI
|
|
9
|
Ko WJ, Song GW, Sukpyo S, Kim DH, Yoo JH,
WonHee K, Kwon C II, Ko KH, Hahm KB, Hong SP, et al: Natural
orifice translumenal endoscopic surgery: Current status and future
perspective. Gastrointestinal Endoscopy. 83:AB6472016. View Article : Google Scholar
|
|
10
|
Morgan M, Olweny EO and Cadeddu JA: LESS
and NOTES instrumentation: Future. Curr Opin Urol. 24:58–65. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zorron R, Phillips HN, Wynn G, Neto MP,
Coelho D and Vassallo RC: ‘Down-to-Up’ transanal NOTES Total
mesorectal excision for rectal cancer: Preliminary series of 9
patients. J Minim Access Surg. 10:144–150. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bernhardt J, Sasse S, Ludwig K and Meier
PN: Update in natural orifice translumenal endoscopic surgery
(NOTES). Curr Opin Gastroenterol. 33:346–351. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Marescaux J, Dallemagne B, Perretta S,
Wattiez A, Mutter D and Coumaros D: Surgery without scars: Report
of transluminal cholecystectomy in a human being. Arch Surg.
142:823–827. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu B, Du B and Pan Y: Video of the Month:
Transrectal gallbladder-preserving cholecystolithotomy via pure
natural orifice transluminal endoscopic surgery: First time in
humans. Am J Gastroenterol. 110:16552015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Schwaitzberg SD, Roberts K, Romanelli JR,
Desilets DJ, Earle D, Horgan S, Swanstrom L, Hungness E, Soper N,
Kochman ML, et al: The NOVEL trial: Natural orifice versus
laparoscopic cholecystectomy-a prospective, randomized evaluation.
Surg Endosc. 32:2505–2516. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tang P, Zhang X, Guo H, Kong J, Sun G, HL
E and Yang Y: Natural orifice transgastric endoscopic operation for
diaphragmatic repair in a dog model. Biomedical Res. 28:1333–1336.
2017.
|