Introduction
Chronic heart failure (CHF) is a chronic disease, in
which myocardial structure and function are changed due to
cardiomyopathy, inflammation, myocardial infarction and other
causes, ultimately leading to decline in ventricular pump function
(1,2). CHF occurs in the terminal stage of
various heart diseases and is a major cause of death in heart
disease patients, seriously endangering the life of patients. With
the aging of populations and improvement of life expectancy in
heart disease patients, CHF have become an important public health
concern. Some studies have manifested that the incidence rate of
CHF in the Chinese people aged ≥65 years old is as high as 10%, and
elderly CHF patients tend to be complicated with malnutrition
(3). With a half-life of about 2
days, pre-albumin (PA) is a sensitive indicator for monitoring
nutritional status, and the decrease in PA level may be correlated
with the poor prognosis of the patients with cardiovascular system
disease, without related studies on its role in evaluating the
prognosis of CHF (4-6).
N-terminal pro-B-type natriuretic peptide (NT-pro BNP) acts as a
common indicator for the diagnosis of acute and CHF and the
evaluation of their severity and has a significant correlation with
left ventricular ejection fraction (LVEF), but it is more closely
associated with age, volume load, renal function and diet habit
(7,8). The present study explored the
significance of blood PA and NT-pro BNP for disease progression and
prognosis in elderly CHF patients to accumulate data for clinical
research of CHF.
Patients and methods
Subjects
A total of 410 elderly patients aged ≥65 years
admitted to Beijing Chaoyang Hospital (Beijing, China) for CHF from
January 2011 to June 2014 were enrolled in this study. There were
194 males and 216 females with the mean age of (77.18±6.34) years.
The patients were diagnosed with CHF based on the Framingham
Criteria for Congestive Heart Failure, and their cardiac function
was classified into grades II-IV (41 cases of grade II, 146 cases
of grade III and 223 cases of grade IV) according to the New York
Heart Association (NYHA) cardiac function classification standards.
Exclusion criteria: i) Patients with malignant tumors, severe
infection or tuberculosis, severe liver or kidney disease, thyroid
disease, severe malnutrition or acute myocardial infarction, ii)
those suffering from severe dehydration, gastrointestinal
hemorrhage, shock or hypovolemia and iii) those who underwent major
surgical operations in the last 3 months.
This study was approved by the Ethics Committee of
Beijing Chaoyang Hospital. Patients who participated in this
research had complete clinical data. The signed informed consents
were obtained from the patients or the guardians.
General information
The general information of the subjects was
collected, including the basic information of age, sex, routine
blood test results, blood biochemical analysis results,
echocardiograms and hospital stay. On the second day of admission,
fasting venous blood was drawn to determine the serum PA and plasma
NT-pro BNP concentrations and routine blood test and biochemistry
indicators. The blood biochemistry indicators and PA were
determined using the automatic biochemistry analyzer (Beckman
Coulter, Inc.), and NT-pro BNP was measured using Elecsys 2010
fully automated electrochemiluminescence immunoassay analyzer
(Roche Diagnostics). Echocardiography was performed in patients
with Sonos 5500 color Doppler ultrasound system (Philips Medical
Systems B.V.) within 3 days after admission. The probe frequency is
2-4 mhz. The machine is equipped with harmonic imaging technology
(HI) and AQi technology analysis system. All the patients LVESD,
LVEDD and other indicators were measured, and the LVEF indicator
was calculated by Simpson's method.
Treatment and follow-up
All the patients received standardized treatment
based on the ‘2016 ESC Guidelines for the Diagnosis and Treatment
of Acute and Chronic Heart Failure’. After discharge, they were
followed up by telephone or outpatient visit, and the follow-up
lasted for 14-60 months with the occurrence of major adverse
cardiac events (MACE) as the end of follow-up observation. The
patients were divided into MACE group and non-MACE group according
to the occurrence of MACE that is defined as re-hospitalization for
heart failure and all-cause death.
Statistical analysis
All statistics were analyzed using SPSS 20.0 (IBM
Corp.). The measurement data conforming to the normal distribution
were expressed as (mean ± SD), and t-test/z-test was performed for
the comparisons between groups. The count data were presented as
percentage or rate, and the comparisons between groups were made
using Chi-square test. The variables with statistically significant
differences were subjected to univariate logistic analysis, and
multivariate logistic regression was used to analyze the potential
risk factors. The receiver operating characteristics (ROC) curve
analysis was used to analyze the diagnosis efficacy. P<0.05
indicates statistical significance.
Results
Baseline characteristics
The comparisons indicated statistically significant
differences in age, heart rate at admission, NYHA cardiac function
classification, left ventricular diastolic dimension (LVEDD), LVEF,
NT-pro BNP, albumin (ALB), PA, hemoglobin (Hb), hematocrit (Hct),
total cholesterol (TC), triglyceride (TG), total bilirubin (TBIL),
serum creatinine (Scr) and cystatin C (Cys C) between the two
groups (P<0.05; Table I), and
MACE group had an obviously higher level of plasma NT-pro BNP, but
a notably lower level of serum PA than non-MACE group
[(8,864.52±9,718.36) pg/ml vs. (4,165.62±6,437.28) pg/ml, and
(0.14±0.07) g/l vs. (0.19±0.05) g/l; P<0.001]. However, there
were no statistically significant differences in the sex, cardiac
troponin I, D-dimer, alanine aminotransferase, aspartate
aminotransferase, uric acid, hypersensitive C-reactive protein and
hospital stay between the two groups (P>0.05; Table I).
 | Table IComparison of baseline characteristics
between MACE and non-MACE group. |
Table I
Comparison of baseline characteristics
between MACE and non-MACE group.
| Variables | MACE group
(n=249) | Non-MACE group
(n=161) |
t/χ2/z | P-value |
|---|
| Male, n (%) | 118 (47.39) | 75 (46.58) |
χ2=1.35 | 0.764 |
| Age (years) | 77.82±6.57 | 76.39±6.18 | t=-3.36 | 0.025 |
| HR at admission
(bpm) | 87.24±21.63 | 82.76±16.52 | t=-1.94 | 0.043 |
| NYHA stage (II &
III/IV, %) | 93.02 | 71.28 |
χ2=5.27 | 0.008 |
| LVEDD (mm) | 50.54±14.62 | 45.78±12.39 | t=-2.58 | 0.021 |
| LVEF (%) | 48.15±11.96 | 52.97±11.06 | t=4.92 | 0.001 |
| NT-pro BNP
(pg/ml) |
8,864.52±9,718.36 |
4,165.62±6,437.28 | z=-3.71 | <0.001 |
| cTNI | 1.56±5.42 | 1.39±6.02 | t=-0.04 | 0.892 |
| ALB (g/l) | 35.29±4.14 | 37.83±3.39 | t=4.29 | <0.001 |
| PA (g/l) | 0.14±0.07 | 0.19±0.05 | t=5.76 | <0.001 |
| Hb (g/l) | 113.27±23.54 | 119.86±20.76 | t=3.43 | 0.019 |
| D-D
(μg/l) | 638.93±931.12 | 544.26±749.83 | t=-2.15 | 0.341 |
| Hct (%) | 34.16±6.39 | 36.57±6.62 | t=4.94 | 0.037 |
| TC (mmol/l) | 3.82±1.07 | 4.33±1.14 | t=5.13 | 0.002 |
| TG (mmol/l) | 1.09±0.53 | 1.48±0.87 | t=6.02 | <0.001 |
| TBIL
(μmol/l) | 16.46±9.82 | 13.05±7.18 | t=-3.58 | 0.035 |
| ALT (U/l) | 56.49±98.25 | 39.62±70.54 | t=-0.38 | 0.467 |
| AST (U/l) | 61.54±125.39 | 54.63±160.36 | t=-0.54 | 0.926 |
| Scr
(μmol/l) | 104.64±65.37 | 95.35±57.42 | t=-2.76 | 0.046 |
| UA
(μmol/l) | 417.81±169.26 | 398.05±150.48 | t=-1.33 | 0.317 |
| Cys C (mg/l) | 1.64±0.78 | 1.43±0.62 | t=-2.15 | 0.036 |
| hs-CRP (ng/ml) | 20.63±85.12 | 15.32±60.81 | t=-1.17 | 0.418 |
| Hospital stay
(days) | 12.68±5.34 | 11.26±3.72 | t=-1.92 | 0.072 |
Results of logistic regression
analysis
With the median as the boundary, the variables with
statistically significant differences in baseline comparisons were
classified into binary variables for univariate logistic regression
analysis. According to the analysis results, NYHA cardiac function
classification, LVEDD and NT-pro BNP had an OR value >1, and
served as risk factors for the occurrence of MACE (P<0.05;
Table II), while with the OR values
<1, LVEF, ALB, PA, Hb, Hct and TC were protective factors
against MACE (P<0.05; Table II).
In the multivariate logistic regression analysis, despite of
potential affecting factors indicated in Table III (NYHA, LVEDD, LVEF, ALB, Hb, Hct
and TC), PA and NT-pro BNP were still statistically significant for
the occurrence of MACE (P<0.05; Table III), indicating that the decrease
in PA and increase in NT-pro BNP have a strong correlation with
chronic heart dysfunction to heighten the risk of such poor
prognoses as all-cause death or re-hospitalization in elderly CHF
patients.
 | Table IIUnivariate regression analysis of
prognosis in patients with CHF. |
Table II
Univariate regression analysis of
prognosis in patients with CHF.
| Variables | OR | 95% CI | P-value |
|---|
| NYHA (%, II &
III/IV) | 1.926 | 1.174-2.985 | 0.005 |
| LVEDD (mm, >48.23
vs. ≤48.23) | 1.847 | 1.214-2.892 | 0.017 |
| LVEF (%, >51.69
vs. ≤51.69) | 0.623 | 0.357-0.931 | 0.024 |
| NT-pro BNP (pg/ml
>3,305.46 vs. ≤3,305.46) | 3.059 | 1.758-5.027 | <0.001 |
| ALB (g/l, >36.50
vs. ≤36.50) | 0.417 | 0.275-0.618 | <0.001 |
| PA (g/l >0.16 vs.
≤0.16) | 0.224 | 0.135-0.349 | <0.001 |
| Hb (g/l >118 vs.
≤118) | 0.502 | 0.259-0.649 | 0.009 |
| Hct (%, >36.32 vs.
≤36.32) | 0.475 | 0.312-0.796 | 0.007 |
| TC (mmol/l, >3.83
vs. ≤3.83) | 0.538 | 0.346-0.822 | 0.004 |
 | Table IIIMultivariate regression analysis of
prognosis in patients with CHF. |
Table III
Multivariate regression analysis of
prognosis in patients with CHF.
| Variables | OR | 95% CI | P-value |
|---|
| NYHA (%, II &
III/ IV) | 1.952 | 1.471-3.383 | 0.420 |
| LVEDD (mm, >48.23
vs. ≤48.23) | 1.548 | 1.062-2.891 | 0.062 |
| LVEF (%, >51.69
vs. ≤51.69) | 0.617 | 0.324-1.225 | 0.323 |
| NT-pro BNP (pg/ml,
>3,305.46 vs. ≤3,305.46) | 1.847 | 1.024-3.158 | 0.036 |
| ALB (g/l, >36.50
vs. ≤36.50) | 0.415 | 0.246-1.029 | 0.052 |
| PA (g/l, >0.16
vs. ≤0.16) | 0.242 | 0.137-0.406 | <0.001 |
| Hb (g/l, >118
vs. ≤118) | 0.416 | 0.198-1.132 | 0.085 |
| Hct (%, >36.32
vs. ≤36.32) | 0.625 | 0.423-1.819 | 0.327 |
| TC (mmol/l,
>3.83 vs. ≤3.83) | 0.834 | 0.697-1.238 | 0.131 |
Comparisons of heart failure severity
and prognosis between PA ≤0.16 g/l group and PA >0.16 g/l
group
With the median of PA level as the boundary, the
patients followed up were assigned into two groups, namely PA ≤0.16
g/l group (n=198) and PA >0.16 g/l group (n=212). PA ≤0.16 g/l
group consisted of 98 males and 100 females, aged (78.74±6.73)
years on average, while PA >0.16 g/l group was composed of 102
males and 110 females, with the mean age of (76.21±6.16) years. PA
≤0.16 g/l group had an older age and higher plasma NT-pro BNP level
and incidence rate of MACE than PA >0.16 g/l group, and the
differences were statistically significant (P<0.05; Table IV), and the NYHA cardiac
classification grade based on the percentages of cases of grades
II-IV in PA ≤0.16 g/l group were lower than that in PA >0.16 g/l
group, with statistically significant differences (P<0.05;
Table IV).
 | Table IVComparison of heart failure severity
and prognosis between PA ≤0.16 g/l and PA >0.16 g/l CHF
patients. |
Table IV
Comparison of heart failure severity
and prognosis between PA ≤0.16 g/l and PA >0.16 g/l CHF
patients.
| Variables | PA ≤0.16 g/l
(n=198) | PA >0.16 g/l
(n=212) |
t/χ2/z | P-value |
|---|
| Age (years) | 78.74±6.73 | 76.21±6.16 | t=-3.47 | 0.035 |
| NYHA stage (II
& III/IV, %) | 94.53 | 140.30 | χ2=
4.65 | 0.023 |
| MACE (%) | 79.14 | 37.61 |
χ2=36.14 | <0.001 |
| NT-pro BNP
(pg/ml) |
9287.46±10164.82 |
4,895.37±6,910.58 | z=5.32 | <0.001 |
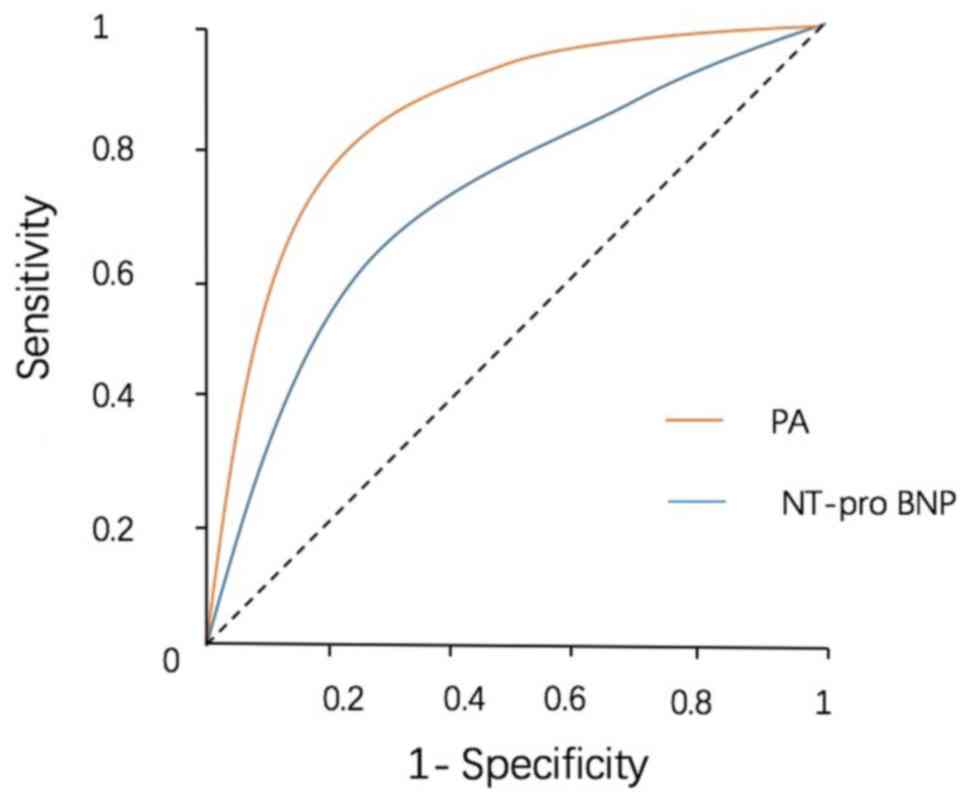
Efficacy of serum NT-pro BNP and PA in
the diagnosis of CHD patients
The sensitivity of NT-pro BNP in the diagnosis of
CHF patients is 77.65%, the specificity is 69.12%, and the
corresponding best cut-off point is 3,147.83 pg/ml; the sensitivity
of PA in the diagnosis of CHF patients is 84.32%, the specificity
is 76.57%, and the corresponding best cut-off point is 0.16 g/l;
ROCAUCNT-pro BNP>ROCAUCPA (0.854 vs. 0.784, P<0.05, Table V; Fig.
1).
 | Table VReceiver operating characteristic
(ROC) curve of PA and NT-pro BNP in predicting MACE events in
patients with CHF. |
Table V
Receiver operating characteristic
(ROC) curve of PA and NT-pro BNP in predicting MACE events in
patients with CHF.
| Variables | AUC | SE | 95% CI | Sensitivity | Specificity |
|---|
| NT-pro BNP
(pg/ml) | 0.784 | 0.056 | 0.695-0.863 | 77.65% | 69.12% |
| PA (g/l) | 0.845 | 0.031 | 0.726-0.938 | 84.32% | 76.57% |
Discussion
As a complex clinical syndrome in the severe stage
of various cardiovascular diseases, CHF has a very high incidence
rate in the elderly, and is characterized by recurrent attack,
continuous aggravation, multiple hospitalizations and high
mortality rate (2). Therefore, early
detection and treatment of CHF in the elderly patients is of great
significance for improving the survival rate of the patients. In
the present study, MACE occurred in 249 cases during follow-up,
accounting for 60.73% of the total subjects, and there were 88
cases of all-cause death, representing 21.46% of the total
subjects. Comparisons were made between MACE group and non-MACE
group, and it was found that the age, cardiac function grade based
on the NYHA classification standards and NT-pro BNP were positively
correlated with the occurrence of MACE, while ALB and PA levels
were negatively associated with the occurrence of MACE.
NT-pro BNP is a non-bioactive polypeptide that is
secreted by cardiomyocytes and enters the blood circulation through
cell stretching. Under normal conditions, NT-pro BNP is mainly
derived from atrial tissues, with a lower circulation level, while
its level will be obviously raised under such pathophysiological
conditions as altered ventricular volume, increased ventricular
wall tension and myocardial ischemia and hypoxia. Previous studies
have found that CHF patients with different grades of cardiac
function of the NYHA standards exhibit an obvious inter-group
difference in NT-pro BNP level, but NT-pro level varies
dramatically among individuals and its measurement can be affected
by multiple factors such as sex, age and body mass (7-10).
For example, diuretic and vasoactive drugs produce great influences
on the level of circulating NT-pro BNP. According to the results of
this study, the level of NT-pro BNP was obviously higher in MACE
group than that in non-MACE group, and the results of univariate
and multivariate regression analysis revealed that the increase in
NT-pro BNP level was significantly correlated with the occurrence
of MACE in elderly CHF patients, implying that NT-pro BNP level is
closely associated with the prognosis of heart failure, and that
serum NT-pro BNP level can be monitored to effectively judge the
prognosis of CHF. Although NT-pro BNP has a favorable application
value in the severity grading and prognosis evaluation of CHF,
there is no set threshold of NT-pro BNP for predicting acute onset
of CHF, which remains to be further explored.
Previous studies have demonstrated that malnutrition
is an independent predictor for adverse cardiac events in CHF
patients, and it is closely associated with CHF in the elderly as
well. ALB is commonly used as the indicator for monitoring
nutrition level, and a lower level of ALB has been found in some
studies to serve as a risk factor for the poor prognosis of CHF
patients, but with a longer half-life, ALB is not sensitive in
reflecting short-term acute malnutrition (11). PA is an indicator for the early
detection of malnutrition, and determining the concentration of
plasma PA, more sensitive than ALB, has a special diagnostic value
for understanding malnutrition, liver and kidney dysfunctions and
disease severity (12-14).
One study measured the level of serum PA in patients with renal
failure, and the results manifested that it can be used as one of
the highly sensitive indicators reflecting the nutrition status and
survival rate of renal failure patients. Moreover, serum PA level
declines in the patients with AMI and can be used for judging the
conditions and prognosis of such patients, and it is also related
to the short-term prognosis of patients with cerebral infarction
(5). Besides, the study of Lourenço
et al (6) revealed that the
concentration of serum PA can promptly reflect the nutrition status
in organisms, and it declines as cardiac function is weakened.
Additionally, the 6 month mortality rate is obviously raised in HR
patients with PA <150 mg/l. It was found in the present study
that PA ≤0.16 g/l group had higher plasma NT-pro BNP level and
incidence rate of MACE, suggesting that low PA level is positively
correlated with the severity of HR in the elderly, consistent with
the results of the above-mentioned studies. The results of the
study of Cabassi et al (15)
manifested that PA is more accurate in predicting the death risk of
the elderly CHF patients with a higher level of BNP, and it can be
used for recognizing the high-risk CHF patients who need
nutritional support. In the present study, multivariate regression
analysis was performed with the cardiac events as the dependent
variable, and it was discovered that decline in PA level is
strongly associated with the occurrence of MACE.
PA is more sensitive in evaluating early changes in
nutrition level, and it can be used for predicting heart failure
probably because worsened HF impairs liver function and raises the
secretion of inflammatory factors through the chronic inflammatory
process, thereby increasing consumption of PA and decreasing its
synthesis, and ultimately reducing PA level. Therefore, PA level is
valuable in predicting the prognosis to a certain degree.
Blood PA and NT-pro BNP levels are effective
indicators for predicting the occurrence of cardiac events in
elderly CHF patients, and they are of great clinical significance
for evaluating the severity and prognosis of the disease. However,
lack of ECG data and time recording for MACE follow-up is a
limitation of present study, time data should be supplemented in
the future research to permit time-based analysis and Cox
regression. Since CHF is a complex clinical syndrome due to the
synergy of multiple factors, and the present study has a relative
small sample size, the specific mechanisms of action of changes in
blood PA and NT-pro BNP levels in elderly CHF patients remain to be
further explored.
In conclusion, the levels of PA and NT-proBNP are
significantly related to the severity of heart failure in elderly
CHF patients. The detection of PA and NT-proBNP has guiding
significance in evaluating the prognosis of elderly patients with
CHF.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
LS, MC and XY designed the study and performed the
experiments. LS and YZ established the animal models. MC and JZ
collected the data. YG and JL analyzed the data. LS, MC and XY
prepared the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The current study was approved by the Ethics
Committee of Beijing Chaoyang Hospital (Beijing, China). Patients
who participated in this research had complete clinical data. The
signed informed consents were obtained from the patients or the
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare they have no competing
interests.
References
|
1
|
Schulz M, Griese-Mammen N, Anker SD,
Koehler F, Ihle P, Ruckes C, Schumacher PM, Trenk D, Böhm M, Laufs
U, et al: PHARM-CHF Investigators: Pharmacy-based interdisciplinary
intervention for patients with chronic heart failure: Results of
the PHARM-CHF randomized controlled trial. Eur J Heart Fail.
21:1012–1021. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mancini A, Vergani E, Bruno C, Olivieri G,
Di Segni C, Silvestrini A, Venuti A, Favuzzi A and Meucci E:
Oxidative stress as a possible mechanism underlying multi-hormonal
deficiency in chronic heart failure. Eur Rev Med Pharmacol Sci.
22:3936–3961. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
He WM, Luo YT, Shui X, Liao XX, Liu JL and
Zhuang XD: Critical appraisal of international guidelines on
chronic heart failure: Can China AGREE? Int J Cardiol. 203:111–114.
2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fan L, Chi C, Guo S, Wang Y, Cai W, Shao
X, Xu F, Pan J, Zhu Y, Shangguan X, et al: Serum pre-albumin
predicts the clinical outcome in metastatic castration-resistant
prostate cancer patients treated with abiraterone. J Cancer.
8:3448–3455. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Cubedo J, Padró T, Alonso R, Cinca J, Mata
P and Badimon L: Differential proteomic distribution of TTR
(pre-albumin) forms in serum and HDL of patients with high
cardiovascular risk. Atherosclerosis. 222:263–269. 2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lourenço P, Silva S, Friões F, Alvelos M,
Amorim M, Torres-Ramalho P, Teles MJ, Guimarães JT and Bettencourt
P: Does pre-albumin predict in-hospital mortality in heart failure?
Int J Cardiol. 166:758–760. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Whitman IR, Vittinghoff E, DeFilippi CR,
Gottdiener JS, Alonso A, Psaty BM, Heckbert SR, Hoogeveen RC,
Arking DE, Selvin E, et al: NT-pro-BNP as a mediator of the racial
difference in incident atrial fibrillation and heart failure. J Am
Heart Assoc. 8(e010868)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Letsas KP, Filippatos GS, Pappas LK, Mihas
CC, Markou V, Alexanian IP, Efremidis M, Sideris A, Maisel AS and
Kardaras F: Determinants of plasma NT-pro-BNP levels in patients
with atrial fibrillation and preserved left ventricular ejection
fraction. Clin Res Cardiol. 98:101–106. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Olsson LG, Swedberg K, Cleland JG, Spark
PA, Komajda M, Metra M, Torp-Pedersen C, Remme WJ, Scherhag A and
Poole-Wilson P: COMET Investigators. Prognostic importance of
plasma NT-pro-BNP in chronic heart failure in patients treated with
a beta-blocker: Results from the Carvedilol Or Metoprolol European
Trial (COMET) trial. Eur J Heart Fail. 9:795–801. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Pfister R, Tan D, Thekkanal J, Hellmich M
and Schneider CA: Predictors of elevated NT-pro-BNP in
cardiovascular patients without acute heart failure. Int J Cardiol.
131:277–280. 2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Gotsman I, Shauer A, Zwas DR, Tahiroglu I,
Lotan C and Keren A: Low serum albumin: A significant predictor of
reduced survival in patients with chronic heart failure. Clin
Cardiol. 42:365–372. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Player EL, Morris P, Thomas T, Chan WY,
Vyas R, Dutton J, Tang J, Alexandre L and Forbes A: Bioelectrical
impedance analysis (BIA)-derived phase angle (PA) is a practical
aid to nutritional assessment in hospital in-patients. Clin Nutr.
38:1700–1706. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fattah SA, El-Hamshary NK, Kilany YF,
Salem MN, Ismael SA, Mostafa BD and El-Dessouky YM: Prognostic and
predictive values of MELD score, platelet count and pre-albumin in
patients with compensated and decompensated liver cirrhosis with
acute variceal bleeding. J Egypt Soc Parasitol. 42:443–452.
2012.PubMed/NCBI View
Article : Google Scholar
|
|
14
|
Ruperto M, Sánchez-Muniz FJ and Barril G:
Predictors of protein-energy wasting in haemodialysis patients: A
cross-sectional study. J Hum Nutr Diet. 29:38–47. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Cabassi A, de Champlain J, Maggiore U,
Parenti E, Coghi P, Vicini V, Tedeschi S, Cremaschi E, Binno S,
Rocco R, et al: Prealbumin improves death risk prediction of BNP -
added Seattle Heart Failure Model: Results from a pilot study in
elderly chronic heart failure patients. Int J Cardiol.
168:3334–3339. 2013.PubMed/NCBI View Article : Google Scholar
|