Introduction
Laser-assisted in situ keratomileusis (LASIK)
is the default choice of refractive surgery procedures as it can be
addressed to a wide spectrum of ametropias and can treat high order
wavefront aberrations or topographic irregularities (1,2). Since
some complications of the mechanical microkeratome (free caps,
incomplete, irregular or displaced flaps) can be avoided using the
femtosecond laser technology, many surgeons prefer using this new
technology to perform the LASIK flaps (1,2).
Comparing to mechanical microkeratome, femtosecond laser can create
customized flaps - centration, diameter, thickness of the flap,
position and length of the hinge and also the side cut angle can be
set by the surgeon according to the characteristics of each patient
(1-4).
However, the Femtosecond-LASIK (FemtoLASIK)
technique is not risk-free (1,2).
Performing the flap assisted by the femtosecond laser can produce
specific cavitation bubble related complications: opaque bubble
layer (OBL), buttonhole formation and presence of an air bubble in
the anterior chamber (1,5). Complications of the classic LASIK
technique can also be encountered (1).
Ten years after having started the Femtosecond-LASIK
surgeries in Romania, we are reviewing our results, in order to
assess the incidence of intraoperative flap and interface-related
complications and their management.
Patients and methods
Data collection
A retrospective, non-comparative consecutive case
series study was performed on eyes with different refractive errors
that underwent FemtoLASIK surgeries. Patients were operated by the
same refractive surgeon (H.T.S.) in two refractive centers: Europe
Eye - Metropolitan Hospital in Bucharest and Timisoara Clinical
Emergency Hospital, between June 2011 and April 2020. For the flap
creation step all surgeries were performed using
VisuMax® (Carl Zeiss Meditec) femtosecond laser.
A descriptive case series is reported of the
intraoperative flap and interface-related complications encountered
to the eyes included in the study.
Inclusion and exclusion criteria
Inclusion criteria for the surgery were as follows:
patients ≥ 22 years of age with no refractive change for at least 2
years before surgery, central endothelial cell count ≥2,000
cells/mm2, stable peripheral retina (normal or already
treated by laser photocoagulation if at-risk peripheral lesions
were present) and good compliance (1,6).
Eye-related exclusion criteria for the surgery were:
evidence or suspected ectasia, thinnest point on pachymetry ≤500
µm, insufficient corneal thickness for laser ablation (estimated
residual thickness of the stromal bed after treatment ≤300 µm),
severe dry eye syndrome, any sign of ocular inflammation or
infection (1,6), any ocular disease that might interfere
with visual acuity (e.g., cataract, congenital or acquired macular
pathology, optic nerve pathology) (1,7-13),
any previous ocular trauma, any previous ocular procedures (e.g.,
vitreo-retinal surgery, glaucoma laser procedures or glaucoma
surgery) (14-21),
and patients taking medications with high risk of ocular side
effects (e.g., amiodarone, isotretinoin) (1,22).
Orbital anatomy was assessed in order to permit the
proper suction cup positioning. There were excluded patients with
very deep-set eyes, patients with narrow palpebral fissures or
periocular tumors (23-25).
Pregnancy or lactation were exclusion criteria for
the surgery (1,6). Also excluded were patients with
systemic diseases that could interfere with the wound-healing
process (e.g., diabetes mellitus, autoimmune disorders) (1,6,26,27) or
with risk of postoperative low visual acuity due to possible
vascular complications including ischemic optic neuropathy or
vascular occlusion (e.g., severe systemic hypertension, severe
dyslipidemia and cardiovascular diseases) (7,9,28-30).
The psychological profile was also considered and
patients with unreasonable expectations or unable to understand the
perioperative conditions were excluded.
Preoperative assessment
Patients underwent preoperative ocular examination
that included: uncorrected and corrected distance visual acuity,
manifest and cycloplegic refractions, fogging refraction (in
hyperopic and mixed astigmatic patients), non-contact tonometry,
keratometry, ultrasound corneal pachymetry, white-to-white corneal
diameter, corneal topography and tomography (Scheimpflug),
pupillometry, corneal endothelial cell count, anterior segment
slit-lamp examination and mydriatic fundus examination.
Soft contact lens wearing should have been
discontinued 2 weeks prior to preoperative investigations and then
2 weeks prior to surgery.
The study was approved by the Ethics Committee of
‘Carol Davila’ University of Medicine and Pharmacy (Bucharest,
Romania). After being fully informed about the benefits and risks
of the procedure, all patients signed an informed consent in
accordance with the Declaration of Helsinki.
Surgical technique
All surgeries were performed using the same protocol
and technique, by a single refractive surgeon (HTS) with the same
femtosecond laser (VisuMax®, Carl Zeiss Meditec).
Topical anesthesia with oxybuprocaine 0.4% was used
before surgery. The eyelids were sterilized with 10%
povidone-iodine solution, then a sterile surgical drape was applied
and a lid speculum was inserted. The eye to be treated was
positioned under the femtosecond laser integrated surgical
microscope. The patient was asked to fix the target flashing light.
The size of the docking cup was chosen according to the
white-to-white corneal diameter. While the patient was asked not to
move the head, after an appropriate centration, the surgeon
initiated the automatic suction. When the suction was complete, the
surgeon initiated the femtosecond laser procedure, settled at 1,043
nm wavelength and 500 kHz pulse frequency. For the corneal flap
cutting, the parameters were 7.9-8.9 mm diameter, 100-130 µm depth,
3.45-3.84 mm hinge width (50˚ angle) in superior position and 90˚
side cut angle. In patients operated in both eyes, the procedure
started with the right eye, and then the fellow eye was treated
identically.
The dissection of the flap was performed using a
double-ended flap lifter. After drying the corneal bed with special
sponges, the underlying stroma was treated for refractive
correction using an excimer laser. According to situation, when
both eyes needed to be treated, the right eye was treated first. At
the end of the surgery, a disposable bandage contact lens was
applied and antibiotic (moxifloxacin 0.5%) and artificial tear
drops were instilled in the treated eye/eyes.
Patients were examined at the slit lamp thirty
minutes after the surgery, in order to assess the flap position,
the flap regularity and the interface clarity.
Postoperative care
Postoperative treatment started after the surgery
and consisted in topical eye drops: antibiotic q.d.s. for one week
(moxifloxacin 0.5%), non-steroid anti-inflammatory t.d.s. for 2
weeks (pranoprofen 0.1% or indomethacin 0.1%), artificial tears
q.d.s. for 12 months and steroids (fluorometolone 0.2%),
recommended to be applied q.d.s. for 2 weeks, then gradually
tapered (t.d.s., b.d.s. and q.d. 2 weeks each).
The bandage contact lens was removed at the first
day postoperative visit when the evaluation consisted in
measurement of the manifest refraction, uncorrected distance visual
acuity and slit-lamp examination of the cornea.
The following postoperative visits were carried out
at one, three, six and twelve months. At every of these
examinations a slit-lamp examination of the anterior segment and
several investigations were performed: manifest refraction,
uncorrected distance visual acuity, non-contact tonometry, corneal
topography and tomography (Scheimpflug). For the eyes where a
residual refraction was determined or the visual acuity was
uncorrelated withe the manifest refraction, we also tested the
corrected distance visual acuity and the cycloplegic
refraction.
Results
Patient demographics and operative
data
Four thousand and thirty-two eyes (2,086 right eyes
and 1,946 left eyes) from 2,310 patients (1,344 females and 966
males) were reviewed in our retrospective interventional
consecutive case series study. Mean patient age at the time of
surgery was 31.28±6.724 years (range, 22-49 years). One thousand
seven hundred and twenty-two patients had FemtoLASIK performed
bilaterally on the same day (3,444 eyes) and 588 patients had
unilateral FemtoLASIK, being anisometropic cases (588 eyes). Eight
hundred and ninety-six eyes (22.22%) had myopic FemtoLASIK surgery,
1,498 eyes (37.15%) were operated for myopic astigmatism, 1,036
eyes (25.69%) were mixed astigmatic eyes before surgery, 406 eyes
(10.07%) were operated for hyperopic astigmatism and 196 eyes
(4.87%) underwent FemtoLASIK surgery for hyperopia.
Intraoperative flap and
interface-related complications
Intraoperative flap and interface complications
included difficult docking (n=28; 0.69%), suction loss (n=52;
1.29), cavitation gas bubble related complications (n=854; 21.18%),
bleeding from limbal blood vessels (n=14; 0.35%), difficult
dissection of the flap (n=24; 0.59%), de-epithelialization of the
flap (n=5; 0.12%) and interface debris (n=1; 0.025%) (Table I).
 | Table IIntraoperative flap and
interface-related complications. |
Table I
Intraoperative flap and
interface-related complications.
| Intraoperative
complications | No of cases
(%) |
|---|
| Difficult
docking | 28 (0.69) |
| Suction loss | 52 (1.29) |
| Cavitation gas
bubble related complications | 854 (21.18) |
|
Opaque
bubble layer (OBL) | 854 (21.18) |
|
Vertical gas
breakthrough with buttonhole formation | 0 (0) |
|
Air bubbles
in the anterior chamber | 0 (0) |
| Bleeding from
limbal blood vessels | 14 (0.35) |
| Difficult
dissection of the flap | 24 (0.59) |
|
Free
flap | 0 (0) |
|
De-epithelialization of the flap | 5 (0.12) |
| Interface
debris | 1 (0.025) |
Difficult docking was encountered in 28 cases
(0.69%) due either to unfavourable orbital anatomy or to
inappropriate patient cooperation. All cases required multiple
repeated maneuvers of repositioning of the docking cup.
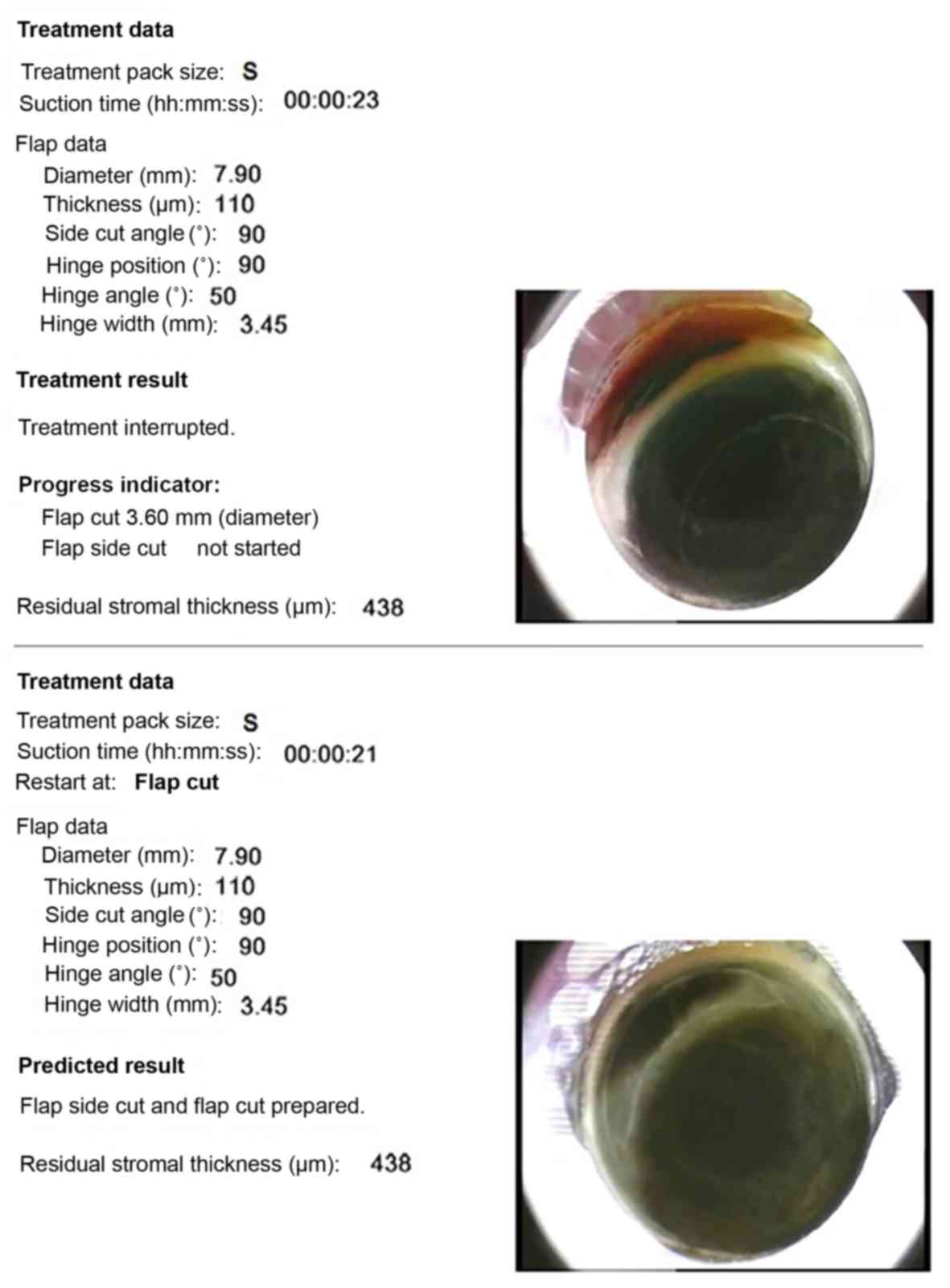
Suction loss occurred in 52 eyes (1.29%). The causes
for suction loss were: excessive eyelid squeezing (19 eyes, 0.47%),
inappropriate docking (16 eyes, 0.39%), patient head movement (12
eyes, 0.29%), conjunctiva penetrating under the suction cup (2
eyes, 0.05%), flat corneas (keratometric power - 38.50D,
respectively, 38.75D for the same patient, 0.05%) and interruption
of the power supply of the femtosecond laser machine (1 eye,
0.025%). There were different situations of losing suction
(Table II). In most cases (31 eyes,
1.02%) suction break occurred during building up the vacuum,
requiring another placement of the suction cup. The challenging
situations were losing suction after the femtosecond laser
treatment began. If the suction loss occurs after flap creation has
started, managing the case may be quite complicated. In one
patient, in the left eye, the second to be treated, the suction
loss occurred during the flap creation. In this one case (0.025%),
we dissected the flap in the right eye where the femtosecond laser
treatment was already performed, but without excimer laser
treatment, then the procedure was aborted and rescheduled after
three months for both eyes. At retreatment time, the femtosecond
laser treatment for the left eye was set and performed 20 µm
deeper, followed by excimer laser treatment and for the right eye,
the already cut flap was only lifted and the excimer laser was
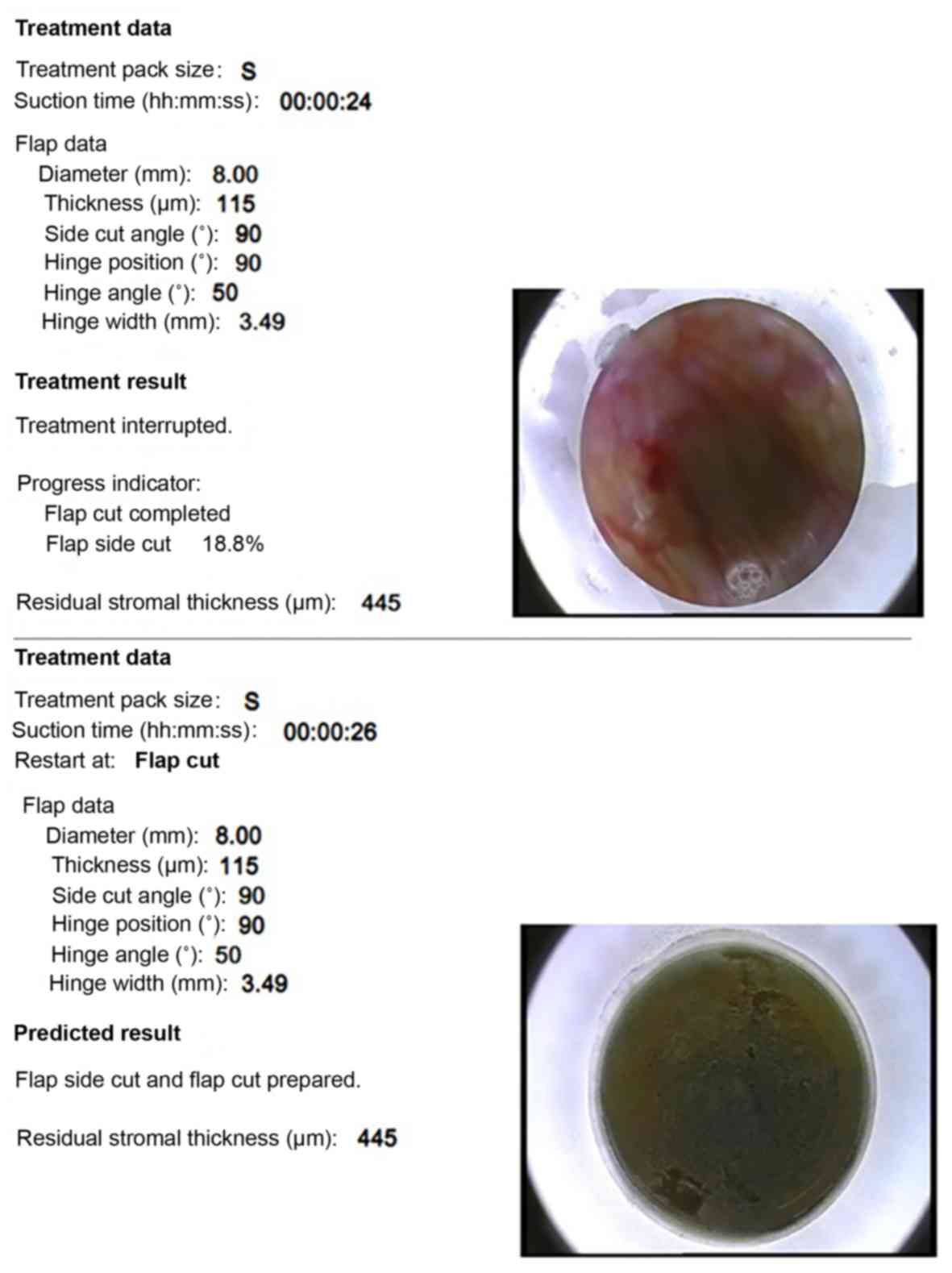
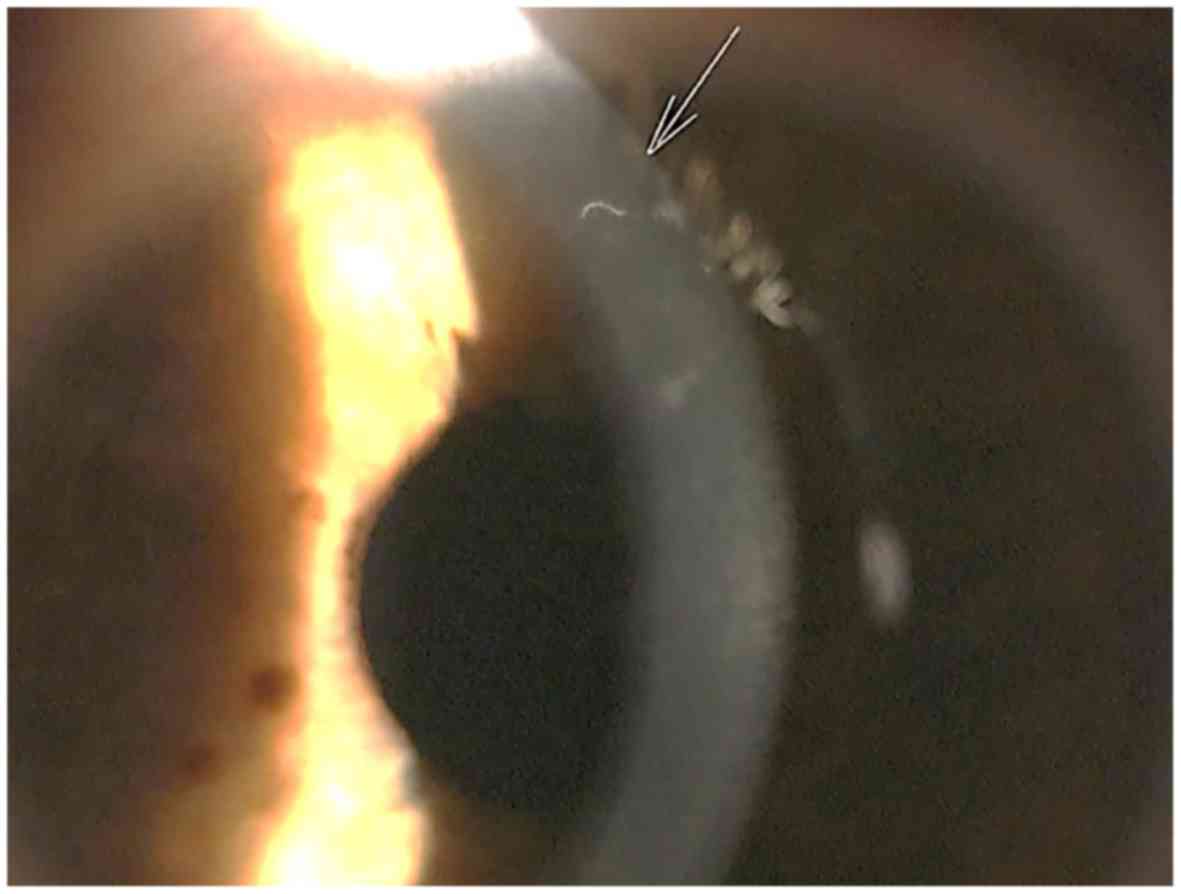
applied. In all the other cases, the suction loss occurred either
after the flap cut was done but before side cut creation (4 eyes,
0.1%) (Fig. 1) or during the side
cut time (16 eyes, 0.15%) (Fig. 2).
In all these cases the surgeon could recenter the suction cup, the
eyes could be re-docked and the femtosecond procedure could be
continued from the moment when the suction was lost.
 | Table IIIntraoperative suction loss. |
Table II
Intraoperative suction loss.
| Time of suction
loss | No of cases
(%) |
|---|
| During building-up
the vacuum | 31 (1.02) |
| During the flap
creation | 1 (0.025) |
| After the flap was
created but before the side cutting began | 4 (0.1) |
| During the side
cutting | 16 (0.15) |
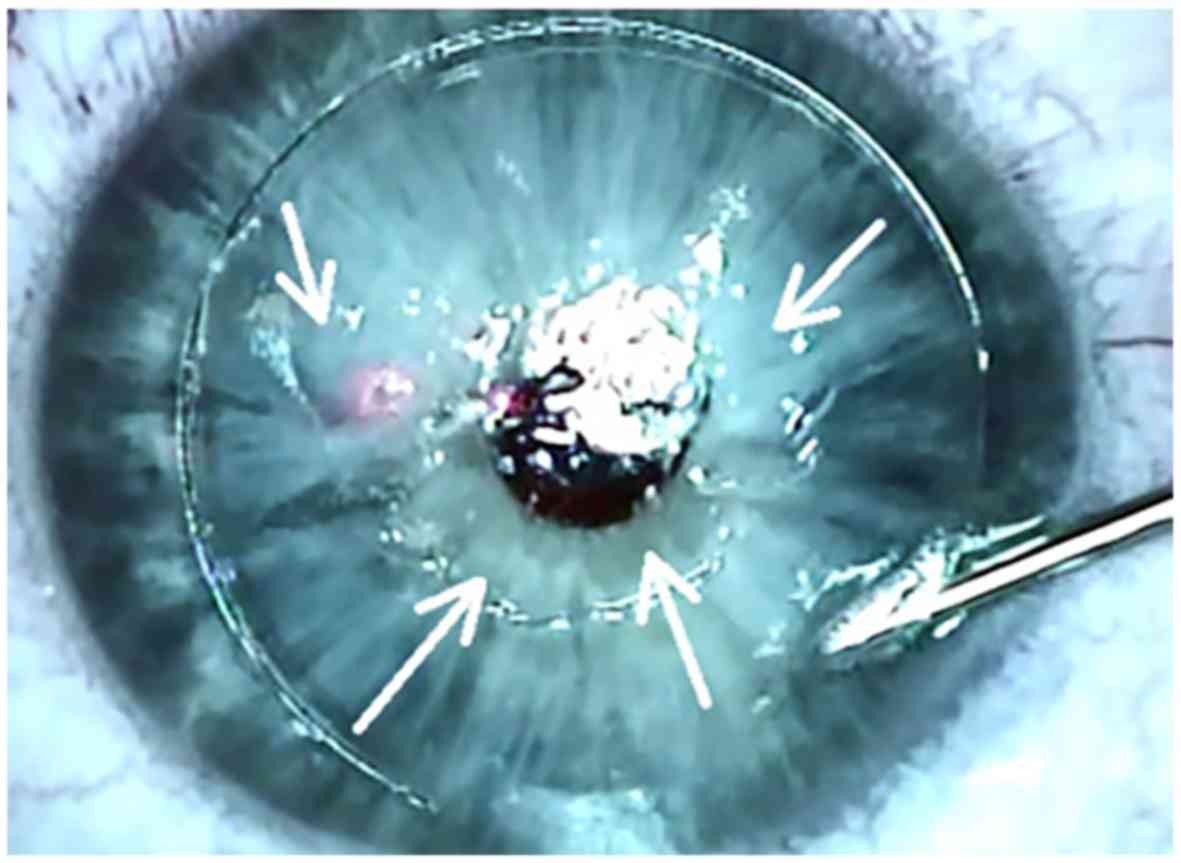
In order to assess the impact of the OBL on the
laser procedure we divided the OBL according to its extension and
position, as follows: minimal (OBL located at the periphery of the
flap and/or width <2 mm), moderate (OBL located near the
pupillary area and/or width between 2-4 mm) and severe (OBL located
centrally and/or width >4 mm). Mild OBL was encountered
(Fig. 3) in 742 cases (18.40%),
moderate OBL (Fig. 4) in 112 cases
(2.77%) and not severe OBL (Table
III). In none of the OBL cases was difficulties or incidents
encountered in dissecting or lifting the flap or in the subsequent
excimer laser treatment. No other cavitation bubble complication
such as buttonhole formation or presence of air bubbles in the
anterior chamber were encountered.
 | Table IIIIntraoperative OBL. |
Table III
Intraoperative OBL.
| Type of OBL | No of cases
(%) |
|---|
| Mild OBL (OBL
located at the periphery of the flap and/or width <2 mm) | 742 (18.40) |
| Moderate OBL (OBL
located near the pupillary area and/or width 2-4 mm) | 112 (2.77) |
| Severe OBL (OBL
located centrally and/or width >4 mm) | 0 (0) |
Bleeding from limbal blood vessels immediately after
the flap creation occurred in 14 cases (0.35%), all those patients
being chronic contact lens wearers before the surgery. In all the
cases, the haemorrhage was stopped before the excimer laser
ablation and there were no visual consequences.
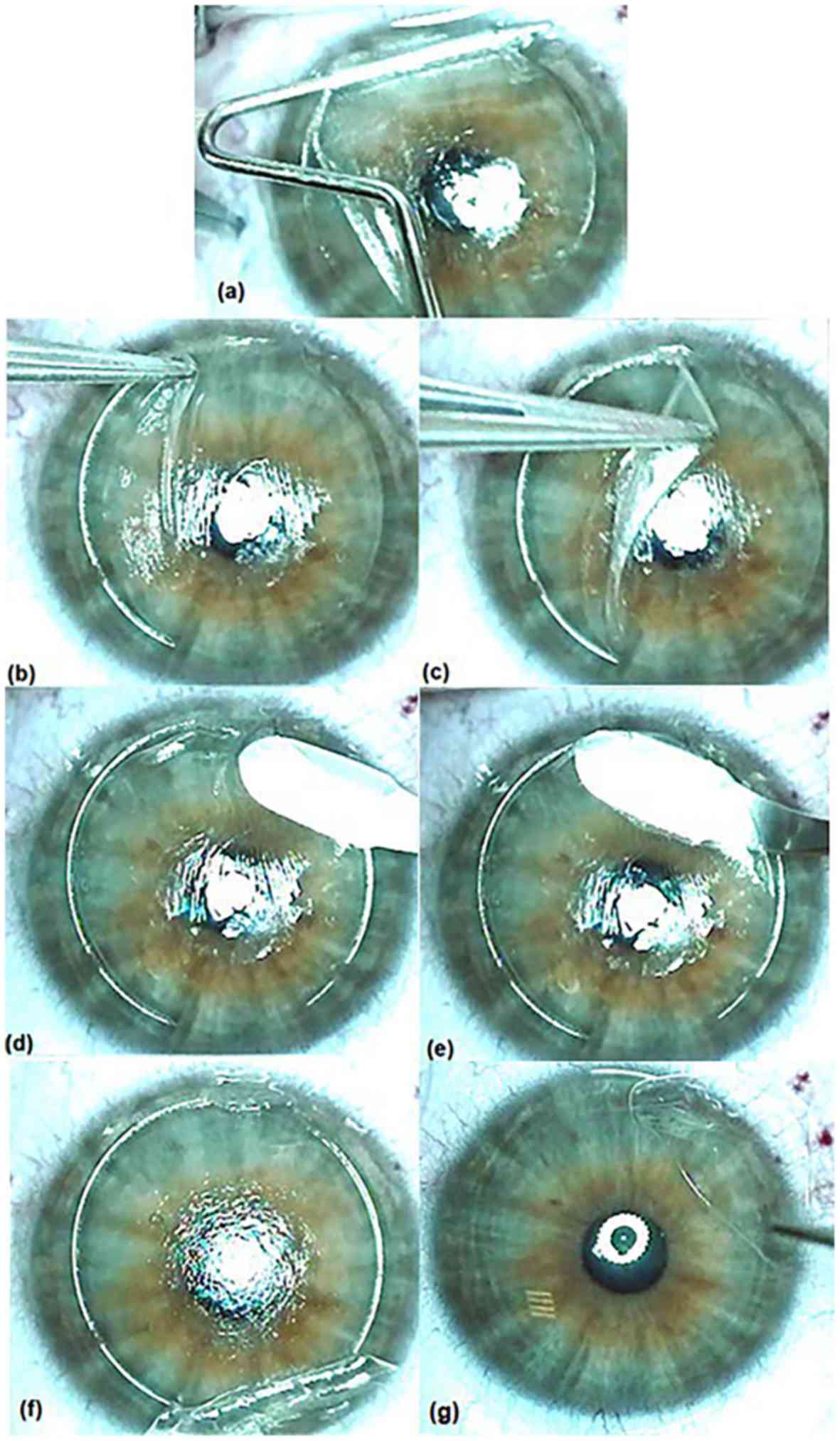
In 24 eyes (0.59%) the dissection of the flap was
difficult to perform, due to the impossibility of opening of the
side cut on its entire circumference. All cases were preceded by
suction loss, leading to the presence of some adhesions at the side
cut or incomplete side cut. Dissection of the areas of adhesion and
flap lifting were possible using a spatula, a LASIK flap forceps
and a crescent blade (Fig. 5).
Epithelial defects of the flap (Fig. 6) were encountered in 5 eyes (0.12%)
and this situation was due to multiple surgical maneuvers in the
context of inappropriate patient cooperation (3 eyes, 0.07%) or
anterior basement membrane dystrophy (both eyes of the same
patient, 0.05%). Surgical approach included de-epithelialization of
the entire corneal surface, permanent removal of the epithelial
debris avoiding contact with flap margins and continuous wear of
the bandage contact lens until complete re-epithelialization
occurred.
Immediately after the surgical procedure, when
assessing the flap position and interface clarity at the slit-lamp,
we found in one eye (0.025%) a textile debris at the flap interface
(Fig. 7). Surgical solution was
lifting the flap, removal of the textile debris by irrigating the
interface with saline solution and proper repositioning of the
flap.
Discussion
Laser refractive surgery techniques and technology
have undergone continuous advancements in the last decades, being
increasingly precise and highly predictable (1,2,31,32).
Although small incision lenticule extraction (SMILE) is the newest
and promising refractive technique with controversial advantages
(31), LASIK is still currently the
most popular refractive procedure worldwide, as it can be used to
correct all types of ametropias, between large diopters limits
(1,2,33-35).
The essential step of LASIK is the corneal flap creation which is
performed nowadays in the most modern way, assisted by a
femtosecond laser (1,33). Compared with the mechanical
microkeratome, the femtosecond laser-assisted flaps are more
precise, more accurate, can be customized and have a high
reproducibility (1,2,36).
However, this step is not risk-free but fortunately, flap-related
complications are quite rare in FemtoLASIK technique (1,33).
Docking is the step that connects the eye to the
femtosecond laser system. The time required for proper docking
reduces with the learning curve (37). Docking can be difficult in case of
deep set orbits or tight palpebral aperture (38).
Suction loss is a femtosecond laser specific
complication. The suction loss occurs more likely when the suction
cup is not perfectly applied on the eye, allowing the fluid to pass
between the eye and the suction cup (39). Other predisposing factors for suction
loss are: flat corneas, excessive tearing reflex, narrow palpebral
aperture, bad positioning of the patient, poor compliance of the
patient due to anxiety or inability to follow instructions
(40-42).
Suction loss can occur in any step of flap creation. Managing the
result of a suction break varies according with the moment of
occurrence. If the suction loss occurs during the flap creation,
the procedure should be aborted and rescheduled for up to 2 months
(1,42). If the suction loss occurs either
after the flap was fully created or during the creation of the side
cut, the procedure can be resumed from the moment of interruption
after proper re-docking (1,42).
Cavitation gas bubbles produced by the femtosecond
laser can lead to specific complications (1,42). OBL
occurs when these bubbles expand and become trapped in the anterior
stroma, at the interface plane (1,42). The
incidence of OBL ranges up to 48% (42,43), its
formation being influenced by flap diameter under 8 mm (44), thick corneas (43,45),
high hysteresis (43,45) and laser settings such as: spot
spacing, pocket size and energy level (42). Severe OBL presence can interfere with
interface dissection (42) and can
disturb eye tracking of the excimer laser (46). In addition to the OBL, the cavitation
gas bubbles can produce other complications: vertical gas
breakthrough with buttonhole formation or presence of the bubbles
in the anterior chamber (42).
Bleeding from limbal blood vessels in chronic
contact lens wearers can be avoided using, if possible, smaller
suction cups. If perilimbal haemorrhage lead to interface haze,
according to severity it is possible either to medically treat with
steroid drops or to lift the flap and to irrigate the interface
with saline solution (47,48).
Compared with microkeratome-created flaps,
dissecting and lifting the femtosecond laser-assisted flaps can be
more difficult, the risk of flap tears being increased (42). If a small peripheral flap tear is
present and the dissection is complete, the excimer ablation can be
performed (42). In case of large or
central flap tear, the procedure is recommended to be aborted,
considering further a surface ablation (42).
Epithelial defects are uncommon in FemtoLASIK
technique (42). Predisposing
factors include: use of excessive topical anaesthetic, recurrent
erosion syndrome and anterior basement membrane dystrophy (42). Manipulation of the spatula along the
side cut edge can produce epithelial defects (42).
Interface debris can result due to Meibomian gland
secretions, eyelashes, textile material from compresses or sponges,
or talc from gloves (42). Despite
prevention methods, debris is still reported to be noted at the
postoperative visit (42). If it is
not visually significant or it does not cause infection or
inflammation, interface debris can be just observed. Otherwise,
flap lifting and thoroughly irrigation of the interface is
necessary (42).
FemtoLASIK technique has revolutionized refractive
surgery since its introduction. Although the procedure is highly
safe, complications can occur (49).
Refractive surgeons should be aware of all the intraoperative
flap-related complication in FemtoLASIK procedure. Fortunately,
these complications are rare and with proper management, studies
have shown no alteration of the visual function (33).
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The data that support the findings of this study are
available from the corresponding author (HTS) upon reasonable
request.
Authors' contributions
BT, HTS, SS, MZ and VM contributed to the conception
and design of the study, the acquisition, analysis and
interpretation of the data. BT, HTS, SS, MZ and VM also contributed
to the drafting of the manuscript and its critical revision for
important intellectual content. MM contributed to the analysis and
interpretation of the data, the drafting of the manuscript and its
critical revision for important intellectual content. All authors
read and approved the final version of the manuscript and agreed to
be accountable for all aspects of the study in ensuring that
questions related to the accuracy or integrity of any part of the
work are appropriately investigated and resolved.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
‘Carol Davila’ University of Medicine and Pharmacy (Bucharest,
Romania). All participants signed an informed consent.
Patient consent for publication
This manuscript does not contain case details,
personal information or images that may enable an individual to be
identified.
Competing interests
The authors have no financial or proprietary
interest to declare in any device presented in this article.
References
|
1
|
Tăbăcaru B: Femtosecond Laser - Excimer
Laser Platform for ametropias surgery (unpublished PhD thesis)
‘Carol Davila’ University of Medicine and Pharmacy, no. TD 4697,
2019.
|
|
2
|
Shah R: History and results; Indications
and contraindications of SMILE Compared With LASIK. Asia Pac J
Ophthalmol (Phila). 8:371–376. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Soong HK and Malta JB: Femtosecond lasers
in ophthalmology. Am J Ophthalmol. 147:189–197.e2. 2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sugar A: Ultrafast (femtosecond) laser
refractive surgery. Curr Opin Ophthalmol. 13:246–249.
2002.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Stonecipher KG, Ignacio TS and Stonecipher
KG: Complications and management with the femtosecond laser In:
Management of Complications in Refractive Surgery. Alio JL and Azar
DT (eds). 1st edition. Springer-Verlag Berlin Heidelberg,
pp169-177, 2008.
|
|
6
|
Stanca HT, Munteanu M, Jianu DC, Motoc
AGM, Jecan CR, Tăbăcaru B, Stanca S and Preda MA: Femtosecond-LASIK
outcomes using the VisuMax®-MEL® 80 platform
for mixed astigmatism refractive surgery. Rom J Morphol Embryol.
59:277–283. 2018.PubMed/NCBI
|
|
7
|
Cameron BD, Saffra NA and Strominger MB:
Laser in situ keratomileusis-induced optic neuropathy.
Ophthalmology. 108:660–665. 2001.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Stanca HT, Suvac E, Munteanu M, Jianu DC,
Motoc AGM, Roşca GC and Boruga O: Giant cell arteritis with
arteritic anterior ischemic optic neuropathy. Rom J Morphol
Embryol. 58:281–285. 2017.PubMed/NCBI
|
|
9
|
Maden A, Yilmaz S and Yurdakul NS:
Nonarteritic ischemic optic neuropathy after LASIK with femtosecond
laser flap creation. J Neuroophthalmol. 28:242–243. 2008.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Munteanu M, Rosca C and Stanca H:
Sub-inner limiting membrane hemorrhage in a patient with Terson
syndrome. Int Ophthalmol. 39:461–464. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Vingolo EM, Grenga PL, Meduri A, Lupo S
and Grenga R: Refractive surgery in patients with retinitis
pigmentosa. Eur J Ophthalmol. 20:271–275. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Branisteanu DC, Munteanu M, Branisteanu
DE, Stanca HT, Moraru A and Balta F: ‘Off-label’ drug use-ethical
challenges-case study-AVASTIN®. Rev Rom Bioet. 13:83–88.
2015.
|
|
13
|
Stanca HT, Stanca S, Tabacaru B, Boruga M
and Balta F: Bevacizumab in Wet AMD treatment: A tribute to the
thirteen years of experience from the beginning of the anti-VEGF
era in Romania. Exp Ther Med. 18:4993–5000. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Panozzo G and Parolini B: Relationships
between vitreoretinal and refractive surgery. Ophthalmology.
108:1663–1668; discussion 1668-1669. 2001.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Osman E: Laser refractive surgery in
glaucoma patients. Saudi J Ophthalmol. 25:169–173. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kozobolis V, Konstantinidis A, Sideroudi H
and Labiris G: The effect of corneal refractive surgery on
glaucoma. J Ophthalmol. 2017(8914623)2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Stanca HT, Munteanu M, Jianu DC, Motoc
AGM, Tăbăcaru B, Stanca S, Ungureanu E, Boruga VM and Preda MA: New
perspectives in the use of laser diode transscleral
cyclophotocoagulation. A prospective single center observational
cohort study. Rom J Morphol Embryol. 59:869–872. 2018.PubMed/NCBI
|
|
18
|
Ahmad M, Chocron I and Shrivastava A:
Considerations for refractive surgery in the glaucoma patient. Curr
Opin Ophthalmol. 28:310–315. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Preda MA, Karancsi OL, Munteanu M and
Stanca HT: Clinical outcomes of micropulse transscleral
cyclophotocoagulation in refractory glaucoma - 18 months follow-up.
Lasers Med Sci: Jan 14, 2020 (Epub ahead of print). doi: https://doi.org/10.1007/s10103-019-02934-x.
|
|
20
|
Shrivastava A, Madu A and Schultz J:
Refractive surgery and the glaucoma patient. Curr Opin Ophthalmol.
22:215–221. 2011.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Bashford KP, Shafranov G, Tauber S and
Shields MB: Considerations of glaucoma in patients undergoing
corneal refractive surgery. Surv Ophthalmol. 50:245–251.
2005.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Bower KS and Woreta F: Update on
contraindications for laser-assisted in situ keratomileusis and
photorefractive keratectomy. Curr Opin Ophthalmol. 25:251–257.
2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Abell RG, Kerr NM and Vote BJ: Femtosecond
laser-assisted cataract surgery compared with conventional cataract
surgery. Clin Exp Ophthalmol. 41:455–462. 2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Roberts TV, Lawless M, Bali SJ, Hodge C
and Sutton G: Surgical outcomes and safety of femtosecond laser
cataract surgery: A prospective study of 1500 consecutive cases.
Ophthalmology. 120:227–233. 2013.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Boruga O, Bălăşoiu AT, Giuri S, Munteanu
M, Stanca HT, Iovănescu G and Preda MA: Caruncular late-onset
junctional nevus: Apropos of an anatomo-clinical observation. Rom J
Morphol Embryol. 58:1461–1464. 2017.PubMed/NCBI
|
|
26
|
Garcia-Gonzalez M, Gros-Otero J,
Rodriguez-Perez I, Rodero A and Teus MA: Effect of age on visual
and refractive results after LASIK: Mechanical microkeratome versus
femtosecond laser. Int J Ophthalmol. 12:488–495. 2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Simpson RG, Moshirfar M, Edmonds JN,
Christiansen SM and Behunin N: Laser in situ keratomileusis in
patients with collagen vascular disease: A review of the
literature. Clin Ophthalmol. 6:1827–1837. 2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Balint GS, Iovanescu G, Stanca H, Popoiu
CM, Boia E, Popovici RA and Bolintineanu SL: The protective effect
of HDL-cholesterol in patients with essential hypertension. Rev
Chim. 68:949–952. 2017.
|
|
29
|
Smith BT, Park CH and Fekrat S:
Hemi-retinal vein occlusion following LASIK. Ann Ophthalmol
(Skokie). 38:139–140. 2006.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Stanca HT, Petrović Z and Munteanu M:
Transluminal Nd:YAG laser embolysis - a reasonable method to
reperfuse occluded branch retinal arteries. Vojnosanit Pregl.
71:1072–1077. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Hamed AM, Abdelwahab SM and Soliman TT:
Intraoperative complications of refractive small incision lenticule
extraction in the early learning curve. Clin Ophthalmol.
12:665–668. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Alio J: Refractive surgery today: Is there
innovation or stagnation? Eye Vis (Lond). 1(4)2014.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Espandar L and Meyer J: Intraoperative and
postoperative complications of Laser in situ keratomileusis flap
creation using IntraLase Femtosecond Laser and mechanical
microkeratomes. Middle East Afr J Ophthalmol. 17:56–59.
2010.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Tăbăcaru B and Stanca HT: One year
refractive outcomes of Femtosecond-LASIK in mild, moderate and high
myopia. Rom J Ophthalmol. 61:23–31. 2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Tăbăcaru B and Stanca HT: Scheimpflug
topographical changes after Femtosecond LASIK for mixed astigmatism
- theoretical aspects and case study. Rom J Ophthalmol. 61:69–75.
2017.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Perez-Straziota C and Randleman JB:
Femtosecond-assisted LASIK: Complications and management. Int
Ophthalmol Clin. 56:59–66. 2016.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Christy JS, Nath M, Mouttapa F and
Venkatesh R: Learning curve of femtosecond laser-assisted cataract
surgery: Experience of surgeons new to femtosecond laser platform.
Indian J Ophthalmol. 65:683–689. 2017.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Moshirfar M, Churgin DS and Hsu M:
Femtosecond laser-assisted cataract surgery: A current review.
Middle East Afr J Ophthalmol. 18:285–291. 2011.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Hamed AM, Heikal MA, Soliman TT, Daifalla
A and Said-Ahmed KE: SMILE intraoperative complications: Incidence
and management. Int J Ophthalmol. 12:280–283. 2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Wong CW, Chan C, Tan D and Mehta JS:
Incidence and management of suction loss in refractive lenticule
extraction. J Cataract Refract Surg. 40:2002–2010. 2014.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Qiu PJ and Yang YB: Analysis and
management of intraoperative complications during small-incision
lenticule extraction. Int J Ophthalmol. 9:1697–1700.
2016.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Tucker SH and Sood P: Flap complications
from femtosecond laser-assisted in situ keratomileusis. US
Ophthalmic Rev. 12:21–27. 2019.
|
|
43
|
Courtin R, Saad A, Guilbert E, Grise-Dulac
A and Gatinel D: Opaque bubble layer risk factors in femtosecond
laser-assisted LASIK. J Refract Surg. 31:608–612. 2015.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Mastropasqua L, Calienno R, Lanzini M,
Salgari N, De Vecchi S, Mastropasqua R and Nubile M: Opaque bubble
layer incidence in Femtosecond laser-assisted LASIK: Comparison
among different flap design parameters. Int Ophthalmol. 37:635–641.
2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Wu N, Christenbury JG, Dishler JG, Bozkurt
TK, Duel D, Zhang L and Hamilton DR: A technique to reduce
incidence of opaque bubble layer formation during LASIK flap
creation using the VisuMax femtosecond laser. J Refract Surg.
33:584–590. 2017.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Wei CH, Dai QY, Mei LX, Ge Y, Zhang PF and
Song E: Paired eye-control study of unilateral opaque bubble layer
in femtosecond laser assisted laser in situ keratomileusis. Int J
Ophthalmol. 12:654–659. 2019.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Au J and Krueger RR: Interface blood as a
new indication for flap lift after LASIK using the WaveLight FS200
femtosecond laser. J Refract Surg. 30:858–860. 2014.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Vajpayee RB, Balasubramanya R, Rani A,
Sharma N, Titiyal JS and Pandey RM: Visual performance after
interface haemorrhage during laser in situ keratomileusis. Br J
Ophthalmol. 87:717–719. 2003.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Shah DN and Melki S: Complications of
femtosecond-assisted laser in-situ keratomileusis flaps. Semin
Ophthalmol. 29:363–375. 2014.PubMed/NCBI View Article : Google Scholar
|