Introduction
Severe burns can be fatal and are associated with
complex and long-term pathological effects known as ‘burn disease’,
which can occur within hours of the incident in question (1). Clinical studies have previously
demonstrated that myocardial damage occurs in the initial stages of
severe burns, with burn areas that cover >30% of the total body
surface area (TBSA) (2,3). In the absence of immediate medical
intervention after severe burn, myocardial injury can lead to
cardiac dysfunction, where potential burn shock can occur,
resulting in impaired circulatory function and possible mortality
(4). Although the precise mechanism
of burn-induced myocardial damage have not been fully elucidated,
accumulating evidence have indicated that myocardial damage
involves a number of processes, including hypoxia, inflammation,
calcium signaling, apoptosis, sepsis and oxidative stress (5-7).
Previous research efforts have focused on the development of novel
therapeutic agents to effectively treat burn injury and reduce
life-threatening burn-induced complications (8).
Radix Puerariae lobatae, also known as Gegen
in Chinese, is the dry root of P. lobata (Willd.) Ohwi.
Radix Puerariae lobatae has been applied therapeutically as
a Traditional Chinese Herbal Medicine or as food for general
consumption in East and Southeast Asian countries, particularly in
ancient China (9). As a result of
the abundant pharmacological properties and mild side effects
exhibited by this plant, Radix Puerariae lobatae has been
extensively used to treat diarrhea, diabetes, cardiac dysfunction,
liver injury, weight loss and toxicosis (10). Puerarin
(4'-7-dihydroxy-8-b-D-glucosylisoflavone) is a major isoflavone
compound that can be found in the root of Radix Puerariae
lobatae (11). Previous studies
have reported puerarin to be beneficial for the treatment of a
number of conditions, including cardiovascular diseases (12), neurological dysfunction (13), diabetes, liver injury (14), osteoporosis (15) and rheumatoid arthritis (16). In addition, puerarin has also been
observed to confer protective effects against inflammation,
hyperlipidemia, metabolic disorders and oxidative damage (10,11,17).
Puerarin can be administered alone or as an adjuvant in combination
with other pharmacological agents (17), in the form of an injectable, tablet
or capsule. In particular, a puerarin injection has been approved
by the State Food and Drug Administration in China for clinical
treatment (e.g., angina pectoris and coronary heart disease)
(18,19).
Puerarin has been previously demonstrated to exert
substantial therapeutic effects against cardiovascular diseases,
including widening of the coronary artery, preservation of arterial
endothelial integrity and myocardial ultrastructure, reduction of
myocardial oxygen consumption, relief of myocardial ischemia and
protection against myocardial ischemic-reperfusion injury (20-23).
Mechanistic studies in animals and clinical settings have revealed
that puerarin may exert cardioprotective effects by inhibiting the
production and release of inflammatory cytokines, preventing
oxidative stress in addition to regulating cardiomyocyte apoptosis
and calcium signaling (24-27).
Although a number of studies have examined the
mechanism underlying the therapeutic effects of puerarin in
cardiovascular diseases, the protective effects of puerarin against
severe burn-induced myocardial injury remain poorly understood.
Therefore, in the present study, in vivo experiments were
performed to investigate the potential protective effects of
puerarin on severe burn-induced myocardial injury and to
characterize the potential mechanisms underlying these effects.
Materials and methods
Animals
In total, 40 adult male Wistar rats (age, 6-8 weeks;
weight, 210-250 g) were purchased from Shanghai SLAC Laboratory
Animal Co., Ltd. (Shanghai, China). All animal experimental
procedures were approved by the Ethics Committee of Gansu
Provincial Hospital (Lanzhou, China), according to the Guide for
the Care and Use of Laboratory Animals, published by the United
States National Institutes of Health (28). The rats were housed at 2-3 rats/cage,
at 23±1˚C with 50% humidity on a 12 h light/dark cycle for ≥7 days
prior to experimental procedures. All the rats were provided
standard food and water ad libitum.
Experimental procedures
Rats were assigned into the following four groups
(n=10 for each group): i) Sham; ii) burn; iii) burn + puerarin (10
mg/kg; (Aladdin Scientific Ltd.), and iv) puerarin (10 mg/kg). All
the rats were anesthetized using pentobarbital (40 mg/kg,
intraperitoneal), following which the fur on the back and upper
sides of the body was removed. The burn model was established in
accordance with that described in a previous study (29). Briefly, the rats were restrained on a
template device, where their naked skin was exposed to water
(100˚C) for 12 sec to produce 30% TBSA full-thickness burns
(30,31). Sham rats and rats in the P group were
immersed in room-temperature water instead of 100˚C. The rats were
then promptly dried following water exposure. For acute
resuscitation, all rats in the S and B groups were
intraperitoneally injected with lactated Ringer's solution (4
ml/kg/TBSA), whereas the BP and P groups were injected with 10
mg/kg/TBSA puerarin dissolved in lactated Ringer's solution
(31) immediately after burn. The
rats were then euthanized with 5% ketamine/xylazine (32), following which blood samples were
collected by retroorbital exsanguination 12 h after burn
treatment.
Measurement of cardiac function
parameters
The right common carotid arteries of the rats were
first separated and exposed. A polyethylene catheter filled with 25
U/l heparin saline was then inserted through the right common
carotid artery into the left ventricle. The end of the catheter was
in turn connected to a physiological signal acquisition system
(model no. RM6240B; Chengdu Instrument Factory) for the acquisition
of data. Following 5 min of calibration, left ventricular systolic
pressure (LVSP) and the maximum rates of increase/decrease in left
ventricular pressure (±dp/dtmax) were measured to
determine cardiac function.
Evaluation of myocardial injury
Serum samples were obtained at 12 h following the
burn procedure and subsequently centrifuged at 2,000 x g for 15 min
at 4˚C. The supernatants were collected and stored at 4˚C until
further use. Myocardial injury was assessed by measuring cardiac
troponin T (cTnT) levels and creatine kinase MB fraction (CK-MB)
activity in the serum. Serum CK-MB activity was analyzed using a
chemistry autoanalyzer (VITROS® 750; Johnson &
Johnson), while cTnT levels were measured using a rat cTnT ELISA
kit (CSB-E16443r; CUSABIO) according to manufacturer's
protocols.
Determination of moisture content in
myocardial tissues
Myocardial moisture content was measured using the
dry/wet weight method. Appropriate amounts (200 mg) of myocardial
tissue were dried using filter paper and weighed, which would be
designated as the wet weight. The tissue samples were then
incubated at 100˚C for 48 h in an electric oven, and weighed using
an electronic balance, which is designated as the dry weight.
Moisture content was then measured using the formula: Moisture
content = (wet weight - dry weight)/wet weight x100%.
Quantification of IL-1β, TNF-α, and
IL-6 level in the serum
Serum levels of interleukin (IL)-1β (cat. no.
ab100767), tumor necrosis factor-α (TNF-α; cat. no. ab46070) and
IL-6 (cat. no. ab234570) were measured using ELISA kits (Abcam)
according to the manufacturer's protocols.
Measurement of myeloperoxidase (MPO)
activity and heart malondialdehyde (MDA) concentration
An appropriate amount of myocardial tissue (50 mg)
was homogenized in reagent II of the myeloperoxidase assay kit
(cat. no. A044-1-1; weight:volume ratio, 1:19). Myocardial MPO
activity was measured according to the manufacturer's protocols
(Nanjing Jiancheng Bioengineering Institute). One unit of MPO (U/g)
was defined as the amount of MPO required to degrade 1 µM
peroxide/g wet heart tissue at 37˚C.
MDA content was determined using the thiobarbituric
method in myocardial tissue homogenates. The myocardial tissue was
homogenized in reagent II at a weight: volume ratio of myocardial
tissue and reagent II of 1:9. Tissue homogenates were centrifuged
at 700 x g for 30 min at 4˚C, following which the supernatants were
collected for analysis using a malondialdehyde (MDA) assay kit
(cat. no. A003-1-2) according to manufacturer's protocols (Nanjing
Jiancheng Bioengineering Institute). Biuret method was used to
minimize protein interference and correct for protein content. MDA
content was reported as nmol/mg protein.
TUNEL apoptosis assay
Myocardial tissues (20 mg) from the right ventricle
was first fixed with 4% paraformaldehyde for 12 h at 4˚C, following
which the tissue was embedded in paraffin wax and cut into 5 µm
sections for plating. TUNEL staining was performed according to
manufacturer's protocols of the TUNEL Assay Kit-HRP-DAB (cat. no.
ab206386; Abcam). The rehydration and specimen were performed with
xylene and ethanol before the permeabilization with 1% proteinase K
at room temperature for 20 min. The endogenous peroxidases were
inactivated by incubating in 3% H2O2 at room
temperature for 5 min. Then labeling reaction was performed by
incubating with TdT Labeling Reaction Mix at 37˚C for 1.5 h after
incubating the specimens in TdT Equilibration buffer at room
temperature for 30 min. The specimens were detected by incubating
with 1X Conjugate at room temperature for 30 min and developed by
incubating with working DAB solution at room temperature for 15 min
after termination of labeling reaction and blocking. All reaction
mixes, buffers, conjugates and solutions were included in the TUNEL
Assay kit. Finally, nuclei were stained with hematoxylin (cat. no.
G1140; Beijing Solarbio Science & Technology Co., Ltd.) at room
temperature for 10 min and the specimen were mounted by neutral
balsam (cat. no. 822941; MACKLIN) on glass slides. The number of
total cardiomyocytes and apoptotic cardiomyocytes were counted from
10 randomly selected non-overlapping fields of view under a light
microscopy (magnification, x400) per condition. The percentage of
apoptotic cardiomyocytes was calculated using the formula: %
apoptotic cardiomyocytes = number of apoptotic cardiomyocytes/total
number of cardiomyocytes x100%.
Western blotting
Myocardial tissue was homogenized in RIPA buffer
(cat. no. R0020; Solarbio) containing 1% PMSF (Solarbio), which
were then centrifuged at 12,000 x g for 5 min at 4˚C. Protein
concentration was quantified using bicinchoninic acid protein assay
(Pierce; Thermo Fisher Scientific, Inc.) and was adjusted to 5
µg/µl using lysis buffer. A total of 10 µg protein was
loaded per lane for SDS-PAGE, electrophoresis was then performed by
10% SDS-PAGE to separate the protein extracts. The separated
proteins were subsequently transferred to PVDF membranes (EMD
Millipore) and blocked for 1 h at room temperature in TBS
supplemented with 0.05% Tween-20 (TBST) containing 5% non-fat milk.
The membranes were then incubated with primary antibodies against
cleaved caspase-3 (dilution: 1:1,000; cat. no. ab49822; Abcam), p38
(dilution: 1:5,000; cat. no. ab170099; Abcam), phosphorylated
(p)-p38 (dilution: 1:1,000; cat. no. ab47363; Abcam), JNK
(dilution: 1:5,000; cat. no. ab199380; Abcam), p-JNK (dilution:
1:2,000; cat. no. ab47337; Abcam), Akt (dilution: 1:10,000; cat.
no. ab179463; Abcam), p-Akt (dilution: 1:1,000; cat. no. ab192623;
Abcam), ERK (dilution: 1:1,000; cat. no. AF1576; R&D Systems,
Inc.), p-ERK (dilution: 1:1000; cat. no. AF1018; R&D Systems,
Inc.) overnight at 4˚C. Following washing in TBST three times, the
membranes were incubated with horseradish peroxidase-conjugated
secondary antibodies (dilution: 1:1,000; cat. no. HAF008; R&D
Systems, Inc.) at room temperature for 1 h. Protein bands were
visualized using an ECL Western Blotting Detection Reagent (GE
Healthcare Life Sciences). Densitometric analysis was performed
using ImageJ software, version 1.41 (National Institutes of
Health), which was normalized further to the loading control
.β-actin.
Statistical analysis
All values are presented as the mean ± standard
error of the mean. Statistical analyses were performed using
GraphPad Prism version 6.0 (GraphPad Software, Inc.). Statistical
differences between the groups were analyzed by one-way analysis of
variance with Bonferroni's correction or Student's t-test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
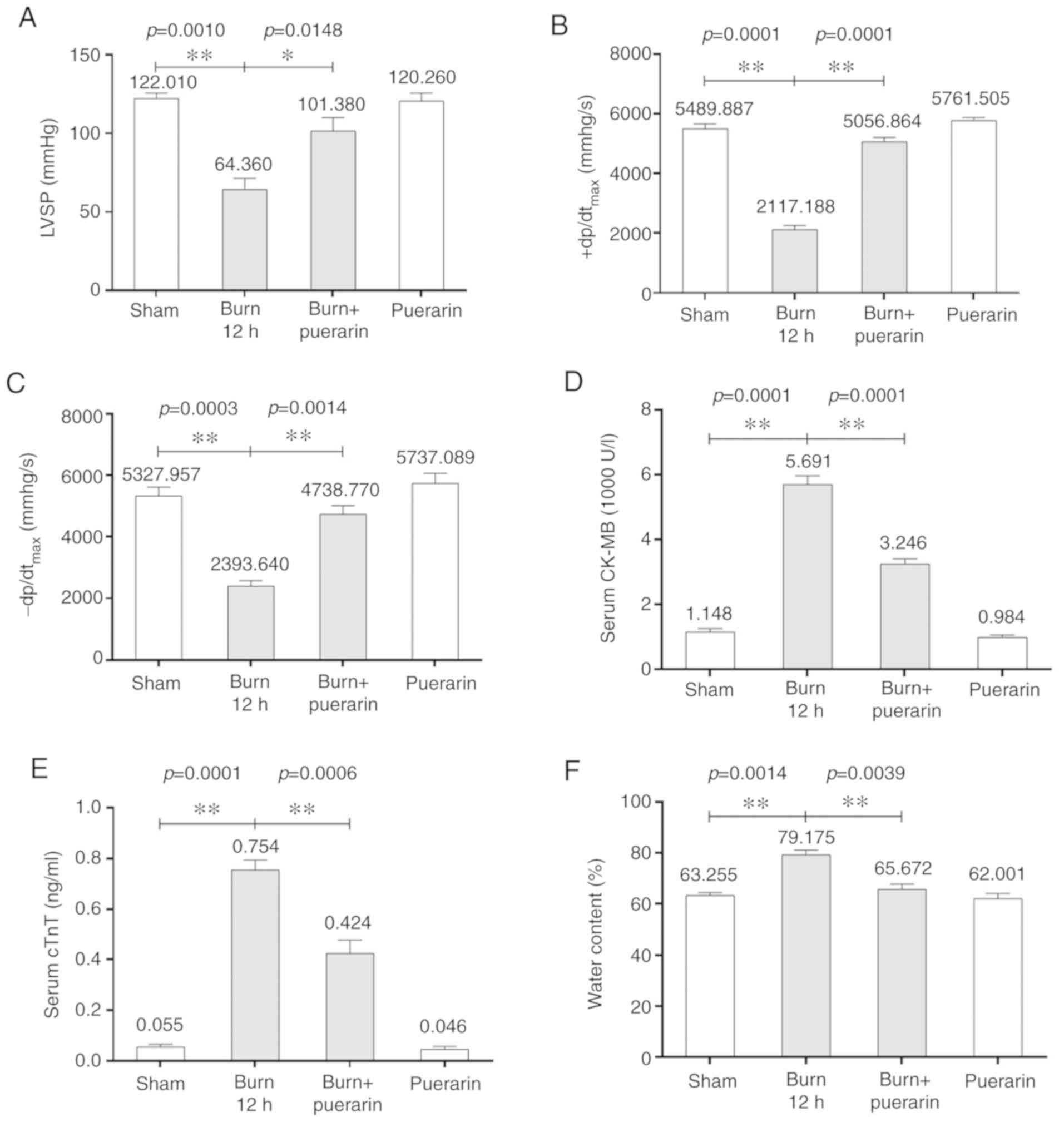
Puerarin relieves severe burn-induced
myocardial injury
To evaluate the effects of puerarin treatment on
burn-induced myocardial injury, the rats first underwent a 30% TBSA
full-thickness burns, following which hemodynamic parameters and
indices of myocardial injury were measured 12 h post-injury. LVSP,
which represents left ventricle contractile function, was
significantly lower in the burn group 12 h post-burn compared with
that in the sham group (Fig. 1A).
Similarly, the ±dp/dtmax in the burn group were also
significantly lower compared with those in the sham control
(Fig. 1B and C). Puerarin treatment significantly
reversed cardiac dysfunction in the burn + puerarin group, as
evidenced by the significant higher LVSP and ±dp/dtmax
in the burn + puerarin group compared with those in the burn group
(Fig. 1A-C).
CK-MB activity and serum cTnT levels were
subsequently measured as indices of myocardial injury. In the burn
group, serum CK-MB activity was significantly higher compared with
that in the sham group (Fig. 1D). In
addition, serum CK-MB activity in rats in the burn + puerarin group
was significantly lower compared with that in the burn group 12 h
following the burning procedure (Fig.
1D). Within the same timeframe, serum cTnT levels of rats in in
the burn group were significantly higher compared with that in the
sham group (Fig. 1E). Rats in the
burn + puerarin group exhibited significantly lower serum cTnT
compared with that in the burn group (Fig. 1E).
Edema in myocardial tissue in the burn group was
found to be significantly higher compared with that in the sham
group (Fig. 1F), whereas that in the
burn + puerarin group was significantly lower compared with that in
the burn group (Fig. 1F).
Interestingly, no differences were observed in any
of the aforementioned parameters between the sham and puerarin only
groups, suggesting that puerarin treatment did not produce adverse
effects in animals that did not receive severe burns.
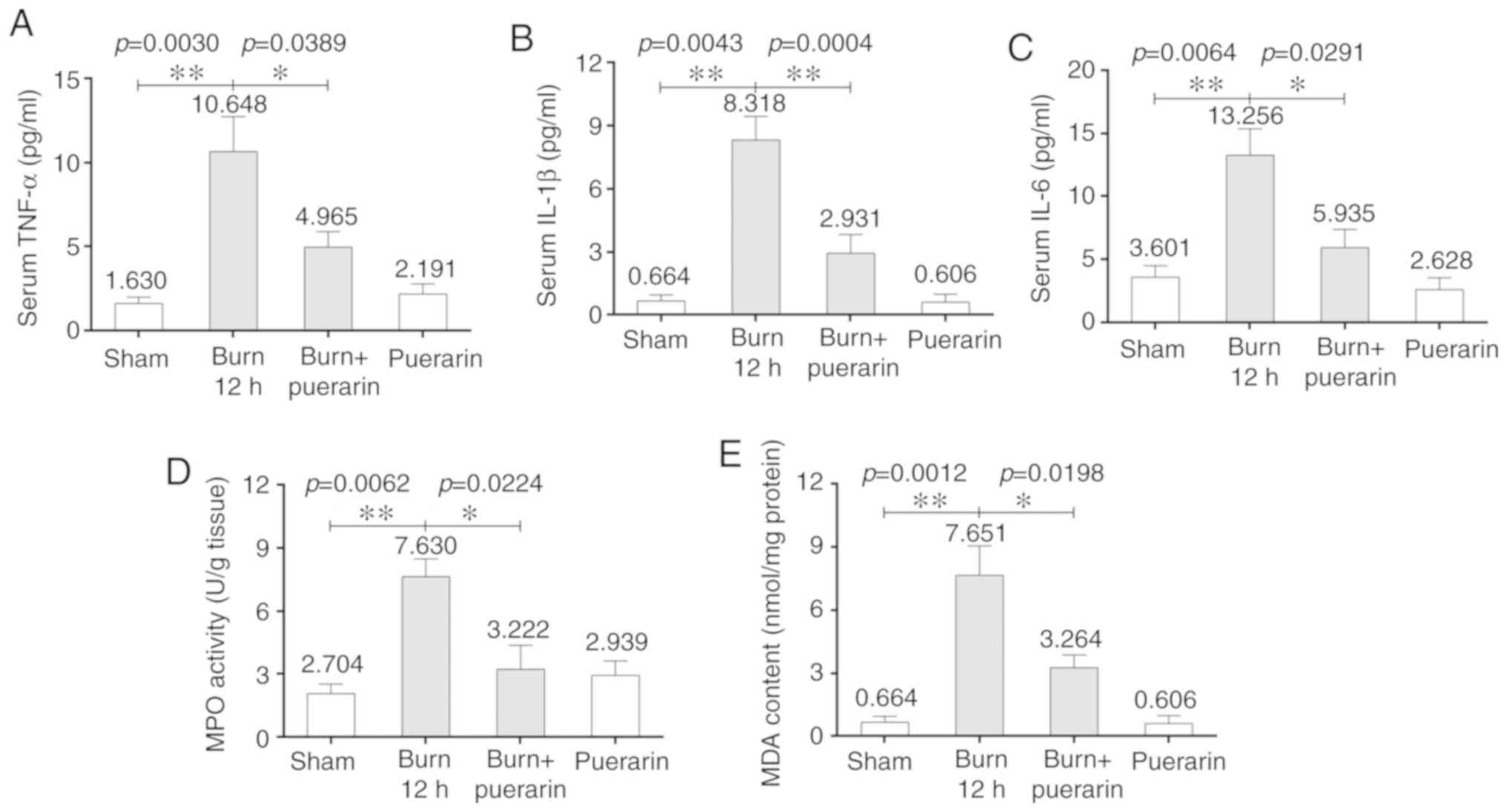
Puerarin alleviates cardiac
inflammation and oxidative stress caused by severe burn injury
Inflammatory cytokines have been previously
demonstrated to contribute to the pathogenesis of severe
burn-induced myocardial injury, which can be alleviated puerarin
treatment (2,33-35).
To investigate the effect of puerarin on burn-induced acute
inflammation, serum levels of inflammatory cytokines IL-6, IL-1β
and TNF-α were measured. Serum levels of IL-6, IL-1β and TNF-α in
rats in the burn group were significantly higher compared with
those in the sham group 12 h post-burn (Fig. 2A-C). Rats in the burn + puerarin
group exhibited significantly lower serum levels of IL-6, IL-1β and
TNF-α compared with those in the burn group (Fig. 2A-C).
MPO activity was subsequently measured to evaluate
neutrophil accumulation in the heart tissues. Compared with the
sham group, MPO activity in myocardial issues from the burn group
was found to be significantly higher 12 h post-burn compared with
that in the Sham group (Fig. 2D).
Myocardial tissues isolated from rats in the burn + puerarin group
exhibited significantly lower MPO activity compared with those from
the burn group (Fig. 2D).
Tissue MDA accumulation is considered an indicator
of oxidative stress and lipid peroxidation (36). To determine the effects of puerarin
on burn-induced oxidative stress, the concentration of MDA was
measured in myocardial tissues isolated from rats from each
treatment group. MDA levels were found to be significantly higher
in tissues isolated from rats in the burn group compared with those
in the sham group 12 h after the burn procedure (Fig. 2E). By contrast, tissues from rats in
the burn + puerarin group demonstrated significantly lower MDA
levels compared with those in the burn group (Fig. 2E).
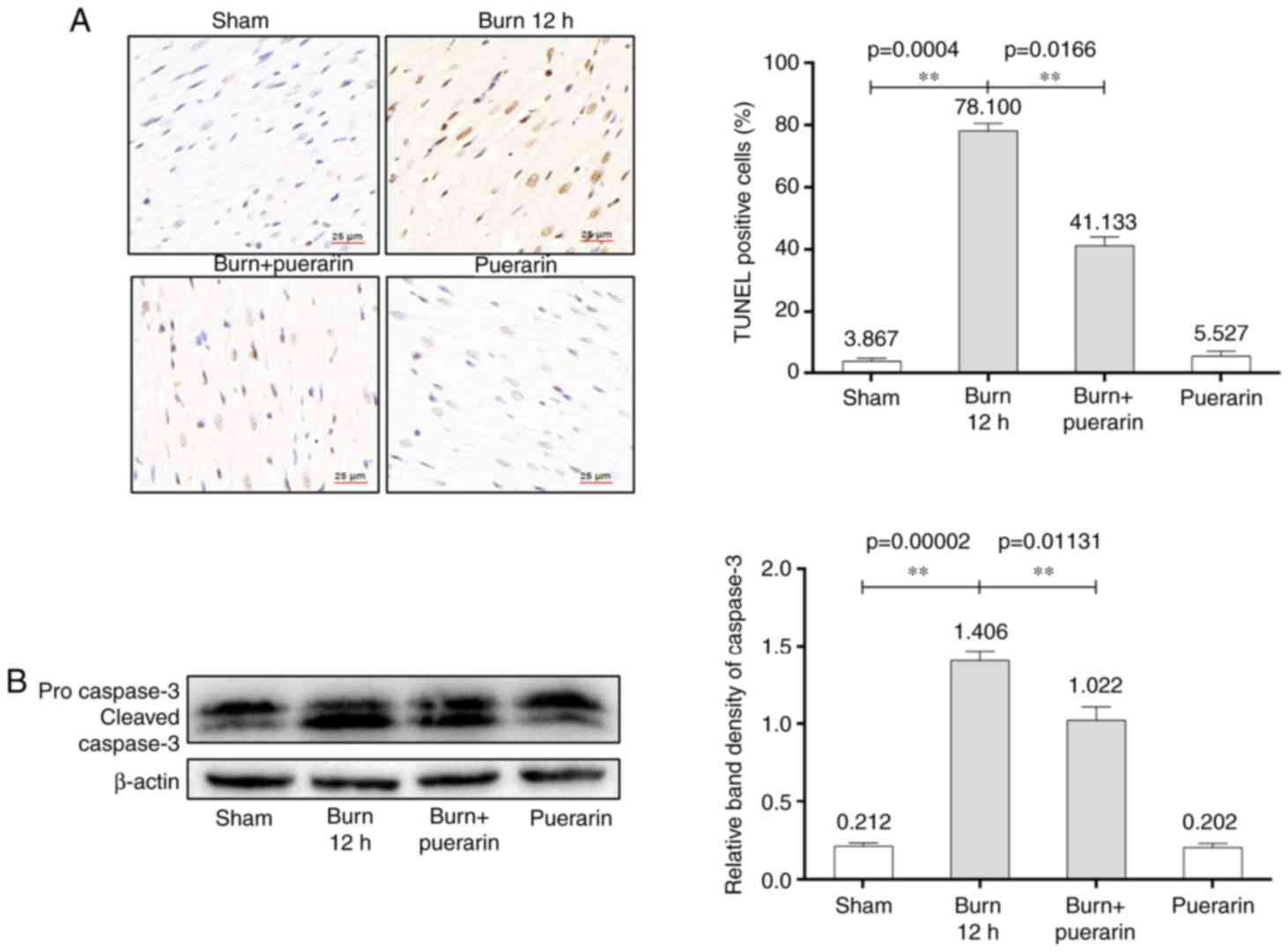
Puerarin attenuates severe
burn-induced cardiomyocyte apoptosis
Cardiomyocyte apoptosis typically occurs within
hours of burn injury, where previous studies have demonstrated that
increased apoptotic rates may affect cardiac function (37). To evaluate the effect of puerarin on
cardiac apoptosis, TUNEL staining was performed of myocardial
tissue slices isolated from rats in each treatment group.
Myocardial cell death was found to be significantly higher in the
burn group compared with that in the sham group (Fig. 3A). Tissues isolated from rats in the
burn + puerarin group demonstrated significantly reduced
cardiomyocyte apoptosis compared with that in the burn group.
Protein levels of cleaved caspase-3, a marker of apoptosis, was
also revealed to be significantly increased in myocardial tissues
isolated from rats in the burn group 12 h after burn injury
compared with those in the Sham group (Fig. 3B). Cleaved caspase-3 levels were
lower in the burn + puerarin group compared with that in the burn
group (Fig. 3B).
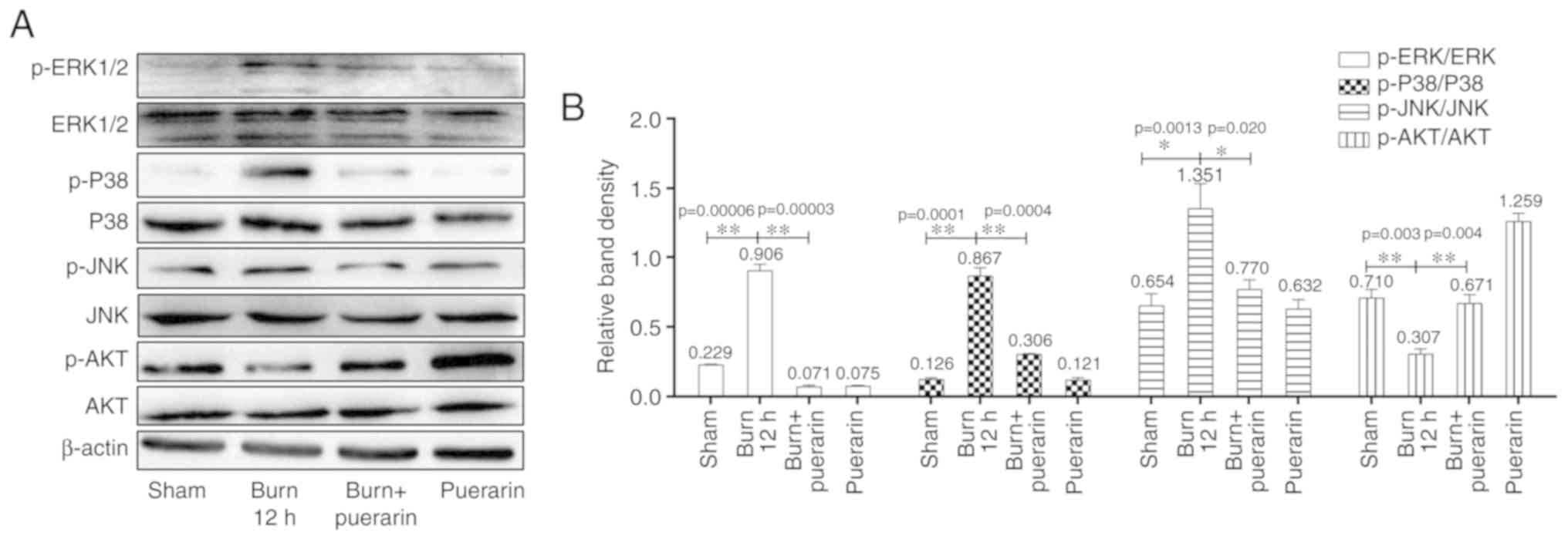
Puerarin attenuates burn-induced MAPK
and Akt activation
Although data presented in the present study
provided evidence for the protective effects of puerarin against
myocardial injury as a result of severe burn, the mechanism
underlying the protective effects of puerarin remains poorly
characterized. Since previous studies have demonstrated that burn
injury promoted apoptotic signaling through the inhibition of Akt
and activation of p38-MAPK (38,39), The
effects of puerarin treatment on MAPK and Akt activation following
burn-induced cardiomyocyte injury was next evaluated.
Phosphorylation levels of p38, ERK and JNK were found to be
significantly higher in the burn group compared with those in the
Sham group at 12 h post-injury, whilst the opposite was observed in
terms of Akt phosphorylation (Fig.
4). p38, ERK and JNK phosphorylation were found to be
significantly lower in the burn + puerarin group compared with
those in the burn group; but the opposite was observed for Akt
phosphorylation (Fig. 4).
Discussion
Recent clinical and animal studies have demonstrated
that myocardial damage occurs in the early stages of severe burns
(2,40). Myocardial injury results in cardiac
dysfunction, which aggravates ischemic and hypoxic damage in other
tissues and organs (3,4). Therefore, early intervention in
preventing burn-induced myocardial injury has become a significant
focus in previous studies. Puerarin, one of the major bioactive
components found in Radix Puerariae lobatae, a traditional
Chinese herb, has been historically applied therapeutically for
cardiovascular disease (17,21). However, the potential therapeutic
effects of puerarin on severe burn-induced myocardial damage have
yet to be fully elucidated.
Although the present study and a previous study
performed by Liu et al (31)
investigated the therapeutic effects of puerarin on rat myocardial
injury as a result of burn, differences exist. In addition to the
sham, burn and burn + puerarin groups, a puerarin only group was
included into the present study. The present study also included
IL-1β and IL-6 measurements, which reflected myocardial
inflammation. LVSP, ±dp/dtmax and water content of the
heart were measured to analyze myocardial function. Finally, the
protein levels of cleaved caspase-3, ERK, p-ERK, JNK, p-JNK, Akt
and p-Akt, key components of the MAPK and Akt signal pathways, were
analyzed further to elucidate the mechanism underlying myocardial
injury formation. However, the full-thickness burn was not
demonstrated in this study, which serves as a limitation of the
present study.
LVSP and dp/dtmax, which directly reflect
cardiac function, were significantly reduced 12 h after severe
burn, suggesting that rats suffered from reduced myocardial
contractility, heart rate, left ventricular systolic and diastolic
function. Puerarin treatment effectively reversed the
aforementioned effects on cardiac function, suggesting that
myocardial injury was mitigated. Serum CK-MB activity and cTnT
levels, which served as indicators of myocardial damage in the
present study, were found to be increased by severe burns, which
was reversed by puerarin treatment. These findings suggest that
puerarin alleviated acute myocardial damage induced by severe burns
in rats.
MPO is a major producer of ROS which promotes
endothelial dysfunction through oxidation of low-density
lipoprotein (OxLDL) (41). Elevated
circulating MPO levels are associated with coronary artery disease
(CAD) (42). Puerarin has been
previously reported to exhibit antioxidant effects, resulting in
reduced neutrophil infiltration and MPO activity in the heart
(31). MPO-induced OxLDL
peroxidation can result in reduced nitric oxide (NO)
bioavailability, thereby weakening vasodilation and promotion of a
pro-inflammatory state (43).
Previous studies have shown that high MPO levels are associated
with increased risks of cardiovascular events (44). Additionally, elevation in MPO levels
as a result of leukocyte activation was negatively correlated with
the tissue availability and microvascular permeability index of
constitutive nitric oxide synthase (cNOS) (45). In the present study, myocardial MPO
activity was significantly increased following severe burn. This
observation was associated positively with burn-induced changes in
serum CK-MB activity and cTnT levels, which were reversed by
puerarin treatment.
Severe burn has been previously demonstrated to
substantially increase proinflammatory cytokine production
(46-48).
The present study showed that severe burn significantly increased
levels of IL-1β, IL-6 and TNF-α in the serum. Consistent with
previous studies, puerarin treatment reversed the burn-induced
increases in IL-6, IL-1β and TNF-α production. TNF-α is a
multifunctional cytokine in myocardial cells, which can inhibit
myocardial cell contraction and inhibit cAMP signaling (49). In addition to its role in
inflammation, TNF-α also serves a critical role in microvascular
and cardiac damage by inducing the adherence of neutrophils to the
endothelium (50). In this study,
MPO activity directly reflects neutrophil sequestration in heart
tissue, which was significantly increased in response to severe
burn and reversed by puerarin treatment (Fig. 2F), same as in the previous study
(51). These results suggested that
the cardioprotective effects of puerarin following severe burns
were associated with the inhibition of TNF-α production and
neutrophil infiltration.
Burn injury results in the mitochondrial release of
an apoptotic factors, which is associated with the pathogenesis of
myocardial injury (52). Cleavage of
caspase-3 is a key step in the regulation of apoptotic DNA
fragmentation (53). Caspase-3
activation induces edema, which can be inhibited by puerarin
(54). p38-MAPK has been previously
shown to mediate oxidative stress-dependent apoptosis in neurons
and cardiac cells (55,56). By contrast, the PI3K-Akt pathway is
known to inhibit apoptosis in response to extracellular signals
through transcriptional regulation or direct phosphorylation.
Previous studies showed that burn injury promoted apoptosis by
inhibiting of Akt activation while activating p38-MAPK signaling
(38,39). Suppression of apoptosis through the
inhibition of p38-MAPK signaling can reduce TNF-α expression and
oxidative stress following burn injury in the current study. These
findings suggest that puerarin can inhibit burn-induced oxidative
stress, cardiac edema and apoptosis by modulating the MAPK and Akt
signaling pathways.
In conclusion, puerarin was demonstrated to exert
protective effects against burn-induced cardiac dysfunction by
attenuating inflammation, oxidative stress and myocardial
apoptosis. The protective effects of puerarin are likely to be
mediated through Akt activation and concomitant p38-MAPK
inhibition.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
JuL and JiL made significant contributions to data
acquisition, data analysis and the manuscript draft. MB and HW
conducted data interpretation. JiL conceived and designed the study
and revised the manuscript critically for important intellectual
content. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
All animal experiments were approved by the Ethics
Committee of Gansu Provincial Hospital (Lanzhou, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Soussi S, Dépret F, Benyamina M and
Legrand M: Early Hemodynamic Management of Critically Ill Burn
Patients. Anesthesiology. 129:583–589. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Guillory AN, Clayton RP, Herndon DN and
Finnerty CC: Cardiovascular Dysfunction Following Burn Injury: What
We Have Learned from Rat and Mouse Models. Int J Mol Sci.
17(53)2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Horton JW, Maass DL, White DJ, Sanders B
and Murphy J: Effects of burn serum on myocardial inflammation and
function. Shock. 22:438–445. 2004.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fozzard HA: Myocardial injury in burn
shock. Ann Surg. 154:113–119. 1961.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhang DX, Yan H, Hu JY, Zhang JP, Teng M,
Tong DL, Xiang F, Zhang Q, Fang YD, Liang GP, et al: Identification
of mitochondria translation elongation factor Tu as a contributor
to oxidative damage of postburn myocardium. J Proteomics.
77:469–479. 2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Meldrum DR, Wang M, Tsai BM, Kher A,
Pitcher JM, Brown JW and Meldrum KK: Intracellular signaling
mechanisms of sex hormones in acute myocardial inflammation and
injury. Front Biosci. 10:1835–1867. 2005.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Horton JW, Maass DL and Ballard-Croft C:
Rho-associated kinase modulates myocardial inflammatory cytokine
responses. Shock. 24:53–58. 2005.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhang Z, Zhang Y, Deng Y, Li S, Zhou W,
Yang C, Xu X and Li T: Polymerized human placenta haemoglobin
attenuates myocardial injury and aortic endothelial dysfunction in
a rat model of severe burns. Artif Cells Nanomed Biotechnol.
46:1141–1145. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Prasain JK, Jones K, Kirk M, Wilson L,
Smith-Johnson M, Weaver C and Barnes S: Profiling and
quantification of isoflavonoids in kudzu dietary supplements by
high-performance liquid chromatography and electrospray ionization
tandem mass spectrometry. J Agric Food Chem. 51:4213–4218.
2003.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wong KH, Li GQ, Li KM, Razmovski-Naumovski
V and Chan K: Kudzu root: Traditional uses and potential medicinal
benefits in diabetes and cardiovascular diseases. J Ethnopharmacol.
134:584–607. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yan LP, Chan SW, Chan AS, Chen SL, Ma XJ
and Xu HX: Puerarin decreases serum total cholesterol and enhances
thoracic aorta endothelial nitric oxide synthase expression in
diet-induced hypercholesterolemic rats. Life Sci. 79:324–330.
2006.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Pan ZY, Bao ZS, Wu ZM, Wang XM, Zheng JZ,
Shen YL and Zhang XM: The myocardial protective effects of puerarin
on STZ-induced diabetic rats. Fen Zi Xi Bao Sheng Wu Xue Bao.
42:137–144. 2009.PubMed/NCBI
|
|
13
|
Lin F, Xie B, Cai F and Wu G: Protective
effect of Puerarin on β-amyloid-induced neurotoxicity in rat
hippocampal neurons. Arzneimittelforschung. 62:187–193.
2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Zhao M, Du YQ, Yuan L and Wang NN:
Protective effect of puerarin on acute alcoholic liver injury. Am J
Chin Med. 38:241–249. 2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wong R and Rabie B: Effect of puerarin on
bone formation. Osteoarthritis Cartilage. 15:894–899.
2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Xiao C, Li J, Dong X, et al:
Anti-oxidative and TNF-alpha suppressive activities of puerarin
derivative (4AC) in RAW264.7 cells and collagen-induced arthritic
rats. Eur J Pharmacol. 666:242–250. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zhou YX, Zhang H and Peng C: Puerarin: a
review of pharmacological effects. Phytother Res. 28:961–975.
2014.PubMed/NCBI View
Article : Google Scholar
|
|
18
|
Hwang YP and Jeong HG: Mechanism of
phytoestrogen puerarin-mediated cytoprotection following oxidative
injury: Estrogen receptor-dependent up-regulation of PI3K/Akt and
HO-1. Toxicol Appl Pharmacol. 233:371–381. 2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Hou SZ, Su ZR, Chen SX, Ye MR, Huang S,
Liu L, Zhou H and Lai XP: Role of the interaction between puerarin
and the erythrocyte membrane in puerarin-induced hemolysis. Chem
Biol Interact. 192:184–192. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Xiao LZ, Gao LJ and Ma SC: Comparative
study on effects of puerarin and granulocyte colony-stimulating
factor in treating acute myocardial infarction. Zhongguo Zhong Xi
Yi Jie He Za Zhi. 25(210)2005.(In Chinese). PubMed/NCBI
|
|
21
|
Fan LL, Sun LH, Li J, Yue XH, Yu HX and
Wang SY: The protective effect of puerarin against myocardial
reperfusion injury. Study on cardiac function. Chin Med J (Engl).
105:11–17. 1992.PubMed/NCBI
|
|
22
|
Wu L, Qiao H, Li Y and Li L: Protective
roles of puerarin and Danshensu on acute ischemic myocardial injury
in rats. Phytomedicine. 14:652–658. 2007.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Feng ZQ, Wang YY, Guo ZR, Chu FM and Sun
PY: The synthesis of puerarin derivatives and their protective
effect on the myocardial ischemia and reperfusion injury. J Asian
Nat Prod Res. 12:843–850. 2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sun XH, Ding JP, Li H, Pan N, Gan L, Yang
XL and Xu HB: Activation of large-conductance calcium-activated
potassium channels by puerarin: The underlying mechanism of
puerarin-mediated vasodilation. J Pharmacol Exp Ther. 323:391–397.
2007.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wattanapitayakul SK and Bauer JA:
Oxidative pathways in cardiovascular disease: Roles, mechanisms,
and therapeutic implications. Pharmacol Ther. 89:187–206.
2001.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Yuan Y, Zong J, Zhou H, Bian ZY, Deng W,
Dai J, Gan HW, Yang Z, Li H and Tang QZ: Puerarin attenuates
pressure overload-induced cardiac hypertrophy. J Cardiol. 63:73–81.
2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Gao L, Ji X, Song J, Liu P, Yan F, Gong W,
Dang S and Luo Y: Puerarin protects against ischemic brain injury
in a rat model of transient focal ischemia. Neurol Res. 31:402–406.
2009.PubMed/NCBI View Article : Google Scholar
|
|
28
|
National Research Council (US) Institute
for Laboratory Animal Research. Guide for the Care and Use of
Laboratory Animals. National Academies Press (US), Washington, DC.
1996.PubMed/NCBI
|
|
29
|
Korompai FL and Yuan SY: Ventral burn in
rats: An experimental model for intravital microscopic study of
microcirculation. Burns. 28:321–327. 2002.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Hernekamp JF, Hu S, Schmidt K, Walther A,
Lehnhardt M and Kremer T: Methysergide attenuates systemic burn
edema in rats. Microvasc Res. 89:115–121. 2013.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Liu S, Ren HB, Chen XL, Wang F, Wang RS,
Zhou B, Wang C, Sun YX and Wang YJ: Puerarin attenuates severe
burn-induced acute myocardial injury in rats. Burns. 41:1748–1757.
2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Matos VSB, Gomes FDS, Oliveira TM, Schulz
RDS, Ribeiro LCV, Gonzales ADF, Lima JM and Guerreiro MLDS: Effects
of emissions from sugar cane burning on the trachea and lungs of
Wistar rats. J Bras Pneumol. 43:208–214. 2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Yao X, Wigginton JG, Maass DL, Ma L,
Carlson D, Wolf SE, Minei JP and Zang QS: Estrogen-provided cardiac
protection following burn trauma is mediated through a reduction in
mitochondria-derived DAMPs. Am J Physiol Heart Circ Physiol.
306(H882-H894)2014.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Wang J, Zhang T, Ma C and Wang S: Puerarin
attenuates airway inflammation by regulation of eotaxin-3. Immunol
Lett. 163:173–178. 2015.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Liu CM, Ma JQ, Liu SS, Feng ZJ and Wang
AM: Puerarin protects mouse liver against nickel-induced oxidative
stress and inflammation associated with the TLR4/p38/CREB pathway.
Chem Biol Interact. 243:29–34. 2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
França LFC, Vasconcelos ACCG, da Silva
FRP, Alves EHP, Carvalho JS, Lenardo DD, de Souza LKM, Barbosa ALR,
Medeiros JR, de Oliveira JS, et al: Periodontitis changes renal
structures by oxidative stress and lipid peroxidation. J Clin
Periodontol. 44:568–576. 2017.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Zhang JP, Ying X, Liang WY, Luo ZH, Yang
ZC, Huang YS and Wang WC: Apoptosis in cardiac myocytes during the
early stage after severe burn. J Trauma. 65:401–408; discussion
408. 2008.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Lv GF, Dong ML, Hu DH, Zhang WF, Wang YC,
Tang CW and Zhu XX: Insulin-mediated inhibition of p38
mitogen-activated protein kinase protects cardiomyocytes in severe
burns. J Burn Care Res. 32:591–599. 2011.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Huang Y, Zheng J, Fan P and Zhang X:
Transfection of antisense p38 alpha gene ameliorates myocardial
cell injury mediated by hypoxia and burn serum. Burns. 33:599–605.
2007.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Huang YS: Autophagy and hypoxic ischemic
myocardial damage after severe burn. Zhonghua Shao Shang Za Zhi.
34:3–7. 2018.(In Chinese). PubMed/NCBI View Article : Google Scholar
|
|
41
|
Carr AC, McCall MR and Frei B: Oxidation
of LDL by myeloperoxidase and reactive nitrogen species: Reaction
pathways and antioxidant protection. Arterioscler Thromb Vasc Biol.
20:1716–1723. 2000.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Zhang R, Brennan ML, Fu X, Aviles RJ,
Pearce GL, Penn MS, Topol EJ, Sprecher DL and Hazen SL: Association
between myeloperoxidase levels and risk of coronary artery disease.
JAMA. 286:2136–2142. 2001.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Eiserich JP, Baldus S, Brennan ML, Ma W,
Zhang C, Tousson A, Castro L, Lusis AJ, Nauseef WM, White CR, et
al: Myeloperoxidase, a leukocyte-derived vascular NO oxidase.
Science. 296:2391–2394. 2002.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Posa A, Szabó R, Kupai K, Berkó AM,
Veszelka M, Szűcs G, Börzsei D, Gyöngyösi M, Pávó I, Deim Z, et al:
Cardioprotective Effect of Selective Estrogen Receptor Modulator
Raloxifene Are Mediated by Heme Oxygenase in Estrogen-Deficient
Rat. Oxid Med Cell Longev. 2017(2176749)2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Posa A, Pavo N, Hemetsberger R, Csonka C,
Csont T, Ferdinandy P, Petrási Z, Varga C, Pavo IJ, Laszlo F Jr, et
al: Protective effect of ischaemic preconditioning on
ischaemia/reperfusion-induced microvascular obstruction determined
by on-line measurements of coronary pressure and blood flow in
pigs. Thromb Haemost. 103:450–460. 2010.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Covelli V, Munno I, Pellegrino NM, Di
Venere A, Jirillo E and Buscaino GA: Exaggerated spontaneous
release of tumor necrosis factor-alpha/cachectin in patients with
migraine without aura. Acta Neurol (Napoli). 12:257–263.
1990.PubMed/NCBI
|
|
47
|
Covelli V, Munno I, Pellegrino NM,
Altamura M, Decandia P, Marcuccio C, Di Venere A and Jirillo E: Are
TNF-alpha and IL-1 beta relevant in the pathogenesis of migraine
without aura? Acta Neurol (Napoli). 13:205–211. 1991.PubMed/NCBI
|
|
48
|
Rietschel ET, Schletter J, Weidemann B,
El-Samalouti V, Mattern T, Zähringer U, Seydel U, Brade H, Flad HD,
Kusumoto S, et al: Lipopolysaccharide and peptidoglycan:
CD14-dependent bacterial inducers of inflammation. Microb Drug
Resist. 4:37–44. 1998.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Maass DL, White J and Horton JW: IL-1beta
and IL-6 act synergistically with TNF-alpha to alter cardiac
contractile function after burn trauma. Shock. 18:360–366.
2002.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Liu XJ, Zhao J and Gu XY: The effects of
genistein and puerarin on the activation of nuclear factor-kappaB
and the production of tumor necrosis factor-alpha in asthma
patients. Pharmazie. 65:127–131. 2010.PubMed/NCBI
|
|
51
|
Goldmann BU, Rudolph V, Rudolph TK, Holle
AK, Hillebrandt M, Meinertz T and Baldus S: Neutrophil activation
precedes myocardial injury in patients with acute myocardial
infarction. Free Radic Biol Med. 47:79–83. 2009.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Yang Y, Duan W, Jin Z, Yi W, Yan J, Zhang
S, Wang N, Liang Z, Li Y, Chen W, et al: JAK2/STAT3 activation by
melatonin attenuates the mitochondrial oxidative damage induced by
myocardial ischemia/reperfusion injury. J Pineal Res. 55:275–286.
2013.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Grütter MG: Caspases: Key players in
programmed cell death. Curr Opin Struct Biol. 10:649–655.
2000.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Zhang Y, Yang X, Ge X and Zhang F:
Puerarin attenuates neurological deficits via Bcl-2/Bax/cleaved
caspase-3 and Sirt3/SOD2 apoptotic pathways in subarachnoid
hemorrhage mice. Biomed Pharmacother. 109:726–733. 2019.PubMed/NCBI View Article : Google Scholar
|
|
55
|
De Zutter GS and Davis RJ: Pro-apoptotic
gene expression mediated by the p38 mitogen-activated protein
kinase signal transduction pathway. Proc Natl Acad Sci USA.
98:6168–6173. 2001.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Saurin AT, Martin JL, Heads RJ, Foley C,
Mockridge JW, Wright MJ, Wang Y and Marber MS: The role of
differential activation of p38-mitogen-activated protein kinase in
preconditioned ventricular myocytes. FASEB J. 14:2237–2246.
2000.PubMed/NCBI View Article : Google Scholar
|