Introduction
An autoimmune disease (AID) is marked by tissue
damage, inflicted by the self-reactivity of the various mechanisms
of the immune system, antibodies and T cells. Its on-set could be
associated with genetic and/or environmental triggers. Although,
individually, each AID is present in a small number of individuals,
overall, its prevalence is estimated to be between 7.6 and 9.4%
(1). All autoimmune diseases, to
some extent, have repercussions for obstetrics and not only. For
example, in the general population, ~80% of the abortions happen
during the first 12 weeks of pregnancy, and the risk of spontaneous
abortion in women aged <35 years is ~10%, while in those aged
>40 years is exceeding 45% (2,3).
Clinical immunology studies have shown that autoimmune thyroiditis
is associated with high rates of infertility and early miscarriages
due to associated hormonal changes and instability. The presence of
anti-thyroid antibodies may react against the structures of the
placenta or fertilized egg and may cause embryo implantation
problems (4).
The need for systematic thyroid function and TAb
evaluation in early pregnancy may seem fairly obvious, but this is
far from being a unanimous opinion (5,6). It is 8
years since we called for thyroid function screening in pregnancy
and 5 years since the American Association of Clinical
Endocrinologists (AACE) recommended thyroid function screening in
all women during the first trimester of pregnancy. The most recent
joint guideline published by the Endocrine Society recommends an
aggressive case-finding approach during early pregnancy in
high-risk populations rather than routine screening.
In the present analysis, data were pooled from the
clinical database that spans over 57 months of the Department of
Obstetrics Gynecology of the University Emergency Hospital
Bucharest, in order to evaluate the connection between AIDs
(autoimmune thyroiditis and inherited thrombophilia) in a
sufficiently large sample of pregnant women.
Patients and methods
In the present retrospective analysis, it was aimed
to determine the prognosis, regarding fetal and maternal morbidity,
when autoimmune thyroid pathologies associate with inherited
thrombophilia, simultaneously throughout the pregnancy. The
patients that met our criteria were divided into three groups -
pregnancies associating only autoimmune thyroid pathology (mainly
autoimmune thyroiditis), pregnancies affected only by inherited
thrombophilia, and cases marked by the two diseases simultaneously.
The inclucion criteria for the first two groups were based on the
presence of a gene mutation such as Factor V Leiden (FVL)
mutation (C677T), hyperhomocysteinaemia mutation (A506G),
prothrombin mutation (G20210A) or prothrombin II (PTII) mutation,
or protein S and/or C deficiency detected according to the
guidelines of the American College of Obstetricians and
Gynecologists Practice Bulletin No. 124 (7,8) for the
first group, and the presence of thyroid antibodies (ATAs)
[anti-thyroglobulin (anti-TG) and anti-thyroid peroxidase
(anti-TPO)], on two or more occasions, at least 6 weeks apart, for
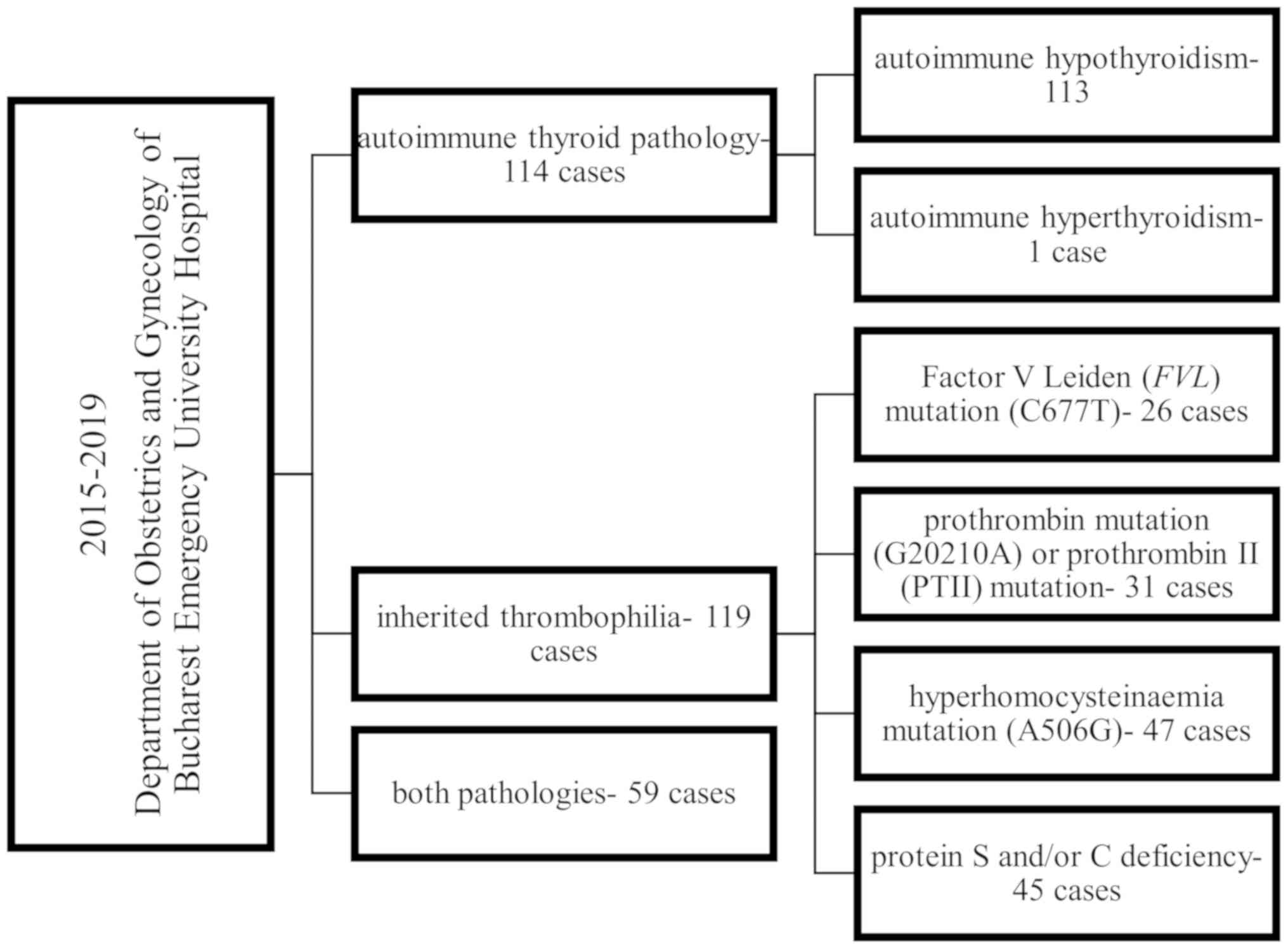
the second group. Thus, the studied population consisted of 82
pregnancies marked only by autoimmune thyroid pathology, 65
pregnancies affected by inherited thrombophilia, and a total of 27
pregnancies that associated both diseases (Fig. 1). The patients were followed at the
outpatient clinic of the Department of Obstetrics Gynecology,
University Emergency Hospital Bucharest. Informed consent was
obtained from all patients. Patients' medical charts were
retrospectively evaluated for clinical and laboratory data.
Clinical data collection was based on a standardized interview
completed by all patients presenting with features of autoimmune
diseases.
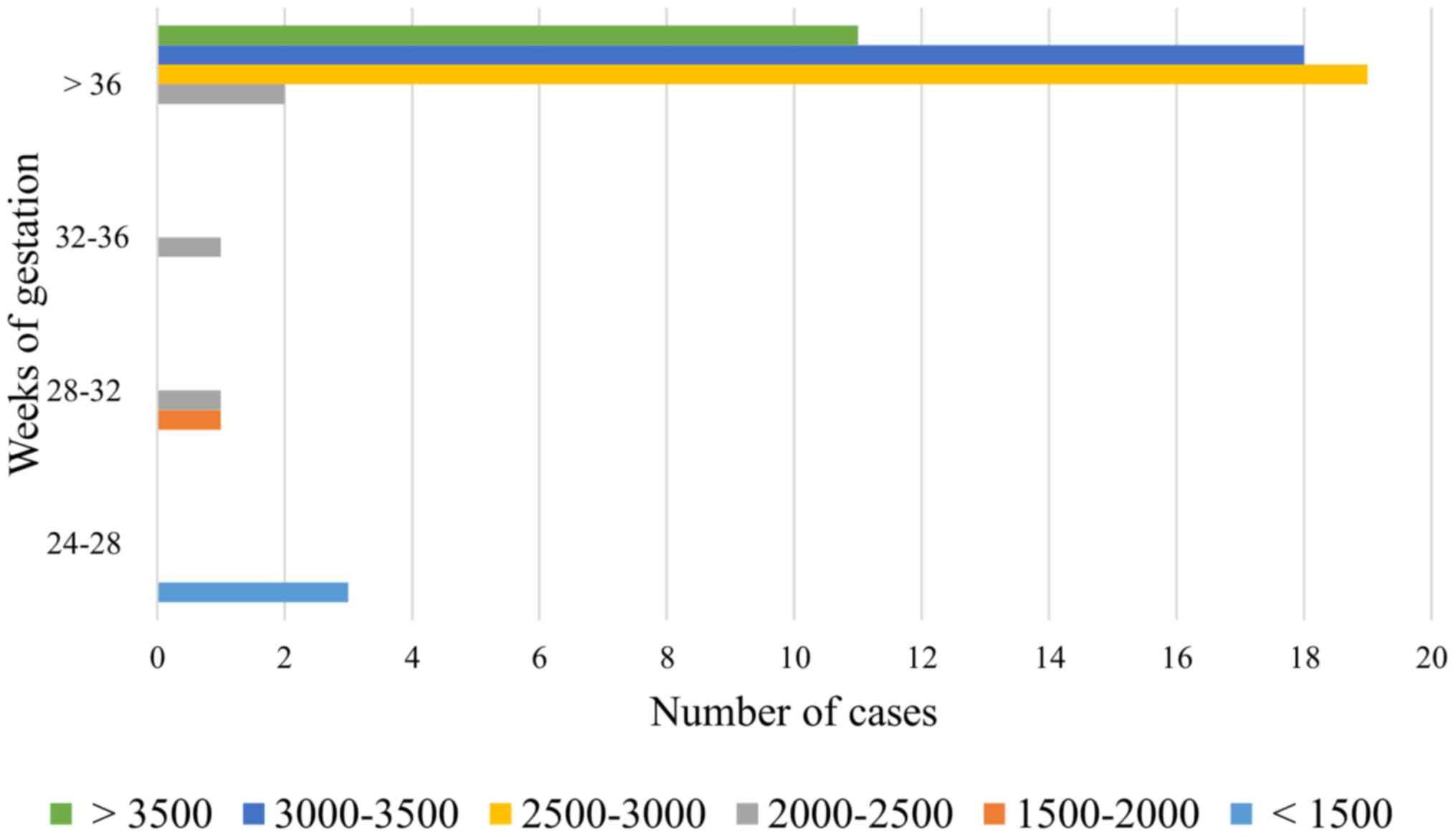
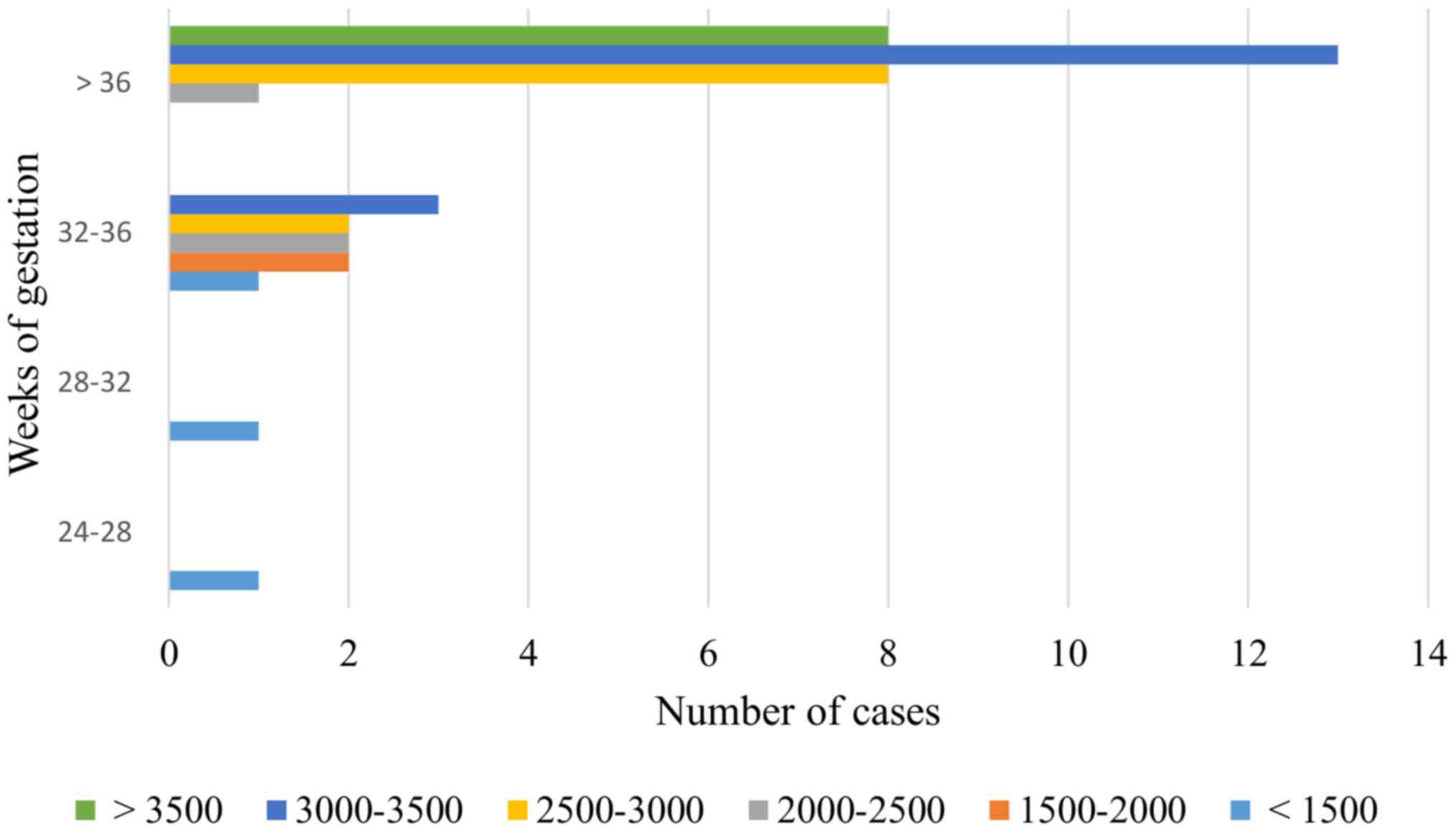
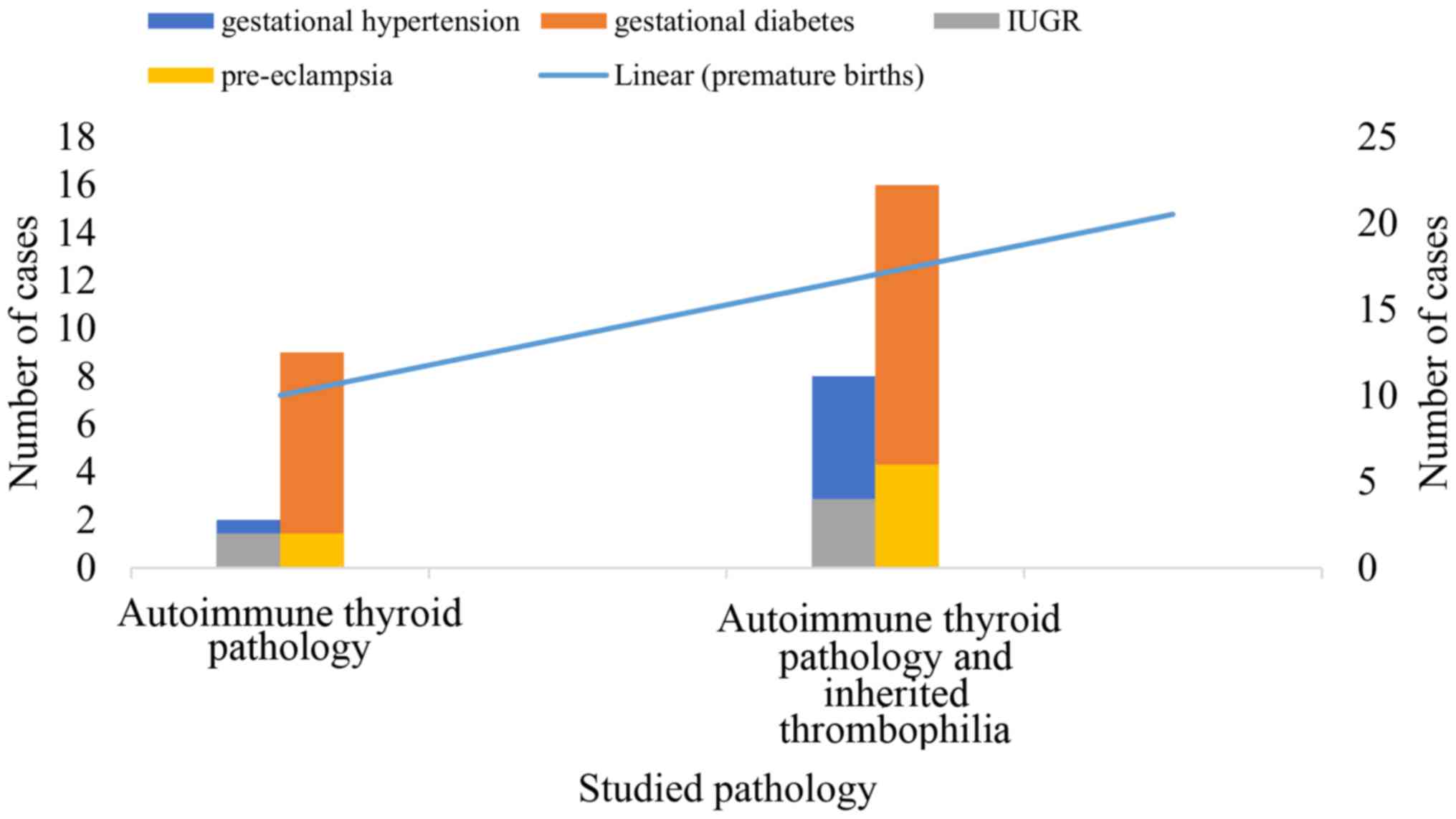
In the first stage of statistical evaluation,
descriptive tests were applied while monitoring the presence of
risk factors and complications in the studied groups. The main
parameters analyzed were the fetal weight at birth and Apgar score
(to assess the impact on the fetal outcome) - Figs. 2 and 3, as well as the risk of developing
pre-eclampsia, intrauterine growth restriction, diabetes, abruption
placentae and premature birth. The frequency for each studied group
and their comparative reproduction is shown in Fig. 4.
Results
In the analysis conducted above, of the cases
admitted to the Department of Obstetrics Gynecology of the
University Emergency Hospital Bucharest from January 2015 up to
September 2019, we identified 171 pregnancies marked by
hypothyroidism and 8 cases with hyperthyroidism.
Twenty-seven cases of autoimmune thyroiditis also
associated hereditary thrombophilia, compared with one case of
hyperthyroidism (Fig. 1). This is
also reflective of the fact that Romania belongs to an
iodine-replete area.
Regarding the comparative analysis of the three
studied groups and the implications of the studied pathologies in
pregnancy a significant and direct statistical significant relation
between thrombophilia and mild preeclampsia were obtained, P=0.007
(<0.05), Cramer V = 0.19; OR, 10.23; 95% CI, 1.22-85.79.
There is a significant statistical correlation
between the presence of thrombophilia and autoimmune thyroiditis,
P=0.004, Cramer V = 0.20; OR, 4.57; 95% CI, 1.46-14.27.Continuing
this context, based on our statistical analysis if a patient is
associated with thrombophilia and autoimmune thyroiditis the risk
for the presence of another autoimmune disease is increased
3.86-fold, P=0.008, Cramer V = 0.19; OR, 3.86; 95% CI,
1.36-10.94.
We obtained significant results by comparative
analysis of group 1 with group 3, respectively, patients with only
autoimmune thyroid pathology (mainly autoimmune thyroiditis) and
patients with inherited thrombophilia and autoimmune thyroid
pathology for the incidence of premature birth, which appears with
a significantly increased incidence in patients associating both
pathologies. Gestational diabetes also appears with a significantly
increased incidence in group 3.
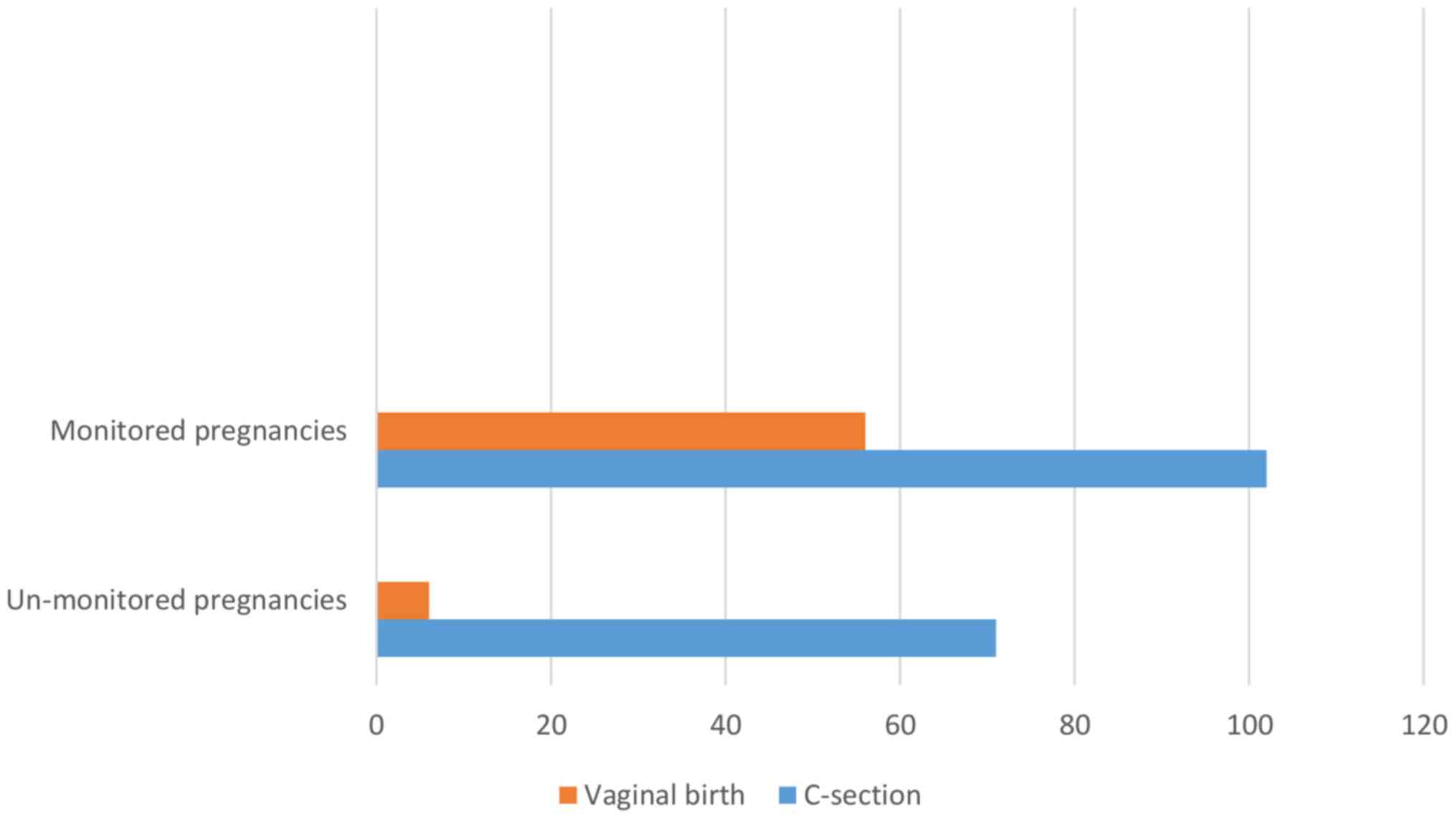
Consequently, we also observed that out of the 27
pregnancies associating thyroid pathology and inherited
thrombophilia, in 24 cases the pregnancy was not monitored by any
kind of health care provider (Fig.
5). This is a major factor in a developing country, and a
continuous source of monetary loss for our health care system.
Discussion
Regarding the statistics of the two pathologies
affecting the pregnant woman, the data collected in Romania is
scarce. The prevalence and incidence of thyroid dysfunction are
difficult to compare across countries due to differences in
diagnostic thresholds, assay sensitivities, population selection
and fluxes in iodine nutrition and population dynamics.
A meta-analysis of European studies estimated a mean
prevalence rate for autoimmune thyroiditis of 0.75% for males and
females combined and an incidence rate of 51 cases per 100,000 per
year (9). However, a database for
this pathology associated with pregnancy is not yet available.
Thyrotoxicosis in pregnancy has an estimated incidence of 0.2% for
overt thyrotoxicosis and 2.5% for subclinical thyrotoxicosis
(10-12).
Iodine deficiency and autoimmune disease (Hashimoto
thyroiditis) are responsible for the majority of cases of primary
hypothyroidism (13). A third of the
world's population lives in iodine-deficient areas, and the
devastating consequences of severe iodine deficiency on the
neurological development of fetuses and children are well
recognized. In addition, the possible effects of less severe grades
of iodine deficiency during pregnancy on offspring cognitive
development are also becoming recognized (14). In Europe, 44% of school-age children
still have insufficient iodine intake. The prevalence of overt
hypothyroidism in the general population ranges from between 0.2
and 5.3% in Europe (15,16).
A point of discussion worth pursuing is the link
between autoimmune thyroid pathology and pregnancy loss. Autoimmune
factors seem to play a pivotal role in infertility. The prevalence
of antiphospholipid antibodies (aPL), ANA, and antithyroid
antibodies was found to be particularly higher in women with
unknown infertility. Implantation is a process based on immunologic
tolerance and requires cross-talk between the embryo and the
maternal immune system. Impaired implantation and high pregnancy
loss rates in women with autoimmune antibodies could be caused by
injury to the syncytiotrophoblasts, endothelial cells of the spiral
veins, superficial/glandular epithelial cells of the decidua or
autoantibody inflammatory processes. These biological events result
in impaired implantation and disturbed fetal perfusion (17). During the analysis presented above,
we also observed 25 cases of autoimmune hypothyroidism associated
with spontaneous abortions at gestational ages ranging between 8
and 22 weeks, out of which 4 cases also suffered from inherited
thrombophilia. Although exact screening and management protocols
for infertile patients positive for autoimmune antibodies have not
been established, it seems reasonable to devise a patient-centered,
individualized approach for these patients.
The present analysis had several limitations. Due to
financial and geographic limitations, a few of the pregnant women
did not report to the outpatient clinic regularly, in order to be
tested. After giving birth, some of the patients did not return to
the 6-week check-up, in order to evaluate their state of health
outside the stress of the pregnancy. We did not pursue the
implications of the AIDs during pregnancy on the foetus (weight,
neurological and morphological features). Furthermore, the small
number of patients, the retrospective design of the study, and that
it reflects the experience of a single center. However, this study
was designed to stress the importance of knowing the immunological
background of the pregnant woman.
This analysis pointed to the need to consider also
testing for other AIDs such as antiphospholipid syndrome. Although
the presence of antiphospholipid antibodies in patients with
autoimmune thyroiditis has been previously reported (18), only a small study highlights the
prevalence of antibodies against thyroid antigens in patients with
antiphospholipid syndrome (APS). Moreover, the increasingly
recognized association of thyroid autoimmunity with central nervous
system (CNS) disease and pregnancy morbidity features, which can
both be found in the APS (19),
prompts us to further investigate the connection between thyroid
autoimmunity, APS and pregnancy. In addition, continued vigilance
against iodine deficiency remains essential in developed countries,
particularly in Europe. Universal thyroid screening associated with
thrombophilia screening in pregnancy is therefore contentious in
iodine-replete areas, although it has been shown to be
cost-effective in analytical economic models.
Besides the well-accounted impact of hereditary
thrombophilia during pregnancy, which is emphasized in our study by
the incidence of moderate preeclampsia, we also account for a
direct and statistically significant relationship between
thrombophilia and moderate intensity autoimmune diseases (including
autoimmune thyroiditis). Furthermore, if these two pathologies are
combined there is an increased risk of the presence of another
autoimmune disease.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
FPP, REB and NT collected, analyzed and interpreted
the patient data regarding the testing for ATAs, anti-TG, anti-TPO,
TSH, freeT3 and freeT4. FPP, REB and NT also
collected the data of immunological and genetic markers specific
for thrombophilia and antiphospholipid syndrome of the pregnant
women included in the present study. FG, DN and MMC substantially
contributed to the conception of the study, the interpretation of
the data and the writing of the manuscript. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
Informed consent was obtained from all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cooper GS, Bynum ML and Somers EC: Recent
insights in the epidemiology of autoimmune diseases: Improved
prevalence estimates and understanding of clustering of diseases. J
Autoimmun. 33:197–207. 2009.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hurt KJ, Guile MW, Bienstock JL, Fox HE
and Wallach EE (eds): The Johns Hopkins Manual of Gynecology and
Obstetrics (Lippincott Manual Series). 4th, North American edition.
Lippincott Williams and Wilkins, Philadelphia, PA. pp73–77.
2011.
|
|
3
|
Pearce EN, Andersson M and Zimmermann MB:
Global iodine nutrition: Where do we stand in 2013? Thyroid.
23:523–528. 2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Grassi G, Balsamo A, Ansaldi C, Balbo A,
Massobrio M and Benedetto C: Thyroid autoimmunity and infertility.
Gynecol Endocrinol. 15:389–396. 2001.PubMed/NCBI
|
|
5
|
Abalovich M, Amino N, Barbour LA, Cobin
RH, De Groot LJ, Glinoer D, Mandel SJ and Stagnaro-Green A:
Management of thyroid dysfunction during pregnancy and postpartum:
An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol
Metab. 92 (Suppl)(S1-S47)2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
American College of Obstetrics and
Gynecology. ACOG practice bulletin. Thyroid disease in pregnancy.
Number 37, August 2002. Int J Gynaecol Obstet. 79:171–180.
2002.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Negro R, Formoso G, Mangieri T, Pezzarossa
A, Dazzi D and Hassan H: Levothyroxine treatment in euthyroid
pregnant women with autoimmune thyroid disease: Effects on
obstetrical complications. J Clin Endocrinol Metab. 91:2587–2591.
2006.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lockwood C and Wendel G: Committee on
Practice Bulletins - Obstetrics: Practice bulletin no. 124:
Inherited thrombophilias in pregnancy. Obstet Gynecol. 118:730–740.
2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Stevens SM, Woller SC, Bauer KA, Kasthuri
R, Cushman M, Streiff M, Lim W and Douketis JD: Guidance for the
evaluation and treatment of hereditary and acquired thrombophilia.
J Thromb Thrombolysis. 41:154–164. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Innocencio RM, Romaldini JH and Ward LS:
High prevalence of thyroid autoantibodies in systemic sclerosis and
rheumatoid arthritis but not in the antiphospholipid syndrome. Clin
Rheumatol. 22(494)2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Garmendia Madariaga A, Santos Palacios S,
Guillén-Grima F and Galofré JC: The incidence and prevalence of
thyroid dysfunction in Europe: A meta-analysis. J Clin Endocrinol
Metab. 99:923–931. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Turcan N, BohîlŢea R, Neacsu A, Baros A
and Cîrstoiu MM: The role of anticoagulant therapy in the
prevention of preeclampsia pharmacokinetic and pharmacodynamic
mechanisms. Rev Chim. 70:1424–1428. 2019. View Article : Google Scholar
|
|
13
|
Asvold BO, Vatten LJ and Bjøro T: Changes
in the prevalence of hypothyroidism: The HUNT Study in Norway. Eur
J Endocrinol. 169:613–620. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
BohîlŢea RE, Zugravu CA, Neacsu A, Navolan
D, Berceanu C, Nemescu D, Bodean O, Turcan N, Baros A and Cîrstoiu
MM: The prevalence of vitamin D defficiency and its obstetrical
effects. A prospective study on Romanian patients. Rev Chim.
70:1228–1233. 2019.
|
|
15
|
Okosieme OE and Lazarus JH: Important
considerations in the management of Graves' disease in pregnant
women. Expert Rev Clin Immunol. 11:947–957. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Taylor PN and Vaidya B: Side effects of
anti-thyroid drugs and their impact on the choice of treatment for
thyrotoxicosis in pregnancy. Eur Thyroid J. 1:176–185.
2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chaker L, Bianco AC, Jonklaas J and
Peeters RP: Hypothyroidism. Lancet. 390:1550–1562. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
BohîlŢea R, Turcan N, Ionescu C, Toader O,
Nastasia S, Neculcea D, Movileanu I, Munteanu O and Cîrstoiu M: The
incidence of prematurity and associated short-term complications in
a multidisciplinary emergency hospital from Romania. In:
Proceedings of the 5th Congress of the Romanian Society of
Ultrasound in Obstetrics and Gynecology, Filodiritto Editore.
pp105–112. 2017.
|
|
19
|
Nabriski D, Ellis M, Ness-Abramof R,
Shapiro M and Shenkman L: Autoimmune thyroid disease and
antiphospholipid antibodies. Am J Hematol. 64:73–75.
2000.PubMed/NCBI View Article : Google Scholar
|