Introduction
Acute ischemic stroke, resulting from large artery
occlusion (LAO), has been established as a major cause of mortality
and severe disability. Numerous randomized controlled trials (RCTs)
have indicated that mechanical thrombectomy (MT), alongside a stent
retriever, represents an effective therapeutic procedure in
patients with LAO (1-5).
In addition to the use of the classic stent retriever for MT,
several additional procedures and devices have been introduced that
improve outcomes and prognoses, including the balloon guide
catheter (BGC) (6-8).
The principle and concept of the BGC is that when a mechanical clot
is retracted using a stent retriever, simultaneous aspiration is
performed through the BGC, which facilitates successful
revascularization and results in the reduced occurrence of
iatrogenic embolic events (6-8).
However, there have been concerns regarding the use of BGCs during
MT, including time consumption, technique requirements, cost
effectiveness and the risk of local complications. Certain studies
have reported advantages of BGCs, such as prevention of
thromboembolic complications, increased suction effectiveness,
facilitation of clot removal, minimization of distal embolization
and a shorter procedure time (7,9-11).
MT using BGCs has been indicated to facilitate improved clinical
and radiological outcomes, compared with other techniques, via a
reduction in both the number of stent passages' and incidence of
distal emboli (10,12,13).
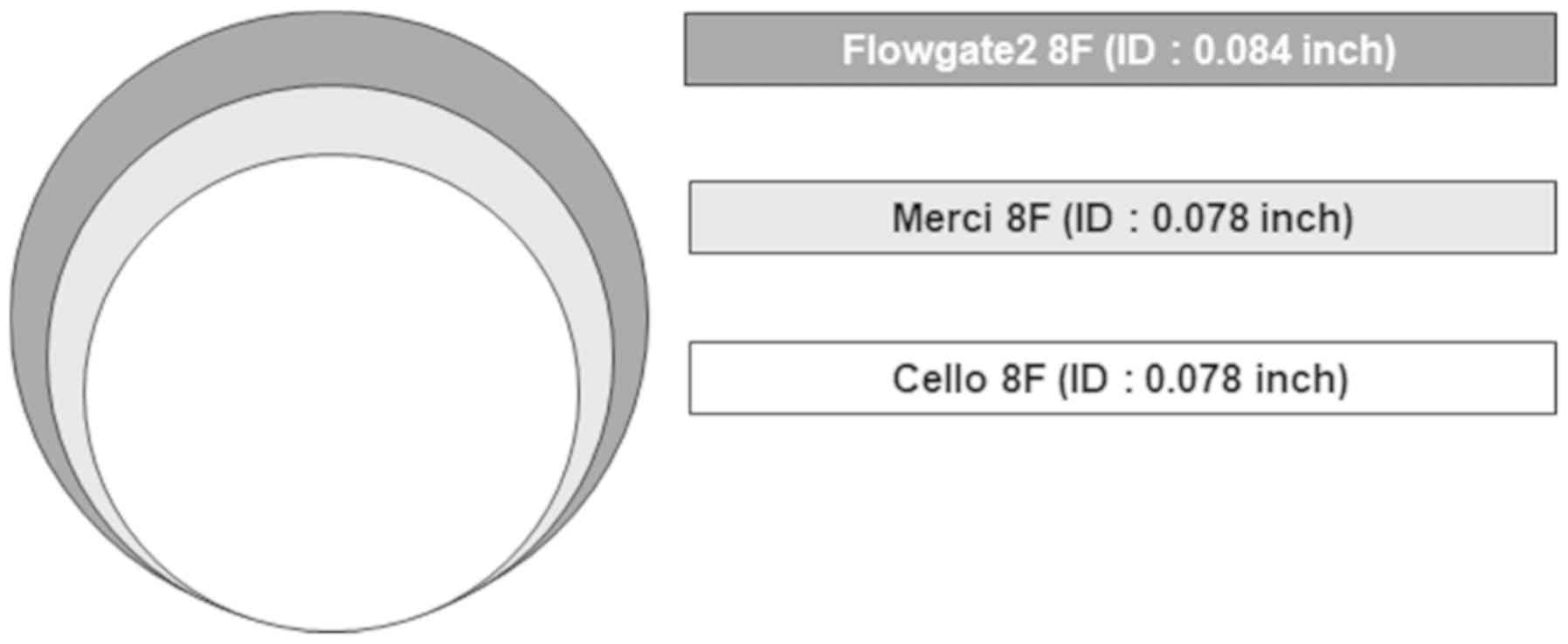
The BGC 8-French FlowGate2™ (FG2; Stryker
Neurovascular) has been introduced and used. Teleb et al
(14) reported a single center
observational study for Flowgate BGC, and the authors of the
present study have also previously reported their experience using
the FG2(15). However, these reports
were not of comparative studies that included other BGCs, and
therefore studies regarding the efficacy of FG2 compared with other
BGCs are yet to be performed. These previous studies indicated that
FG2 has good trackability which allows for smooth navigation to the
target proximal artery, due to its atraumatic and flexible design.
In addition, it is readily able to control proximal flow using a
maximal 10-mm compliant balloon. Compared with other BGC products,
it has the largest distal inner luminal diameter (0.084 inch), and
therefore theoretically offers a higher aspiration flow rate and
greater force of clot capture (Fig.
1). The majority of previous studies evaluating BGCs have
focused on two BGCs: Merci (Concentric Medical) and Cello
(Medtronic Neurovascular). Previously, Merci was used at the
authors' institution, and its efficacy compared with non-BGCs has
been previously reported (12). From
June 2017, FG2 was used as the BGC during MT, instead of Merci BGC.
Therefore, the present study aimed to assess the potential benefits
of using an FG2 BGC for stent retrieval during MT, in comparison to
the Merci BGC. The primary focus of the present study was to
compare FG2 efficacy with that of Merci, by assessing the technical
feasibility, clinical and radiological outcomes, time-associated
factors and safety concerns of each device.
Materials and methods
Study population
The current study comprised prospectively collected
data and a retrospective review, and was approved by the local
Institutional Review Board of each participating center. A total of
245 patients (median age 69.0, age range 22-93, 54.9% male)
underwent MT using stent retrieval procedures for acute stroke
using either the FG2 or Merci BGC, between January 2015 and
September 2018, and were subsequently included in the study. BGC
application to the proximal lesion of target vessel was attempted
in 255 patients; however, the BGC application failed due to severe
tortuosity or angulation of the aorta in 20 cases. Patients who
received intravenous (IV) alteplase [tissue-plasminogen activator
(t-PA)] ≤4.5 after stroke onset at a maximum dose of 0.9 mg/kg were
enrolled. The inclusion criteria were as follows: i) Acute ischemic
stroke due to LAO confirmed by computed tomography (CT) angiography
or perfusion CT; ii) National Institutes of Health Stroke Scale
score ≥2 (range, 0-42; with higher scores indicating more severe
neurological deficits); and iii) patients who underwent stent
retrieval MT using a BGC. The exclusion criteria were as follows:
i) Presence of hemorrhage on CT scan; ii) presence of a large
ischemic core with an Alberta Stroke Program Early CT Score
(ASPECTS) of ≤6; iii) contraindication(s) for contrast-enhanced CT;
iv) MT with non-stent retrievers such as 5 MAX ACE (Penumbra,
Inc.); and v) MT conducted with a BGC that was not Merci or FG2. In
addition, all patients underwent follow-up non-contrast-enhanced CT
immediately after the intervention to evaluate hemorrhages.
Endovascular procedure
All stroke intervention procedures were performed by
two neuro-interventionists with >5 years of experience each. All
procedures were performed on a Siemens Artis Zee biplane system
(Siemens AG) in a dedicated neuro-angiography suite, with patients
under local anesthesia. Equipment selection for each procedure was
determined according to the preference of the treating
neuro-interventionist. In all cases, arterial access was obtained
via the common femoral artery with an 8F 45-cm sheath (Cordis
Corporation). An 8F BGC (FG2 or Merci) was positioned at the
proximal cervical or petrous segment of the internal carotid artery
(ICA) or proximal vertebral artery (VA) for balloon inflation, and
a microcatheter (0.014 or 0.021 inches) was placed over the wire of
the occluded area. The typical procedure involved thrombus
retraction with a retrievable stent, using the 'push and fluff'
technique (16). A Solitaire Flow
Restoration stent retriever (ev3; Covidien) or Trevo stent
retriever (Stryker Neurovascular) was delivered through the
microcatheter and positioned at the occluded site for 5 min, and
the stent was subsequently retrieved. Immediately prior to stent
retrieval, the balloon of the BGC was inflated to arrest the
antegrade proximal flow. Aspiration was then performed through the
BGC using a 50 ml syringe. After the stent was retrieved, the
balloon was immediately deflated to allow for re-circulation of the
proximal artery, and secondary manual aspiration was performed
through the BGC. In certain cases, an additional intermediate
catheter, the 5F SOFIA (MicroVention; Terumo) or 6F AXS Catalyst 6
(Stryker Neurovascular), was used.
Outcomes and complications
Several factors were reviewed, including the failure
rate of BGC application, patient sex and age, risk factors, history
of previous anti-platelet or anti-coagulant use, history of prior
stroke or transient ischemic attack (TIA), IV t-PA, level site of
arterial occlusion, use of intermediate catheter, interventionist
and stent type. All patients underwent a clinical assessment using
the modified Rankin scale (mRS) score at 3 months post-surgery, and
a favorable clinical outcome was defined as an mRS ≤2. Procedure
time was defined as the time from groin puncture to reperfusion
time (min). The radiological results were evaluated according to
the Thrombolysis in Cerebral Infarction (TICI) grading system
(17). A successful recanalization
was defined as a TICI grade 2b or 3, and the ratio of TICI grade 3
to TICI grade 2b (TICI 3/TICI 2b) was also analyzed. The number of
stent passages for successful recanalization was measured. Safety
variables and complications were analyzed in terms of
post-thrombectomy hemorrhage, symptom-associated hemorrhage, vessel
perforation, arterial dissection, vasospasm, distal emboli and
mortality for 3 months postoperatively. Post-thrombectomy
hemorrhage was defined as the occurrence of intracerebral
hemorrhage (ICH) or subarachnoid hemorrhage on a CT scan taken
immediately following the procedure. Distal emboli were defined as
visible fragmented thrombi or emboli downstream at the distal
branch of the primary occlusion site or other new territory on
angiography during MT. In addition, subgroup analysis of the
concomitant use of BGC and an intermediate catheter, and
multivariate analyses for predicting the occurrence of distal
emboli, were performed. All multimodal factors and clinical data
were analyzed by all the authors.
Statistical analysis
All data were analyzed using Stata statistical
software v.15 (StataCorp LP). Between-group comparisons were
calculated using Student's t-test/Mann–Whitney U test or
χ2/Fisher's exact test. The χ2 test and mean
comparison test (student's t-test) were employed to evaluate the
differences in multiple variable factors, outcomes and
complications between the two groups. Univariate analysis was used
to verify the factors that correlated with distal emboli, and
P<0.20 in univariate analysis were entered into a backward
multivariate binary logistic regression analysis. Two-tailed P≤0.05
was considered to indicate a statistically significant
difference.
Results
Baseline characteristics
The failure rate of BGC application to the proximal
lesion of the target vessel was significantly lower in the FG2
group (2.5%) compared with the Merci group (10.8%; P=0.016).
Overall, FG2 was successfully applied in 85 patients (48 men,
56.5%) and the Merci was used in 150 patients (81 men, 54.0%) for
MT with LAO. The mean and median age of patients who underwent BGC
application were 67.9 years [standard deviation (SD), 13.1] and
69.0 years (interquartile range, 22-93 years), respectively. There
were no significant differences between the FG2 and Merci groups in
multiple risk factors, such as hypertension, diabetes mellitus,
atrial fibrillation, coronary artery disease, dyslipidemia,
smoking, history of anti-platelet or anti-coagulant use and history
of prior stroke/TIA. The site of arterial occlusion was as follows:
(FG2: Merci) Middle cerebral artery M1 segment, 42:80; Middle
cerebral artery M2 segment, 11:20; distal ICA, 11:18; proximal ICA,
9:15; and posterior circulation, 8:9). The rate of left hemispheric
stroke was 44.7% (38/85) in the FG2 group and 50.0% (75/150) in the
Merci group. IV t-PA was applied in 35 (41.2%) patients in the FG2
group and 65 (43.3%) patients in the Merci group. In 101 (42.9%)
patients, an additional intermediate catheter was used (FG2:Merci
groups, 43:61). Regarding the interventionists, 131 procedures were
performed by one interventionist (A), while the other
interventionist (B) performed 104 procedures. A total of 120
Solitaire and 115 Trevo retriever stents were used. There was no
statistically significant difference between the two groups in
multiple factors such as arterial occlusion site, left hemisphere
stroke, IV t-PA, interventionists, use of intermediate catheter,
and the type of retriever stent (Table
I).
 | Table IBaseline characteristics. |
Table I
Baseline characteristics.
| Baseline
characteristics | Total, n | FG2, n | Merci, n | P-value |
|---|
| Patients in whom BGC
application was attempted | 255 | 87 | 168 | - |
| Failure of BGC
application (%) | 20 (7.8) | 2 (2.5) | 18 (10.8) | 0.016a |
| FG2 successfully
applied | | | | |
| Total | 235 | 85 | 150 | |
| Sex, male (%) | 129 (54.9) | 48 (56.5) | 81 (54.0) | 0.867 |
| Mean age, years
(SD) | 67.9 (13.1) | 68.9 (13.0) | 67.2 (13.1) | 0.300 |
| Median age, years
(IQR) | 69.0 (22-93) | 70.0 (31-92) | 68.0 (22-93) | - |
| HTN (%) | 130 (55.3) | 45 (54.9) | 85 (56.7) | 0.340 |
| DM (%) | 91 (38.7) | 33 (38.9) | 58 (38.7) | 0.733 |
| AF (%) | 115 (48.9) | 41 (48.2) | 74 (49.3) | 0.351 |
| CAD (%) | 60 (25.5) | 21 (24.7) | 39 (26.0) | 0.663 |
| Dyslipidemia (%) | 106 (45.1) | 35 (41.2) | 71 (47.3) | 0.270 |
| Smoking (%) | 86 (36.6) | 29 (34.1) | 57 (38.0) | 0.258 |
| Previous
anti-platelet use (%) | 92 (39.1) | 34 (40.0) | 58 (38.7) | 0.624 |
| Previous
anti-coagulant use (%) | 27 (11.5) | 10 (11.8) | 17 (11.3) | 0.385 |
| Prior stroke or TIA
(%) | 31 (13.2) | 12 (14.1) | 19 (12.7) | 0.412 |
| Site of arterial
occlusion | | | | |
|
M1 (%) | 122 (48.8) | 42 (49.4) | 80 (53.3) | 0.712 |
|
M2 (%) | 32 (12.8) | 11 (12.9) | 20 (13.3) | 0.883 |
|
Distal ICA
(%) | 30 (12.0) | 11 (12.9) | 18 (12.0) | 0.619 |
|
Mid ICA
(%) | 12 (4.8) | 4 (4.7) | 8 (5.3) | 0.596 |
|
Proximal ICA
(%) | 24 (9.6) | 9 (10.6) | 15 (10.0) | 0.601 |
|
Posterior
circulation (%) | 18 (7.2) | 8 (9.4) | 9 (6.0) | 0.201 |
| Others | | | | |
|
Occlusions
in the left hemisphere (%) | 113 (48.1) | 38 (44.7) | 75 (50.0) | 0.696 |
| t-PA (%) | 100 (42.6) | 35 (41.2) | 65 (43.3) | 0.418 |
| Use of intermediate
catheter (%) | 101 (42.9) | 43 (50.6) | 61 (40.7) | 0.230 |
| Interventionists,
A:B | 131:104 | 49:36 | 82:68 | 0.423 |
| Retriever stent,
Solitaire:Trevo | 120:115 | 40:45 | 80:70 | 0.515 |
Outcomes and complications
The proportion of patients who achieved favorable
3-month mRS scores (mRS 0-2) was 54.1% in the FG2 group, and 50.7%
in the Merci group; the difference was not statistically
significant (P=0.144). In addition, there were no significant
differences in the median value of procedure time between the two
groups (FG2, 39 mins vs. Merci group, 48 min; P=0.208). The mean
value (SD) of stent passes was 1.8 (1.1) in the FG2 group and 2.2
(1.8) in the Merci group, the difference not being statistically
significant. Overall, the number of stent passes were as follows:
(FG2:Merci; 1 pass, 40:61; 2 passes, 34:64; 3 passes, 5:7; >3
passes, 6:18). Successful recanalization (TICI 2b or 3) was
achieved in 79 patients (92.9%) in the FG2 group and 133 patients
(88.7%) in the Merci group. There were no significant differences
in each TICI score (0, 1, 2a, 2b, and 3) nor the rate of successful
recanalization between the groups. However, the ratio of TICI 3
recanalization with the first stent passage was significantly
higher in the FG2 group (44.7%) than in the Merci group (34.7%;
P=0.033). Furthermore, the FG2 group revealed a significantly
higher TICI 3:2b ratio (1.93) than that in the Merci group (1.18;
P=0.031). Regarding the complications, the FG2 group showed a 5.9%
rate of post thrombectomy hemorrhage, 0% rate of symptomatic
hemorrhage, 0% rate of vessel perforation and arterial dissection,
4.3% rate of vasospasm and 5.9% rate of mortality, compared with
those of Merci group (6.7, 1.3, 0 and 0.7%, 6.0, and 7.3%,
respectively). These values were not significantly different
between the groups. However, the incidence rate of distal emboli in
the FG2 group (4.7%) was significantly lower than that in the Merci
group (7.3%; P=0.012; Table
II).
 | Table IIOutcomes, procedure time, number of
passes and complications. |
Table II
Outcomes, procedure time, number of
passes and complications.
| Outcome measured | FG2, n | Merci, n | P-value |
|---|
| Favorable 3-month
mRS (%) | 46 (54.1) | 76 (50.7) | 0.144 |
| Median procedure
time, min (IQR) | 39 (16-91) | 48 (17-115) | 0.208 |
| Number of passes,
mean (SD) | 1.8 (1.1) | 2.2 (1.8) | 0.081 |
|
1 (%) | 40 (47.1) | 61 (40.7) | |
|
2 (%) | 34 (40.0) | 64 (42.7) | |
|
3 (%) | 5 (5.9) | 7 (4.7) | |
|
> 3
(%) | 6 (7.1) | 18 (12.0) | |
| TICI score (%) | | | |
|
0 | 0 (0) | 7 (4.7) | 0.611 |
|
1 | 2 (2.3) | 5 (3.3) | 0.427 |
|
2a | 5 (5.9) | 5 (3.3) | 0.211 |
|
2b | 27 (31.8) | 61 (40.7) | 0.122 |
|
3 (%) | 52 (61.2) | 72 (48.0) | 0.074 |
| Successful
recanalization (%) | 79 (92.9) | 133 (88.7) | 0.226 |
| First-pass
recanalization with TICI 3 | 38 (44.7) | 52 (34.7) | 0.033a |
| TICI 3 to 2b ratio
(TICI 3/TICI 2b) | 1.93 | 1.18 | 0.031a |
| Complications | | | |
|
Post
thrombectomy hemorrhage (%) | 5 (5.9) | 10 (6.7) | 0.462 |
|
Symptomatic
hemorrhage (%) | 0 (0) | 2 (1.3) | 0.182 |
|
Vessel
perforation (%) | 0 (0) | 0 (0) | 0.727 |
|
Arterial
dissection (%) | 0 (0) | 1 (0.7) | 0.422 |
|
Vasospasm
(%) | 3 (4.3) | 9 (6.0) | 0.102 |
|
Distal
emboli (%) | 3 (4.7) | 11 (7.3) | 0.012b |
|
Mortality
(%) | 5 (5.9) | 11 (7.3) | 0.326 |
Subgroup analysis and multivariate
analysis
A subgroup analysis was conducted on patients in
whom a BGC and an intermediate catheter had been used
simultaneously; 43 patients from the FG2 group and 61 patients from
the Merci group were included. Similar factors to those of the
previous analysis were investigated and there were no statistically
significant differences between the two groups for the majority of
factors; however, the TICI 3 recanalization rate with the first
stent passage and the incidence of distal emboli was significantly
different in the FG2 group. The rate of first-pass TICI 3
recanalization was significantly higher in the FG2 group (46.5%)
than in the Merci group (34.4%; P=0.029). Moreover, the incidence
rate of distal emboli in the FG2 group was 2.3% (only 1 patient),
which was statistically significantly lower than that in the Merci
group (6.6%; P=0.038; Table III).
In the multivariate analysis models, two factors were associated
with a decrease in distal emboli: The use of an intermediate
catheter [odds ratio (OR), 0.75; 95% confidence interval (CI),
0.66-0.94; P=0.029], and the use of the FG2 BGC (OR 0.59; 95% CI
0.25-0.93, P=0.020) significantly reduced the incidence rate of
distal emboli (Table IV).
 | Table IIISubgroup analysis of concomitant use
of BGC and an intermediate catheter. |
Table III
Subgroup analysis of concomitant use
of BGC and an intermediate catheter.
| Factor | FG2, n | Merci, n | P-value |
|---|
| Total | 43 | 61 | - |
| Retriever stent
(Solitaire:Trevo) | (16:27) | (21:40) | - |
| Favorable mRS
(%) | 22 (51.2) | 33 (54.1) | 0.662 |
| Procedure time, min
(IQR) | 37 (16-86) | 49 (17-99) | 0.108 |
| Number of passes,
mean (SD) | 1.8 (1.0) | 2.0 (1.2) | 0.482 |
|
1 (%) | 21 (48.8) | 26 (42.6) | |
|
2 (%) | 18 (41.8) | 26 (42.6) | |
|
3 (%) | 2 (4.7) | 4 (6.6) | |
|
>3
(%) | 2 (4.7) | 5 (4.9) | |
| TICI score | | | |
|
2b (%) | 15 (34.9) | 23 (37.7) | 0.422 |
|
3 (%) | 25 (58.1) | 32 (52.5) | 0.174 |
| Successful
recanalization (%) | 40 (93.0) | 55 (90.2) | 0.213 |
| First-pass
recanalization with TICI 3 | 20 (46.5) | 21 (34.4) | 0.029a |
| TICI 3 to 2b ratio
(TICI 3/TICI 2b) | 1.67 | 1.39 | 0.318 |
| Distal emboli
(%) | 1 (2.3) | 4 (6.6) | 0.038a |
 | Table IVFactors for predicting the occurrence
of distal emboli. |
Table IV
Factors for predicting the occurrence
of distal emboli.
| | Univariate
analysis | Multivariate
analysis |
|---|
| Factor | OR (95% CI) | P-value | OR (95% CI) | P-value |
|---|
| Sex | 0.78
(0.50-1.72) | 0.715 | - | - |
| Hypertension | 0.82
(0.23-2.02) | 0.550 | - | - |
| Diabetes
mellitus | 1.24
(0.28-4.20) | 0.932 | - | - |
| Atrial
fibrillation | 2.55
(0.80-7.04) | 0.724 | - | - |
| Dyslipidemia | 0.85
(0.40-3.22) | 0.478 | - | - |
| Smoking | 3.33
(0.71-9.43) | 0.947 | - | - |
| Anti-platelet
use | 0.88
(0.40-4.00) | 0.235 | - | - |
| Anti-coagulant
use | 1.74
(0.63-3.43) | 0.494 | - | - |
| Tissue-plasminogen
activator | 3.10
(0.59-9.12) | 0.721 | - | - |
|
Interventionists | 0.84
(0.44-1.79) | 0.727 | - | - |
| Stent type | 1.68
(0.33-4.25) | 0.602 | - | - |
| Single passage of
stent | 0.88
(0.53-3.85) | 0.601 | - | - |
| Use of intermediate
catheter | 0.78
(0.64-0.92) | 0.041a | 0.75
(0.66-0.94) | 0.029a |
| Use of
FlowGate2 | 0.68
(0.44-0.92) | 0.030a | 0.59
(0.25-0.93) | 0.020a |
Discussion
The FG2 has been demonstrated to have less stiffness
and improved trackability compared with the prior version of BGC,
thus it facilitates smooth delivery to the distal cervical and
proximal petrous segment of the ICA (14). These characteristics of the FG2 BGC
allow it to function more effectively, resulting in greater
reversal of proximal flow when administered at a more distal
location. In the present study, the FG2 BGC demonstrated a lower
application failure rate and incidence of distal emboli, whilst
also exhibiting a higher percentage of TICI 3 recanalization in the
first stent passage and a higher TICI 3:2b ratio, compared with the
Merci BGC. Failure of FG2 application in the proximal lesion of the
target vessel occurred in two cases (2.5%) due to severe tortuosity
and angulation of the aorta. There is a lack of literature
detailing BGC application failure, making direct comparisons
between FG2 and other BGCs problematic. In addition, the 2.5%
failure rate of FG2 in the present study was significantly lower
than that of the Merci (10.8%). Better accessibility and
trackability of the FG2 may have resulted in the lower application
failure rate that for the Merci device. In fact, the authors
regularly experienced a failure to approach the proximal lesion of
the target vessel when using the Merci device, and often could not
overcome the tortuosity of the aorta due to its poor flexibility
and trackability. In particular, flexible and trackable BGCs may be
beneficial for older patients, as they tend to have increased
vessel tortuosity. Therefore, in terms of accessibility, the FG2
may be more useful than the Merci, considering the recent
increasing trend of elderly patients undergoing MT.
In the present study, there was no significant
difference between the FG2 and Merci groups in terms of favorable
mRS, procedure time, mean number of stent passages and successful
recanalization. The FG2 used exhibited acceptable recanalization
rates (92.9%), TICI 3 recanalization with the first passage (44.7%)
and procedure time (39 min) compared with previous studies of other
BGCs; for example, Telebs et al (14) reported values for each of these
categories of 94, 47%, and 38.7 min, respectively, using an FG2
device. In previous studies using other BGCs (such as the Merci or
Cello), varying values of successful recanalization rate (85-95%)
and procedure time (24-69 min) have been reported (9-11,13).
The variation in these values may have resulted from differences in
factors between each study, such as the baseline characteristics,
use of an additional intermediate catheter, and thrombectomy
devices or techniques used. However, the FG2 group of the present
study indicated non-inferior results in clinical and radiological
outcomes compared with previous studies.
The BGC allows for effective MT with an increased
possibility of clot removal and reduced distal emboli, via proximal
blood flow arrest and increasing suction effectiveness (9,10,18). The
effect of proximal blood flow control in FG2 and Merci is
considered to be the same, because they have same 8 F outer
diameter and balloon size; however, the incidence rate of distal
emboli was significantly lower in the FG2 group compared with the
Merci group, and the use of FG2 was revealed to be associated with
reduced distal emboli in the multivariate analysis. The 4.7% distal
emboli occurrence rate in the FG2 group was lower than that
(6.8-25.0%) reported in other studies with other BGC types, such as
the Merci or Cello (12,13). The increased aspiration power due to
the larger inner diameter (ID) of the FG2 (0.084 inch), compared
with that of the Merci (0.078 inch) may have contributed to this
result. Furthermore, the higher ratio of TICI 3 at the first stent
passage and TICI 3:2b ratio in the FG2 group compared with the
Merci group may be associated with the improved aspiration power of
the FG2. Recently, the importance of a first pass effect (FPE) has
been emphasized, and the FPE yielded a good clinical outcome with a
short procedure time (19). In the
present study, the improved mRS score and procedure time did not
significantly differ between the FG2 and Merci groups, but the TICI
3 achievement at the first stent passage of the FG2 group was
higher than that of the Merci group. This result also demonstrates
the advantage of the FG2 in improving the FPE, via facilitation of
improved aspiration power due to a larger ID compared with that of
the Merci.
The enlarged inner lumen of the FG2 allowed for
concomitant use of intermediate large-bore aspiration catheters for
salvage techniques, as well as increased aspiration power. In
previous studies, the use of an intermediate catheter and the
‘Solumbra technique’ have been reported to result in better
clinical and radiological outcomes (20,21).
Moreover, in the present study, the multivariate analysis revealed
that the use of an intermediate catheter reduced the occurrence of
distal emboli. Thus, subgroup analysis with concomitant use of a
BGC and intermediate catheter was conducted and indicated that the
FG2, when used with an intermediate catheter, resulted in a higher
TICI 3 recanalization ratio at the first stent passage and lower
incidence rate of distal emboli compared with the Merci used with
an intermediate catheter. This indicates that better results can be
obtained with FG2 than with Merci, even with concomitant use of
BGCs and an intermediate catheter.
The major limitations of this study are its
relatively small population size and its retrospective nature. In
addition, MT using the Merci BGC was performed before the use of
the FG2; therefore, it may be assumed that habituation to the
experimental procedure and increased experience and practice may
have skewed the results towards the FG2 device. However, all
procedures in this study were performed by two
neuro-interventionists with >5 years of experience, both of whom
perform at least 50 MT procedures annually. Baseline
characteristics in the two groups were well-balanced, with no
statistically significant differences. Thus, any between-group
differences associated with a learning curve would not represent an
important consideration. Finally, although every effort was made to
control for potential confounding variables, potential confounding
variables (including device selection and interpretation of
angiographic images), considering the observational nature of the
study, the potential effect of variables not accounted for cannot
be ignored.
In conclusion, FG2 BGC enables effective stent
retrieval MT with a lower application failure rate, lower incidence
of distal emboli and higher TICI 3 recanalization at the first
stent passage, compared with the Merci BGC. The FG2 may be suitable
for MT with little application failure as a result of its good
accessibility and trackability in tortuous vessels, and FG2 may
induce aggressive aspiration and contribute to the reduction of
distal embolus incidence due to its large luminal size. In
addition, improved outcomes may also be facilitated by simultaneous
use of the FG2 BGC and an intermediate catheter. Additional
multicenter studies and randomized controlled trials should be
performed to verify the present findings.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HJY and DHL designed the study. HJY, DHL and JHS
performed data acquisition, analysis, interpretation of the data
and drafting of the manuscript. HJY carried out statistical
analysis. DHL supervised the study. HJY, DHL, JHS checked the
integrity of the data and accuracy of the data analysis. All
authors read and approved the final manuscript.
Ethical approval and consent to
participate
The present study was approved by the local ethical
committee and institutional review board (IRB No. VC18RESI0027).
Informed consent was obtained from all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Campbell BC, Mitchell PJ, Kleinig TJ,
Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley
TJ, et al: Endovascular therapy for ischemic stroke with
perfusion-imaging selection. N Engl J Med. 372:1009–1018.
2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Goyal M, Demchuk AM, Menon BK, Eesa M,
Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL,
et al: Randomized assessment of rapid endovascular treatment of
ischemic stroke. N Engl J Med. 372:1019–1030. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Saver JL, Goyal M, Bonafe A, Diener HC,
Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, et
al: Stent-retriever thrombectomy after intravenous t-PA vs t-PA
alone in stroke. N Engl J Med. 372:2285–2295. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jovin TG, Chamorro A, Cobo E, de Miquel
MA, Molina CA, Rovira A, San Román L, Serena J, Abilleira S, Ribó
M, et al: Thrombectomy within 8 hours after symptom onset in
ischemic stroke. N Engl J Med. 372:2296–2306. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Berkhemer OA, Fransen PS, Beumer D, van
den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn
PJ, Wermer MJ, et al: A randomized trial of intraarterial treatment
for acute ischemic stroke. N Engl J Med. 372:11–20. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Pereira VM, Gralla J, Davalos A, Bonafé A,
Castaño C, Chapot R, Liebeskind DS, Nogueira RG, Arnold M, Sztajzel
R, et al: Prospective, multicenter, single-arm study of mechanical
thrombectomy using solitaire flow restoration in acute ischemic
stroke. Stroke. 44:2802–2807. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chueh JY, Kühn AL, Puri AS, Wilson SD,
Wakhloo AK and Gounis MJ: Reduction in distal emboli with proximal
flow control during mechanical thrombectomy: A quantitative in
vitro study. Stroke. 44:1396–1401. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mokin M, Ionita CN, Nagesh SV, Rudin S,
Levy EI and Siddiqui AH: Primary stentriever versus combined
stentriever plus aspiration thrombectomy approaches: In vitro
stroke model comparison. J Neurointerv Surg. 7:453–457.
2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Nguyen TN, Malisch T, Castonguay AC, Gupta
R, Sun CH, Martin CO, Holloway WE, Mueller-Kronast N, English JD,
Linfante I, et al: Balloon guide catheter improves
revascularization and clinical outcomes with the solitaire device:
Analysis of the North American Solitaire Acute Stroke Registry.
Stroke. 45:141–145. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Velasco A, Buerke B, Stracke CP,
Berkemeyer S, Mosimann PJ, Schwindt W, Alcazar P, Cnyrim C,
Niederstadt T, Chapot R and Heindel W: Comparison of a balloon
guide catheter and a non-balloon guide catheter for mechanical
thrombectomy. Radiology. 280:169–176. 2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Chueh JY, Puri AS, Wakhloo AK and Gounis
MJ: Risk of distal embolization with stent retriever thrombectomy
and ADAPT. J Neurointerv Surg. 8:197–202. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lee DH, Sung JH, Kim SU, Yi HJ, Hong JT
and Lee SW: Effective use of balloon guide catheters in reducing
incidence of mechanical thrombectomy related distal embolization.
Acta Neurochir (Wien). 159:1671–1677. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Oh JS, Yoon SM, Shim JJ, Doh JW, Bae HG
and Lee KS: Efficacy of balloon-guiding catheter for mechanical
thrombectomy in patients with anterior circulation ischemic stroke.
J Korean Neurosurg Soc. 60:155–164. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Teleb MS: Endovascular acute ischemic
stroke treatment with flowgate balloon guide catheter: A
single-center observational study of flowgate balloon guide
catheter use. Interv Neurol. 7:327–333. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yi HJ, Sung JH, Lee MH and Lee DH:
Experience of the new Flow Gate2 device as a balloon
guide catheter for ischemic stroke intervention. World Neurosurg.
126:e736–e742. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Haussen DC, Rebello LC and Nogueira RG:
Optimizating clot retrieval in acute stroke: The push and fluff
technique for closed-cell stentrievers. Stroke. 46:2838–2842.
2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zaidat OO, Yoo AJ, Khatri P, Tomsick TA,
von Kummer R, Saver JL, Marks MP, Prabhakaran S, Kallmes DF,
Fitzsimmons BF, et al: Recommendations on angiographic
revascularization grading standards for acute ischemic stroke: A
consensus statement. Stroke. 44:2650–2663. 2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kammerer S, du Mesnil de Rochemont R,
Wagner M, You S, Tritt S, Mueller-Eschner M, Keil FC, Lauer A and
Berkefeld J: Efficacy of mechanical thrombectomy using stent
retriever and balloon-guiding catheter. Cardiovasc Intervent
Radiol. 41:699–705. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Zaidat OO, Castonguay AC, Linfante I,
Gupta R, Martin CO, Holloway WE, Mueller-Kronast N, English JD,
Dabus G, Malisch TW, et al: First pass effect: A new measure for
stroke thrombectomy devices. Stroke. 49:660–666. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Delgado Almandoz JE, Kayan Y, Young ML,
Fease JL, Scholz JM, Milner AM, Hehr TH, Roohani P, Mulder M and
Tarrel RM: Comparison of clinical outcomes in patients with acute
ischemic strokes treated with mechanical thrombectomy using either
Solumbra or ADAPT techniques. J Neurointerv Surg. 8:1123–1128.
2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wong JHY, Do HM, Telischak NA, Moraff AM,
Dodd RL, Marks MP, Ingle SM and Heit JJ: Initial experience with
SOFIA as an intermediate catheter in mechanical thrombectomy for
acute ischemic stroke. J Neurointerv Surg. 9:1103–1106.
2017.PubMed/NCBI View Article : Google Scholar
|