Introduction
Atrial fibrillation (AF) is a clinical arrhythmia
with an incidence of <1% in people <60 years, >12% in
people >60 years and >20% in people >85 years (1,2). The
occurrence of AF significantly increases the risk of death from
underlying heart disease up to 3-fold in patients with chronic
heart failure (3,4). AF also results in hemodynamic disorders
and thrombosis, and arterial embolism caused by thrombus detachment
can result in severe clinical consequences, especially stroke
(3,4). Patients with AF benefit from medication
and surgery; however, the overall prognosis remains poor,
especially in older patient. Therefore, discovery of novel
therapeutic targets to prevent the progression of AF is
necessary.
It has been revealed that interleukin (IL) family
members serve critical roles in the occurrence and progression of
AF (5). A previous study reported
that polymorphism of the IL-1 receptor antagonist gene allele 2
resulted in a poorly restricted inflammatory response and promoted
the presence of lone AF (6).
However, improved cardioversion outcomes were reported in AF
patients with low serum IL-2 levels compared with those with high
serum IL-2 levels (7). The -174G/C
IL-6 polymorphism was reported to increase the incidence of AF in
patients who underwent coronary artery bypass surgery (8). In addition, anti-IL-17A monoclonal
antibodies markedly decrease the development of AF induced by
transesophageal burst pacing, while elevated circulating IL-17A
levels increased the recurrence rate of AF following catheter
ablation (9,10). The G allele and the GG genotype of
the IL-27 gene rs153109 polymorphism significantly elevated AF
susceptibility in the Chinese Han population (11).
IL-22 is a multifunctional cytokine and its
expression is mainly affected by inflammation. It is involved in a
variety of biological processes, including inflammatory reactions,
oxidative stress, apoptosis, autophagy, cell migration and
endothelial dysfunction (12-16).
Previous studies revealed that IL-22 regulates the progression of a
variety of cardiovascular diseases, including hypertension, cardiac
fibrosis, aortic dissection, atherosclerosis and viral myocarditis
(16-21).
However, the expression of IL-22 in patients with AF is yet to be
elucidated. Therefore, in the present study, the expression of
IL-22 in atrial tissue and plasma from patients with AF was
measured and the effects of IL-22 on transforming growth factor β1
(TGF-β1)-treated cardiac fibroblasts were determined.
Materials and methods
Sample collection
For atrial tissue sample collection, patients with
valvular and rheumatic heart disease who had undergone heart valve
replacement were enrolled in the present study. Based on their AF
histories and the results of a 12-lead electrocardiogram, the
patients (n=56) were divided into a permanent AF group (n=35),
which included patients who had experienced AF for >6 months,
and a sinus rhythm group (n=21), which included patients without a
history of AF. No significant pathological changes were observed in
the atrial tissue structure in patients of the sinus rhythm group.
Both the left and right atrial appendages were collected by cardiac
surgeons at the time of surgery and then divided into two subsets.
One subset was fixed in 4% paraformaldehyde, and the other subset
was rapidly cooled in liquid nitrogen and transferred to a -80˚C
freezer for preservation.
For blood sample collection, consecutive patients
with AF were prospectively enrolled in the present study. Among all
patients, those who had a history or were recently found to suffer
from diseases that affect IL-22 expression, including chronic
kidney failure, tumors, coronary heart disease, chronic heart
failure, connective tissue disease, additional arrhythmias and
cardiac structural abnormalities, were excluded from the present
study. Patients with other diseases, such as connective tissue
disease, that affect IL-22 secretion were also excluded.
Dependent on the duration of AF, the remaining
patients (n=155) were divided into paroxysmal AF (n=35), persistent
AF (n=45) and permanent AF (n=75) groups, according to the American
College of Cardiology/American Heart Association/Heart Rhythm
Society AF guidelines published in 2014 (22-24).
AF lasting <7 days was defined as paroxysmal AF, AF lasting
>7 days that was successfully converted into sinus rhythm was
defined as persistent AF and AF lasting >7 days that could not
be converted into sinus rhythm was defined as permanent AF.
Additional donors without history of AF (n=40) were used as
controls. All blood samples were obtained from the ulnar vein by
nurses and were then centrifuged (4,000 x g, 4˚C, 15 min) and
stored at -80˚C.
All patients provided written informed consent. All
samples were collected at the People's Hospital of Guangxi Zhuang
Autonomous Region. The study protocol was approved by the Medical
Ethics Committee of the People's Hospital of Guangxi Zhuang
Autonomous Region (Nanning, China; approval no. 201725GX-H).
Western blot analysis
Human atrial tissue was dissolved in RIPA buffer [50
mM; Tris (pH 7.4), 150 mM NaCl, 1% TritonX-100, 1% sodium
deoxycholate, 0.1% SDS, 2 mM sodium pyrophosphate, 25 mM
odglycerophosphate, 1 mM EDTA, 1 mM Na3VO4,
0.5 µ/ml leupeptin 25˚C] and further lysed at 5,000 Hz using an
Ultrasonic Lysimeter (model, XL-2000; Misonix). Subsequently, the
atrial tissue homogenate was centrifuged at 6,000 x g at 4˚C for 15
min. The supernatant of each sample was collected and total protein
concentration was detected using a bicinchoninic acid Protein Assay
kit (Thermo Fisher Scientific, Inc.). A total of 30 µg protein with
different molecular weights were separated via electrophoresis on a
10% gel. After transferring the separated proteins to Immobilon-FL
PVDF membranes (EMD Millipore) at 200 mA for 1 h, the blots were
blocked with 5% nonfat milk (25˚C, 1 h) and incubated with
antibodies against IL-22R1 (1:1,000; cat. no. GTX16978; GeneTex,
Inc.), IL-10R2 (1:1,000; cat. no. GTX00131-pro; GeneTex, Inc.),
IL-22 (1:1,000; cat. no. GTX109659; GeneTex, Inc.) and GAPDH
(1:1,000; cat. no. 5174; Cell Signaling Technology, Inc.) at 4˚C
for 10 h. Following incubation with goat anti-rabbit IgG H&L
Alexa Fluor 647 secondary antibody (1:10,000; cat. no. 150079;
Abcam) at 25˚C for 1 h, the blots were scanned using the Odyssey
Imaging System (LI-COR Biosciences).
Detection of collagen expression in
atria
After fixation at 25˚C for 4 days, the atrial tissue
was removed from 4% paraformaldehyde and embedded in paraffin.
Subsequently, the atria were cut into 5-6 mm slices, and
picrosirius red staining (25˚C; 1 h) was performed to detect the
fibrotic areas in the atrium of each sample using a light
microscope at x200 magnification. Collagen expression was
quantified using ImageJ software v1.8.0 (National Institutes of
Health).
Detection of fibrosis marker mRNA
expression
Atrial tissue was cut into small pieces and lysed
using 1 ml TRIzol® Reagent (cat. no. 15596026;
Invitrogen; Thermo Fisher Scientific, Inc.) per 100 mg tissue
according to the manufacturer's instructions. Cardiac fibroblasts
were also lysed using TRIzol® Reagent (Invitrogen;
Thermo Fisher Scientific, Inc.). Total mRNA was collected and the
concentration was determined using a NanoDrop™ 2000C
spectrophotometer (Thermo Fisher Scientific, Inc.). mRNA was
reverse transcribed into cDNA using a Transcriptor First Strand
cDNA Synthesis kit (cat. no. 04896866001; Roche Diagnostics) at
92˚C for 5 min. PCR amplification was performed to detect the mRNA
levels of TGF-β1, collagen I, collagen III and α-smooth muscle
actin (SMA) using the FastStart Universal SYBR Green Mastermix
(cat. no. 04913914001; Roche Diagnostics). The following
thermocycling conditions were used for the PCR: 35 cycles at 92˚C
for 30 sec, 58˚C for 40 sec, and 72˚C for 35 sec. Gene expression
levels were normalized to GAPDH levels using the 2-ΔΔCq
method (25). Primers were purchased
from Tsingke Biological Technology Co., Ltd., and the sequences are
listed in Table I.
 | Table ISequences of primers used in reverse
transcription-quantitative PCR. |
Table I
Sequences of primers used in reverse
transcription-quantitative PCR.
| Species | Gene | Forward primer
(5'→3') | Reverse primer
(5'→3') |
|---|
| Human | TGF-β1 |
TGCTTCAGCTCCACAGAAA |
GTATCCAGGCTCCAGATGTAAG |
| Human | Collagen I |
GAGGGCCAAGACGAAGACATC |
CAGATCACGTCATCGCACAAC |
| Human | Collagen III |
CTGGACCCCAGGGTCTTC |
CATCTGATCCAGGGTTTCCA |
| Human | GAPDH |
GAAGGTGAAGGTCGGAGTC |
CTGGGTGGCAGTGATGGCATGG |
| Mouse | α-SMA |
TCCTGACGCTGAAGTATCCGATA |
GGCCACACGAAGCTCGTTAT |
| Mouse | Collagen I |
TGGTACATCAGCCCGAAC |
GTCAGCTGGATAGCGACA |
| Mouse | Collagen III |
ACGTAGATGAATTGGGATGCAG |
GGGTTGGGGCAGTCTAGTC |
| Mouse | GAPDH |
AACTTTGGCATTGTGGAAGG |
CACATTGGGGGTAGGAACAC |
Measurement of plasma IL-22 and TGF-β1
levels
Blood samples were thawed at 4˚C. Plasma IL-22 and
TGF-β1 levels in each sample were then investigated using IL-22
(cat. no. BMS2047; Invitrogen; Thermo Fisher Scientific, Inc.) and
TGF-β1 (cat. no. PHG9211; Invitrogen; Thermo Fisher Scientific,
Inc.) ELISA kits, according to the manufacturer's instructions.
Cell culture and treatment
Primary mouse cardiac fibroblasts were purchased
from ScienCell Research Laboratories (cat. no. M6300) and cultured
in DMEM/F12 (cat. no. A4192101; Gibco; Thermo Fisher Scientific,
Inc.) with 10% FBS (cat. no. 16140071; Gibco; Thermo Fisher
Scientific, Inc.). Following culture in serum-free DMEM/F12 for 12
h, the cardiac fibroblasts were treated with vehicle (DMSO; cat.
no. D12345; Invitrogen; Thermo Fisher Scientific, Inc.),
recombinant mouse IL-22 (10 ng/ml; cat. no. AF-210-22-2; PeproTech,
Inc.), JNK pathway inhibitor SP600125 (30 µM; cat. no. tlrl-sp60;
InvivoGen) or recombinant TGF-β1 (10 ng/ml; PeproTech, cat. no.
AF-100-21M-2; PeproTech, Inc.) (17,26,27), and
saline treatment as control. Following treatment at 37˚C for 12 h,
fibrosis expression in cardiac fibroblasts was detected. First, a
subset of cardiac fibroblasts were seeded on glass coverslips.
After fixation with 4% paraformaldehyde at 25˚C for 15 min, cells
were stained with anti-α-SMA antibody (1:200; cat. no. ab32575;
Abcam) at 25˚C and Alexa 568-conjugated secondary antibody (1:200;
cat. no. ab175473; Abcam) at 25˚C for 2 h. Stained cells were
observed using a fluorescence microscope (Olympus Corporation) at
x400 magnification.
Statistical analysis
SPSS 23.0 (IBM Corp.) was used to analyze the data.
Continuous variables are expressed as the mean ± SD. Unpaired
Student's t-test was used to analyze differences between two
groups, while one-way ANOVA followed by the Tukey's post-hoc test
was performed to analyze differences between three or more groups.
Classification variables are expressed as percentages and were
compared using Fisher's exact test. The correlation between IL-22
expression and fibrosis marker expression was analyzed using
Spearman's correlation analysis. Linear regression was performed to
determine whether IL-22 or TGF-β1 levels were associated with the
occurrence of AF. P<0.05 was considered to indicate a
statistically significant difference.
Results
Clinical characteristics
Among the patients who provided atrial samples,
longer durations of AF and larger left atrial dimensions were found
in the permanent AF group compared with the sinus rhythm group. No
differences were observed in other clinical characteristics,
including sex, age, incidence of hypertension, type 2 diabetes,
basic heart disease, valve disease, left ventricular (LV)
end-diastolic diameter and LV ejection fraction. The clinical
characteristics of these two groups are listed in Table II.
 | Table IIClinical characteristics of patients
in the sinus rhythm and permanent AF groups. |
Table II
Clinical characteristics of patients
in the sinus rhythm and permanent AF groups.
| Characteristic | Sinus rhythm
(n=21) | Permanent AF
(n=35) | P-value |
|---|
| Male, n (%) | 12.0 (57.1) | 25.0 (71.4) | 0.383 |
| Age (years) | 55.2±11.2 | 57.6±14.0 | 0.411 |
| Smoking, n (%) | 7.0 (33.3) | 19.0 (54.3) | 0.170 |
| Hypertension, n
(%) | 6.0 (28.6) | 19.0 (57.1) | 0.096 |
| Type 2 diabetes, n
(%) | 3.0 (14.3) | 12.0 (34.3) | 0.128 |
| Duration of AF
(days) | 0.0 | 149.2±88.5 | <0.001 |
| Basic heart
disease | | | |
|
Rheumatic
heart disease (n, %) | 14.0 (66.7) | 28.0 (80.0) | 0.343 |
|
Valvular
heart disease, n (%) | 7.0 (33.3) | 7.0 (20.0) | 0.343 |
| Diseased valve | | | |
|
Mitral
valves involved, n (%) | 9.0 (42.9) | 17.0 (48.6) | 0.785 |
|
Aortic
valves involved, n (%) | 5.0 (23.8) | 9.0 (25.7) | 0.999 |
|
Combined
valvular disease, n (%) | 7.0 (33.3) | 9.0 (25.7) | 0.557 |
| Cardiac
structure | | | |
|
LA dimension
(mm) | 36.5±4.6 | 49.1±11.1 | <0.001 |
|
LV
end-diastolic diameter (mm) | 44.1±4.7 | 46.9±6.7 | 0.099 |
|
LV ejection
fraction (%) | 56.9±4.7 | 55.1±4.2 | 0.143 |
Among the blood sample donors, those in the
permanent AF group were older compared with the control group. The
duration of AF gradually increased from the control group to the
paroxysmal AF group, to the persistent AF group to the permanent AF
group. In addition, the left atrium (LA) dimensions and LV
end-diastolic diameter were larger and the LV ejection fraction was
lower in the permanent AF group compared with the other three
groups. Other characteristics, including sex, incidence of smoking,
hypertension, type 2 diabetes and basic heart disease, did not
differ between the four groups. The clinical characteristics of
each group are listed in Table
III.
 | Table IIIClinical characteristics of non-AF
donors and patients with AF. |
Table III
Clinical characteristics of non-AF
donors and patients with AF.
| | AF |
|---|
| Characteristic | Non-AF | Paroxysmal | Persistent | Permanent |
|---|
| Male, n (%) | 22.0 (55.0) | 23.0 (65.7) | 30.0 (66.7) | 53.0 (70.7) |
| Age (years) | 58.1±12.8 | 61.4±14.0 | 64.3±15.4 |
66.3±15.2a |
| Smoking, n (%) | 11.0 (27.5) | 15.0 (42.9) | 19.0 (47.5) | 32.0 (42.6) |
| Hypertension, n
(%) | 13.0 (32.5) | 14.0 (40.0) | 21.0 (52.5) | 31.0 (42.7) |
| Type 2 diabetes
(n,%) | 3.0 (7.5) | 2.0 (5.7) | 4.0 (10.0) | 7.0 (9.3) |
| Duration of AF
(days) | 0.0 |
2.0±0.7a |
4.7±1.9a,b |
128.1±56.2a-c |
| Basic heart
disease | | | | |
|
Rheumatic
heart disease, n (%) | 13.0 (32.5) | 9.0 (25.7) | 11.0 (27.5) | 33.0 (44.0) |
|
Valvular
heart disease, n (%) | 6.0 (15.0) | 4.0 (11.4) | 9.0 (22.5) | 13.0 (17.3) |
|
Dilated
cardiomyopathy, n (%) | 7.0 (17.5) | 7.0 (20.0) | 5.0 (12.5) | 11.0 (14.7) |
|
Hypertrophic
cardiomyopathy, n (%) | 6.0 (15.0) | 3.0 (8.6) | 8.0 (20.0) | 8.0 (20.0) |
|
Others, n
(%) | 8.0 (20.0) | 8.0 (20.0) | 7.0 (17.5) | 11.0 (14.7) |
| Cardiac
structure | | | | |
|
LA dimension
(mm) | 33.7±5.1 | 32.8±6.2 | 34.1±6.4 |
39.1±6.6a-c |
|
LV dimension
(mm) | 47.6±7.2 | 49.3±6.4 | 49.3±7.2 |
52.1±7.1a-c |
|
LV ejection
fraction (%) | 59.7±5.3 | 58.8±4.7 | 59.1±4.5 | 54.6±5.9 |
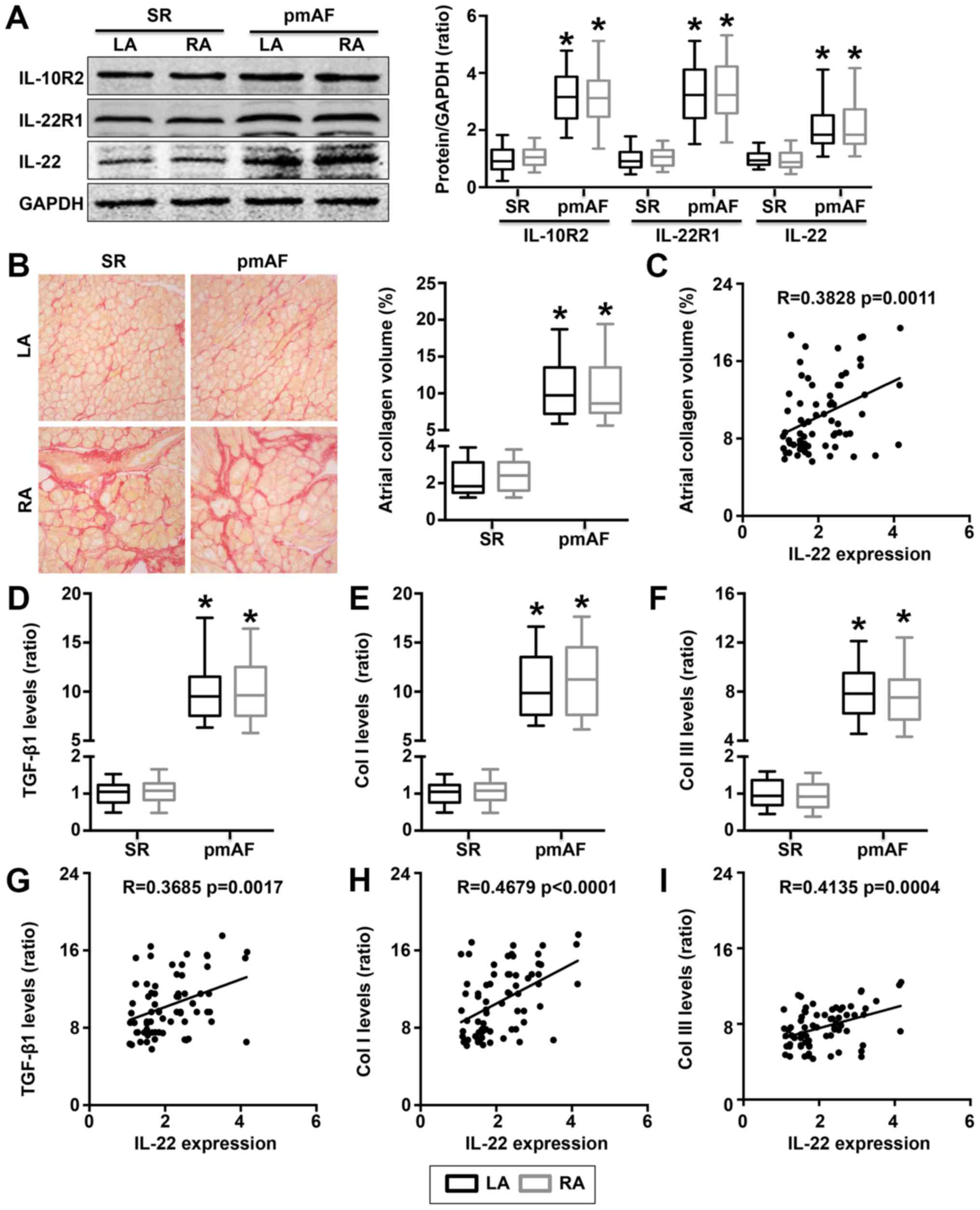
IL-22 levels are increased in the
atria of patients with permanent AF
Western blotting results indicated that IL-10R2,
IL-22R1 and IL-22 levels significantly increased in both the LA and
right atrium (RA) in the permanent AF group compared with the sinus
rhythm group (Fig. 1A). Increased
trends of IL-22 levels were observed in the collagen area (Fig. 1B). Atrial IL-22 expression positively
correlated with the atrial collagen area percentage in patients
with permanent AF (Fig. 1C). In
addition, levels of fibrosis-related signaling pathway members and
fibrosis markers, such as TGF-β1, collagen I and collagen III,
significantly increased in both the LA and RA of patients with
permanent AF compared with the sinus rhythm group (Fig. 1D-F). Positive correlations were
observed between elevated TGF-β1, collagen I and collagen III mRNA
levels and increased IL-22 expression (Fig. 1G-I).
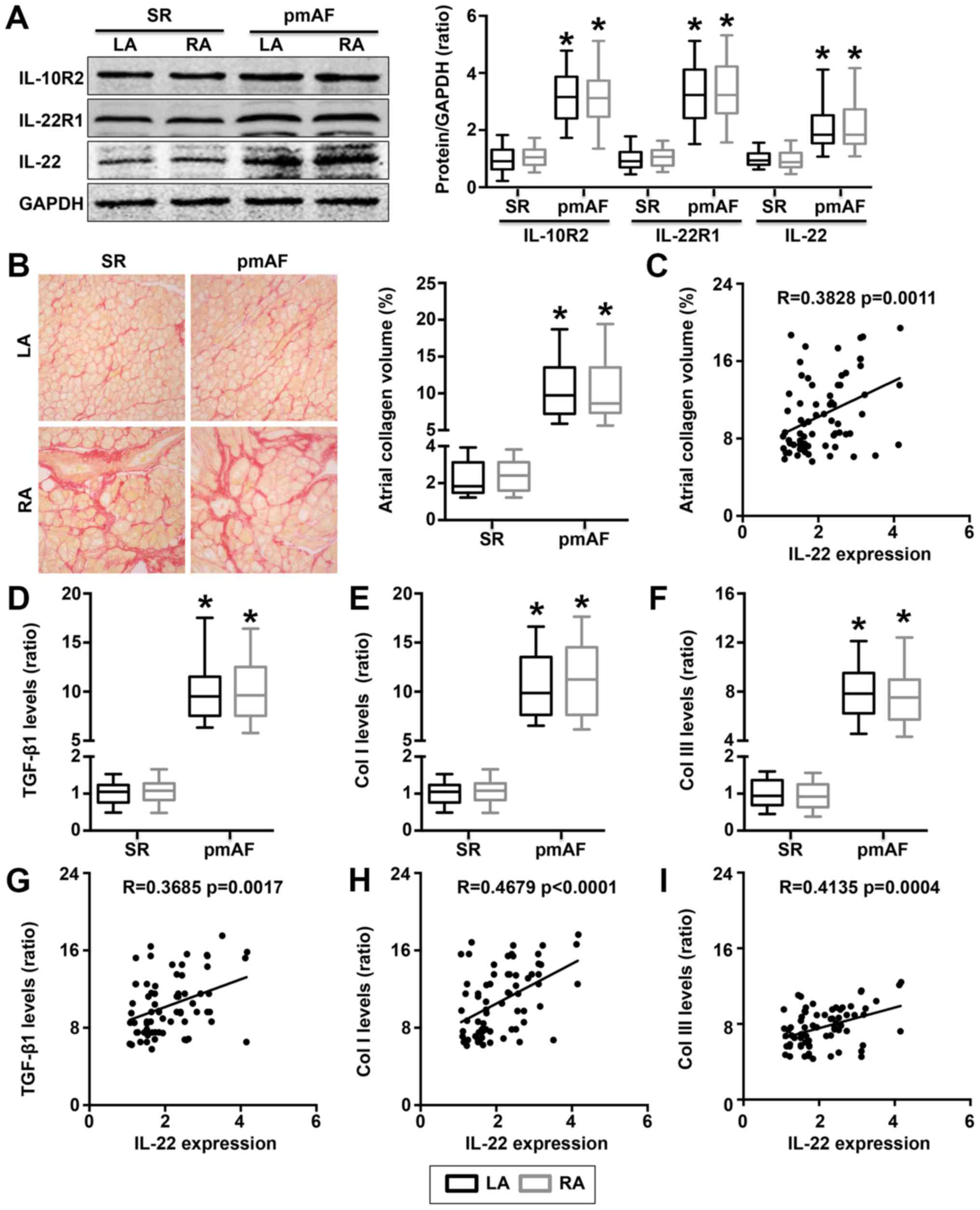 | Figure 1Atrial IL-22 expression in patients
with pmAF. (A) IL-10R2, IL-22R1 and IL-22 expression in both the LA
and RA of the SR and pmAF patient groups. (B) Atrial collagen
volume in the LA and RA in the two groups were quantified by Image
J softwore after magnification by 400 by a light microscope. (C)
Correlation between atrial IL-22 and atrial collagen area. (D)
TGF-β1, (E) collagen I and (F) collagen III mRNA expression in the
LA and RA of each group of all AF patients. Correlation between
atrial (G) TGF-β1, (H) collagen I and (I) collagen III mRNA
expression and atrial IL-22 expression. *P<0.05 vs.
the SR group. AF, atrial fibrillation; SR, sinus rhythm; pmAF,
permanent atrial fibrillation; IL, interleukin; LA, left atrium;
RA, right atrium; Col I, collagen I; Col III, collagen III; TGF-β1,
transforming growth factor-β1. |
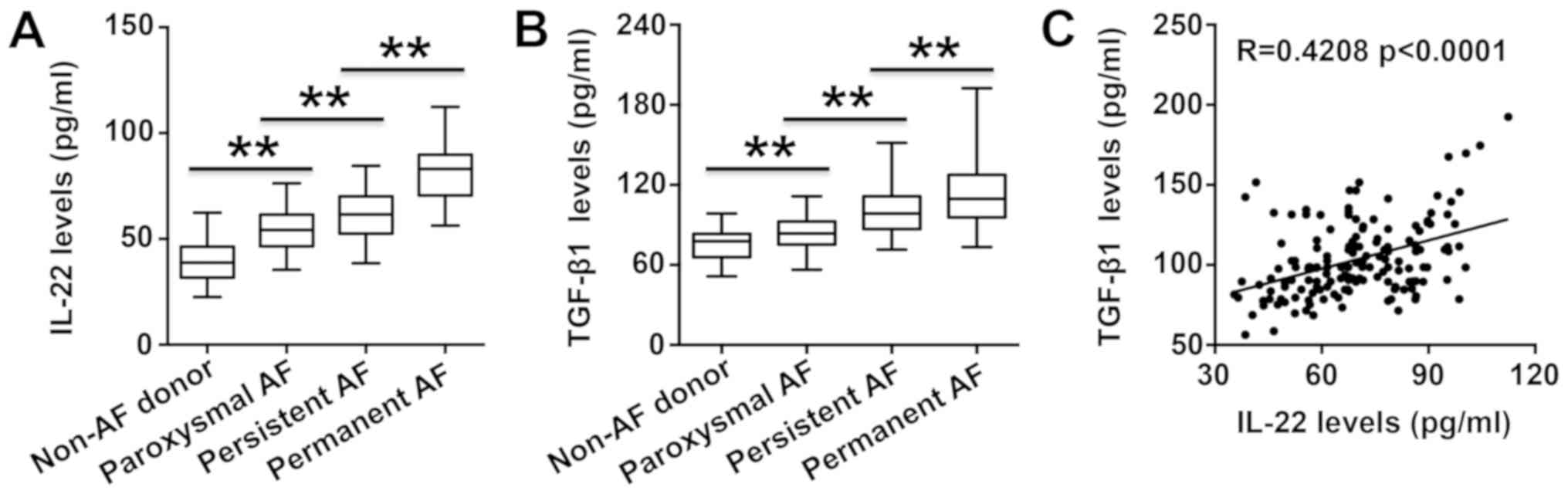
Plasma IL-22 levels are elevated in
patients with AF
As demonstrated by ELISA, plasma IL-22 levels were
significantly higher in all AF groups compared with the non-AF
group (Fig. 2A). IL-22 levels
gradually increased with increasing AF duration (from the
paroxysmal AF group to the persistent AF group to the permanent AF
group) (Fig. 2A). Circulating TGF-β1
levels also revealed similar trends to plasma IL-22 levels
(Fig. 2B). A positive correlation
between TGF-β1 levels and IL-22 levels was demonstrated in all
patients with AF (Fig. 2C).
IL-22 expression is associated with
AF
Clinical characteristics which were demonstrated
with fibrosis or related to the presence of AF, including IL-22
levels, TGF-β1 levels, sex, age, incidence of smoking,
hypertension, and type 2 diabetes and the left atrial dimension,
were included in univariate analysis. IL-22 levels, TGF-β1 levels,
smoking incidence, hypertension incidence and left atrial dimension
may be related to the presence of AF. These variables were used for
further multivariate linear regression analysis. The results
demonstrated that both plasma IL-22 and TGF-β1 levels were
independently associated with the presence of AF. The β, 95%
confidence interval and P-values for each variable are listed in
Table IV.
 | Table IVUnivariate analysis and multivariate
linear regression analysis results. |
Table IV
Univariate analysis and multivariate
linear regression analysis results.
| | Univariate
analysis | Multivariate
analysis |
|---|
| Variable | β-value | 95% CI | P-value | β-value | 95% CI | P-value |
|---|
| IL-22 | 0.578 | 0.319-0.837 | <0.001 | 0.276 | 0.319-0.837 | 0.008 |
| TGF-β1 | 0.411 | 0.257-0.565 | <0.001 | 0.197 | 0.148-0.246 | 0.017 |
| Male | 0.233 | 0.174-0.292 | 0.247 | | | |
| Age | 0.171 | 0.125-0.217 | 0.566 | | | |
| Smoking | 0.204 | 0.152-0.256 | 0.046 | 0.094 | 0.068-0.120 | 0.392 |
| Hypertension | 0.116 | 0.098-0.134 | 0.015 | 0.067 | 0.037-0.097 | 0.037 |
| Type 2
diabetes | 0.098 | 0.079-0.117 | 0.174 | | | |
| LA dimension | 0.218 | 0.161-0.275 | 0.025 | 0.103 | 0.071-0.135 | 0.059 |
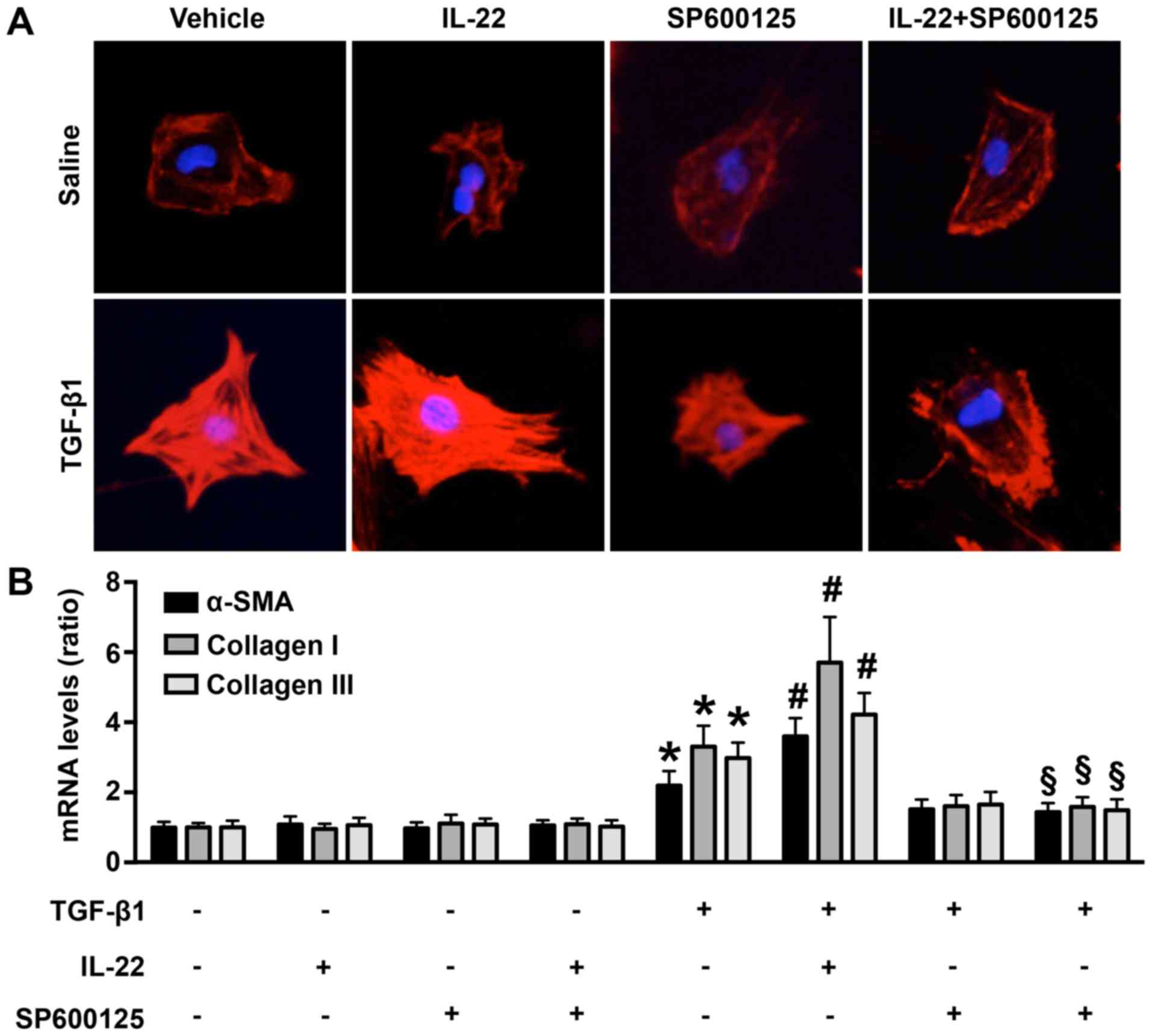
Recombinant IL-22 treatment
upregulates collagen synthesis in TGF-β1-treated cardiac
fibroblasts
In vitro, TGF-β1 treatment markedly increased
the expression of α-SMA in cardiac fibroblasts, indicating the
buildup of fibrosis following TGF-β1 treatment. These effects were
increased by IL-22 treatment, but partially reversed by SP600125
treatment (Fig. 3A). In addition,
TGF-β1 treatment significantly increased the mRNA expression levels
of the fibrosis markers α-SMA, collagen I and collagen III in
fibroblasts compared with groups not treated with TGF-β1 (Fig. 3B). The addition of exogenous IL-22
further increased fibrosis marker mRNA expression compared with
TGF-β1 alone (Fig. 3B). The
pro-fibrotic effect of IL-22 was partially reversed by SP600125
treatment (Fig. 3B). Neither IL-22
nor SP600125 affected collagen synthesis in cardiac fibroblasts
without TGF-β1 treatment (Fig.
3B).
Discussion
The present study examined the expression of IL-22
in patients with AF and investigated the association between IL-22
and fibrosis. Atrial IL-22 levels were elevated and positively
correlated with atrial fibrosis in permanent AF patients. In
addition, circulating IL-22 levels were also elevated and
positively correlated with TGF-β1 levels in patients with AF.
Moreover, in vitro, IL-22 treatment increased TGF-β1-induced
collagen fiber expression in mouse cardiac fibroblasts, and this
effect was partially restored by a JNK pathway inhibitor.
IL-22 is an immune-related cytokine secreted
primarily by macrophages and CD4+ T lymphocytes. An
increasing number of studies have reported that IL-22 expression is
increased in inflammation-mediated cardiovascular disease (16-21). Previous studies
reported that both T helper (Th) 22 and IL-22 levels were increased
in Coxsackie virus B3-induced acute and chronic viral myocarditis
and dilated cardiomyopathy (26,27). In
our previous study, circulating Th22/IL-22 levels were elevated in
patients with acute coronary syndrome (28). In addition, animal studies revealed
that circulating Th22 and IL-22 levels and cardiac IL-22 and
IL-22R1 levels were higher than baseline levels in angiotensin
II-infused mice (15,16). In clinical experiments, both
circulating IL-22 levels and aortic IL-22 expression were increased
in patients with human aortic dissection (17,18). The
present study obtained atrial tissue from patients with AF and
detected the expression of IL-22 and IL-22 receptors, including
IL-10R2 and IL-22R1. The current results revealed that IL-10R2,
IL-22R1 and IL-22 were all upregulated in the atrial tissue of
patients with AF. Similarly, it was demonstrated that circulating
IL-22 levels were elevated in patients with AF. The current
findings of elevated circulating IL-22 and atrial IL-22 levels
suggest that increased IL-22 expression is associated with AF.
Although the specific mechanisms underlying AF are
yet to be elucidated, multiple pathological factors were revealed
to influence the occurrence of AF, including inflammatory
responses, oxidative stress and left atrial apoptosis (8,9,29,30).
These injury factors may result in atrial remodeling, including
atrial structural changes and atrial fibrosis, which can cause
electrical remodeling and ultimately contribute to the onset and
progression of AF (31). Although it
has been reported that delaying atrial remodeling reduces the
occurrence and duration of AF (31,32), a
recently published long-term clinical follow-up study revealed that
both atrial fibrosis and atrial structural remodeling affected the
success rate and postoperative recurrence rate of AF following
radiofrequency ablation (32). These
indicates that electrical remodeling induced by atrial fibrosis may
represent the primary cause of the occurrence and development of AF
(32). In fact, increasing studies
have focused on atrial fibrosis as a mechanism for atrial
fibrillation, as data from animal studies and clinical experiments
have revealed that severe atrial fibrosis can result in a higher
incidence and duration of AF; in addition, the hypothesis that
inhibition of atrial fibrosis significantly inhibits the occurrence
and progression of AF has been increasingly accepted (33-35).
Inflammatory response-mediated fibrosis has been
widely researched, and the participation of inflammatory cytokines
in the progression of AF via mediation of atrial fibrosis has been
well documented (8,9). Furthermore, increased atrial
inflammatory responses have been associated with increased risk of
recurrent AF during follow-up (36).
Although the regulatory effect of IL-22 on the fibrotic process was
confirmed in previous studies (16-19),
the association between IL-22 and fibrosis in patients with AF was
further investigated in the present study. It was evidenced that
IL-22 expression positively correlates with TGF-β1, collagen I and
collagen III expression in the atrium, and with TGF-β1 levels in
plasma. According to the current results, IL-22 may participate in
AF progression via regulating atrial fibrosis. In addition, the
results of linear regression analysis indicated that both IL-22 and
TGF-β1 were associated with the occurrence of AF, further
supporting the aforementioned hypothesis.
IL-22 initiates downstream signaling pathways via
binding to IL-22 receptors, including IL-10R2 and IL-22R1, on
target cells, thereby regulating multiple biological effects,
including inflammation, oxidative stress, apoptosis and autophagy
(15). A variety of immune and
non-immune cells are targets of IL-22, including cardiac
fibroblasts (14). The downstream
signaling pathways of IL-22 include the STAT3 and mitogen-activated
protein kinase (ERK, JNK and P38) pathways. Previous research has
demonstrated that IL-22 regulates fibrosis via the JNK pathway
(16,37). Therefore, to further explore the
possible mechanisms underlying IL-22 regulation of AF, the effects
of exogenous IL-22 on collagen synthesis in TGF-β1-treated cardiac
fibroblasts were investigated. In addition, SP600125 was used to
block the JNK signaling pathway in cardiac fibroblasts. It was
revealed indicate that IL-22 may further increase TGF-β1-induced
collagen synthesis and that this effect was inhibited by treatment
with SP600125. These findings indicate that IL-22 activates the JNK
signaling pathway to increase fibrosis in vitro, and also
indicate that IL-22 increases atrial fibrosis via activation of the
JNK pathway during inflammatory response, thereby regulating the
progression of AF. However, animal studies still need to be
performed to confirm this hypothesis.
In summary, the present study revealed that IL-22
expression significantly increased in both the plasma and atrial
tissue of patients with AF compared with non-AF individuals, and
that elevated IL-22 expression positively correlated with the
expression of fibrosis-related markers. The results of the in
vitro studies suggested that IL-22 may regulate fibrosis via
the JNK signaling pathway. The present results also indicate that
IL-22 is closely associated with the occurrence of AF and may
represent a potential target for the clinical treatment of this
condition. However, the present research had certain limitations.
Firstly, the sample size of specimens, particularly atrial tissue
samples, was small; more patients should be included in future
studies. In addition, while the present results indicated that
IL-22 may participate in AF via regulating atrial fibrosis; the
specific mechanisms have not been investigated, and further in
vivo research is necessary to confirm this hypothesis.
Acknowledgements
The authors would like to thank Dr Jiao Lan from the
laboratory of Guangxi Zhuang Autonomous Region People's Hospital
for their technical support.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant nos. 81760051 and
81460061).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LL and YL conceived and designed the study; TZ and
YS collected the samples; YW, LT, LS, YX, YS and ZY performed the
experiments; TZ and YX analyzed the data; TZ and YS were involved
in drafting the manuscript or revising it critically for important
intellectual content; YW and YL reviewed and edited the manuscript;
YS and ZY gave final approval of the version to be published. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Medical
Ethics Committee of the People's Hospital of Guangxi Zhuang
Autonomous Region (Nanning, China; approval no. 201725GX-H).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Miyasaka Y, Barnes ME, Gersh BJ, Cha SS,
Bailey KR, Abhayaratna WP, Seward JB and Tsang TS: Secular trends
in incidence of atrial fibrillation in Olmsted County, Minnesota,
1980 to. 2000, and implications on the projections for future
prevalence. Circulation. 114:119–125. 2006.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Magnani JW, Rienstra M, Lin H, Sinner MF,
Lubitz SA, McManus DD, Dupuis J, Ellinor PT and Benjamin EJ: Atrial
fibrillation: Current knowledge and future directions in
epidemiology and genomics. Circulation. 124:1982–1993.
2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Wang TJ, Larson MG, Levy D, Vasan RS, Leip
EP, Wolf PA, D'Agostino RB, Murabito JM, Kannel WB and Benjamin EJ:
Temporal relations of atrial fibrillation and congestive heart
failure and their joint influence on mortality: The Framingham
Heart Study. Circulation. 107:2920–2925. 2003.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Olsson LG, Swedberg K, Ducharme A, Granger
CB, Michelson EL, McMurray JJ, Puu M, Yusuf S and Pfeffer MA: CHARM
Investigators. Atrial fibrillation and risk of clinical events in
chronic heart failure with and without left ventricular systolic
dysfunction: Results from the Candesartan in Heart
failure-Assessment of Reduction in Mortality and morbidity (CHARM)
program. J Am Coll Cardiol. 47:1997–2004. 2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Iscan S, Eygi B, Besir Y, Yurekli I, Cakir
H, Yilik L, Gokalp O and Gurbuz A: Inflammation, atrial
fibrillation and cardiac surgery: Current medical and invasive
approaches for the treatment of atrial fibrillation. Curr Pharm
Des. 24:310–322. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gungor B, Ekmekci A, Arman A, Ozcan KS,
Ucer E, Alper AT, Calik N, Yilmaz H, Tezel T, Coker A and Bolca O:
Assessment of interleukin-1 gene cluster polymorphisms in lone
atrial fibrillation: New insight into the role of inflammation in
atrial fibrillation. Pacing Clin Electrophysiol. 36:1220–1227.
2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Rizos I, Tsiodras S, Rigopoulos AG,
Dragomanovits S, Kalogeropoulos AS, Papathanasiou S, Sakadakis EA
and Kremastinos DT: Interleukin-2 serum levels variations in recent
onset atrial fibrillation are related with cardioversion outcome.
Cytokine. 40:157–164. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gaudino M, Andreotti F, Zamparelli R, Di
Castelnuovo A, Nasso G, Burzotta F, Iacoviello L, Donati MB,
Schiavello R, Maseri A and Possati G: The -174G/C interleukin-6
polymorphism influences postoperative interleukin-6 levels and
postoperative atrial fibrillation. Is atrial fibrillation an
inflammatory complication? Circulation. 108 (Suppl 1):II195–II199.
2003.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Fu XX, Zhao N, Dong Q, Du LL, Chen XJ, Wu
QF, Cheng X, Du YM and Liao YH: Interleukin-17A contributes to the
development of post-operative atrial fibrillation by regulating
inflammation and fibrosis in rats with sterile pericarditis. Int J
Mol Med. 36:83–92. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Xu L, Wang N, Liang Y, Zhou H and Yan J:
Interleukin-17A contributes to atrial fibrillation recurrence and
left atrial reservoir function after catheter ablation. Pol Arch
Intern Med. 129:432–435. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Chen Y, Zeng J, Zhang R, Zeng L, Li Y, Wei
H and Yang Q: Effect of interleukin-27 genetic variants on atrial
fibrillation susceptibility. Genet Test Mol Biomarkers. 21:97–101.
2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ki SH, Park O, Zheng M, Morales-Ibanez O,
Kolls JK, Bataller R and Gao B: Interleukin-22 treatment
ameliorates alcoholic liver injury in a murine model of
chronic-binge ethanol feeding: Role of signal transducer and
activator of transcription 3. Hepatology. 52:1291–1300.
2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Mo R, Lai R, Lu J, Zhuang Y, Zhou T, Jiang
S, Ren P, Li Z, Cao Z, Liu Y, et al: Enhanced autophagy contributes
to protective effects of IL-22 against acetaminophen-induced liver
injury. Theranostics. 8:4170–4180. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Perriard G, Mathias A, Enz L, Canales M,
Schluep M, Gentner M, Schaeren-Wiemers N and Du Pasquier RA:
Interleukin-22 is increased in multiple sclerosis patients and
targets astrocytes. J Neuroinflammation. 12(119)2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Dudakov JA, Hanash AM and van den Brink
MR: Interleukin-22: Immunobiology and pathology. Annu Rev Immunol.
33:747–785. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ye J, Ji Q, Liu J, Liu L, Huang Y, Shi Y,
Shi L, Wang M, Liu M, Feng Y, et al: Interleukin-22 promotes blood
pressure elevation and endothelial dysfunction in angiotensin
II-treated mice. J Am Heart Assoc. 6(005875)2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ye J, Liu L, Ji Q, Huang Y, Shi Y, Shi L,
Liu J, Wang M, Xu Y, Jiang H, et al:
Anti-interleukin-22-neutralizing antibody attenuates angiotensin
II-induced cardiac hypertrophy in mice. Mediators Inflamm.
2017(5635929)2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ye J, Wang M, Jiang H, Ji Q, Huang Y, Liu
J, Zeng T, Xu Y, Wang Z, Lin Y and Wan J: Increased levels of
interleukin-22 in thoracic aorta and plasma from patients with
acute thoracic aortic dissection. Clin Chim Acta. 486:395–401.
2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ye J, Wang Y, Wang Z, Ji Q, Huang Y, Zeng
T, Hu H, Ye D, Wan J and Lin Y: Circulating Th1, Th2, Th9, Th17,
Th22, and Treg levels in aortic dissection patients. Mediators
Inflamm. 2018(5697149)2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Rattik S, Hultman K, Rauch U, Söderberg
I, Sundius L, Ljungcrantz I, Hultgårdh-Nilsson A, Wigren M,
Björkbacka H, Fredrikson GN and Nilsson J: IL-22 affects smooth
muscle cell phenotype and plaque formation in apolipoprotein E
knockout mice. Atherosclerosis. 242:506–514. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kong Q, Xue Y, Wu W, Yang F, Liu Y, Gao M,
Lai W and Pan X: IL-22 exacerbates the severity of CVB3-induced
acute viral myocarditis in IL-17A-deficient mice. Mol Med Rep.
7:1329–1335. 2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
January CT, Wann LS, Alpert JS, Calkins H,
Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD,
Field ME, et al: 2014 AHA/ACC/HRS guideline for the management of
patients with atrial fibrillation: A report of the American College
of Cardiology/American Heart Association Task Force on Practice
Guidelines and the Heart Rhythm Society. J Am Coll Cardiol.
64:e1–e76. 2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Works MG, Yin F, Yin CC, Yiu Y, Shew K,
Tran TT, Dunlap N, Lam J, Mitchell T, Reader J, et al: Inhibition
of TYK2 and JAK1 ameliorates imiquimod-induced psoriasis-like
dermatitis by inhibiting IL-22 and the IL-23/IL-17 axis. J Immunol.
193:3278–3287. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Guillemot L and Citi S: Cingulin regulates
claudin-2 expression and cell proliferation through the small
GTPase RhoA. Mol Biol Cell. 17:3569–3577. 2006.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ma ZG, Yuan YP, Zhang X, Xu SC, Wang SS
and Tang QZ: Piperine attenuates pathological cardiac fibrosis Via
PPAR-γ/AKT pathways. EBioMedicine. 18:179–187. 2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Kong Q, Wu W, Yang F, Liu Y, Xue Y, Gao M,
Lai W, Pan X, Yan Y, Pang Y and Deng Y: Increased expressions of
IL-22 and Th22 cells in the coxsackievirus B3-induced mice acute
viral myocarditis. Virol J. 9(232)2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Guo Y, Wu W, Cen Z, Li X, Kong Q and Zhou
Q: IL-22-producing Th22 cells play a protective role in
CVB3-induced chronic myocarditis and dilated cardiomyopathy by
inhibiting myocardial fibrosis. Virol J. 11(230)2014.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lin YZ, Wu BW, Lu ZD, Huang Y, Shi Y, Liu
H, Liu L, Zeng QT, Wang X and Ji QW: Circulating Th22 and Th9
levels in patients with acute coronary syndrome. Mediators Inflamm.
2013(635672)2013.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Dong Z, Lin C, Liu Y, Jin H, Wu H, Li Z,
Sun L, Zhang L, Hu X, Wei Y, et al: Upregulation of sestrins
protect atriums against oxidative damage and fibrosis in human and
experimental atrial fibrillation. Sci Rep. 7(46307)2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Rosenberg JH, Werner JH, Plitt GD, Noble
VV, Spring JT, Stephens BA, Siddique A, Merritt-Genore HL, Moulton
MJ and Agrawal DK: Immunopathogenesis and biomarkers of recurrent
atrial fibrillation following ablation therapy in patients with
preexisting atrial fibrillation. Expert Rev Cardiovasc Ther.
17:193–207. 2019.PubMed/NCBI View Article : Google Scholar : 30. Jalife J and
Kaur K: Atrial remodeling, fibrosis, and atrial fibrillation.
Trends Cardiovasc Med 25: 475-484, 2015.
|
|
32
|
Thomas L and Abhayaratna WP: Left atrial
reverse remodeling: Mechanisms, evaluation, and clinical
significance. JACC Cardiovasc Imaging. 10:65–77. 2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Ali RL, Hakim JB, Boyle PM, Zahid S,
Sivasambu B, Marine JE, Calkins H, Trayanova NA and Spragg DD:
Arrhythmogenic propensity of the fibrotic substrate after AF
ablation: A longitudinal study using MRI-based atrial models.
Cardiovasc Res. 115:1757–1765. 2019.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Chang SH, Yeh YH, Lee JL, Hsu YJ, Kuo CT
and Chen WJ: Transforming growth factor-β-mediated CD44/STAT3
signaling contributes to the development of atrial fibrosis and
fibrillation. Basic Res Cardiol. 112(58)2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Cochet H, Dubois R, Yamashita S, Al
Jefairi N, Berte B, Sellal JM, Hooks D, Frontera A, Amraoui S,
Zemoura A, et al: Relationship between fibrosis detected on late
gadolinium-enhanced cardiac magnetic resonance and re-entrant
activity assessed with electrocardiographic imaging in human
persistent atrial fibrillation. JACC Clin Electrophysiol. 4:17–29.
2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Qu X, Chen L, Sun L, Chen C, Gao Z, Huang
W and Zhou H: Serum relaxin level predicts recurrence of atrial
fibrillation after radiofrequency catheter ablation. Heart Vessels.
34:1543–1551. 2019.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Rolla S, Alchera E, Imarisio C, Bardina V,
Valente G, Cappello P, Mombello C, Follenzi A, Novelli F and Carini
R: The balance between IL-17 and IL-22 produced by
liver-infiltrating T-helper cells critically controls NASH
development in mice. Clin Sci (Lond). 130:193–203. 2016.PubMed/NCBI View Article : Google Scholar
|