Introduction
Regarding the complications, respectively, maternal
and fetal morbidity and mortality, preeclampsia remains an ongoing
topic. Preeclampsia is called the disease of ‘theories’, given the
fact that it remains an enigma from many points of view. In the
last two decades, however, significant progress has been made in
elucidating the pathogenesis of preeclampsia, which is the key to
early detection of this condition and to the appropriate
therapeutic pathway (1). Even though
there are numerous studies concerning this topic, it is imperative
we clarify the methods of prevention and treatment, through a
well-established protocol with clear classification of the patient
in the high risk group and individualization of management and
monitoring according to a well-established scheme. The prevalence
of pathologies due to placental dysfunction superimposed on
pregnancy is constantly increasing in the context in which the
maternal age is also increasing from one decade to another.
However, in a significant number of cases, preeclampsia occurs in
nulliparous patients, with an apparent health status that presents
no obvious risk factors (2). The
impact of preeclampsia is not only limited to the specific
complications during pregnancy, birth or postpartum, but also
continues for a long time. The risk of maternal death is
significantly higher in patients who develop severe, early
preeclampsia with HR, 9.54; 95% CI, 4.50-20.25(3).
The prognosis of the cases complicated by
gestational hypertension is usually good, significantly better
compared with that of the cases associating preeclampsia, but the
concern about the complications that may occur should be just as
great. About half of the cases with gestational hypertension will
progress to preeclampsia, the risk of decompensation being
inversely proportional to the gestational age of the onset of
gestational hypertension (4).
Respectively, the earlier the gestational hypertension occurs
during pregnancy, the greater the risk of progression to
preeclampsia (5).
Subjects and methods
The present study, analyzed the cases of pregnancy
and postpartum complicated by pathologies related to placental
dysfunction, during a period of 5 years (2015-2019), by collecting
data from the medical statistics department of the University
Emergency Hospital Bucharest. The case groups include the control
group 1, respectively the general population, group 2, patients
with preexisting pregnancy hypertension, group 3 patients with
gestational hypertension, group 4 patients with moderate
preeclampsia, group 5 patients with severe preeclampsia, and group
6 patients with eclampsia. In the first stage of statistical
processing, descriptive tests were applied and the presence of risk
factors and complications in the studied groups was analyzed. In
the context in which the distribution of the data was not a
Gaussian one, non-parametric tests, respectively, Man Whitney U
were applied. For a better visualization and interpretation of the
results, classification tests were used. The program used was SPSS
12.0 and the statistical significance threshold considered was
P<0.05.
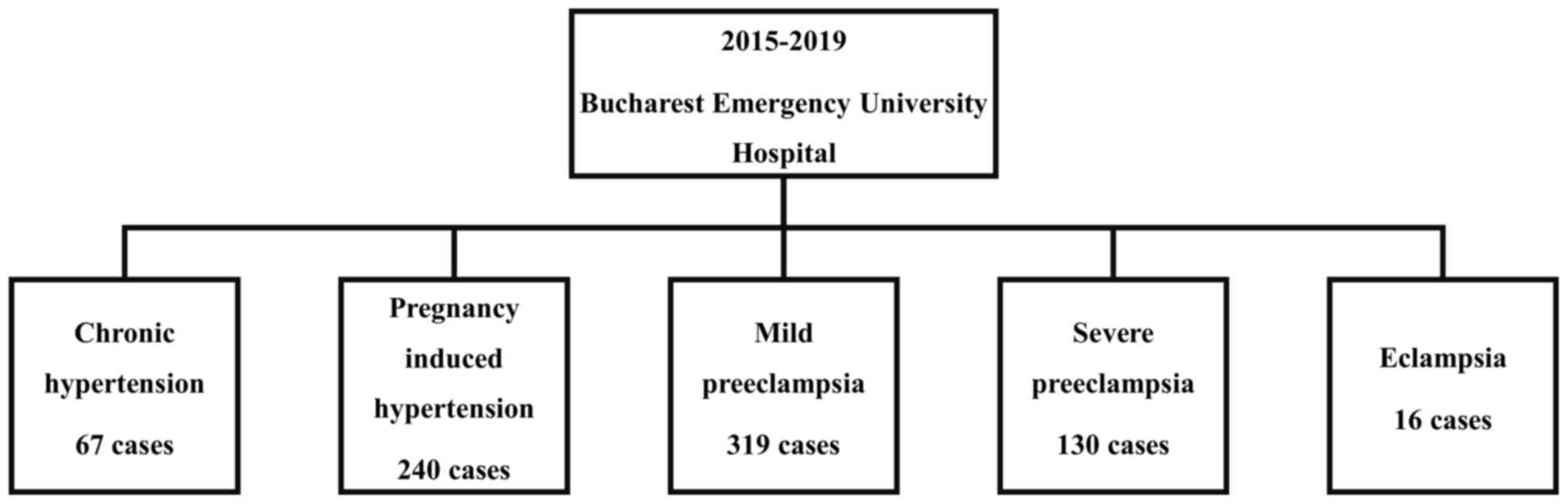
During the 5 years of study there were 67 cases of
pre-existing hypertension, 240 cases of gestational hypertension,
319 cases of moderate preeclampsia, 130 cases of severe
preeclampsia and 16 cases of eclampsia (Fig. 1).
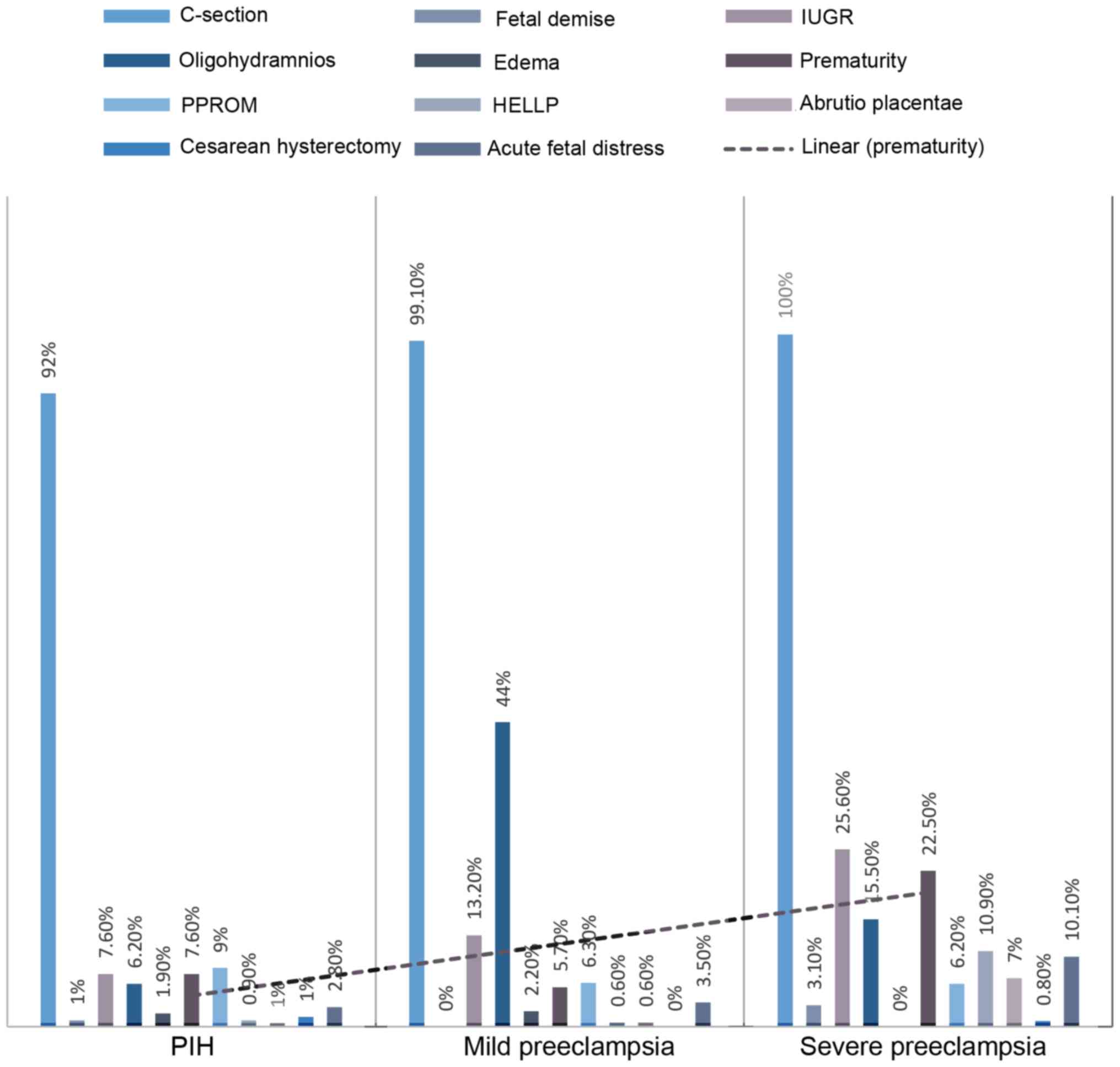
The main associated complications analyzed were
birth by Caesarean section, fetal death, intrauterine growth
restriction, oligohydramnios, gestational edema, premature birth,
preterm and premature rupture of membranes, HELLP syndrome,
abruptio placentae and caesarean hysterectomy. The frequency for
each studied group and their comparative reproduction is shown in
Fig. 2.
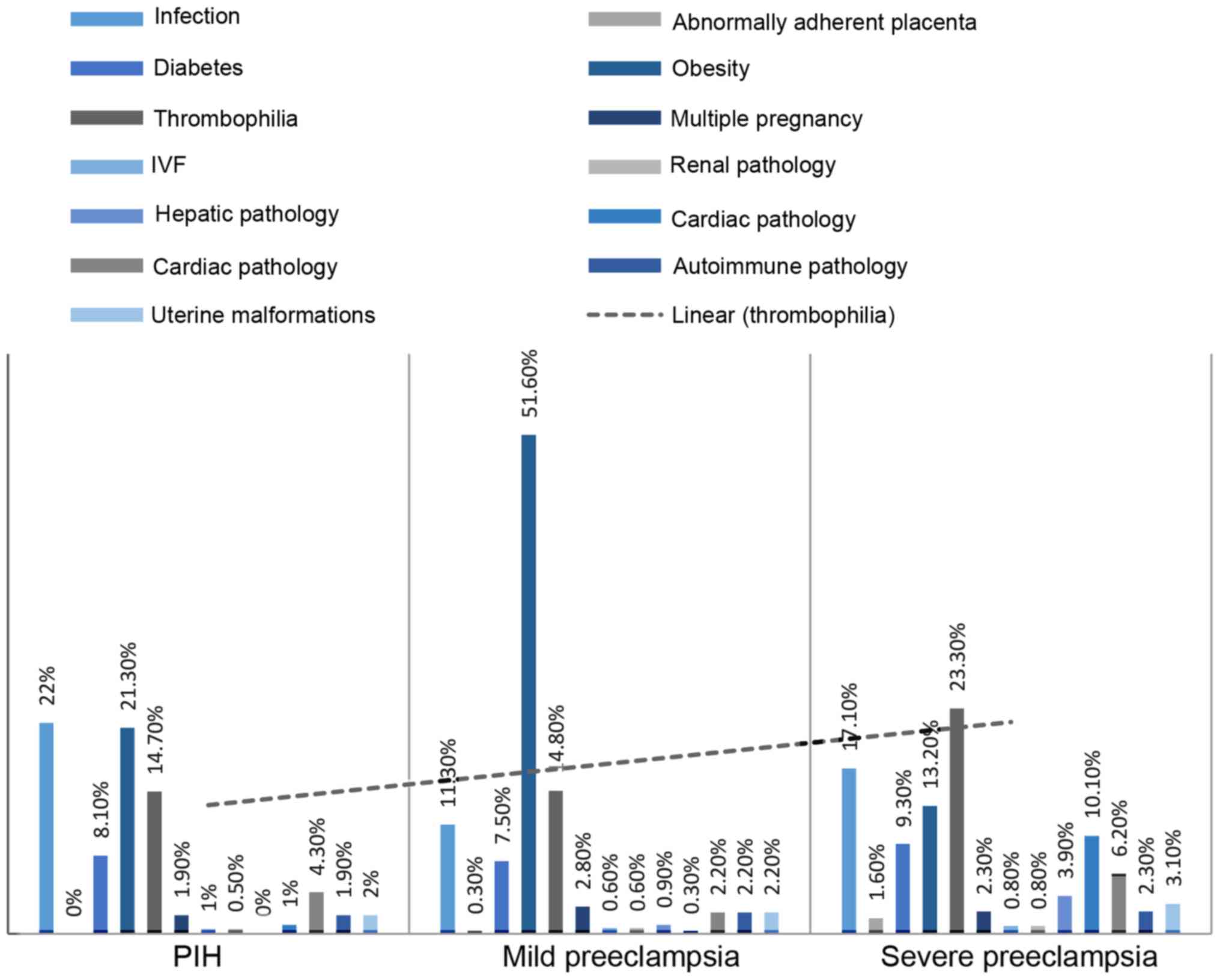
The risk factors analyzed were the presence of
infections during pregnancy, diabetes, thrombophilia, pregnancy
obtained by in vitro fertilization, abnormal adherence of
the placenta, obesity, multiple pregnancy, the presence of an
earlier hepatic, endocrine, renal, cardiac or autoimmune pathology,
and the existence of an uterine malformation. The frequency on the
studied groups is shown comparatively in Fig. 3.
Results
According to Mann Whitney tests, significant results
for the incidence of obesity were obtained by comparative analysis
of control group-1 (general population) with groups 3, 4 and 5,
respectively, patients with gestational hypertension, moderate
preeclampsia and severe preeclampsia. Obesity appears with a
significantly increased incidence in patients with gestational
hypertension and middle preeclampsia. IUGR appears with a
significantly increased incidence in patients with mild
preeclampsia. Complications such as prematurity, acute fetal
distress and abruption placentae had a significantly increased
incidence in patients with severe preeclampsia. The results of the
Mann Whitney tests are shown in Table
I, where only the coefficients of statistically significant
relationships are shown.
 | Table IRisk factors and complications for the
general population, in groups of women with gestational
hypertension, moderate preeclampsia and severe preeclampsia. |
Table I
Risk factors and complications for the
general population, in groups of women with gestational
hypertension, moderate preeclampsia and severe preeclampsia.
| | PIH | Mild
preeclampsia | Severe
preeclampsia |
|---|
|
Factor/complication | U | z | P-value | r | U | z | P-value | r | U | z | P-value | r |
|---|
| Obesity | 8,961 | -2.3 | 0.02 | -0.13 | 9,449 | -7.16 | 0 | -0.35 | | | | |
| Thrombophilia | | | | | 14,663 | -2 | 0.04 | -0.1 | -0.1 | -3.1 | 0 | -0.21 |
| IUGR | | | | | 14,595 | -2.2 | 0.02 | -0.11 | | | | |
| Oligohydramnios | | | | | 9,377 | -7.5 | 0 | -0.37 | 5,643.5 | -3.1 | 0 | -0.21 |
| Fetal demise | | | | | 15,264 | -3.5 | 0 | -0.17 | | | | |
| Prematurity | | | | | | | | | 5,387 | -3.4 | 0 | -0.23 |
| Acute fetal
distress | | | | | | | | | 5,929 | -2.4 | 0.01 | -0.16 |
| Abruptio
placentae | | | | | | | | | 6,064.5 | -2.2 | 0.03 | -0.15 |
Following the value of r, medium size effect was
recorded for obesity as a risk factor for mild preeclampsia,
compared with the general population, and varying from the upper
limit to large effect for oligohydramnios as a complication of mild
preeclampsia. Thus, the results show an important statistical
association and a cause-effect relationship for the conditions
described above compared with the other variables. For patients
with mild preeclampsia, we obtained a significantly higher
incidence of obesity and a high risk of oligohydramnios.
The effect of obesity is medium compared between the
two groups, respectively mild and severe preeclampsia, and
significantly differentiates the risk for mild preeclampsia.
In the context in which obesity was found as a
significant risk factor through non-parametric comparative tests
between the studied groups, a statistical analysis was used to
establish the severity index. It appears that the impact of this
condition is more significant for gestational hypertension and mild
preeclampsia, having a lower impact as a risk factor for severe
preeclampsia (Table II).
 | Table IIFrequency of obesity in study
groups. |
Table II
Frequency of obesity in study
groups.
| Group | No (%) | Yes (%) |
|---|
| Pregnancy induced
hypertension | 77.7 | 22.3 |
| Mild
preeclampsia | 48.4 | 51.6 |
| Severe
preeclampsia | 86.8 | 13.2 |
The ‘tree’ classification test on the impact of
obesity as a risk factor for the studied groups shows the existence
of a statistically significant difference depending on belonging to
one of the three categories. Thus, obese patients have a higher
risk of moderate preeclampsia, following gestational hypertension
and finally severe preeclampsia (Fig.
3).
Through the binary logistic regression model, which
has the category as dependent variable, the analysis of group 4,
patient with mild preeclampsia was compared with group 5, patients
with severe preeclampsia regarding the predictive value of the
significant risk factors obtained from the previous statistical
analysis, considered as independent variables. Thus, we intended to
highlight the predictive factors that significantly influence the
development of severe preeclampsia in patients with moderate
preeclampsia. The model has a χ2 (3) = 15.9, P<0.05 and explains 26.4% of
patients' probability of developing severe preeclampsia, when they
have moderate preeclampsia (Nagelkerke = 0.264). There are no large
correlation factors between the independent variables, so the
collinearity can be excluded (Table
III).
 | Table IIIMultinominal regression model for the
group of patients with moderate preeclampsia compared with the
group of patients with severe preeclampsia. |
Table III
Multinominal regression model for the
group of patients with moderate preeclampsia compared with the
group of patients with severe preeclampsia.
| | 95% CI for Exp
(B) |
|---|
| Factor | B (SE) | Inferior | Superior |
|---|
| Obesitya |
7.02 |
3.9 |
12.6 |
| Thrombophilia |
1.12 |
0.62 |
2.03 |
| Cardiac
pathologya |
0.035 |
0.004 |
0.293 |
| Hepatic
pathologya |
0.12 |
0.023 |
0.604 |
| Endocrine
pathology |
0.359 |
0.113 |
1.14 |
According to the results presented in Table III, obesity seems to be a
protective factor for patients with obesity and mild preeclampsia
to develop severe preeclampsia, instead a cardiac pathological
substrate or impaired hepatic function of patients with moderate
preeclampsia is an important negative predictor, increasing the
risk of developing severe preeclampsia. In order of impact, the
cardiac pathological substrate prevails, followed by the associated
liver pathology.
Discussion
In the study group, patients with mild preeclampsia
predominated, the incidence during the 5 years of study was 2.8%,
with a 1.3% incidence of severe preeclampsia and 3.57% of these
cases were complicated with eclampsia. According to the data
reported in the literature, namely a declared incidence of
pre-eclampsia of 2-8% with a progression rate to severe forms of
3.4-3.8% (6) our results
corresponded with these data. The incidence of cesarean birth
exceeded 90% in all the studied groups, and was 100% in the group
of patients with eclampsia, which is justified by the urgent nature
of these cases, the presentation in the stage of decompensation of
a significant proportion of these cases and the need for an
emergency termination of pregnancy, for both maternal and fetal
purposes (7).
At first glance, through the graphical presentation
of the study group, it can be observed that preterm birth
predominates, with a significant incidence in severe preeclampsia.
As noted in the results chapter, obesity is a dominant factor,
present in >50% of cases with mild preeclampsia.
Obesity is considered to be a mild risk factor for
preeclampsia (8), the relationship
between these two pathologies has long been studied in the context
in which in the last quarter of century has experienced a constant
upward trend of both preeclampsia and obesity (9). In a previous study (10), the association of obesity and
gestational hypertension with preeclampsia was investigated, and it
was reported that the risk of developing a hypertensive disease in
pregnancy increases proportionally to the increase of BMI.
We can conclude regarding the risk for a certain
category of hypertensive disease of obese patients that obesity, as
a risk factor, significantly impacts all categories of hypertension
in pregnancy, from gestational hypertension to severe preeclampsia,
but has an impact more significant as a risk factor for mild
preeclampsia (r=7.16).
The mechanism by which obesity is an important risk
factor for mild preeclampsia is dictated by the multiple common
features of both obesity and preeclampsia, namely: hyperinsulinism,
increased insulin resistance, increased leptin, TNF-α, IL-6 and
quantitative C-reactive protein with altered lipid profile and
decreased flow-mediated vasodilation (11). Both hyperinsulinism and increased
insulin resistance are conditions that precede pre-eclampsia
(12), all of which are among the
most important associations of obesity. Regarding the role of
adiponectins, leptin and proinflammatory cytokines in the
pathophysiological mechanism of preeclampsia, adipose tissue has
been shown to produce low levels of adiponectin with increased
levels of proinflammatory cytokines, such as TNF-α, and IL-6
leading to a proinflammatory status characterized by endothelial
dysfunction and increased insulin resistance (13). In obese patients, there is an
increased production of leptin, with a inflammatory effect and a
low production of adiponectins with an anti-inflammatory effect
resulting in a low degree systemic inflammation and increased
insulin resistance, status that also characterizes preeclampsia,
cardiovascular disease and type II diabetes (14). The importance of leptin in the
development of preeclampsia is due to the fact that its high levels
found in obesity, reduce the proliferation of the cytotrophoblast,
a basic pathophysiological mechanism of preeclampsia, and increase
the blood pressure and the level of placental factors (15).
Endothelial dysfunction is undoubtedly present in
obese persons, being caused by the unbalanced production of
metabolites of adipose tissue. The context characterized by an
increased BMI, respectively, with increased leptin levels and other
pro-inflammatory adiponectins, affects nicotinamide adenine
dinucleotide phosphate (NADPH) oxidase, which influences
endothelium-dependent vasodilation by increasing nitric oxide
degradation (16). Nitric oxide
deficiency affects the integrity and functioning of the
endothelium, which in a pregnancy context, where the role of the
endothelium is fundamental in the remodeling of uterine arteries
and in hemodynamic adaptations, becoming a determining factor in
the development of preeclampsia.
Nitric oxide (NO) results from the synthesis of the
amino acid L-arginine in the presence of NO synthase, which is a
family of enzymes dependent on NADPH and calcium. NO-endothelial
synthase is expressed at the level of human placental
syncytiotrophoblast and at the level of extravillous trophoblast,
indicating that placental nitric oxide production plays an
important role in the vascular adaptation required to ensure proper
flow and avoid generalized peripheral vasoconstriction status
(17), which undoubtedly
characterizes preeclampsia.
Through the above mentioned arguments, an
association link is clear between the existence of obesity,
preeclampsia and the pathophysiological mechanisms involved. This
remains a current problem, in the context in which the rate of
obesity and preeclampsia in pregnancy has tripled in the recent
decades and is constantly increasing and giving the fact that these
pathologies associate a significant rate of maternal and fetal
morbidity and mortality. The results obtained show that obesity is
an important risk factor for mild preeclampsia, but not for severe
preeclampsia.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DN, FG and NT contributed substantially to the
statistical analysis of the data. FPP, ID and MMC collected,
analyzed and interpreted the patient data regarding the impact of
obesity on the evolution of a hypertensive pathology that
complicates pregnancy. REB, CAZ and NT contributed substantially to
the conception of the study and the data interpretation, and were
major contributors in the writing of the manuscript. All authors
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
No authors listed. Report of the National
High Blood Pressure Education Program Working Group on high blood
pressure in pregnancy. Am J Obstet Gynecol.
183(S1-S22)2000.PubMed/NCBI
|
|
2
|
Sibai BM and Stella CL: Diagnosis and
management of atypical preeclampsia-eclampsia. Am J Obstet Gynecol.
200(481.e1-481.e7)2009.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Thornton CE, Makris A, Ogle RF, Tooher JM
and Hennessy A: Role of proteinuria in defining pre-eclampsia:
Clinical outcomes for women and babies. Clin Exp Pharmacol Physiol.
37:466–470. 2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Homer CS, Brown MA, Mangos G and Davis GK:
Non-proteinuric pre-eclampsia: A novel risk indicator in women with
gestational hypertension. J Hypertens. 26:295–302. 2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Barton JR and Sibai BM: Diagnosis and
management of hemolysis, elevated liver enzymes, and low platelets
syndrome. Clin Perinatol. 31807–833. (vii)2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Osmanağaoğlu MA, Erdoğan I, Zengin U and
Bozkaya H: Comparison between HELLP syndrome, chronic hypertension,
and superimposed preeclampsia on chronic hypertension without HELLP
syndrome. J Perinat Med. 32:481–485. 2004.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Murray D, O'Riordan M, Geary M, Phillips
R, Clarke T and McKenna P: The HELLP syndrome: Maternal and
perinatal outcome. Ir Med J. 94:16–18. 2001.PubMed/NCBI
|
|
8
|
Brown CE, Cunningham FG and Pritchard JA:
Convulsions in hypertensive, proteinuric primiparas more than 24
hours after delivery. Eclampsia or some other cause? J Reprod Med.
32:499–503. 1987.PubMed/NCBI
|
|
9
|
Zeeman GG: Neurologic complications of
pre-eclampsia. Semin Perinatol. 33:166–172. 2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Belfort MA, Saade GR, Grunewald C, Dildy
GA, Abedejos P, Herd JA and Nisell H: Association of cerebral
perfusion pressure with headache in women with pre-eclampsia. Br J
Obstet Gynaecol. 106:814–821. 1999.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ghulmiyyah L and Sibai B: Maternal
mortality from pre-eclampsia/eclampsia. Semin Perinatol. 36:56–59.
2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
LeFevre ML: U.S. Preventive Services Task
Force. Low-dose aspirin use for the prevention of morbidity and
mortality from preeclampsia: U.S. Preventive Services Task Force
recommendation statement. Ann Intern Med. 161:819–826.
2014.PubMed/NCBI View
Article : Google Scholar
|
|
13
|
Wang Y, Beydoun MA, Liang L, Caballero B
and Kumanyika SK: Will all Americans become overweight or obese?
Estimating the progression and cost of the US obesity epidemic.
Obesity (Silver Spring). 16:2323–2330. 2008.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yogev Y and Catalano PM: Pregnancy and
obesity. Obstet Gynecol Clin North Am. 36285–300.
(viii)2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sierra-Laguado J, García RG, Celedón J,
Arenas-Mantilla M, Pradilla LP, Camacho PA and López-Jaramillo P:
Determination of insulin resistance using the homeostatic model
assessment (HOMA) and its relation with the risk of developing
pregnancy-induced hypertension. Am J Hypertens. 20:437–442.
2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lopez-Jaramillo P: The role of adiponectin
in cardiometabolic diseases: Effects of nutritional interventions.
J Nutr. 146(422S-426S)2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Spradley FT, Palei AC and Granger JP:
Increased risk for the development of preeclampsia in obese
pregnancies: Weighing in on the mechanisms. Am J Physiol Regul
Integr Comp Physiol. 309(R1326-R1343)2015.PubMed/NCBI View Article : Google Scholar
|