Introduction
Laparoscopy is performed worldwide due to its
limited side effects and optimal healing efficacy compared with
traditional surgery. Despite these advantages, laparoscopy has
adverse effects, including atelectasis and ischemia-reperfusion
injury (IRI), due to CO2 accumulation during ventilation
in a head-down position, in particular during gynecological
laparoscopic surgery (1,2). These may sometimes result in severe
disorders and affect the postoperative recovery, prolong the
hospitalization (3,4).
Several different mechanisms account for the adverse
effects of pneumoperitoneum and ventilation. Specific trials have
been performed proposing that hyperinflation and repetitive tidal
recruitment may promote the release of pro-inflammatory mediators,
which may lead to lung injury (5).
Previous clinical investigations have demonstrated that free
reactive oxygen species produced by activation of neutrophils and
by the inflammatory response are an essential factor for inducing
lung IRI (6). A previous trial
suggested that impairment of oxygenation contributed to the
development of atelectasis. Ventilation is provided due to
impairment of lung function, which is accompanied by increased
expression of cytokines, including tumor necrosis factor-α (TNF-α)
and interleukin 1β (IL-β) (7). To
date, several trials have demonstrated that mechanical ventilation
with lower tidal volumes and positive end-expiratory pressure can
prevent pulmonary inflammation and protect against post-operative
pulmonary complications (8,9). The underlying mechanism for this could
be the reduction of myeloperoxidase and elastase levels in the
bronchoalveolar lavage fluid in addition to the inhibition of
polymorphonuclear cells activity, which were recruited to the
pulmonary compartment (8,9). However, there is currently no consensus
regarding the optimal protective ventilation during general
anesthesia.
Transcutaneous electrical acupoint stimulation
(TEAS) is a complementary and alternative treatment method that
combines transcutaneous electrical nerve stimulation (TENS) with
traditional acupuncture in order to deliver a specific
low-frequency pulse current to the body through the skin. It has
been demonstrated to improve the inflammatory response during
general anesthesia (10). The
present study was performed to test the hypothesis that TEAS
protects against lung injury occurring in patients undergoing
gynecological laparoscopy under general anesthesia, which is most
commonly performed in a head-down position.
Patients and methods
Study population and design
Ethical approval of this study was granted by the
Human Research Ethical Committee of Shengjing Hospital (Shenyang,
China; IRB registration no. 2015PS57J). Informed consent was
obtained from all participants. The present study was registered at
http://www.clinicaltrials.gov prior to
enrollment of the patients (registration no. NCT02850471).
A total of 100 patients aged between 18 and 65 years
who were scheduled for gynecological laparoscopic surgery under
general anesthesia at Shengjing Hospital of China Medical
University (Shenyang, China) were included in the present study.
The subjects were recruited between March 2015 and July 2015 and
were classified according to the American Society of
Anesthesiologists physical status classification of I or II
(11). The exclusion criteria were
as follows: Pre-existing lung or cardiac disease, impaired kidney
or liver function, history of bronchial asthma or chronic
obstructive pulmonary disease, history of smoking, respiratory
infection two weeks prior to enrollment and pre-operative use of a
bronchodilator or a steroid.
Randomization and blinding
The patients were randomly assigned either to the
TEAS or the control groups using a computer-generated random number
sequence. The group assignment was performed in sealed opaque
envelopes that were numbered sequentially. The acupuncturist from
the Department of Traditional Chinese Medicine of the Shengjing
Hospital (Shenyang, China) was informed of the randomization
allocation and was only responsible for placing the electrodes and
turning on and/or off the stimulator. No communication occurred
between him and the investigators of the study. The patients,
attending anesthesiologists, surgeons and data collectors were all
blinded to the allocation. In order to enhance the reliability of
the study, the patients in the control group had electrodes placed
at the same acupoints as the patients in the TEAS group. Patients
in either of the two groups were told that the acupuncture points
would be stimulated by the instrument with a low stimulation
frequency so that a person may experience only a mild electric
current sensation or feel nothing at all (12).
Study protocol
The patients in the TEAS group were treated with a
stimulator (Hwato Electronic Acupuncture Treatment Instrument;
model no. SDZ-II; Suzhou Medical Appliances Co., Ltd.) on the
Feishu (BL13), Hegu (LI4) and Chize (LU5) acupoints 30 min prior to
the induction of anesthesia. The stimulus wave exhibited an
alternate ‘dense-disperse’ form with the frequency of the disperse
wave being 2 Hz and that of the dense wave being 100 Hz. The
optimal intensity was adjusted to maintain a slight twitching of
the regional muscle according to the individual maximum tolerance.
The stimulus continued until 5 min prior to the end of surgery. The
patients in the control group were also connected to the apparatus,
although no electronic stimulation was applied.
Standardized anaesthesia and
peri-operative management
All patients fasted overnight and received no
pre-medication. Upon arrival in the operating room, standard
monitoring, including an electrocardiogram lead II, non-invasive
arterial blood pressure and pulse oximetry to measure the oxygen
saturation (SpO2) were applied. Furthermore, venous
access was established using a 18-gauge cannula on the dorsum of
the hand, connected to a T-connector. Transfusion was performed
with lactated Ringer's solution at a rate of 30 drops per min.
General anesthesia was induced with Sufentanil citrate injection
(0.2 µg/kg) and Etomidate fat emulsion injection (2.5 mg/kg).
Cisatracurium Besylate injection (0.2 mg/kg) was used to facilitate
intubation. After adequate jaw relaxation was attained, tracheal
intubation was performed and each patient was mechanically
ventilated with the tidal volume and ventilation rate adjusted to
maintain the pressure of end-tidal carbon dioxide at 35–45 mmHg and
the SpO2 at ≥92%. Maintenance of anesthesia was achieved
by administration of sevoflurane in an air-oxygen mixture at a
fresh gas flow rate of 2 l/min. The bispectral index was maintained
between 40 and 55 during the operation by adjusting the flow rate
of sevoflurane. If the MAP was lower than the fundamental value of
30%, the patients were administered 6 mg hydrochloride ephedrine.
If the MAP was >120%, urapidil hydrochloride (0.10–0.15 mg/kg)
was administered. Atropine sulfate (0.2 mg) was administered if the
heart rate (HR) was <50 beats per min. One anaesthesiologist who
was blinded to the grouping performed the anaesthesia. The same
group of experienced surgeons performed all of the surgeries.
Following extubation, the patients were transferred to the
post-anaesthesia care unit for continuous monitoring.
Hemodynamic index and blood gas
analysis index
The mean arterial pressure (MAP), HR and
SpO2 were recorded at the following time-points: Arrival
at the operating room (T0), immediately prior to
induction of the pneumoperitoneum (T1), immediately
after the end of pneumoperitoneum (T2) and on leaving
the operating room (T3). Arterial blood samples were
collected from the radial artery or dorsal artery of the foot for
blood gas analysis to record pH, determine the partial pressure of
carbon dioxide (PCO2) and calculate the oxygenation
index (OI) at T0–3.
Serum concentrations of TNF-α and
IL-1β
Blood samples were taken from the peripheral vein
for determination of serum concentrations of tumor necrosis factor
α (TNF-α) and interleukin 1β (IL-1β) at T0 and
T3. Peripheral venous blood samples were collected into
pre-cooled anti-coagulant tubes and subsequently centrifuged at
3,000 × g for 10 min at the temperature of 4°C. The plasma was
transferred into polyethylene tubes and stored at −80°C. The plasma
concentration levels of TNF-α (cat. no. 20150220), IL-1β (cat. no.
20150208) were measured using ELISA kits (Shanghai Kmaels
Biological Technology Co., Ltd.; http://www.kmsbiotech.com) according to the
manufacturer's protocols, following which absorbance was read at
wavelength of 450 nm using the multifunctional microplate reader
(Thermo Fisher Scientific, Inc.).
Postoperative pulmonary
complications
Post-operative pulmonary complications that occurred
during the first 5 days after surgery were also documented. The
complications included hypoxemia, bronchospasm, suspected pulmonary
infection, pulmonary infiltrate, aspiration pneumonitis,
atelectasis, pleural effusion, pulmonary edema and pneumothorax.
Hypoxaemia was defined as SpO2 <90% during ≥10% of
the total recording time (13).
Bronchospasm was defined as a sudden constriction of the muscles of
bronchioles. It is a symptom of pulmonary conditions, namely
asthma, chronic bronchitis, anaphylaxis, dyspnea, anoxia, asthma
and asphyxia. Pneumonia was defined as a new development of
pulmonary infiltration detected by chest X-ray. It is characterized
by acute respiratory symptoms (cough, fever, sputum production or
pleuritic chest pain) and elevated inflammatory markers. This
condition requires antibiotic treatment (14,15).
Atelectasis was defined as large-size atelectasis of lobar
involvement detected by chest X-ray. Pleural effusion was defined
as an abnormal accumulation of fluid in the pleural cavity, which
is >0.1–0.2 ml/kg body weight (16). Pulmonary edema was defined as
radiologically diagnosed pulmonary interstitial fluid accumulation.
Pneumothorax was defined as an abnormal accumulation of gas within
the pleural space, which is usually confirmed by imaging
techniques. For instance, the chest radiographs of pneumothorax
include a white visceral pleural line separating the lung from the
chest wall, accompanied by loss of standard lung markings located
in the periphery of this white line (17).
Sample size
The sample size calculation was based on the rate of
change of the levels of the IL-1β cytokine prior to and immediately
after the surgery (18,19). A preliminary study demonstrated that
34 patients in each group were required for a 10% difference of
IL-1β between the groups immediately after the surgery, assuming a
two-sided Type I error (α) of 0.05 and a power of 90%. Potential
loss was expected during follow-up or due to dropout and therefore,
the sample size was increased to 100 patients.
Statistical analysis
SPSS 19.0 statistical software (IBM Corp.) was
employed for data analysis. The normality of distribution was
assessed using Kolmogorov-Smirnov test. Data that followed a normal
distribution were expressed as the mean ± standard deviation or n
(%). All continuous variables were compared using an independent
Student's t-test or the Mann-Whitney U-test. The repeated
measurement values were compared at each time-point using repeated
analysis of variance followed by Bonferroni correction for multiple
comparisons. Categorical variables were expressed as n (%) and were
compared using the chi-squared test or Fisher's exact test as
appropriate. P<0.05 was considered to indicate a significant
difference.
Results
Participant Enrollment
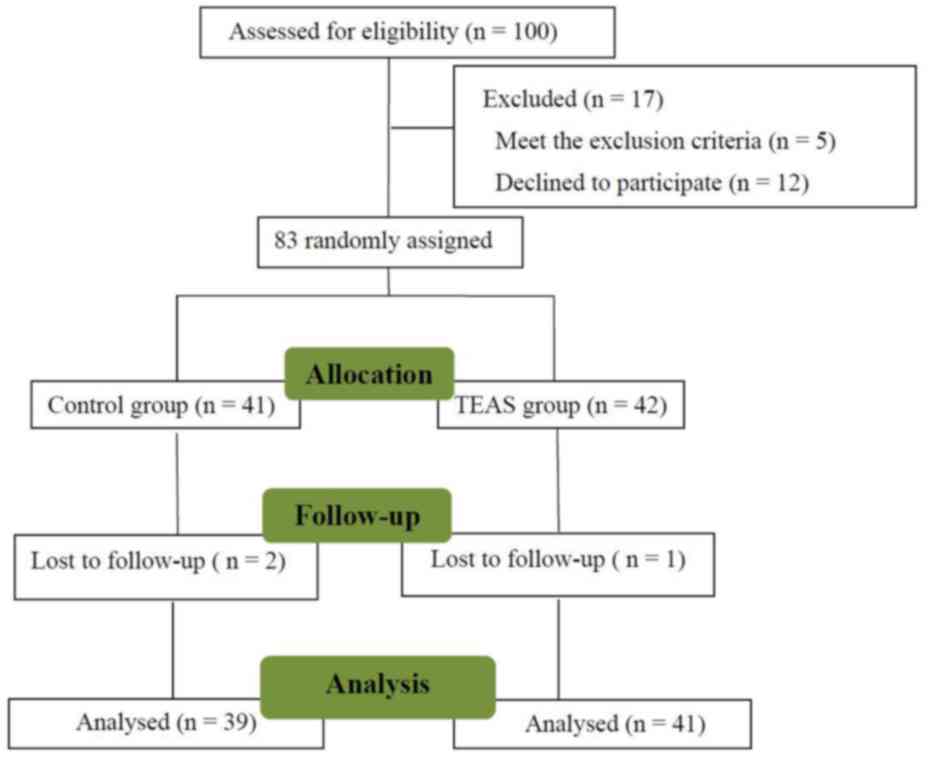
Between March 2015 and July 2015, 100 patients were
enrolled at Shengjing Hospital (Shenyang, China). A flow chart
depicting the patient enrolment and their movement throughout the
study is provided in Fig. 1. A total
of 41 and 39 patients were randomly allocated to the TEAS and the
control group, respectively. A total of 20 patients were excluded
from the analysis due to consent withdrawal (n=12), satisfaction of
exclusion criteria (n=5) and due to loss to follow-up (n=3). The
patient characteristics and the type and duration of their
procedures (including the surgical type) were not significantly
different between the two groups (P>0.05, Table I).
 | Table I.Comparison of patient
characteristics. |
Table I.
Comparison of patient
characteristics.
| Item | TEAS group
(n=41) | Control group
(n=39) | P-value |
|---|
| Age (years) | 44.7±10.8 | 47.3±11.0 | 0.303 |
| Body weight
(kg) | 55.1±5.4 | 57.0±6.1 | 0.148 |
| Body height
(cm) | 160.2±3.9 | 159.9±3.8 | 0.792 |
| Duration of
anaesthesia (min) | 157.2±41.2 | 168.1±51.6 | 0.300 |
| Duration of surgery
(min) | 140.1±39.4 | 149.3±49.3 | 0.364 |
| Surgery type |
| Total
hysterectomy | 9 (22.0) | 9 (23.1) | 0.904 |
|
Subtotal hysterectomy | 3 (7.3) | 1 (2.6) | 0.616 |
| Total
hysterectomy and bilateral appendectomy | 3 (7.3) | 4 (10.3) | 0.709 |
|
Myomectomy | 12 (29.3) | 7 (17.9) | 0.234 |
|
Oophorocystectomy | 12 (29.3) | 13 (33.3) | 0.695 |
| Radical
hysterectomy | 0 (0) | 1 (2.6) | 0.488 |
| Radical
hysterectomy and pelvic lymphadenectomy | 2 (4.9) | 4 (10.3) | 0.426 |
Comparison of MAP, HR,
SpO2, blood pH, PCO2 and OI
The MAP, HR, SpO2, blood pH,
PCO2 and OI were compared at various time-points
(Table II). No significant
differences were noted between the MAP, HR and SpO2 in
these two groups (P>0.05). Blood gas analysis demonstrated no
significant differences in terms of pH and PCO2.
However, the OI in the control group was significantly lower than
that in the TEAS group (P<0.05, Table II) at the timepoints of
T2 and T3.
 | Table II.Comparison of the variables measured
at different time-points. |
Table II.
Comparison of the variables measured
at different time-points.
| Parameters | TEAS group
(n=41) | Control group
(n=39) |
|---|
| MAP (mmHg) |
|
T0 |
89.7±7.9 |
90.7±10.6 |
|
T1 |
86.2±9.6 |
86.2±10.8 |
|
T2 |
83.1±10.9 |
86.2±10.7 |
|
T3 |
86.2±10.1 |
86.1±10.1 |
| HR (beats/min) |
|
T0 |
76.1±10.7 |
74.7±12.7 |
|
T1 |
74.2±10.8 |
69.4±11.7 |
|
T2 |
69.8±9.7 |
70.1±11.2 |
|
T3 |
73.7±10.5 |
78.3±9.8 |
|
SpO2 |
|
T0 |
99.4±0.6 |
99.5±0.5 |
|
T1 |
99.6±0.6 |
99.5±0.7 |
|
T2 |
99.6±0.5 |
99.5±0.9 |
|
T3 |
99.7±0.8 |
99.6±0.9 |
| pH |
|
T0 |
7.4±0.04 |
7.4±0.06 |
|
T1 |
7.3±0.06 |
7.3±0.04 |
|
T2 |
7.3±0.06 |
7.3±0.03 |
|
T3 |
7.4±0.03 |
7.4±0.04 |
| PCO2
(mmHg) |
|
T0 |
42.8±6.1 |
44.4±6.8 |
|
T1 |
44.4±8.8 |
45.0±8.1 |
|
T2 |
42.1±8.1 |
45.2±7.6 |
|
T3 |
39.5±4.9 |
39.9±5.9 |
| OI |
|
T0 |
425.6±21.2 |
423.2±22.0 |
|
T1 |
450.5±30.0 |
442.3±28.9 |
|
T2 |
491.6±37.8a |
460.1±39.3 |
|
T3 |
423.7±25.3a |
395.0±31.5 |
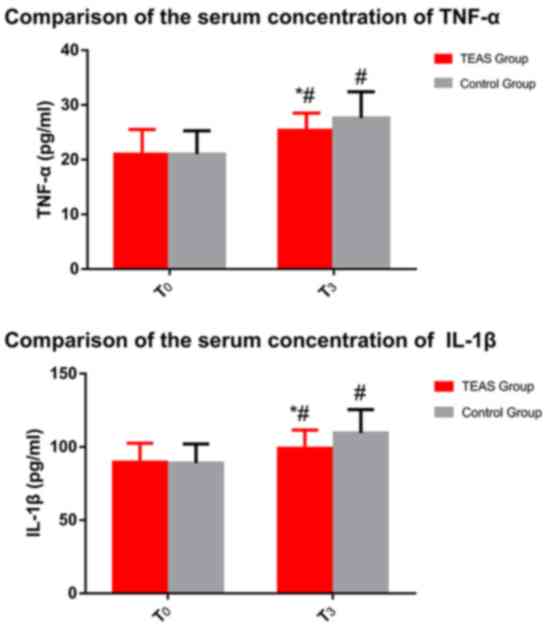
Serum concentrations of TNF-α and
IL-1β
The serum concentrations of TNF-α and IL-1β were
significantly increased following surgery (P<0.05, Fig. 2). The extent of the increase of the
serum concentration of TNF-α and IL-1β in the TEAS group was
significantly lower than that in the control group (P<0.05).
Postoperative pulmonary
complications
Postoperative pulmonary complications were reported
in 3 out of 41 patients (7.3%) in the TEAS group compared with 10
out of 39 patients (25.6%) in the control group (P<0.05;
Table III). The results indicated
that hypoxemia was the most common complication following
laparoscopy, where the incidence was lower in the TEAS group
compared with that in the Control group (P<0.05). But no
significant differences were noted between the two groups in the
other items.
 | Table III.Post-operative pulmonary
complications in the first five days after surgery. |
Table III.
Post-operative pulmonary
complications in the first five days after surgery.
| Item | TEAS group
(n=41) | Control group
(n=39) |
|---|
| Total |
3
(7.3)a |
10
(25.6) |
| Hypoxaemia |
0
(0)a |
4
(10.3) |
| Bronchospasm |
0 (0) |
0 (0) |
| Suspected pulmonary
infection |
1
(2.4) |
1
(2.6) |
| Pulmonary
infiltrate |
0 (0) |
2
(5.1) |
| Aspiration
pneumonitis |
0 (0) |
0 (0) |
| Atelectasis |
1
(2.4) |
1
(2.6) |
| Pleural
effusion |
1
(2.4) |
2
(5.1) |
| Pulmonary
edema |
0 (0) |
0 (0) |
| Pneumothorax |
0 (0) |
0 (0) |
Discussion
Gynecological laparoscopic surgery is frequently
performed in a head-down position to facilitate laparoscopic
surgical manipulation in which carbon dioxide inflation of the
pneumoperitoneum is induced (1,8), which
was also performed in the present study. As a result of the
head-down body position, mechanical ventilation and abdominal
pressure are increased, which impairs the respiratory function.
This increases the risk of post-operative pulmonary complications,
including atelectasis formation and IRI (5,8,20). Atelectasis and ischemia and
reperfusion may trigger several different physiological responses,
including pulmonary edema, as well as lymphocyte and neutrophil
infiltration, which activate the immune system and result in a
hypercoagulable state. IRI is an inflammatory process that occurs
in the organs during anoxia (20).
The pathophysiology of atelectasis and IRI in the
lungs is complex and multifactorial. Previous studies have
indicated that a variety of inflammatory mediators are responsible
for inducing cell damage by regulating vascular permeability and
leukocyte activity (6). Furthermore,
it was demonstrated that cerebral ischemia and reperfusion was due
to inflammation partly caused by cerebral ischemia (21). Cytokine signaling is a unique way to
respond to particular cellular stimuli. Pulmonary injury caused by
atelectasis and IRI is a particular consequence of inflammatory
reaction. During this reaction, the inflammatory effector cells,
including neutrophils, are activated and facilitate the release of
specific cytokines in response to specific chemotactic signals
(22). A previous study showed that
IL-1β and TNF-α contributed to the eradication of the infection by
engaging immune and non-immune cells (23). TNF-α and IL-1β are typical cytokines
released in the early phase of the inflammatory reaction.
Furthermore, TNF-α and IL-1β are able to activate the cytokine
signaling network and induce cellular apoptosis (24–27).
During cerebral ischemia, the expression levels of TNF-α and IL-1β
are significantly increased, which may further exacerbate brain
injury (28). A specific signaling
pathway is activated following nuclear translocation of NF-κB
during IRI. This signaling pathway may further activate downstream
associated pro-inflammatory cytokines, including TNF-α and IL-1β,
which in turn induce inflammatory reactions (29,30).
Cannizzaro et al (31)
demonstrated that atelectasis was associated with the production of
TNF-α, whereas neutrophil infiltration was associated with changes
in IL-1β expression levels. Furthermore, secretion of TNF-α and
IL-1β has been noted in pulmonary edema (32–34).
Atelectasis and IRI may cause damage to pulmonary cells. It was
further indicated that TNF-α and IL-1β levels were increased
following surgery, suggesting that lung atelectasis and IRI may
occur during surgery.
TEAS is a unique treatment method, which delivers a
specific low-frequency pulse current to the body through the skin
at specific acupoints via TENS. TEAS induce less pain and injury
and may cause a lower incidence of infection compared with
traditional electroacupuncture. In addition, it exhibits optimal
patient tolerability. The response efficacy critically depends on
the stimulation parameters. According to the theory of Traditional
Chinese Medicine, the Feishu acupoint (BL13) is mainly used to
treat cough, asthma, chest fullness, spitting blood and other signs
associated with pulmonary infections. Furthermore, acupuncture at
BL13 may improve pulmonary function and reduce lung tissue and cell
inflammation (35–38). Acupuncture at the Hegu acupoint (LI4)
is considered to exert an analgesic and sedative effect and is a
key acupuncture point for anesthesia (39). Previous studies have demonstrated
that acupuncture at LI4 may effectively improve the remodeling of
the cough reflex in patients with tracheotomy following cerebral
hemorrhage and immunosuppression in patients undergoing
pneumonectomy (40,41). The Chize acupoints (LU5) belong to
the Lung Meridian of Hand-Taiyin and may be used to treat cough due
to their potential analgesic effects (42).
TEAS exert various effects, including inhibition of
apoptosis, anti-inflammatory effects and cell protection (43,44).
Previous studies on IRI indicated that electroacupuncture is able
to protect the brain against injury through inhibition of
apoptosis, reduction of oxidative stress and inhibition of the
inflammatory response (45,46). Animal and human studies have
suggested that acupuncture may be used to treat dyspnea by
stimulating the release of endogenous opioid compounds and by
regulating the limbic system (47,48).
Previous studies reported that electroacupuncture exerted
anti-inflammatory effects and that it was able to cause a decrease
in the expression levels of TNF-α and IL-1β (49–51). In
the present study, TEAS decreased the expression levels of TNF-α
and IL-1β and improved the inflammatory response.
The OI is an important indicator of the oxygenation
status of the lung with a higher value indicating better
oxygenation of the lung. The present study suggested that the OI in
the control group was significantly lower than that in the TEAS
group at the different time-points of T2 and
T3. The serum concentrations of TNF-α and IL-1β were
significantly increased following surgery, which indicates
inflammatory reactions during laparoscopic surgery. In addition,
the serum concentrations of TNF-α and IL-1β were increased in the
TEAS group to a lower extent than those in the control group, which
is consistent with the conclusion that TEAS may inhibit the
inflammatory response caused by laparoscopic surgery and protect
against lung injury, as well as reduce the incidence of pulmonary
complications. However, further studies are required to explore the
mechanisms of the protective effect of TEAS against pulmonary
inflammation.
A significant limitation of the present study was
that only relatively healthy female subjects were included in the
study protocol (without cardiovascular and/or cerebrovascular
diseases and/or pulmonary disease). Therefore, it remains to be
determined whether the results may be generalized to patients with
pulmonary diseases or to patients who are critically ill. However,
the present study is the first to demonstrate that TEAS may be
beneficial in reducing the pulmonary injury caused by gynecological
laparoscopic surgery.
In conclusion, ventilation-associated lung injury in
the pneumoperitoneum, which may be attributed to inflammatory
injury, induction of atelectasis and IRI, may be reduced by TEAS,
which is able to protect the lung from these types of injury.
Further studies are necessary to explore the mechanism of action
responsible for these processes.
Acknowledgements
The authors gratefully thank Dr Raymond Koehler from
the Department of Anesthesiology and Critical Care Medicine, Johns
Hopkins University (Baltimore, US) for his valuable input in the
present study.
Funding
The present study was funded by the Ministry of
Science and Technology of Liaoning Province, China (grant no.
20102282) and the Sanxin project of Shengjing Hospital of China
Medical University (grant no. 2015PS57J) and the Support Plan for
Innovative Talents in Liaoning Higher Education Institution (grant
no. 201834).
Availability of data and materials
The datasets used and/or analyzed in the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
WW, WB, YL and JZ designed the study. WW, WB, YY,
XT, YL and YW performed of the study. WW, WB, XT and JZ performed
the data analysis. WW, WB, YY and JZ prepared the manuscript. All
authors contributed to the conception of the study and read and
approved the final manuscript.
Ethics approval and consent to
participate
Ethical approval of this study was granted by the
Human Research Ethical Committee of Shengjing Hospital (Shenyang,
China; IRB registration no. 2015PS57J). Informed consent was
obtained from all of the participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
IRI
|
ischemia-reperfusion injury
|
|
TEAS
|
transcutaneous electrical acupoint
stimulation
|
|
TNF-α
|
tumor necrosis factor α
|
|
IL-1β
|
interleukin 1β
|
|
TENS
|
transcutaneous electrical nerve
stimulation
|
|
MAP
|
mean arterial pressure
|
|
HR
|
heart rate
|
|
SpO2
|
oxygen saturation
|
|
OI
|
oxygen index
|
|
PCO2
|
partial pressure of carbon dioxide
|
References
|
1
|
Valenza F, Chevallard G, Fossali T, Salice
V, Pizzocri M and Gattinoni L: Management of mechanical ventilation
during laparoscopic surgery. Best Pract Res Clin Anaesthesiol.
24:227–241. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Strang CM, Hachenberg T, Fredén F and
Hedenstierna G: Development of atelectasis and arterial to
end-tidal PCO2-difference in a porcine model of pneumoperitoneum.
Br J Anaesth. 103:298–303. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
YP Deng and HS Huang: Effects of different
pneumoperitoneal pressures on hemodynamics and arterial blood gas
in geriatric patients during laparoscopic surgery. J Clin
Anesthesiology. 27:741–743. 2011.
|
|
4
|
Simonson DA, Adams AB, Wright LA, Dries
DJ, Hotchkiss JR and Marini JJ: Effects of ventilatory pattern on
experimental lung injury cause by high airway pressure. Crit Care
Med. 32:781–786. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
PROVE Network Investigators for the
Clinical Trial Network of the European Society of Anaesthesiology,
; Hemmes SN, Gama de Abreu M, Pelosi P and Schultz MJ: High versus
low positive end-expiratory pressure during general anesthesia for
open abdominal surgery (PROVHILO trial): A multicentre randomized
controlled trial. Lancet. 384:495–503. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fard N, Saffari A, Emami G, Hofer S,
Kauczor HU and Mehrabi A: Acute respiratory distress syndrome
induction by pulmonary ischemia-reperfusion injury in large animal
models. J Surg Res. 189:274–284. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Duggan M and Kavanagh BP: Pulmonary
atelectasis: A Pathogenic Perioperative Entity. Anesthesiology.
102:838–854. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cinnella G, Grasso S, Spadaro S, Rauseo M,
Mirabella L, Salatto P, De Capraris A, Nappi L, Greco P and
Dambrosio M: Effects of recruitment maneuver and positive
end-expiratory pressure on respiratory mechanics and transpulmonary
pressure during laparoscopic surgery. Anesthesiology. 118:114–122.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wolthuis EK, Choi G, Dessing MC, Bresser
P, Lutter R, Dzoljic M, van der Poll T, Vroom MB, Hollmann M and
Schultz MJ: Mechanical ventilation with lower tidal volumes and
positive end-expiratory pressure prevents pulmonary inflammation in
patients without preexisting lung injury. Anesthesiology.
108:46–54. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhou F, Guo J, Cheng J, Wu G, Sun J and
Xia Y: Electroacupuncture and brain protection against cerebral
ischemia: Specific effects of acupoints. Evid Based Complement
Alternat Med. 2013:8043972013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Daabiss M: American society of
anaesthesiologists physical status classification. Indian J
Anaesth. 55:111–115. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Arai YC, Kato N, Matsura M, Ito H,
Kandatsu N, Kurokawa S, Mizutani M, Shibata Y and Komatsu T:
Transcutaneous electrical nerve stimulation at the PC-5 and PC-6
acupoints reduced the severity of hypotension after spinal
anaesthesia in patients undergoing Caesarean section. Br J Anaesth.
100:78–81. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ogna A, Nardi J, Prigent H, Quera Salva
MA, Chaffaut C, Lamothe L, Chevret S, Annane D, Orlikowski D and
Lofaso F: Prognostic Value of initial assessment of residual
hypoventilation Using nocturnal capnography in Mechanically
Ventilated neuromuscular Patients: A 5-Year Follow-up study. Front
Med (Lausanne). 3:402016.PubMed/NCBI
|
|
14
|
Kim HJ, Lee J, Park YS, Lee CH, Lee SM,
Yim JJ, Yoo CG, Kim YW, Han SK and Choi SM: Impact of GOLD groups
of chronic pulmonary obstructive disease on surgical complications.
Int J Chron Obstruct Pulmon Dis. 11:281–287. 2016.PubMed/NCBI
|
|
15
|
Kim TH, Lee JS, Lee SW and Oh YM:
Pulmonary complications after abdominal surgery in patients with
mild-to-moderate chronic obstructive pulmonary disease. Int J Chron
Obstruct Pulmon Dis. 11:2785–2796. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Biswas B, Sharma SK, Negi RS, Gupta N,
Jaswal VM and Niranjan N: Pleural effusion: Role of pleural fluid
cytology, adenosine deaminase level and pleural biopsy in
diagnosis. J Cytol. 33:159–162. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
MacDuff A, Arnold A and Harvey J: BTS
Pleural Disease Guideline Group; Management of spontaneous
pneumothorax: British thoracic society pleural disease guideline
2010. Thorax. 65:ii18–ii31. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Maissen-Villiger CA, Schweighauser A, van
Dorland HA, Morel C, Bruckmaier RM, Zurbriggen A and Francey T:
Expression profile of cytokines and enzymes mRNA in blood
leukocytes of dogs with leptospirosis and its associated pulmonary
hemorrhage syndrome. PLoS One. 11:e01480292016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Weng S, Wang L, Rong Y, Liu Y, Wang X,
Guan H and Chen W: Effects of the interactions between dust
exposure and genetic polymorphisms in nalp3, caspase-1 and IL-1β on
the risk of silicosis: A case-control study. PLoS One.
10:e01409522015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gielis JF, Jungraithmayr W, Boulet GA,
Bogers JP, Weder W, Cos P and Van Schil PE: A murine model of lung
ischemia and reperfusion injury: Tricks of the trade. J Surg Res.
194:659–666. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ikeda K, Negishi H and Yamori Y:
Antioxidant nutrients and hypoxia/ischemic brain injury in rodents.
Toxicology. 189:55–61. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Strieter RM, Belperio JA and Keane MP:
Cytokines in innate host defense in the lung. J Clin Invest.
109:699–705. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Funakoshi T, Ishibe Y, Okazaki N, Miura K,
Liu R, Nagai S and Minami Y: Effect of re-expansion after
short-period lung collapse on pulmonary capillary permeability and
pro-inflammatory cytokine gene expression in isolated rabbit lungs.
Br J Anaesth. 92:558–563. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ashkenazi A and Dixit VM: Death receptors:
Signaling and modulation. Science. 281:1305–1308. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nagata S: Apoptosis by death factor. Cell.
88:355–365. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Okusawa S, Gelfand JA, Ikejima T, Connolly
RJ and Dinarello CA: Interleukin 1 induces a shock-like state in
rabbits. Synergism with tumor necrosis factor and the effect of
cyclooxygenase inhibition. J Clin Invest. 81:1162–1172. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ward PA: Role of complement, chemokines
and regulatory cytokines in acute lung injury. Ann N Y Acad Sci.
796:104–112. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lalancette-Hébert M, Phaneuf D, Soucy G,
Weng YC and Kriz J: Live imaging of toll-like receptor two response
in cerebral ischemia reveals the role of olfactory bulb microglia
as modulators of inflammation. Brain. 132:940–954. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Barton GM and Medzhitov R: Toll-like
receptor signaling pathways. Science. 300:1524–1525. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Blanco AM, Pascual M, Valles SL and Guerri
C: Ethanol-induced iNOS and COX-2 expression in cultured astrocytes
via NF-kappa B. Neuroreport. 15:681–685. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Cannizzaro V, Hantos Z, Sly PD and Zosky
GR: Linking lung function and inflammatory responses in
ventilator-induced lung injury. Am J Physiol Lung Cell Mol Physiol.
300:L112–L120. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Iqbal M, Multz AS, Rossoff LJ and Lackner
RP: Reexpansion pulmonary edema after VATS successfully treated
with continuous positive airway pressure. Ann Thorac Surg.
70:669–671. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wake M, Sanagawa Y and Okamoto Y: A case
of anesthetic management for reexpansion pulmonary edema of the
dependent lung saved by superimposed HFJV during one-lung
ventilation for the thoracoscopic operation associated with
bilateral pneumothorax. Masui. 49:643–645. 2000.(In Japanese).
PubMed/NCBI
|
|
34
|
Yanagidate F, Dohi S, Hamaya Y and Tsujito
T: Reexpansion pulmonary edema after thoracoscopic mediastinal
tumor resection. Anesth Analg. 92:1416–1417. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Fang YG, Zhou XZ, Liu BY and Wang YY: A
study on the essential drugs and points for point application in
summer to treat the diseases with attacks in winter. J Tradit Chin
Med. 30:180–184. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Carneiro ER, Carneiro CR, Castro MA,
Yamamura Y and Silveira VL: Effect of electroacupuncture on
bronchial asthma induced by ovalbumin in rats. J Altern Complement
Med. 11:127–134. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ngai SP and Jones AY: Changes in skin
impedance and heart rate variability with application of Acu-TENS
to BL 13 (Feishu). J Altern Complement Med. 19:558–563. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Li J, Wu S, Tang H, Huang W, Wang L, Zhou
H, Zhou M, Wang H and Li J: Long-term effects of acupuncture
treatment on airway smooth muscle in a rat model of the
smoke-induced chronic obstructive pulmonary disease. Acupunct Med.
34:107–113. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhang Q, Gao Z, Wang H, Ma L, Guo F, Zhong
H, Xiong L and Wang Q: The effect of pre-treatment with
transcutaneous electrical acupoint stimulation on the quality of
recovery after ambulatory breast surgery: A prospective, randomized
controlled trial. Anaesthesia. 69:832–839. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Cai GF, Shang L, Liu K, Zhao H, Quan A,
Yan C, Sun H, Li X and Zhuang Z: Remodeling of cross
electro-nape-acupuncture on cough reflex in patients with a
tracheotomy after cerebral hemorrhage: A randomized controlled
trial. Zhongguo Zhen Jiu. 35:3–6. 2015.(In Chinese). PubMed/NCBI
|
|
41
|
Fan WC, Ma W, Zhao C, Tong QY and Shen WD:
Influence of acupuncture-drug compound anesthesia with different
frequency electroacupuncture on immune function in patients
undergoing pneumonectomy. Zhongguo Zhen Jiu. 32:715–719. 2012.(In
Chinese). PubMed/NCBI
|
|
42
|
Fang XJ and Dong L: Acupuncture at Chize
(LU5) for 23 cases of intractable hiccup. Zhongguo Zhen Jiu.
35:10602015.(In Chinese). PubMed/NCBI
|
|
43
|
Chung JH, Lee EY, Jang MH, Kim CJ, Kim J,
Ha E, Park HK, Choi S, Lee H, Park SH, et al: Acupuncture decreases
ischemia-induced apoptosis and cell proliferation in the dentate
gyrus of gerbils. Neurol Res. 29 (Suppl 1):S23–S27. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Kang KA, Shin ES, Hur J, Hasan MR, Lee H,
Park HJ, Park HK and Kim YJ: Acupuncture attenuates neuronal cell
death in middle cerebral artery occlusion model of focal ischemia.
Neurol Res. 32 (Suppl 1):S84–S87. 2010. View Article : Google Scholar
|
|
45
|
Shen MH, Zhang CB, Zhang JH and Li PF:
Electroacupuncture attenuates cerebral ischemia and reperfusion
injury in middle cerebral artery occlusion of rat via modulation of
apoptosis, inflammation, oxidative stress and excitotoxicity. Evid
Based Complement Alternat Med. 2016:94386502016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Iadecola C and Alexander M: Cerebral
ischemia and inflammation. Curr Opin Neurol. 14:89–94. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Parshall MB, Schwartzstein RM, Adams L,
Banzett RB, Manning HL, Bourbeau J, Calverley PM, Gift AG, Harver
A, Lareau SC, et al: An official American Thoracic Society
statement: Update on the mechanisms, assessment and management of
dyspnea. Am J Respir Crit Care Med. 185:435–452. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Bauml J, Haas A, Simone CB II, Li SQ,
Cohen RB, Langer CJ and Mao JJ: Acupuncture for dyspnea in lung
cancer: Results of a feasibility trial. Integr Cancer Ther.
15:326–332. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Jiang JH, Yang EJ, Baek MG, Kim SH, Lee SM
and Choi SM: Anti-inflammatory effects of electroacupuncture in the
respiratory system of asymptomatic amyotrophic lateral sclerosis
animal model. Neurodegener Dis. 8:504–514. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Gu G, Zhang Z, Wang G, Han F, Han L, Wang
K, Liu J and Li W: Effects of electroacupuncture pretreatment on
inflammatory response and acute kidney injury in endotoxemic rats.
J Int Med Res. 39:1783–1797. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Lan L, Tao J, Chen A, Xie G, Huang J, Lin
J, Peng J and Chen L: Electroacupuncture exerts anti-inflammatory
effects in cerebral ischemia-reperfusion injured rats via
suppression of the TLR4/NF-κB pathway. Int J Mol Med. 31:75–80.
2013. View Article : Google Scholar : PubMed/NCBI
|