Introduction
Paraquat is a type of bipyridine compound that is
widely used as a herbicide (1).
Self-poisoning with pesticides is a major public health problem in
developing countries (2). As a
result of its widespread use, paraquat is regarded as the main
herbicide involved in accidental and intentional poisoning
(3). Paraquat poisoning can be fatal
after ingestion, and its mortality rate is 80% after confirmed
exposure (4,5). Multiple organ dysfunction syndrome
(MODS) is the main cause of mortality induced by paraquat poisoning
(6).
MODS occurs in patients with severe infection or
trauma, triggering the release of inflammatory mediators (7). The dysregulation of the inflammatory
response plays a crucial role in the development of MODS (8,9).
Anti-inflammatory treatment is the primary therapy for the early
treatment of paraquat poisoning (5).
A number of genes that are differentially expressed during the
occurrence and development of inflammation are candidate targets
for gene therapy, including some microRNAs (miRNAs/miRs) (10). A recent study reported that miR-146a
can regulate the occurrence and immune response of lung injury
induced by paraquat poisoning, and that interleukin (IL)-6 is
involved in the regulation of this process (11).
IL-10 is a pluripotent anti-inflammatory cytokine
that plays a crucial role in the immune response (12). He et al (13) reported that IL-10 mRNA expression
levels are increased in rats treated with paraquat, suggesting a
crucial role of IL-10 in lung injury of poisoned rats. In a
previous study investigating sucralfate intervention for paraquat
poisoning, IL-10 was shown to be decreased by sucralfate treatment
in rats treated with paraquat, and both lung and kidney injuries of
the rats were improved (14). The
role of miRNAs in regulating IL-10 has been widely studied
(15,16). A previous study showed the protective
mechanism of miR-98 in hepatocellular carcinoma (HCC) and IL-10 was
found to be the target gene of miR-98, therefore miR-98 may
suppress the progression of HCC by targeting IL-10 (14). Additionally, miR-27b-3p and
miR-340-5p were reported to target the 3′untranslated regions
(3′UTR) of IL-10 (17). Transfection
and transduction assays showed that upregulation of miR-27b-3p and
miR-340-5p downregulated IL-10 expression levels (17). Xie et al (18) reported that miR-27a can regulate the
inflammatory response of macrophages by targeting IL-10, and the
downregulation of miR-27a was considered to be part of a
negative-regulatory mechanism to prevent the inflammatory response.
In the present study, to investigate the regulatory mechanism of
IL-10, the potential miRNA factors regulating IL-10 were predicted
using bioinformatics prediction software and databases including
miRanda, TargetScan, PiTa, RNAhybrid and PicTar. The present
bioinformatic results suggested that miR-27a was a potential
regulator for IL-10. The present results suggested that miR-27a may
play a role in MODS induced by paraquat poisoning via the
regulation of IL-10.
In the present study, the serum expression levels of
miR-27a and IL-10 in patients with paraquat poisoning induced MODS
were measured and the clinical significance of miR-27a was
investigated.
Materials and methods
Patients and sample collection
A total of 82 patients with MODS induced by acute
paraquat poisoning were enrolled and were diagnosed according to
the diagnostic criteria reported by Fry (19). Patients were admitted to the
Emergency Department of The Affiliated Hospital of Weifang Medical
University from June 2011 to December 2016. All patients arrived at
the hospital within 24 h after poisoning; the poison was ingested
orally with an estimated volume of 10–80 ml. In total, 10–15 ml
venous blood was collected from all patients on admission to
hospital, and the serum was isolated and stored at −80°C for
further analysis. The patients (age, 17–52 years; mean age,
30.52±6.93; 40 males and 42 females) did not suffer from immune or
immune-related diseases such as diabetes, tumors, chronic liver
disease, chronic kidney disease and connective tissue disease. All
patients were treated based on a standard treatment protocol
including gastric lavage, catharsis, hemoperfusion, antioxidants,
high-dose intravenous methylprednisolone and cyclophosphamide
(20). A further 88 (age, 18–49
years; mean age, 31.31±7.47; 41 males and 47 females) venous blood
samples (5 ml) were collected from healthy fasting participants who
had healthy examination results at the same hospital, and were used
as the control group. The present study was designed under the
review and approval of The Ethics Committee of The Affiliated
Hospital of Weifang Medical University. Written informed consent
was collected from each participant.
Data collection
All data were recorded in a standard collection for
each patient within 24 h of admission, and included: i) Demographic
parameters such as age and gender; ii) time interval from paraquat
ingestion to admittance in the emergency department; iii) estimated
ingestion amount of paraquat; iv) blood biochemical indexes
including white blood count (WBC), blood urea nitrogen (BUN),
alanine transaminase (ALT) and aspartate transaminase (AST); and v)
arterial partial pressure of carbon dioxide (PaCO2) and
blood lactic acid (Lac), PaCO2 and Lac were measured
using i-STAT blood gas analyzer (Abbott Laboratories).
RNA extraction and reverse
transcription-quantitative PCR (RT-qPCR)
Total RNA was extracted from serum samples using
TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc.)
according to the manufacturer's protocol. Reverse transcription was
performed using a miScript RT kit (Qiagen GmbH), and the conditions
were 37°C for 15 min and 98°C for 5 min. SYBR green I Master Mix
kit (Invitrogen; Thermo Fisher Scientific, Inc.) was used for
RT-qPCR to investigate miR-27a expression levels. The following
thermocycling conditions were used for the PCR: Initial
denaturation at 95°C for 5 min; 30 cycles of 95°C for 30 sec, 60°C
for 30 sec and 72°C for 20 sec; and a final extension at 72°C for
10 min. U6 was used as an internal reference for data normalization
of miR-27a expression levels. The relative expression levels of
miR-27a were determined in relation to U6 using the
2−ΔΔCq method (21). The
primers used were as follows: miR-27a forward,
5′-GGGTTCACAGTGGCTA-3′ and reverse, 5′-CTCAACTGGTGTCGTGGA-3′; and
U6 forward, 5′-CTCGCTTCGGCAGCACA-3′ and reverse,
5′-AACGCTTCACGAATTTGCGT-3′.
Bioinformatics analysis
To investigate the regulatory mechanism of IL-10,
the potential miRNA factors regulating IL-10 were predicted using
bioinformatics prediction software, miRanda (http://www.microrna.org/microrna/home.do; date of
access: August 2010; Memorial Sloan-Kettering Cancer Center),
TargetScan (www.targetscan.org/vert_71/; version 7.1), PiTa
(http://genie.weizmann.ac.il/pubs/mir07/mir07_data.html;
version 6; Weizmann Institute of Science), RNAhybrid (http://bibiserv.techfak.uni-bielefeld.de/rnahybrid/;
accessed September 2017; Bielefeld BioInformatics Service) and
PicTar (http://pictar.mdc-berlin.de/;
accessed March, 2007). miRanda was used according to the following
parameters: Energy value ≤-14 kcal/mol, score ≥80 (22). TargetScan, predictions were ranked
according to the predictive efficacy of the target, using context++
scores of the binding sites (23).
PiTa was implemented using high-stringency parameters of 7–8 mers
and setting the energy value ≤-10 kcal/mol as a general cut-off
value (24). RNAhybrid was performed
setting the energy value ≤-20 kcal/mol (25). Prediction using PicTar was based on
the PicTar score and free energy (26). The bioinformatics results suggested
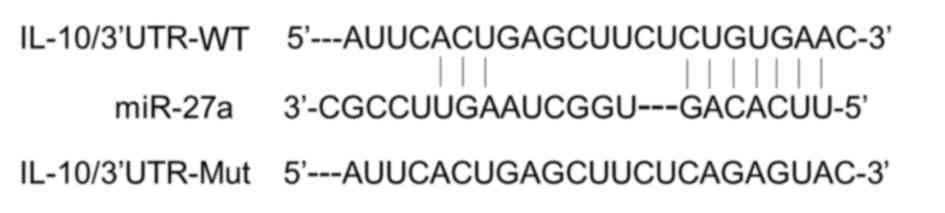
that miR-27a was a potential regulator for IL-10 (Fig. 1).
ELISA for IL-10
Serum expression level of IL-10 was measured by
ELISA using IBL IL-10 ELISA kit (cat. no. 30147233; IBL
International GmBH) according to the manufacturer's instructions.
The concentration of IL-10 was calculated based on standard curves
provided with the kits and results are presented in ng/l.
Statistical analysis
Data are presented as the mean ± SD. The measurement
data was analyzed using Student's t test and the categorical data
were compared using Chi-squared test. The correlation between IL-10
and miR-27a expression levels was assessed using Spearman's
correlation coefficient. A receiver operating characteristic (ROC)
curve was used to calculate the specificity and sensitivity of
miR-27a expression level, and to assess its feasibility to diagnose
MODS induced by paraquat poisoning. Multivariate Cox regression
analyses was performed to examine the association between miR-27a
expression level and mortality rate. All data analysis was
conducted using GraphPad Prism 5.0 software (GraphPad Software,
Inc.) and SPSS version 18.0 software (SPSS, Inc.) P<0.05 was
considered to indicate a statistically significant difference.
Results
Expression level of miR-27a in
patients with paraquat poisoning-induced MODS
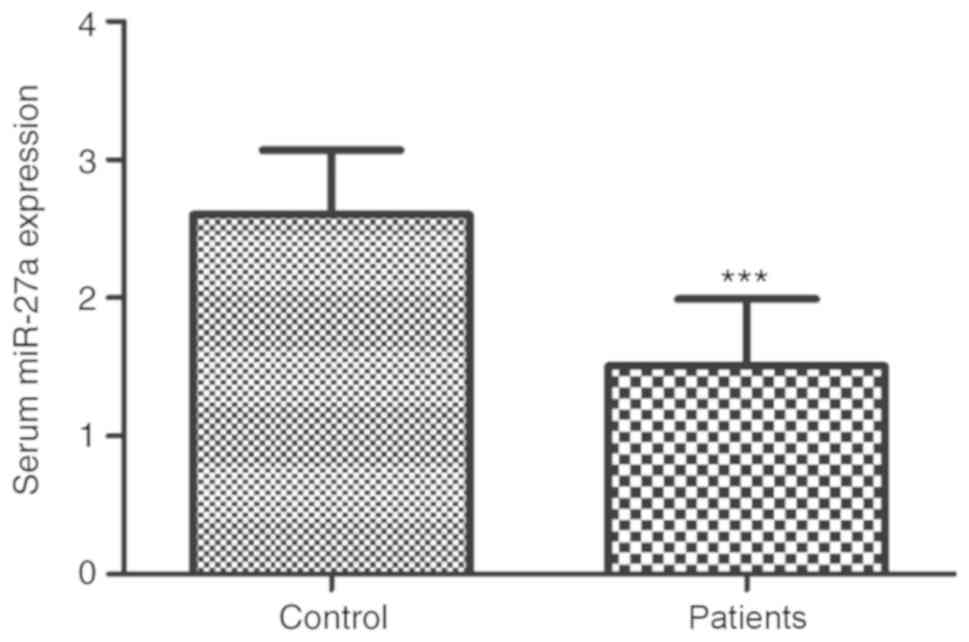
The serum miR-27a expression levels in all
participants were measured using RT-qPCR. The present results
suggested that the serum miR-27a expression level was significantly
decreased in patients with MODS compared with the healthy controls
(Fig. 2; P<0.001).
Association of miR-27a expression
level with the clinicopathological characteristics of patients with
MODS induced by paraquat poisoning
To investigate the clinical role of miR-27a, the
correlation between miR-27a expression level and the
clinicopathological characteristics of all patients was
investigated. All patients were classified into low expression
group (n=47) and high expression group (n=35) based on the mean
value of serum miR-27a expression level (Table I). The present results suggested that
miR-27a expression level was closely associated with BUN (P=0.029),
PaCO2 (P=0.024), Lac (P=0.012) and APACHE II (27) (P=0.001). However, other
clinicopathological parameters showed no significant association
with miR-27a expression level including sex, age, time to hospital,
estimated amount of paraquat, WBC, BUN, ALT and AST (Table I).
 | Table I.Association of miR-27a with the
clinicopathological characteristics of patients with multiple organ
dysfunction syndrome induced by paraquat poisoning. |
Table I.
Association of miR-27a with the
clinicopathological characteristics of patients with multiple organ
dysfunction syndrome induced by paraquat poisoning.
| Variable | Low miR-27a
expression (n=47) | High miR-27a
expression (n=35) | P-value |
|---|
| Sex |
|
| 0.632 |
|
Male | 24 | 16 |
|
|
Female | 23 | 19 |
|
| Age, years | 29.45±6.98 | 31.97±6.68 | 0.103 |
| Time elapsed before
admission to hospital, h | 11.04±4.88 | 11.11±5.31 | 0.950 |
| Estimated volume
paraquat ingested, ml | 37.43±17.81 | 34.77±19.35 | 0.522 |
| WBC | 15.45±1.55 | 15.39±1.19 | 0.834 |
| BUN | 12.03±1.80 | 11.24±1.28 | 0.029 |
| ALT | 152.45±21.08 | 150.57±26.26 | 0.721 |
| AST | 143.83±21.13 | 137.94±16.97 | 0.166 |
|
PaCO2 | 26.59±2.64 | 27.99±2.87 | 0.024 |
| Lac | 2.72±0.54 | 2.41±0.55 | 0.012 |
| APACHE II | 9.98±2.34 | 8.13±2.21 | 0.001 |
ROC analysis of the diagnostic value
of serum miR-27a expression level for MODS induced by paraquat
poisoning
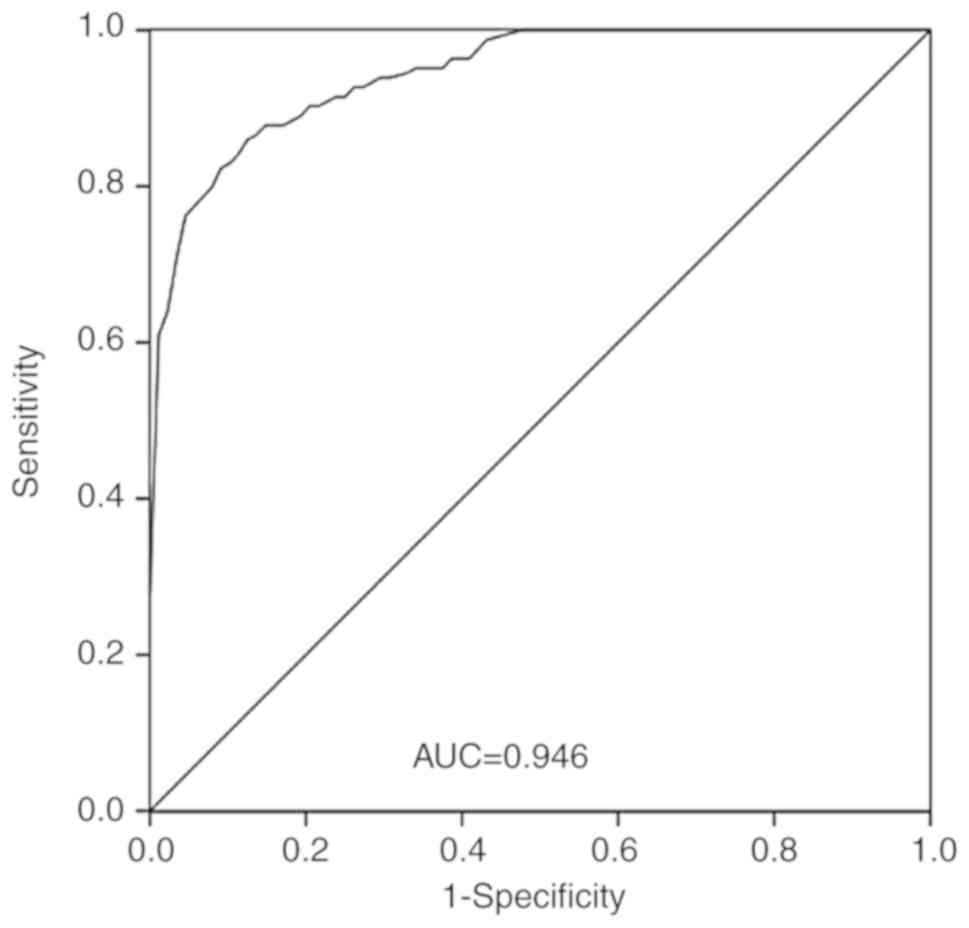
A ROC curve is a graphical representation that
reflects the correlation between sensitivity and specificity of a
laboratory test (28). Based on the
serum miR-27a expression levels in patients and controls groups in
the present study, a ROC curve was generated to assess the
diagnostic value of serum miR-27a expression level for MODS induced
by paraquat poisoning. The area under the curve for miR-27a was
0.946, with a sensitivity of 86.6% and specificity of 87.5% at the
cutoff value of 2.10 (Fig. 3).
Association of serum miR-27a
expression level with mortality rate
All 82 patients with MODS induced by paraquat
poisoning were divided into survival group (n=28) and non-survival
group (n=54) based on their status after 30 days from admission.
The non-survival group had significantly higher levels of WBC, BUN,
ALT, AST and Lac, and lower levels of PaCO2 compared
with the survival group (Table II;
P<0.001). Additionally, the comparison of traditional score
between the survival and non-survival groups showed that
non-survivors had a significantly higher APACHE II score
(P<0.001). Moreover, miR-27a expression level was significantly
different between the survival and non-survival group (P<0.01),
with the non-survival group having more patients with low miR-27a
expression levels.
 | Table II.Comparisons between survivors and
non-survivors of patients with multiple organ dysfunction syndrome
induced by paraquat poisoning. |
Table II.
Comparisons between survivors and
non-survivors of patients with multiple organ dysfunction syndrome
induced by paraquat poisoning.
| Variable | Survivors
(n=28) | Non-survivors
(n=54) | P-value |
|---|
| miR-27a |
|
| 0.004 |
| Low
expression | 10 | 37 |
|
| High
expression | 18 | 17 |
|
| Sex |
|
| 0.759 |
|
Male | 13 | 27 |
|
|
Female | 15 | 27 |
|
| Age, years | 32.00±7.36 | 29.76±6.63 | 0.166 |
| Time elapsed before
admission to hospital, h | 11.46±4.73 | 10.87±5.21 | 0.615 |
| Estimated volume
paraquat ingested, ml | 34.21±17.16 | 37.37±19.10 | 0.465 |
| WBC | 14.55±1.35 | 15.88±1.20 | <0.001 |
| BUN | 10.58±0.89 | 12.27±1.64 | <0.001 |
| ALT | 132.93±24.45 | 161.35±15.62 | <0.001 |
| AST | 129.18±18.25 | 147.61±17.25 | <0.001 |
|
PaCO2 | 29.13±3.03 | 26.18±2.09 | <0.001 |
| Lac | 2.01±0.32 | 2.89±0.40 | <0.001 |
| APACHE II | 7.34±2.20 | 10.14±2.00 | <0.001 |
Furthermore, multivariate Cox regression analyses
was performed to examine the association between miR-27a expression
level and mortality rate. The present results suggested that
miR-27a expression level and APACHE II score may be independent
prognostic factors to determine overall survival rates (Table III; P<0.01).
 | Table III.Multivariate Cox regression analysis
for miR-27a in patients with multiple organ dysfunction syndrome
induced by paraquat poisoning. |
Table III.
Multivariate Cox regression analysis
for miR-27a in patients with multiple organ dysfunction syndrome
induced by paraquat poisoning.
|
| Multivariate
analysis |
|---|
|
|
|
|---|
| Variable | HR | 95% CI | P-value |
|---|
| miR-27a | 7.156 | 3.329–15.384 | <0.001 |
| Age | 0.922 | 0.496–1.713 | 0.797 |
| Sex | 0.620 | 0.320–1.201 | 0.157 |
| Time elapsed before
admission to hospital, h | 1.059 | 0.560–2.004 | 0.859 |
| Estimated volume
paraquat ingested, ml | 1.099 | 0.594–2.034 | 0.763 |
| WBC | 1.297 | 0.707–2.381 | 0.401 |
| BUN | 1.292 | 0.670–2.489 | 0.444 |
| ALT | 1.209 | 0.602–2.429 | 0.595 |
| AST | 1.385 | 0.713–2.689 | 0.336 |
|
PaCO2 | 0.624 | 0.199–1.956 | 0.418 |
| Lac | 1.707 | 0.568–5.125 | 0.341 |
| APACHE II | 2.730 | 1.282–5.810 | 0.009 |
miR-27a expression level is negatively
correlated with IL-10 expression level
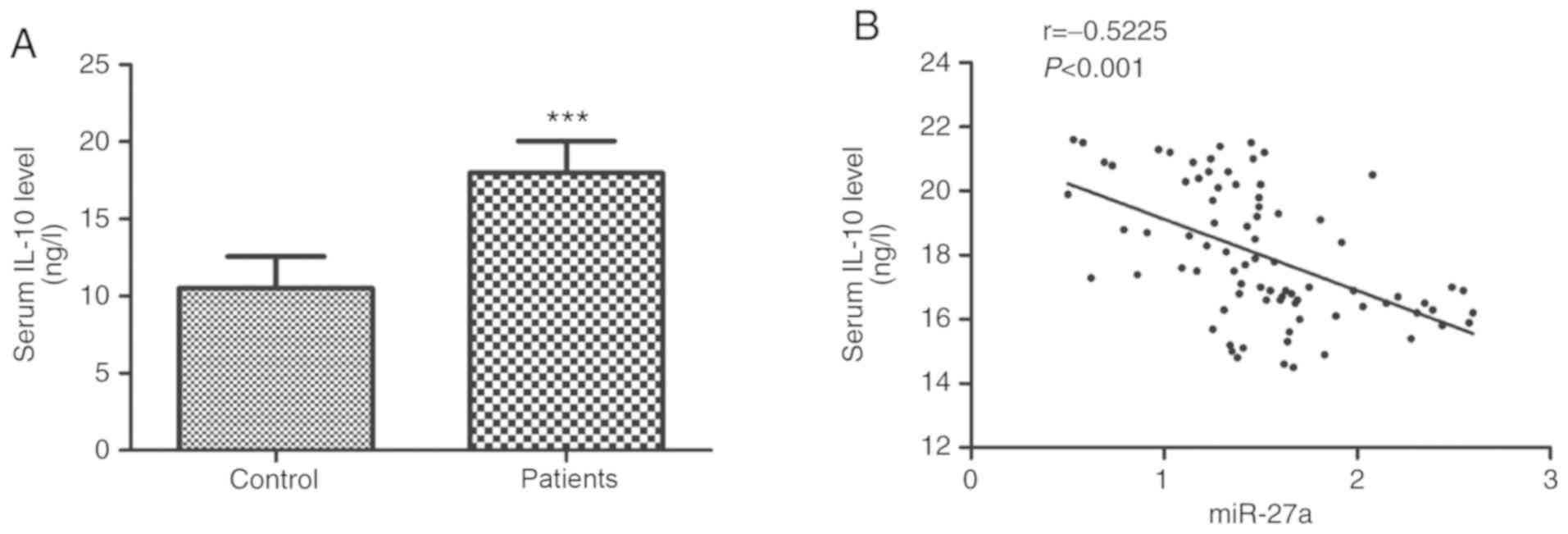
The bioinformatic results suggested that miR-27a was
a potential regulator for IL-10 (Fig.
1). We further investigated the correlation of serum expression
levels of miR-27a with IL-10. ELISA was used for the measurement of
the serum IL-10 expression levels. The present results suggested
that the serum IL-10 expression level was significantly higher in
patients with MODS compared with the healthy controls (Fig. 4A; P<0.001).
The present study also investigated the correlation
between serum expression levels of miR-27a and IL-10 in patients
with MODS. The present results identified a moderately negative
correlation between the serum expressions level of miR-27a and
IL-10 (Fig. 4B; r=−0.5225;
P<0.001).
Discussion
Paraquat is a widely used herbicide and has a
variety of toxic effects (29). The
mechanism of acute paraquat poisoning is complex, with many
inflammatory factors and cytokines involved (30). Acute paraquat poisoning can lead to a
strong inflammatory reaction (31).
Previous studies reported that IL-10 mRNA expression level was
increased in paraquat poisoned rats, IL-10 level was decreased by
sucralfate treatment and the lung and kidney injuries of the rats
were also improved (13,14). Therefore, these previous studies
demonstrated the important role of IL-10 in paraquat poisoning.
IL-10 inhibits the activity of monocyte macrophages, T cells and
natural killer cells (32). IL-10
also inhibits the synthesis and release of other inflammatory
cytokines including IL-1β, tumor necrosis factor-α (TNF-α) and IL-8
(32). Systemic inflammatory
response syndrome (SIRS) occurs when patients have a severe
infection or trauma, and compensated anti-inflammatory response
syndrome (CARS) may be subsequently triggered (33). The imbalance of SIRS and CARS damages
local tissues cells and affects distant organs, eventually leading
to MODS (34). A previous study
showed that the incidence of MODS in patients with paraquat
poisoning was ~84% (6).
miRNAs are regulatory factors that play crucial
roles in regulating growth, maintaining homeostasis of organisms
and mediating various pathophysiological processes of diseases, and
have become important research topics (35–37). The
present bioinformatics results suggested that miR-27a may be a
potential regulator for IL-10, thus indicating the potential role
of miR-27a in paraquat poisoning. Therefore, a total of 82 patients
with MODS induced by paraquat poisoning and 88 healthy controls
were enrolled in the present study, and the serum miR-27a
expression levels were investigated. The present results suggested
the serum miR-27a expression level was significantly lower in
patients with paraquat poisoning-induced MODS compared with the
healthy controls. The present clinical results suggested that
miR-27a may have a significant association with BUN,
PaCO2, Lac and APACHE II score. Patients poisoned with
paraquat may suffer multiple organ dysfunction of the heart, liver,
lungs and kidney (38). BUN is an
indicator that reflects kidney function, while PaCO2 and
Lac are important indexes reflecting respiratory function and lung
injury (39–41). The present study hypothesized that
miR-27a may be involved in kidney and lung injury in patients with
MODS induced by paraquat poisoning. Ju et al (42) reported that miR-27a can alleviate
acute lung injury in mice by inhibiting inflammation. Additionally,
miR-27a was shown to inhibit pulmonary fibrosis in rats (43). Aguado-Fraile et al (44) reported that miR-27a was
differentially expressed in acute kidney injury (AKI) patients
compared with healthy controls, and serum miR-27a expression level
can be used as a biomarker to predict AKI predisposition. Thus,
previous studies have shown the important role of miR-27a in kidney
and lung injury, in line with the present results.
The present study analyzed the diagnostic and
prognostic value of miR-27a in patients with paraquat
poisoning-induced MODS. The present results suggested that serum
miR-27a expression level was decreased in patients with MODS
induced by paraquat poisoning. Furthermore, ROC curve analysis
suggested that miR-27a may be a sensitive diagnostic biomarker for
MODS induced by paraquat poisoning. Previous studies identified
that a majority of patients with MODS have lung and kidney injury,
and miR-27a was suggested to be involved in organ injury (43,44).
Therefore, this may be the possible mechanism for the diagnostic
ability of miR-27a in paraquat poisoning. In the present study,
according to the overall survival rates after 30 days, patients
were divided into survival group and non-survival group. The
present results suggested that patients in the non-survival group
had higher levels of WBC, BUN, ALT, AST and Lac, and a lower level
of PaCO2 compared with the survival group; reflecting
the reduction in kidney, liver and lung injury. The present results
identified that the non-survival group had lower miR-27a expression
levels, suggesting that miR-27a expression may be associated with
the mortality of patients with paraquat poisoning-induced MODS.
Furthermore, the present multivariate Cox regression analysis
results suggested that miR-27a expression level may be an
independent prognostic factor to predict mortality. As previously
reported, APACHE II score can evaluate the prognosis of acute
paraquat poisoning (45). The
present results suggested that serum miR-27a expression level may
have a significant association with APACHE II score, indicating a
significant correlation of miR-27a with the severity of paraquat
poisoning. Therefore, the present results suggested serum miR-27a
may be a useful clinical tool for predicting the outcome of
paraquat poisoning.
As indicated by the present bioinformatics results,
miR-27a may be a potential regulator of IL-10. The serum expression
level of IL-10 was then investigated, and the present results
suggested patients with MODS induced by paraquat poisoning had
significantly higher IL-10 expression levels compared with healthy
controls. In addition, the present results identified a moderate
negative correlation between the serum expression levels of miR-27a
and IL-10. In paraquat poisoned rats, IL-10 mRNA expression level
is upregulated (13). In addition,
early gastrointestinal lavage with sucralfate was found to
effectively reduce cytokine levels including IL-10, and to improve
lung and kidney injury and survival of paraquat poisoned rats
(14). Xie et al (18) showed that miR-27a can regulate the
inflammatory response by regulating IL-10, and IL-10 was identified
to be the target gene of miR-27a in HEK-293 cells. Therefore,
results from previous studies are in line with the present results
indicating that serum expression level of IL-10 and miR-27a may
reflect the inflammatory response and organ damage in MODS induced
by paraquat poisoning. The present results suggested that miR-27a
may be involved in the process of paraquat poisoning induced MODS
by regulating the inflammatory response. Furthermore, a previous
study showed that overexpression of miR-27a decreases STAT3
phosphorylation by downregulating IL-10 expression level, and
regulates the activation of the JNK1/STAT3 pathway (18). This may be a possible mechanism for
miR-27a in the inflammatory response; however, further study is
needed to investigate this mechanism.
The present study has several limitations. The
clinicopathological parameters of the enrolled patients is not
fully comprehensive as a result of incomplete information
collection, and other clinicopathological parameters could have
been included, such as serum creatinine and serum cardiac troponin
I, for a more thorough examination of the association between
miR-27a level and different organ dysfunction. In addition, other
inflammatory factors involved in the inflammatory response
regulated by IL-10 such as IL-6, TNF-α, interferon and IL-12 should
be examined in patients with MODS. This would be helpful for
understanding the inflammatory response in MODS induced by paraquat
poisoning. Additionally, the present sample size was relatively
small, and further studies with larger sample sizes should be
performed.
In conclusion, the present results suggested that
increased expression level of IL-10 and decreased expression level
of miR-27a in serum may reflect the inflammatory response and organ
damage in MODS induced by paraquat poisoning. The serum miR-27a
expression level may be a potential novel diagnostic and prognostic
factor for patients with MODS induced by paraquat poisoning. In
addition, miR-27a may be involved in the process of paraquat
poisoning induced MODS by regulating the inflammatory response.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HD made substantial contributions to conception and
design, analysis and interpretation of data, draft and revision of
the manuscript. HZ and XZ performed the RNA experiments. HW and LW
contributed to acquisition of data from patients and samples. All
authors were involved in drafting the manuscript and revising it.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was designed under the review and
approval of The Ethics Committee of The Affiliated Hospital of
Weifang Medical University (ID of ethics approval: 2011-1-2).
Written informed consent was collected from each participant.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Flechel A, Jolivet A, Boukhari R,
Misslin-Tritsch C, Manca MF, Wiel E, Megarbane B and Pousset F:
Paraquat poisoning in Western French Guyana: A public health
problem persisting ten years after its withdrawal from the French
market. Eur Rev Med Pharmacol Sci. 22:7034–7038. 2018.PubMed/NCBI
|
|
2
|
Eddleston M and Phillips MR: Self
poisoning with pesticides. BMJ. 328:42–44. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zyoud SH: Investigating global trends in
paraquat intoxication research from 1962 to 2015 using bibliometric
analysis. Am J Ind Med. 61:462–470. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gil HW, Kang MS, Yang JO, Lee EY and Hong
SY: Association between plasma paraquat level and outcome of
paraquat poisoning in 375 paraquat poisoning patients. Clin Toxicol
(Phila). 46:515–518. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gawarammana IB and Buckley NA: Medical
management of paraquat ingestion. Br J Clin Pharmacol. 72:745–757.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang W, Li J, Ma G, Li N, Wang P, Xiao Q,
Li B, Liu Y, Gao X and Li W: Effect of rhubarb as the main
composition of sequential treatment in patients with acute paraquat
poisoning: A prospective clinical research. Zhonghua Wei Zhong Bing
Ji Jiu Yi Xue. 27:254–258. 2015.(In Chinese). PubMed/NCBI
|
|
7
|
Maier RV: Pathogenesis of multiple organ
dysfunction syndrome-endotoxin, inflammatory cells, and their
mediators: Cytokines and reactive oxygen species. Surg Infect
(Larchmt). 1:197–205. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kell DB and Pretorius E: To what extent
are the terminal stages of sepsis, septic shock, systemic
inflammatory response syndrome, and multiple organ dysfunction
syndrome actually driven by a prion/amyloid form of fibrin? Semin
Thromb Hemost. 44:224–238. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ramirez M: Multiple organ dysfunction
syndrome. Curr Probl Pediatr Adolesc Health Care. 43:273–277. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Torrecilla J, Del Pozo-Rodriguez A,
Vicente-Pascual M, Solinís MÁ and Rodríguez-Gascón A: Targeting
corneal inflammation by gene therapy: Emerging strategies for
keratitis. Exp Eye Res. 176:130–140. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wu W and Li Y: Lung injury caused by
paraquat poisoning results in increased interleukin-6 and decreased
microRNA-146a levels. Exp Ther Med. 16:406–412. 2018.PubMed/NCBI
|
|
12
|
Tsai TT, Chuang YJ, Lin YS, Wan SW, Chen
CL and Lin CF: An emerging role for the anti-inflammatory cytokine
interleukin-10 in dengue virus infection. J Biomed Sci. 20:402013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
He XY, Sun Q, Li ZW, Lu ZQ, Hong GL, Liang
H, Qiu QM and Hu GX: Expression of inflammatory factors in lung
tissue of acute paraquat poisoned rats. Zhonghua Lao Dong Wei Sheng
Zhi Ye Bing Za Zhi. 27:149–152. 2009.(In Chinese). PubMed/NCBI
|
|
14
|
Junbo Z, Yongtao Y, Hongbo L, Fenshuang Z,
Ruyun L and Chun'ai Y: Experimental study of sucralfate
intervention for paraquat poisoning in rats. Environ Toxicol
Pharmacol. 53:57–63. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zheng Y, Ge W, Ma Y, Xie G, Wang W, Han L,
Bian B, Li L and Shen L: miR-155 regulates IL-10-Producing
CD24hiCD27+ B cells and impairs their
function in patients with crohn's disease. Front Immunol.
8:9142017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Luo XQ, Shao JB, Xie RD, Zeng L, Li XX,
Qiu SQ, Geng XR, Yang LT, Li LJ, Liu DB, et al: Micro RNA-19a
interferes with IL-10 expression in peripheral dendritic cells of
patients with nasal polyposis. Oncotarget. 8:48915–48921.
2017.PubMed/NCBI
|
|
17
|
Rouas R, Merimi M, Najar M, El Zein N,
Fayyad-Kazan M, Berehab M, Agha D, Bron D, Burny A, Rachidi W, et
al: Human CD8+ CD25+ CD127low
regulatory T cells: microRNA signature and impact on TGF-β and
IL-10 expression. J Cell Physiol. 234:17459–17472. 2019.PubMed/NCBI
|
|
18
|
Xie N, Cui H, Banerjee S, Tan Z, Salomao
R, Fu M, Abraham E, Thannickal VJ and Liu G: miR-27a regulates
inflammatory response of macrophages by targeting IL-10. J Immunol.
193:327–334. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fry DE: Multiple system organ failure.
Surg Clin North Am. 68:107–122. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Feng E, Cheng Y, Tan Z and Wang H:
Experience of continuous fluid therapy in successfully rescuing a
patient with acute severe paraquat poisoning. Zhonghua Wei Zhong
Bing Ji Jiu Yi Xue. 31:1043–1044. 2019.(In Chinese). PubMed/NCBI
|
|
21
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Enright AJ, John B, Gaul U, Tuschl T,
Sander C and Marks DS: MicroRNA targets in Drosophila. Genome Biol.
5:R12003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Agarwal V, Bell GW, Nam JW and Bartel DP:
Predicting effective microRNA target sites in mammalian mRNAs.
Elife. 4:2015. View Article : Google Scholar
|
|
24
|
Kertesz M, Iovino N, Unnerstall U, Gaul U
and Segal E: The role of site accessibility in microRNA target
recognition. Nat Genet. 39:1278–1284. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Marin RM and Vanicek J: Efficient use of
accessibility in microRNA target prediction. Nucleic Acids Res.
39:19–29. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Krek A, Grün D, Poy MN, Wolf R, Rosenberg
L, Epstein EJ, MacMenamin P, da Piedade I, Gunsalus KC, Stoffel M
and Rajewsky N: Combinatorial microRNA target predictions. Nat
Genet. 37:495–500. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lee H, Lim CW, Hong HP, Ju JW, Jeon YT,
Hwang JW and Park HP: Efficacy of the APACHE II score at ICU
discharge in predicting post-ICU mortality and ICU readmission in
critically ill surgical patients. Anaesth Intensive Care.
43:175–186. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hoo ZH, Candlish J and Teare D: What is an
ROC curve? Emerg Med J. 34:357–359. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wills BK, Aks S, Maloney GE, Rhee J, Brand
R and Sekosan M: The effect of amifostine, a cytoprotective agent,
on paraquat toxicity in mice. J Med Toxicol. 3:1–6. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhang L, Li Q, Liu W, Liu Z, Shen H and
Zhao M: Mesenchymal stem cells alleviate acute lung injury and
inflammatory responses induced by paraquat poisoning. Med Sci
Monit. 25:2623–2632. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Huang J, Ning N and Zhang W: Effects of
paraquat on IL-6 and TNF-α in macrophages. Exp Ther Med.
17:1783–1789. 2019.PubMed/NCBI
|
|
32
|
Matsui M, Roche L, Soupe-Gilbert ME, Hasan
M, Monchy D and Goarant C: High level of IL-10 expression in the
blood of animal models possibly relates to resistance against
leptospirosis. Cytokine. 96:144–151. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Buerfent BC, Gondorf F, Wohlleber D,
Schumak B, Hoerauf A and Hübner MP: Escherichia coli-induced immune
paralysis is not exacerbated during chronic filarial infection.
Immunology. 145:150–160. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Sauaia A, Moore FA and Moore EE:
Postinjury inflammation and organ dysfunction. Crit Care Clin.
33:167–191. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Huang X, Wang L, Liu W and Li F:
MicroRNA-497-5p inhibits proliferation and invasion of non-small
cell lung cancer by regulating FGF2. Oncol Lett. 17:3425–3431.
2019.PubMed/NCBI
|
|
36
|
Zhang LY, Chen Y, Jia J, Zhu X, He Y and
Wu LM: MiR-27a promotes EMT in ovarian cancer through active
Wnt/β-catenin signalling by targeting FOXO1. Cancer Biomark.
24:31–42. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yang ZQ, Wu CA and Cheng YX: Prognostic
value of microRNA-133a expression and its clinicopathologic
significance in non-small cell lung cancer: A comprehensive study
based on meta-analysis and the TCGA database. Oncol Res Treat.
41:762–768. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Jiang M, Wang J, Gu S, Cai N, Liu Y, Zhang
Q, Xu P and He F: Clinical features and prognosis analysis of the
elderly and youth patients with acute severe poisoning. Zhonghua
Wei Zhong Bing Ji Jiu Yi Xue. 30:790–794. 2018.(In Chinese).
PubMed/NCBI
|
|
39
|
Cakir M, Duzova H, Baysal I, Gül CC, Kuşcu
G, Kutluk F, Çakin H, Şeker Ş, İlbeği E, Uslu S, et al: The effect
of hypericum perforatum on kidney ischemia/reperfusion damage. Ren
Fail. 39:385–391. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Shebl E and Burns B: Respiratory Failure.
StatPearls; Treasure Island (FL): 2019
|
|
41
|
B'Chir A, Mebazaa A, Losser MR, Romieu M
and Payen D: Intravenous almitrine bismesylate reversibly induces
lactic acidosis and hepatic dysfunction in patients with acute lung
injury. Anesthesiology. 89:823–830. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ju M, Liu B, He H, Gu Z, Liu Y, Su Y, Zhu
D, Cang J and Luo Z: MicroRNA-27a alleviates LPS-induced acute lung
injury in mice via inhibiting inflammation and apoptosis through
modulating TLR4/MyD88/NF-κB pathway. Cell Cycle. 17:2001–2018.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Liu L, Qian H, Hu K, Wang L, Zhang Z, Yin
H and He J: miR-27a-3p inhibits pulmonary fibrosis by blocking
Wnt3a/β-catenin pathway in rats. Xi Bao Yu Fen Zi Mian Yi Xue Za
Zhi. 34:1015–1020. 2018.(In Chinese). PubMed/NCBI
|
|
44
|
Aguado-Fraile E, Ramos E, Conde E,
Rodríguez M, Martín-Gómez L, Lietor A, Candela Á, Ponte B, Liaño F
and García-Bermejo ML: A pilot study identifying a set of microRNAs
as precise diagnostic biomarkers of acute kidney injury. PLoS One.
10:e01271752015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Huang NC, Hung YM, Lin SL, Wann SR, Hsu
CW, Ger LP, Hung SY, Chung HM and Yeh JH: Further evidence of the
usefulness of Acute Physiology and Chronic Health Evaluation II
scoring system in acute paraquat poisoning. Clin Toxicol (Phila).
44:99–102. 2006. View Article : Google Scholar : PubMed/NCBI
|