Introduction
Cerebral infarction is a common brain disease. Due
to its danger and the rapid increase in the number of patients
(1), this disease has become one of
the diseases with high mortality in the world. Clinically, cerebral
infarction is caused by cerebral tissue necrosis and low oxidation
due to insufficient blood supply caused by cerebral vascular
stenosis and thrombosis of patients. With the further deterioration
of the condition of patients, cognitive impairment caused by
cerebral infarction will gradually worsen, eventually leading to
dementia, affecting their quality of daily life (2–4).
Therefore, the choice of treatment plan for cerebral infarction is
an important medical research direction.
According to long-term clinical trials, acute
cytokines such as high-sensitivity C-reactive protein (hs-CRP),
serum soluble intercellular adhesion molecule-1 (sICAM-1) and tumor
necrosis factor-α (TNF-α) are closely related to cerebral
infarction, especially acute cerebral infarction (5,6). Hs-CRP,
as an acute inflammatory response protein, has the function of
destroying vascular endothelium, and can activate platelet
activity, promote platelet aggregation and increase the probability
of thrombosis (7), thus increasing
the probability of cerebral thrombosis. The mechanism of action of
TNF-α in cerebral infarction is that free radicals produced by
TNF-α may damage vascular endothelial cells, cause
vasoconstriction, aggravate coagulation state, promote thrombosis,
and eventually lead to ischemia, hypoxia and even necrosis
(8). SICAM-1 is an intercellular
adhesion molecule, which can mediate leukocyte adhesion and
aggregation, and can be used as a corresponding indicator in
various diseases caused by atherosclerosis (9,10).
Therefore, hs-CRP, sICAM-1 and TNF-α can generally be used as
detection factors for cardiovascular and cerebrovascular diseases
including cerebral infarction.
Aspirin and clopidogrel are two common drugs that
are often used clinically. Aspirin can reduce the incidence rate of
thrombosis by inhibiting cyclooxygenase and inhibiting platelet
release and aggregation in vivo. Clopidogrel, as an
antiplatelet drug, can reduce the expression of CD40L, an
inflammatory mediator, in activated platelets induced by adenosine
diphosphate, and may have anti-inflammatory effect (11,12).
Because of their thrombotic and anti-inflammatory effects, they are
often used in the treatment of cardiovascular and cerebrovascular
diseases including cerebral infarction. This investigation was
designed to explore the clinical efficacy of the combination of the
two drugs in the treatment of cerebral infarction and their effects
on serum-related cytokines hs-CRP, sICAM-1 and TNF-α.
Patients and methods
General information
Ninety patients with acute cerebral infarction
treated in Yidu Central Hospital of Weifang (Weifang, China) were
analyzed. According to the different treatment plans of these
patients, those treated with the combination of the two drugs were
divided into group B (n=50), and those treated with aspirin alone
were group A (n=40). Comparing the general clinical baseline data
between group B and A, the difference was not significant
(P>0.05) (Table I).
 | Table I.General clinical baseline data of
group A and B n (%)(mean ± SD). |
Table I.
General clinical baseline data of
group A and B n (%)(mean ± SD).
| Variables | Group A (n=40) | Group B (n=50) |
t-test/χ2 | P-value |
|---|
| Sex |
|
| 0.639 | 0.424 |
| Male | 31 (77.5) | 35 (70.00) |
|
|
| Female | 9 (22.5) | 15 (30.00) |
|
|
| Age (years) |
|
| 0.058 | 0.810 |
| Below 60 | 8 (20.00) | 9 (18.00) |
|
|
| 60 and above | 32 (80.00) | 41 (82.00) |
|
|
| Weight (kg) | 65.54±11.03 | 63.95±10.57 | 0.696 | 0.487 |
| Smoking |
|
| 0.002 | 0.962 |
| Yes | 21 (52.50) | 26 (52.00) |
|
|
| No | 19 (47.50) | 24 (48.00) |
|
|
| Drinking |
|
| 0.143 | 0.706 |
| Yes | 20 (50.00) | 27 (54.00) |
|
|
| No | 20 (50.00) | 23 (46.00) |
|
|
| Hyperlipidemia |
|
| 0.009 | 0.924 |
| Yes | 18 (45.00) | 22 (44.00) |
|
|
| No | 22 (55.00) | 28 (56.00) |
|
|
| Hypertension |
|
| 2.431 | 0.119 |
| Yes | 25 (62.50) | 23 (46.00) |
|
|
| No | 15 (37.50) | 27 (54.00) |
|
|
| Diabetes |
|
| 0.035 | 0.850 |
| Yes | 20 (50.00) | 26 (52.00) |
|
|
| No | 20 (50.00) | 24 (48.00) |
|
|
Inclusion criteria: All patients included in this
study were diagnosed and treated in the above hospital, and were
confirmed as cerebral infarction with complete clinical data.
Exclusion criteria: i) Patients suffering from
serious endocrine diseases; ii) patients whose onset time and
admission time exceed 6 h; iii) patients with gastrointestinal
hemorrhage and gastrointestinal inflammation; iv) patients
suffering from chronic liver diseases, adrenal gland diseases and
serious heart diseases for a long time and (v) patients with
long-term taboo symptoms related to surgical treatment of this
disease.
The family members of the patients were informed by
telephone, and an informed consent was signed voluntarily. The
study was examined and approved by the Ethics Committee of Yidu
Central Hospital of Weifang.
Methods
Group A: Patients were administered aspirin
enteric-coated tablets (SFDA approval no: H20065051; Shenyang
Shuangding Pharmaceutical Co., Ltd.) 100 mg/time, once a day for 3
weeks.
Group B: Patients were administered aspirin
enteric-coated tablets combined with clopidogrel. Aspirin 100
mg/time was taken orally first, followed by clopidogrel sulfate
tablets (SFDA approval no: H20000542; Shenzhen Salubris
Pharmaceutical Co., Ltd.) 75 mg/time, once a day for 3 weeks.
Detection methods
A total of 4 ml venous blood was taken at two time
points, before the first treatment and three weeks after treatment,
in the fasting state of the patient. Serum was obtained by low
speed centrifugation for 4–5 min at 1,800 × g at 4°C. Enzyme-linked
immunosorbent assay was used to detect the expression level of
hs-CRP (SFDA Approval no: 2400848; Getein Biotechnology Co., Ltd.)
BIOBASE2000 automatic enzyme immunoassay analyzer (Jinan Xinbeixi
Biotechnology Co., Ltd.) was used; radioimmunoassay was used to
analyze the expression levels of sICAM-1 (item no: im-E10088;
Shanghai Kanglang Biotechnology Co., Ltd.) and TNF-α (item no:
JLC7047-96T; Wuhan MSK Biotechnology Co., Ltd.); DFM-96
radioimmunoassay γ counter (Hefei Zhongchen Light Industrial
Machinery Co., Ltd.) was used.
Observation indicators and evaluation
standard
The NIHSS scores of patients in group A and B before
and after treatment were compared (NIH Stroke Scale, NIHSS)
(13). Τhe levels of hs-CRP, TNF-α
and sICAM-1 in blood samples taken from patients before and after
treatment were compared between the two groups. Τhe adverse
reactions after treatment, such as gastrointestinal hemorrhage,
malignant vomiting, allergy and arrhythmia, were compared between
the two groups.
The total effective rates of patients in group A and
B were compared: Εvaluation criteria (14): i) Basic rehabilitation: dysfunction
score reduced by 91–100% and degree of disability was 0; ii)
markedly effective: dysfunction score reduced by 46–90%, while the
degree of disability was between 1 and 3; iii) effective:
dysfunction score reduced by 18–45%; iv) no change: dysfunction
score decreased or increased <18%; v) deterioration: dysfunction
score increased >18%; vi) death. Total effective rate = basic
rehabilitation + markedly effective + effective.
Statistical analysis
SPSS 19.0 (SPSS, Inc., Chicago, IL, USA) was used
for statistical analysis of comprehensive data, χ2 test
was used for counting data, and (mean ± SD) for measurement data.
Paired t-test was used for comparison of expression level before
and after treatment in the same group. The expression levels of
groups A and B at the same time point were compared by
independent-samples t-test. P-value <0.05 was considered to be
statistically significant.
Results
Comparison of general clinical
baseline data of the two groups
Basic conditions of group A and B, such as age, sex,
hypertension, hyperlipidemia, diabetes, and personal habits
(smoking and drinking), were compared, and had significant
differences (P>0.05) (Table
I).
Comparison of the expression levels of
serum-related cytokines before and after treatment between groups A
and B
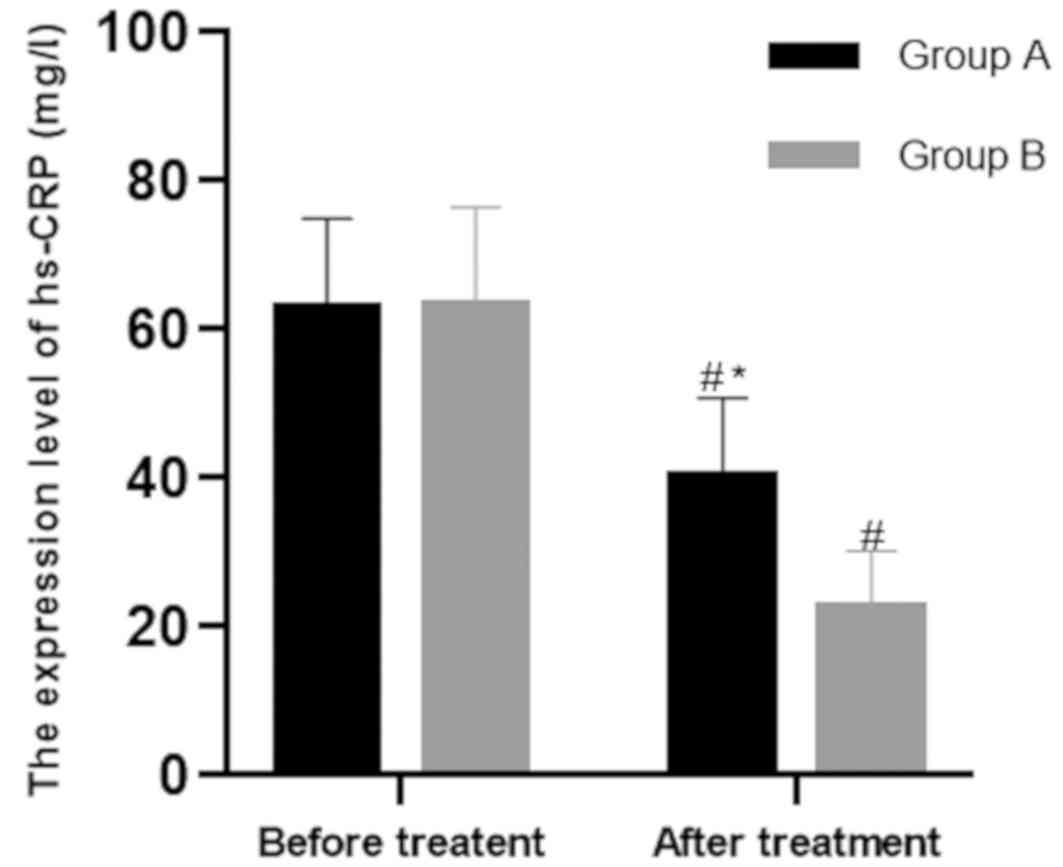
i) Before treatment, the hs-CRP level of patients in
group A was 62.89±12.05 mg/l, while that of patients in group B was
63.27±13.20 mg/l. There was no significant difference in hs-CRP
level between the two groups before treatment (P>0.05). The
post-treatment levels of the two groups were 40.39±10.37 mg/l and
22.59±7.65 mg/l, respectively, with significant difference
(P<0.001). Comparing the levels of groups A and B after
treatment, it was concluded that those of group B were
significantly lower than those of group A after treatment
(P<0.001) (Fig. 1).
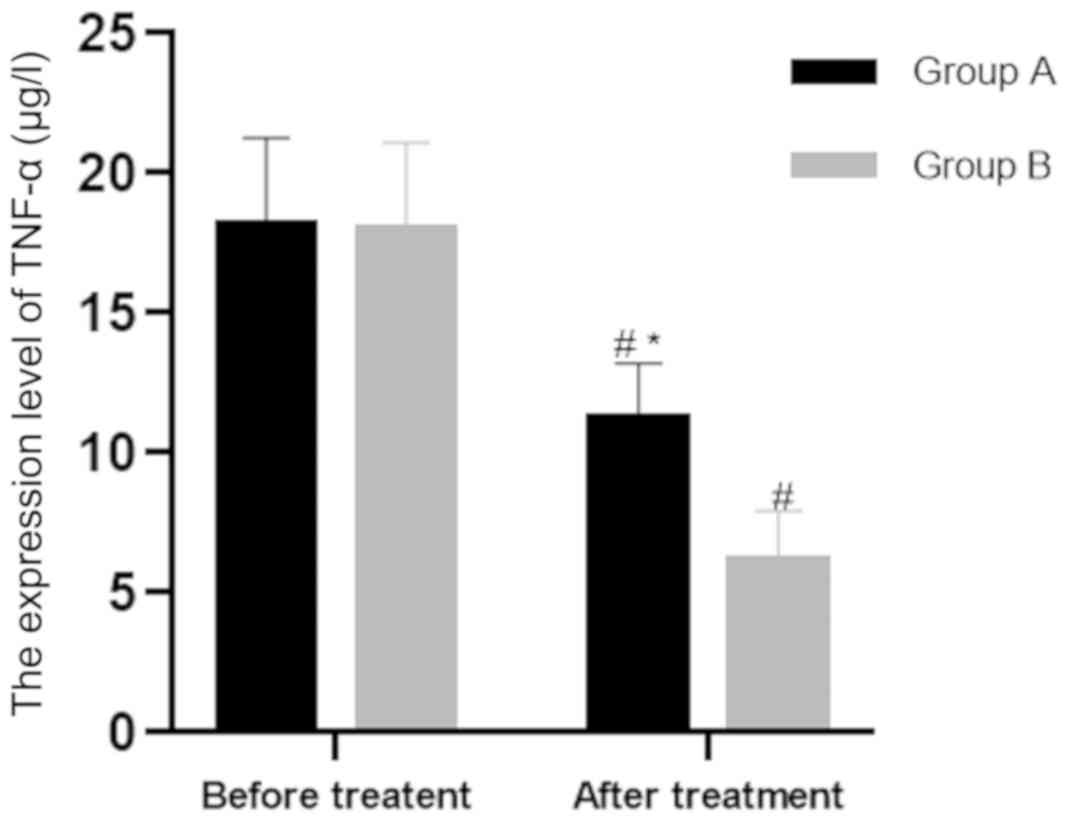
ii) Before treatment, the TNF-α level of patients in
group A was 18.14±3.13 μg/l, while that of patients in group
B was 18.01±3.09 μg/l. There was no significant difference
in hs-CRP level between the two groups before treatment
(P>0.05). The post-treatment levels of the two groups were
11.19±2.01 μg/l and 6.13±1.79 μg/l respectively
(P<0.001). Comparing the levels of groups A and B after
treatment, it was concluded that group B was significantly lower
than group A (P<0.001) (Fig.
2).
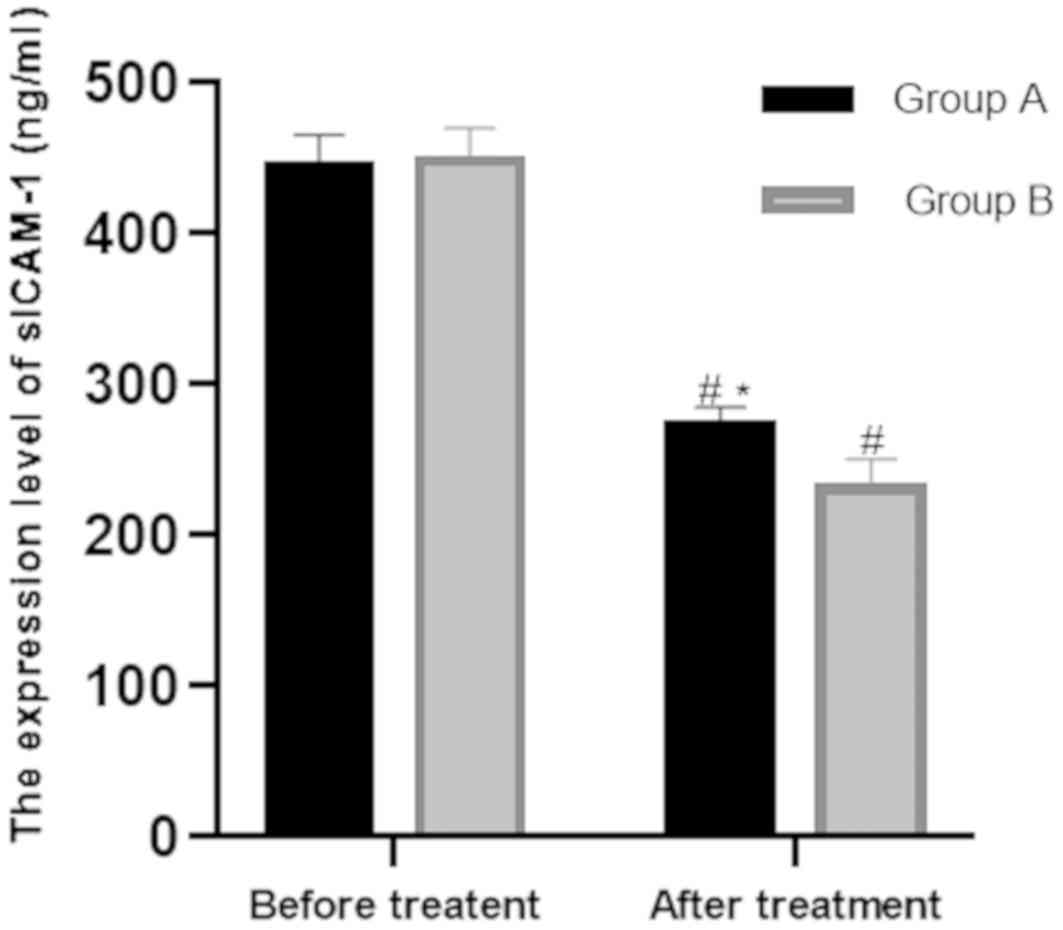
iii) Before treatment, the level of serum-related
cytokine sICAM-1 in group A was 444.74±20.78 ng/ml, while that in
group B was 448.31±22.01 ng/ml. There was no significant difference
in hs-CRP levels between the two groups before treatment
(P>0.05). The post-treatment levels of the two groups were
272.77±12.48 ng/ml and 230.59±20.03 ng/ml respectively, with
significant difference (P<0.001). Comparing the levels of groups
A and B after treatment, it was concluded that those of group B
were significantly lower than those of group A (P<0.001)
(Fig. 3).
Comparison of NIHSS scores of patients
in the two groups
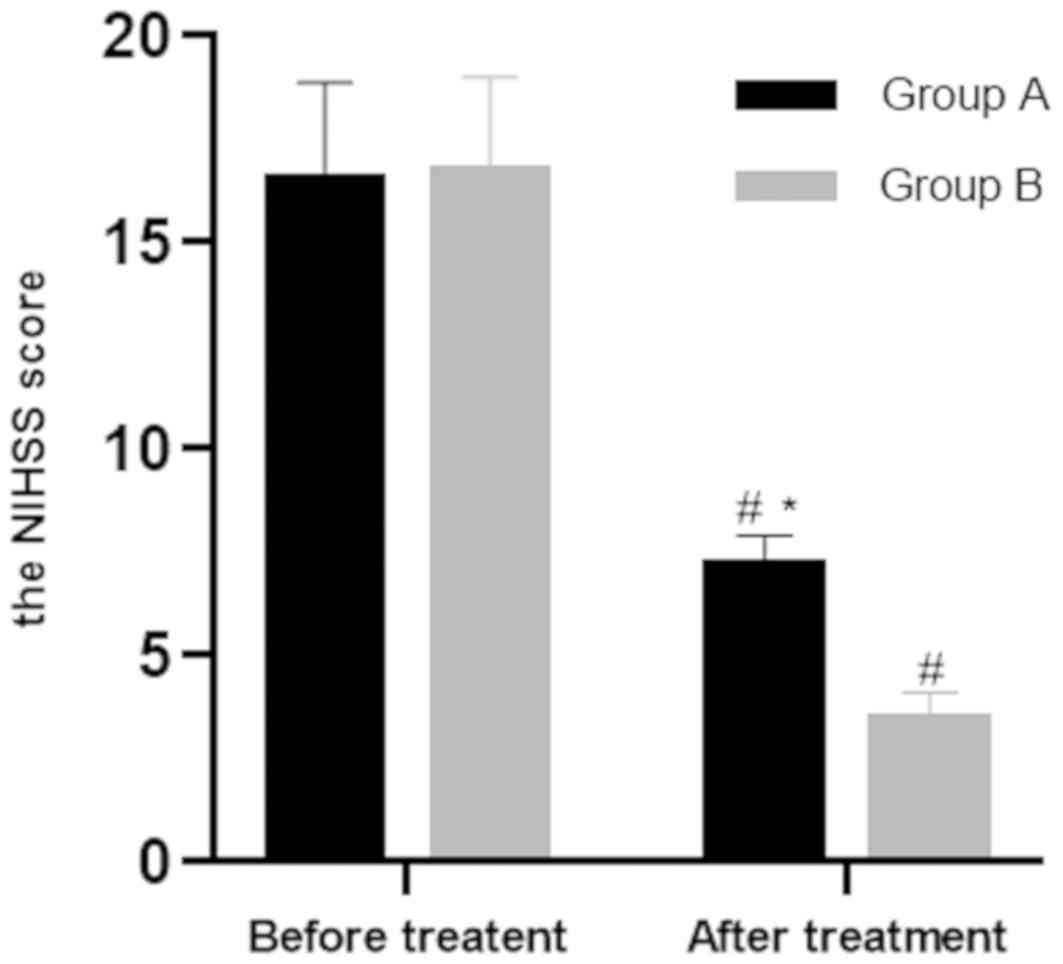
Before treatment, the NIHSS score of patients in
group A was 16.54±2.33, while that in group B was 16.72±2.29. There
was no significant difference between the two groups before
treatment (P>0.05). The post-treatment scores of the two groups
were 7.18±0.72 and 3.43±0.67, respectively, with significant
difference (P<0.001). NIHSS after treatment in group B was
significantly lower than that in group A (P<0.001) (Fig. 4).
Comparison of the clinical efficacy of
patients in the two groups
Clinical efficacy of patients in the two groups were
compared. In group A, there were 6 cases of basic rehabilitation,
15 cases of markedly effective, 10 cases of effective, 9 cases
without change, and no deterioration or death; its total effective
rate was 77.5%. In group B, there were 9 cases of basic
rehabilitation, 20 cases of markedly effective, 19 cases effective,
2 cases without change, and no deterioration or death; its total
effective rate was 96%. The total effective rate of group B was
significantly higher than that of group A, and the difference was
significant (P<0.05) (Table
II).
 | Table II.Comparison of total effective rate of
clinical efficacy of patients between the two groups [n(%)]. |
Table II.
Comparison of total effective rate of
clinical efficacy of patients between the two groups [n(%)].
| Variables | Group A (n=40) | Group B (n=50) | χ2 | P-value |
|---|
| Basic
rehabilitation | 6 (15.00) | 9 (18.00) | – | – |
| Markedly
effective | 15 (37.50) | 20 (40.00) | – | – |
| Effective | 10 (25.00) | 19 (38.00) | – | – |
| No change | 9 (22.50) | 2 (4.00) | – | – |
| Deterioration | 0 (0.00) | 0 (0.00) | – | – |
| Death | 0 (0.00) | 0 (0.00) | – | – |
| Total effective
rate (%) | 77.50 | 96.00 | 7.089 | 0.0078 |
Comparison of adverse reactions of
patients between the two groups
We observed the adverse reactions of
gastrointestinal hemorrhage, malignant vomiting, allergy and
arrhythmia. In group A, there were 3 cases of gastrointestinal
hemorrhage, 6 cases of malignant vomiting, 3 cases of allergy and 7
cases of arrhythmia, totaling 19 cases (47.5%). In group B, there
was 1 case of gastrointestinal hemorrhage, 1 case of malignant
vomiting, 2 cases of allergy and 2 cases of arrhythmia, totaling 6
cases (12%). The incidence of adverse reactions in group B was
significantly lower than that in group A, and the difference was
significant (P<0.05) (Table
III).
 | Table III.Comparison of adverse reactions of
patients between the two groups [n(%)]. |
Table III.
Comparison of adverse reactions of
patients between the two groups [n(%)].
| Variables | Group A (n=40) | Group B (n=50) | χ2 | P-value |
|---|
| Gastrointestinal
hemorrhage | 3 (7.50) | 1 (2.00) | – | – |
| Malignant
vomiting | 6 (15.00) | 1 (2.00) | – | – |
| Allergy | 3 (7.50) | 2 (4.00) | – | – |
| Arrhythmia | 7 (17.50) | 2 (4.00) | – | – |
| Total | 19 (47.50) | 6 (12.00) | 13.960 | 0.0002 |
Discussion
How to treat cerebral infarction more effectively is
an important research issue. Thrombolysis (15) and antiplatelet therapy (16) are both effective methods to treat
cerebral infarction. Its treatment with aspirin and clopidogrel is
one of the commonly used methods. As a predictive diagnostic index
for cerebral infarction (17), the
expression level of relevant cytokines is upregulated in the brain
after stroke, and the brain plug area is enlarged by infiltrating
ischemic areas (18). The purpose of
this study was to investigate the expression level and efficacy of
common serum factors such as hs-CR, TNF-α (19), and sICAM-1 (20) under the influence of aspirin and
clopidogrel in cerebral infarction.
In this study, we compared the differences in the
expression levels of hs-CRP, sICAM-1 and TNF-α between groups A
(aspirin only) and B (both drugs). After data analysis, we found
that the expression levels of hs-CRP, sICAM-1 and TNF-α of patients
in the two groups decreased compared with those before treatment.
The decline in group B was significantly higher than that of group
A, and there were significant differences in statistics. Therefore,
we believed that combined therapy could reduce the expression
levels of hs-CRP, sICAM-1 and TNF-α more rapidy. In the study of Yu
et al (21) clinical
treatment of myocardial infarction, the levels of hs-CRP, TNF-α and
other related cytokines after aspirin combined with clopidogrel
were significantly lower than aspirin alone. In a study on the
treatment of acute coronary syndrome with aspirin and clopidogrel,
the expression level of hs-CRP and TNF-α decreased more obviously
after aspirin and clopidogrel were treated together than aspirin
alone (22). However, the study of
Yin (23) on unstable angina
pectoris, comparing the two experimental groups, a group with
aspirin alone and a group with aspirin combined with clopidogrel,
it was found that the level of serum factor sICAM-1 in the latter
group decreased more significantly after one week of treatment
compared with the former. These results were similar to the results
in the present study, and proved that aspirin combined with
clopidogrel was more effective in reducing the expression levels of
hs-CRP, sICAM-1 and TNF-α.
Our study also compared the total effective rate of
clinical efficacy and adverse reactions of the two groups. It was
discovered that the total effective rate of combined treatment of
the two drugs was significantly higher than that of aspirin alone,
with fewer adverse reactions. Therefore, we concluded that the
efficacy and safety of aspirin combined with clopidogrel were
better than aspirin alone. In the study of Wong et al
(24) on stroke patients,
clopidogrel combined with aspirin was more effective in reducing
microembolization signals than aspirin alone. As to prevention of
stroke or transient cerebral ischemia, Zhang et al (25) reported that compared with
monotherapy, short-term aspirin combined with clopidogrel had a
higher secondary prevention effect on prevention of stroke or
transient cerebral ischemia without increasing the risk of
hemorrhagic stroke and major hemorrhagic events, which was similar
to our results.
In summary, the experimental results proved that the
combined use of aspirin and clopidogrel had a stronger inhibitory
effect on the expression levels of serum-related cytokines hs-CRP,
TNF-α and sICAM-1 than aspirin alone, and reduced the expression
levels of these factors, and achieved better results in clinical
practice.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ML wrote the manuscript, interpreted and analyzed
the data. JW and XW designed the study and performed the
experiments. GL was responsible for the analysis and discussion of
the data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Yidu Central Hospital of Weifang (Weifang, China). Patients who
participated in this research had complete clinical data. Signed
informed consents were obtained from the patients and/or the
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Heit JJ, Ball RL, Telischak NA, Do HM,
Dodd RL, Steinberg GK, Chang SD, Wintermark M and Marks MP: Patient
outcomes and cerebral infarction after ruptured anterior
communicating artery aneurysm treatment. AJNR Am J Neuroradiol.
38:2119–2125. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Guo A, Hao F, Li F, Wang B, Liu L, Zhao Z
and Yao C: Basal ganglia cerebral infarction patient fMRI imaging
analysis before and after acupuncture-medicine therapy. Biomed Res
(Aligarh). 28:9779–9783. 2017.
|
|
3
|
Tan XL, Xue YQ, Ma T, Wang X, Li JJ, Lan
L, Malik KU, McDonald MP, Dopico AM and Liao FF: Partial eNOS
deficiency causes spontaneous thrombotic cerebral infarction,
amyloid angiopathy and cognitive impairment. Mol Neurodegener.
10:242015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shankaran S, McDonald SA, Laptook AR,
Hintz SR, Barnes PD, Das A, Pappas A and Higgins RD; Eunice Kennedy
Shriver National Institute of Child Health and Human Development
Neonatal Research Network, : Neonatal magnetic resonance imaging
pattern of brain injury as a biomarker of childhood outcomes
following a trial of hypothermia for neonatal hypoxic-ischemic
encephalopathy. J Pediatr. 167:987–993. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kitagawa K, Hosomi N, Nagai Y, Ohtsuki T,
Kagimura T, Minematsu K, Uchiyama S and Matsumoto M: HS-CRP level
is an independent predictor for recurrent stroke and vascular
events in patients with non-cardiogenic brain infarction. J Neurol
Sci. 381:869–870. 2017. View Article : Google Scholar
|
|
6
|
Pantović-Stefanović M, Petronijević N,
Dunjić-Kostić B, Velimirović M, Nikolić T, Jurišić V, Lačković M,
Damjanović A, Totić-Poznanović S, Jovanović AA and Ivković M:
sVCAM-1, sICAM-1, TNF-α and IL-6 levels in bipolar disorder type I:
Acute, longitudinal and therapeutic implications. World J Biol
Psychiatry. 19:S41–S51. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vila N, Castillo J, Dávalos A and Chamorro
A: Proinflammatory cytokines and early neurological worsening in
ischemic stroke. Stroke. 31:2325–2329. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wang JH, Chen Q and Wang DL: Clinical
efficacy of edaravone in combined with gangliosides in the
treatment of acute cerebral infarction in elderly patients and the
effect on inflammatory cytokines. Zhongguo Yiyuan Ganranxue Zazhi.
25:2179–2181. 2015.(In Chinese).
|
|
9
|
Liu ZJ, Yang QD, Liu YH, Huang XS and
Zhang N: Changes and clinical significance of serum IL-6, sICAM-1
in patients with cerebral infarcts. Zhong Nan Da Xue Xue Bao Yi Xue
Ban. 29:326–329. 2004.(In Chinese). PubMed/NCBI
|
|
10
|
Ridker PM, Hennekens CH, Roitman-Johnson
B, Stampfer MJ and Allen J: Plasma concentration of soluble
intercellular adhesion molecule 1 and risks of future myocardial
infarction in apparently healthy men. Lancet. 351:88–92. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu MC, Li FP, Han YL and Chen HS:
Argatroban versus aspirin plus clopidogrel in the treatment of
acute ischemic stroke: A pilot, randomised, open-label study. Med J
Chin People's Liberation Army. 40:433–439. 2015.
|
|
12
|
CAPRIE Steering Committee, . A randomised,
blinded, trial of clopidogrel versus aspirin in patients at risk of
ischaemic events (CAPRIE). Lancet. 348:1329–1339. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Naess H, Kurtz M, Thomassen L and
Waje-Andreassen U: Serial NIHSS scores in patients with acute
cerebral infarction. Acta Neurol Scand. 133:415–420. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang X, Chen J, Ding M and Zhang N:
Aspirin plus clopidogrel for angina pectoris in coronary heart
disease patients. Int J Clin Exp Med. 11:13528–13534. 2018.
|
|
15
|
Wardlaw JM, Murray V, Berge E, del Zoppo
G, Sandercock P, Lindley RL and Cohen G: Recombinant tissue
plasminogen activator for acute ischaemic stroke: An updated
systematic review and meta-analysis. Lancet. 379:2364–2372. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chen ZM, Sandercock P, Pan HC, Counsell C,
Collins R, Liu LS, Xie JX, Warlow C and Peto R: Indications for
early aspirin use in acute ischemic stroke: A combined analysis of
40,000 randomized patients from the Chinese acute stroke trial and
the international stroke trial. On behalf of the CAST and IST
collaborative groups. Stroke. 31:1240–1249. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tuttolomondo A, Di Raimondo D, di Sciacca
R, Pinto A and Licata G: Inflammatory cytokines in acute ischemic
stroke. Curr Pharm Des. 14:3574–3589. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhou Z, Zhang J, Li X, Xia C, Han Y and
Chen H: Protein microarray analysis identifies key cytokines
associated with malignant middle cerebral artery infarction. Brain
Behav. 7:e007462017. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang SQ, Fan H, Deng LJ and Wu D: Effects
of Atorvastatin calcium combined with aspirin on serum levels of
Hcy, NSE, UA, hs-CRP and inflammatory factors of patients with
cerebral infarction. J Hainan Med Univ. 23:157–160. 2017.
|
|
20
|
Klein BR, Brown EN and Casden RS:
Preoperative macular spectral-domain optical coherence tomography
in patients considering advanced-technology intraocular lenses for
cataract surgery. J Cataract Refract Surg. 42:537–541. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yu HR, Wei YY, Ma JG and Geng XY:
Beneficial effects of combined administration of clopidogrel and
aspirin on the levels of proinflammatory cytokines, cardiac
function, and prognosis in ST-segment elevation myocardial
infarction: A comparative study. Medicine (Baltimore).
97:e130102018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chen YG, Xu F, Zhang Y, Ji QS, Sun Y, Lü
RJ and Li RJ: Effect of aspirin plus clopidogrel on inflammatory
markers in patients with non-ST-segment elevation acute coronary
syndrome. Chin Med J (Engl). 119:32–36. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yin G: The effect of cilostazol on serum
level of sICAM-1, sVCAM-1 and MMP-9 in patients with unstable
angina. Acta Academiae Medicinae Qingdao Universitatis. 6:532–534.
2007.
|
|
24
|
Wong KS, Chen C, Fu J, Chang HM, Suwanwela
NC, Huang YN, Han Z, Tan KS, Ratanakorn D, Chollate P, et al CLAIR
study investigators, : Clopidogrel plus aspirin versus aspirin
alone for reducing embolisation in patients with acute symptomatic
cerebral or carotid artery stenosis (CLAIR study): A randomised,
open-label, blinded-endpoint trial. Lancet Neurol. 9:489–497. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhang Q, Wang C, Zheng M, Li Y, Li J,
Zhang L, Shang X and Yan C: Aspirin plus clopidogrel as secondary
prevention after stroke or transient ischemic attack: A systematic
review and meta-analysis. Cerebrovasc Dis. 39:13–22. 2015.
View Article : Google Scholar : PubMed/NCBI
|