Introduction
Due to its subcutaneous location, clavicle is one of
the bones that are most frequently fractured in the upper body due
to car accidents and sports trauma. The incidence of distal
clavicle fractures accounts for 12–21% of all clavicular fractures
(1). Distal clavicle fractures are
typically attributed to a direct blow to the point of the shoulder
or a fall on an outstretched hand. In Craig class II type II and
class II type V fractures of the distal one-third which are
unstable fractures, the force of the sternocleidomastoid muscle
moves the proximal fragment upward and the weight of the arm moves
the distal fragment downward; these forces cause displacement and
difficulty in maintaining reduction with conservative treatment.
Although non-surgical strategies can be effective for the treatment
of Craig class II type II and class II type V fractures of the
distal one-third, they lead to higher rates of non-union. Non-union
is painful and symptomatic, which has made many to suggest a series
of early surgical treatments of Craig class II type II and class II
type V fractures of the distal one-third of the clavicle (2). Early surgical treatments have been
developed in order to reduce the complication rate of bone
resorption, prominent deformity, and improve the functional
outcome. The unstable fractures seem to represent a challenge
because of the loss of the attachment of the coracoclavicular
ligaments to the clavicle.
In recent years, a variety of methods of surgical
fixation to treat these unstable fractures have been reported,
including the distal clavicle anatomic plate, clavicular hook
plate, double-plate vertical fixation, and T-shaped steel plate
internal fixation, which provide rigid fixation and good bony union
rates. With the extensive use of the surgical fixation, the
fracture healing rate and functional recovery have improved;
however, there is no current consensus regarding which method is
the most suitable. None of the internal fixation techniques
described has been characterized as the ‘gold standard’. Choosing
among these four internal fixators is still controversial. Each of
these treatment modalities has its advantages and disadvantages.
All these four surgical methods could provide good functional
results for patients according to our clinical experience. However,
there is no previous report on their comparison in the literature
reviews.
From January 2015 to May 2017, a total of 84
patients with distal clavicle Craig class II type II and class II
type V fractures were treated with a distal clavicle anatomic
plate, clavicular hook plate, double-plate vertical fixation, or
T-shaped steel plate internal fixation. The aim of this study was
to retrospectively evaluate the clinical results and compare the
efficacy of these four surgical methods for the treatment of acute
unstable distal clavicle fractures. A retrospective analysis of the
patient data was carried out.
Patients and methods
General information
Complete data of 84 patients with Craig class II
type II and class II type V fractures of the distal one-third of
the clavicle, treated with four types of internal fixation methods,
from January 2015 to May 2017, were analyzed retrospectively. Of
the 84 patients, 54 were males and 30 were females, 52.6±28.4 years
of age. The causes of injury were as follows: Traffic injury, 47
cases; and fall injury, 37 cases. The fracture classification
according to Craig was as follows: Class II type II, 70 cases; and
class II type V, 14 cases. The appropriate internal fixation method
was selected based on the length of the distal clavicle fracture
fragment on X-ray pre-operatively. Four patients with comminuted
fractures and distal fractures <0.5 cm in length underwent
double-plate vertical fixation. The remaining cases were
sequentially divided into four groups based on the internal
fixation method used, as follows: Distal clavicle anatomic plate
fixation group (group A), 18 cases; clavicular hook plate internal
fixation group (group B), 26 cases; double-plate vertical fixation
group (group C), 20 cases; and T-shaped steel plate internal
fixation group (group D), 20 cases. There were no significant
differences in sex, age, Craig classification of fracture, cause of
injury, and time from injury to operation among the four groups
(P>0.05, Table I).
 | Table I.Comparison of preoperative general
data among the four groups of patients. |
Table I.
Comparison of preoperative general
data among the four groups of patients.
|
|
| Sex |
| Craig fracture
classification | Cause of injury |
|
|---|
|
|
|
|
|
|
|
|
|---|
| Group | No. | Male | Female | Age (years) | Class II type II | Class II type V | Traffic injury | Fall injury | Time from injury to
operation (days) |
|---|
| Group A | 18 | 11 | 7 | 55.2±16.3 | 15 | 3 | 8 | 10 | 3.4±2.9 |
| Group B | 26 | 16 | 10 | 51.7±17.1 | 22 | 4 | 13 | 13 | 3.2±3.1 |
| Group C | 20 | 14 | 6 | 51.9±20.3 | 16 | 4 | 14 | 6 | 3.4±2.7 |
| Group D | 20 | 13 | 7 | 47.8±15.1 | 17 | 3 | 12 | 8 | 3.4±3.2 |
| χ2/F
value | – | 0.328 | 0.129 | 3.216 | 2.168 | 4.286 |
| P-value | – | 0.628 | 0.746 | 0.168 | 0.348 | 0.251 |
The study was approved by the Ethics Committee of
Dongying People's Hospital (Dongying, China). Patients who
participated in this research had complete clinical data. Signed
informed consents were obtained from the patients or their
guardians.
Operative method
All of the operations were performed by the same
group of physicians.
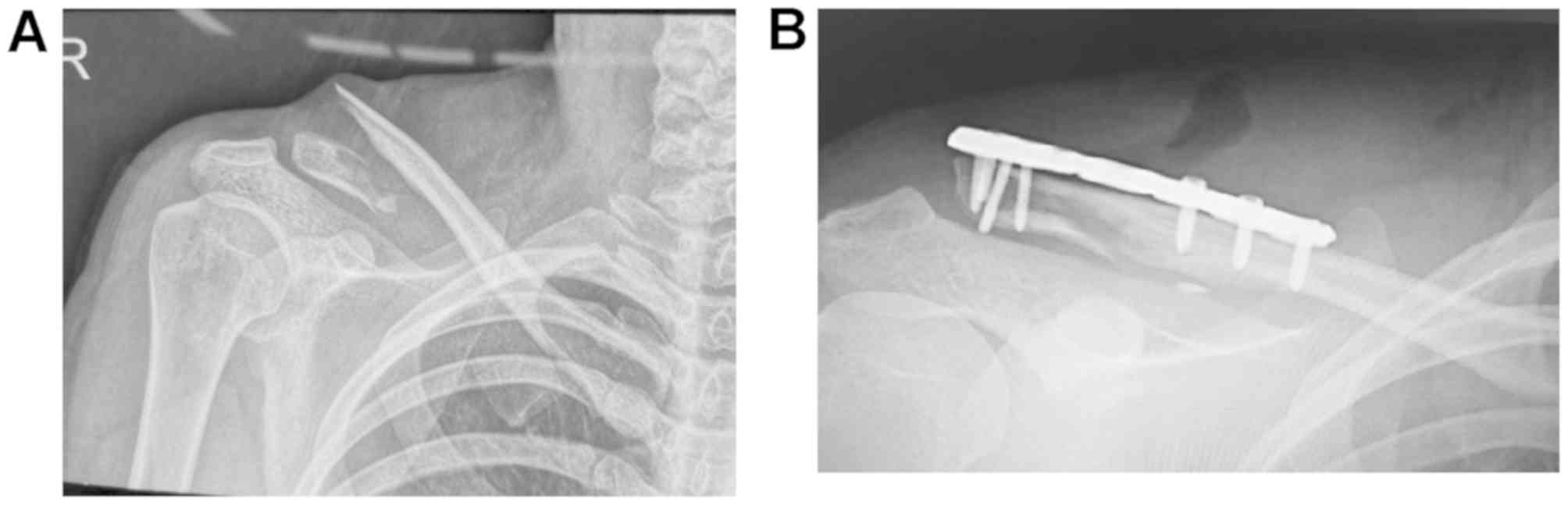
Distal clavicle anatomic plate fixation group (group
A): A transverse incision over the distal clavicle was made to
expose the distal clavicle without completely exposing the
acromioclavicular joint and removing soft tissue. After reduction
of the fracture, the anatomic plate of the distal clavicle was
imbedded. According to the length of the distal end of the
fracture, 3–6 locking screws (2.7 mm) were selected and the
proximal end was fixed with three-to-four 3.5-mm locking screws.
The locking screw did not enter the acromioclavicular joint space.
For comminuted fractures of the distal clavicle, the fracture was
fixed with coarse silk thread with upper and lower annular banding
(Fig. 1).
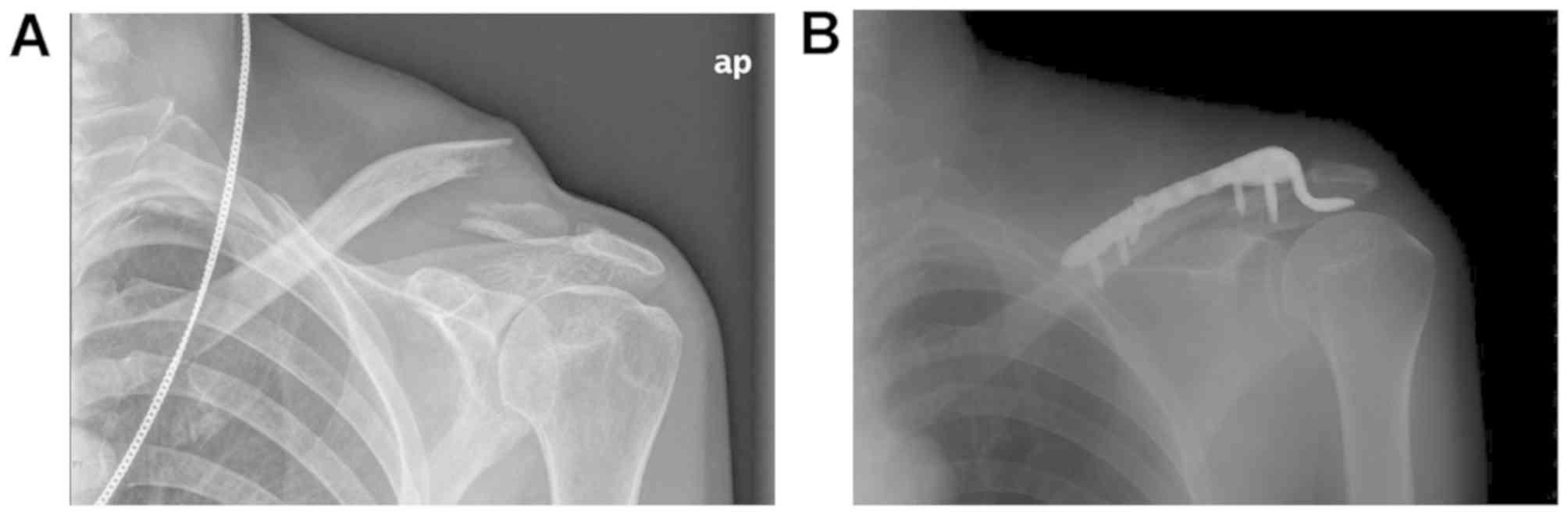
Clavicular hook plate internal fixation group (group
B): An incision was made along the distal surface of the clavicle
to the acromion, the distal clavicle was exposed, a clavicle hook
plate of appropriate length was selected and pre-bent. The clavicle
hook was inserted into the lower rear part of the acromion, and the
plate was placed close to the clavicle. Holes were then drilled
along the proximal and distal ends of the clavicle. The distal
clavicle comminuted fracture was fixed with screws after reduction
and absorbable line was used to bundle up when fixation was not
possible (Fig. 2).
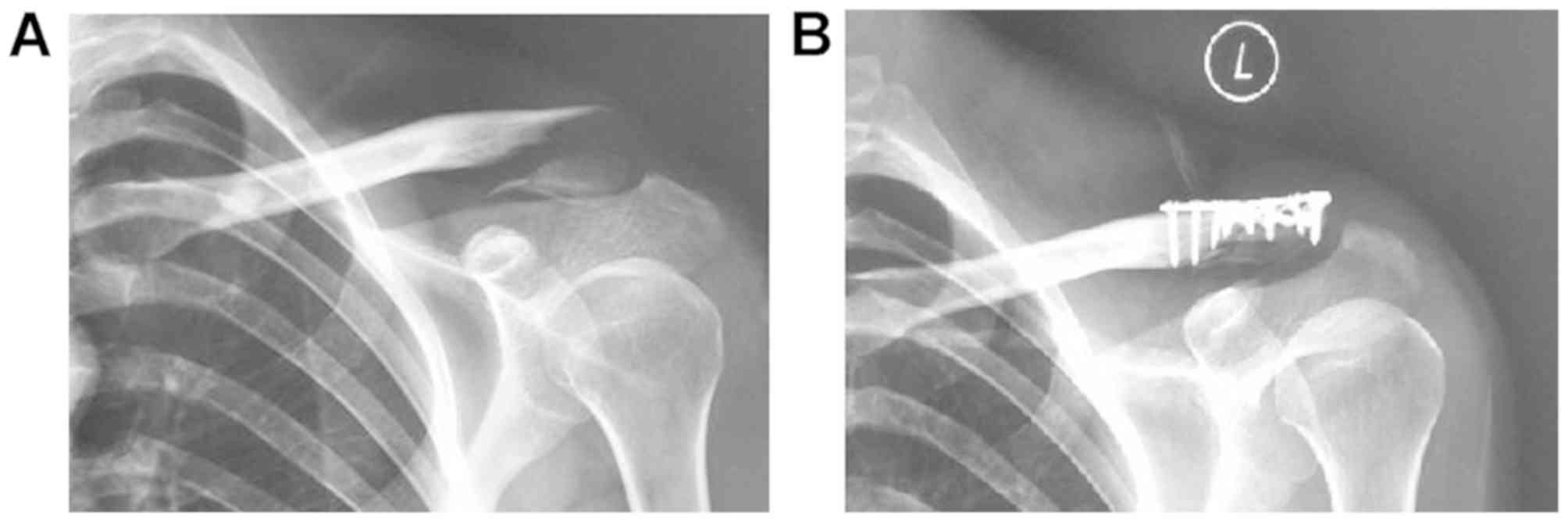
Double-plate vertical internal fixation group (group
C): The fracture end was exposed in layers by a transverse incision
above the clavicle. After reduction of the fracture, two microplate
systems (2.0 mm or 2.5 mm T or L type) were implanted in the
superior and anterior clavicle according to the length from the
fracture line to the articular surface. Screws were selected to fix
the distal and proximal ends of the fracture. For comminuted
fractures of the distal clavicle, it was not necessary to fully
expose the acromioclavicular joint, which could be strapped with
absorbable non-invasive sutures or temporarily fixed with Kirschner
needles. The plate could be bent and shaped according to the
condition of the fracture to enhance attachment to the clavicle
profile, and the distal end of the fracture was fixed with at least
3 screws (Fig. 3).
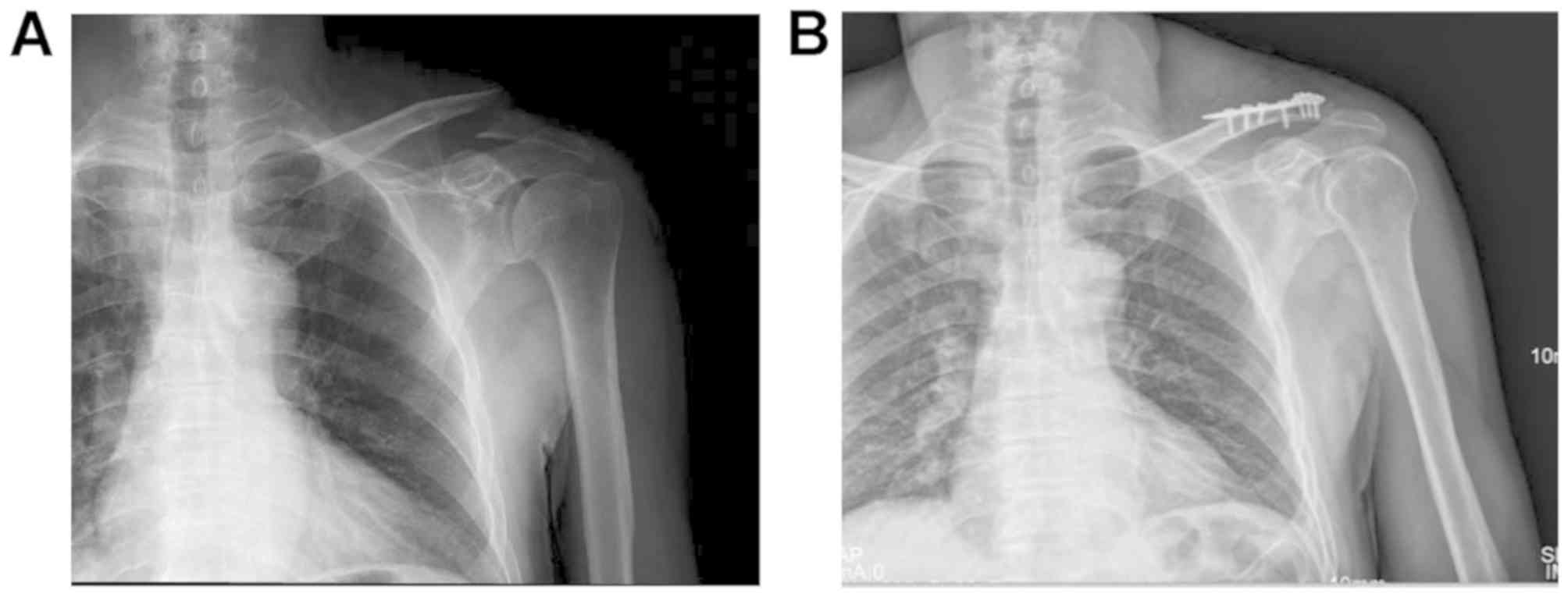
T-shaped steel plate internal fixation group (group
D): A direct incision from the distal clavicle to the acromion was
made, ~5–6 cm in length, layer-by-layer. The fracture end of the
clavicle and the acromioclavicular joint were exposed, the
acromioclavicular ligament was protected, one Kirschner needle was
inserted into the acromioclavicular joint, and screw penetration
was avoided into the acromioclavicular joint. The size of the
distal fracture bone was inspected and determined whether or not
the fracture was comminuted. The distal bone mass was confirmed to
be fixed with at least 3 screws to reset the fracture end.
According to the fracture line, the straight T or oblique T-shaped
steel plate was selected intraoperatively, and the plate was placed
above the clavicle. The suitable length screw was twisted after
drilling the hole. At least 3 screws were screwed in the distal end
of the clavicle and 3–4 cortical screws were screwed into the
proximal end of the clavicle (Fig.
4).
Postoperative management
Patients in each group were treated with wrist bands
to acockbill shoulder joints. Functional activities, such as
forearm rotation and elbow flexion and extension, were performed 6
h postoperatively. Functional exercises, such as anteflexion, back
extension, and shrugging of the upper limbs, were performed 1 week
postoperatively. Proper lifting exercises were performed 3 weeks
postoperatively. The full range of non-load-bearing activities were
gradually restored 6 weeks postoperatively, 1 and 3 months
postoperatively, and every 3 months thereafter. A radiograph was
obtained to observe the fracture healing and gradually complete
weight bearing.
Postoperative evaluation
The operative time, amount of intraoperative
bleeding, cost of hospitalization, time of fracture healing, and
the occurrence of postoperative complications were recorded. The
fracture healing standard was an X-ray showing a fuzzy fracture
line with continuous callus formation. VAS was used to evaluate
pain intensity. At the last follow up, the Constant-Murley
evaluation criteria were used to comprehensively evaluate the
general curative effect on the postoperative shoulder joint
according to the clinical curative effect and imaging results,
which were classified as excellent, good, moderate, or poor. The
postoperative complications in each group were recorded and
compared.
Statistical analysis
SPSS 13.0 statistical software (SPSS, Inc.) was used
to statistically analyze the data expressed as the mean ± SD.
Normally distributed data were analyzed using analysis of variance.
If the difference was statistically significant, then the SNK-q
post hoc test was used to carry out a pairwise comparison.
Enumeration data of the four groups were compared by χ2
test or Fisher's exact probability method. P<0.05 was considered
to indicate a statistically significant difference.
Results
Comparison of preoperative general
data
Because of comminuted fractures and poor distal
screw holding, 2 patients scheduled to undergo double-plate
fixation were treated with clavicular hook plates. Eighteen
patients underwent distal clavicular anatomical plate internal
fixation, 26 patients had clavicular hook plate internal fixation,
20 patients had double-plate vertical internal fixation, and 20
patients underwent T-shaped steel plate internal fixation. The 84
patients were followed up for 13–19 months (average, 17.2 months).
There was no significant difference in age, sex, fracture type, and
time from injury to operation in the four groups (P>0.05;
Table I).
Comparison of intraoperative indexes
and postoperative fracture healing time
There was no significant difference in the operative
time, intraoperative blood loss, hospitalization cost, and fracture
healing time among the four groups (P>0.05; Table II).
 | Table II.Comparison of intraoperative indexes
and postoperative fracture healing time in the four groups of
patients. |
Table II.
Comparison of intraoperative indexes
and postoperative fracture healing time in the four groups of
patients.
| Group | No. | Operative time
(min) | Intraoperative
bleeding (ml) | Hospitalization
expenses (×10,000 CNY) | Fracture healing time
(weeks) |
|---|
| Group A | 18 | 42.3±20.5 | 25.4±10.9 | 1.1±0.8 | 22.7±3.2 |
| Group B | 26 | 41.8±12.4 | 21.8±12.6 | 1.1±0.1 | 22.2±5.1 |
| Group C | 20 | 47.7±26.3 | 28.1±12.2 | 0.9±0.2 | 22.4±2.8 |
| Group D | 20 | 41.2±15.7 | 24.3±11.5 | 1.1±0.2 | 23.1±3.5 |
| F value | – | 2.364 | 4.218 | 2.549 | 4.878 |
| P-value | – | 0.246 | 0.194 | 0.159 | 0.243 |
Comparison of VAS in the four groups
of patients
VAS for the distal clavicle anatomic plate group
(group A), double-plate vertical fixation group (group C), and
T-shaped steel plate internal fixation group (group D) was
significantly better than the clavicular hook plate group (group B)
(P<0.05; Table III).
 | Table III.Comparison of VAS at 2 and 6 months
after operation, 1 week before the removal of internal fixation,
and at the last follow up in the four groups of patients. |
Table III.
Comparison of VAS at 2 and 6 months
after operation, 1 week before the removal of internal fixation,
and at the last follow up in the four groups of patients.
|
| VAS |
|---|
|
|
|
|---|
| Group | 2 months after
operation | 6 months after
operation | 1 week before removal
of internal fixation | Last follow up |
|---|
| Group A |
5.92±0.32a |
2.32±0.22a |
1.43±0.24a |
1.21±0.11a |
| Group B | 6.74±0.26 | 2.89±0.28 | 1.73±0.21 | 1.54±0.11 |
| Group C |
5.82±0.46a |
2.41±0.26a |
1.44±0.46a |
1.30±0.24a |
| Group D |
5.95±0.46a |
2.58±0.58a |
1.55±0.42a |
1.33±0.28a |
| F value | 2.186 | 5.274 | 1.628 | 1.862 |
| P-value | 0.038 | 0.026 | 0.028 | 0.022 |
Comparison of Constant-Murley score
and incidence of postoperative complications in the four groups of
patients
Evaluation of shoulder function according to the
Constant-Murley criteria was as follows: The distal clavicle
anatomic plate group (group A) was classified as excellent (12
cases), good (5 cases), moderate (1 case), and poor (0 cases), with
an excellent and good rate of 94.4%; the clavicular hook plate
group (group B) was classified as excellent (8 cases), good (11
cases), moderate (5 cases), and poor (2 cases), with an excellent
and good rate of 73.1%; the double-plate vertical internal fixation
group (group C) was classified as excellent (13 cases), good (6
cases), moderate (1 case), and poor (0 cases), with an excellent
and good rate of 95%; and the T-shaped steel plate internal
fixation group (group D) was classified as excellent (12 cases),
good (4 cases), moderate (3 cases), and poor (1 case), with an
excellent and good rate of 80%. The excellent and good rates for
the double-plate vertical internal fixation (group C) and distal
clavicle anatomic plate fixation group (group A) were significantly
better than those of the the clavicular hook plate group (group B)
and T-shaped steel plate internal fixation group (group D). There
were significant differences in the Constant-Murley scores between
various follow-up periods postoperatively (P<0.05; Table IV).
 | Table IV.Comparison of Constant-Murley score
at 2 and 6 months after operation, 1 week before the removal of
internal fixation, and at the last follow up, and incidence of
postoperative complications in the four groups of patients. |
Table IV.
Comparison of Constant-Murley score
at 2 and 6 months after operation, 1 week before the removal of
internal fixation, and at the last follow up, and incidence of
postoperative complications in the four groups of patients.
|
| Constant-Murley
score |
|
|---|
|
|
|
|
|---|
| Group | 2 months after
operation | 6 months after
operation | 1 week before
removal of internal fixation | Last follow up | Total occurrence of
complications [n (%)] |
|---|
| Group A |
75.2±5.3a,b |
77.4±5.2a,b |
82.2±4.1a,b |
89.9±2.8a,b | 0a,b |
| Group B | 62.9±4.1 | 72.1±3.4 | 77.1±5.3 | 83.1±5.6 | 4 (15.4) |
| Group C |
76.1±6.4a,b |
78.1±4.6a,b |
83.3±3.6a,b |
90.2±4.4a,b | 1 (5)a,b |
| Group D |
72.5±4.4a |
75.1±5.3a |
80.7±3.7a |
88.3±2.47a | 3 (15) |
| F value | 4.216 | 6.002 | 5.024 | 3.906 |
|
| P-value | 0.00086 | 0.00074 | 0.00062 | 0.00048 |
|
None of the patients in the four groups had
complications, such as wound infections, fractures around the
plate, and fractures of the plate. In the clavicular hook plate
group (group B), 3 patients had osteoarthritis and 1 patient had
shoulder pain. One patient in the double-plate vertical internal
fixation group (group C) and 3 patients in the T-shaped steel plate
internal fixation group (group D) had early removal of nails. The
incidence of postoperative complications in the clavicular hook
plate group (group B) was 15.4% (4/26) and in the T-shaped steel
plate internal fixation group (group D) was 15% (3/20),
significantly higher than those in the distal clavicle anatomic
plate group (group A) and double-plate vertical internal fixation
group (group C).
Discussion
Among the fractures involving the distal one-third
of the clavicle, Craig class II type II and class II type V
fractures most often involve the ligamenta coracoclaviculare and
acromioclavicular joint. Fracture non-union, acromioclavicular
joint dysfunction, and other complications of conservative
treatment are relatively high (3).
The purpose of surgical treatment is to stabilize the distal
clavicle, to avoid non-union of the fracture, to allow early
functional exercise, and to reduce complications (4).
Advantages and disadvantages of the four internal
fixation methods and selection of indications. The clavicular hook
plate is a dynamic internal fixation, the main principle of which
is that the lateral tip hook is inserted under the acromion along
the posterior edge of the acromioclavicular joint, while the medial
plate is fixed on the clavicle. The clavicular hook plate forms a
sustained and stable lever that lifts up the acromion and presses
down the clavicle to reset and fix the displaced distal clavicle
fracture, minimizes the movement of the distal end of the fracture,
and does not interfere with the rotation of the clavicle. This
fixation is widely used in the treatment of distal clavicle
fractures (5). The mechanical
distribution of the clavicular hook plate is uneven, and the stress
near the acromioclavicular joint is greater. Therefore, after
reduction and fixation the distal clavicle tends to sink and
undergo excessive reduction, which affects the therapeutic effect
(6). For elderly patients with
osteoporosis, the brittleness of bone is increased and the clavicle
in contact with the medial end of the hook plate is prone to stress
fractures. Loose bone will also reduce the holding power of screws
and it is easy to lose screws, resulting in failure of internal
fixation. Therefore, use of the clavicle hook plate should be
performed with caution in elderly patients (7). Application of the clavicle hook plate
to juvenile patients with immature bone may interfere with the
normal development of the acromion and cause permanent damage to
the acromion. Therefore, the age of the patients should be
considered first when selecting the clavicle hook plate for
internal fixation. The appropriate depth of the clavicle hook plate
and appropriate bending of the hook plate can be chosen
intraoperatively to avoid excessive lifting up of the acromion, and
to reduce lifting stress of the hook tip acting on the acromion,
subacromial bone erosion, and the occurrence of subacromial
impingement.
The distal clavicle anatomic plate design of the
distal end of the plate is a 2.7-mm small locking screw with a
double row of six different directions with 2.7- and 3.5-mm screw
systems in the distal anterolateral clavicle. There is no
significant difference in bone holding force (8). Therefore, as long as the distal
clavicle has a bone block 2 cm in length, even if the fracture
block is comminuted, >3 locking screws can be used with the
screws in different directions to stabilize the fracture. There is
a gap between the plate and periosteum after the distal
anterolateral clavicle plate is placed, and there is no compression
of bone and periosteum, which reduces the compression of the
periosteum and the destruction of local blood circulation, and
provides a good environment for the fracture to the maximum extent
(9). The distal clavicle anatomic
plate in the distal anterolateral clavicle does not involve the
acromioclavicular joint, there is no interference and stress on the
acromion and the rotator cuff, and no complications, such as
subacromial bone resorption, impingement, and rotator cuff injury,
will arise (10). The passive motion
of the joint is not limited postoperatively, and early functional
exercise creates a good condition for recovery of shoulder joint
function. To our opinion, for patients with a distal clavicle
fracture >2 cm the anterolateral clavicle fixation with a distal
clavicle anatomic plate can be considered.
Miniature steel plates can provide a reliable
control effect for comminuted bone with different direction screws
and reliable fixation for comminuted bone. The vertical placement
of double steel plates on two mutually 90° planes to form a beam
structure also increases the fastness of the flattened frame
structure at the distal end of the clavicle. The miniature steel
plate is thinner and smaller, which ensures that there is enough
space to implant two plates above and in front of the distal
clavicle fracture and vertical fixation to achieve anatomic
reduction. There are at least 3 screws fixed in the vertical plane
in the distal clavicle (11). After
the double miniature steel plate has been shaped and bent, the
plate can be fitted well to the clavicle to achieve firm fixation,
and the anatomic position of the fracture end can be maintained
effectively; the occurrence of bone disunion, loosening, and
fracture of the plate can be reduced (12). The distal end does not involve the
acromioclavicular joint and has no interference and stress on the
acromion. It will not lead to compressive bone absorption and
impact of the subacromial bone nor cut the rotator cuff to cause
injury. The cost of vertical internal fixation with a double plate
is the lowest of the four methods, and double plate improves the
stability of fixation, effectively reduces internal fixation
failure and reduction, provides biological conditions for stable
bone healing, and creates conditions for early postoperative
rehabilitation and exercise (13).
For patients with a small length of distal clavicle fracture, a
double miniature steel plate fixation should be considered.
Because the T-shaped steel plate at the distal end
of the radius is thin and easy to shape, the distal clavicle is
slightly intamescentia, flat, and the clavicle is not loaded, thus
the treatment of distal clavicular fractures with this plate cannot
only fix the end of the fracture, but also it does not interfere
with the acromioclavicular joint and the perioperative soft tissue
injury is also small. A multi-directional locking nail could
provide a stable fixation for the distal end of the fracture
(14). Moreover, because the
T-shaped steel plate is thinner, occupies less space, and the
clavicle tissue is looser. If the patient does not request removal
due to discomfort, the plate can remain in situ after
fracture healing, which can reduce the pain of a second operation
and alleviate the economic burden. Because of the design problem of
the T-shaped plate in the distal radius, it is impossible to fix
all the locking holes in different directions at the outboard end
of the distal radius with locking screws at the same time.
Therefore, it is easy to lose the screws when the locking holes are
fixed with ordinary screws.
Comparison of postoperative complications. The
incidence of postoperative complications in the clavicular hook
plate group (group B) was 15.4%, and in the T-shaped steel plate
internal fixation group (group D) was 15%, significantly higher
than the distal clavicle anatomic plate group (group A) and
double-plate vertical internal fixation group (group C)
(P<0.05). In the clavicular hook plate group (group B), 3
patients had osteoarthritis after the plate was removed, and 1
patient had shoulder pain and other clinical symptoms. The
appearance of osteoarthritis after the removal of the clavicular
hook plate is closely related to the principle of leverage of the
clavicular hook plate. The clavicle hook plate contacts the
acromion through the hook tip, so the bone surface of the acromion
is the concentration point of the lever stress. The pressure caused
by lifting up the hook tip and the friction formed by the movement
of the tip on the acromial surface will result in absorption and
abrasion of the subacromial bone. There will be imaging signs of
osteoarthritis at the hook tip of the removed hook plate (15). In addition to choosing a clavicle
hook plate of suitable depth during surgery, an appropriate shape
of the hook plate can be made so that the hook tip can fit
completely under the shoulder peak, thus avoiding excessive lifting
of the acromion (16). In the
clavicular hook plate group (group B), shoulder pain occurred in 1
patient postoperatively. The subacromian space was narrower in this
patient. It was considered that stimulating the bursae synovialis
of the acromium during the insertion of the hook plate might have
caused synovitis. Compression of the supraspinatus muscle may have
resulted in subacromial impingement. In the T-shaped steel plate
group (group D), early de-nailing occurred in 3 patients
postoperatively. Considering that the original intention of
designing the T-shaped steel plate was not according to the
anatomic structure of the clavicle, it was easy for the patients
with small distal clavicle fractures to be unable to use locking
screws completely. In the patients who choose to use the T-shaped
steel plate the distal radius can be molded according to the shape
of the distal clavicle fracture block during the operation.
Comparison of postoperative functional recovery. The
long-term functional recovery of the distal clavicle anatomic plate
group (group A), the double-plate vertical internal fixation (group
C), and the distal radius T-shaped steel plate internal fixation
group (group D) was significantly better than the clavicular hook
plate group (group B) (P<0.05). The distal anatomic clavicle
plate, double-plate vertical internal fixation, and T-shaped steel
plate of the distal radius do not involve the acromioclavicular
joint, and do not produce interference and stress of the acromion,
avoiding the occurrence of osteoarthritis and impingement in
subacromial iconography, and no damage to the acromion sac and
supraspinatus muscle occurs. The early stability of the T-shaped
steel plate of the distal radius was significantly worse than the
distal clavicular anatomic plate and double-plate vertical
fixation. Therefore, the early functional exercise of the shoulder
joint in the T-shaped steel plate of the distal radius (group D)
was worse than in the distal clavicular anatomic plate (group A)
and double-plate vertical internal fixation group (group C).
Shortcomings of this study. i) It was considered
that two patients with fractures were unable to use at least 3
screws to fix the distal clavicle fracture block and to be switched
to the clavicular hook plate. ii) This study was a retrospective
analysis, however, the patients underwent a non-randomized
selection of pre- and intra-operative procedures. There were
numerous patients with fractures who received clavicular hook
plates, and there was a selection bias in the internal fixation
options, which may be one of the reasons for the poor efficacy of
the clavicular hook plate group. iii) In recent years, the use of a
double-button steel plate for the treatment of Neer II type
fractures has been gradually applied to clinical practice. The
operation is relatively simple, does not involve the
acromioclavicular joint, does not interfere with the subacromial
space, and does not damage the rotator cuff. Moreover, the
procedure reduces postoperative shoulder pain and the button steel
plate is small in size. Compared with the hook and locking plates,
the built-in object is not obvious and more cosmetic. There is no
need for secondary surgery to remove the double-button steel plate,
however, complications including intraoperative coracoid process
fracture, non-union and delayed union have been observed (17). Rieser et al (4) conducted biomechanical experiments and
confirmed that the mechanical strength of the button steel plate or
locking plate fixation was significantly lower than the button
steel plate combined with locking plate fixation. The fixed
stability of this procedure is to be further studied in later
biomechanical experiments. iv) In this study, the sample size was
small, and therefore a randomized controlled study of a larger
sample is needed to confirm the conclusions of this report.
In conclusion, all four methods were effective in
the treatment of distal clavicle fractures. The distal clavicular
anatomic plate and double-plate vertical internal fixation led to a
decreased incidence of shoulder pain, increased the range of motion
of the shoulder, and reduced complications. Hence, the distal
clavicular anatomic plate and double plate vertical internal
fixation are preferable for the early functional recovery of the
limbs.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LL and HW were involved in the writing of the
manuscript. LL made substantial contributions to the conception and
design of the current study and gave final approval of the version
to be published. PJ contributed to the design of the study. SC
approved the version to be published, analyzed and interpreted the
patient data regarding the distal clavicle fracture. XH and HW were
involved in the conception of the study. XY contributed to the
interpretation of the data. XH and SC were accountable for all
aspects of the work in ensuring that questions related to the
accuracy or integrity of any part of the work were appropriately
investigated and resolved. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Dongying People's Hospital (Dongying, China). Patients who
participated in this research had complete clinical data. Signed
informed consents were obtained from the patients or their
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gstettner C, Tauber M, Hitzl W and Resch
H: Rockwood type III acromioclavicular dislocation: Surgical versus
conservative treatment. J Shoulder Elbow Surg. 17:220–225. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Martetschläger F, Kraus TM, Schiele CS,
Sandmann G, Siebenlist S, Braun KF, Stöckle U, Freude T and
Neumaier M: Treatment for unstable distal clavicle fractures (Neer
2) with locking T-plate and additional PDS cerclage. Knee Surg
Sports Traumatol Arthrosc. 21:1189–1194. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Oe K, Gaul L, Hierholzer C, Woltmann A,
Miwa M, Kurosaka M and Buehren V: Operative management of
periarticular medial clavicle fractures-report of 10 cases. J
Trauma Acute Care Surg. 72:E1–E7. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rieser GR, Edwards K, Gould GC, Markert
RJ, Goswami T and Rubino LJ: Distal-third clavicle fracture
fixation: A biomechanical evaluation of fixation. J Shoulder Elbow
Surg. 22:848–855. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Deng Z, Cai L, Ping A, Ai Q and Wang Y:
Anatomical research on the subacromial interval following
implantation of clavicle hook plates. Int J Sports Med. 35:857–862.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gu X, Cheng B, Sun J and Tao K:
Arthroscopic evaluation for omalgia patients undergoing the
clavicular hook plate fixation of distal clavicle fractures. J
Orthop Surg Res. 9:462014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jou IM, Chiang EP, Lin CJ, Lin CL, Wang PH
and Su WR: Treatment of unstable distal clavicle fractures with
Knowles pin. J Shoulder Elbow Surg. 20:414–419. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yoo JH, Chang JD, Seo YJ and Shin JH:
Stable fixation of distal clavicle fracture with comminuted
superior cortex using oblique T-plate and cerclage wiring. Injury.
40:455–457. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Johnston PS, Sears BW, Lazarus MR and
Frieman BG: Fixation of unstable type II clavicle fractures with
distal clavicle plate and suture button. J Orthop Trauma.
28:e269–e272. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Andersen JR, Willis MP, Nelson R and
Mighell MA: Precontoured superior locked plating of distal clavicle
fractures: A new strategy. Clin Orthop Relat Res. 469:3344–3350.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Madsen W, Yaseen Z, LaFrance R, Chen T,
Awad H, Maloney M and Voloshin I: Addition of a suture anchor for
coracoclavicular fixation to a superior locking plate improves
stability of type IIB distal clavicle fractures. Arthroscopy.
29:998–1004. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sohn HS, Shin SJ and Kim BY: Minimally
invasive plate osteosynthesis using anterior-inferior plating of
clavicular midshaft fractures. Arch Orthop Trauma Surg.
132:239–244. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bisbinas I, Mikalef P, Gigis I, Beslikas
T, Panou N and Christoforidis I: Management of distal clavicle
fractures. Acta Orthop Belg. 76:145–149. 2010.PubMed/NCBI
|
|
14
|
Schliemann B, Roßlenbroich SB, Schneider
KN, Petersen W, Raschke MJ and Weimann A: Surgical treatment of
vertically unstable lateral clavicle fractures (Neer 2b) with
locked plate fixation and coracoclavicular ligament reconstruction.
Arch Orthop Trauma Surg. 133:935–939. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lin HY, Wong PK, Ho WP, Chuang TY, Liao YS
and Wong CC: Clavicular hook plate may induce subacromial shoulder
impingement and rotator cuff lesion-dynamic sonographic evaluation.
J Orthop Surg Res. 38:1461–1468. 2014.
|
|
16
|
Dou Q and Ren X: Clinical therapeutic
effects of AO/ASIF clavicle hook plate on distal clavicle fractures
and acromioclavicular joint dislocations. Pak J Med Sci.
30:868–871. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cho CH, Jung JH and Kim BS:
Coracoclavicular stabilization using a suture button device for
Neer type IIB lateral clavicle fractures. J Shoulder Elbow Surg.
26:804–808. 2017. View Article : Google Scholar : PubMed/NCBI
|