Introduction
Capsular contraction syndrome (CCS) was first named
by Davison in 1993, and has been correlated with the application of
continuous curvilinear capsulorhexis (CCC) in phacoemulsification
(1,2). CCS primarily occurs within 3-30 weeks
following surgery (1,2). Manifestations of CCS include the
equatorial diameter reduction of the capsula lentis and narrowing
of the CCC opening in operated eyes post-surgery; fibrosis
opacification development in the anterior capsular membrane; and
tilting, displacement or dislocation of the intraocular lens (IOL),
which leads to decreased visual acuity and quality, and obstruction
of fundoscopy and treatment (3).
Neodymium-doped yttrium aluminum garnet (Nd:YAG) laser treatment is
an effective and safe treatment method for CCS that can loosen the
hyperplastic fibers (also known as annular fibers) of the
contracted capsular bag, enlarge the capsular opening area and
restore visual function (4).
However, for patients with serious CCS, the severe hyperplasia of
fibers could not be shattered by the laser, the large fragments of
fibrous membrane was not absorbed spontaneously following the
shattering of the hyperplastic fibers or the hyperplastic fibers
were in the central optical area; in addition, Nd:YAG laser
treatment may damage the intraocular lens (5). For patients who cannot tolerate Nd:YAG
laser treatment, who cannot sit for long periods, with nystagmus or
who are in areas without laser equipment and other medical
equipment, capsular bag relaxation surgery (CBRS) is a suitable
option (6,7). The present study investigated the
effect of CBRS on 25 eyes from 25 patients with CCS in order to
determine whether CBRS has good therapeutic effects.
Materials and methods
Subjects.
The retrospective case study comprised of the data
from 25 patients, who received CBRS due to CCS in the Ophthalmology
Center of Taizhou City Hospital between January 2005 and December
2015. Among these patients, 10 patients with 10 diseased eyes were
male and 15 patients with 15 diseased eyes were female. The age of
these patients ranged from 60 to 79 years old, with a mean age of
71.0±3.5 years old. A total of 4 patients developed cataracts
following glaucoma trabeculectomy and received phacoemulsification
and foldable IOL implantation. A total of 21 patients received
phacoemulsification and foldable IOL implantation due to cataracts.
All surgeries were successful and no early intraoperative or
postoperative complications occurred. Visual acuity upon discharge
following cataract surgery ranged between 4.4 and 4.9. None of the
25 patients unwent Nd:YAG treatment.
Occurrence of CCS
Time for CCS occurrence was monitored between
discharge from hospital following phacoemulsification and the date
patients complained of decreased visual acuity during the 4-, 12-
and 24-week follow-ups. A total of 4 cases (4 eyes) of CCS occurred
within week 4 to 5 following phacoemulsification, and the same
number occurred within week 7-9; however, 7 cases (7 eyes) of CCS
occurred within week 11-14, 8 cases (8 eyes) of CCS occurred within
week 18-22 and 2 cases (2 eyes) of CCS occurred within week 24-27.
The mean time was 14±2 weeks following phacoemulsification.
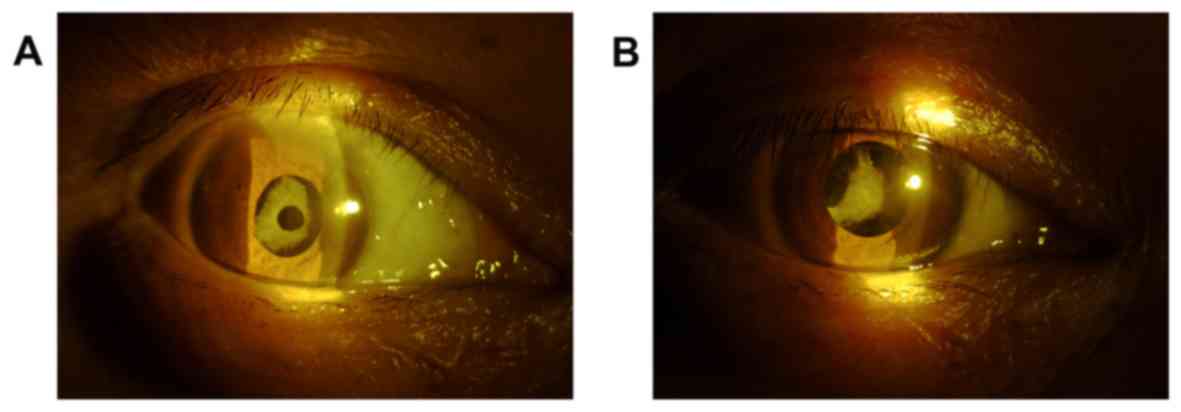
Clinical manifestations
All patients complained that the visual acuity of
the operated eye significantly decreased compared with the visual
acuity upon discharge following cataract surgery. Among these
patients, 6 eyes had a visual acuity of <4.0, 14 eyes had a
visual acuity that ranged between 4.0-4.2 and 5 eyes had a visual
acuity that ranged between 4.3-4.5. In addition, glare occurred in
7 eyes and monocular diplopia occurred in 3 eyes. Seven eyes (7
patients) exhibited a white anterior capsular membrane behind the
pupillary margin under a slit lamp. During pupil examination, white
hyperplasia of the fibrous membrane appeared under the anterior
capsule, annular fiber of the anterior capsule opening proliferated
and thickened, and dislocation of the anterior capsule opening
occurred in all cases. Furthermore, the transparent area shrunk and
was deformed, with a diameter that ranged within 1.5-2.5 mm.
Surrounding capsule shrinkage and folds of the posterior capsule
were evident. In addition, the central optical region was covered
completely (Fig. 1). Seven eyes
exhibited IOL decentration and 5 eyes exhibited tilted IOL.
Furthermore, the IOL was clamped inside the capsule in 1 eye and 2
eyes exhibited opacity in the mid-peripheral part of the cornea.
The ocular fundi in the majority of diseased eyes could not be
clearly viewed.
Surgical indications
Several indications suggested eyes were not suitable
to receive Nd:YAG laser treatment. First, if the anterior capsule
opening and anterior capsule hyperplasia were thicker, the fiber
ring width was ≥1.5 mm and the anterior capsule opening was closed
or ≤1.5 mm, it was determined that laser treatment would not
achieve a beneficial therapeutic effect. The anterior capsule
opening and anterior capsule hyperplasia were determined to be
'thicker' based on the experiences of the examining doctor.
Furthermore, Nd:YAG laser treatment was not suitable if IOL
deviation was evident, the IOL was hard to spontaneously reset
following laser capsular relaxation, corneal scarring was present
(this made it difficult for the laser to accurately focus on the
eye), nystagmus or fixation could not be achieved, patients did not
cooperate, IOL was prone to laser damage or the IOL was clamped
inside the capsule.
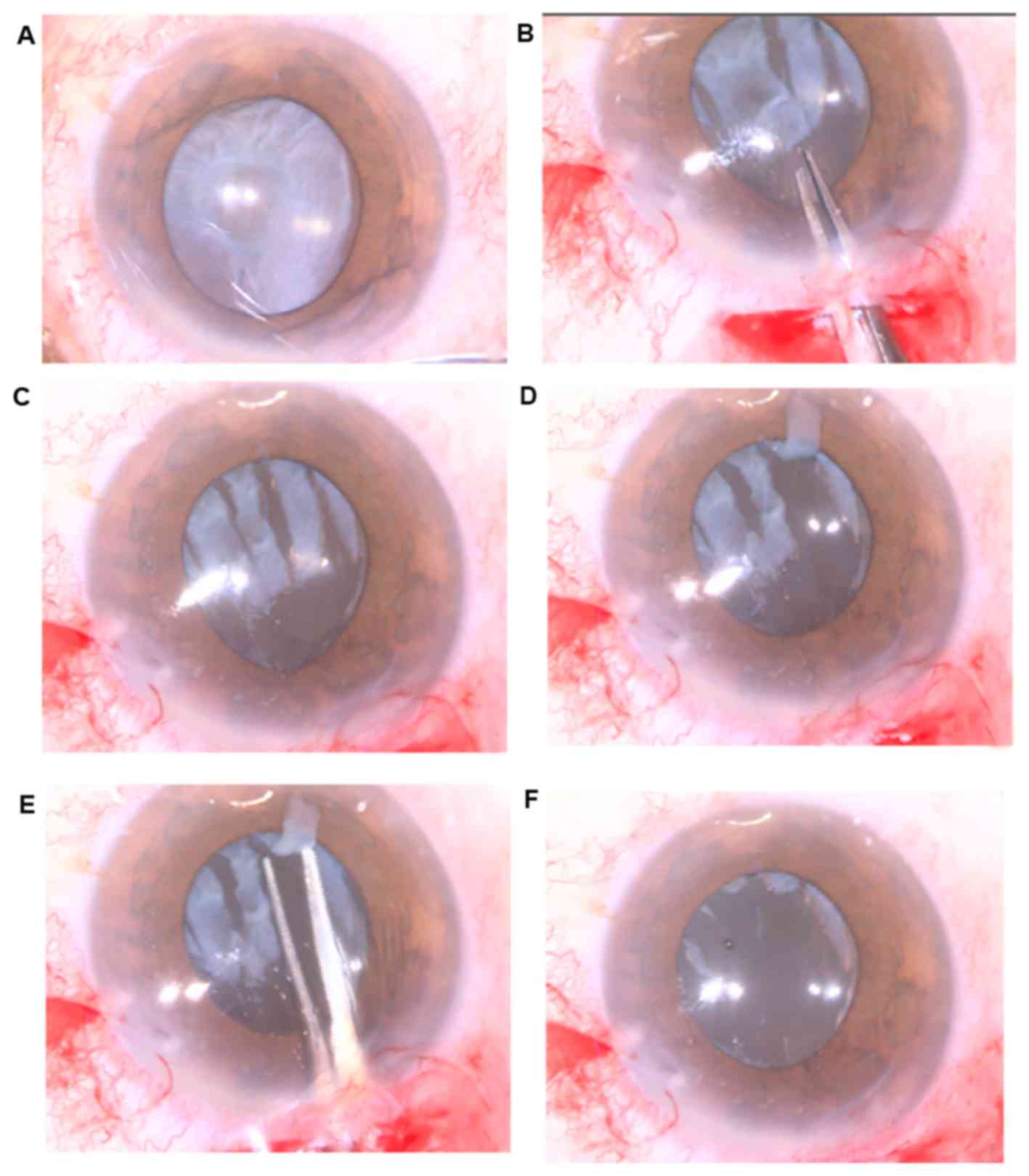
Surgical methods
Radial incision surgery were performed. Prior to
surgery, mydriasis was fully induced using compound tropicamide eye
drops. Under surface anesthesia, a 3.0-mm corneal incision was made
at the 11 o'clock position and the viscoelastic agent was injected
into anterior chamber and under the anterior capsule. For eyes with
adhesions, the fibrous membrane and IOL edge were separated with a
discission needle or the loop adhesion was separated to fully free
the anterior capsular membrane at the predetermined incision. The
organized thickening edge of the anterior capsule opening was cut
into four to six 1.5-2.5 mm equidistant actinoid incisions using
capsule scissors. The IOL was adjusted to reset the correct
position. If the fibrous membrane at the 2 o'clock position of the
anterior capsule opening was difficult to cut, an aperture was
first made at the site 1.5-2.5 mm from the fibrous membrane of the
anterior capsule opening edge using a paracentesis knife or
capsulotomy. Following this, the viscoelastic agent was injected
into the aperture to induce swelling. The inferior scissor of the
capsule scissors was pierced into the aperture and the membrane was
cut off at the central opening. Following actinoid relaxing
incision, the anterior capsule opening would grow zig-zag-like or
hub-and-spoke-organized anterior capsular segments. These thick and
tough segments can be cut off from the root with capsule scissors
or removed using a vitrectomy knife. These surgical procedures can
expand the anterior capsule opening to a relative circular shape.
In the present study, a total 15 eyes (15 cases) underwent actinoid
relaxing incisions (Fig. 2). Other
patients did not receive actinoid relaxing incisions, as the
surgeons were able to perform annular capsulorhexis.
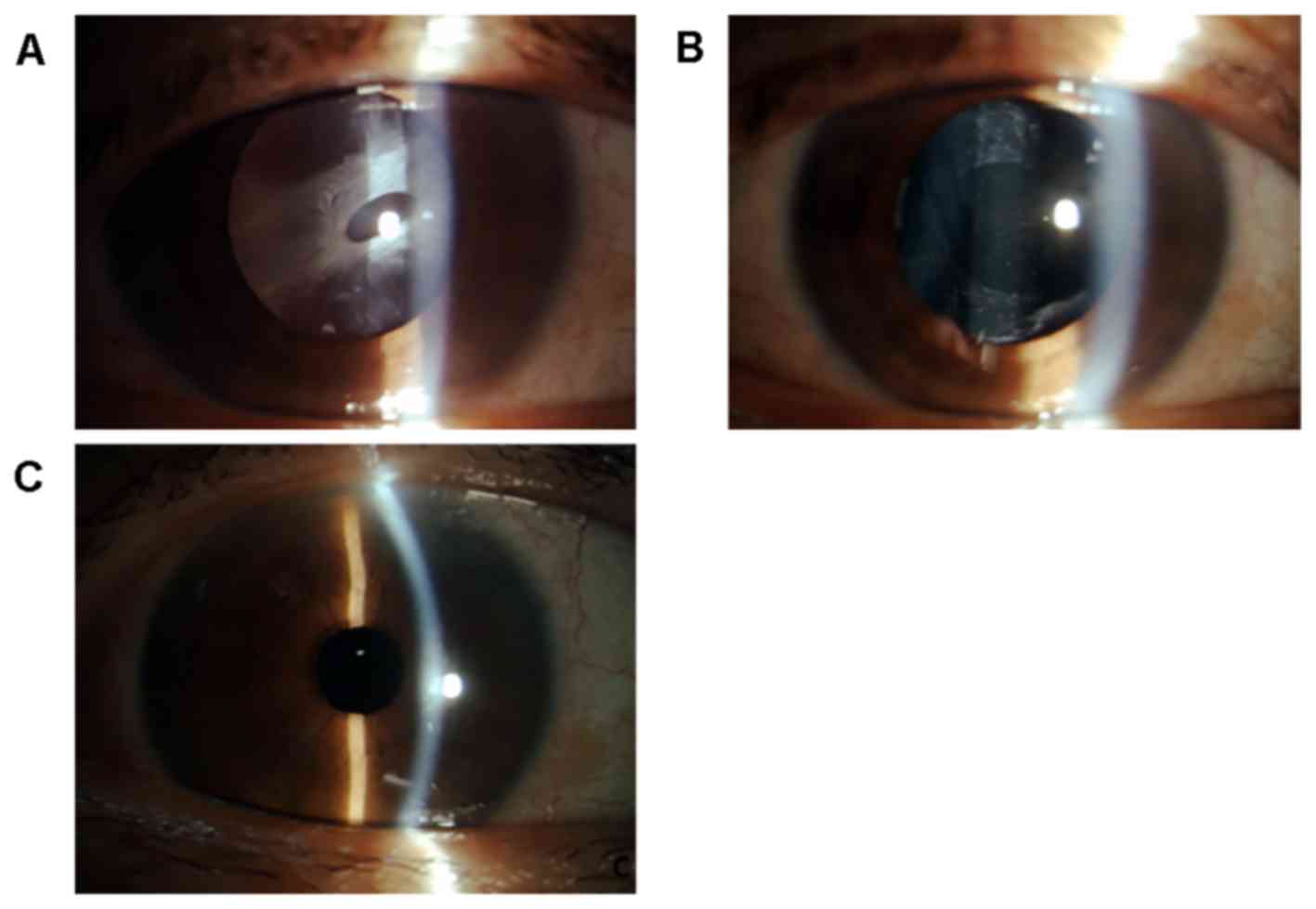
CCC was also performed twice on diseased eyes to
remove the fiber membrane under specific conditions. For these
diseased eyes that had a completely closed anterior capsule
opening, an aperture was first made in the center, paracenter or
edge of the fibrous membrane with a straight knife or 1-ml needle
bend at the head, which was used as a cystotome. Subsequently, the
viscoelastic agent was injected into the aperture to separate the
adhesion between the fibrous membrane and the optical part of the
IOL, and a strip of triangle segment obliquely stretching beneath
the nose or temporal was made on the edge of the aperture.
Following this, the root of the triangle segment was clipped with
capsulorhexis forceps to remove the fibrous membrane using the CCC
method. For diseased eyes with an anterior capsule opening that was
almost closed, a triangle segment was made at the 3 or 9 o'clock
position on the edge of the anterior capsule opening, followed by a
secondary CCC. Following capsule relaxation, the IOL was stretched
to a flat shape by itself. An appropriate adjustment should be
conducted to reset the IOL to the correct position. In the present
study, a total of 10 diseased eyes (10 cases) received CCC
(Fig. 3). In the remaining patients,
the fibrous membrane could not be dissected during CCC due to the
thick hyperplasia of the Lens Epithelial Cells.
Slit lamp examination
All operated eyes were examined using a slit-lamp,
under non-mydriatic and mydriatic states. During the 1-, 3- and
6-month follow-ups, non-mydriatic and mydriatic slit lamp
examinations were conducted.
Visual acuity examination
In the present study, preoperative and postoperative
visual acuity was assessed using the quintile method (8). Patients were followed-up once at 1, 3
and 6 months following surgery.
Statistical analysis
Data were analyzed using SPSS 13.0 statistical
analysis software (SPSS, Inc., Chicago, IL, USA). Preoperative and
postoperative visual acuity changes were compared using a signed
rank sum test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Postoperative visual acuity
Visual acuity of all operated eyes improved to
different extents. Visual differences pre- and post-surgery were
statistically significant (u=5.143; P<0.01), suggesting
the objective visual clarity was significantly improved following
surgery. Glare and monocular diplopia were no longer evident.
Preoperative and postoperative uncorrected visual acuity (UCVA)
obtained during the final follow-up are indicated in Table I. One diseased eye with a
postoperative UCVA of 4.1 at the final follow-up was confirmed to
have cystoid macular edema following a fundus examination and
optical coherence tomography. Notably, this condition may be
associated with the stimuli on the macula in the cataract surgery,
radial incision surgery and a second CCC.
 | Table IComparison of preoperative and
postoperative the final follow-up. |
Table I
Comparison of preoperative and
postoperative the final follow-up.
| Variable | Number of
preoperative eyes | Number of
postoperative eyes |
|---|
| Eyesight score |
|
<4.0 | 6 | 0 |
|
4.0-4.2 | 14 | 1 |
|
4.3-4.5 | 5 | 5 |
|
4.6-4.8 | 0 | 15 |
|
>4.8 | 0 | 4 |
| Total number | 25 | 25 |
Slit lamp examination
Under the non-mydriatic state, all pupil areas were
clear and no white fibrous membrane of the anterior capsule was
observed. Under the mydriatic state, the fibrous ring of anterior
capsule opening was identified as relaxed, the lens capsular bag
shrunk or was no longer evident and the area of the transparent
zone of the anterior capsule opening was expanded to a diameter of
5.0-6.0 mm. The IOL was located inside the lens capsular bag and
was centrally positioned without deviation or tilt. The optical
part of the IOL was stretched, flat and not clipped. There was also
no occurrence of fracture of the IOL optical section, zonular
dehiscence or actinoid tear at any site, except for the anterior or
posterior capsular membranes. The posterior capsule was closely
attached to the posterior surface of the IOL. Sectional edges of
the anterior capsule openings of diseased eyes that underwent
actinoid relaxing incisions were slightly serrated, while diseased
eyes that underwent secondary CCC were smooth.
Postoperative follow-up
Patients were followed-up once at 1, 3 and 6 months
postoperatively. Under the non-mydriatic state, the pupil area was
clear and the anterior capsule opening edge was not visible. Under
the mydriatic state, the IOL position was good, the area of the
transparent zone of the anterior capsule opening did not reveal any
shrinkage and no recurrence of CCS was identified. At the last
follow-up, only one operated eye that underwent secondary CCC was
indicated to have fibrous ring hyperplasia at the edge of the CCC.
The capsular opening was not reduced in this case.
Discussion
CCS is a rare complication that occurs after
phacoemulsification if a CCC procedure is adopted (9). CCS is associated with surgical trauma,
IOL material stimulus, postoperative inflammation, damage of the
blood aqueous barrier and blood-retinal barrier, the inappropriate
small diameter of CCC and decentration (8,9). The
above factors cause residual lens epithelial cells (LECs) under the
anterior capsular membrane to proliferate and differentiate into
fibroblasts with the sphincter contraction effect. LECs begin to
accumulate under the capsulorhexis opening and the surrounding
capsule, forming a thick fibrous ring membrane, which causes the
anterior capsule to undergo centripetal contraction (10,11).
Subsequently, the anterior capsule opening area and the equatorial
diameter is reduced; causing visual impairment, glare, refractive
change, IOL tilt and deviation (12). Hence, CCS is a rare clinical
manifestation that can occur after CCC, and LECs serve a leading
role in capsule contraction (13,14).
At present, the primary treatment for CCS is Nd:YAG
laser treatment or surgery (5).
Nd:YAG laser treatment is an effective, safe, convenient and cheap
treatment method for CCS (15). This
method can expand the area of the anterior capsule opening
transparent zone and restore visual function (15). However, some diseased eyes are not
suitable for laser treatment due to a number of reasons. Patients
with obvious IOL deviations whose IOL was difficult to
spontaneously reset following laser capsular release, whereas in
other patients with corneal scars, focusing the laser accurately
into the eyes is difficult; in addition, patients who had
nystagmus, whose IOL was easily damaged by laser and or with the
intracapsular clamping of IOL are also not suitable for laser
treatment (5,14). In the authors' clinical experience,
they have determined that for some diseased eyes that have received
laser treatment without therapeutic effect, although increased
laser energy can cut off the anterior capsule, under this
condition, the adverse reaction has been severe, the number of
complications has been large and the relaxing effect has been poor.
Additionally, the authors of the current study have found that the
deviated or clipped IOL has been difficult to reset, or have even
caused damage to the IOL (16,17).
Therefore, surgical treatment (CBRS) should be performed (18). Our previous study reported the
results of CBRS (19). On the basis
of previous studies (4,5,7), more
cases and imaging data were collected to assess the surgical
procedure of CBRS more visually in the present study.
In the present study, the CBRS procedure comprised
of two methods; namely, the actinoid relaxing incision and
secondary CCC. Actinoid relaxing incisions can be applied to the
following types of patients: Patients who refuse to cooperate,
patients whose eyes are not tolerant to Nd:AG laser treatment or
patients who do not have serious anterior capsular membrane
closure. In actinoid relaxing incisions, capsule scissors were
pierced in the aperture from the edge of the anterior capsule
opening. Following this, an incision was cut every 60˚ or 90˚ to
form an actinoid shape. When cutting, the incisions were made to
co-elongate and be equidistant as far as possible in order to
achieve the following objectives: Make the incision tension equal,
ease capsular tension, enable the edge of the anterior capsule
opening to cover the edge of the IOL optical part at 0.5-1.0 mm and
flatten the IOL optical part. In addition, the IOL was adjusted to
a central position. Since corneal incisions are located at the
upper part of the fibrous hyperplastic membrane, it is difficult to
cut off the fibrous ring at the edge of the anterior capsule
opening. If the fibrous ring cannot be cut off, dicing should be
conducted with the side cutting edge of the discission needle. For
diseased eyes with a thick fibrous ring at the anterior capsule
opening, an aperture should be pre-made in the fibrous membrane
above the anterior capsule opening with a straight knife or
capsule-cutting knife. The inferior scissor of the capsule scissors
was pierced into the aperture, and the fibrous ring of capsule
opening was cut as described previously (14). Following this, in the present study,
relaxing incisions in other parts were made. From the clinical
experience of the authors of the current study, once actinoid
relaxing incision was performed, the anterior capsule opening can
grow zig-zag-like or hub-and-spoke-organized anterior capsular
segments. The authors have found that the majority of these
segments are thick and tough, and some of the front-end may cock up
and move with the contraction and relaxation of the pupil.
Additionally, the authors determined that these may rub the pupil
edge and iris pigment membrane, and lead to iritis or the
accumulation of free iris pigments in the anterior chamber angle;
and further result in elevated intraocular pressure. Therefore,
considering this situation, these large, long, thick and tough
segments should be cut off from the root with capsule scissors and
taken out or removed using a vitrectomy knife; expanding the
capsulorhexis opening to a relative circular shape. However,
resection using an anterior vitrectomy knife can be time consuming
(20). In the present study, 15 eyes
underwent actinoid incisions of the anterior capsule opening; in
which fibrous segments were removed from 4 eyes using a vitrectomy
knife.
The CCC method is also known as secondary
capsulorhexis; that is, an expanding capsulorhexis is conducted
again outside the narrowing anterior capsule opening (21). The present study found that this
method is suitable for diseased eyes that have closed or
near-closed fibrotic tissue in the anterior capsule opening in
patients who exhibited no fibrosis or thin fibrosis in the
peripheral anterior capsule of the fibrous membrane. The authors
also demonstrated that the edge of the anterior capsule opening can
be swollen with viscoelastic agent, an oblique segment can be made
at the 3 or 9 o'clock position with capsule scissors, the root of
the segment may be clipped with capsulorhexis forceps and secondary
expanding CCC is conducted. Following this, the IOL may be adjusted
and restored to its correct position. In the present study, the
area of the transparent zone was set to 5.0-6.0 mm in diameter and
the effect was the optimal when the edge of anterior capsule
opening covered 0.5 mm of the edge of the IOL optical part. From
the clinical experience of the authors of the current study, if the
anterior capsule opening is completely closed, an aperture should
be made on the fibrous membrane of the anterior capsule in advance,
as aforementioned. Then, CCC may be conducted. However, the authors
note that it is sometimes difficult to conduct capsulorhexis, since
the trajectory is exactly on the thick fibrous membrane. Hence, an
oblique segment should be made on the other side, and reverse
capsulorhexis can be conducted. When necessary, a combination of
tearing and cutting should be used; that is, when a fibrous tissue
is difficult to tear apart, it can be cut open using capsule
scissors; and then, these are torn apart. The authors advise that
when tearing and cutting, caution should be given in performing
these procedures and making excessive expansions or rupturing the
capsular opening should be avoided. The advantage of the CCC method
is that its edge is smooth; hence, the stability of the IOL in the
capsule is improved (22). However,
the authors of the current study noted that during their clinical
experience, if the fibrous membrane is wide and thick, the zonule
would be tugged during the capsulorhexis. A forced capsulorhexis
may lead to rupture of the zonule. Hence, under this condition, the
authors hypothesize that the actinoid segment method is
suitable.
The disadvantage of the radial incision sac lysis
and annular capsulorhexis lysis methods is indicated during poor
zonular function, when the procedure may injure a zonule and induce
the IOL to deviate, particularly in diseased eyes with a can-shaped
capsular opening (15). Primary
complications, including anterior vitreous prolapse, pupillary
block, elevated intraocular pressure, capsular rupture, zonular
dehiscence, corneal edema and macular edema have been specified in
a previous study (23). However, in
the present study, these complications did not occur. Measures
should be taken to avoid these injuries and care should be taken
during the separation of the adhesion. Furthermore, force should be
avoided when shearing the tough, thick fibrous membrane or
performing secondary capsulorhexis. From their clinical experience,
the authors of the current study observed that adhesions between
the fibrous membrane and anterior capsule membrane or IOL were
sometimes serious and were difficult to separate. Hence, these
adhesions should be first sliced with a discission needle once the
edge of the anterior capsule opening is exposed. Cutting should be
performed whilst pushing with the capsule scissors to fully free
the anterior capsular membrane being removed. The authors of he
current study also found that the proliferation ability of LECs was
reduced 3 months after cataract surgery; hence, the possibility of
recurrence of CCS following CBRS was very small. CCS relapse
depends on the condition of capsular lens bag, which can be normal
or contracted and the front of anterior capsule opening can be
normal or contracted. Although one case had an edema, this occurred
in the macula retinae, not in the lens capsular bag. Therefore, in
the present study, no CCS relapse was identified in the 25 diseased
eyes.
CCS is a rare complication after cataract
phacoemulsification that is associated with CCC contraction
(9). In order to avoid this, focus
should be made on prevention, emphasis should be made on perfecting
phacoemulsification, the CCC procedure should be normalized, the
fibrous membrane should be removed thoroughly, the capsule should
be polished and the implanted IOL should be centered (24). Furthermore, patients should be
regularly followed-up following phacoemulsification and IOL
implantation. Mydriatic examination should be conducted when
patients complain of vision or visual change in order to detect CCS
early and provide timely treatment. Laser and surgery are the
primary treatments for CCS (25,26).
However, in some severe cases or cases not suitable for laser
treatment, surgery is the sole choice. In the present study, CBRS
was conducted. Actinoid relaxing incision and secondary CCC methods
were demonstrated to have positive effects. Hence, a suitable
method should be chosen based on the local features of CCS or a
combination of these two methods.
Acknowledgements
Not applicable.
Funding
The current study was funded by the Project of
Taizhou Techonology Bureau in Zhejiang province (grant no.
1301ky31).
Availability of data and materials
The datasets used and/or analyzed during the present
study available from the corresponding author on reasonable
request.
Authors' contributions
DJX performed the surgery and drafted the
manuscript. LJZ revised the manuscript and guided the treatment
plan. HJW acquired, analyzed and interpretation of data.
Ethics approval and consent to
participate
The current study was conducted with approval from
the Ethics Committee of Taizhou Municipal Hospital of Taizhou
University (Zhejiang, China). Written informed consent was obtained
from all individuals involved.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Davison JA: Capsule contraction syndrome.
J Cataract Refract Surg. 19:582–589. 1993.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Werner L, Pandey SK, Escobar-Gomez M,
Visessook N, Peng Q and Apple DJ: Anterior capsule opacification: A
histopathological study comparing different IOL styles.
Ophthalmology. 107:463–471. 2000.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Michael K, O'Colmain U, Vallance JH and
Cormack TG: Capsule contraction syndrome with haptic deformation
and flexion. J Cataract Refract Surg. 36:686–689. 2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wang YL, Wang ZZ, Zhao L, Xiong SH, Li Q,
Wang NL and Sun AQ: Finite element analysis of neodymium:
Yttrium-aluminum-garnet incisions for the prevention of anterior
capsule contraction syndrome. Chin Med J (Engl). 126:692–696.
2013.PubMed/NCBI
|
|
5
|
Shin MH, Kang HJ, Kim SJ, Chung IY, Seo
SW, Yoo JM, Park JM and Han YS: Effect of Nd:YAG Laser Capsulotomy
on anterior segment parameters in patients with posterior capsular
opacification after phacovitrectomy. Korean J Ophthalmol.
32:369–375. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Panagopoulos A, Chalioulias K and Kirkby
GR: A new approach in the surgical management of anterior capsular
phimosis syndrome. Ophthalmic Res. 42:221–223. 2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Altintas AG, Dal D and Simsek S:
Significant intraocular lens folding due to severe capsular
contraction. Jpn J Ophthalmol. 52:134–136. 2008.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhai J: Thirty-years studying of Mullerian
logarithmic visual acuity chart and 5 points recording. J Wenzhou
Med Univ. 29:37–38. 1990.
|
|
9
|
Agarwal A and Jacob S: Current and
effective advantages of femto phacoemulsification. Curr Opin
Ophthalmol. 28:49–57. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Sorenson AL, Holladay JT, Kim T, Kendall
CJ and Carlson AN: Ultrasonographic measurement of induced myopia
associated with capsular bag distention syndrome. Ophthalmology.
107:902–908. 2000.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Malik A, Gupta N and Sood S: Capsular
contraction syndrome following insertion of hydrophilic acrylic
lens. Int Ophthalmol. 31:121–123. 2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zaugg B, Werner L, Neuhann T, Burrow M,
Davis D, Mamalis N and Tetz M: Clinicopathologic correlation of
capuslorhexis phimosis with anterior flexing of single-piece
hydrophilic acrylic intraocular lens haptics. J Cataract Refract
Surg. 36:1605–1609. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Vock L, Georgopoulos M, Neumayer T, Buehl
W and Findl O: Effect of the hydrophilicity of acrylic intraocular
lens material and haptic angulation on anterior capsule
opacification. Br J Ophthalmol. 91:476–480. 2007.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lam FC, Livingstone I, Imrie FR and Mantry
S: Delayed dislocation of an injectable hydrophilic acrylic lens
after Nd:YAG capsulotomy in anterior capsular contraction syndrome.
Cont Lens Anterior Eye. 34:193–195. 2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Page TP and Whitman J: A stepwise approach
for the management of capsular contraction syndrome in hinge-based
accommodative intraocular lenses. Clin Ophthalmol. 10:1039–1046.
2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lanzl IM and Kopp C: Ciliary body
detachment caused by capsule contraction. J Cataract Refract Surg.
25:1412–1414. 1999.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tian T, Liu W and Ji J: Current progress
in capsular contractionsyndrome. Zhonghua Yan Ke Za Zhi. 49:79–83.
2013.(In Chinese). PubMed/NCBI
|
|
18
|
Caravella LP: Laser treatment alternative
to IOL exchange for capsulorhexis phimosis with anterior flexing of
single-piece hydrophilic acrylic IOL haptics. J Cataract Refract
Surg. 36:2222–2223. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Hayashi K, Yoshida M, Hirata A and Hayashi
H: Anterior capsule relaxing incisions with neodymium: YAG laser
for patients at high-risk for anterior capsule contraction. J
Cataract Refract Surg. 37:97–103. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wu H, Zhang L, Jin L, Xu Z and Xu D:
Capsular bag relaxing surgery for capsular contraction syndrome.
Int J Clin Exp Med. 9:21842–21847. 2016.
|
|
21
|
McCannel CA: Continuous curvilinear
capsulorhexis training and Non-Rhexis related vitreous loss: The
specificity of virtual reality simulator surgical training (An
American Ophthalmological Society Thesis). Trans Am Ophthalmol Soc.
115(T2)2017.PubMed/NCBI
|
|
22
|
Yeh PC, Goins KM and Lai WW: Managing
anterior capsule contraction by mechanical widening with
vitrector-cut capsulotomy. J Cataract Refract Surg. 28:217–220.
2002.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Reyntjens B, Tassignon MJ and Van Marck E:
Capsular peeling in anterior capsule contraction syndrome: Surgical
approach and histopathological aspects. J Cataract Refract Surg.
30:908–912. 2004.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Jin-Poi T, Shatriah I, Khairy-Shamel ST
and Zunaina E: Rapid anterior capsular contraction after
phacoemulsification surgery in a patient with retinitis pigmentosa.
Clin Ophthalmol. 7:839–842. 2013.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Elies Amat D, Coret Moreno A, Mauricio
Casanovas J, Rombouts Matamala A and Gatell Tortajada J: Surgical
management of the capsular contraction syndrome. Arch Soc Esp
Oftalmol. 77:377–380. 2002.PubMed/NCBI
|
|
26
|
Balestrazzi A, Malandrini A, Martone G,
Marigliani D, Caporossi T and Tosi GM: Capsule contraction syndrome
with a microincision foldable hydrophilic acrylic intraocular lens:
Two case reports and review of the literature. Case Rep Ophthalmol.
5:329–335. 2014.PubMed/NCBI View Article : Google Scholar
|