Introduction
As a common cardiovascular disease, coronary artery
disease (CAD) is mainly caused by coronary artery lesions. In
recent years, with the change in social environment and living
habits, morbidity and mortality have been increasing (1,2).
Coronary atherosclerosis is the pathological basis of CAD.
Incomplete or complete occlusion of the coronary artery caused by
coronary atherosclerosis is also one of the key factors for the
occurrence of CAD (3). CAD,
particularly the formation of plaque, is likely to cause major
adverse cardiovascular events (MACEs) and the occurrence of MACEs
is one of the major causes of death in patients with CAD (4). Therefore, the ability to rapidly judge
a patient's condition and predict the occurrence of MACEs is
particularly important.
Myeloperoxidase (MPO) is an important inflammatory
mediator in the progression of atherosclerotic plaque from stable
to unstable stages (5). Homocysteine
(Hcy) is an important intermediate metabolite of the protein
metabolism pathway and it is formed by modification by enzymes
after methionine enters the human body. Numerous studies have
indicated that Hcy may be an independent risk factor for
cardiovascular disease and there is a close association between the
condition and thrombosis (6,7). High-sensitivity C-reactive protein
(hs-CRP) is involved in the inflammatory reaction. As a highly
sensitive inflammatory marker, once the body is in an inflammatory
state, levels of hs-CRP rapidly increase within a short period of
time (8). It has been indicated that
hs-CRP also has an important role in CAD and it may be used as a
prognostic marker of cardiovascular disease (9). At present, MPO, Hcy and hs-CRP are used
as convenient inflammatory markers in the clinic that may be
rapidly detected (10,11). However, few studies have explored the
association between these factors and the severity of CAD (12).
Therefore, in the present study, the association
between the presence or severity of CAD and the expression of MPO,
Hcy or hs-CRP was assessed in order to provide further reference
data for judging the condition of patients with CAD and selecting
treatment options.
Materials and methods
Patients
A total of 112 patients (58 males and 54 females)
with CAD admitted to Xingtai People's Hospital from March 2014 to
July 2016 were included in the patient group (PG). All patients
were aged between 57-73 years, with an average age of 66.12±7.47
years. In addition, 112 healthy individuals who came to Xingtai
People's Hospital from March 2014 to July 2016 for physical
examinations were included in the control group (CG). The inclusion
criterion was as follows: Patients with CAD that had been confirmed
by coronary angiography. The exclusion criteria were as follows:
Patients with severe infections or immune diseases, other malignant
tumors, severe liver and kidney dysfunction, types of severe heart
disease other than CAD and cognitive or communication impairment,
as well as those who did not wish to participate in the present
study. All patients and their families agreed to participate in the
study and signed the informed consent form after understanding the
procedure and risks. This study was approved by the Ethics
Committee of Xingtai People's Hospital (Xingtai, China).
Laboratory indexes
The patient's fasting venous blood (5 ml) was
sampled in the morning after admission. The blood sample was
centrifuged at a speed of 1500 x g for 10 min. After
centrifugation, serum and plasma were separated. The level of MPO
in the plasma was detected by a colorimetric immunoassay (Raleigh
Bioengineering Co., Ltd.). The serum level of Hcy was detected by
an enzymatic cycling assay (cat. no. 59400370417; Zhonghan Shengtai
Biotechnology Co., Ltd.) on a fully automatic biochemical analyzer
(BS-380, Shenzhen Mindray Bio-Medical Electronics Co., Ltd.) and
the expression of hs-CRP was detected by immunoturbidimetry on a
fully automatic biochemical analyzer (Y70105-1, Zhejiang Erkn
Biological Technology Co., Ltd.). The operative procedures were
performed strictly in accordance with the manufacturer's
protocols.
Outcome measures
i) The plasma levels of MPO, Hcy and hs-CRP were
compared between the two groups. ii) According to the arteriography
results, the patients were divided into the single-vessel disease
group (SVG), double-vessel disease group (DVG) or multi-vessel
disease group (MVG). The Gensini scores of the three groups were
evaluated according to the Gensini score standard (13). iii) The correlations between the
Gensini score and the levels of MPO, Hcy and hs-CRP were analyzed.
iv) Patients were followed up by telephone consultations for 6
months and MACEs were recorded and compared. MACEs included
myocardial infarction, heart failure and cardiogenic death. v) The
predictive values of MPO, Hcy and hs-CRP for MACEs were determined
and compared.
Statistical analysis
SPSS 19.0 software (IBM Corp.) was used in the
present study for statistical analysis. GraphPad Prism 6 software
(GraphPad, Inc.) was used to visualize the data in the present
study. The χ2 test was used to assess differences in
count data. Values are expressed as the mean ± standard deviation
or n (%). The independent-samples t-test was used to compare the
data between two groups, and ANOVAs were used to compare data among
multiple groups. Tukey's tests were used for post hoc tests.
Receiver operating characteristic (ROC) curve analysis was used to
assess the predictive performance of MPO, Hys and hs-CRP for MACEs.
Pearson's linear correlation analysis was used to determine
correlations between the parameters and the Gensini score. The Cox
regression model was used to analyze the risk factors of MACE.
P<0.05 was considered to indicate statistical significance.
Results
Comparison of general data
There were no differences in sex, age and BMI
between the two groups (P>0.05) and the general data were
comparable (Table I).
 | Table IClinicopathological characteristics of
the patients and comparison of demographic data between the patient
and control groups. |
Table I
Clinicopathological characteristics of
the patients and comparison of demographic data between the patient
and control groups.
| Item | Patient group
(n=112) | Control group
(n=112) | t/χ2 | P-value |
|---|
| Sex | | | 0.018 | 0.894 |
|
Male | 58 (51.79) | 59 (52.68) | | |
|
Female | 54 (48.21) | 53 (47.32) | | |
| Age (years) | | | 0.018 | 0.893 |
|
≥66 | 61 (54.46) | 60 (53.57) | | |
|
<66 | 51 (45.53) | 52 (46.43) | | |
| BMI
(kg/m2) | | | 0.018 | 0.894 |
|
≥23 | 57 (50.89) | 58 (51.79) | | |
|
<23 | 55 (49.11) | 54 (48.21) | | |
| Number of
lesions | | | - | - |
|
Single | 41 (36.61) | - | | |
|
Double | 39 (34.82) | - | | |
|
Multiple | 32 (28.57) | - | | |
| Coagulation
function |
|
APTT
(sec) | 28.65±2.72 | 29.03±2.65 | 1.059 | 0.251 |
|
PT
(sec) | 12.24±1.11 | 12.18±0.94 | 0.437 | 0.663 |
|
FIB
(g/l) | 3.03±0.14 | 3.05±0.15 | 1.032 | 0.303 |
|
TT
(sec) | 14.65±1.44 | 14.53±1.38 | 0.637 | 0.525 |
| History of
surgery | | | 0.019 | 0.889 |
|
Yes | 41 (36.61) | 40 (35.71) | | |
|
No | 71 (63.39) | 72 (64.29) | | |
| Renal function
indices (µmol/l) |
|
Creatinine | 63.22±4.17 | 63.86±4.19 | 1.146 | 0.253 |
|
Urea | 5.47±0.66 | 5.53±0.79 | 0.617 | 0.538 |
|
Uric
acid | 331.87±13.64 | 330.98±14.05 | 0.481 | 0.631 |
Plasma levels of MPO, Hcy and hs-CRP
in the two groups
The plasma levels of MPO, Hcy and hs-CRP in the PG
were 2,671.46±426.85 pmol/l, 18.91±6.75 µmol/l and 4.33±1.59 mg/l,
respectively. The plasma levels of MPO, Hcy and hs-CRP in the CG
were 351.67±32.89 pmol/l, 11.32±4.12 µmol/l and 1.12±0.45 mg/l,
respectively. Of note, the levels of MPO, Hcy and hs-CRP in the PG
were higher than those in the CG (P<0.001; Table II).
 | Table IIExpression of plasma MPO and serum
Hcy and hs-CRP levels in the two groups. |
Table II
Expression of plasma MPO and serum
Hcy and hs-CRP levels in the two groups.
| Parameter | Patient group
(n=112) | Control group
(n=112) | t | P-value |
|---|
| MPO (pmol/l) |
2,671.46±426.85 | 351.67±32.89 | 57.35 | <0.001 |
| Hcy (µmol/l) | 18.91±6.75 | 11.32 ±4.12 | 10.16 | <0.001 |
| hs-CRP (mg/l) | 4.33±1.59 | 1.12 ±0.45 | 20.56 | <0.001 |
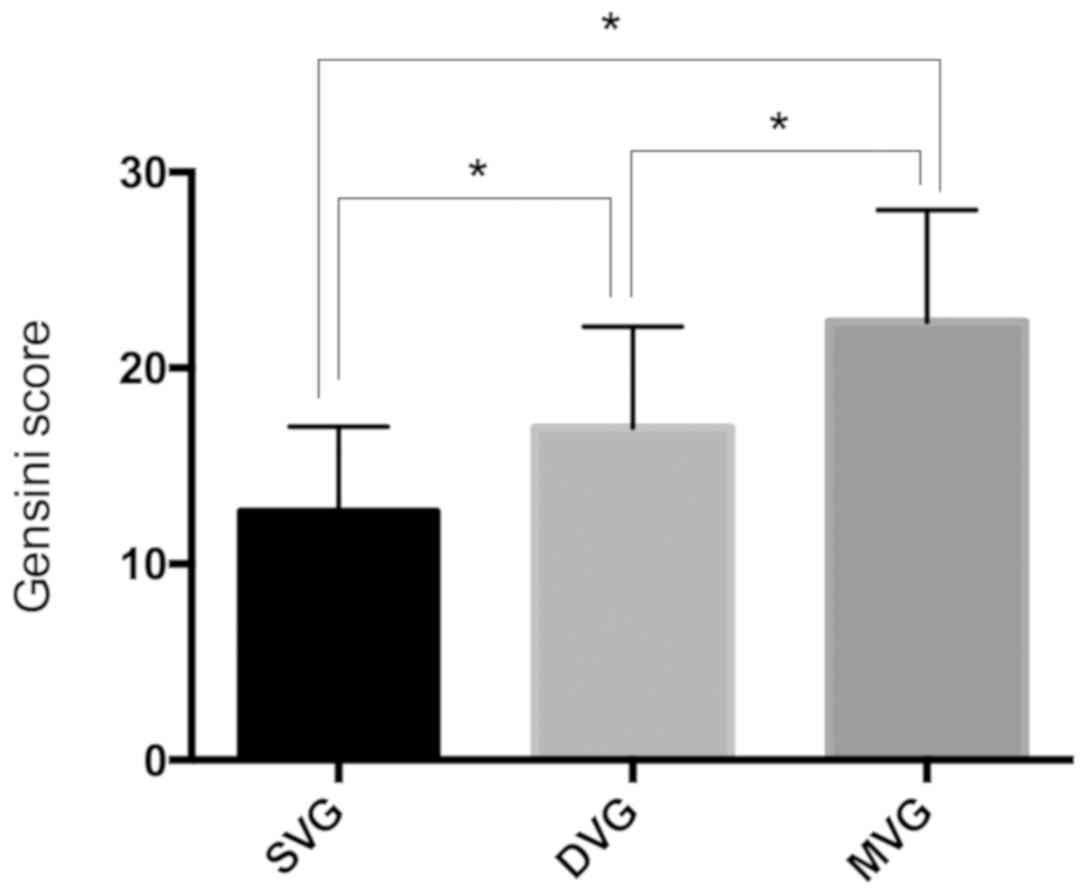
Gensini score in the PG
According to their arteriography results, the
patients were stratified into the SVG, DVG and MVG groups. The
Gensini score of each group was then compared. The Gensini scores
of the SVG, DVG and MVG were 12.68±4.33, 16.95±5.15 and 22.35±5.71,
respectively. The Gensini score of the MVG was higher than that of
the SVG and the DVG, and the Gensini score of the DVG was higher
than that of the SVG (P<0.05). This indicated that the severity
of coronary artery lesions in patients with multi-vessel disease
was higher than that in patients with double-vessel and
single-vessel disease, and the severity of coronary artery lesions
in patients with double-vessel disease was higher than that in
patients with single-vessel disease (Fig. 1).
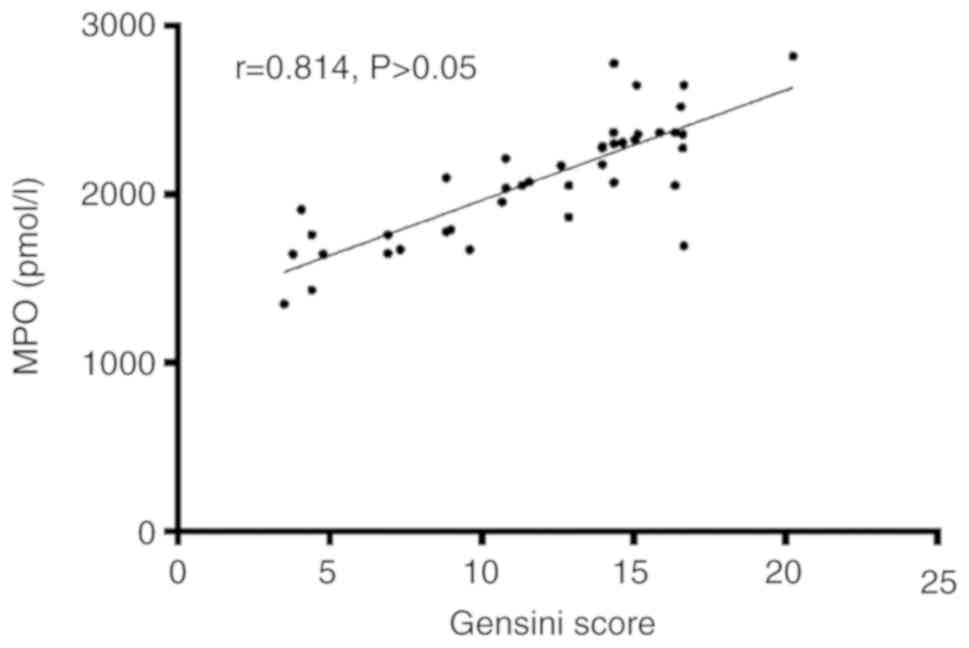
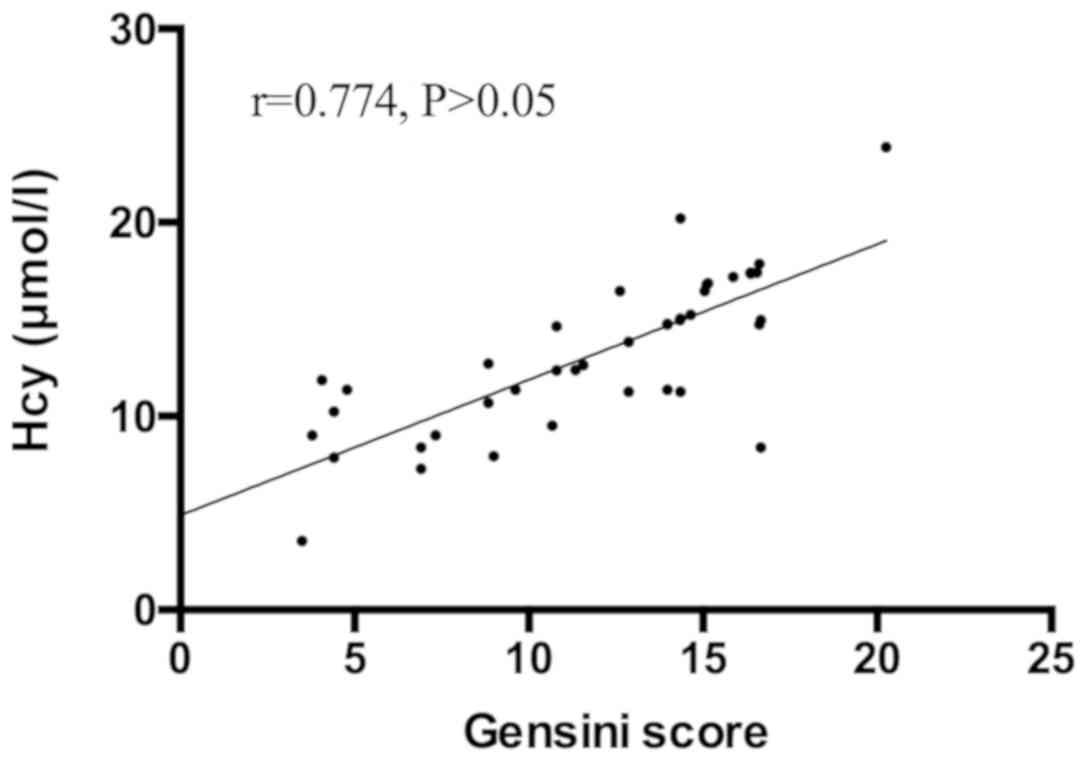
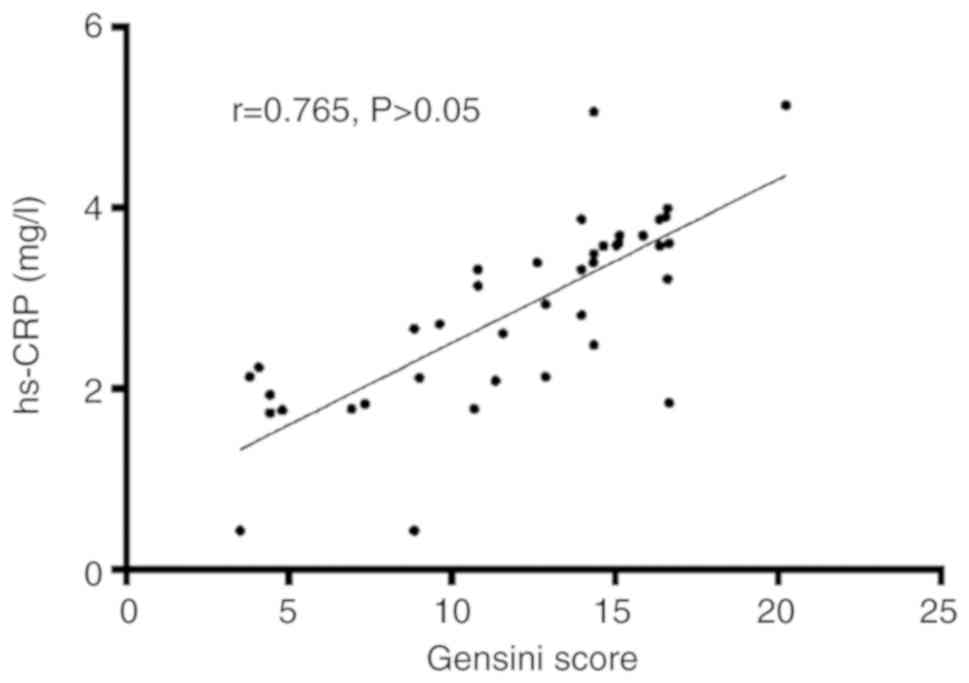
Correlation between Gensini score and
MPO, Hcy or hs-CRP
The levels of MPO, Hcy and hs-CRP were
2,149.83±359.61 pmol/l, 13.57±4.26 µmol/l and 3.11±1.02 mg/l,
respectively, in the SVG, 2,651.33±419.65 pmol/l, 18.69±6.51 µmol/l
and 4.39±1.41 mg/l, respectively, in the DVG and 3,169.42±466.73
pmol/l, 23.88±7.24 µmol/l and 5.46±1.63 mg/l, respectively, in the
MVG. The levels of MPO, Hcy and hs-CRP in the MVG were higher than
those in the DVG and the SVG, and those in the DVG were higher than
those in the SVG (P<0.05; Table
III). There was a positive correlation between the Gensini
score and the levels of MPO (r=0.814, P<0.05; Fig. 2), Hcy (r=0.774, P<0.05; Fig. 3) and hs-CRP (r=0.765, P<0.05;
Fig. 4). This showed that high
expressions of plasma MOP, serum Hys and hs-CRP indicated a severe
degree of disease progression in patients with CAD.
 | Table IIIPlasma levels of MPO, serum Hcy and
hs-CRP in patients with different numbers of vessels involved. |
Table III
Plasma levels of MPO, serum Hcy and
hs-CRP in patients with different numbers of vessels involved.
| Parameter | SVG (n=41) | DVG (n=39) | MVG (n=32) | F | P-value |
|---|
| MPO (pmol/l) |
2,149.83±359.61 |
2,651.33±419.65 |
3,169.42±466.73 | 54.91 | <0.001 |
| Hcy (µmol/l) | 13.57±4.26 | 18.69±6.51 | 23.88±7.24 | 26.41 | <0.001 |
| hs-CRP (mg/l) | 3.11±1.02 | 4.39±1.41 | 5.46±1.63 | 27.54 | <0.001 |
MACEs in the PG
A total of 37 MACEs were recorded for the 112
patients in the PG, including 7 cases of cardiac death and 30
re-hospitalized patients with heart failure or myocardial
infarction. Among them, there were 0 cases of cardiac death in the
SVG and 7 re-hospitalized patients with heart failure or myocardial
infarction, and the total incidence of MACEs was 17.07%. There were
2 cases of cardiac death in the DVG and 10 re-hospitalized patients
with heart failure or myocardial infarction, and the total
incidence of MACEs was 30.77%. There were 5 cases of cardiac death
in the MVG and 13 re-hospitalized patients with heart failure or
myocardial infarction, and the total incidence of MACEs was 56.25%.
The total incidence of MACEs in the MVG was higher than that in the
DVG and SVG (P<0.05). Furthermore, the total incidence of MACEs
in the DVG was higher than that in the SVG (P<0.05; Table IV).
 | Table IVMACEs in patients with different
numbers of vessels involved. |
Table IV
MACEs in patients with different
numbers of vessels involved.
| MACE | SVG (n=41) | DVG (n=39) | MVG (n=32) | χ2 | P-value |
|---|
| Cardiogenic
death | 0 (0.0) | 2 (5.13) | 5 (15.63) | 7.617 | 0.022 |
| Heart failure | 3 (7.320) | 4 (10.26) | 6 (18.75) | 2.396 | 0.302 |
| Myocardial
infarction | 4 (9.76) | 6 (15.38) | 7 (21.88) | 2.052 | 0.358 |
| Total
incidence | 7 (17.07) | 12 (30.77) | 18 (56.25) | 12.61 | <0.001 |
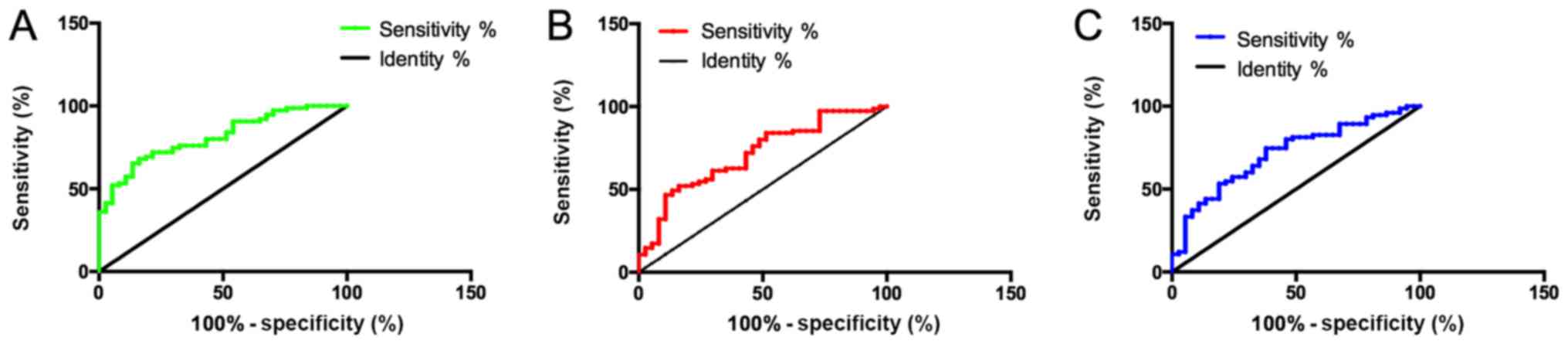
Predictive value of the levels of MPO,
Hcy and hs-CRP regarding MACEs
The 112 patients in the PG were divided into the
MACE and non-MACE groups based on whether any MACE occurred. The
area under the ROC curve (AUC) and prediction sensitivity of MPO
regarding MACEs were higher than those of Hcy and hs-CRP
(P<0.05). There was no significant difference in AUC and
prediction sensitivity between Hcy and hs-CRP (P<0.05). The
specificity of MACE prediction with hs-CRP was higher than that of
MPO and Hcy (P<0.05; Table V,
Fig. 5).
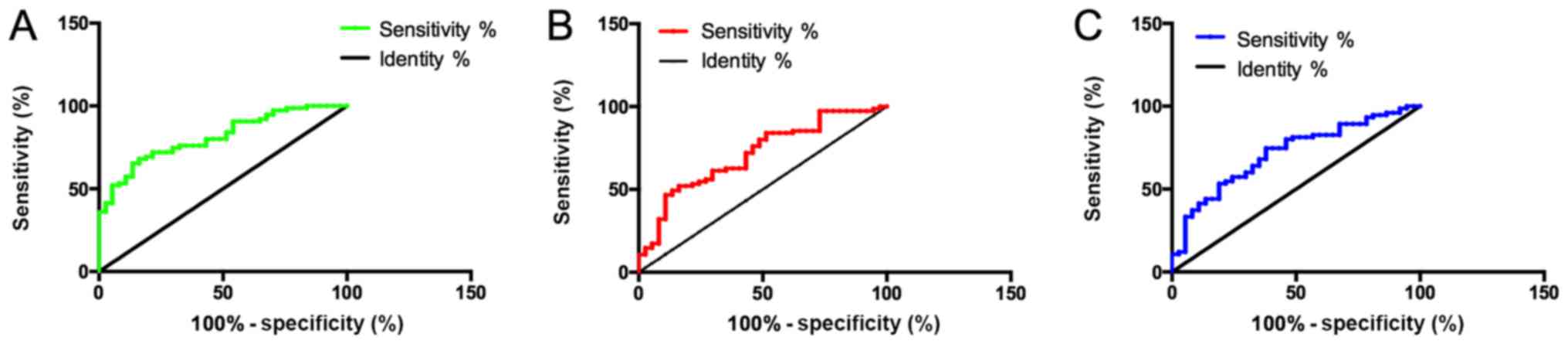 | Figure 5Receiver operating characteristic
curve analysis for determining the predictive value of plasma MPO,
Hcy and hs-CRP for MACE. (A) Predictive value of expression of MPO
for MACE. The sensitivity, specificity and AUC of plasma MPO for
predicting MACE were 78.67%, 56.76% and 0.812, respectively. The
cut-off value was 2906 pmol/l. (B) Predictive value of expression
of Hcy for MACE. The sensitivity, specificity and AUC of plasma MPO
for predicting MACE were 73.33%, 54.05% and 0.711, respectively.
The cut-off value was 20.30 µmol/l. (C) Predictive value of
expression of hs-CRP for MACE. The sensitivity, specificity and AUC
of plasma MPO for predicting MACE were 69.33%, 62.16% and 0.715,
respectively. The cut-off value was 4.795 mg/l. MPO,
myeloperoxidase; Hcy, homocysteine; hs-CRP, high-sensitivity
C-reactive protein; AUC, area under curve; MACE, major adverse
cardiovascular event. |
 | Table VPredictive value of plasma MPO, serum
Hcy and hs-CRP expression for major adverse cardiovascular
events. |
Table V
Predictive value of plasma MPO, serum
Hcy and hs-CRP expression for major adverse cardiovascular
events.
| Parameter | Sensitivity
(%) | Specificity
(%) | AUC | Cut-off value |
|---|
| MPO (pmol/l) | 78.67 | 56.76a | 0.812 | 2,906 |
| Hcy (µmol/l) | 73.33b | 54.05a | 0.711b | 20.30 |
| hs-CRP (mg/l) | 69.33b | 62.16 | 0.715b | 4.795 |
Univariate analysis of MACEs
Univariate analysis suggested that the number of
lesions, hypertension, diabetes, MPO, Hys and hs-CRP were
significantly associated with the occurrence of MACEs (P<0.05).
However, sex, age, BMI and smoking habits were not significantly
associated with MACE (P>0.05, Table
VI).
 | Table VIUnivariate analysis for the
association of various parameters with MACEs. |
Table VI
Univariate analysis for the
association of various parameters with MACEs.
| Item | MACE group
(n=37) | Non-MACE group
(n=75) | χ2 | P-value |
|---|
| Sex | | | 0.114 | 0.736 |
|
Male
(n=58) | 20 (54.05) | 38 (50.67) | | |
|
Female
(n=54) | 17 (45.95) | 37 (49.33) | | |
| Age (years) | | | 0.117 | 0.732 |
|
≥66
(n=61) | 21 (56.76) | 40 (53.33) | | |
|
<66
(n=51) | 16 (43.24) | 35 (46.67) | | |
| BMI
(kg/m2) | | | 0.005 | 0.946 |
|
≥23
(n=57) | 19 (51.35) | 38 (50.67) | | |
|
<23
(n=55) | 18 (48.65) | 37 (49.33) | | |
| Number of
lesions | | | 18.24 | <0.001 |
|
Single
(n=41) | 7 (18.92) | 34 (45.33) | | |
|
Double
(n=39) | 10 (27.03) | 29 (38.67) | | |
|
Multiple
(n=32) | 20 (54.05) | 12 (16.00) | | |
| Hypertension | | | 22.66 | <0.001 |
|
Yes | 31 (83.78) | 27 (36.00) | | |
|
No | 6 (16.22) | 48 (64.00) | | |
| Diabetes | | | 20.14 | <0.001 |
|
Yes | 29 (73.38) | 25 (33.33) | | |
|
No | 8 (21.62) | 50 (66.67) | | |
| Smoking | | | 0.040 | 0.841 |
|
Yes | 18 (48.65) | 38 (50.67) | | |
|
No | 19 (51.35) | 37 (49.33) | | |
| MPO (pmol/l) |
2,998.33l/l))74 |
2,465.91±462.55 | 6.133 | <0.001 |
| Hcy (µmol/l) | 20.51±5.43 | 16.59±6.21 | 3.217 | <0.001 |
| hs-CRP (mg/l) | 5.15±1.59 | 3.97±1.59 | 3.694 | <0.001 |
Multivariate analysis of MACEs
The number of lesions, hypertension, diabetes, MPO,
Hys and hs-CRP were taken as independent variables and they were
assigned with values (Table VII).
The occurrence of MACEs was treated as a dependent variable and
logistic regression analysis was adopted for multivariate analysis.
It was revealed that the number of lesions, hypertension, diabetes,
MPO, Hys and hs-CRP were independent risk factors for MACEs
(Table VIII).
 | Table VIIAssignments. |
Table VII
Assignments.
| Factor | Assignment |
|---|
| Number of
lesions | Single and double;
1; mutiple, 2 |
| Hypertension | Yes, 1; No, 2 |
| Diabetes | Yes, 1; No, 2 |
| MPO | Continuous variable
and analyzed using raw data |
| Hys | Continuous variable
and analyzed using raw data |
| hs-CRP | Continuous variable
and analyzed using raw data |
 | Table VIIIMultivariate analysis of the
association of various factors on major adverse cardiovascular
events. |
Table VIII
Multivariate analysis of the
association of various factors on major adverse cardiovascular
events.
| Factor | β | SE | Wald | HR | 95% CI | P-value |
|---|
| Number of
lesions | 0.346 | 0.155 | 5.448 | 1.452 | 1.019-1.885 | 0.003 |
| Hypertension | 1.154 | 0.519 | 4.784 | 3.206 | 1.121-9.163 | 0.001 |
| Diabetes | 1.004 | 0.321 | 9.409 | 2.743 | 1.441-5.222 | 0.021 |
| MPO | 0.564 | 0.118 | 9.482 | 2.679 | 1.734-4.319 | 0.017 |
| Hys | 0.502 | 0.088 | 8.624 | 2.427 | 1.506-3.773 | <0.001 |
| hs-CRP | 0.422 | 0.131 | 6.255 | 1.751 | 1.168-2.355 | 0.004 |
Discussion
With the incidence of CAD on the rise, the condition
is increasingly threatening human life and health (14). If patients are not treated in a
timely manner, they may experience MACEs including cardiogenic
death, and their survival and safety may be seriously affected
(15). Studies have indicated that
CAD is caused by a variety of factors and certain biochemical
indicators have been clinically proven to be closely linked to CAD
(16). For instance, MPO, as a
lysosomal enzyme in the cytoplasm of neutrophilic granulocytes, is
a potential mediator of vascular injury. The oxidative products of
MPO released by granulocytes during an inflammatory reaction are
closely associated with the occurrence of atherosclerosis (17,18). Hcy
and hs-CRP are also biochemical indicators that are considered to
be closely linked to CAD (19,20). In
the present study, the value of MPO, Hcy and hs-CRP to predict the
severity and of CAD and the prognosis of affected patients was
assessed with the aim of providing more accurate biochemical data
for the evaluation of CAD and selection of treatments.
The present results indicated that the plasma levels
of MPO, Hcy and hs-CRP in the PG were higher than those in CG. A
previous study indicated high expression of MPO in venous blood of
patients with acute coronary syndrome (21). Another study demonstrated that MPO
may serve as an inflammatory marker and that it damages vascular
endothelium by oxidizing cholesterol and low-density lipoprotein
while degrading the extracellular matrix and corroding patches
(22). Furthermore, another study
has indicated that hs-CRP and Hcy levels were significantly
increased in patients with CAD and that the expression of hs-CRP
and Hcy varied with the severity of CAD (23). The results of these studies were
consistent with those of the present study. Patients in the PG were
divided into three groups, SVG, DVG and MVG, according to the
arteriography results. The Gensini scores of the three groups were
evaluated and the correlations between the plasma levels of MPO,
Hcy or hs-CRP and the Gensini score were determined. The results
indicated that the Gensini score and expression of MPO, Hcy and
hs-CRP in the MVG were higher than those in the DVG and SVG, and
the Gensini score and expression of MPO, Hcy and hs-CRP in the DVG
were higher than those in the SVG (P<0.05). There was a positive
correlation between the Gensini score and the levels of MPO, Hcy
and hs-CRP, which indicated that higher expression of MPO, Hcy and
hs-CRP were directly linked to the severity of the CAD. Next, the
MACEs recorded were compared among the three groups with different
degrees of lesions and the results suggested that the total
incidence of MACEs in the MVG was higher than that in the SVG and
the DVG, and the total incidence of MACEs in the DVG was higher
than that in the SVG (P<0.05). This further indicated that
higher expression of MPO, Hcy and hs-CRP was directly linked to the
severity of CAD and increased risk of MACEs. A previous study
explored the association between MPO and acute coronary syndrome,
indicating that the concentration of MPO in the plasma of patients
with acute coronary syndrome is able to predict the risk of heart
disease (24); higher levels of MPO
were associated with a higher risk of death, and therefore, this
was consistent with the conclusion of the present study. In terms
of the expression of Hcy and hs-CRP in the serum, one study
suggested that high levels of Hcy are able to cause damage to blood
vessels and destroy the elasticity of the blood vessel wall
(25). One study demonstrated a
positive correlation between the increased expression of Hcy and
the incidence of acute coronary syndrome and MACEs (26). Hs-CRP may induce macrophages to
absorb and oxidize low-density lipoproteins, and it is also able to
stimulate macrophages to release pre-thrombotic tissue factor
(27). In addition, one study
suggested that the expression of hs-CRP varied in the sera of
patients with different degrees of CAD (28). The severity of CAD was directly
linked to the expression of hs-CRP (29). All of the above studies confirmed the
conclusions of the present study and briefly explained the
mechanism. Finally, the predictive value of MPO, Hcy and hs-CRP for
MACEs was analyzed. The results suggested that the three factors
had high predictive value for MACEs and the predictive value of MPO
for MACEs was higher than that of the other two factors. This
suggested that MPO, Hcy and hs-CRP are somewhat accurate in
predicting MACE, but the predictive value of MPO is higher,
although hs-CRP showed a higher specificity. A previous study
explored the predictive value of MPO and Hcy for MACEs in patients
with acute coronary syndrome and demonstrated that MPO and Hcy had
a high predictive value (30). A
further study clearly indicated that MPO has a higher predictive
value for MACEs in patients with CAD within six months when
compared to other conventional indicators (31). This was similar to the result of the
present study. Logistic multivariate analysis indicated that the
number of lesions, hypertension, diabetes, MPO, Hys and hs-CRP were
independent risk factors for MACEs, suggesting that the prognosis
of patients may be improved by prompt intervention in these
factors. A previous study has clearly indicated that MPO and hs-CRP
may be used to predict MACEs in patients with CAD (32). In addition, the combination of hs-CRP
and Hcy had a high predictive value for increased risk of coronary
artery disease in a Korean population (33). This is consistent with the present
results.
In conclusion, elevated plasma levels of MPO, Hcy
and hs-CRP were directly associated with the severity of CAD and
the risk of MACEs. MPO, Hcy and hs-CRP may be used to effectively
predict the occurrence of MACEs in patients with CAD, and they have
important clinical significance for judging the condition of
patients and improving prognosis. However, the present study has
certain limitations. For instance, the specific mechanism
underlying the role of MPO, Hcy and hs-CRP in CAD remains to be
fully explored and only relevant studies were cited to briefly
describe the mechanism. In future studies, the association of MPO,
Hcy and hs-CRP with CAD, as well as the mechanism, should be
further verified.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MuC and MgC conceived and designed the study and
interpreted the results. QW contributed to the design of the study
and interpretation of the results. MuC and QW performed
experiments, analyzed data, prepared figures and drafted the
manuscript. MuC, MgC and QW approved final version of the
manuscript. mgC edited and revised the manuscript. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Xingtai People's Hospital (Xingtai, China). All study participants
provided written informed consent prior to participating in the
study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ahmadi A, Min J, Berger A, Achenbach S,
Alaamri S, Al-Mallah M, Berman D, Budoff M, Cademartiri F,
Callister T, et al: Does prognosis change depending on number and
composition of non obstructive plaques? Results from the
multinational coronary CT angiography evaluation for clinical
outcome: An international multicenter registry (CONFIRM). J Am Coll
Cardiol. 63(A980)2014.
|
|
2
|
Holman RR, Coleman RL, Chan JCN, Chiasson
J-L, Feng H, Ge J, Gerstein HC, Gray R, Huo Y, Lang Z, et al: ACE
Study Group: Effects of acarbose on cardiovascular and diabetes
outcomes in patients with coronary heart disease and impaired
glucose tolerance (ACE): A randomised, double-blind,
placebo-controlled trial. Lancet Diabetes Endocrinol. 5:877–886.
2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Li H, Sun K, Zhao R, Hu J, Hao Z, Wang F,
Lu Y, Liu F and Zhang Y: Inflammatory biomarkers of coronary heart
disease. Front Biosci. 22:504–515. 2017.PubMed/NCBI View
Article : Google Scholar
|
|
4
|
Brown AJ, Shah ASV, West NEJ, Costopoulos
C, Orzalkiewicz M, Newby DE, Bennett MR, Mills NL and Calvert PA:
High-Sensitivity Troponin I Is Associated With High-Risk Plaque and
MACE in Stable Coronary Artery Disease. JACC Cardiovasc Imaging.
10A:A1200–A1203. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Loria V, Dato I, Graziani F and Biasucci
LM: Myeloperoxidase: A new biomarker of inflammation in ischemic
heart disease and acute coronary syndromes. Mediators Inflamm.
2008:135625. 2008.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Masud R and Baqai HZ: The communal
relation of MTHFR, MTR, ACE gene polymorphisms and
hyperhomocysteinemia as conceivable risk of coronary artery
disease. Appl Physiol Nutr Metab. 42:1009–1014. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Karolczak K, Kubalczyk P, Glowacki R,
Pietruszynski R and Watala C: Aldosterone modulates blood
homocysteine and cholesterol in coronary artery disease patients -
a possible impact on atherothrombosis? Physiol Res. 67:197–207.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tayefi M, Tajfard M, Saffar S, Hanachi P,
Amirabadizadeh AR, Esmaeily H, Taghipour A, Ferns GA, Moohebati M
and Ghayour-Mobarhan M: hs-CRP is strongly associated with coronary
heart disease (CHD): A data mining approach using decision tree
algorithm. Comput Methods Programs Biomed. 141:105–109.
2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Nortamo S, Ukkola O, Lepojärvi S, Kenttä
T, Kiviniemi A, Junttila J, Huikuri H and Perkiömäki J: Association
of sST2 and hs-CRP levels with new-onset atrial fibrillation in
coronary artery disease. Int J Cardiol. 248:173–178.
2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Rifaie O, Ahmed Abdel-Rahman M and Mabrouk
Salem Omar A: Favorable inflammatory status following intermittent
fasting in patients with atherosclerotic coronary heart disease
after revascuralization. Eur Heart J. 34 (Suppl 1)(P5502)2013.
|
|
11
|
Yang K, Dong G, Tian Y and Li J: Effects
of compound Danshen injection combined with magnesium sulfate on
serum MPO and hs-CRP in patients with severe preeclampsia. Exp Ther
Med. 16:167–170. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Liu C, Chen L, Yang Y, Huang C, Luo J and
Peng D: Myeloperoxidase and high-sensitivity C-reactive protein for
predicting major adverse cardiovascular events in patients with
coronary heart disease. Int J Clin Med. 6:262–270. 2015.
|
|
13
|
Nurkalem Z, Hasdemir H, Ergelen M, Aksu H,
Sahin I, Erer B, Yilmaz HY, Comert N, Sargin M and Eren M: The
relationship between glucose tolerance and severity of coronary
artery disease using the Gensini score. Angiology. 61:751–755.
2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Zhao W, Rasheed A, Tikkanen E, Lee J-J,
Butterworth AS, Howson JMM, Assimes TL, Chowdhury R, Orho-Melander
M, Damrauer S, et al: CHD Exome+ Consortium; EPIC-CVD Consortium;
EPIC-Interact Consortium; Michigan Biobank: Identification of new
susceptibility loci for type 2 diabetes and shared etiological
pathways with coronary heart disease. Nat Genet. 49:1450–1457.
2017.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Lee JH, Han D, Hartaigh BÓ, Gransar H, Lu
Y, Rizvi A, Park MW, Roudsari HM, Stuijfzand WJ, Berman DS, et al:
Influence of symptom typicality for predicting MACE in patients
without obstructive coronary artery disease: From the CONFIRM
Registry (Coronary Computed Tomography Angiography Evaluation for
Clinical Outcomes: An International Multicenter Registry). Clin
Cardiol. 41:586–593. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hashemian M, Poustchi H,
Mohammadi-Nasrabadi F and Hekmatdoost A: Systematic review of zinc
biochemical indicators and risk of coronary heart disease. ARYA
Atheroscler. 11:357–365. 2015.PubMed/NCBI
|
|
17
|
Luyao C, Shushan Z, Ruizheng S and Guogang
Z: GW24-e0526 The Relationship Between MPO-463 G/A, MPO-129 G/A
Gene Polymorphism and Coronary Heart Disease: A Meta-Analysis.
Heart. 99 (Suppl 3):A117–A118. 2013.
|
|
18
|
Hu J, Xu J, Zhou X, Jiang T, Li Y and
Zhang M: Correlation between MPO 129 A/G polymorphism and severity
of coronary artery disease. Zhongguo Ying Yong Sheng Li Xue Za Zhi.
27:306–310. 2011.PubMed/NCBI
|
|
19
|
Bjørnestad EØ, Borsholm RA, Svingen GFT,
Pedersen ER, Seifert R, Midttun Ø, Ueland PM, Tell GS, Bønaa KH and
Nygård O: Neopterin as an Effect Modifier of the Cardiovascular
Risk Predicted by Total Homocysteine: A Prospective 2-Cohort Study.
J Am Heart Assoc. 6(e006500)2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wang L-Y, Zhang H-L and Chen S: Effect of
atorvastatin combined with trimetazidine on oxidative stress,
hemorheology and NT-proBNP, hs-CRP in patients with coronary heart
disease. Hainan Yixueyuan Xuebao. 23:2323–2327. 2017.
|
|
21
|
Fong SW, Few LL, See Too WC, Khoo BY, Nik
Ibrahim NN, Yahaya SA, Yusof Z, Mohd Ali R, Abdul Rahman AR and
Yvonne-Tee GB: Systemic and coronary levels of CRP, MPO, sCD40L and
PlGF in patients with coronary artery disease. BMC Res Notes.
8(679)2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Karakas M, Koenig W, Zierer A, Herder C,
Rottbauer W, Baumert J, Meisinger C and Thorand B: Myeloperoxidase
is associated with incident coronary heart disease independently of
traditional risk factors: Results from the MONICA/KORA Augsburg
study. J Intern Med. 271:43–50. 2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Mansori K and Ayubi E: Comments on
association of sST2 and hs-CRP levels with new-onset atrial
fibrillation in coronary artery disease. Int J Cardiol.
257(32)2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Zhang X, Dong L, Wang Q and Xie X: The
relationship between fasting plasma glucose and MPO in patients
with acute coronary syndrome. BMC Cardiovasc Disord.
15(93)2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Huang X, Lv X, Song H, Yang Q, Sun Y,
Zhang W, Yu X, Dong S, Yao W, Li Y, et al: The relationship between
S-adenosylhomocysteine and coronary artery lesions: A case control
study. Clin Chim Acta. 471:314–320. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Szalai AJ, McCrory MA, Xing D, Hage FG,
Miller A, Oparil S, Chen Y-F, Mazzone M, Early R, Henry SP, et al:
Inhibiting C-reactive protein for the treatment of cardiovascular
disease: promising evidence from rodent models. Mediators Inflamm.
2014(353614)2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Li S, Jiao Y, Wang H, Shang Q, Lu F, Huang
L, Liu J, Xu H and Chen K: Sodium tanshinone IIA sulfate adjunct
therapy reduces high-sensitivity C-reactive protein level in
coronary artery disease patients: A randomized controlled trial.
Sci Rep. 7(17451)2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Abhashi SA, Kryeziu FU and Nazreku FD:
Increased carotid intima-media thickness associated with high
hs-CRP levels is a predictor of unstable coronary artery disease.
Cardiovasc J Afr. 24:270–273. 2013.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Tajfard M, Tavakoly Sany SB, Avan A,
Latiff LA, Rahimi HR, Moohebati M, Hasanzadeh M, Ghazizadeh H,
Esmaeily H, Doosti H, et al: Relationship between serum high
sensitivity C-reactive protein with angiographic severity of
coronary artery disease and traditional cardiovascular risk
factors. J Cell Physiol. 234:10289–10299. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Emami Razavi A, Basati G, Varshosaz J and
Abdi S: Association between HDL particles size and myeloperoxidase/
paraoxonase-1 (MPO/PON1) ratio in patients with acute coronary
syndrome. Acta Med Iran. 51:365–371. 2013.PubMed/NCBI
|
|
31
|
Kaya mg, Yalcin R, Okyay K, Poyraz F,
Bayraktar N, Pasaoglu H, Boyaci B and Cengel A: Potential role of
plasma myeloperoxidase level in predicting long-term outcome of
acute myocardial infarction. Tex Heart Inst J. 39:500–506.
2012.PubMed/NCBI
|
|
32
|
Tang WH, Shrestha K, Troughton RW,
Borowski AG and Klein AL: Integrating plasma high-sensitivity
C-reactive protein and myeloperoxidase for risk prediction in
chronic systolic heart failure. Congest Heart Fail. 17:105–109.
2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Cho D-Y, Kim K-N, Kim K-M, Lee D-J and Kim
B-T: Combination of high-sensitivity C-reactive protein and
homocysteine may predict an increased risk of coronary artery
disease in Korean population. Chin Med J (Engl). 125:569–573.
2012.PubMed/NCBI
|