Introduction
Primary tracheal tumor is a rare type of
respiratory-tract cancer. According to worldwide statistics, the
annual incidence rate of primary tracheal tumors is approximately
one case per million. Of all tracheal tumors, the rate of
malignancy is ~90% in adults and ~30% in children. Tracheal
malignancies account for ~0.2% of all respiratory-tract cancers and
<0.05% of all malignancies (1-4).
Treatments of common tracheal tumors include surgical resection,
radiotherapy and chemotherapy. Surgery has been considered the
treatment of choice for a long time (5). The 5-year survival rate for patients
treated with surgical resection of tracheal malignant tumors has
been reported to be 50%, compared to only 10% for non-surgically
treated patients (6). However, this
procedure has been limited due to the high risk associated with
anaesthesia and surgery, the length of the tracheal resection and
the extent of the lesion. Two large-sample studies reported a rate
of surgical interventions of only 11.6 and 6.9% (2,3).
With the development of endoscopic intervention
techniques, the treatment of tracheal tumors has also advanced. As
a result, interventional therapies including bronchoscopic stent
placement, electric snare resection, argon plasma coagulation knife
(APC), laser treatment and CO2 cryotherapy have been
applied to the treatment of tracheal tumors. In particular, the
application of bronchoscopic intervention prior to surgical
treatment has been indicated to reduce tumors, improve airway
stenosis, relieve anhelation and reduce the risk of surgery. In the
present study, the clinical data and therapeutic effects of
comprehensive interventional treatment with a flexible bronchoscope
in patients with primary tracheal tumors at the Shandong Provincial
Hospital (Jinan, China) in the past 7 years were retrospectively
analysed.
Patients and methods
Patients
Patients with primary tracheal tumors who underwent
bronchoscopic intervention between January 2011 and December 2017
at Shandong Provincial Hospital Affiliated to Shandong University
(Jinan, China) were considered for inclusion. All patients provided
written informed consent. This study was approved by the Ethics
Committee of the Shandong Provincial Hospital Affiliated to
Shandong University (Jinan, China).
All patients had been diagnosed via bronchoscopic
biopsy. Except for secondary tracheal tumors, all patients had
undergone interventional treatment with a flexible bronchoscope
(IT260 Bronchovideoscope; Olympus Corp.). Of these patients, 3 had
benign tumors, including 1 with schwannoma, 1 with glomus tumor and
1 with hamartoma. In addition, 35 patients had malignant tumors,
including 1 with squamous cell carcinoma with short-term recurrence
after surgery and 1 with adenoid cystic carcinoma that had relapsed
30 months after surgery plus radiotherapy; the remaining 33
patients presented with tracheal malignant tumors that were not
eligible for surgical resection.
Treatment methods
An individualized treatment plan was selected
according to the location, size, shape and other characteristics of
the primary tracheal tumor. A tracheal stent, high-frequency
electric trap, electric knife, laser, APC, cryotherapy and balloon
dilation were used. In cases with a more pronounced tracheal
stenosis (stenosis >50%), parallel APC/laser and cryotherapy was
performed, as the numerous lesions were difficult to completely
remove, which had resulted in breathing difficulty and challenging
tracheal stent placement. In cases with limited tumor lesions, the
basement may be ligated and the tumur may be removed using a
high-frequency electric snare and electric knife. The patient may
then be treated with APC or cryotherapy to cauterize the basal
area. In this way, 22 patients underwent bronchoscopy within 1 week
after surgery and 17 patients underwent a second intervention for
further removal of tumors present in the open airways. After
interventional treatment of patients with malignant tumors, most of
the follow-up patients underwent radiation therapy and/or
chemotherapy. Certain patients discontinued due to intolerance to
chemoradiography or by choice. All patients were followed up at the
outpatient or inpatient clinics or via telephone.
Efficacy assessment
Differences in airway stenosis and anhelation prior
to and after bronchoscopic intervention were evaluated and a
follow-up analysis of patient survival was performed. i) The
evaluation criteria of the curative effects of airway stenosis
recanalization included the following: Complete response (CR),
partial response (PR), mild response (MR) and no response (NR)
(6). Overall efficiency=(cases of CR
+ cases of PR)/total patients. ii) Airiness symptom scores
(7): Level 0: Normal; level 1:
Breathing difficulties when walking fast; level 2: Breathing
difficulties when walking at a normal speed; level 3: Unable to
walk due to anhelation during normal speed; level 4: Anhelation
after slight activity.
Statistical analysis
Statistical analysis was performed using SPSS 22.0
(IBM Corp.). Values are expressed as the mean ± standard deviation.
The efficacy prior to and after treatment was compared using an
unpaired Student's t-test. Survival curves were calculated using
the Kaplan-Meier method and compared using the log-rank test.
P<0.05 was considered to indicate statistical significance.
Results
Baseline characteristics and
circumstances of misdiagnosis
The basic clinical data of the 38 patients who
underwent comprehensive interventional therapy along with flexible
bronchoscopy are provided in Table I
(age 24-76; male:female=23:15). Clinical symptoms mainly included a
progressively worsening cough, dyspnea and wheezing. Approximately
half of the patients developed a small amount of haemoptysis, with
none developing severe haemoptysis. Due to the occurrence of
non-specific symptoms, there was a high rate of misdiagnosis, and
36.8% (14/38) of patients were misdiagnosed at the first visit as
having bronchial asthma or bronchitis (see Table II for details). The time from onset
to diagnosis was 0-60 months, with an average of 8.1±11.6 months
and a median of 4.2 months. Thoracic X-rays were performed in 8
patients, of which 2 patients (25%) displayed tracheal/superior
mediastinum lesions. Prior to treatment, all 38 patients had
tracheal tumors, as demonstrated by chest CT. Tracheal tumor sites
were more common in the middle and lower segments, accounting for
84.2% (32/38) of all tumor sites. A total of 6 patients had
tracheal tumors in the upper segment, accounting for only 15.8% of
all patients. Furthermore, 35 (92.1%) underwent bronchoscopy, which
demonstrated that >50% of the lumen was obstructed. In 20
patients (57.1%); >75% of the lumen was obstructed. Serious
obstruction of the lumen may lead to dysfunction in
ventilation.
 | Table IBaseline characteristics of the
patients (n=38). |
Table I
Baseline characteristics of the
patients (n=38).
| Characteristics | Value |
|---|
| Sex |
|
Male | 23 (60.5) |
|
Female | 15 (39.5) |
| Age (years) | 61 (24-76) |
| Smoking | 21 (55.3) |
| Symptom |
|
Difficulty
breathing | 35 (92.1) |
|
Cough with
or without expectoration | 37 (97.4) |
|
Haemoptysis | 19 (50.0) |
|
Stridor
wheezing | 8 (21.1) |
|
Hoarse
voice | 7 (18.4) |
|
Chest
pain | 2 (5.3) |
|
Feeling of a
foreign body | 1 (2.6) |
|
Dysphagia,
swallowing difficulty | 2 (5.3) |
| Tumor site |
|
Upper
section | 6 (15.8) |
|
Middle
section | 12 (31.6) |
|
Lower
section | 17 (44.7) |
|
Middle and
lower segment | 3 (7.9) |
| Tracheal stenosis
degree (%) |
|
<50 | 3 (7.9) |
|
50-74 | 15 (39.5) |
|
75-89 | 17 (44.7) |
|
90-100 | 3 (7.9) |
 | Table IICases of misdiagnosis within the
cohort. |
Table II
Cases of misdiagnosis within the
cohort.
| Disease | n (%) |
|---|
| Bronchial asthma | 4 (10.5) |
| Bronchitis | 4 (10.5) |
| Chronic obstructive
pulmonary disease | 3 (7.9) |
| Pneumonia | 1 (2.6) |
| Coronary heart
disease | 1 (2.6) |
| Pharyngitis | 1 (2.6) |
| Total | 14 (36.8) |
Comparison of the different
pathological subtypes of tracheal malignant tumors in 35
patients
Benign and malignant primary tracheal tumors are
clinically rare, with malignant tumors being more common than
benign ones in adults. A total of 3 cases of benign tumor were
identified among the 38 patients, namely peripheral glioma,
angiomyoneuroma and hamartoma. The tracheal tumors affecting the
remaining 35 patients were malignant and were most commonly
squamous cell carcinoma and adenoid cystic carcinoma, with squamous
cell carcinoma accounting for 40.0% (14/35) and adenoid cystic
carcinoma accounting for 37.1% (13/35). Overall, compared to other
types of cancer, squamous cell carcinoma exhibited a stronger
association with males and smoking. The age of onset for squamous
cell carcinoma was higher than that for adenoid cystic carcinoma
(Table III). Patients suffering
from tracheal malignant tumors underwent immunohistochemical
examination for different markers. Among them, 83.3% (15/18) were
positive for P63 and 14.3% (2/14) were positive for thyroid
transcription factor-1. Of the patients with adenoid cystic
carcinoma, 88.9% (8/9) were positive for CD117. Of the patients
with squamous cell carcinoma, adenoid cystic carcinoma,
adenocarcinoma and small-cell carcinoma, 50-70, 1-20, 20-40 and
30-40% were positive for Ki-67, respectively. Squamous cell
carcinoma had the highest proliferation index.
 | Table IIIComparison of demographics between
different pathological types of 35 patients with tracheal malignant
tumors. |
Table III
Comparison of demographics between
different pathological types of 35 patients with tracheal malignant
tumors.
| Pathological
type | Patients (n) | Mean age (years) | Sex
(male/female) | Smoking (yes/no) |
|---|
| Squamous cell
carcinoma | 14 | 62.3±8.4 | 10/4 | 10/4 |
| Adenoid cystic
carcinoma | 13 | 56.4±16.2 | 6/7 | 4/9 |
| Adenocarcinoma | 4 | 62.8±13.5 | 2/2 | 2/2 |
| Small cell
carcinoma | 2 | 69.5±4.9 | 2/0 | 2/0 |
| Adenosquamous
carcinoma | 1 | 72a | 1/0 | 1/0 |
| Plasmacytoma | 1 | 65a | 0/1 | 0/1 |
Therapeutic effect of bronchoscopy
intervention and recanalization of tracheal stenosis and
complications
The curative effects of the comprehensive
interventional treatments involving flexible bronchoscopes,
tracheal stenosis recanalization and potential complications are
presented in Table IV. Within 1
week after the operation, bronchoscopy was performed in 22
patients, of which 17 patients underwent a second interventional
treatment to further clear the tumor-obstructed airways. The
patients tolerated the course of treatment well with no serious
complications noted. The most common intra-operative complication
was haemorrhage. Altogether, 19 patients (34.5%) developed
haemorrhage in 55 separate events. A total of 12 patients had a
small amount of haemorrhage and haemostasis was achieved by washing
with norepinephrine (1:10,000). Furthermore, 7 patients had a small
amount of blood in their sputum after surgery, which stopped
spontaneously after 2-3 days without treatment. In addition, 2
patients developed hypotension during surgery. After interventional
therapy, the overall efficiency (CR+PR) of airway stenosis
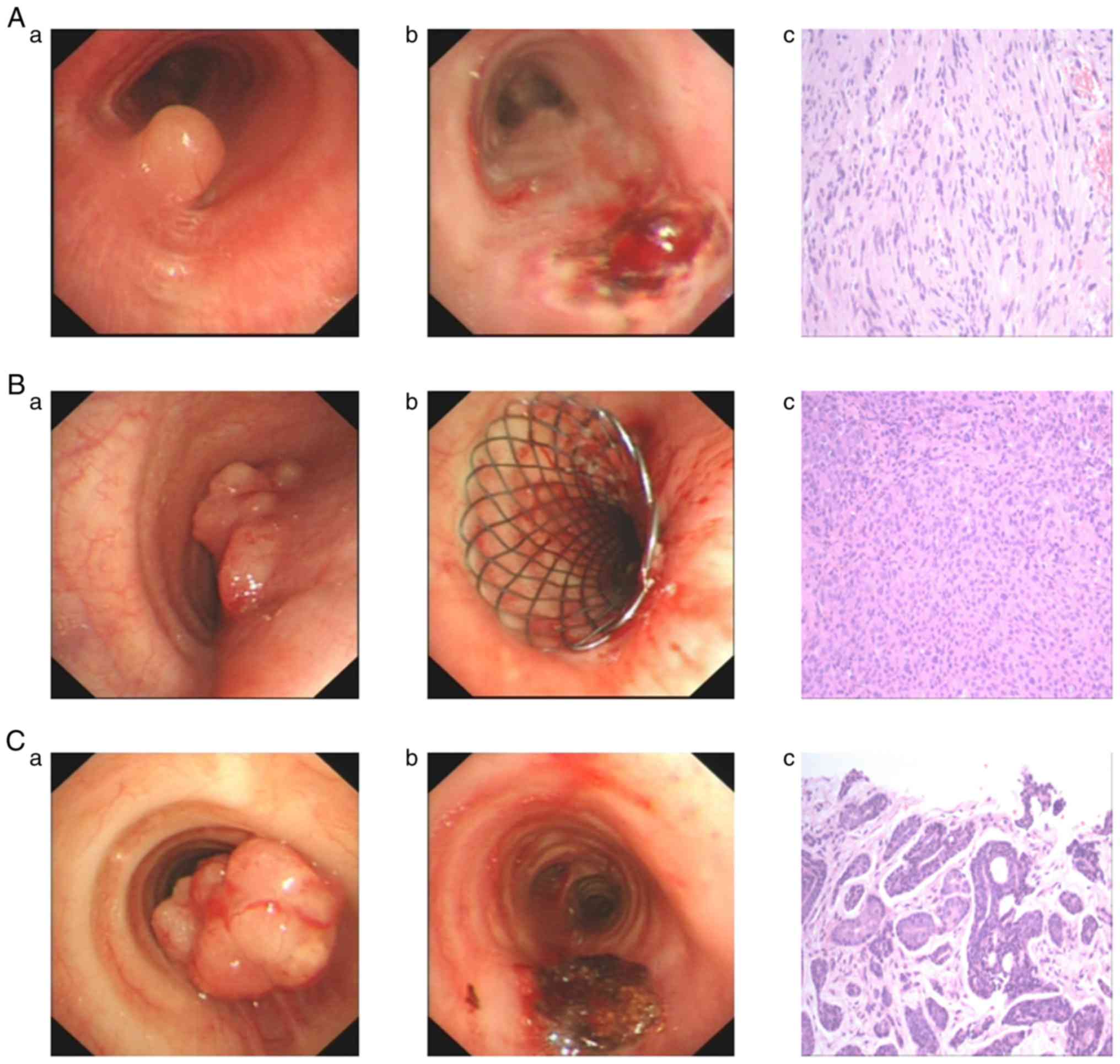
recanalization in the 38 patients was 89.5%. In Fig. 1, representative images of patients
with Schwannoma (Fig. 1A-a and
1A-b), adenocarcinoma (Fig. 1B-a and 1B-b) and adenoid cystic carcinoma (Fig. 1C-a and 1C-b) who underwent endotracheal
intervention are presented. Histopathological images of patients
with Schwannoma (Fig. 1A-c),
adenocarcinoma (Fig. 1B-c) and
adenoid cystic carcinoma (Fig. 1C-c)
are provided. The anhelation score was 3.13±1.21 prior to treatment
and 1.00±0.77 after treatment (t=15.0, P<0.001).
 | Table IVTypes of bronchoscopy intervention,
complications and therapeutic effects of recanalization of tracheal
stenosis. |
Table IV
Types of bronchoscopy intervention,
complications and therapeutic effects of recanalization of tracheal
stenosis.
| Item | Patients (n) |
|---|
| Interventional
treatment |
|
Tracheal
stent | 27 |
|
Electric
trap | 12 |
|
APC | 39 |
|
CO2
freezing | 17 |
|
High-frequency
electric knife | 12 |
|
Laser | 3 |
|
Balloon
expansion | 1 |
| Anaesthetic
method |
|
Local
anaesthesia | 47 |
|
Local
anaesthesia + intravenous general anaesthesia | 8 |
| Complications |
|
Hemorrhage | 19 |
|
Slight
bleeding | 12 |
|
Significant
bleeding (>50 ml) | 7 |
|
Hypotension | 2 |
| Tracheal stricture
recanalization |
|
CR | 9 (23.68%) |
|
PR | 25 (65.79%) |
|
MR | 4 (10.53%) |
|
NR | 0 |
Gastrin scores, treatment methods,
pathological types and follow-up results of the patients with
primary tracheal tumors
All 38 patients who received follow-ups from March
2017 to March 2018 were followed up either face-to-face or via
telephone. Out of the 35 patients (20%) with malignant tracheal
tumors, 7 of patients received radiotherapy combined with
chemotherapy and 7 patients were followed up with radiotherapy
alone (20.0%), while 11 patients were followed up with chemotherapy
alone (31.4%). Among the patients, 1 case was lost to follow-up and
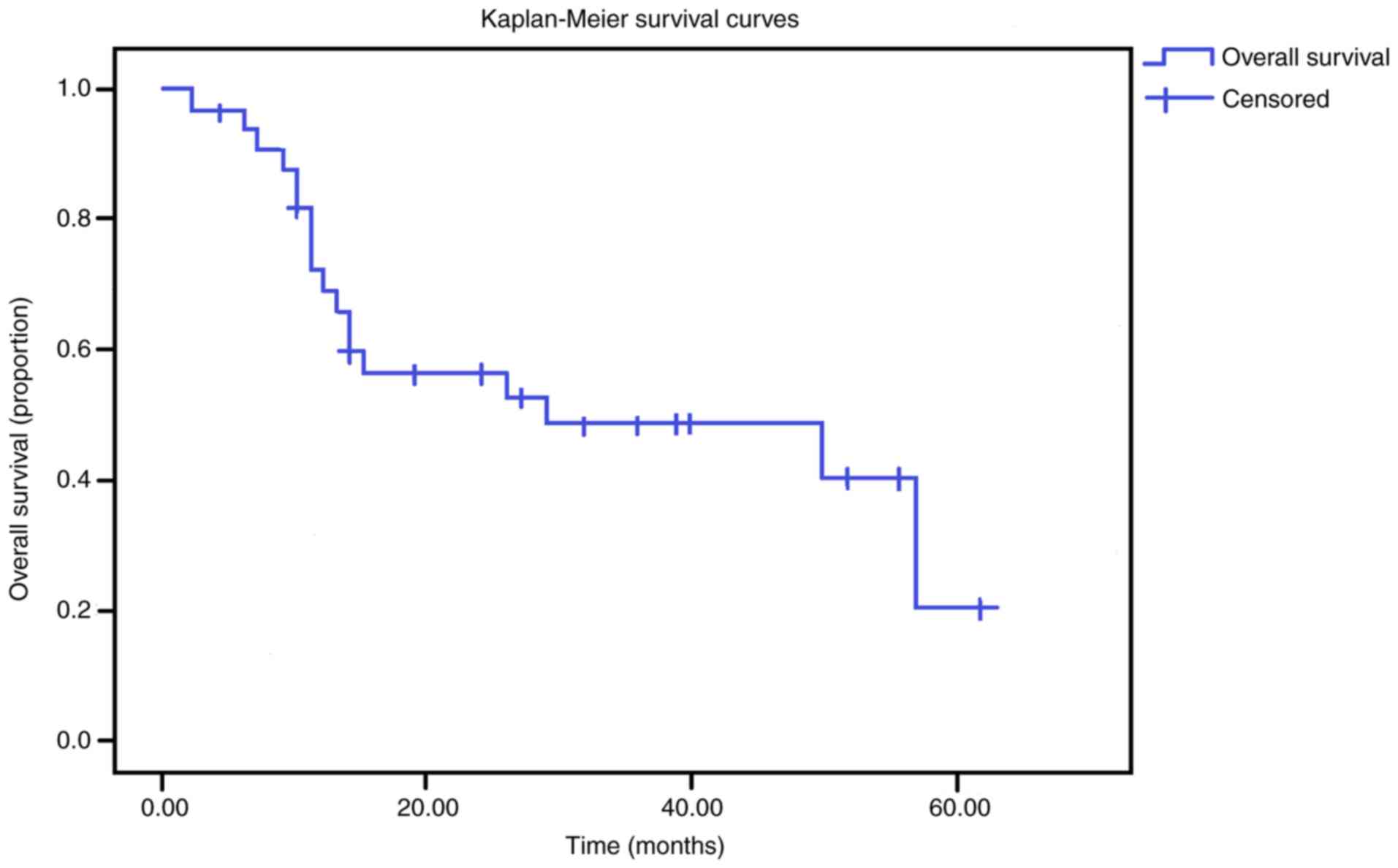
18 mortalities occurred. The overall 1-year survival rate of
patients with malignant tracheal cancer was 69.3%, the 3-year
survival rate was 48.7% and the 5-year survival rate was 20.3%. The
survival curve is presented in Fig.
2, these results demonstrated that relief of airway obstruction
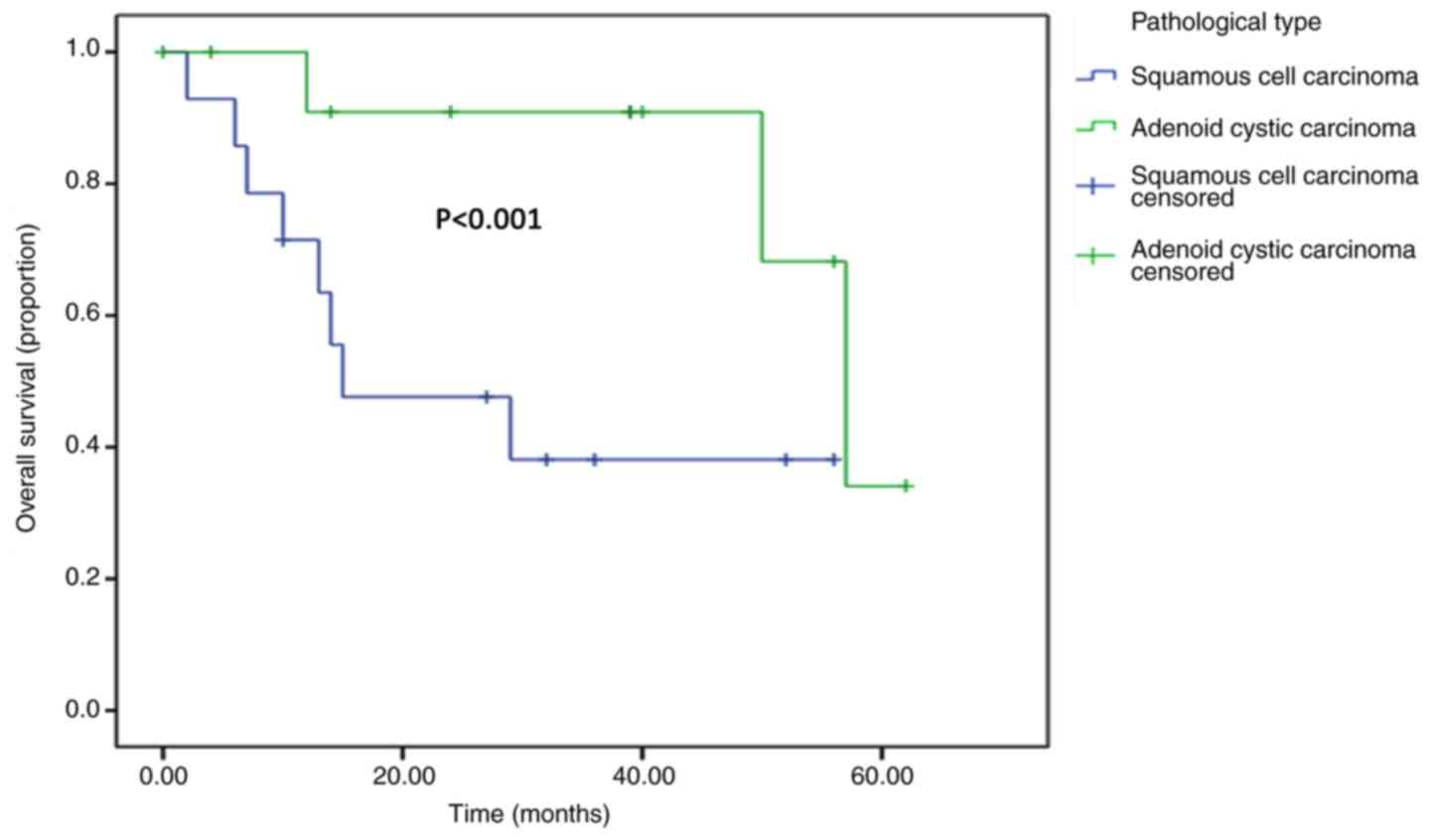
increases the quality of life. The 14 patients diagnosed with
squamous cell carcinoma had a 1-year survival rate of 71.4% and a
5-year survival rate of 38.1% and the median survival time was 15
months. Out of the 13 cases with adenoid cystic carcinoma, 1
patient was lost to follow-up and 3 patients died. The remaining
patients received follow-up for 4-62 months. The median follow-up
period was 39 months. The survival time of patients suffering from
adenoid cystic carcinoma was significantly longer than that of
patients diagnosed with squamous cell carcinoma. The survival
curves are presented in Fig. 3.
Discussion
The clinical manifestations of primary tracheal
tumor commonly include symptoms of airway obstruction, e.g. cough,
sputum, bloody sputum, dyspnea and wheezing. By the time these
clinical manifestations are observed, airway stenosis has
frequently exceeded half of the lumen (8). The low incidence of tracheal tumors,
slow tumor growth and a lack of specific clinical manifestations
appear to be the cause for patients not to seek timely medical
attention. The sensitivity of chest X-rays in distinguishing
tracheal tumors is low, ranging from only 18 to 28% (9), leading to frequent misdiagnosis. As a
result, the rate of misdiagnosis at the first visit was as high as
36.8% in the 38 patients. Diagnosis was delayed for numerous
patients by several months or even several years, with an average
of 8.1±11.6 months. An analysis of a large sample undertaken using
Shandong Provincial Hospital Affiliated to Shandong University's
internal data between January 2001 and July 2017 reported an
average delay of 2.5±8 months. While most patients were referred to
a specialist for diagnosis in a timely manner, 10% of the patients
faced delays of >6 months. The most common misdiagnosis for
these patients was bronchial asthma and bronchitis. Of all
misdiagnosed patients of the present study, 28.6% (4/14) were
misdiagnosed as having bronchial asthma. Since delayed diagnosis
and treatment may impair patient survival (10), these results suggest that clinicians
should enhance their awareness of the disease. In cases of poorly
controlled bronchial asthma and dyspnea, particularly those with
chronic coughing and wheezing, a chest CT or bronchoscopy should be
considered in order to exclude tracheal tumors (11,12).
According to the different pathological
manifestations, primary tracheal tumors may be divided into
different grades, including benign, low-grade or highly malignant.
Adult tracheal malignancies are far more common than benign tumors.
In accordance with the results of the present study, Urdaneta et
al (13) reported that squamous
cell carcinoma and adenoid cystic carcinoma are the two most common
pathological types. In this cohort, the age of the patients
suffering from squamous cell carcinoma was greater than that of
patients with adenoid cystic carcinoma and the survival time was
also shorter than that of patients with adenoid cystic carcinoma.
Adenoid cystic carcinoma has a longer median survival and higher
survival rate than squamous cell carcinoma, but distant metastasis
is more common than in squamous cell carcinoma (14). The positive rate of CD117 in patients
with adenoid cystic carcinoma was 88.9% (8/9). It has been
previously reported that positive expression of CD117 may have a
certain reference value for the diagnosis of adenoid cystic
carcinoma (15).
The first treatment of choice for primary tracheal
tumors is surgery. For patients with symptoms of severe tracheal
obstruction, pre-operative bronchoscopic intervention may
effectively improve these symptoms. Studies including that by
Chhajed et al (16) indicated
that in patients with malignant airway obstruction, prior
bronchoscopic intervention may improve lung function and may allow
lung cancer patients to undergo lung parenchymal preservation
surgeries. The length of a tracheotomy is usually limited to 6 cm
due to the lack of ideal substitute material. As a consequence, if
a tumor involving the trachea is too long and cannot be anastomosed
without tension, or it the tumor cannot be removed completely, or
by the time the tumor has metastasized and other serious
complications arise, the opportunity for surgical resection and the
associated benefits are lost (17).
Radiotherapy is an alternative treatment for this subset of
patients with inoperable malignancies. However, early radiotherapy
may not be preferred in cases with severe airway stenosis due to
the risk of local tissue swelling, further increase in airway
stenosis and even suffocation due to radiography. Recently, a case
report on a tracheal primary tumor was published, demonstrating the
efficacy of radiation therapy without chemotherapy (18). However, to avoid these risks,
pre-operative bronchoscopic interventional therapy may be
performed, which may effectively relieve airway obstruction,
particularly during tracheal stent placement.
Bronchoscopic intervention has become an important
method for the treatment of central airway stenosis. Interventional
therapy has a unique advantage over surgery in that it leads to the
rapid removal of any obstruction caused by tracheal tumors and
improves the palliative conditions (19). In the present study, different
integrated interventions were used for different clinical
manifestations in patients with tracheal tumors, including tracheal
stent, high-frequency electric knife, electric snare resection,
cryogenic therapy or APC. Laser, electrocautery and APC of
bronchial ablations use heat to solidify or evaporate tissues,
resulting in tissue damage (20).
After interventional treatment, airway obstruction and anhelation
symptoms were effectively relieved, which is consistent with the
efficacy of interventional treatments in benign and malignant
central airway stenosis reported in the literature (21,22).
Interventional treatment of tracheal tumors
involving a bronchoscope has been reported to be safe, with the
most common complications typically including a relatively small
amount of bleeding, which may be easily controlled. Compared to
rigid bronchoscopy, flexible bronchoscopy has the advantage of
causing less trauma, being more tolerable, having a lower risk and
being of lower cost. Based on the present assessment, it is
suggested that special attention must be paid to the following
considerations during the application of respiratory intervention
for primary tracheal tumors: Pre-operative assessment of the
existence of large blood vessels should be carefully performed and
adequate preparations should be made to prevent the occurrence of
life-threatening haemorrhage. One patient of the present study
suffered from bronchial artery embolization prior to surgery.
In the field of tracheal tumors, unified TNM staging
is yet to be formulated. While survival analyses have proven
useful, the results are not comparable between studies due to their
differences. A previous study reported that the overall 5-year
survival rate of tracheal malignancies was 5-15% and that the
10-year survival rate was 6-7% (23). The prognosis therefore remains poor.
Another study reported that patients with surgically treated
tracheal squamous cell carcinomas had a 5-year survival rate
ranging from 40 to 50% and a 10-year survival rate ranging from 20
to 40% (5). For this group, the
overall 1-year survival rate was 69.3%, the 3-year survival rate
was 48.7% and the 5-year survival rate was 20.3% (5). The 1-year survival rate of the squamous
cell carcinoma patients of the present study was 71.4% and the
5-year survival rate was 38.1%. In recent years, studies have
indicated improved survival rates of patients with tracheal tumors
with an early definitive diagnosis, specialist surgery and the
availability of endotracheal interventional therapy. Overall,
previous studies and the present study suggest that endotracheal
treatment is a new avenue for providing treatment and relief for
patients unsuitable for surgery (24).
In conclusion, treatment of patients with primary
tracheal tumor with bronchoscopy intervention therapy results in
effectively unobstructed airways, alleviates the symptoms of
anhelation, has broad application prospects and may be considered
safe. Bronchoscopic intervention may effectively relieve the
symptoms of the disease in patients with relevant surgical
restrictions and missed surgical opportunities, particularly in
combination with radiotherapy or chemotherapy, and may prolong
patient survival.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Natural
Science Foundation of Shandong Province of China (grant no.
ZR2016HL27).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZRH and DJL designed the experiment. ZHY, JQZ, DZL,
YYW and YMK carried out data acquisition, data analysis and
statistical analysis together. ZRH, ZHY and DJL carried out
literature search and manuscript editing. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
the Shandong Provincial Hospital Affiliated to Shandong University
(Jinan, China).
Patient consent for publication
All patients provided written informed consent.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Licht PB, Friis S and Pettersson G:
Tracheal cancer in Denmark: A nationwide study. Eur J Cardiothorac
Surg. 19:339–345. 2001.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Honings J, van Dijck JA, Verhagen AF, van
der Heijden HF and Marres HA: Incidence and treatment of tracheal
cancer: A nationwide study in the Netherlands. Ann Surg Oncol.
14:968–976. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Nouraei SM, Middleton SE, Nouraei SA, Virk
JS, George PJ, Hayward M and Sandhu GS: Management and prognosis of
primary tracheal cancer: A national analysis. Laryngoscope.
124:145–150. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Shadmehr MB, Farzanegan R, Graili P,
Javaherzadeh M, Arab M, Pejhan S, Karam MB and Abbasidezfouli A:
Primary major airway tumors; management and results. Eur J
Cardiothorac Surg. 39:749–754. 2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Behringer D, Könemann S and Hecker E:
Treatment approaches to primary tracheal cancer. Thorac Surg Clin.
24:73–76. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gaissert HA, Grillo HC, Shadmehr MB,
Wright CD, Gokhale M, Wain JC and Mathisen DJ: Longterm survival
after resection of primary adenoidcystic and squamous cell
carcinoma of the trachea and carina. Ann Thorac Surg. 78:1889–1897.
2004.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Bestall JC, Paul EA, Garrod R, Garnham R,
Jones PW and Wedzicha JA: Usefulness of the Medical Research
Council (MRC) dyspnoea scale as a measure of disability in patients
with chronic obstructive pulmonary disease. Thorax. 54:581–586.
1999.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Dahl R.Textbook of respiratory medicine,
2nd edition, Vols 1 & 2: J. F. Murray and J. A. Nadel (Eds)
Philadelphia: W. B. Saunders Company, 1994. Respiratory Medicine
90(4): 243-244, (96)90296-6, 1996.
|
|
9
|
Brand-Saberi BE and Schäfer T: Trachea:
Anatomy and physiology. Thorac Surg Clin. 24:1–5. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wu CC and Shepard JA: Tracheal and airway
neoplasms. Semin Roentgenol. 48:354–364. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Andolfi M, Vaccarili M, Crisci R and Puma
F: Managemengt of tracheal chondrosarcoma almost completely
obstructing the airway: A case report. J Cardiothorac Surg.
11(101)2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Chen YB, Jiang JH, Guo LC and Huang JA:
Primary tracheal papilloma disguised as asthma: A case report. J
Asthma. 53:1090–1093. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Urdaneta AI, Yu JB and Wilson LD:
Population based cancer registry analysis of primary tracheal
carcinoma. Am J Clin Oncol. 34:32–37. 2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rea F and Zuin A: Tracheal resection and
reconstruction for malignant disease. J Thorac Dis. 8(Suppl
2):S148–S152. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Tang Y, Liang X, Zheng M, Zhu Z, Zhu G,
Yang J and Chen Y: Expression of c-kit and Slug correlates with
invasion and metastasis of salivary adenoid cystic carcinoma. Oral
Oncol. 46:311–316. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chhajed PN, Eberhardt R, Dienemann H,
Azzola A, Brutsche MH, Tamm M and Herth FJ: Therapeutic
bronchoscopy interventions before surgical resection of lung
cancer. Ann Thorac Surg. 81:1839–1843. 2006.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wright CD: Tracheal resection. In: ESTS
Textbook of Thoracic Surgery. Kuzdzal J (ed). Medycyna Praktyczna,
Cracow, Poland, pp420-427, 2014.
|
|
18
|
Lisi R, Abate G, D'Urso P, Martinetti MT,
Siniscalchi B, Marampon F, Bulzonetti N and Tombolini V: Successful
role of adjuvant radiotherapy in a rare case of tracheal
inflammatory myofibroblastic tumor: A case report. Tumori.
105:NP1–NP3. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lin CY and Chung FT: Central airway
tumors: Interventional bronchoscopy in diagnosis and management. J
Thorac Dis. 8:E1168–E1176. 2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bolliger CT, Sutedja TG, Strausz J and
Freitag L: Therapeutic bronchoscopy with immediate effect: Laser,
electrocautery, argon plasma coagulation and stents. Eur Respir J.
27:1258–1271. 2006.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Li YQ, Li Q, Bai C, Huang Y, Zhao LJ, Yao
XP and Dong YC: Causes of benign central airway stenoses and the
efficacy of interventional treatments through flexible
bronchoscopy. Zhonghua Jie He He Hu Xi Za Zhi. 31:364–368.
2008.PubMed/NCBI(In Chinese).
|
|
22
|
Ost DE, Ernst A, Grosu HB, Lei X,
Diaz-Mendoza J, Slade M, Gildea TR, Machuzak MS, Jimenez CA, Toth
J, et al: Therapeutic bronchoscopy for malignant central airway
obstruction: Success rates and impact on dyspnea and quality of
life. Chest. 147:1282–1298. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Honings J, Gaissert HA, van der Heijden
HF, Verhagen AF, Kaanders JH and Marres HA: Clinical aspects and
treatment of primary tracheal malignancies. Acta Otolaryngol.
130:763–772. 2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sherani K, Vakil A, Dodhia C and Fein A:
Malignant tracheal tumors: A review of current diagnostic and
management strategies. Curr Opin Pulm Med. 21:322–326.
2015.PubMed/NCBI View Article : Google Scholar
|