1. Introduction
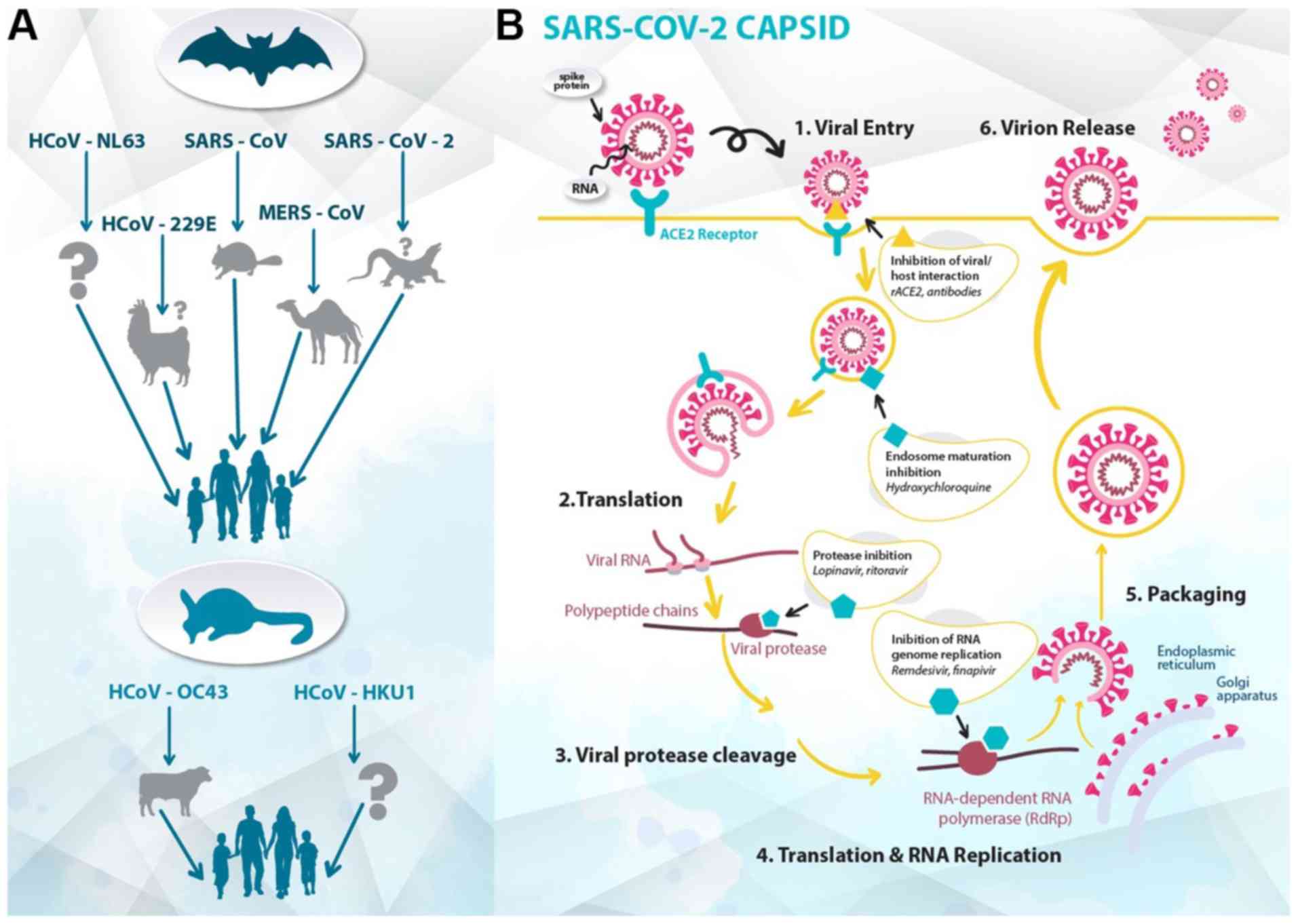
The outbreak of the 2019 novel coronavirus in Wuhan,
China, spread worldwide, becoming a pandemic in the beginning of
2020(1). The World Health
Organization (WHO) announced the name of the disease to be
coronavirus disease-19 (COVID-19), and the Coronaviridae Study
Group of the International Committee on Taxonomy of Viruses
classified its etiological agent as severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2) (Fig. 1) (2).
This respiratory pathogen belongs to the viral family
Coronaviridae, which was first identified in the mid-1960s
(3,4). Mutation and adaptation have driven the
co-evolution of coronaviruses and their hosts, including humans,
for thousands of years (5).
Recently, in 2002-2003, the outbreak of severe acute respiratory
syndrome coronavirus (SARS-CoV) increased the awareness of the
fatal risk and medical importance of virulent coronavirus strains
(6). In 2012, a novel zoonotic
coronavirus related to SARS was identified in the Middle East,
known as Middle East respiratory syndrome coronavirus (MERS-CoV),
which had a mortality rate of 36% (7). Phylogenetic analysis revealed that
SARS-CoV-2 is quite distant from SARS-CoV (~79%) and MERS-CoV
(~50%) (8). Compared with the latter
two strains, SARS-CoV-2 has a lower case-fatality rate; however, it
spreads more efficiently (9). In
response to the emergence of the pandemic, a third of the global
population was set on lockdown, and the authorities implemented
measures to slow the spread of the infection, from mandatory
geographic quarantines to non-mandatory recommendations. At
present, as there is neither prophylactic nor therapeutic treatment
for COVID-19, the world has accelerated research on treatments and
vaccines for this threat (10). Due
to the urgency of the situation, a number of already approved and
marketed drugs are being tested for repurposing, conforming to a
recent strategic innovation in medicinal chemistry and drug
discovery (11).
2. Currently available drugs against
SARS-CoV-2
Antimalarial regimen: Chloroquine and
hydroxychloroquine (Fig 2)
Chloroquine and its derivative hydroxychloroquine
have previously been used as clinical treatments in various
diseases (12-14).
Chloroquine hydrochloride and phosphate, and its derivative,
hydroxychloroquine sulfate, have been commercialized for the
prophylaxis and treatment of malaria, chronic Q-fever and
autoimmune diseases (15). Both
chloroquine and hydroxychloroquine are available as racemates,
which may exhibit stereoselective metabolism and efficacy (16). Chloroquine is a 4-aminoquinoline
analogue that acts effectively as a schizonticidal drug against the
erythrocytic forms of all types of plasmodia (17). It has also been reported to have
modest results against chronic hepatitis C (12). Numerous mechanisms of action have
been suggested to clarify the activity and the side effects of
chloroquine and hydroxychloroquine, most of them implicating
lysosomal activity on a molecular level (18), autophagy and signaling pathways
(19), and/or immunomodulatory
potency, by reducing anti-inflammatory cytokines (20). This observation might lead to a new
perspective and the therapeutic consideration of lysosomotropic
agents and/or sigma receptor(s)-related drugs for the treatment of
COVID-19 (21,22).
In vitro
studies have revealed that chloroquine is highly
effective against SARS-CoV-2. In an in vitro study by
Keyaerts et al (23), it was
shown that chloroquine exhibited antiviral activity with an IC50 of
8.8 M. Wang et al (24) also
reported that the 90% maximal effective concentration value of
chloroquine against SARS-CoV-2 in Vero E6 cells was 6.90 µM, thus
being potentially clinically applicable. In addition,
hydroxychloroquine was tested in vitro by Liu et al
(25), where it was found to
efficiently inhibit SARS-CoV-2 by blocking the entry step of the
virus, as well as its post-entry stages. Until new medications are
approved, chloroquine phosphate or its derivative,
hydroxychloroquine, in combination with azithromycin and/or
antimicrobial therapy, are being adjuvantly used for patients with
COVID-19 in various countries, such as France, Greece, China and
USA (26,27). The first results on humans were
obtained from Chinese hospitals, which revealed the superiority of
chloroquine compared with the control group, as it reduced the
exacerbation of pneumonia, duration of symptoms and delayed viral
clearance (27,28). Therefore, China recommended
chloroquine for the treatment and prevention of COVID-19(14). Patients with COVID-19 pneumonia may
benefit from the anti-viral and anti-inflammatory action of
chloroquine (29).
As well as treating malaria, chloroquine and
hydroxychloroquine have been used in the past against various
rheumatic diseases, including systemic lupus erythematosus and
rheumatoid arthritis. Both drugs exhibit their antiviral action in
a short time after their administration and cause immune
modification, as they reduce the production of cytokines (14). With regards to the reduced production
of proinflammatory cytokines, these drugs mainly affect IL-1 and
IL-6, and inhibit the activation of Toll-like receptors (TLRs)
(30).
An investigation led by Professor Didier Raoult
recently released the results of a new hydroxychloroquine treatment
study on 1,061 patients in Marseille, France (26). In this cohort study, the patients
were administered a hydroxychloroquine-azithromycin (HCQ-AZ)
combination, for ≥3 days, and then were followed-up for ≥9 days.
HCQ-AZ led to a good clinical outcome within 10 days of treatment
(91.7%) and mortality was lower in patients who had received the
HCQ-AZ combination for >3 days. This study revealed that HCQ-AZ
in the early phases of mild COVID-19 could prevent exacerbation of
the infection; however, it still remains a question if it has any
effects on severe cases (26).
The optimal dosages of chloroquine and
hydroxychloroquine, as well as the required duration of
administration for the treatment of COVID-19, have not been
determined, and several clinical studies have used different dosing
regimens (31-33).
The ongoing PATCH Trial (34)
(randomized study with 400 participants) aims to compare different
dosage forms of hydroxychloroquine in terms of their effectiveness
against COVID-19. However, for patients with renal or hepatic
impairment, there are no specific dosage recommendations, except
for the advice ‘use with caution’. Treatment with chloroquine can
lead to severe adverse effects and overdosing can lead to pulmonary
edema and circulatory collapse, which are even more severe in the
elderly, thus dose reduction is recommended (35).
Particular care is required in the use of
chloroquine phosphate, hydroxychloroquine and azithromycin, due to
their cardiotoxicity and QT prolongation (35). A multinational cohort study conducted
by Lane et al (36) indicated
that when azithromycin was added to hydroxychloroquine, patients
exhibited increased risk of 30-day cardiovascular mortality, chest
pain and heart failure. Therefore, due to the potentially
synergistic effects of HCQ-AZ on QT length, caution should be
taken. Patients with chronic diseases, including kidney failure,
liver disease, epilepsy and myasthenia gravis, or patients on
medications that include active substances incompatible with these
drugs, will require strict monitoring because they are likely to
cause serious arrhythmias. Other risk factors that can cause
arrhythmias (e.g. torsades de pointes) include hypomagnesaemia,
hypokalemia, bradycardia, heart failure, advanced age and QT
>450-500 msec. In addition, chronic treatment or high doses of
chloroquine and hydroxychloroquine may lead to damage to the
retina. It is also important that checks for lack of the G6PD
enzyme are conducted, as lack of this enzyme is associated with the
toxicity of these drugs, mainly leading to retinopathy (37).
Recently, a multinational worldwide study conducted
on patients hospitalized with COVID-19 revealed that the use of
hydroxychloroquine or chloroquine (in combination with or without a
macrolide) was associated with no evidence of benefit, but instead
was associated with an increased risk of ventricular arrhythmias
and a greater hazard for in-hospital mortality (38). However, the article was retracted as
several concerns were raised with regards to the validity of the
patients' data. Currently, there is no effective and safe
chloroquine dosage treatments for COVID-19. Karalis et al
(39) used simulation techniques for
optimization of dosage regimens and suggested specific
recommendations to healthcare specialists.
Targeting cardioprotective
derivatives: Colchicine
COVID-19 has various cardiovascular implications, in
particular : i) Patients with COVID-19 and pre-existing
cardiovascular disease exhibit a high risk of severe disease and
death; ii) COVID-19 has multiple direct and indirect cardiovascular
complications; and iii) currently used therapies against COVID-19
may have cardiovascular side effects. For all these reasons,
colchicine has been proposed to be added to the therapeutic regimen
against SARS-CoV-2(40). This drug
has been used for several years against diseases such as gout,
Mediterranean fever and pericarditis, and in addition to its other
properties, it has exhibited anti-inflammatory action (41). COLCORONA (42) is a multi-center, randomized,
double-blind trial with 6,000 participants that is currently in
progress, which aims to investigate whether short-term treatment
with colchicine may reduce mortality and lung complications in
patients with COVID-19. Moreover, GRECCO-19(41) is a smaller randomized clinical trial,
with an estimated 180 participants, which was launched in Greece
with the aim of identifying the role of colchicine in patients with
COVID-19 and determining whether it has an effect on the clinical
course of COVID-19 by reducing myocardial necrosis and pneumonia
(41).
Targeting angiotensin-converting
enzyme 2 (ACE2) (Fig 3)
The entry of SARS-CoV-2 into cells is associated
with the binding of the viral spike S protein with ACE2(43). A defined receptor-binding domain in
the aforementioned spike protein specifically recognizes its host
receptor on ACE2. Both coronavirus strains, SARS-CoV and
SARS-CoV-2, share a high sequence identity in spike S protein
(~76%) (44). This similarity of
receptor recognition may be a major factor associated with host
range and cross-species mutations, and with the emergence of
coronavirus infections (45). ACE2
is a zinc metalloproteinase and is part of the renin-angiotensin
system (RAS), which maintains cardiovascular homeostasis and
regulates blood pressure through electrolyte balance (46). ACE2 hydrolyzes the carboxy-terminal
leucine from angiotensin I (decapeptide) to produce the nonapeptide
angiotensin-(1-9).
ACE2 also converts angiotensin II (octapeptide) to
angiotensin-(1-7),
which induces blood vessel relaxation, and anti-proliferative and
anti-oxidative stress activities. Regarding coronavirus infections,
ACE2 mediates S protein-driven host cell entry (47,48).
Moreover, the viral spike S protein has been suggested to
downregulate ACE2 expression in host cells, thus leading to severe
lung injury and acute lung failure (49). The formation of the S protein-ACE2
complex has also been reported to lead to a partial decrease or
total loss of the enzymatic ACE2 function in these cells, thus
increasing the tissue concentration of proinflammatory angiotensin
II. This is affected by decreasing its degradation and reducing the
concentration of angiotensin-(1-7),
which is its physiological antagonist. High levels of angiotensin
II in the lung interstitium can promote apoptosis, thus initiating
an inflammatory process and resulting in the release of
proinflammatory cytokines, which may eventually lead to acute
respiratory distress syndrome (ARDS) (50).
The therapeutic approaches (51) against ACE2-mediated COVID-19 may
involve: i) Vaccine production based on the spike S protein
(52), ii) inhibition of virus and
host cell fusion via transmembrane protease serine 2 (TMPRSS2)
(53,54) and iii) blocking ACE2 receptor
(55,56).
Another valuable regulating factor of the RAS with
regards to COVID-19 are angiotensin II receptor blockers (ARBs),
previously described as angiotensin II type 1 (AT1) receptor
antagonists. Initially, it was hypothesized that patients treated
with ARBs or ACE inhibitors would be at a higher risk of new
coronavirus infection (57,58). This is due to the fact that
expression of ACE2, which is the enzyme that SARS-CoV-2 binds to,
is increased in patients treated with ARBs or ACE inhibitors
(57). ARBs directly protect the
endothelial barrier integrity of the lungs and indirectly
upregulate ACE2, reducing inflammation, organ fibrosis and
endothelial injury (56). Among
these blockers, losartan has been suggested to be a drug candidate
as it can strongly bind to AT1(59).
Notably, Zhang et al (60)
revealed that hospitalized patients with COVID-19 and hypertension,
when treated with ACE inhibitors or ARBs, exhibited a lower risk of
all-cause mortality compared with non-users. According to Rothlin
et al (50), out of all of
the ARBs available, telmisartan may have best pharmacological
properties to be evaluated for COVID-19.
It has also been reported that statins upregulate
ACE2 via epigenetic modifications and interfere with its signaling.
Castiglione et al (61)
hypothesized that adjuvant treatment or continuation of already
existing statin therapy could improve the clinical course of
patients with COVID-19. This finding may be due to their
immunomodulatory action or by the prevention of cardiovascular
damage (62). Alongside their
lipid-lowering activity, statins may reduce inflammation and
oxidative stress, thus contributing to their beneficial action on
cardiovascular diseases. In addition, statins intervene in the
immune response at different levels, including immune cell adhesion
and migration, and cytokine production (61). Statins also restore the vascular
redox balance by reducing reactive oxygen species, and ameliorating
nitric oxide bioavailability, endothelial function and integrity
(61). Statins, alongside ARBs, have
been reported to be effective in targeting the host response and
preventing endothelial barrier damage in patients infected with the
Ebola virus during the recent Ebola outbreak in West Africa
(63). These findings propose a
research direction against the SARS-CoV-2 virus (64).
Targeting antivirals Remdesivir
(Fig. 4)
Experimental nucleosides and approved nucleoside
analogues have been used against SARS-CoV-2(65). Remdesivir (GS-5734) is a
monophosphoramidate analogue of adenosine with potency against
Ebola virus (66). The
1'-cyano-substituted adenine ribose analogues have exhibited
significant activity against RNA viruses (67). In addition, C-nucleosides are
more stable than the natural and synthetic N-nucleoside
congeners, which are vulnerable to enzymatic and acid-catalyzed
hydrolysis of the nucleosidic bond (68). GS-5734 has to be anabolized
intracellularly to the active triphosphate metabolite, which acts
as a chain terminator of viral RNA-dependent RNA-polymerases. The
parent nucleoside is modified by a monophosphate prodrug moiety of
the 2-ethylbutyl L-alaninate and enhances the intracellular
triphosphate metabolite concentrations, bypassing the rate-limiting
first phosphorylation kinetics (69).
Remdesivir has a broad-spectrum of antiviral
activity against several emerging viral pathogens, including Ebola,
Marburg, MERS and SARS. In vitro testing conducted by Gilead
Sciences, Inc. demonstrated that remdesivir may be active against
the SARS-CoV-2 virus. Currently, the safety and efficacy of
remdesivir for the treatment of COVID-19 are being evaluated in
numerous ongoing phase III clinical trials (70). However, although several antiviral
drugs are being tested against SARS-CoV-2 in vitro, no drugs
are currently available with proven effectiveness in patients with
severe COVID-19 infection (71).
A cohort study by Grein et al (72) on hospitalized patients with severe
COVID-19 who were treated with compassionate use of remdesivir
revealed that improvement was observed in 68% of patients in the
respiratory support category (ambient air, non-invasive oxygen
support, invasive mechanical ventilation and extracorporeal
membrane oxygenation). In another randomized, double-blind,
multicenter trial, the Adaptive COVID-19 Treatment Trial (ACTT)
(73), the antiviral drug remdesivir
was compared with a placebo in hospitalized patients with severe
COVID-19 symptoms. At present, ACTT results from patients treated
with remdesivir compared with a placebo had a 31% faster time to
recovery (median time to recovery: 11 vs. 15 days). Other clinical
trials are under way to assess the safety and efficacy of
remdesivir (74,75).
Gilead Sciences, Inc. has initiated two randomized,
open-label, multi-center phase III clinical trials for remdesivir,
the SIMPLE trials (74,75), in countries with a high prevalence of
COVID-19. The first aims to evaluate the safety and efficacy of 5-
and 10-day dosing regimens of intravenous remdesivir in
hospitalized patients with severe manifestations of COVID-19, and
the second in patients with moderate symptoms of COVID-19, compared
with standard of care. According to Gilead Sciences, Inc., in an
exploratory analysis, 10-day treatment with remdesivir achieved
similar improvement in the clinical status of patients compared
with a 5-day treatment course (70).
Favipiravir (Fig. 5)
Favipiravir (T-705) is a guanine analogue against
influenza, which was approved in Japan in 2014. T-705 inhibits the
RNA-dependent RNA polymerase of RNA viruses, such as influenza,
Ebola, yellow fever, chikungunya, norovirus and enterovirus
(76), and was recently quite
successfully tested against SARS-CoV-2(65). Favipiravir undergoes intracellular
phosphoribosylation to form the active ribofuranosyl triphosphate
metabolite (77,78).
Favipiravir has shown encouraging results in Chinese
clinical trials; in particular, it accelerated the recovery of
hospitalized patients and improved lung function. It has a broad
spectrum of activity against RNA viruses, but not against DNA
viruses (76). Cai et al
(79) compared favipiravir with
lopinavir/ritonavir for the treatment of COVID-19 in a
non-randomized clinical trial, and revealed that favipiravir had a
greater effect on viral clearance and greater improvements on chest
computed tomography scans. In addition, Chen et al (80) designed a multi-center randomized
superiority clinical trial of favipiravir versus umifenovir for the
treatment of patients with COVID-19 in Wuhan, China (77). It was revealed that favipiravir
significantly improved pyrexia and cough, but did not significantly
improve the clinical recovery rate at day 7. Currently, this drug
is not available in Europe; however, there are ongoing randomized
clinical trials (81-84),
which aim to evaluate the role of favipiravir in patients with
COVID-19; further results are expected after May, 2020.
Ribavirin
Ribavirin is a purine nucleoside analogue that is
used to treat numerous viruses, such as respiratory syncytial virus
and hepatitis C (85). Ribavirin
prevents the replication of viruses by inhibiting the cellular
enzyme inosine monophosphate dehydrogenase (86). Additionally, the 5'-triphosphate
metabolite of ribavirin inhibits viral polymerase activity.
Although ribavirin has been reported to have little
inhibitory effect on coronavirus replication, it decreased the
production of proinflammatory cytokines, such as IL-1 and TNF-α, in
the macrophages of mice (87).
Ribavirin exhibits immunomodulatory potency as well as antiviral
activity, and has already been used against SARS-CoV and MERS-CoV
(85). Ribavirin is being tested in
clinical trials against COVID-19 and has shown promising results
when used as a triple combination with interferon (IFN)β-1b and
lopinavir-ritonavir (88).
HIV protease inhibitors: Kaletra
(lopinavir/ritonavir)
Lopinavir and ritonavir are HIV protease inhibitors
(89), which have been specifically
designed to fit a certain HIV protease dimer pocket that is not
present in coronavirus proteases. The combination of
lopinavir/ritonavir was initially thought to be a promising
combination against COVID-19, based on its mechanism of action, but
ultimately did not prove useful in combating COVID-19. Initially,
significant antiviral activity of lopinavir/ritonavir against
SARS-CoV was reported in cell cultures; however, there were
conflicting results for MERS-CoV (90). A randomized, controlled, open-label
trial by Cao et al (91)
revealed that the combination of lopinavir/ritonavir in
hospitalized adult patients with severe COVID-19 had no benefit
compared with the control group. No significant effect was detected
on primary outcome and time to clinical improvement (HR, 1.31); in
addition, mortality at 28 days was similar in the
lopinavir/ritonavir group compared with the standard-care group
(19.2 vs. 25.0%) (91).
Another ongoing multicenter randomized clinical
trial (currently in phase II; estimated completion: May, 2020) aims
to compare the lopinavir/ritonavir combination with
hydroxychloroquine in patients with mild COVID-19, and will
investigate whether these treatments reduce the viral load from the
respiratory specimens of these patients (32). More randomized clinical trials
(92,93) are still ongoing, and the results will
soon become available. Recently, the results of a multicenter
randomized phase II trial were published, which compared a 14-day
triple combination of lopinavir/ritonavir, ribavirin and IFNβ-1b
with lopinavir-ritonavir alone, for the treatment of hospitalized
patients with mild to moderate COVID-19(94). The results revealed that early triple
antiviral combination improved the symptoms of patients compared
with lopinavir/ritonavir alone; it also reduced the duration of
hospitalization (91). Another
possible treatment includes homoharringtonine, which has been
reported to be active against herpes viruses, coronaviruses and
rhabdoviruses (95). An in
vitro study reported that homoharringtonine inhibited
SARS-CoV-2 (half maximal effective concentration, 2.10 µM);
therefore, it could serve as a potential agent to be used in
clinical trials for COVID-19(96).
The combinational therapies of the aforementioned drugs may
decrease the effective concentration of the antivirals below
therapeutic plasma concentrations and provide better clinical
benefits (96).
Targeting proinflammatory
hypercytokinemia: Tocilizumab and leronlimab
Increased death rates have been noted in patients
with certain risk factors, due to an overwhelming reaction of the
immune system to the virus, causing hypercytokinemia (termed
cytokine storm), i.e. cytokine-release syndrome (CRS) and
macrophage activation syndrome (MAS), which can result in ARDS
(97). CRS has been seen in response
to coronaviruses, including SARS and MERS, with a high expression
of IL-6. Several research reports have demonstrated that some
proinflammatory cytokines are increased in the plasma of patients
with COVID-19 (96,97). Therefore, it was suggested that
cytokine-targeted biological therapies may improve outcomes in CRS
or MAS (97).
Therapies that are being investigated for the
treatment of patients with COVID-19 with severe respiratory
distress, symptom exacerbation and hyperinflammatory syndrome
include monoclonal antibodies, such as tocilizumab (IL-6
antagonist), leronlimab (C-C chemokine receptor type 5 inhibitor)
and Janus kinase inhibitors (98,99). The
CORIMUNO-19 clinical trial platform was designed and developed
quickly to evaluate the efficacy and safety of various immune
system regulators, as well as other treatments in adult patients
with severe COVID-19 infection (100). The primary outcome was the need for
ventilation or death at day 14; the results revealed that a
significantly lower proportion of patients in the tocilizumab arm
reached the primary outcome (101).
IL-6 is a cytokine that is thought to increase even
further the inflammation in COVID-19, thus leading to the
production of more cytokines, macrophages and cytotoxic lymphocytes
that increase lung inflammation. Increased IL-6 levels have been
reported to be related to ARDS (102). Tocilizumab, an anti-IL-6 receptor
(IL-6R) biological therapy, has been approved for the treatment of
CRS and is also used to treat patients with MAS. A small clinical
trial from China exhibited good efficacy in patients with COVID-19
treated with tocilizumab (103).
Phase II trials (104,105) have shown that tocilizumab, by
blocking IL-6R, may reduce inflammatory markers in patients with
COVID-19 and accelerate clinical improvement.
COVACTA (106) is a
phase III randomized clinical trial, which aims to evaluate
intravenous tocilizumab combined with standard of care, compared
with a placebo plus standard of care in patients with severe
COVID-19 pneumonia. Early data from a clinical trial in France has
shown encouraging results of tocilizumab in critically ill patients
with COVID-19(107). The National
Health Commission of China has also suggested the use of
tocilizumab in patients with COVID-19 with extensive bilateral lung
lesions opacity or in critically ill patients with increased IL-6
levels (102).
IFNλs
IFNλs are crucial for maintaining a balanced
antiviral response in the respiratory tract, by inducing viral
resistance to cells and helping them deal with the virus load
(108). Recombinant or pegylated
forms of IFNλ can prevent a cytokine storm and reduce viral load,
thus preventing lung tissue damage (109). IFNλ may be a promising therapy for
the treatment of patients with COVID-19, which should be tested in
clinical trials, as it may prevent severe pneumonia symptoms and
ARDS, and thus death. Lung inflammation and tissue damage are some
of the severe signs of COVID-19 infection, which arise due to
cytokine storm (110). However, it
still needs to be evaluated whether, by stimulating IFNλs or if
severe inflammation is present, they can be upregulated and thus
increase the possibility of adverse effects on humans (111).
Antiparasitics
Ivermectin, an antiparasitic agent by Merck Sharp
& Dohme, is the generic name given to a mixture of two
chemically modified avermectins containing ≥80%
22,23-dihydroavermectin B1a and <20% of the
corresponding B1b homologue. Avermectins are macrolide
antibiotics derived from the fermentation products of the
actinomycete Streptomyces avermitilis (112). Ivermectin demonstrated in
vitro inhibitory action against the replication of
SARS-CoV-2(113). Ivermectin has an
established safety profile for human use and has been approved for
the treatment of several parasitic infections (114,115).
Therefore, it is worthy of further consideration as an antiviral
agent against SARS-CoV-2. Furthermore, nitazoxanide, a US Food and
Drug Administration-approved drug with a broad spectrum of
antiparasitic and antiviral activity, has been suggested to be
included in a new protocol for the early management of COVID-19, in
combination with azithromycin (116). Nitazoxanide has already been
repurposed for the treatment of influenza-like infections and may
exhibit a synergistic effect with hydroxychloroquine. In addition,
because nitazoxanide upregulates the innate immune response in
order to prevent viral replication, it could reduce overall viral
load of SARS-CoV2(117).
3. Miscellaneous
Nicotine
Nicotine is a cholinergic agonist and an inhibitor
of proinflammatory cytokines (118). Notably, nicotine inhibits TNF, IL-1
and IL-6, which are increased in patients with COVID-19 and are
involved in the cytokine storm, leading to rapid deterioration
(118). Thus, nicotine, by acting
on the cholinergic anti-inflammatory system, has anti-inflammatory
properties that may have a protective role in patients with
COVID-19, by preventing the cytokine storm. Therefore, nicotine
administration could be considered as an add-on therapy, alongside
other medications, for the treatment of COVID-19. However, clinical
studies are required in order to confirm this hypothesis.
Vitamin D
Vitamin D deficiency is a major problem worldwide
and low serum levels of vitamin D may increase susceptibility to
respiratory tract infections. Martineau et al (119) performed a systematic review and
reported that vitamin D may protect against acute respiratory tract
infections; people with a severe vitamin D deficiency experienced
the most benefit from its administration. Vitamin D has been
reported to prevent the release of increased inflammatory cytokines
by changing the response of macrophages (120). Moreover, it has been demonstrated
that infection with COVID-19 may lead to the release of
proinflammatory cytokines, thus vitamin D may have a protective
role against this (121).
Spironolactone
Recently, there have been some concerns about the
use of spironolactone for the treatment of acne in patients with
COVID-19 a small study from 2005 reported that macrophages taken
from 10 patients with heart failure, who had been on spironolactone
daily for a month, had increased ACE2 activity (122). However, spironolactone may have a
protective action, as SARS-CoV-2 requires androgens to infect cells
(123). In general, the entry of
coronaviruses into host cells relies on binding of their viral
spike S proteins to cellular receptors, and on S protein priming by
host cell proteases. SARS-CoV-2 uses the receptor ACE2 for entry
and the serine protease TMPRSS2 for S protein priming (53). Therefore, spironolactone, being an
androgen blocker, may have a protective role against the virus, as
well as having some lung and heart benefits (122). The lack of androgens could be a
possible explanation for the rare cases of mortality among children
with COVID-19, and the high number of male COVID-19-related
fatalities in comparison to female fatalities (124). An ongoing randomized clinical trial
aims to evaluate the role of spironolactone in COVID-19-induced
ARDS (125).
4. Immunization
Vaccines
As of May, 2020, there is no approved vaccine
against COVID-19, but several are being tested in clinical trials
(52). As well as research into
vaccines against SARS-CoV-2, there have been some reports that
Bacillus Calmette-Guérin (BCG), a vaccine against tuberculosis, may
have a protective role against viral infections. Specifically, this
vaccine affects the release of proinflammatory cytokines, which
have a significant role in fighting viral infections (126). An epidemiological analysis revealed
that countries with a BCG vaccination policy, such as Japan, had
lower mortality rates compared with Italy, which does not have a
BCG vaccination policy (127). BCG
vaccination has also been shown to offer protection against viral
infections and sepsis, by offering bystander immunity (128); therefore, it might have a positive
impact against COVID-19. The BRACE and BADAS randomized trials,
which are still recruiting patients, aim to determine whether the
BCG vaccine reduces the incidence and severity of COVID-19
(129,130).
It has also been suggested that the Measles Mumps
Rubella vaccine may provide a protective role against COVID-19, as
it increases the ability of the immune system to fight infection
(131). Moreover, there are some
structural similarities between measles and COVID-19, which may
cause cross-reactivity and thus protection against infection
(131). However, for both vaccines,
randomized clinical trials are essential in order to evaluate their
role against SARS-CoV-2. There are currently several potent
vaccines against COVID-19, which are being tested, some of which
have already entered phase I.
Passive immunization
Current data have suggested that collected IgM and
IgG antibodies from patients who have recovered from COVID-19
infection might be a therapeutic option for SARS-CoV-2, as they
increase neutralizing antibodies (132). Until vaccines are discovered,
passive immunization could be an alternative treatment strategy,
particularly for high-risk groups, such as the elderly or patients
with cancer (132). Keith et
al (133) suggested the use of
therapeutic plasma exchange (TPE) as a possible treatment for
COVID-19 early in the clinical course, before patients proceed to
septic shock or multiple organ failure. Plasma obtained from
convalescent donors could be a possible therapeutic option against
viral infections, an approach that has also been tried in the past
(134). However, Honore et
al (135) expressed serious
doubts over the use of TPE, as it poses a risk in altering the host
immune response. Notably, TPE may aggravate immunoparalysis, as it
can remove protective antibodies from the patients and dilute the
adaptive response to infection (135). Thus, the safety, efficacy and
associated risks of TPE should be tested in randomized clinical
trials.
5. Conclusions
In conclusion, the treatment regimens used to treat
COVID-19, based on recent protocols, consist of known drugs that
act against other diseases. The urgent need to treat this deadly
pandemic requires the use of known drugs, at least until novel
drugs and vaccines with specific/selective action against the virus
are discovered. Four randomized trials have already been launched
internationally in order to identify effective drugs, the first one
for remdesivir (ACTT), the second and third for lopinavir/ritonavir
[CATCO (136) and REMAP-CAP
(137)] and the fourth for
remdesivir and lopinavir/ritonavir, with or without IFNβ-1α and
hydroxychloroquine [DisCoVeRy (138)]. The European Medicines Agency is in
contact with those responsible for the development of twelve
possible vaccines against COVID-19, and two vaccines have already
been introduced in phase I clinical trials. Vaccine development
schedules are difficult to predict, but it is estimated that it
will take at least one year for a vaccine to be approved and be
available in sufficient quantities in order to be widely used.
Acknowledgements
The authors would like to thank Ms. Mirto Altani, a
graphic designer, for generating Figs.
1, 3, 4 and 5.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
SK and IPP were involved in data reviewing and
writing. SK and IPP have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Authors' information
Miss Sofia Konstantinidou is an Onassis Foundation
Scholar.
References
|
1
|
Anastassopoulou C, Russo L, Tsakris A and
Siettos C: Data-based analysis, modelling and forecasting of the
COVID-19 outbreak. PLoS One. 15(e0230405)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Coronaviridae Study Group of the
International Committee on Taxonomy of Viruses. The species Severe
acute respiratory syndrome-related coronavirus: Classifying
2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 5:536–544. 2020.
View Article : Google Scholar
|
|
3
|
Almeida JD and Tyrrell DAJ: The morphology
of three previously uncharacterized human respiratory viruses that
grow in organ culture. J Gen Virol. 1:175–178. 1967.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Docea AO, Tsatsakis A, Albulescu D,
Cristea O, Zlatian O, Vinceti M, Moschos SA, Tsoukalas D, Goumenou
M, Drakoulis N, et al: A new threat from an old enemy: Re emergence
of coronavirus (Review). Int J Mol Med. 45:1631–1643.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ye ZW, Yuan S, Yuen KS, Fung SY, Chan CP
and Jin DY: Zoonotic origins of human coronaviruses. Int J Biol
Sci. 16:1686–1697. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ksiazek TG, Erdman D, Goldsmith CS, Zaki
SR, Peret T, Emery S, Tong S, Urbani C, Comer JA, Lim W, et al:
SARS Working Group: A novel coronavirus associated with severe
acute respiratory syndrome. N Engl J Med. 348:1953–1966.
2003.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Fehr AR, Channappanavar R and Perlman S:
Middle East respiratory syndrome (MERS): Emergence of a pathogenic
human Coronavirus. Annu Rev Med. 68:387–399. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H,
Wang W, Song H, Huang B, Zhu N, et al: Genomic characterisation and
epidemiology of 2019 novel coronavirus: Implications for virus
origins and receptor binding. Lancet. 395:565–574. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Gates B: Responding to Covid-19 - A
Once-in-a-Century Pandemic? N Engl J Med. 382:1677–1679.
2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Gates B: Innovation for Pandemics. N Engl
J Med. 378:2057–2060. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wu G, Zhao T, Kang D, Zhang J, Song Y,
Namasivayam V, Kongsted J, Pannecouque C, De Clercq E, Poongavanam
V, et al: Overview of recent strategic advances in medicinal
chemistry. J Med Chem. 62:9375–9414. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Touret F and de Lamballerie X: Of
chloroquine and COVID-19. Antiviral Res. 177(104762)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cortegiani A, Ingoglia G, Ippolito M,
Giarratano A and Einav S: A systematic review on the efficacy and
safety of chloroquine for the treatment of COVID-19. J Crit Care.
57:279–283. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Colson P, Rolain JM, Lagier JC, Brouqui P
and Raoult D: Chloroquine and hydroxychloroquine as available
weapons to fight COVID-19. Int J Antimicrob Agents.
55(105932)2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ben-Zvi I, Kivity S, Langevitz P and
Shoenfeld Y: Hydroxychloroquine: From malaria to autoimmunity. Clin
Rev Allergy Immunol. 42:145–153. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Witiak DT, Grattan DA, Heaslip RJ and
Rahwan RG: Synthesis and preliminary pharmacological evaluation of
asymmetric chloroquine analogues. J Med Chem. 24:712–717.
1981.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chloroquine- an overview | ScienceDirect
Topics. Sci Direct.
|
|
18
|
Circu M, Cardelli J, Barr MP, O'Byrne K,
Mills G and El-Osta H: Modulating lysosomal function through
lysosome membrane permeabilization or autophagy suppression
restores sensitivity to cisplatin in refractory non-small-cell lung
cancer cells. PLoS One. 12(e0184922)2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Schrezenmeier E and Dörner T: Mechanisms
of action of hydroxychloroquine and chloroquine: Implications for
rheumatology. Nat Rev Rheumatol. 16:155–166. 2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
van den Borne BEEM, Dijkmans BAC, de Rooij
HH, le Cessie S and Verweij CL: Chloroquine and hydroxychloroquine
equally affect tumor necrosis factor-α, interleukin 6, and
interferon-γ production by peripheral blood mononuclear cells. J
Rheumatol. 24:55–60. 1997.PubMed/NCBI
|
|
21
|
Gordon DE, Jang GM, Bouhaddou M, Xu J,
Obernier K, White KM, O'Meara MJ, Rezelj VV, Guo JZ, Swaney DL, et
al: A SARS-CoV-2 protein interaction map reveals targets for drug
repurposing. Nature. Apr 30. 2020.(Epub ahead of print).PubMed/NCBI View Article : Google Scholar
|
|
22
|
Encinar JA and Menendez JA: Potential
drugs targeting early innate immune evasion of SARS-coronavirus 2
via 2'-O-methylation of viral RNA. Viruses. 12(E525)2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Keyaerts E, Vijgen L, Maes P, Neyts J and
Van-Ranst M: In vitro inhibition of severe acute respiratory
syndrome coronavirus by chloroquine. Biochem Biophys Res Commun.
323:264–268. 2004.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Wang M, Cao R, Zhang L, Yang X, Liu J, Xu
M, Shi Z, Hu Z, Zhong W and Xiao G: Remdesivir and chloroquine
effectively inhibit the recently emerged novel coronavirus
(2019-nCoV) in vitro. Cell Res. 30:269–271. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Liu J, Cao R, Xu M, Wang X, Zhang H, Hu H,
Li Y, Hu Z, Zhong W and Wang M: Hydroxychloroquine, a less toxic
derivative of chloroquine, is effective in inhibiting SARS-CoV-2
infection in vitro. Cell Discov. 6(16)2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Hache Guillaume RJMGP, DJBPRDHS:
Hydroxychloroquine-Azithromycin and COVID-19 - IHU, 2020.
|
|
27
|
Rosenberg ES, Dufort EM, Udo T,
Wilberschied LA, Kumar J, Tesoriero J, Weinberg P, Kirkwood J, Muse
A, DeHovitz J, et al: Association of treatment with
hydroxychloroquine or azithromycin with in-Hospital Mortality in
patients with COVID-19 in New York State. JAMA. May 11.
2020.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print). View Article : Google Scholar
|
|
28
|
Doudier B and Courjon J:
Hydroxychloroquine and azithromycin as a treatment of COVID-19.
2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Gao J, Tian Z and Yang X: Breakthrough:
Chloroquine phosphate has shown apparent efficacy in treatment of
COVID-19 associated pneumonia in clinical studies. Biosci Trends.
14:72–73. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Zhao M: Cytokine storm and
immunomodulatory therapy in COVID-19: Role of chloroquine and
anti-IL-6 monoclonal antibodies. Int J Antimicrob Agents.
55(105982)2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Efficacy and safety of hydroxychloroquine
for treatment of COVID-19. uriClinicalTrials.govsimpleClinicalTrials.gov.
|
|
32
|
Comparison of lopinavir/ritonavir or
hydroxychloroquine in patients with mild coronavirus disease
(COVID-19). uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04307693.
Accessed March 13, 2020.
|
|
33
|
Yao X, Ye F, Zhang M, Cui C, Huang B, Niu
P, Liu X, Zhao L, Dong E, Song C, et al: In vitro antiviral
activity and projection of optimized dosing design of
hydroxychloroquine for the treatment of severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2). Clin Infect Dis. Mar 9.
2020.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print). View Article : Google Scholar
|
|
34
|
The PATCH Trial (prevention and treatment
of COVID-19 with hydroxychloroquine). uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04329923.
Accessed April 1, 2020.
|
|
35
|
Karalis V, Ismailos G and Karatza E:
Chloroquine dosage regimens in patients with COVID-19: safety risks
and optimization using simulations. Saf Sci.
129(104842)2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Lane JC, Weaver J, Kostka K, Duarte-Salles
T, Abrahao MT, Alghoul H, Alser O, Alshammari TM, Biedermann P,
Burn E, et al: Safety of hydroxychloroquine, alone and in
combination with azithromycin, in light of rapid wide-spread use
for COVID-19: a multinational, network cohort and self-controlled
case series study. medRxiv. May 31. 2020. View Article : Google Scholar : (Epub ahead of
print). View Article : Google Scholar
|
|
37
|
Al-Bari MA: Chloroquine analogues in drug
discovery: New directions of uses, mechanisms of actions and toxic
manifestations from malaria to multifarious diseases. J Antimicrob
Chemother. 70:1608–1621. 2015.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Mehra MR, Desai SS, Ruschitzka F and Patel
AN: Articles Hydroxychloroquine or chloroquine with or without a
macrolide for treatment of COVID-19: A multinational registry
analysis. Lancet. 6736:1–10. 2020. View Article : Google Scholar
|
|
39
|
Karalis V, Ismailos G and Karatza E:
Chloroquine dosage regimens in patients with COVID-19: Safety risks
and optimization using simulations. Saf Sci.
129(104842)2020.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Driggin E, Madhavan MV, Bikdeli B, Chuich
T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar
DA, Haythe J, et al: Cardiovascular considerations for patients,
health care workers, and health systems during the COVID-19
pandemic. J Am Coll Cardiol. 75:2352–2371. 2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Deftereos SG, Siasos G, Giannopoulos G,
Vrachatis DA, Angelidis C, Giotaki SG, Gargalianos P, Giamarellou
H, Gogos C, Daikos G, et al: The Greek study in the effects of
colchicine in COvid-19 complications prevention (GRECCO-19 study):
Rationale and study design. Hellenic J Cardiol. Apr 3.
2020.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print). View Article : Google Scholar
|
|
42
|
Colchicine Coronavirus SARS-CoV2 Trial
(COLCORONA). uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04322682.
Accessed March 26, 2020.
|
|
43
|
Walls AC, Park YJ, Tortorici MA, Wall A,
McGuire AT and Veesler D: Structure, function, and antigenicity of
the SARS-CoV-2 spike glycoprotein. Cell.
181(281-292.e6)2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Morse JS, Lalonde T, Xu S and Liu WR:
Learning from the past: Possible urgent prevention and treatment
options for severe acute respiratory infections caused by
2019-nCoV. ChemBioChem. 21:730–738. 2020.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Li F: Receptor recognition and
cross-species infections of SARS coronavirus. Antiviral Res.
100:246–254. 2013.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Ocaranza MP, Michea L, Chiong M, Lagos CF,
Lavandero S and Jalil JE: Recent insights and therapeutic
perspectives of angiotensin-(1-9) in the cardiovascular system.
Clin Sci (Lond). 127:549–557. 2014.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Li SR, Tang ZJ, Li ZH and Liu X: Searching
therapeutic strategy of new coronavirus pneumonia from
angiotensin-converting enzyme 2: the target of COVID-19 and
SARS-CoV. Eur J Clin Microbiol Infect Dis. 39:1021–1026.
2020.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Yan T, Xiao R and Lin G:
Angiotensin-converting enzyme 2 in severe acute respiratory
syndrome coronavirus and SARS-CoV-2: A double-edged sword? FASEB J.
34:6017–6026. 2020.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Imai Y, Kuba K and Penninger JM: The
discovery of angiotensin-converting enzyme 2 and its role in acute
lung injury in mice. Exp Physiol. 93:543–548. 2008.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Rothlin RP, Vetulli HM, Duarte M and
Pelorosso FG: Telmisartan as tentative angiotensin receptor blocker
therapeutic for COVID-19. Drug Dev Res. May 1. 2020.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print). View Article : Google Scholar
|
|
51
|
Zhang H, Penninger JM, Li Y, Zhong N and
Slutsky AS: Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2
receptor: Molecular mechanisms and potential therapeutic target.
Intensive Care Med. 46:586–590. 2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Thanh Le T, Andreadakis Z, Kumar A, Gómez
Román R, Tollefsen S, Saville M and Mayhew S: The COVID-19 vaccine
development landscape. Nat Rev Drug Discov. 19:305–306.
2020.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Hoffmann M, Kleine-Weber H, Schroeder S,
Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH,
Nitsche A, et al: SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2
and is blocked by a clinically proven protease inhibitor. Cell.
181(271-280.e8)2020.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Iwata-Yoshikawa N, Okamura T, Shimizu Y,
Hasegawa H, Takeda M and Nagata N: TMPRSS2 contributes to virus
spread and immunopathology in the airways of murine models after
coronavirus infection. J Virol. 93(93)2019.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Verdecchia P, Cavallini C, Spanevello A
and Angeli F: The pivotal link between ACE2 deficiency and
SARS-CoV-2 infection. Eur J Intern Med. 76:14–20. 2020.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Saavedra JM: Angiotensin receptor blockers
and COVID-19. Pharmacol Res. 156(104832)2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Fang L, Karakiulakis G and Roth M: Are
patients with hypertension and diabetes mellitus at increased risk
for COVID-19 infection? Lancet Respir Med. 8(e21)2020.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Diaz JH: Hypothesis:
angiotensin-converting enzyme inhibitors and angiotensin receptor
blockers may increase the risk of severe COVID-19 Running Title:
Angiotensin Receptor and COVID-19. J Travel Med.
27(taaa041)2020.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Gurwitz D: Angiotensin receptor blockers
as tentative SARS-CoV-2 therapeutics. Drug Dev Res.
1(4)2020.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Zhang P, Zhu L, Cai J, Lei F, Qin JJ, Xie
J, Liu YM, Zhao YC, Huang X, Lin L, et al: Association of inpatient
use of angiotensin converting enzyme inhibitors and angiotensin II
receptor blockers with mortality among patients with hypertension
hospitalized with COVID-19. Circ Res. 126:1671–1681.
2020.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Castiglione V, Chiriacò M, Emdin M, Taddei
S and Vergaro G: Statin therapy in COVID-19 infection. Eur Heart J
Cardiovasc Pharmacother. Apr 29. 2020.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print). View Article : Google Scholar
|
|
62
|
Pertzov B, Eliakim-Raz N, Atamna H,
Trestioreanu AZ, Yahav D and Leibovici L: Hydroxymethylglutaryl-CoA
reductase inhibitors (statins) for the treatment of sepsis in
adults - A systematic review and meta-analysis. Clin Microbiol
Infect. 25:280–289. 2019.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Fedson DS, Opal SM and Rordam OM: Hiding
in plain sight: An approach to treating patients with severe
covid-19 infection. mBio. 11(e00398-20)2020.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Journal EH, Pharmacotherapy C, East M: OUP
accepted manuscript. Eur Hear J Cardiovasc Pharmacother 2020.
|
|
65
|
Li G and De Clercq E: Therapeutic options
for the 2019 novel coronavirus (2019-nCoV). Nat Rev Drug Discov.
19:149–150. 2020.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Warren TK, Jordan R, Lo MK, Ray AS,
Mackman RL, Soloveva V, Siegel D, Perron M, Bannister R, Hui HC, et
al: Therapeutic efficacy of the small molecule GS-5734 against
Ebola virus in rhesus monkeys. Nature. 531:381–385. 2016.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Cho A, Saunders OL, Butler T, Zhang L, Xu
J, Vela JE, Feng JY, Ray AS and Kim CU: Synthesis and antiviral
activity of a series of 1'-substituted 4-aza-7,9-dideazaadenosine
C-nucleosides. Bioorg Med Chem Lett. 22:2705–2707. 2012.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Stambaský J, Hocek M and Kocovský P:
C-nucleosides: Synthetic strategies and biological applications.
Chem Rev. 109:6729–6764. 2009.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Eastman RT, Roth JS, Brimacombe KR,
Simeonov A, Shen M, Patnaik S and Hall MD: Remdesivir: A review of
its discovery and development leading to emergency use
authorization for treatment of COVID-19. ACS Cent Sci. 6:672–683.
2020.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Gilead announces results from phase 3
trial of investigational antiviral remdesivir in patients with
severe COVID-19. Gilead Sciences, Inc., 2020.
|
|
71
|
Wang Y, Zhang D, Du G, Du R, Zhao J, Jin
Y, Fu S, Gao L, Cheng Z, Lu Q, et al: Remdesivir in adults with
severe COVID-19: A randomised, double-blind, placebo-controlled,
multicentre trial. Lancet. 395:1569–1578. 2020.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Grein J, Ohmagari N, Shin D, Diaz G,
Asperges E, Castagna A, Feldt T, Green G, Green ML, Lescure FX, et
al: Compassionate Use of Remdesivir for Patients with Severe
Covid-19. N Engl J Med. 382:2327–2336. 2020.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Adaptive COVID-19 Treatment Trial (ACTT).
uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04280705.
Accessed February 21, 2020.
|
|
74
|
Study to evaluate the safety and antiviral
activity of remdesivir (GS-5734TM) in participants with moderate
coronavirus disease (COVID-19) compared to standard of care
treatment. uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04292730.
Accessed March 3, 2020.
|
|
75
|
Study to Evaluate the safety and antiviral
activity of remdesivir (GS-5734TM) in participants with severe
coronavirus disease (COVID-19). uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04292899.
Accessed March 3, 2020.
|
|
76
|
Furuta Y, Komeno T and Nakamura T:
Favipiravir (T-705), a broad spectrum inhibitor of viral RNA
polymerase. Proc Jpn Acad, Ser B, Phys Biol Sci. 93:449–463.
2017.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Furuta Y, Takahashi K, Kuno-Maekawa M,
Sangawa H, Uehara S, Kozaki K, Nomura N, Egawa H and Shiraki K:
Mechanism of action of T-705 against influenza virus. Antimicrob
Agents Chemother. 49:981–986. 2005.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Smee DF, Hurst BL, Egawa H, Takahashi K,
Kadota T and Furuta Y: Intracellular metabolism of favipiravir
(T-705) in uninfected and influenza A (H5N1) virus-infected cells.
J Antimicrob Chemother. 64:741–746. 2009.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Cai Q, Yang M, Liu D, Chen J, Shu D, Xia
J, Liao X, Gu Y, Cai Q, Yang Y, et al: Experimental treatment with
favipiravir for COVID-19: An open-label control study. Engineering
(Beijing). Mar 18. 2020.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print). View Article : Google Scholar
|
|
80
|
Chen C, Huang J, Cheng Z, Wu J, Chen S,
Yongxi Zhang Y, Chen B, Lu M, Luo Y, Zhang J, et al: Favipiravir
versus Arbidol for COVID-19: A Randomized Clinical Trial. medRxiv.
April 15. 2020.(Epub ahead or ptint). View Article : Google Scholar
|
|
81
|
Clinical study to evaluate the performance
and safety of favipiravir in COVID-19. uriClinicalTrials.govsimpleClinicalTrials.gov.
|
|
82
|
Efficacy and safety of favipiravir in
management of COVID-19. uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04349241.
Accessed April 16, 2020.
|
|
83
|
Clinical trial of favipiravir tablets
combine with chloroquine phosphate in the treatment of novel
coronavirus pneumonia. uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04319900.
Accessed March 24, 2020.
|
|
84
|
Favipiravir combined with tocilizumab in
the treatment of corona virus disease 2019. uriClinicalTrials.govsimpleClinicalTrials.gov.
|
|
85
|
Cinatl J Jr, Michaelis M, Hoever G,
Preiser W and Doerr HW: Development of antiviral therapy for severe
acute respiratory syndrome. Antiviral Res. 66:81–97.
2005.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Leyssen P, Balzarini J, De Clercq E and
Neyts J: The predominant mechanism by which ribavirin exerts its
antiviral activity in vitro against flaviviruses and
paramyxoviruses is mediated by inhibition of IMP dehydrogenase. J
Virol. 79:1943–1947. 2005.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Ning Q, Brown D, Parodo J, Cattral M,
Gorczynski R, Cole E, Fung L, Ding JW, Liu MF, Rotstein O, et al:
Ribavirin inhibits viral-induced macrophage production of TNF,
IL-1, the procoagulant fgl2 prothrombinase and preserves Th1
cytokine production but inhibits Th2 cytokine response. J Immunol.
160:3487–3493. 1998.PubMed/NCBI
|
|
88
|
Sheahan TP, Sims AC, Leist SR, Schäfer A,
Won J, Brown AJ, Montgomery SA, Hogg A, Babusis D, Clarke MO, et
al: Comparative therapeutic efficacy of remdesivir and combination
lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat
Commun. 11(222)2020.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Agbowuro AA, Huston WM, Gamble AB and
Tyndall JD: Proteases and protease inhibitors in infectious
diseases. Med Res Rev. 38:1295–1331. 2018.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Delang L and Neyts J: Medical treatment
options for COVID-19. Eur Heart J Acute Cardiovasc Care. 9:209–214.
2020.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Cao B, Wang Y, Wen D, Liu W, Wang J, Fan
G, Ruan L, Song B, Cai Y, Wei M, et al: A Trial of
Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N
Engl J Med. 382:1787–1799. 2020. View Article : Google Scholar
|
|
92
|
The efficacy of lopinavir plus ritonavir
and arbidol against novel coronavirus infection. uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04252885.
Accessed February 5, 2020.
|
|
93
|
Lopinavir/ritonavir ribavirin and IFN-beta
combination for nCoV treatment. uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04276688.
Accessed February 19, 2020.
|
|
94
|
Hung IF, Lung KC, Tso EY, Liu R, Chung TW,
Chu MY, Ng YY, Lo J, Chan J, Tam AR, et al: Triple combination of
interferon beta-1b, lopinavir-ritonavir, and ribavirin in the
treatment of patients admitted to hospital with COVID-19: An
open-label, randomised, phase 2 trial. Lancet. 395:1695–1704. 2020.
View Article : Google Scholar
|
|
95
|
Andersen PI, Krpina K, Ianevski A, Shtaida
N, Jo E, Yang J, Koit S, Tenson T, Hukkanen V, Anthonsen MW, et al:
Novel antiviral activities of obatoclax, emetine, niclosamide,
brequinar, and homoharringtonine. Viruses. 11:1–15. 2019.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Choy KT, Wong AY, Kaewpreedee P, Sia SF,
Chen D, Hui KP, Chu DK, Chan MC, Cheung PP, Huang X, et al:
Remdesivir, lopinavir, emetine, and homoharringtonine inhibit
SARS-CoV-2 replication in vitro. Antiviral Res.
178(104786)2020.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Zhang C, Wu Z, Li JW, Zhao HW and Wang GQ:
The cytokine release syndrome (CRS) of severe COVID-19 and
interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the
key to reduce the mortality. Int J Antimicrob Agents. 11:1–6.
2020.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Hennon TR, Penque MD, Abdul-Aziz R,
Alibrahim OS, McGreevy MB, Prout AJ, Schaefer BA, Ambrusko SJ,
Pastore JV, Turkovich SJ, et al: COVID-19 associated multisystem
inflammatory syndrome in children (MIS-C) guidelines; a Western New
York approach. Prog Pediatr Cardiol. 21(101232)2020. View Article : Google Scholar
|
|
99
|
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu
Y, Zhang L, Fan G, Xu J, Gu X, et al: Clinical features of patients
infected with 2019 novel coronavirus in Wuhan, China. Lancet.
395:497–506. 2020.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Vijayvargiya P, Garrigos ZE, Almeida NE,
Gurram PR, Stevens RW and Razonable RR: In reply-The ‘Perfect
Cytokine Storm’ of COVID-19. Mayo Clin Proc. May 29. 2020.
View Article : Google Scholar : (Epub ahead of
print). View Article : Google Scholar
|
|
101
|
CORIMUNO-19 - Tocilizumab Trial - TOCI
(CORIMUNO-TOCI). uriClinicalTrials.govsimpleClinicalTrials.gov.
https://www.clinicaltrials.gov/ct2/show/NCT04331808.
Accessed April 2, 2020.
|
|
102
|
Fu B, Xu X and Wei H: Why tocilizumab
could be an effective treatment for severe COVID-19? J Transl Med.
18(164)2020.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Zhang Q, Wang Y, Qi C, Shen L and Li J:
Response to ‘Comments on Zhang et al: Clinical trial analysis of
2019-nCoV therapy registered in China’. J Med Virol.
92(713)2020.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Tocilizumab treatment in patients with
COVID-19. uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04363853.
Accessed April 27, 2020.
|
|
105
|
Tocilizumab in the treatment of
coronavirus induced disease (COVID-19). uriClinicalTrials.govsimpleClinicalTrials.gov.
https://www.clinicaltrials.gov/ct2/show/NCT04335071.
Accessed April 6, 2020.
|
|
106
|
A study to evaluate the safety and
efficacy of tocilizumab in patients with severe COVID-19 pneumonia.
uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04320615.
Accessed March 25, 2020.
|
|
107
|
Genentech's arthritis drug tocilizumab
shows promise in Covid-19 trial. ClinicalTrials Arena, 2020.
https://www.clinicaltrialsarena.com/uncategorized/genentechs-arthritis-drug-tocilizumab-shows-promise-in-covid-19-trial/.
Accessed April 29, 2020.
|
|
108
|
Andreakos E and Tsiodras S: COVID-19:
Lambda interferon against viral load and hyperinflammation. EMBO
Mol Med. 12(e12465)2020.PubMed/NCBI View Article : Google Scholar
|
|
109
|
Davidson S, McCabe TM, Crotta S, Gad HH,
Hessel EM, Beinke S, Hartmann R and Wack A: IFNλ is a potent
anti-influenza therapeutic without the inflammatory side effects of
IFNα treatment. EMBO Mol Med. 8:1099–1112. 2016.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Mehta P, McAuley DF, Brown M, Sanchez E,
Tattersall RS and Manson JJ: HLH Across Speciality Collaboration,
UK. COVID-19: Consider cytokine storm syndromes and
immunosuppression. Lancet. 395:1033–1034. 2020.PubMed/NCBI View Article : Google Scholar
|
|
111
|
Prokunina-Olsson L, Alphonse N, Dickenson
RE, Durbin JE, Glenn JS, Hartmann R, Kotenko SV, Lazear HM, O'Brien
TR, Odendall C, et al: COVID-19 and emerging viral infections: The
case for interferon lambda. J Exp Med. 217:5–8. 2020.PubMed/NCBI View Article : Google Scholar
|
|
112
|
Bray M, Rayner C, Noël F, Jans D and
Wagstaff K: Ivermectin and COVID-19: A report in Antiviral
Research, widespread interest, an FDA warning, two letters to the
editor and the authors' responses. Antiviral Res.
178(104805)2020.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Caly L, Druce JD, Catton MG, Jans DA and
Wagstaff KM: The FDA-approved drug ivermectin inhibits the
replication of SARS-CoV-2 in vitro. Antiviral Res.
178(104787)2020.PubMed/NCBI View Article : Google Scholar
|
|
114
|
González Canga A, Sahagún Prieto AM, Diez
Liébana MJ, Fernández Martínez N, Sierra Vega M and García Vieitez
JJ: The pharmacokinetics and interactions of ivermectin in humans -
a mini-review. AAPS J. 10:42–46. 2008.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Buonfrate D, Salas-Coronas J, Muñoz J,
Maruri BT, Rodari P, Castelli F, Zammarchi L, Bianchi L, Gobbi F,
Cabezas-Fernández T, et al: Multiple-dose versus single-dose
ivermectin for Strongyloides stercoralis infection (Strong Treat 1
to 4): A multicentre, open-label, phase 3, randomised controlled
superiority trial. Lancet Infect Dis. 19:1181–1190. 2019.
View Article : Google Scholar
|
|
116
|
Kelleni MT: Nitazoxanide/azithromycin
combination for COVID-19: A suggested new protocol for early
management. Pharmacol Res. 157(104874)2020.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Padmanabhan S: Potential dual therapeutic
approach against SARS-CoV-2/COVID-19 with nitazoxanide and
hydroxychloroquine. Preprint. 2020.PubMed/NCBI View Article : Google Scholar
|
|
118
|
Ulloa L: The vagus nerve and the nicotinic
anti-inflammatory pathway. Nat Rev Drug Discov. 4:673–684.
2005.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Martineau AR, Jolliffe DA, Hooper RL,
Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa
D, Ginde AA, et al: Vitamin D supplementation to prevent acute
respiratory tract infections: Systematic review and meta-analysis
of individual participant data. BMJ. 356(i6583)2017.PubMed/NCBI View Article : Google Scholar
|
|
120
|
Helming L, Böse J, Ehrchen J, Schiebe S,
Frahm T, Geffers R, Probst-Kepper M, Balling R and Lengeling A:
1α,25-Dihydroxyvitamin D3 is a potent suppressor of interferon
γ-mediated macrophage activation. Blood. 106:4351–4358.
2005.PubMed/NCBI View Article : Google Scholar
|
|
121
|
Ilie PC, Stefanescu S and Smith L: The
role of Vitamin D in the prevention of Coronavirus Disease 2019
infection and mortality. Aging Clin Exp Res. May 6. 2020.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print). View Article : Google Scholar
|
|
122
|
Alexander OM: Evidence on spironolactone
safety in COVID-19 reassuring. Medscape. April 29. 2020.(Epub ahead
of print).
|
|
123
|
Gustavo Carlos Wambier GA: Severe acute
respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is likely
to be androgen mediated. J Am Acad Dermatol. 21:1–9.
2020.PubMed/NCBI View Article : Google Scholar
|
|
124
|
Jin JM, Bai P, He W, Wu F, Liu XF, Han DM,
Liu S and Yang JK: Gender differences in patients with COVID-19:
Focus on severity and mortality. Front Public Health.
8(152)2020.PubMed/NCBI View Article : Google Scholar
|
|
125
|
Spironolactone in Covid-19 Induced ARDS.
uriClinicalTrials.govsimpleClinicalTrials.gov.
https://www.smartpatients.com/trials/NCT04345887.
Accessed April, 2020.
|
|
126
|
Kleinnijenhuis J, Quintin J, Preijers F,
Benn CS, Joosten LA, Jacobs C, van Loenhout J, Xavier RJ, Aaby P,
van der Meer JW, et al: Long-lasting effects of BCG vaccination on
both heterologous Th1/Th17 responses and innate trained immunity. J
Innate Immun. 6:152–158. 2014.PubMed/NCBI View Article : Google Scholar
|
|
127
|
Gearoid R: Japan was expecting a
coronavirus explosion. Where is it? The Japan Times. 2020.
|
|
128
|
Moorlag SJ, Arts RJ, van Crevel R and
Netea MG: Non-specific effects of BCG vaccine on viral infections.
Clin Microbiol Infect. 25:1473–1478. 2019.PubMed/NCBI View Article : Google Scholar
|
|
129
|
BCG Vaccination to Protect Healthcare
Workers Against COVID-19. uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04327206.
Accessed March 31, 2020.
|
|
130
|
BCG vaccine for health care workers as
defense against COVID-19. uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04348370.
Accessed April 16, 2020.
|
|
131
|
Saad M and Elsalamony R: Measles vaccines
may provide partial protection against COVID-19. Int J Cancer
Biomed Res. 5:14–19. 2020. View Article : Google Scholar
|
|
132
|
Fischer JC, Zänker K, van Griensven M,
Schneider M, Kindgen-Milles D, Knoefel WT, Lichtenberg A,
Tamaskovics B, Djiepmo-Njanang FJ, Budach W, et al: The role of
passive immunization in the age of SARS-CoV-2: An update. Eur J Med
Res. 25(16)2020.PubMed/NCBI View Article : Google Scholar
|
|
133
|
Keith P, Day M, Perkins L, Moyer L, Hewitt
K and Wells A: A novel treatment approach to the novel coronavirus:
An argument for the use of therapeutic plasma exchange for
fulminant COVID-19. Crit Care. 24(128)2020. View Article : Google Scholar
|
|
134
|
Lennart H, Hassan A, Fausto B, Harold M
and Hammarström QP: Development of passive immunity against
SARS-CoV-1 2 for management of immunodeficient patients - a
perspective. J Allergy Clin Immunol. May 12. 2020.(Epub ahead of
print). View Article : Google Scholar
|
|
135
|
Honore PM, Mugisha A, Kugener L, Redant S,
Attou R, Gallerani A and De Bels D: Therapeutic plasma exchange as
a routine therapy in septic shock and as an experimental treatment
for COVID-19: We are not sure. Crit Care. 24(226)2020.PubMed/NCBI View Article : Google Scholar
|
|
136
|
Treatments for COVID-19: Canadian Arm of
the SOLIDARITY Trial. uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT04330690.
Accessed April 1, 2020.
|
|
137
|
Randomized embedded multifactorial
adaptive platform trial for community- acquired pneumonia.
uriClinicalTrials.govsimpleClinicalTrials.gov.
https://clinicaltrials.gov/ct2/show/NCT02735707.
Accessed April 13, 2016.
|
|
138
|
Trial of treatments for COVID-19 in
hospitalized adults. uriClinicalTrials.govsimpleClinicalTrials.gov.
https://www.centerwatch.com/clinical-trials/listings/241173/corona-virus-infection-trial-treatments-covid-19-hospitalized/?&radius=50.
Accessed June 2020.
|