Introduction
Ossification of the ligamentum flavum (OLF)
frequently occurs in the thoracic spine or at the junction of the
thoracic and lumbar spine, but rarely in the cervical spine,
particularly in the upper cervical spine (1-3).
Miyazawa and Akiyama (4) previously
reported on 50 cases of OLF of the cervical spine. However, OLF at
the C1-2 level of the cervical spine is uncommon (4). A study reported on two cases of
cervical myelopathy resulting from combined OLF and posterior
longitudinal ligament (5). The
present case study describes two cases of cervical myelopathy
resulting from OLF alone. To the best of our knowledge, no similar
cases have been reported in the English literature.
Case reports
Case 1. A 37-year-old female presented with limb
numbness and gradually progressive gait disturbance and clumsiness
for 1 year. After 7 months, the patient fell and was subsequently
not able to walk independently. The patient consulted a clinic
accompanied by her husband and was then referred to the Department
of Orthopedics of the First Affiliated Hospital of the University
of Science and Technology of China (Hefei, China). On admission
(March 2018), the patient exhibited gait disturbance due to
cervical myelopathy without any fall or injury. Her grip strength
was also decreased. Tests revealed elevated bilateral deep tendon
reflexes of the limbs. Bilateral pathological reflexes were
positive and bilateral Hoffmann's sign was positive. Motor weakness
was noted mainly on the right side at and below the level of the
deltoid. Sensory tests revealed significant hypoalgesia at and
below the C6 level. The Japanese Orthopedic Association (JOA) score
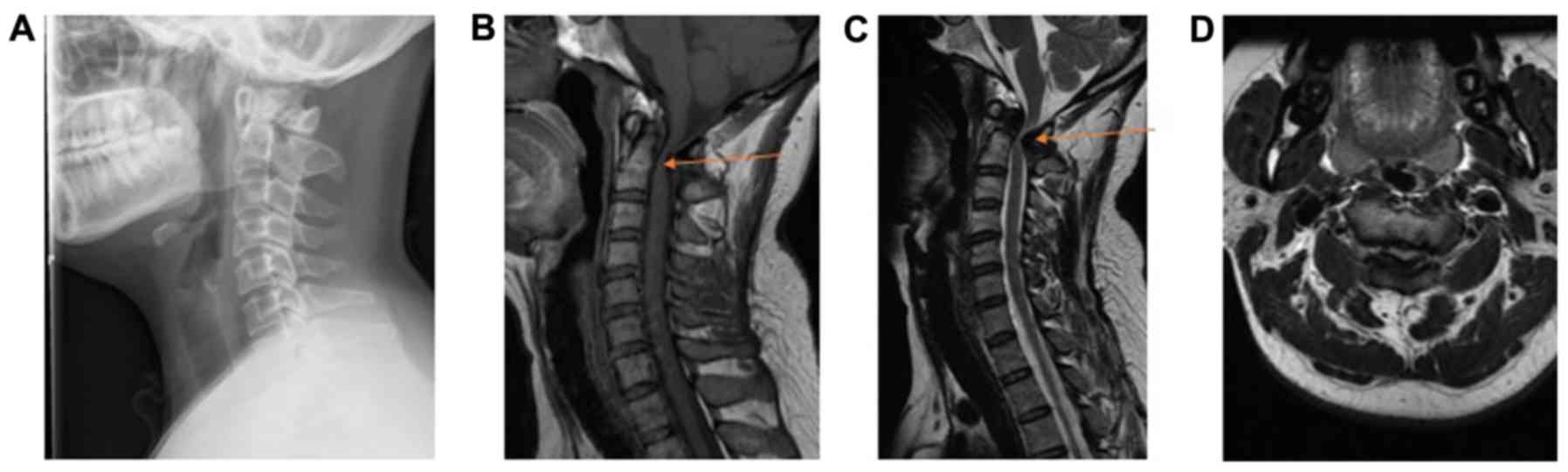
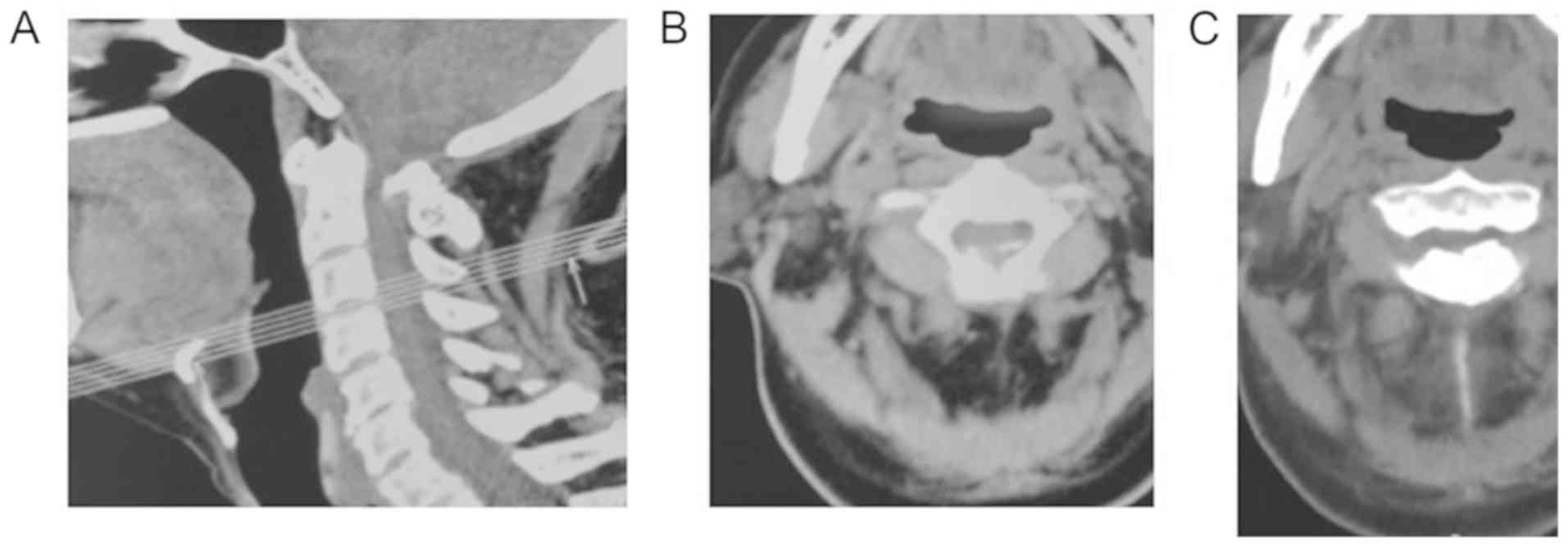
was 6 out of 17(6). T1- and
T2-weighted MRI revealed severe spinal cord compression at the C1-2
level. In the sagittal view, the dural sac was compressed from the
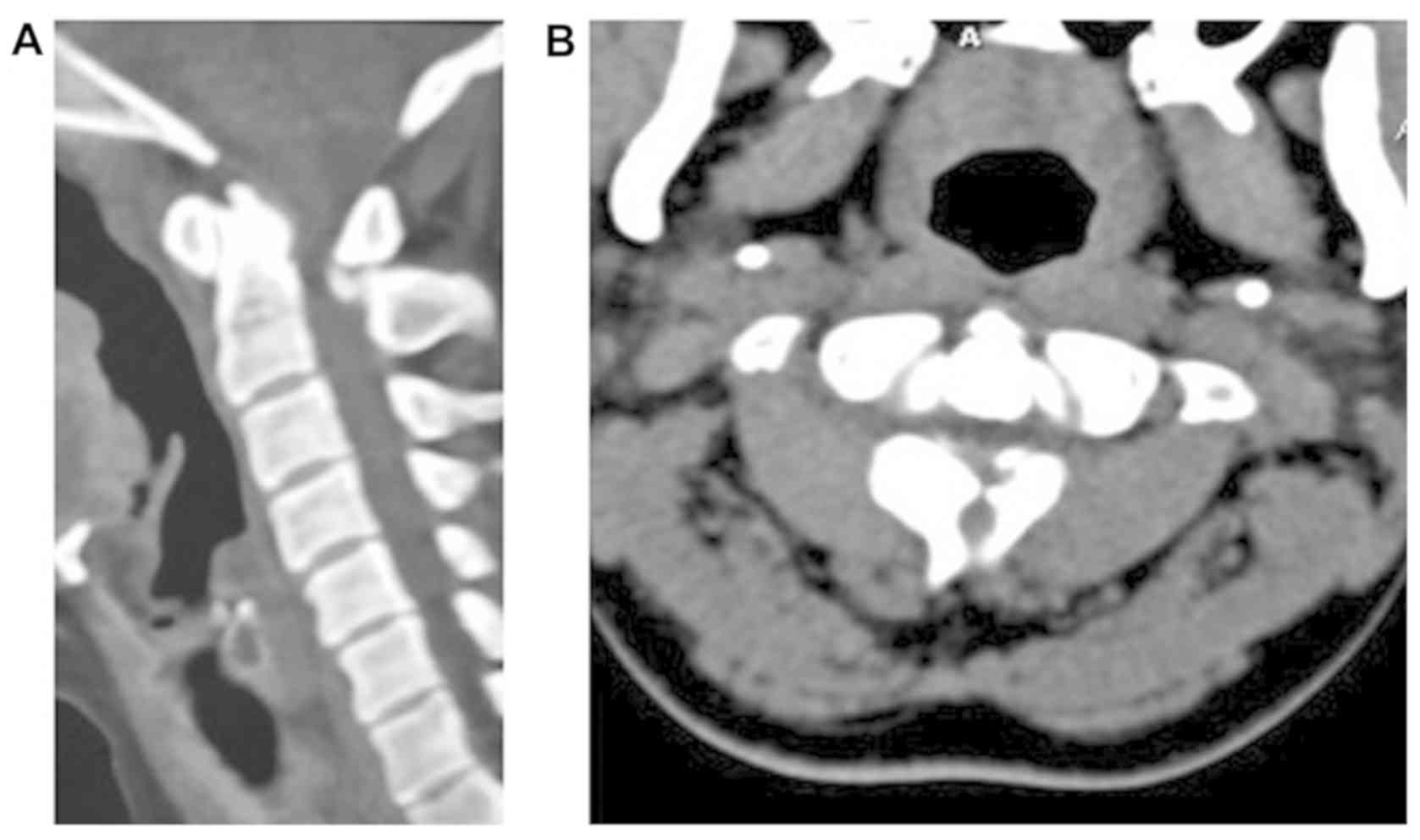
posterior side by a hypointense mass (Fig. 1). CT indicated OLF at the C1-2 level
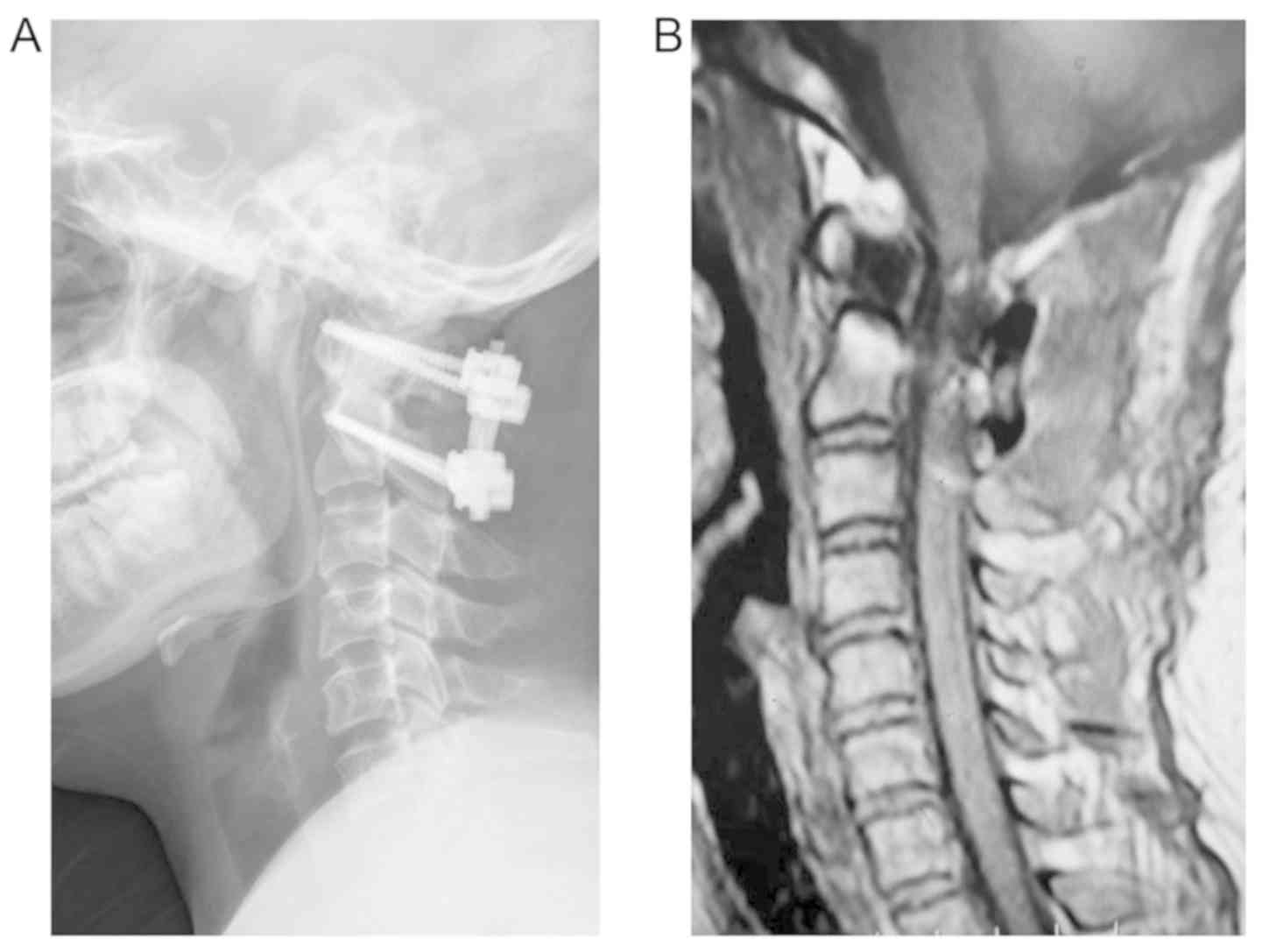
(Fig. 2). A C1-2 laminectomy and OLF
resection were performed (Fig. 3).
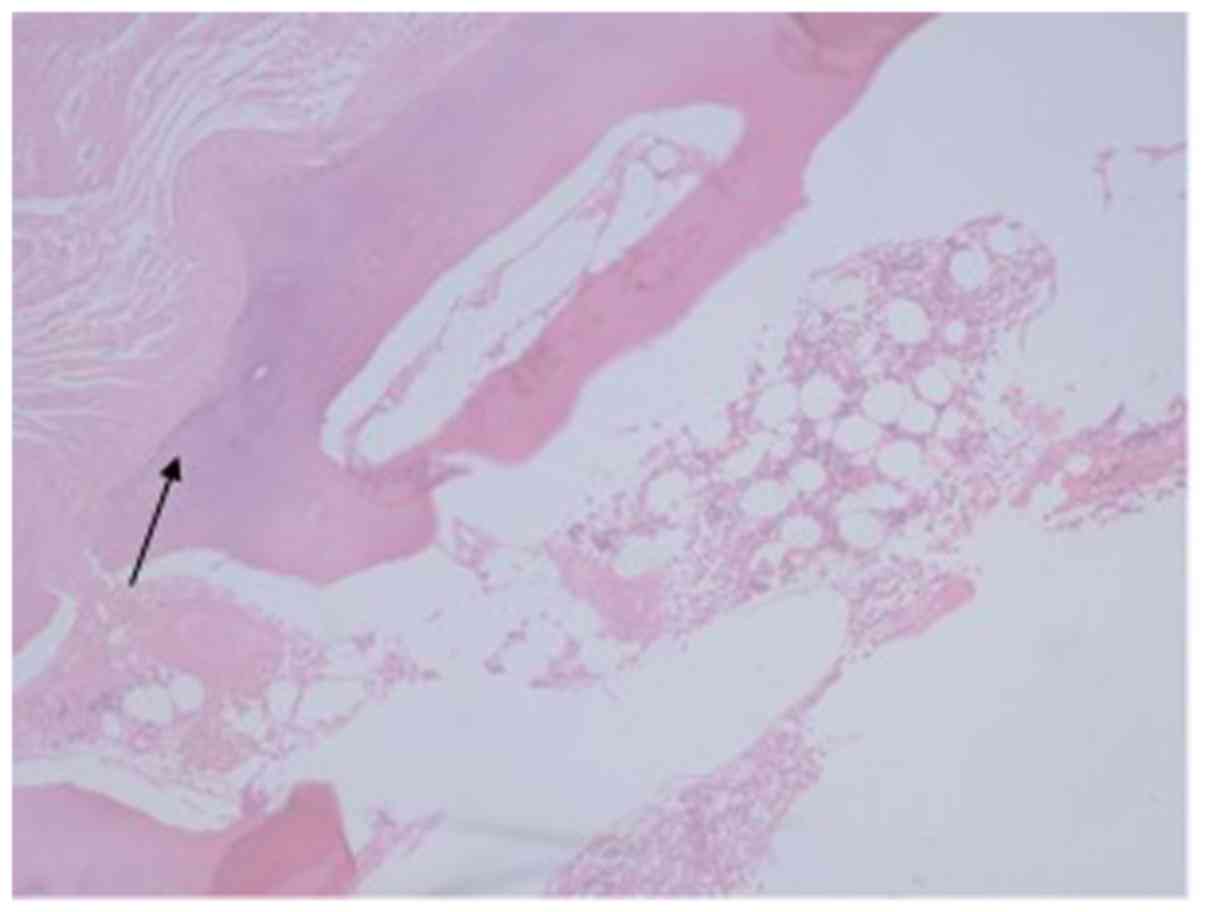
H&E staining of the resected ligamentum flavum was performed as
previously described (7). Glass
slides holding the paraffin sections were placed in staining racks.
The paraffin was cleared from the samples with three 2-minchanges
of xylene. Samples were then hydrated and stained in hematoxylin
solution for 3 min. Subsequently, the samples were stained with
working eosin Y solution for 2 min and dehydrated. Finally, the
slides were viewed using a microscope. The post-operative
histological examination of surgical specimens revealed osseous
tissues and enchondral ossification within the ligament, which
confirmed the diagnosis of OLF (Fig.
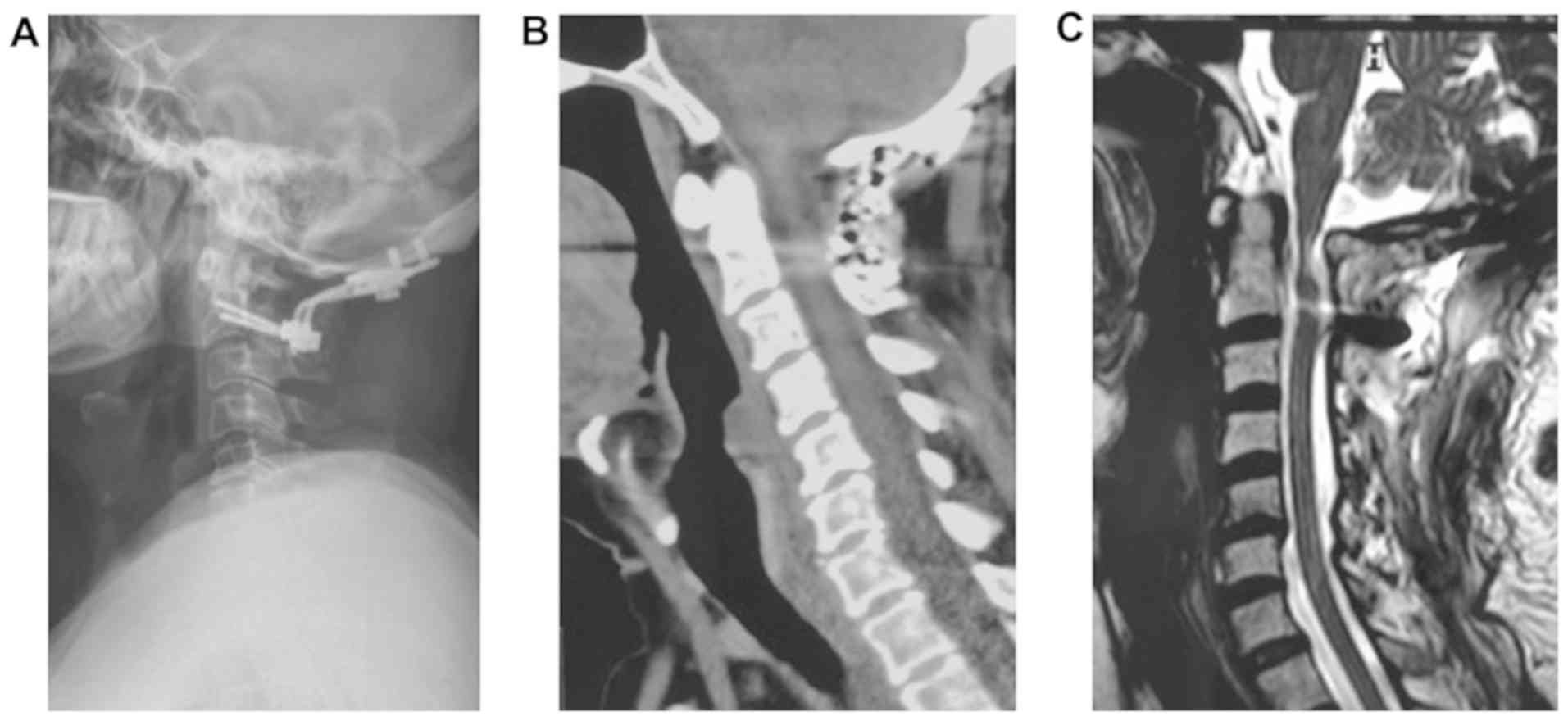
4). At 1 month after the operation, the patient was able to
walk independently. The imaging materials demonstrated that the
internal fixation was successful and that the spinal cord was
decompressed at the C1-2 level (Fig.
5). The post-operative JOA score was also improved to 11, and
this further improved to 12.5 at the 3-month follow-up. In
addition, the patient's JOA score was still 12 at the 13-month
follow-up.
Case 2. A 63-year-old male presented with sensory
disturbance in the right upper extremity for 3 years, aggravated
with weakness in lower extremities for 3 months. Recently (March
2018), he had experienced difficulties with fine finger activities.
After consulting a clinic due to concern about his symptoms, the
patient was admitted to the Department of Orthopedics of the First
Affiliated Hospital of the University of Science and Technology of
China (Hefei, China). Physical examination revealed a spastic gait
and decreased bilateral grip, with decreased lower-extremity muscle
strength. The deep tendon reflexes were elevated at the level of
the biceps and triceps. The bilateral Hoffmann's sign and
pathological reflexes in the lower extremities were positive.
Sensory tests indicated hypoalgesia at and below the level of C5.
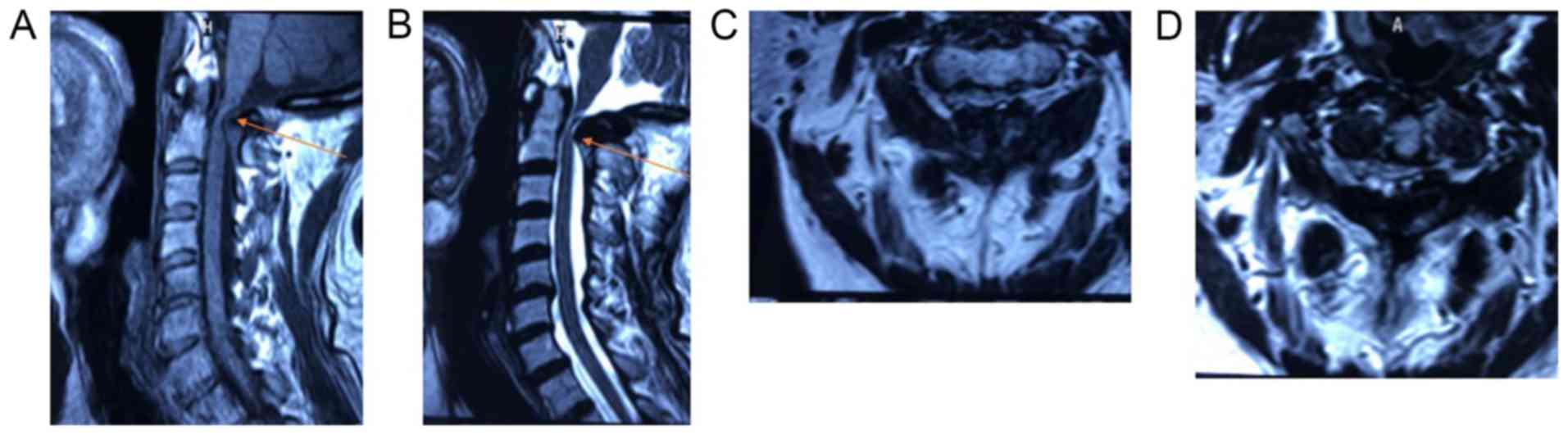
The JOA score was 6 out of 17.T1- and T2-weighted MRI revealed a
hypointense mass compressing the dural sac from the posterior at
C1-2 in the sagittal view and from the bilateral side of the lamina
in the axial view (Fig. 6). Cervical
dislocation at the level of C5-6 was also noted. No dural sac
compression from the anterior aspect was noted in the cervical
spine. CT revealed OLF at the C1-C2 level in the sagittal view and
from the bilateral sides of the lamina in the axial view (Fig. 7). A C1-2 laminectomy and OLF
resection were performed. A deformity in the posterior arch of the
atlas was present, making it difficult to fix screws during the
operation. Therefore, occipitocervical fusion and internal fixation
were adopted in this case. H&E staining was performed as
described above. After the surgery, histological examination of
surgical specimens revealed osseous tissue and ossification within
the ligamentum flavum, which confirmed the diagnosis of OLF in the
upper cervical spine (Fig. 8). MRI
scans revealed that the spinal cord was decompressed at the C1-2
level and that the OLF was totally resected (Fig. 9). The patient's symptoms
significantly improved at one week after the operation and his JOA
score improved to 12 at the 3-month follow-up. In addition, the
patient's JOA score was still 12 at the 13-month follow-up.
Discussion
The first report of a case of OLF was in the 1920s
(8). Thereafter, numerous cases were
reported in Asian countries (1).
Liang et al (9) determined
that the prevalence of cervical OLF (C-OLF) was 0.3% and there was
no significant difference in the prevalence of C-OLF between males
and females in the Chinese population. Symptomatic OLF has
predominantly been reported in the lower thoracic spine (10-12).
However, symptomatic OLF in the cervical spine is rarely observed
(13). OLF tends to arise from the
lateral capsular portion of the ligamentum flavum, whereas OLF
characteristically occurs in the thoracic spine of older females
(14,15). Miyazawa and Akiyama (4) reviewed 50 cases of OLF in the cervical
spine that were reported between 1962 and 2005. The mean age of the
patients was 56.3 years, with a male/female ratio of
1.44:1(16). Sensorimotor deficits
were common in those patients with OLF. Sensory disturbance in the
extremities is usually the initial symptom of OLF (4). Rahimizadeh et al (17) reviewed 68 cases of C-OLF resulting in
progressive quadriparesis and demonstrated that C-OLF rarely leads
to cervical myeloradiculopathy. Different imaging techniques have
different advantages in the diagnosis of disease (18). MRI may reveal hypertrophy of the
ligamentum flavum and compression of the spinal cord in the
cervical spine (18). The causes of
OLF in the cervical spine remain to be elucidated (19). The diagnosis of OLF is thought to be
different from that of other pathologies in that the clinician must
distinguish OLF from other pathologies including spinal tumors
(19). Based on CT scans, bone
destruction may at times be observed. The lesion maybe easily
detected on MRI. The long axis of the tumor is parallel to the long
axis of the spinal cord. As the disease progresses, cystic changes
and spinal cavities are prone to occur. Regarding chondroma in the
ligamentum flavum or the laminar arch, X-rays may display round or
irregular bone-like density shadows adjacent to the vertebral body.
The internal density was uneven, the lesions were clear and side
attachment was involved in both of the reported cases. MRI, CT and
myelography may be used to assess the size and extent of the damage
caused by osteochondroma and reveal the structures obscured by
ordinary X-rays. CT is advantageous compared with MRI for the
observation of osteochondroma, and is able to reveal details of the
cartilage and bones, whereas MRI displays the nerve structure more
clearly than CT. However, the diagnosis must rely on pathological
biopsy. Post-operative pathology also proved the diagnosis of
C-OLF. According to several studies, the characteristics of C-OLF
are similar to those observed in thoracic OLF. Yayama et al
(20) reported that certain
metabolic disorders may promote the ossification of ligaments and
that specific osteogenic cytokines, including bone morphogenetic
protein 2 and transforming growth factor-β, may have a role in the
development of ossification. The optimal treatment for C-OLF
remains to be determined, since only a small number of clinical
reports are currently available (21). However, for patients with apparent or
progressive neurological deficits, lesional resection and
decompression of the cervical spinal cord are usually the preferred
treatment options (22). Various
tools (such as clam, ultrasonic osteotome and rongeur) may be used
to remove the lesion. The actual tools used depend on the
facilities at the local hospital, the surgeon's proficiency and the
financial ability of the patients (22). During the surgeries of the two cases
in the present report, enlarged and hardened ligamentum flavum were
observed. The white powder-like substance inside the ligament was
solid. The dorsal side of the cervical spinal cord was compressed.
In the two patients of the present study, the surgeries were
performed with the aid of an ultrasonic osteotome. The ultrasonic
osteotome has the advantage of tissue selectivity and eliminates
the dangerous rotatory motion of the high speed burr, thus allowing
a more safe removal of C-OLF (23).
In the present study, since the lesion was located at the junction
between the occipital bone and the neck, once the laminectomy was
performed, cervical instability was likely to occur (24). Therefore, fusion surgery was selected
for these patients rather than stand-alone decompressive
laminectomy. A search of the English literature revealed the
importance of decompression, but few studies mentioned the method
of internal fixation (25,26). It was hypothesized that the process
of decompression may partially destroy the stability of the
cervical spine. There are certain difficulties in performing the
process of internal fixation in the upper cervical spine. The
experience of the surgeon, deformity of the upper cervical spine
and facilities of local hospitals may ultimately influence the
choice of modality of internal fixation. Further research is
required to develop guidelines for treating these diseases. During
surgery, spinal cord injury and cerebrospinal fluid leakage may
occur due to dural adhesion (27).
To ensure the safety of the operation, it may be recommended that
only doctors with specific experience in upper cervical surgery
perform these operations. A longer follow-up period may further
confirm the diagnosis and therapy of these cases found in the
present report. The patients were actively followed up for 18
months and it was determined that their clinical symptoms did not
recur. However, due to economic reasons, the patients did not
receive a complete imaging assessment.
In conclusion, the present study described two cases
of neurological deficits resulting from C-OLF alone. The symptoms
were significantly improved in both patients following laminectomy
and internal fixation. On the basis of the literature review,
further research is required to reveal optimal treatment for
C-OLF.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
RH and HF examined patients and collected clinical
data; RH performed the surgery and analyzed radiological imaging
data; RH and HF wrote the manuscript. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
Informed consent was obtained from the study
subjects and the study followed the institute's committee on human
research protocols.
Patient consent for publication
Informed written consent was obtained from the
patients prior to all procedures described in the report, as well
as for the use of the patient's clinical information and images for
published scientific purposes.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Aizawa T, Sato T, Sasaki H, Kusakabe T,
Morozumi N and Kokubun S: Thoracic myelopathy caused by
ossification of the ligamentum flavum: Clinical features and
surgical results in the Japanese population. J Neurosurg Spine.
5:514–519. 2006.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ben Hamouda K, Jemel H, Haouet S and
Khaldi M: Thoracic myelopathy caused by ossification of the
ligamentum flavum: A report of 18 cases. J Neurosurg. 99 (Suppl
2):157–161. 2003.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chou YC, Lee CC, Yen PS, Lin JF, Su CF,
Lin SZ and Chen WF: Cough induced by ossification of the ligamentum
flavum in the high cervical spine. Case report. J Neurosurg. 100
(Suppl 4):364–366. 2004.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Miyazawa N and Akiyama I: Ossification of
the ligamentum flavum of the cervical spine. J Neurosurg Sci.
51:139–144. 2007.PubMed/NCBI
|
|
5
|
Kotani Y, Takahata M, Abumi K, Ito M, Sudo
H and Minami A: Cervical myelopathy resulting from combined
ossification of the ligamentum flavum and posterior longitudinal
ligament: report of two cases and literature review. Spine J.
13:e1–6. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gupte G, Peters CM, Buchowski JM, Zebala
LP, Sudo H and Minami A: Reliability of the Neck Disability Index
and Japanese Orthopedic Association questionnaires in adult
cervical radiculopathy and myelopathy patients when administered by
telephone or via online format. Spine J. 19:1154–1161.
2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Cardiff RD, Miller CH and Munn RJ: Manual
hematoxylin and eosin staining of mouse tissue section. Cold Spring
Harb Protoc. 2014:655–658. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Polgar F: Über interarkuelle
Wirbelverkalkung. Fortschr Geb Rontgen. 40:292–298. 1929.(In
German).
|
|
9
|
Liang H, Liu G, Lu S, Chen S, Jiang D, Shi
H and Fei Q: Epidemiology of ossification of the spinal ligaments
and associated factors in the Chinese population: A cross-sectional
study of 2000 consecutive individuals. BMC Musculoskelet Disord.
20(253)2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ando K, Imagama S, Kobayashi K, Hida T,
Ito K, Tsushima M, Ishikawa Y, Matsumoto A, Nishida Y and Ishiguro
N: Comparative study of surgical treatment and nonsurgical follow
up for thoracic ossification of the posterior longitudinal
ligament: radiological and clinical evaluation. Spine. 42:407–410.
2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Singhal U, Jain M, Jaiswal AK and Behari
S: Unilateral ossified ligamentum flavum in the high cervical spine
causing myelopathy. Indian J Orthop. 43:305–308. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Christiano LD, Assina R and Goldstein IM:
Ossification of the ligamentum flavum: A unique report of a
Hispanic woman. Neurosurg Focus. 30(E15)2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kawaguchi Y, Nakano M, Yasuda T, Seki S,
Hori T, Suzuki K, Makino H and Kimura T: Characteristics of
ossification of the spinal ligament; incidence of ossification of
the ligamentum flavum in patients with cervical ossification of the
posterior longitudinal ligament - Analysis of the whole spine using
multidetector CT. J Orthop Sci. 21:439–445. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Miyasaka K, Kaneda K, Sato S, Iwasaki Y,
Abe S, Takei H, Tsuru M, Tashiro K, Abe H and Fujioka Y: Myelopathy
due to ossification or calcification of the ligamentum flavum:
Radiologic and histologic evaluations. AJNR Am J Neuroradiol.
4:629–632. 1983.PubMed/NCBI
|
|
15
|
Takahashi T, Hanakita J and Minami M:
Pathophysiology of calcification and ossification of the ligamentum
flavum in the cervical spine. Neurosurg Clin N Am. 29:47–54.
2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ohara Y: Ossification of the ligaments in
the cervical spine, including ossification of the anterior
longitudinal ligament, ossification of the posterior longitudinal
ligament, and ossification of the ligamentum flavum. Neurosurg Clin
N Am. 29:63–68. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Rahimizadeh A, Asgari N, Soufiani H and
Rahimizadeh S: Ossification of the cervical ligamentum flavum and
case report with myelopathy. Surg Neurol Int. 9(263)2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ponte A, Orlando G and Siccardi GL: The
true ponte osteotomy: By the one who developed it. Spine Deform.
6:2–11. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Muthukumar N and Muthukumar N:
Ossification of the ligamentum flavum as a result of fluorosis
causing myelopathy: Report of two cases. Neurosurgery.
56(E622)2005.PubMed/NCBI
|
|
20
|
Yayama T, Uchida K, Kobayashi S, Kokubo Y,
Sato R, Nakajima H, Takamura T, Bangirana A, Itoh H and Baba H:
Thoracic ossification of the human ligamentum flavum:
Histopathological and immunohistochemical findings around the
ossified lesion. J Neurosurg Spine. 7:184–193. 2007.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chen Y, Chen DY, Wang XW, Lu XH, Yang HS
and Miao JH: Single-stage combined decompression for patients with
tandem ossification in the cervical and thoracic spine. Arch Orthop
Trauma Surg. 132:1219–1226. 2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Liang H, Liu G, Lu S, Chen S, Jiang D, Shi
H and Fei Q: Epidemiology of ossification of the spinal ligaments
and associated factors in the Chinese population: a cross-sectional
study of 2000 consecutive individuals. BMC Musculoskelet Disord.
20(253)2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kim CH, Renaldo N, Chung CK and Lee HS:
Use of an ultrasonic osteotome for direct removal of beak-type
ossification of posterior longitudinal ligament in the thoracic
spine. J Korean Neurosurg Soc. 58:571–577. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Li J, Yan DL, Gao LB, Tan PX, Zhang ZH and
Zhang Z: Comparison percutaneous cervical disc nucleoplasty and
cervical discectomy for the treatment of cervical disc herniation.
Zhonghua Wai Ke Za Zhi. 44:822–825. 2006.PubMed/NCBI(In Chinese).
|
|
25
|
An B, Li XC, Zhou CP, Wang BS, Gao HR, Ma
HJ, He Y, Zhou HG, Yang HJ and Qian JX: Percutaneous full
endoscopic posterior decompression of thoracic myelopathy caused by
ossification of the ligamentum flavum. Eur Spine J. 28:492–501.
2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ikuta K, Tarukado K, Senba H, Kitamura T,
Komiya N, Fukutoku Y and Shidahara S: Decompression procedure using
a microendoscopic technique for thoracic myelopathy caused by
ossification of the ligamentum flavum. Minim Invasive Neurosurg.
54:271–273. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Yang H, Lu X, Wang X, Chen D, Yuan W, Yang
L and Liu Y: A new method to determine whether ossified posterior
longitudinal ligament can be resected completely and safely: Spinal
canal ‘Rule of Nine’ on axial computed tomography. Eur Spine J.
24:1673–1680. 2015.PubMed/NCBI View Article : Google Scholar
|