Introduction
Acute pancreatitis (AP) is one of the most common
acute abdominal diseases in the clinic worldwide and is typically
caused by cholelithiasis, alcoholism and hyperlipidemia (1,2). In
recent years, the incidence of hyperlipidemic acute pancreatitis
(HTGAP) has been increasing, becoming the secondary cause of AP
under biliary AP (3). Patients with
HTGAP are prone to recurrence, occasionally with uncontrolled
seizures, which seriously endangers the health of the patient
(4,5). At present, the diagnosis of HTGAP is
primarily based on clinical signs, blood urine amylase levels and
serum triacylglycerol levels. However, these diagnostic criteria
have a number of limitations, which make the clinical diagnosis and
treatment of HTGAP difficult (6,7).
Therefore, it is imperative to identify specific biomarkers for the
diagnosis of HTGAP.
MicroRNAs (miRNAs/miRs) are a class of endogenous,
non-coding small RNAs 19-25 nucleotides in length, which
participate in a number of pathophysiological processes, such as
cancer and diabetes (8-11).
Numerous studies have reported that miRs are closely related to the
occurrence and development of AP; therefore, miRs serve as novel
markers for the diagnosis and prognosis of the disease (10-12).
However, whether miRs can be used as markers for the diagnosis of
HTGAP and for predicting the severity of the disease has not been
reported.
Abnormal expression of miR-372 has been widely
identified in various tumors, including pancreatic adenocarcinoma,
as well as ovarian and parathyroid cancer (13-15).
It has been reported that miR-372 expression is significantly
reduced in human pancreatic adenocarcinoma (13); however, the relationship between
miR-372 expression, and the occurrence and development of HTGAP
remains unclear. In the present study, the relative expression of
miR-372 was detected in 115 patients with AP, and the correlation
between miR-372 expression and HTGAP was investigated.
Materials and methods
Patient samples
Patients with AP were admitted to the Department of
General Surgery, Jinling Clinical Medical College between November
2018 and December 2018. Clinical data were collected during
hospitalization to evaluate the acute physiology and Acute
Physiology and Chronic Health Evaluation (APACHE) II score
(16) of each patient. Inclusion
criteria were as follows: i) Aged between 18 and 65 years; and ii)
conformed to the AP diagnostic standard. The AP diagnostic standard
consists of i) displaying abdominal pain consistent with AP (acute
sudden persistent upper abdominal pain, often radiating to the
back); ii) serum amylase and/or lipase levels ≥3 times higher than
the upper limit of the normal levels; and iii) imaging results
consistent with AP lesions. The following exclusion criteria were
used: i) patients with cancer; ii) pregnant patients; iii) patients
with psychiatric conditions or patients who refused to cooperate;
and iv) patients who give up treatment, transferred out of the
department or died.
According to the aforementioned criteria, 115
patients with AP were enrolled (60 male patients and 55 female
patients; age, 22-66 years; mean age, 47.3±11.5 years). Patients
with serum lipid concentrations ≥11.3 mmol/l or serum lipid levels
5.65-11.3 mmol/l with chylous serum were included in group A
(n=40). Subsequently, group A was subdivided into patients with
mild (HTG-MAP) or severe (HTG-SAP) HTGAP, according to the AP
classification standard (n=20 per group). The remainder of the
patients with AP did not have HTGAP and were included in group B. A
further 25 patients with hyperlipidemia but not AP (group C)
admitted to the Department of General Surgery, Jinling Clinical
Medical College (China) between November 2018 and December 2018 (12
males and 13 females; age range, 34-68 years; mean age, 48.9±16.8
years) and 30 healthy volunteers (group D) from the Physical
examination Center, Jinling Clinical Medical College (China)
between November 2018 and December 2018 (16 males and 14 females;
age range, 42-71 years; mean age, 46.9±15.3 years) were recruited
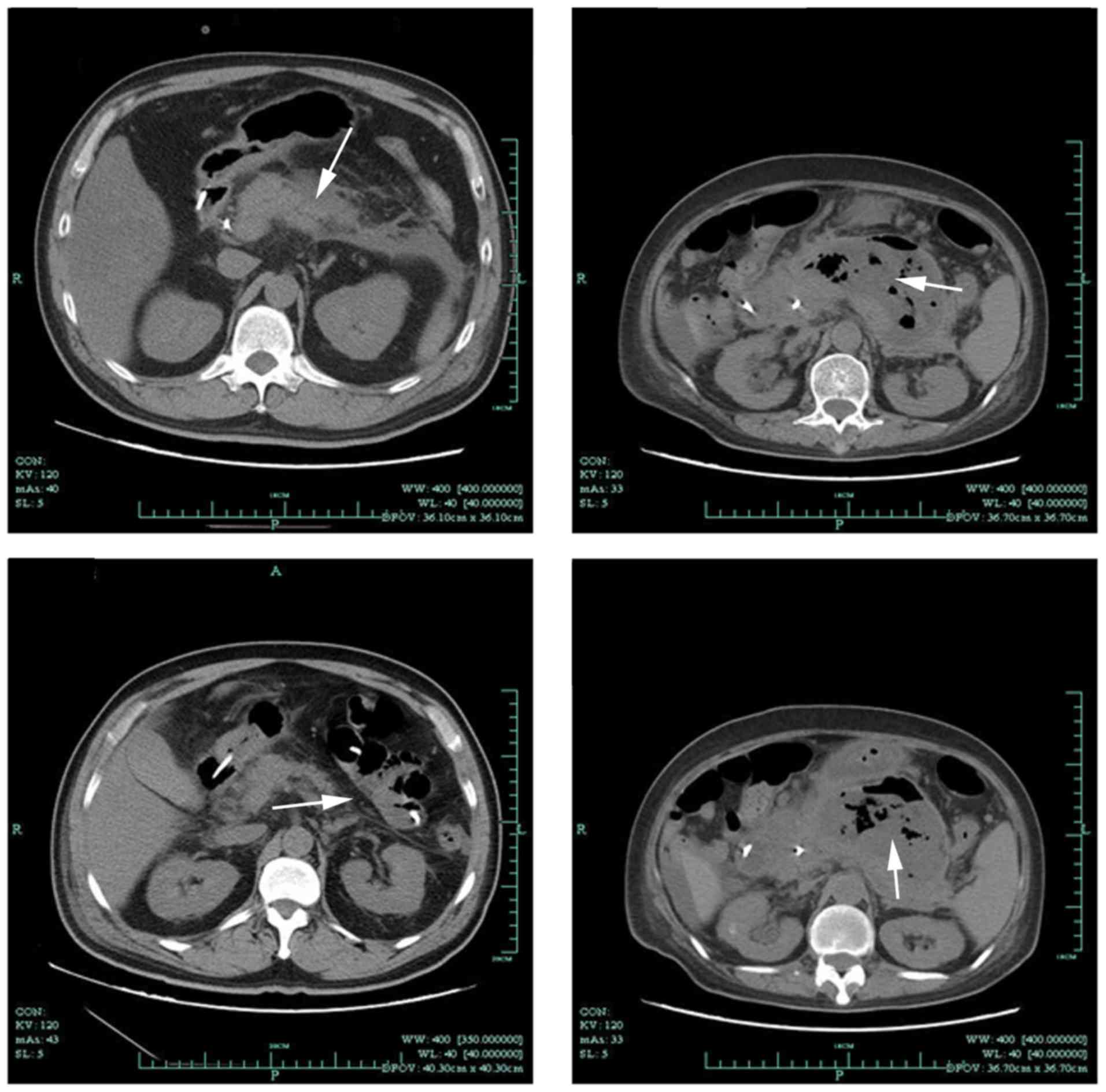
as controls. Computed tomography (CT) images displaying AP status
are presented in Fig. 1. The present
study was approved by the Ethics Committee of Nanjing Medical
University, and written informed consent was obtained from all
patients.
Determination of triglyceride and
serum amylase levels
3 ml venous blood was collected from the subjects
and placed in heparin anticoagulant tubes. Plasma was detected
using an amylase test kit (cat. no. AY7747; Shanghai Zhicheng
Biological Technology Co., Ltd.) and triglyceride test kit (cat.
no. TR7734; Shanghai Zhicheng Biological Technology Co., Ltd.)
using a TBA-120FR automatic biochemical analyzer (Toshiba).
Reverse transcription-quantitative PCR
(RT-qPCR)
Peripheral blood samples were collected from the
patients immediately after admission. Total RNA was extracted from
the serum samples using the TRIzol® method (17), and the purity and integrity of the
RNA was detected by measuring the optical density (OD) at
wavelengths of 260 and 280 nm using an Orion AquaMate 7000 Vis
spectrophotometer (Thermo Fisher Scientific, Inc.). Total RNA was
reverse transcribed to cDNA using TaqMan™ MicroRNA Reverse
Transcription kit (Applied Biosystems' Thermo Fisher Scientific,
Inc.) according to the manufacturer's instructions. cDNA was stored
at -20˚C until further analysis. qPCR was performed using the
PowerUp SYBR Green master mix (Applied Biosystems; Thermo Fisher
Scientific, Inc.) with 1 µl cDNA as the template. The following
thermocycling conditions were used for the qPCR: Initial
denaturation at 95˚C for 10 sec; 39 cycles at 95˚C for 3 min, 95˚C
for 10 sec and 58˚C for 30 sec; and a final extension at
72˚C for 10 min. miRNA levels were quantified using the
2-ΔΔCq method (18) and normalized to the internal
reference gene U6. qPCR was performed in triplicate wells. The
following primer pairs were use for the qPCR: miR-372-RT:
5'-GTCGTATCCAGTGCAGGGTCCGAGGTATTCGCACTGGATACGACAGAATA-3'; U6-RT:
5'-GTCGTATCCAGTGCAGGGTCCGAGGTATTCGCACTGGATACGACAAAATG-3'; miR-372
forward, 5'-GCCCTCAAATGTGGAGCAC-3'; U6 forward,
5'-GCGCGTCGTGAAGCGTTC-3' and universal reverse primer (Sangon
Biotech Co., Ltd.), 5'-GTGCAGGGTCCGAGGT-3'.
Statistical analysis
Data are presented as the mean ± SD. The unpaired
Student's t-test was used to make comparisons between two groups.
One-way ANOVA followed by Tukey's post hoc test was used to make
comparisons between >2 groups. Receiver operating characteristic
(ROC) curves were used to assess the value of miR-372 as a
biomarker, and the area under the curve (AUC) was reported. Pearson
correlation assay demonstrated the level of miR-372 and
triglyceride levels, serum amylase levels. Statistical analyses
were performed using SPSS software (version 20.0; IBM Corp.).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Comparison of general characteristics
between the HTG-MAP group and the HTG-SAP group
There was no significant difference in sex or age
between the HTG-MAP and HTG-SAP groups. The levels of
triacylglycerol in the HTG-SAP group were higher compared with the
HTG-MAP group (Table I). Compared
with the HTG-MAP group, the levels of CRP were significantly
increased in the HTG-SAP group (Table
I). The amylase levels in the HTG-SAP group were significantly
lower compared with the HTG-MAP group (Table I). Increased levels of serum lipase
were also observed in the HTG-SAP group compared with the HTG-MAP
group, but the difference was not significant (Table I). Although the APACHE II scores in
the HTG-SAP group were higher compared with the HTG-MAP group, the
difference was not significant (Table
I).
 | Table IGeneral characteristics of the HTG-MAP
group and the HTG-SAP group. |
Table I
General characteristics of the HTG-MAP
group and the HTG-SAP group.
| Characteristic | HTG-MAP | HTG-SAP | P-value |
|---|
| Sex
(male/female) | 11/9 | 12/8 | 0.821 |
| Age (years) | 41.3±3.5 | 45.6±3.8 | 0.436 |
| Triacylglycerol
(mmol/l) | 10.2±2.7 | 15.9±4.3 | 0.075 |
| CRP (mg/l) | 27.4±21.9 | 139.8±101.3 | 0.015 |
| Amylase (U/l) | 460.5±132.6 | 207.9±45.2 | 0.021 |
| Lipase (U/l) | 1,177.9±675.1 | 1,738.5±1668.4 | 0.085 |
| APACHE II score | 4.5±0.4 | 12.7±1.1 | 0.130 |
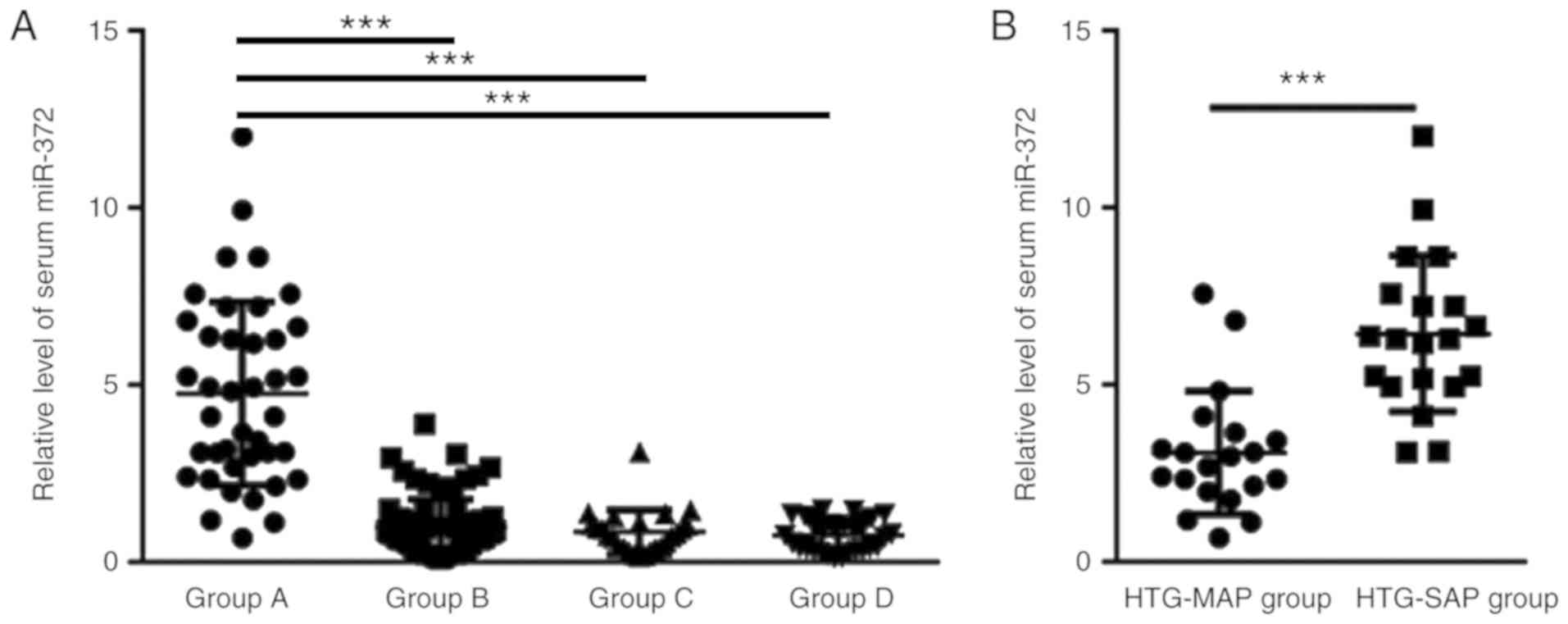
miR-372 expression in the serum of the
four different groups
The level of miR-372 expression in the serum of
group A (4.76±2.60) was significantly higher compared with groups B
(0.98±0.80), C (0.85±0.62) and D (0.76±0.44); however, there was no
significant difference in the expression of miR-372 between groups
B, C and D (Fig. 2A). The level of
serum miR-372 was significantly increased in the HTG-SAP group
(6.45±2.20) compared with the HTG-MAP group (3.08±1.74; Fig. 2B).
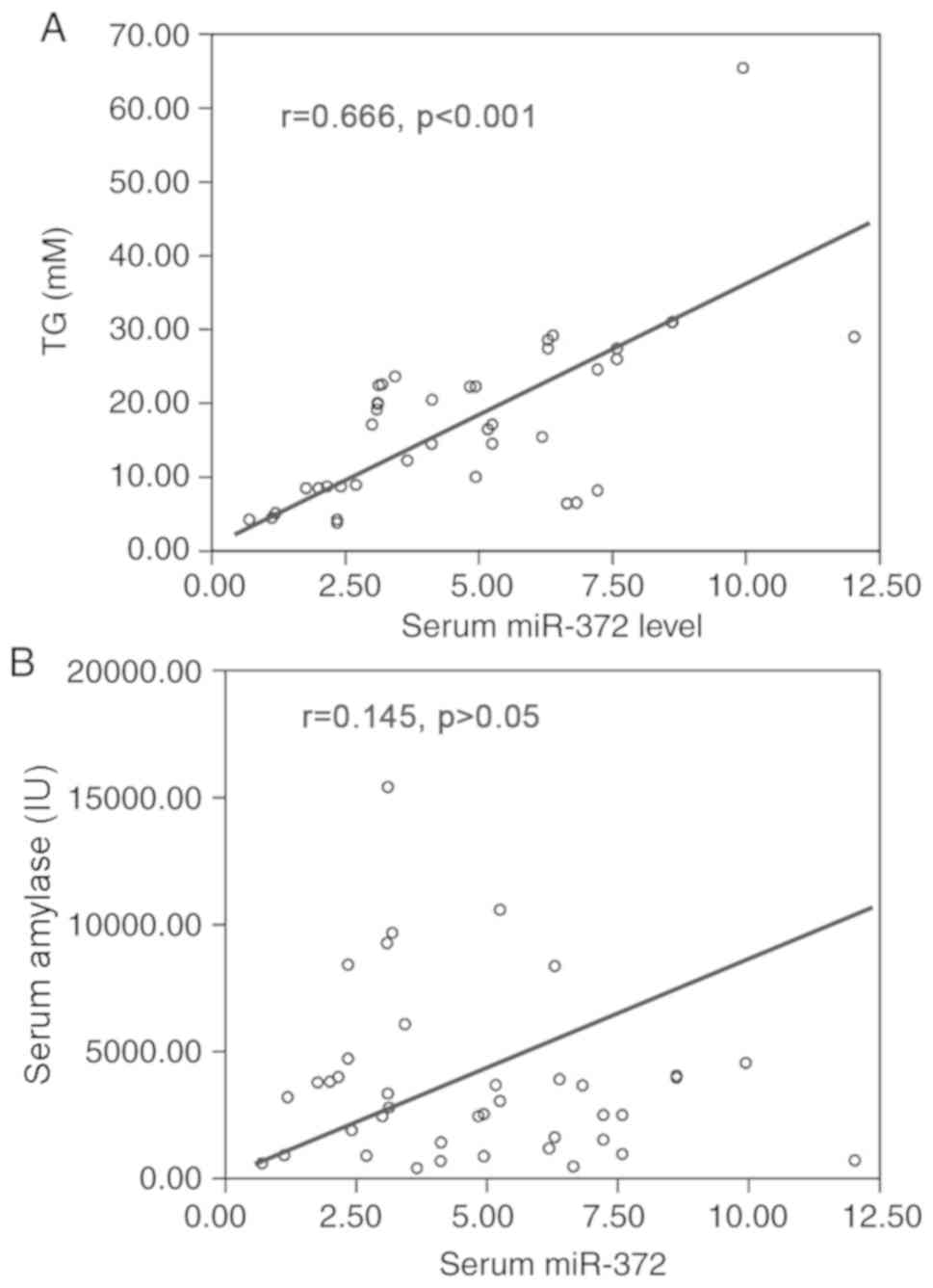
miR-372 expression levels are
positively correlated with triglyceride levels in patients with
HTGAP
The expression of miR-372 was positively correlated
with triglyceride levels (r=0.666; P<0.001), but not with serum
amylase levels in patients with HTGAP (r=-0.145; P>0.05;
Fig. 3A and B).
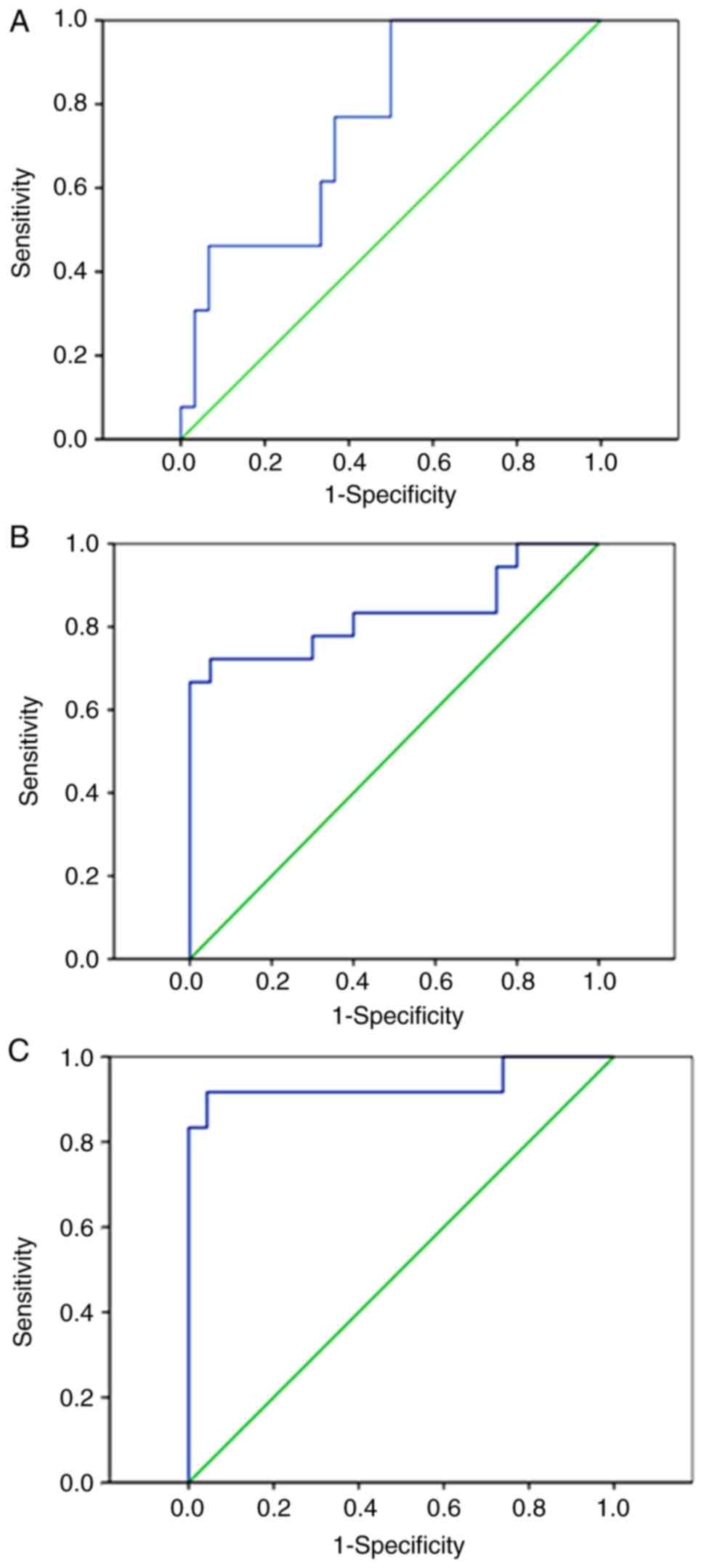
Diagnostic value of miR-372 in
HTGAP
ROC curve analysis suggested that the AUC for APACHE
II scoring, which is used for the diagnosis of HTGAP, was 0.759
with 85.3% sensitivity and 82.1% specificity (Fig. 4A). Furthermore, the miR-372
expression levels for the diagnosis of HTGAP displayed an AUC of
0.831 with 86.7% sensitivity and 79.5% specificity (Fig. 4B). The AUC for the combined use of
the APACHE II scoring system and miR-372 expression levels was
0.935 with 89.5% sensitivity and 87.61% specificity (Fig. 4C).
Discussion
Compared with patients with AP caused by other
factors, including, gallstones and alcohol consumption, patients
with HTGAP are more prone to recurrence, systemic inflammatory
response syndrome (SIRS) and multiple organ failure (MOF), and
display high mortality and poor prognosis (19-21).
At present, the clinical diagnosis of HTGAP primarily relies on
serological and imaging examinations (22,23).
Serological examination is typically based on triacylglycerol and
amylase levels (24); however, since
triacylglycerol often interferes with amylase measurements,
increases in amylase in patients with HTGAP are not obvious, which
makes it easy for the diagnosis of HTGAP to be missed in the clinic
(25,26).
In recent years, a number of studies have reported
that miRs are closely related to the occurrence and development of
AP (11,27); however, the role of miRs in HTGAP has
not been extensively reported. In the present study, RT-qPCR
results suggested that the level of miR-372 in the serum of
patients with HTGAP was significantly increased compared with
patients who did not have HTGAP, indicating that the expression of
miR-372 was abnormally high in patients with HTGAP. Therefore,
abnormally high miR-372 expression may serve as a reference index
for the diagnosis of HTGAP. ROC curve analysis indicated that
miR-372 had diagnostic value for HTG-SAP, with an AUC of 0.831. The
results suggested that miR-372 may serve as a specific marker for
HTGAP, which may provide a novel strategy for the clinical
diagnosis of HTGAP. However, the sample size of the present study
was limited; therefore, further investigation using larger sample
sizes is required to support the use of miR-371 for the clinical
diagnosis of HTGAP.
Early prediction of disease severity is also
important for the treatment and prognostic evaluation of HTGAP
(28), as the progression of HTGAP
is often rapid. Distinguishing HTG-MAP and HTG-SAP is important for
the treatment and control of HTGAP (29). At present, the most common methods
used to predict AP are the APACHE II and Ranson scoring systems
(30). These scores often need to be
evaluated within 24 or 48 h of admission, and involve numerous
steps and a complicated process (30). In the present study, ROC curve
analysis of the APACHE II score and miR-372 expression was
performed, and the AUC was 0.759 and 0.831, respectively. Both
methods displayed good sensitivity and specificity, suggesting that
miR-372 could be used as a predictor of AP severity.
In addition, the present study examined the
correlation between miR-372 expression, and triacylglycerol and
amylase levels. The results suggested that the expression of serum
miR-372 in HTGAP was positively correlated with triacylglycerol
levels, but not with amylase levels. A possible explanation for the
result is that in the hypertriglyceride environment, amylase, which
is the most commonly used indicator of AP, inaccurately appears to
be at normal levels (31).
The present study had a number of limitations.
Firstly, the sample size was relatively small. Secondly, it is
important to include other types of patients to validate the
specificity of abnormal miR-372 expression, since abnormal
expression of serum miR-372 is also present in other diseases.
Thirdly, as a potential biomarker, it is important to evaluate the
combined use of serum miR-372 and existing indicators, which may
improve the specificity of the diagnosis in patients with
HTGAP.
In conclusion, the expression of miR-372 in HTGAP
was significantly upregulated and increased with the severity of
the disease. The results of the present study suggested a novel
strategy for the diagnosis and severity assessment of HTGAP in the
clinic.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Zhejiang
Public Welfare Technology Application Research Project (grant no.
2016C33SA100062).
Availability of data and materials
The datasets used and/or analyzed in the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YS performed the experiments, analyzed the data and
wrote the manuscript. WK, AZ, JZ and RY performed the RT-qPCR
experiments. WZ designed the study, analyzed the data and gave
final approval of the manuscript to be published. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Nanjing Medical University. All patients provided
written informed consent.
Patient consent for publication
All patients provided written informed consent for
the publication of their data in the present study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Brown TT and Prahlow JA: Postmortem serum
amylase and lipase analysis in the diagnosis of acute pancreatitis.
Acad Forensic Pathol. 8:311–323. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cao X, Wang HM, Du H, Chen EX, Yang XF,
Wang SL, Ding Y and She ZF: Early predictors of hyperlipidemic
acute pancreatitis. Exp Ther Med. 16:4232–4238. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Dolay K, Hasbahceci M, Hatipoglu E, Ümit
Malya F and Akçakaya A: Endoscopic diagnosis and treatment of
biliary obstruction due to acute cholangitis and acute pancreatitis
secondary to Fasciola hepatica infection. Ulus Travma Acil Cerrahi
Derg. 24:71–73. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Durmaz MS, Arslan S, Özbakır B, Güngör G,
Tolu İ, Arslan FZ, Sivri M and Koplay M: Effectiveness of Shear
Wave Elastography in the diagnosis of acute pancreatitis on
admission. Med Ultrason. 20:278–284. 2018.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Charlesworth A, Steger A and Crook MA:
Hyperlipidemic acute pancreatitis and the Apolipoprotein E4 allele.
Pancreas. 46:e3–e4. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
French JM, Twedt DC, Rao S and Marolf AJ:
Computed tomographic angiography and ultrasonography in the
diagnosis and evaluation of acute pancreatitis in dogs. J Vet
Intern Med. 33:79–88. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Durval A, Zamidei L, Bettocchi D, Luzzio
MG and Consales G: Hyperlipidemic acute pancreatitis: A possible
role of antiretroviral therapy with entecavir. Minerva Anestesiol.
77:1018–1021. 2011.PubMed/NCBI
|
|
8
|
Noorolyai S, Baghbani E, Aghebati Maleki
L, Baghbanzadeh Kojabad A, Shanehbansdi D, Khaze Shahgoli V,
Mokhtarzadeh A and Baradaran B: Restoration of miR-193a-5p and
miR-146 a-5p expression induces G1 arrest in colorectal cancer
through targeting of MDM2/p53. Adv Pharm Bull. 10:130–134.
2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zhao C, Fei X, Xu B, Lu Y and Zhang Q:
Long non-coding RNA HEIH contributes to diabetic retinopathy by
regulating miR-939/VEGF axis. Int J Clin Exp Pathol. 12:2022–2033.
2019.PubMed/NCBI
|
|
10
|
Lu P, Wang F, Wu J, Wang C, Yan J, Li ZL,
Song JX and Wang JJ: Elevated Serum miR-7, miR-9, miR-122, and
miR-141 are noninvasive biomarkers of acute pancreatitis. Dis
Markers. 2017(7293459)2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Miao B, Qi WJ, Zhang SW and Wang H, Wang
C, Hu L, Huang GW, Li SR and Wang H: miR-148a suppresses autophagy
by down-regulation of IL-6/STAT3 signaling in cerulein-induced
acute pancreatitis. Pancreatology. 19:557–565. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Dixit AK, Sarver AE, Yuan Z, George J,
Barlass U, Cheema H, Sareen A, Banerjee S, Dudeja V, Dawra R, et
al: Comprehensive analysis of microRNA signature of mouse
pancreatic acini: Overexpression of miR-21-3p in acute
pancreatitis. Am J Physiol Gastrointest Liver Physiol.
311:G974–G980. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chen H, Zhang Z, Lu Y, Song K, Liu X, Xia
F and Sun W: Downregulation of ULK1 by microRNA-372 inhibits the
survival of human pancreatic adenocarcinoma cells. Cancer Sci.
108:1811–1819. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Guan X, Zong ZH, Chen S, Sang XB, Wu DD,
Wang LL, Liu Y and Zhao Y: The role of miR-372 in ovarian carcinoma
cell proliferation. Gene. 624:14–20. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Verdelli C, Forno I, Morotti A, Creo P,
Guarnieri V, Scillitani A, Cetani F, Vicentini L, Balza G, Beretta
E, et al: The aberrantly expressed miR-372 partly impairs
sensitivity to apoptosis in parathyroid tumor cells. Endocr Relat
Cancer. 25:761–771. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yuan S, Gao Y, Ji W, Song J and Mei X: The
evaluation of acute physiology and chronic health evaluation II
score, poisoning severity score, sequential organ failure
assessment score combine with lactate to assess the prognosis of
the patients with acute organophosphate pesticide poisoning.
Medicine (Baltimore). 97(e10862)2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wang D, Guo C, Kong T, Mi G, Li J and Sun
Y: Serum miR-22 may be a biomarker for papillary thyroid cancer.
Oncol Lett. 17:3355–3361. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Jagannath S and Garg PK: Recurrent acute
pancreatitis: Current concepts in the diagnosis and management.
Curr Treat Options Gastroenterol. 16:449–465. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Jin DX, Lacson R, Cochon LR, Alper EC,
McNabb-Baltar J, Banks PA and Khorasani R: A clinical model for the
early diagnosis of acute pancreatitis in the emergency department.
Pancreas. 47:871–879. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Hang Y, Chen Y, Lu LX and Zhu CQ: Acute
hyperlipidemic pancreatitis in a pregnant woman. World J Emerg Med.
4:311–313. 2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kaya M, Değirmenci S, Göya C, Tuncel ET,
Uçmak F and Kaplan MA: The importance of acoustic radiation force
impulse (ARFI) elastography in the diagnosis and clinical course of
acute pancreatitis. Turk J Gastroenterol. 29:342–347.
2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Huang YX, Jia L, Jiang SM, Wang SB, Li MX
and Yang BH: Incidence and clinical features of hyperlipidemic
acute pancreatitis from Guangdong, China: A retrospective
multicenter study. Pancreas. 43:548–552. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Lopes CV, Pereira-Lima J and Hartmann AA:
The role of linear endosonography for the diagnosis of acute
pancreatitis when other methods failed. Clin Res Hepatol
Gastroenterol. 43:98–103. 2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Senates E: Toward a new ultrasound-based
imaging method for the diagnosis of acute pancreatitis: A
preliminary study suggesting that it may be feasible. Turk J
Gastroenterol. 29:256–258. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Li MQ, Shi ZX, Xu JY, Lu B, Li JQ, Xu YJ,
Wang XM, Li SM and Mo X: Hemodiafiltration combined with
resin-mediated absorption as a therapy for hyperlipidemic acute
pancreatitis. Cell Biochem Biophys. 69:699–702. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Li X, Lin Z, Wang L, Liu Q, Cao Z, Huang
Z, Zhong M, Peng S, Zhang Y, Li Y and Ma X: RNA-Seq analyses of the
role of miR-21 in acute pancreatitis. Cell Physiol Biochem.
51:2198–2211. 2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Zhang Y, Yan L and Han W: Elevated level
of miR-551b-5p is associated with inflammation and disease
progression in patients with severe acute pancreatitis. Ther Apher
Dial. 22:649–655. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lu J, Xie Y, Du J, Kang M, Jin W, Li Y,
Xie H, Cheng R, Tian R and Wang R: Penta-therapy for severe acute
hyperlipidemic pancreatitis. Am J Emerg Med. 36:1789–1795.
2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Markota A, Knehtl M, Sinkovic A, Ekart R,
Hojs R and Bevc S: Plasma exchange treatment for acute
hyperlipidemic pancreatitis with falsely low levels of serum
triglycerides-a case report. Transfus Apher Sci. 51:178–180.
2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Yang L, Zhao Z, Zhou K and Zhang Y: Acute
hyperlipidemic pancreatitis accompanied by chylous ascites with
normal amylase and lipase in pregnancy. J Clin Lipidol.
11:1091–1094. 2017.PubMed/NCBI View Article : Google Scholar
|