Introduction
Most silicosis patients are quarrying, coal mine,
glass, ceramics factory workers because silicosis is an
occupational disease caused by long-term exposure and inhalation of
silica dust (1,2). Silica dust enters the respiratory tract
and alveoli by breathing, causing inflammation in the lungs, and
then causing pulmonary fibrosis, which seriously affects the
pulmonary function (3). According to
statistics, the number of silicosis patients in developing
countries has exceeded 600,000; the number of new cases has
increased rapidly, and the rate of death from silicosis continues
to increase (4). Silicosis is an
irreversible chronic disease that continues to deteriorate. The
treatment is based on the principle of avoiding complications as
far as possible and needs long-term medication, and the quality of
life of patients will be seriously affected with the development of
the disease (5). The silicotic lung
has the characteristics of high medical costs, high disability rate
and high mortality rate, heavy financial burden and psychological
pressure on the patient's family, and no special drugs have been
developed for the treatment of silicosis so far, therefore, the
treatment can only be the basis of controlling and delaying the
development of the disease, and the main purpose is to improve the
immune function and quality of life of patients at the same time
(6). Dyspnea in silicosis patients
is caused by obstruction of the airway, while the relevant Chinese
literature shows that 6-min walk test (6MWT) is related to dyspnea,
which can be used as an index to evaluate patient's exercise
tolerance. 6MWT is currently an objective evaluation index for
exercise tolerance in patients with chronic obstructive pulmonary
disease, respiratory failure and other lung diseases (7,8).
Acetylcysteine, the main active component of
acetylcysteine effervescent tablets, is widely used in the
treatment of many respiratory diseases, such as bronchial asthma,
chronic obstructive pulmonary disease because it can dissolve
concentrated phlegm (9). In
addition, it has been reported that acetylcysteine has antioxidant
and inhibitory effects on neutrophil chemotaxis in bronchial mucosa
of silicosis patients (10).
Tetrandrine, as an alkaloid, plays a major role in analgesia,
anti-inflammation, and can effectively improve pulmonary vascular
smooth muscle spasm, thereby improving pulmonary microcirculation,
thus reducing clinical features such as cough and chest tightness
in patients (11,12).
Because most of the previous studies focused on lung
ventilation and pulmonary function in silicosis patients, the
clinical efficacy of acetylcysteine combined with tetrandrine
tablets on the basis of conventional therapy in treatment of
silicosis and the observation of exercise tolerance and pulmonary
function in patients were conducted in this study to provide a
certain theoretical basis and clues for the clinical application of
drugs.
Patients and methods
Methods
In total, 248 cases of silicosis patients with an
average age of 50.42±9.67 years and treated in Branch of Tai'an
City Central Hospital (Tai'an, China) from October 2015 to 2017
were retrospectively analyzed in this study, including 226 males
and 22 females. Further 116 cases with conventional therapy were
the control group, and 132 cases treated with acetylcysteine and
tetrandrine tablets on the basis of conventional therapy were the
observation group. There was no significant difference in general
information between the two groups (P>0.05). All patients met
the criteria for diagnosis and staging of silicosis (13). The cases were excluded due to
pregnancy, lactation, other tumors, liver and kidney dysfunction,
emphysema, pulmonary tuberculosis and other lung related diseases.
Patients with incomplete clinical data or lost to follow-up were
also excluded. This study was approved by the Ethics Committee of
the hospital. All the subjects were informed and agreed to
participate in the clinical study, and the patients and their
families signed a fully informed consent form. General information
is provided in Table I.
 | Table IGeneral information (n). |
Table I
General information (n).
| Factors | Observation group
(n=132) | Control group
(n=116) | χ2
value | P-value |
|---|
| Age (years) | | | 0.183 | 0.703 |
|
<50 | 59 | 55 | | |
|
≥50 | 73 | 61 | | |
| Sex | | | 1.051 | 0.374 |
|
Male | 118 | 108 | | |
|
Female | 14 | 8 | | |
| Stage | | | 0.267 | 0.878 |
|
Ⅰ | 84 | 76 | | |
|
Ⅱ | 32 | 25 | | |
|
Ⅲ | 16 | 15 | | |
| Dust exposure time
(year) | | | 0.283 | 0.678 |
|
<10 | 94 | 79 | | |
|
≥10 | 38 | 37 | | |
| Complication | | | 1.051 | 0.374 |
|
Yes | 14 | 8 | | |
|
No | 118 | 108 | | |
| Smoking | | | 0.762 | 0.683 |
|
Past
smoker | 79 | 65 | | |
|
Current
smoker | 24 | 20 | | |
|
Never
smoked | 29 | 31 | | |
Medicines and instruments
Ambroxol Hydrochloride oral liquid was from Hong
Kong Bright Future Pharmaceutical Laboratories Limited (SFDA
approval no. H20067008). Xiaokechuan tablet was from the sixth
pharmaceutical factory of Harbin Pharmaceutical Group Co., Ltd.
(SFDA approval no. Z23021362). Acetylcysteine effervescent tablets
and tetrandrine were from Zhejiang Jinhua Conba Biopharma Co., Ltd.
(SFDA approval no. H20057334, SFDA approval no. H33022075). British
BTL08 lung function instrument was from Chengdu Buywells Science
and Technology Co., Ltd.
Treatment methods
All patients stayed at home and stopped working
during treatment, avoiding contact with silica dust and severely
damaging working environment. All patients took the medicine on
time, did not take other health care products or medicines
privately, and did not use other means of recovery. The daily
intake of the diet was light and varied. The control group was
treated with conventional therapy: Dosage of ambroxol hydrochloride
oral liquid 10 ml/time, 2 times daily. At the same time,
Xiaokechuan tablet were taken orally 4 tablets/time, 3 times daily.
The observation group was treated with acetylcysteine and
tetrandrine tablets on the basis of routine treatment: Dosage of
acetylcysteine effervescent tablets 0.6 g/time, 2 times daily;
dosage of tetrandrine tablets 100 mg/time, 2 times daily. After 6
days, the drug was stopped for 1 day. The two groups were treated
with 4 courses for 8 months. The treatment course of the patient
was decided by the attending doctor according to the condition of
the patient, and the treatment time was adequate (14).
Evaluation of clinical efficacy,
adverse reactions and side effects
The respiratory symptoms 1 week before and after
treatment of the two groups were evaluated according to the
internationally accepted St. George's Respiratory questionnaire
(SGRQ) (15), including chest
tightness, chest pain, cough and sputum production.
Improvement rate = (number of patients with the
above symptoms before treatment, number patients with the above
symptoms after treatment)/number of patients with the above
symptoms before treatment x100%.
Side effects of the drug include mild lethargy,
fatigue, epigastric discomfort, nausea and vomiting.
Evaluation of pulmonary function
Pulmonary function before and after treatment was
measured by pulmonary function instrument, including the following
indicators: Forced vital capacity (FVC) and forced expiratory
volume in 1 sec (FEV1).
Evaluation of exercise tolerance
Exercise tolerance before and after treatment was
measured by 6MWT (16). A straight
line of 30 m long was drawn on the indoor floor with a marker at
each end, and the patient controlled the speed and walked along the
line to and fro. The walking distance within 6 min was
calculated.
Statistical analysis
Statistical analysis was carried out using SPSS 19.0
(IBM, Corp.) software. The count data were expressed as [n(%)], and
analyzed with the χ2 test. The measurement data were
expressed as (mean ± SD). The data of the two groups were compared
by t-test, and the data of multiple groups were compared by Oneway
ANOVA. P<0.05, indicates a statistically significant
difference.
Results
Clinical symptoms and adverse
reactions of the two groups before and after treatment
The symptoms of chest tightness, chest pain, cough
and sputum production in the observation group and the control
group after treatment were significantly lower than those before
treatment, the difference was statistically significant
(P<0.05). There was no significant difference in chest
tightness, chest pain, cough and sputum production between the two
groups before treatment (P>0.05). The improvement rate of chest
tightness, chest pain, cough and sputum production in the
observation group after treatment was significantly higher than
that in the control group, and the difference was statistically
significant (P<0.05).
According to the follow-up results, the control
group did not have adverse reactions during the treatment period;
in the observation group, there were 4 patients with adverse
reactions such as nausea, abdominal pain and abdominal distension
during treatment. One of them had an increase in transaminase
activity, the adverse reaction disappeared 1 month after the drug
was stopped according to the doctor's advice. According to the
results of reexamination, there was no significant changes in ECG,
renal function, and blood routine indicators between the
observation group and the control group (Table II).
 | Table IIClinical symptoms of the both groups
before and after treatment (n). |
Table II
Clinical symptoms of the both groups
before and after treatment (n).
| Indicator | Observation
group | Control group | χ2
value | P-value |
|---|
| Chest tightness | 132 | 116 | 4.616 | 0.035 |
|
Before
treatment | 124 | 109 | | |
|
After
treatment | 77 | 82 | | |
|
Improvement
rate (%) | 37.90 | 24.77 | | |
| Chest pain | | | 6.853 | 0.013 |
|
Before
treatment | 117 | 104 | | |
|
After
treatment | 62 | 73 | | |
|
Improvement
rate (%) | 47.01 | 29.81 | | |
| Cough | | | 17.768 | <0.001 |
|
Before
treatment | 121 | 102 | | |
|
After
treatment | 35 | 58 | | |
|
Improvement
rate (%) | 71.07 | 43.14 | | |
| Sputum
production | | | 13.873 | <0.001 |
|
Before
treatment | 128 | 105 | | |
|
After
treatment | 42 | 60 | | |
|
Improvement
rate (%) | 67.19 | 42.86 | | |
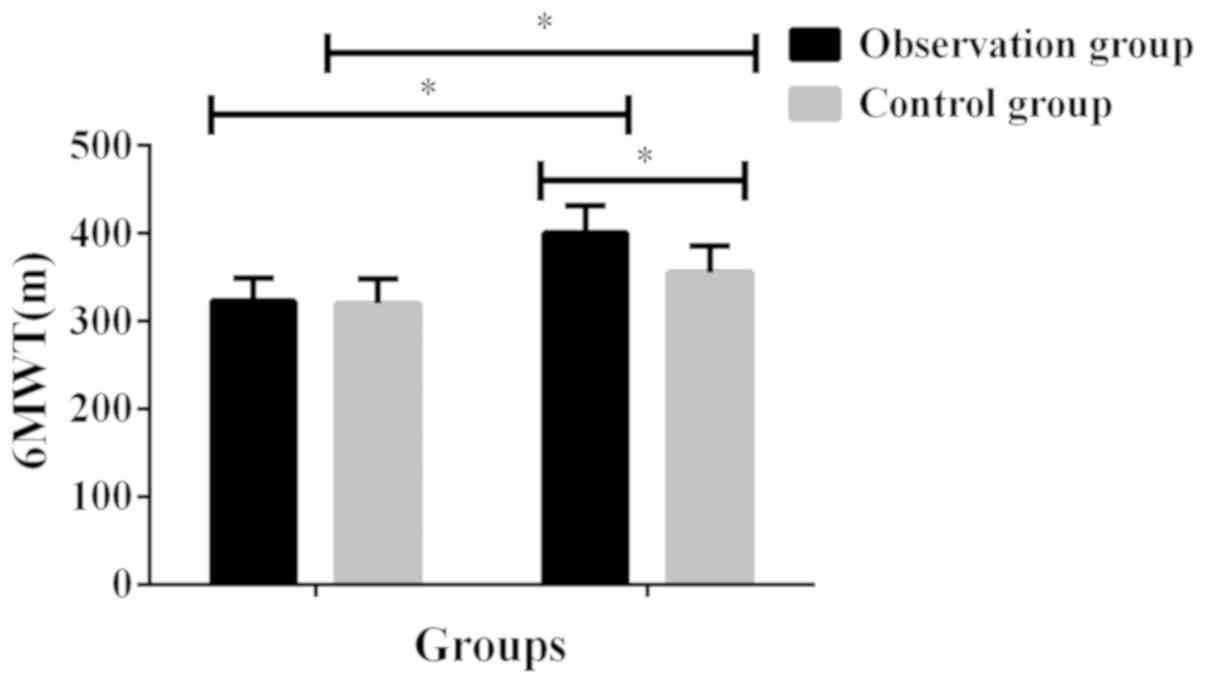
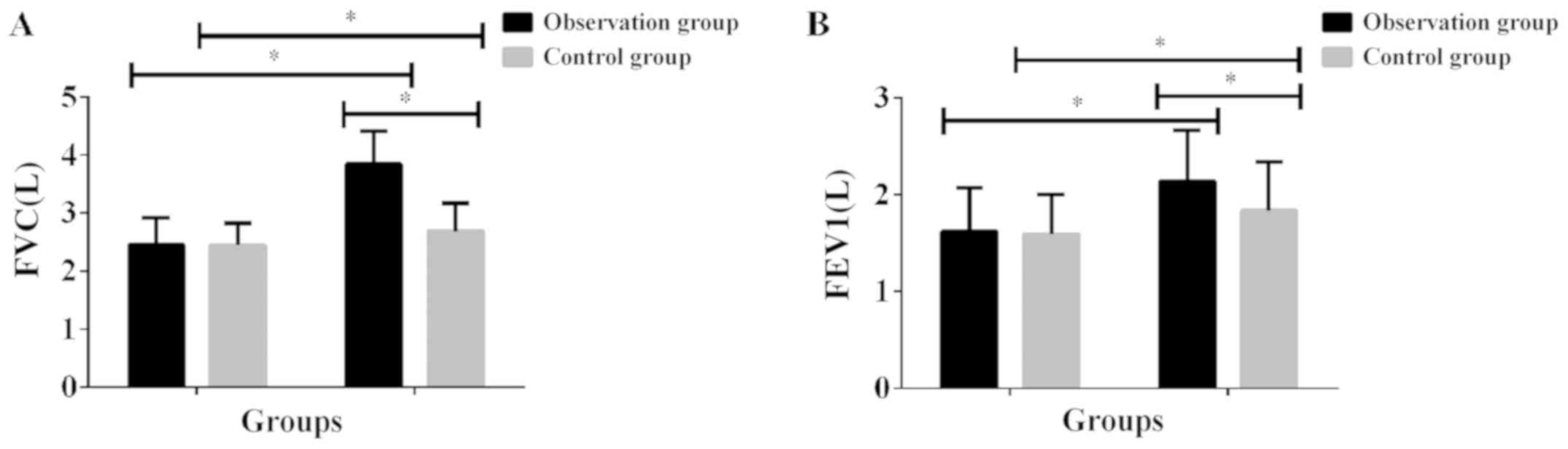
Exercise tolerance and pulmonary
function before and after treatment in the groups
The 6MWT, FVC and FEV1 in the observation group and
the control group after treatment was significantly higher than
that before treatment, and the difference was statistically
significant (P<0.001). There was no significant difference in
6MWT, FVC, FEV1 between the two groups before treatment
(P>0.05). The 6MWT, FVC and FEV1 in the observation group after
treatment was significantly higher than that in the control group,
and the difference was statistically significant (P<0.001)
(Table III and Figs. 1 and 2).
 | Table IIIExercise tolerance and pulmonary
function in both groups before and after treatment. |
Table III
Exercise tolerance and pulmonary
function in both groups before and after treatment.
| Groups | Cases | Treatment
duration | 6MWT (m) | FVC (L) | FEV1 (L) |
|---|
| Observation
group | 132 | Before
treatment | 323.24±25.83 | 2.45±0.46 | 1.62±0.45 |
| | | After
treatment |
400.67±31.27a |
3.84±0.57a |
2.14±0.52a |
| | | t value | 21.93 | 21.80 | 8.688 |
| | | P-value | <0.001 | <0.001 | <0.001 |
| Control group | 116 | Before
treatment | 320.13±28.46 | 2.44±0.39 | 1.59±0.41 |
| | | After
treatment | 355.71±30.28 | 2.69±0.48 | 1.83±0.51 |
| | | t value | 9.222 | 4.354 | 3.950 |
| | | P-value | <0.001 | <0.001 | <0.001 |
Side effects after treatment in the
groups
The comparison of the two groups showed that the
incidence of drug side effects in the observation group was
significantly lower than that in the control group (P<0.05)
(Table IV).
 | Table IVPulmonary function in both groups
before and after treatment. |
Table IV
Pulmonary function in both groups
before and after treatment.
| Groups | Cases | Treatment
duration | FVC (L) | FEV1 (L) |
|---|
| Observation
group | 132 | Before
treatment | 2.45±0.46 | 1.62±0.45 |
| | | After
treatment |
3.84±0.57a |
2.14±0.52a |
| | | t value | 21.80 | 8.688 |
| | | P-value | <0.001 | <0.001 |
| Control group | 116 | Before
treatment | 2.44±0.39 | 1.59±0.41 |
| | | After
treatment | 2.69±0.48 | 1.83±0.51 |
| | | t value | 4.354 | 3.950 |
| | | P-value | <0.001 | <0.001 |
Discussion
Pulmonary fibrosis is the main clinical
manifestation of silicosis which will exacerbate with the
prolongation of the course of disease. First of all, the pulmonary
blood circulation is blocked, which damages the defense system of
the respiratory tract, and results in the decrease of the patient's
immune function, the formation of repeated infection, and even
irreversible pulmonary failure in severe patients (17,18).
Because silicosis has no typical clinical symptoms in the early
stage and no special drug treatment, it is already serious when the
symptoms of chest tightness, chest pain, cough, sputum production,
etc. emerge (19). Airway
obstruction of respiratory system in silicosis patients also
affects motor function. Therefore, inhibition of pulmonary fibrosis
is the main criterion for treatment of silicosis. The efficacy of
acetylcysteine combined with tetrandrine tablets on the basis of
conventional therapy in the treatment of silicosis was evaluated
for clinical efficacy, exercise tolerance and pulmonary function in
patients.
No other studies have been found to verify the
effect of acetylcysteine combined with tetrandrine tablets on 6MWT
in patients with silicosis. However, this study showed that the
6MWT in the observation group and the control group after treatment
was significantly higher than that before treatment, and the
difference was statistically significant (P<0.001). There was no
significant difference in 6MWT between the two groups before
treatment (P>0.05). The 6MWT in the observation group after
treatment was significantly higher than that in the control group,
and the difference was statistically significant (P<0.001). The
results showed that the improvement of motor function by the
combined treatment of these two drugs was better than that by
conventional therapy. In addition, the symptoms of chest tightness,
chest pain, cough and sputum production in the observation group
and the control group after treatment were significantly lower than
those before treatment, and the difference was statistically
significant (P<0.05). There was no significant difference in
chest tightness, chest pain, cough and sputum production between
the two groups before treatment (P>0.05). The improvement rate
of chest tightness, chest pain, cough and sputum production in the
observation group after treatment was significantly higher than
that in the control group, and the difference was statistically
significant (P<0.05). The FVC and FEV1 in the observation group
and the control group after treatment were significantly higher
than those before treatment, and the difference was statistically
significant (P<0.001). There was no significant difference in
FVC and FEV1 between the two groups before treatment (P>0.05).
FVC and FEV1 in the observation group after treatment were
significantly higher than those in the control group, and the
difference was statistically significant (P<0.001). The findings
of Weiss et al (20) and
Luckhardt et al (21) are
consistent with ours. In their studies, the improvement rate of
cough, sputum, chest tightness, chest pain and dyspnea after
treatment with acetylcysteine combined with tetrandrine was
significantly higher than that in the control group; the FVC, FEV1
and FEV1/FVC in the treatment of silicosis with acetylcysteine
combined with tetrandrine tablets after treatment were
significantly improved compared with those before treatment in the
observation group, and the degree of improvement in the observation
group was higher than that in the control group, and the difference
was statistically significant. These results suggested that
acetylcysteine combined with tetrandrine tablets was effective in
the treatment of silicosis and could improve the clinical symptoms
and pulmonary function. According to literature, the destruction of
the structure and function of the tracheal mucosa in silicosis
patients is caused by the release of toxic substances by
neutrophils in the bronchial mucosa, while acetylcysteine can
control the inflammatory factors in patients' serum, and exert
antioxidant and antiinflammatory effects to slow down the
development of the disease (22).
Zhang et al (23) showed that
acetylcysteine reduced the reactive oxygen species in rats exposed
to silica, and also inhibited the mitochondrial apoptotic pathway,
thereby reducing the severity of pulmonary fibrosis. Tetrandrine is
a calcium antagonist that blocks the calcium channel of fiber cells
and inhibits their proliferation (24). Moreover, it can inhibit collagen
synthesis in silicosis tissue and act on cell microtubules to make
collagen form fibrous structure only outside the cells, and reduce
collagen protein in silicosis tissue and loosen or even degrade the
tubercle of patients with silicotic nodules. Tetrandrine can
inhibit various diseases such as hypertension, silicosis and
arthritis, and has a good prospect of protecting liver cells,
resisting liver fibrosis, reducing portal hypertension, inducing
tumor cell apoptosis and reversing multidrug resistance (25). The role of tetrandrine in various
signal transduction pathways such as reactive oxygen species,
enhanced autophagy flux, multidrug resistance reversal, caspase
pathway, cell cycle arrest, and calcium channel modification has
been demonstrated (26). As a
result, the patients with silicotic nodules who received
tetrandrine were effectively improved, shadow decreased and faded,
and symptoms such as chest tightness and cough were alleviated
(27).
In conclusion, acetylcysteine combined with
tetrandrine tablets on the basis of conventional therapy in
treatment of silicosis is more effective than conventional therapy
alone, which can also improve exercise tolerance, pulmonary
function and clinical symptoms such as chest tightness, chest pain,
cough, sputum production of silicosis patients, and is helpful for
clinical application.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XG and JQ led the conception and design of this
study. XG, JQ and HL were responsible for the data collection and
analysis. JQ, HL and ZX were in charge of interpreting the data and
drafting the manuscript. XG and ZX made revision from critical
perspective for important intellectual content. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Branch of Tai'an City Central Hospital (Tai'an, China). Signed
informed consents were obtained from the patients and/or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Akgün M and Ergan B: Silicosis in Turkey:
Is it an endless nightmare or is there still hope? Turk Thorac J.
19:89–93. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Brhel P, Petrovová M and Lorenzová D:
Ventilatory function in patients with silicosis or coal workers'
pneumoconiosis. Vnitr Lek. 61:1023–1027. 2015.PubMed/NCBI(In Czech).
|
|
3
|
Rimal B, Greenberg AK and Rom WN: Basic
pathogenetic mechanisms in silicosis: Current understanding. Curr
Opin Pulm Med. 11:169–173. 2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Richter K and Kietzmann T: Reactive oxygen
species and fibrosis: Further evidence of a significant liaison.
Cell Tissue Res. 365:591–605. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Peng HB, Wang RX, Deng HJ, Wang YH, Tang
JD, Cao FY and Wang JH: Protective effects of oleanolic acid on
oxidative stress and the expression of cytokines and collagen by
the AKT/NFκB pathway in silicotic rats. Mol Med Rep. 15:3121–3128.
2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Huaux F: New developments in the
understanding of immunology in silicosis. Curr Opin Allergy Clin
Immunol. 7:168–173. 2007.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Gurjar D, Gupta M, Sharma H and Pathak S:
Study to find out the efficacy of 6 minute walk test in assessing
response to medical intervention in chronic obstructive pulmonary
disease patients. IJAM. 3(3)2019.
|
|
8
|
Saglam M, Vardar-Yagli N, Savci S,
Inal-Ince D, Calik-Kutukcu E, Arikan H and Coplu L: Functional
capacity, physical activity, and quality of life in hypoxemic
patients with chronic obstructive pulmonary disease. Int J Chron
Obstruct Pulmon Dis. 10:423–428. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yeh ST, Guo HR, Su YS, Lin HJ, Hou CC,
Chen HM, Chang MC and Wang YJ: Protective effects of
nacetylcysteine treatment post acute paraquat intoxication in rats
and in human lung epithelial cells. Toxicology. 223:181–190.
2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
McLaughlin MF, Donoviel DB and Jones JA:
Novel indications for commonly used medications as radiation
protectants in spaceflight. Aerosp Med Hum Perform. 88:665–676.
2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Li FQ, Lu B, Chen WB and Yang H:
Tetrandrine loaded sustainedrelease microcapsules for lung
targeting. Yao Xue Xue Bao. 36:220–223. 2001.PubMed/NCBI(In Chinese).
|
|
12
|
Liu C, Gong X, Xiao X, Yuan X and Cai B:
Effects of tetrandrine combined with large volume whole lung lavage
on the quality of life and oxidative stress of pneumoconiosis
patients. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi.
32:219–221. 2014.PubMed/NCBI(In Chinese).
|
|
13
|
Suut S, Al-Ani Z, Allen C, Rajiah P,
Durr-E-Sabih Al-Harbi A, Al-Jahdali H and Khan AN: Pictorial essay
of radiological features of benign intrathoracic masses. Ann Thorac
Med. 10:231–242. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Reychler G, Audag N, Mestre NM and Caty C:
Assessment of validity and reliability of the 1-minute sit-to-stand
test to measure the heart rate response to exercise in healthy
children. JAMA pediatr. 173:692–693. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ringbaek T, Martinez G and Lange P: A
comparison of the assessment of quality of life with CAT, CCQ, and
SGRQ in COPD patients participating in pulmonary rehabilitation.
COPD. 9:12–15. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ora J, Calzetta L, Pezzuto G, Senis L,
Paone G, Mari A, Portalone S, Rogliani P, Puxeddu E and Saltini C:
A 6MWT index to predict O2 flow correcting exercise
induced SpO2 desaturation in ILD. Respir Med.
107(20142021)2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Huff JE, Dinger CY, Kline BW, Whitfield BL
and Hammons AS: A health view of asbestos: An annotated literature
collection. 1960-1974. Environ Health Perspect. 9:341–462.
1975.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Zhang Y, Yang F, Liu Y, Peng HB, Geng YC,
Li SF, Xu H, Zhu LY, Yang XH and Brann D: Influence of the
interaction between Ac-SDKP and Ang II on the pathogenesis and
development of silicotic fibrosis. Mol Med Rep. 17:7467–7476.
2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wang SX, Liu P, Wei MT, Chen L, Guo Y,
Wang RY, Tu ZG and Liang XC: Roles of serum clara cell protein 16
and surfactant protein D in the early diagnosis and progression of
silicosis. J Occup Environ Med. 49:834–839. 2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Weiss DJ, Chambers D, Giangreco A, Keating
A, Kotton D, Lelkes PI, Wagner DE and Prockop DJ: ATS Subcommittee
on Stem Cells and Cell Therapies. An official American Thoracic
Society workshop report: Stem cells and cell therapies in lung
biology and diseases. Ann Am Thorac Soc. 12:79–97. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Luckhardt TR, Müller-Quernheim J and
Thannickal VJ: Update in diffuse parenchymal lung disease 2011. Am
J Respir Crit Care Med. 186:24–29. 2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ning JX, Zhang LP and Cui Y: Evaluation of
clinical efficacy of tretrandrine combined with acetylcysteine
effervescent tablets in the treatment of silicosis. Zhonghua Lao
Dong Wei Sheng Zhi Ye Bing Za Zhi. 35:298–299. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
23
|
Zhang L, He YL, Li QZ, Hao XH, Zhang ZF,
Yuan JX, Bai YP, Jin YL, Liu N, Chen G, et al: Nacetylcysteine
alleviated silica induced lung fibrosis in rats by downregulation
of ROS and mitochondrial apoptosis signaling. Toxicol Mech Methods.
24:212–219. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Li C, Lu Y, Du S, Li S, Zhang Y, Liu F,
Chen Y, Weng D and Chen J: Dioscin exerts protective effects
against crystalline silica-induced pulmonary fibrosis in mice.
Theranostics. 7:4255–4275. 2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Cai XH, Wang S and Chen BA: Research
advances on the pharmacological effects of tetrandrine. Chin J Nat
Med. 9:473–480. 2011.
|
|
26
|
Bhagya N and Chandrashekar KR: Tetrandrine
- A molecule of wide bioactivity. Phytochemistry. 125:5–13.
2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Weiss DJ, Bates JH, Gilbert T, Liles WC,
Lutzko C, Rajagopal J and Prockop D: Stem cells and cell therapies
in lung biology and diseases: Conference report. Ann Am Thorac Soc.
10:S25–S44. 2013.PubMed/NCBI View Article : Google Scholar
|