Introduction
Kawasaki disease (KD) is a self-limiting, acute
disease characterized by fever, rash and vasculitis. In total, ~85%
of patients with KD are younger than 5 years old, with an average
age of 2 years. The prevalence of KD among children under 5 years
of age is >50/100,000 in areas, such as Korea, Japan and Taiwan.
The prevalence has increased over the past 20 years for unknown
reasons (1). If patients with KD are
not correctly diagnosed on time and treated accordingly, it may
result in the formation of coronary artery lesions (CAL). A
Previous study demonstrated that the risk for untreated children
with KD younger than 1 year developing CAL is >60% (2).
As KD can only be diagnosed by identifying the
clinical symptoms, the diagnosis and treatment of patients with KD
are sometimes delayed, especially in patients with incomplete KD,
which is characterized by incomplete manifestation of clinical
symptoms. Therefore, in cases with vague clinical symptoms,
diagnosis must rely on auxiliary diagnostic markers, such as
increased C-reactive protein (CRP) levels and erythrocyte
sedimentation rate (ESR) levels, and low albumin, anemia and
alanine aminotransferase (ALT) levels (1,2).
Previously, developments in molecular biology and
laboratory medicine have promoted the understanding of the
association between KD and clinical indicators, including
N-terminal pro-B-type natriuretic peptide (NT-proBNP) and cardiac
troponin I (cTnI). Monitoring the dynamic variations of NT-proBNP,
cTnI and other clinical indicators in patients with KD is effective
for evaluating the risk of CAL and predicting prognosis (3). Color Doppler echocardiography is an
imaging technique utilized to identify coronary artery anomalies
and assess myocardial function. Coronary artery diameter and its
Z-score are useful in diagnosis of patients with KD and CAL risk
stratification (4). Children with
KD, particularly infants, tend to have atypical signs and symptoms,
which makes it difficult to diagnose. Therefore, color Doppler
echocardiography is particularly critical for diagnosis of KD in
this population group (5). To the
best of the authors' knowledge, only a few previous studies have
evaluated the association of color Doppler ultrasonography and
clinical indicators in patients with KD with CAL (5,6).
Therefore, the present study aimed to analyze the benefit of color
Doppler echocardiography combined with clinical indicators in the
diagnosis and prognosis prediction of KD complicated with CAL.
Patients and methods
Patients
The present study recruited 102 children with KD
hospitalized in The Affiliated Hospital of Inner Mongolia Medical
University from September 2012 to October 2018. This prospective
work was approved by The Ethics Committee of the Affiliated
Hospital of Inner Mongolia Medical University, and informed
consents were obtained from the legal guardians of the enrolled
children. KD was diagnosed according to the criteria recommended by
The American Heart Association, 2004 (7,8).
Inclusion criteria consisted of patients who were: i) Younger than
18 years old; ii) signed informed consent; and iii) met the
diagnostic criteria for KD in children. Exclusion criteria
consisted of patients with: i) Insufficient clinical data; ii)
inherited metabolic illnesses and developmental malformations; and
iii) cardiopulmonary insufficiency or other critical illnesses. The
Z-score of the coronary artery diameter was set with respect to the
body surface area of patients in the CAL group, and it was set as
≥2.5. However, it was set to ≤2.5 in the non-coronary artery lesion
(NCAL) group (9).
Clinical examination
Whole blood, plasma and serum samples were collected
from patients with acute KD before any treatment with intravenous
immunoglobulin (IVIG). White blood cell count, blood platelet
count, IVIG resistance, NT-proBNP, hemoglobin, serum albumin (ALB),
cTnI, CRP, ESR, ALT and aspartate aminotransferase (AST) levels
were measured using a Mindray BC-5000 automatic blood cell
analyzer, a BS-600 automatic biochemical analyzer and a CL-2000i
chemiluminescence immunoassay analyzer (all purchased from Mindray
Bio-medical Electronics Co., Ltd.), respectively. The patients were
divided into four subgroups based on age: i) <1 year old; ii)
1-3 years old; iii) 3-5 years old; and iv) ≥5 years old.
Color Doppler echocardiography
Color Doppler echocardiography was carried out when
the patient was initially hospitalized, as well as 2 and 5 weeks
after IVIG administration. ‘Zworst’ was defined as the
higher Z-scores of the right coronary artery and the left anterior
descending coronary artery at any point during the active disease.
The aortic root was measured parallel to the long axis near the
sternum over the mid-systolic phase. A Z-score ≥2.0 for the aortic
sinus after normalizing to the body surface area was considered as
dilation (10). According to The
American Heart Association's adjusted standards, expansion of the
right coronary artery and left anterior descending coronary artery
is defined as Zworst ≥2.5 (standard deviation of mean
internal diameter standardized by body surface area) (8). The patients in the CAL group were
divided into three grades based on the severity of dilation. The
first grade involved small aneurysms or local dilation (mild) in
0-5 years old children whose coronary artery diameter was <4 mm,
or in children >5 years old whose coronary artery diameter was
1.5 times less than that in the adjacent sectors. The second grade
involved medium-sized aneurysms (moderate) in children aged 0-5
years whose coronary artery diameter was 4-8 mm, or in children
>5 years old whose coronary artery diameter in the measured
segment was 1.5-4 times less than that in the nearby sections. The
third grade included giant aneurysms (severe) in children aged 0-5
years whose coronary artery diameter was >8 mm or in children
>5 years old whose artery segment's diameter was 4 times larger
compared with the nearby sections (11). Cardiac echocardiography was conducted
for follow-up in these children, 6 months, 1 year and 2 years after
discharge.
Statistical analysis
Statistical analysis was conducted using STATA 14.0
software (StataCorp LP) and GraphPad Prism 7.0 (GraphPad Software,
Inc.) was used to construct figures. The measurement data are
presented as the mean ± standard deviation, and the enumeration
data are presented as cases (%). For continuous variables analysis
between CAL and NCAL groups, Mann-Whitney U test or t-test was
utilized. Differences in the classified variables was compared
using the Kruskal-Wallis rank-sum test, Fisher's exact test or
χ2 test. Kendall's rank correlation was used to analyze
the correlation between rank variables. The general data, blood
routine parameters and biochemical indexes between the CAL and NCAL
groups were included in the logistic regression analysis model.
Their impacts on CAL occurrence were analyzed using the stepwise
regression technique. The test level of variables included in the
equation was 0.10, and the retention level of variables was 0.015.
Multiple linear regression was performed between coronary artery
diameter and blood routine, and biochemical parameters. P<0.05
was considered to indicate a statistically significant
difference.
Results
Patient characteristics
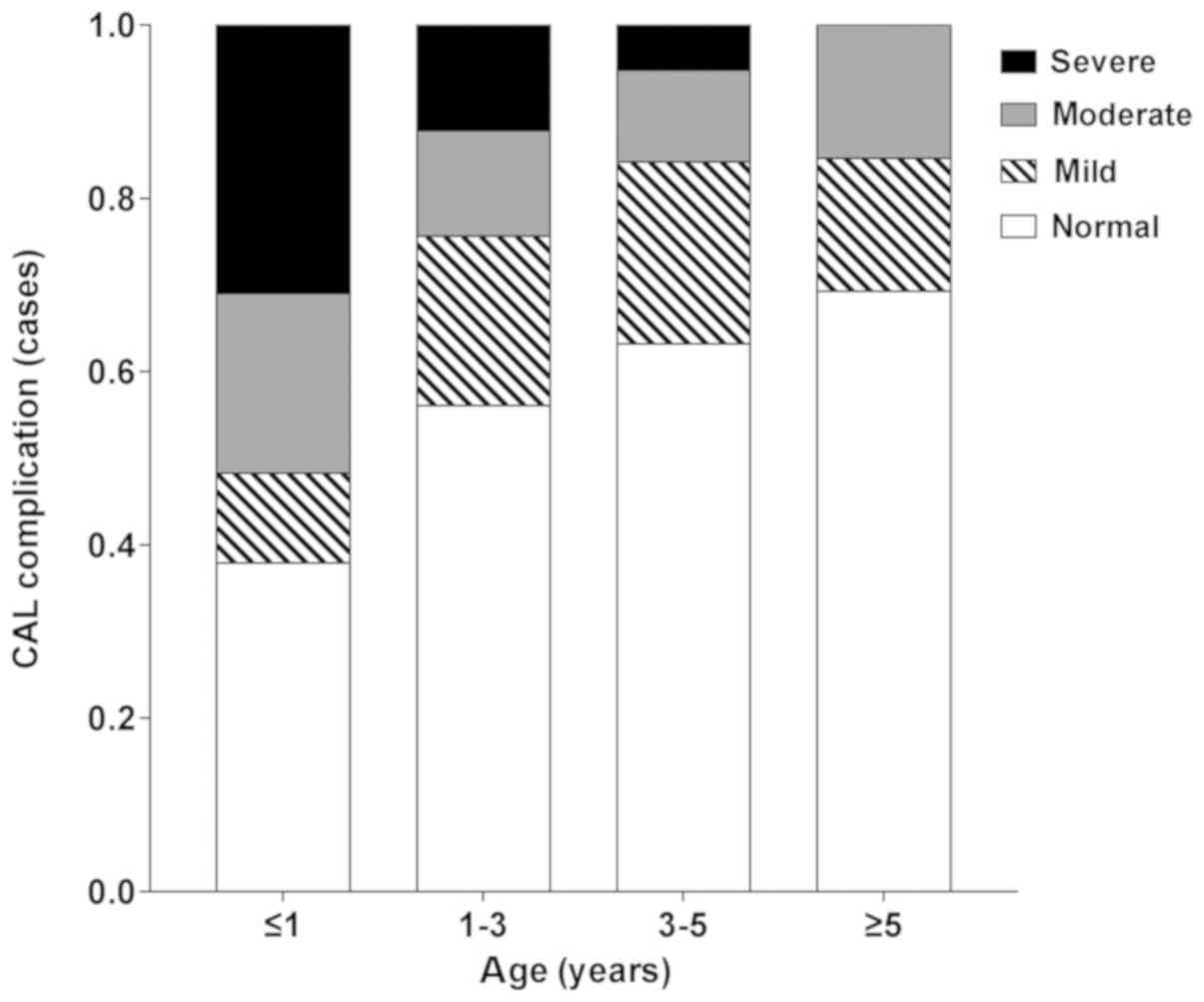
Among the total 102 cases, 47 cases (46.08%)
presented with CAL complications. This included 11 cases of right
coronary artery dilatation, 16 cases of left coronary artery
dilatation, 6 cases of giant coronary artery aneurysm and 14 cases
of bilateral coronary artery dilatation (Table I). The ratio of male to female cases
was 1.37:1 (59:43), and the average age was 2.5±1.9 years old. No
significant differences were identified in the occurrence of CAL
among various age groups (P=0.176; Table
I). Although, there was a difference in the severity of CAL
among different age groups (P=0.063) and a significant correlation
was identified between them (P=0.004; Table II; Fig.
1).
 | Table IOccurrence rate of CAL in different
age groups. |
Table I
Occurrence rate of CAL in different
age groups.
| Age group | <1 year, n=29 | 1-3 year(s),
n=41 | 3-5 years, n=19 | ≥5 year, n=13 | Total, n=102 |
|---|
| Left coronary artery
dilatation, n (%) | 6 (20.69) | 6 (14.63) | 2 (10.53) | 2 (15.38) | 16 (15.69) |
| Right coronary artery
dilatation, n (%) | 4 (13.79) | 4 (9.76) | 2 (10.53) | 1 (7.69) | 11 (10.78) |
| Bilateral coronary
artery dilation, n (%) | 6 (20.69) | 5 (12.20) | 2 (10.53) | 1 (7.69) | 14 (13.73) |
| Giant coronary artery
aneurysm, n (%) | 2 (6.90) | 3 (7.32) | 1 (5.26) | 0 (0.00) | 6 (5.88) |
| Total, n (%) | 18 (62.07) | 18 (43.90) | 7 (36.84) | 4 (30.77) | 47 (46.08) |
 | Table IISeverity of CAL in different age
groups. |
Table II
Severity of CAL in different age
groups.
| Age group | <1 year, n=29 | 1-3 year (s),
n=41 | 3-5 years, n=19 | ≥5 year, n=13 | Total, n=102 |
|---|
| None, n (%) | 11 (37.93) | 23 (56.10) | 12 (63.16) | 9 (69.23) | 55 (53.92) |
| Mild, n (%) | 3 (10.34) | 8 (19.51) | 4 (21.05) | 2 (15.38) | 17 (16.67) |
| Moderate, n (%) | 6 (20.69) | 5 (12.20) | 2 (10.53) | 2 (15.38) | 15 (14.71) |
| Severe, n (%) | 9 (31.03) | 5 (12.20) | 1 (5.26) | 0 (0.00) | 15 (14.71) |
Univariate analysis
In the CAL group, fever duration, levels of
NT-proBNP, cTnI, IVIG resistance, CRP, ESR, platelet, ALT and AST
were significantly higher compared with the NCAL group (all
P<0.05; Tables III and IV). The serum ALB levels were
significantly lower in the CAL group compared with the NCAL group
(P<0.05; Tables III and IV).
Logistic regression analysis
Logistic regression analysis was conducted with the
coronary artery lesions as dependent variables and the indices with
significant differences in univariate analysis as independent
variables. The assignments of continuous variables in routine blood
parameters and the biochemical indicators are presented in Table V. The logistic regression analysis
results demonstrated that fever duration (OR=2.014), NT-proBNP
(OR=3.004), cTnI level (OR=2.638), ESR (OR=1.461) and CRP elevation
(OR=1.094) were the parameters affecting CAL in KD
(R2=0.691; Table
VI).
 | Table VAssignment Table of logistic
regression analysis. |
Table V
Assignment Table of logistic
regression analysis.
| | Assignment | |
|---|
| Parameter | <0 | 1 | 2 | Weight
coefficient |
|---|
| PLT,
x103/mm3 | <400 | ≥400, <600 | ≥600 | 1 |
| ALB, g/l | <20 | ≥20, <40 | ≥40 | 1 |
| ESR, mm/h | <50 | ≥50, <70 | ≥70 | 1 |
| CRP, mg/l | <50 | ≥50, <70 | ≥70 | 1 |
| ALT, IU/l | <30 | ≥30, < 50 | ≥50 | 1 |
| AST, IU/l | <40 | ≥40, <70 | ≥70 | 1 |
| NT-proBNP,
ng/ml | <1.1 | ≥1.1, <1.8 | ≥1.8 | 1 |
| cTnI, ng/ml | <0.01 | ≥0.01,
<0.02 | ≥0.02 | 1 |
 | Table VIResult of logistic regression
analysis. |
Table VI
Result of logistic regression
analysis.
| Parameter | β | SE | χ2
(wald) | P-value | OR |
|---|
| Constant | -25.04 | 11.35 | 4.87 | | |
| Days of fever | 0.7 | 0.32 | 4.79 | 0.03 | 2.014 |
| NT-proBNP | 1.1 | 0.34 | 10.47 | 0.00 | 3.004 |
| cTnI | 0.97 | 0.44 | 4.86 | 0.03 | 2.638 |
| ESR | 0.38 | 0.189 | 4.04 | 0.04 | 1.461 |
| CRP | 0.09 | 0.04 | 5.06 | 0.02 | 1.094 |
Logistic regression (stepwise regression method) was
also conducted by taking the pre-treatment coronary artery diameter
(mm) and the indices with significant differences in univariate
analysis as independent variables and with the coronary artery
lesions as dependent variables. Finally, Y (CAL=1/NCAL=0)=0.24
* coronary artery diameter + 0.59 * fever
duration + 1.15 * NT-proBNP + 0.83 * cTnI +
0.61 * ESR-6.73 (R2=0.952). This improved the
determinant coefficient of the logistic regression model.
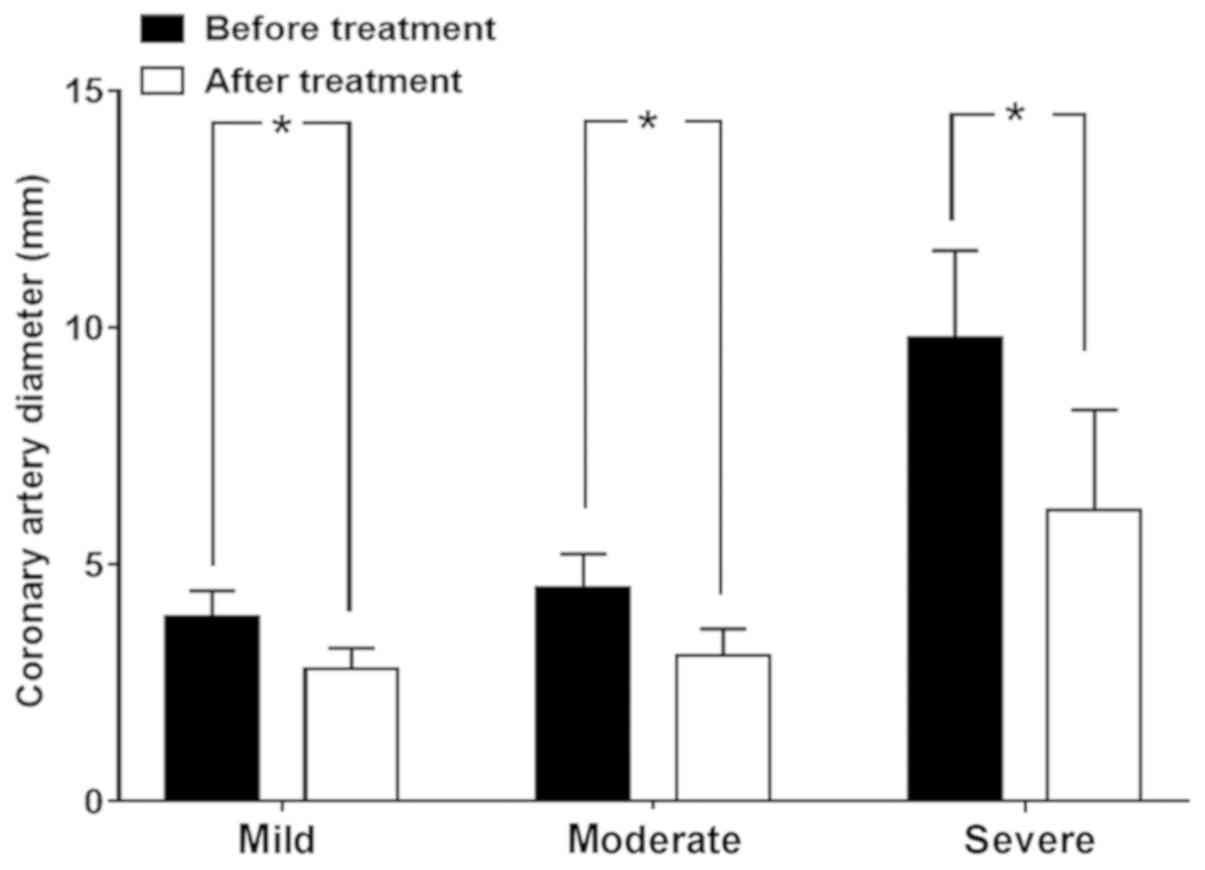
Significant differences were identified in dilated
lesions within the patients with CAL at different levels in the
follow-up (χ2=11.48, P=0.003). The follow-up of mild CAL
patients was better than that of moderate and severe CAL patients
(χ2=6.48 and 11.48, respectively, P<0.01). The
diameter of coronary artery in the recovery period of patients with
different severity in CAL group was significantly reduced. The
t-values of mild, moderate and severe patients were 6.31, 6.03 and
5.00, respectively, P-values were <0.001 (Table VII; Fig.
2).
 | Table VIIResults of cardiac ultrasound
examination in the coronary artery lesion group in the
follow-up. |
Table VII
Results of cardiac ultrasound
examination in the coronary artery lesion group in the
follow-up.
| | Severity of
disease |
|---|
| Result | Mild, n=17 | Moderate, n=15 | Severe, n=15 |
|---|
| Dilated
lesionsa | | | |
| Return to
normal | 17 | 10 | 7 |
| Reduction of inner
diameter | 0 | 4 | 5 |
| Continued
expansion | 0 | 1 | 3 |
| Coronary artery
diameter, mm | | | |
| Before
treatment | 3.89±0.56 | 4.51±0.72 | 9.78±1.85 |
| After
treatment |
2.80±0.44b |
3.08±0.57b |
6.15±2.12b |
Multiple linear regression
The blood routine parameters and biochemical indexes
of the patients were taken as independent variables and the
coronary artery diameters after the treatment was taken as a
dependent variable to establish a multiple linear regression model.
The results showed the coronary artery diameter after
treatment=0.21 * fever duration + 0.73 *
NT-proBNP + 0.94 * cTnI + 0.59 * ESR + 0.47
* C-reactive protein-1.58 (R2=0.636).
Discussion
KD is an inflammatory febrile disease occurring in
children and is the initial cause for childhood-acquired heart
illness. Coronary artery aneurysm is a severe KD complication,
which causes ischemic heart disease, myocardial infarction and
unexpected cardiac death (1).
Coronary artery Z-score measurement using echocardiography within
the acute phase of KD not only provides vascular health
information, but also provides the risk assessment of
cardiovascular disease and aids in clinical decision-making
(12). CAL in patients with KD leads
to atherosclerotic vascular remodeling during recovery by intimal
hyperplasia and neovascularization after vasculitis (13). Based on the current recommendations,
it is stated that echocardiography must be conducted during the
diagnosis for complex KD cases without any obvious signs of
coronary artery disease, then again at 1-2 weeks and 4-6 weeks
following treatment. More frequent evaluation is required for
patients with progressive abnormalities to detect thrombosis and
aneurysms (14,15).
The signs and symptoms, clinical data and
echocardiographic results of 200 children with KD were analyzed in
a previous study and it was identified that the signs and symptoms
of KD in infants <3 months old were varied, and these patients
were exposed to a higher risk of coronary artery anomalies;
nevertheless, barring the patients suffering from giant coronary
artery aneurysms, all other patients successfully recovered after
an average follow-up period of 18 months with no complications
(16). A previous retrospective
study performed by Cameron et al (17) compared the severity of coronary
artery dilatation in 93 infants within the age of 1 year and 170
children older than 1 year old treated at the same time. The
previous study identified that there was a significantly higher
average maximum Z-score in the infants than the older children.
Furthermore, the infants had a higher occurrence of aneurysms
compared with the older children (11 vs. 3% for moderate aneurysms
and 8 vs. 1% for giant aneurysms) (15). These previous studies also suggested
that as the children's age increases, the occurrence of coronary
artery dilatation and the severity of arterial dilatation were
reduced.
The majority of patients with KD recover well after
treatment; however, coronary artery aneurysms may develop in ~25%
of untreated cases (18). Early
diagnosis and treatment together with follow-up by echocardiography
play important roles for positive outcomes. The risk of
cardiovascular complications can be considerably reduced by
combining IVIG and aspirin over 10 days of KD onset (15). In total, 10-15% of children with KD
do not respond positively against initial IVIG and there is an
elevated risk of CAL in these children (19). A previous meta-analysis performed by
Baek and Song (19) on 2,745
patients from 12 studies demonstrated that raised NT-proBNP, ALT,
bilirubin and CRP, and reduced ALB and sodium levels were risk
factors for non-response to primary treatment with IVIG. A
multicenter retrospective study carried out in 38 Korean hospitals
identified that serum NT-proBNP levels and the percentage of
polymorphonuclear leukocytes in the IVIG resistant group were
considerably higher compared with the control group. Based on the
correlation between NT-proBNP levels and IVIG resistance, it was
suggested that NT-proBNP may be valuable in prediction prognosis
(20).
In recent years, developments in molecular biology
and clinical medicine techniques have made it possible to discover
biomarkers as a powerful instrument for stratifying the risk and
predicting the prognosis of cardiovascular diseases (21). Myocardial cell stress-related
biomarkers are raised in most patients suffering from acute KD;
NT-proBNP is associated with inflammation, while oxidative stress
markers and echocardiographic results indicate diastolic
dysfunction (22). Myocardial cells
release NT-proBNP against the inflammatory cytokines and
ventricular dilatation. It was primarily utilized in diagnosing
cardiac disease in adults, and it was demonstrated that this marker
was effective in diagnosing and treating patients with KD as well
(23). In the early stage of KD,
myocardial inflammation is common. NT-proBNP may be a more useful
biomarker for diagnosing KD compared with the highly sensitive CRP
(19). The mean NT-proBNP levels in
patients with complete and incomplete KD was considerably higher
than that of age-matched patients with simple fever (22). In addition, the mean NT-proBNP levels
in patients with complete KD was higher than that of patients with
incomplete KD (23,24). A previous study identified that high
NT-proBNP levels exist in patients with KD who are resistant to
IVIG treatment as well as those who have a coronary artery
aneurysm, indicating its prognostic utility (24). There is a high risk of incomplete KD
and early CAL in infants <3 months compared with older patients.
Therefore, it is recommended that infants with fever lasting for
>2 days are evaluated by echocardiography and also for NT-proBNP
levels, irrespective of the presence or absence of other KD-related
symptoms (25). The present results
suggested that NT-proBNP levels in the CAL group were considerably
higher when compared with the NCAL group. Based on the logistic
regression analysis, it was observed that the OR of NT-proBNP was
3.004, indicating that there is an association between NT-proBNP
levels and the incidence of CAL.
cTnI is a cardiomyocyte injury or death marker and
is increased in both patients with KD and fever controls (24). Based on unexpected increments in cTnI
in the majority of patients with KD in convalescence, it was
suggested that myocardial cell damage occurs even after the
systemic inflammatory markers reduced to normal levels. In all
patients tested 1-2 years after disease onset, cTnI levels returned
to normal, further suggesting that the previous increase in cTnI
was related to the myocardial cell damage or death (26). In patients with incomplete KD, the
acute and sub-acute age-corrected hemoglobin levels were reduced;
however, the sub-acute platelet counts increased in patients with
complete KD. Furthermore, it is known that the platelet counts in
KD patients are positively correlated with fever duration, and a
longer inflammation period may be reflected in the increase in
platelet counts (27). Jeon et
al (28) observed that coronary
artery aneurysms developed in 30 of 392 patients with KD within a
month of diagnosis while in 20% they persisted even after 1 year of
follow-up. High platelet counts and long-term fever are independent
indicators of coronary artery aneurysm immediately after diagnosis.
According to the univariate analysis in a previous study, increased
white blood cell count and the primary coronary artery severity
were independent risk factors for the persistence of enhanced
coronary artery aneurysms. Nevertheless, no considerable difference
was identified in the multivariate analysis (15). Previous studies have demonstrated
that platelet counts and age-corrected hemoglobin can be utilized
not only as specific indicators of KD but also as predictors of
coronary artery dilatation in patients with complete and incomplete
KD, respectively. Elevated platelet counts and CRP levels, and
lower hemoglobin and ALB levels are also risk factors for acute
coronary artery aneurysms (12,29). In
general, these previous studies were in agreement with the
univariate analysis in the present study. However, platelet count,
hemoglobin and ALB were not considered for logistic regression in
the present study as independent factors for the incidence of
CAL.
The clinical markers analyzed in the present study
are very simple to measure, and most are associated with
significant differences in patients with CAL and NCAL. However, the
present study had some limitations. First, there were numerous
indicators for analysis and classifying the patients based on the
age was too narrow. Consequently, future studies should aim to
increase the sample size and carry out a multi-center study to
validate the results obtained in the present study. There was a
correlation between clinical markers and KD with concurrent CAL;
however, more data are required to validate these markers as risk
factors for disease incidence. Ultimately, the markers evaluated in
the logistic regression analysis had shown differences in the
univariate analysis; therefore, the key risk factors may be
eliminated due to the confounding factors.
In conclusion, color Doppler echocardiography is
able to measure the degree of illness in patients with KD and
predict the outcome of coronary artery disease in real time since
it is useful for both early diagnosis and long-term follow-up.
Fever duration, NT-proBNP, cTnI levels, ESR and elevated CRP may be
high-risk factors for CAL in KD. The fever duration, cTnI level,
NT-proBNP and ESR were also correlated with coronary artery
diameter. Comprehensive use of these clinical parameters may more
accurately determine the occurrence of CAL in KD.
Acknowledgements
Not applicable.
Funding
The present study was supported by The Natural
Science Foundation of Inner Mongolia (grant no. 2018MS08080).
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MX helped collect the data, perform the ultrasound
diagnosis and follow-up, write the manuscript and perform the
statistical analysis. JW contributed in the conception and design
of the study, data gathering, ultrasound diagnosis and follow-up,
and manuscript guidance. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
This prospective work was approved by The Ethics
Committee of the Affiliated Hospital of Inner Mongolia Medical
University, and informed consents were obtained from the legal
guardians of the enrolled children.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Singh S, Vignesh P and Burgner D: The
epidemiology of Kawasaki disease: A global update. Arch Dis Child.
100:1084–1088. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hedrich CM, Schnabel A and Hospach T:
Kawasaki Disease. Front Pediatr 6. 198:2018. View Article : Google Scholar
|
|
3
|
JCS Joint Working Group: Guidelines for
diagnosis and management of cardiovascular sequelae in Kawasaki
disease (JCS 2013). Digest version. Circ J 78: 2521-2562, 2014.
|
|
4
|
McCrindle BW and Cifra B: The role of
echocardiography in Kawasaki disease. Int J Rheum Dis. 21:50–55.
2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Argyropoulou OD, Protogerou AD and
Sfikakis PP: Accelerated atheromatosis and arteriosclerosis in
primary systemic vasculitides: Current evidence and future
perspectives. Curr Opin Rheumatol. 30:36–43. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kato M, Ayusawa M, Watanabe H, Komori A,
Abe Y, Nakamura T, Kamiyama H and Takahashi S: Cardiac function on
3-D speckle tracking imaging and cytokines in Kawasaki disease.
Pediatr Int (Roma). 60:342–348. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Singh S, Jindal AK and Pilania RK:
Diagnosis of Kawasaki disease. Int J Rheum Dis. 21:36–44.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Pilania RK, Bhattarai D and Singh S:
Controversies in diagnosis and management of Kawasaki disease.
World J Clin Pediatr. 7:27–35. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Newburger JW, Takahashi M, Gerber MA,
Gewitz MH, Tani LY, Burns JC, Shulman ST, Bolger AF, Ferrieri P,
Baltimore RS, et al: Committee on Rheumatic Fever, Endocarditis,
and Kawasaki Disease, Council on Cardiovascular Disease in the
Young, American Heart Association: Diagnosis, treatment, and
long-term management of Kawasaki disease: A statement for health
professionals from the Committee on Rheumatic Fever, Endocarditis,
and Kawasaki Disease, Council on Cardiovascular Disease in the
Young, American Heart Association. Pediatrics. 114:1708–1733.
2004.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ravekes WJ, Colan SD, Gauvreau K, Baker
AL, Sundel RP, van der Velde ME, Fulton DR and Newburger JW: Aortic
root dilation in Kawasaki disease. Am J Cardiol. 87:919–922.
2001.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Noto N, Komori A, Ayusawa M and Takahashi
S: Recent updates on echocardiography and ultrasound for Kawasaki
disease: Beyond the coronary artery. Cardiovasc Diagn Ther.
8:80–89. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ha KS, Jang GY, Lee J, Lee KC and Son CS:
Laboratory Markers in Incomplete Kawasaki Disease according to
Coronary Artery Outcome. Korean Circ J. 48:287–295. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cameron SA, Robinson JD, Carr MR and Patel
A: Giant coronary artery aneurysms in an infant with Kawasaki
disease: Evaluation by echocardiography and computed tomographic
angiography. Echocardiography. 35:1692–1694. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
de Ferranti SD, Gauvreau K, Friedman KG,
Tang A, Baker AL, Fulton DR, Tremoulet AH, Burns JC and Newburger
JW: Association of Initially Normal Coronary Arteries With Normal
Findings on Follow-up Echocardiography in Patients With Kawasaki
Disease. JAMA Pediatr. 172(e183310)2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Dionne A and Dahdah N: Myocarditis and
Kawasaki disease. Int J Rheum Dis. 21:45–49. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Li W, Zhang L, Huang P and Zhang Z:
Clinical features and mid-term follow-up in infants younger than 3
months with Kawasaki disease in a Chinese population. J Paediatr
Child Health. 55:523–527. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Cameron SA, Carr M, Pahl E, DeMarais N,
Shulman ST and Rowley AH: Coronary artery aneurysms are more severe
in infants than in older children with Kawasaki disease. Arch Dis
Child. 104:451–455. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Toyono M, Takagi D, Oyamada J, Shimada S,
Aoki-Okazaki M and Takahashi T: Coronary artery aneurysm after
kawasaki disease in a single coronary artery. Circ J. 77:2409–2411.
2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Baek JY and Song MS: Meta-analysis of
factors predicting resistance to intravenous immunoglobulin
treatment in patients with Kawasaki disease. Korean J Pediatr.
59:80–90. 2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kim MK, Song MS and Kim GB: Factors
Predicting Resistance to Intravenous Immunoglobulin Treatment and
Coronary Artery Lesion in Patients with Kawasaki Disease: Analysis
of the Korean Nationwide Multicenter Survey from 2012 to 2014.
Korean Circ J. 48:71–79. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Maggio MC, Corsello G, Prinzi E and Cimaz
R: Kawasaki disease in Sicily: Clinical description and markers of
disease severity. Ital J Pediatr. 42(92)2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lee SH, Song ES, Yoon S, Hong S, Cho HJ,
Yang EM, Eom GH, Kang G and Cho YK: Usefulness of Age-Stratified
N-Terminal Prohormone of Brain Natriuretic Peptide for Diagnosing
Kawasaki Disease. Dis Markers. 2017(6263121)2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Dionne A and Dahdah N: A Decade of
NT-proBNP in Acute Kawasaki Disease, from Physiological Response to
Clinical Relevance. Children (Basel). 5(E141)2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sato YZ, Molkara DP, Daniels LB, Tremoulet
AH, Shimizu C, Kanegaye JT, Best BM, Snider JV, Frazer JR, Maisel
A, et al: Cardiovascular biomarkers in acute Kawasaki disease. Int
J Cardiol. 164:58–63. 2013.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Satoh K, Wakejima Y, Gau M, Kiguchi T,
Matsuda N, Takasawa R, Takasawa K, Nishioka M and Shimohira M: Risk
of coronary artery lesions in young infants with Kawasaki disease:
Need for a new diagnostic method. Int J Rheum Dis. 21:746–754.
2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Liu W, Liu C, Zhang L, Xie X, Gu X, Sang
C, Xu M, Xu W and Jia H: Molecular basis of coronary artery
dilation and aneurysms in patients with Kawasaki disease based on
differential protein expression. Mol Med Rep. 17:2402–2414.
2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Chen J, Liu Y, Liu W and Wu Z: A
meta-analysis of the biomarkers associated with coronary artery
lesions secondary to Kawasaki disease in Chinese children. J
Huazhong Univ Sci Technolog Med Sci. 31:705–711. 2011.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Jeon SK, Kim G, Ko H, Byun JH and Lee HD:
Risk factors for the Occurrence and Persistence of Coronary
Aneurysm in Kawasaki Disease. Korean J Pediatr. 62:138–143.
2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kim HJ, Choi EH, Lim YJ and Kil HR: The
Usefulness of Platelet-derived Microparticle as Biomarker of
Antiplatelet Therapy in Kawasaki Disease. J Korean Med Sci.
32:1147–1153. 2017.PubMed/NCBI View Article : Google Scholar
|