Introduction
Meniscus is an important crescent-shaped structure
of the knee joint cavity, which has the functions of transferring
load, lubricating joints, distributing stress, stabilizing and
coordinating joint movement (1).
Meniscus injury of knee joints is a type of muscle system injury
that mainly involves degeneration of meniscus morphology (2). The incidence of meniscus injury in a
high-load moving crowd is 20-35% and in elderly patients with
osteoporosis is 30-40% (3). The
distribution of meniscus blood vessels is not abundant and the
repair potential is limited. Only a small part of a meniscus tear
can be repaired. The healing of meniscus is uncertain even under
optimal conditions (4). Surgical
treatment is necessary.
At present, the commonly used surgical method is
meniscus repair surgery in knee joints (5). However, the traditional open new
surgery is traumatic and patients are prone to complications, such
as joint stiffness and joint adhesion after treatment (6). Due to the continuous development of the
minimally invasive amplification technology and the update on the
minimally invasive concept, the minimally invasive surgical
treatment has been applied to various surgical treatments and has
achieved good results (7). In view
of the extensive application of arthroscopic meniscus surgery in
recent years, more evidence-based practical studies are needed to
support meniscus surgery and improve its efficacy. In recent years,
systematic research reports have questioned the efficacy of
arthroscopic knee surgery for middle-aged and elderly patients with
degenerative meniscus tear, with or without knee osteoarthritis
(8,9). In addition, patients often suffer from
persistent pain after partial or complete meniscectomy. Preventing
and reducing the occurrence of postoperative pain is of great
significance to the rehabilitation of patients and the improvement
of their quality of life.
The present study explored the efficacy of
arthroscopic minimally invasive treatment of meniscus injury of
knee joints in middle-aged and elderly patients and the risk
factors related to postoperative pain, in order to provide
reference for the clinical treatment of meniscus injury of knee
joints and reduce postoperative pain.
Patients and methods
Research subjects
From May 2012 to April 2015, 128 patients with
meniscus injury of knee joints, 45-75 year of age, were selected.
After the diagnosis of patients, clinicians put forward treatment
methods and reached a consensus. Altogether 42 patients received
conservative treatment (conservative group), 40 patients received
open knee surgery (open group), and 46 patients received
arthroscopic knee surgery (minimally invasive group). Inclusion
criteria: All patients had obvious meniscus injury symptoms;
patients had grade I or II injury, indicated by MRI of chronic
injury, or their injury in acute stage was small (<5 mm) with
stable edge longitudinal tear and there was no typical bounce and
interlocking clinical symptoms, apart from pain and discomfort of
knee joint; patients had unilateral injury; no meniscus tear,
anterior cruciate ligament or posterior cruciate ligament
reconstruction surgery was performed before treatment; and no
pregnant or nursing women were enrolled. Exclusion criteria:
Patients with other joint injuries, serious infections, tumor,
lower limb fracture within 24 weeks before surgery, bone metabolic
diseases, such as osteoporosis, with contraindications to surgery,
history of drug allergy, and mental and communication disorders.
The study conformed to the Helsinki Declaration, and was approved
by the Ethics Committee of the Quwo County People's Hospital
(Linfen, China). Patients who participated in this research had
complete clinical data. Signed written informed consents were
obtained from the patients and/or guardians.
Treatment methods
Conservative treatment: In the acute stage, splint
or plaster was applied to fix the knee joint and keep at rest
position. During this period, patients were guided to do active
contraction exercise of lower limbs to prevent muscle contracture.
The fixation was continued for 4-6 weeks. After the fixative was
removed, patients were guided to stretch and bend the knee joint
and walk following a rehabilitation training program once every
other day, 20 min/time, for 1 month. If necessary, acupuncture and
massage were used.
Open knee joint surgery: Patients underwent spinal
anesthesia. After anesthesia was accomplished, the skin and
subcutaneous tissue were opened, and the joint cavity was exposed;
the torn edge was removed with a small curette or scalpel to
promote meniscus healing, and the meniscus was sutured. If the
meniscus could not be sutured, the meniscus tissue was removed, the
wound was cleaned, and the surgical incision was closed after there
was no residue.
Arthroscopic knee surgery: Patients were
anesthetized with spinal anesthesia. After anesthesia was
accomplished, transverse incisions of 0.5 cm were made on both
sides of the knee infrapatellar ligament at the approach points and
the suprapatellar bursa of the knee was inflated with 300 ml of
normal saline. The arthroscope was inserted through the
infrapatellar medial-lateral incision, and the meniscus was excised
after the specific damage was confirmed. The damaged meniscus was
repaired with blue forceps, the hyperplastic synovium in the joint
was cleaned with planer and plasma knife, the debris was cleaned
with negative pressure suction, and the meniscus was sutured and
partially or completely removed when necessary. The wound was
cleaned up, the surgical incision was closed after there was no
residue and the wound was bound up under pressure for 1 day. On the
next day after surgery, patients were instructed to get out of bed
and stand up. Generally, patients could get out of bed and move
after 3 days and a proper amount of straight leg-raising exercises
and knee-bending exercises were carried out in order to restore the
function of knee tissue.
Observation indicators
The clinical effects of patients in the three groups
at 24 weeks after treatment were observed. Knee joint activity,
knee injury and osteoarthritis outcome score (KOOS), Lysholm knee
joint function score, VAS pain score and WOMAC score were recorded
before treatment, at 24 weeks after treatment and at 2 years after
treatment. The complications that occurred within 2 years were also
recorded. The related risk factors of postoperative pain were
analyzed.
Efficacy evaluation: Markedly effective: After
treatment, symptoms such as knee joint pain and swelling
disappeared, knee joint function basically returned to normal, and
normal life could be achieved. Effective: After treatment, symptoms
such as knee joint pain and swelling were obviously improved, and
the limitation of knee joint function and activity was obviously
relieved. Ineffective: After treatment, symptoms such as knee joint
pain and swelling had no obvious change, and knee joint function
and activity were limited.
Statistical analysis
SPSS 19.0 software (AsiaAnalytics; formerly SPSS
China) was used for statistical analysis. The measurement data were
expressed as percentages (%) and χ2 test was used for
the comparison of rates. The counting data were expressed as the
mean ± SD. Comparison between the two groups was made using t-test,
between multiple groups was made using analysis of variance
(ANOVA), and comparison of data at different time points in the
same group was made using repeated measures ANOVA. The post hoc
test employed was LSD test. Postoperative pain-related risk factors
were analyzed by logistic regression analysis. P<0.05 was
considered to indicate a statistically significant difference.
Results
General data
There were 42 patients in the conservative group,
including 29 male patients and 13 female patients, 55.93±9.75 years
of age; there were 40 patients in the open group, including 28 male
patients and 12 female patients, 54.33±8.09 years of age; and there
were 46 patients in the minimally invasive group, including 35 male
patients and 11 female patients, 54.39±8.27 years of age. According
to the results, there was no significant difference among the three
groups (P>0.05) in sex, age, body mass index (BMI), course of
the disease and other factors presented in Table I (P>0.05).
 | Table IPatient general characteristics. |
Table I
Patient general characteristics.
| Characteristics | Conservative group
(n=42) | Open group
(n=40) | Minimally invasive
group (n=46) | χ2/F | P-value |
|---|
| Sex (n, %) | | | | 0.639 | 0.726 |
|
Male | 29 (69.05) | 28 (70.00) | 35 (76.09) | | |
|
Female | 13 (30.95) | 12 (30.00) | 11 (23.91) | | |
| Age (years) | 55.93±9.75 | 54.33±8.09 | 54.39±8.27 | 0.456 | 0.635 |
| BMI
(kg/m2) | 21.96±2.63 | 22.14±2.05 | 22.32±2.54 | 0.057 | 0.945 |
| Course of disease
(months) | 5.62±0.28 | 5.58±0.35 | 5.66±0.46 | 0.489 | 0.614 |
| Type of meniscus
injury (n, %) | | | | 11.185 | 0.083 |
|
Degenerative
injury | 8 (19.05) | 5 (12.50) | 7 (15.22) | | |
|
Simple
horizontal tear | 13 (30.95) | 7 (17.50) | 7 (15.22) | | |
|
Complex
horizontal tear | 4 (9.52) | 14 (35.00) | 17 (36.96) | | |
|
Longitudinal
tear of meniscus | 17 (40.48) | 14 (35.00) | 15 (32.61) | | |
| WOMAC index | 110.77±6.10 | 108.97±10.07 | 113.33±8.92 | 2.861 | 0.061 |
| Knee joint (n,
%) | | | | 0.065 | 0.968 |
|
Left | 19 (45.24) | 17 (42.50) | 20 (43.48) | | |
|
Right | 23 (54.76) | 23 (57.50) | 26 (56.52) | | |
| MRI grading (n,
%) | | | | 0.136 | 0.943 |
|
I | 24 (57.14) | 24 (60.00) | 28 (60.87) | | |
|
II | 18 (42.86) | 16 (40.00) | 18 (39.13) | | |
| Articular cartilage
injury (n, %) | | | | 0.762 | 0.683 |
|
Yes | 7 (16.67) | 9 (22.50) | 11 (23.91) | | |
|
No | 35 (83.33) | 31 (77.50) | 35 (76.09) | | |
| Meniscectomy (n,
%) | | | | 1.329 | 0.249 |
|
Yes | | 31 (77.50) | 40 (86.96) | | |
|
No | | 9 (22.50) | 6 (13.04) | | |
| Postoperative
weight bearing (n, %) | | | | 0.870 | 0.647 |
|
<1
week | 6 (14.29) | 8 (20.00) | 6 (13.04) | | |
|
≥1 week | 36 (85.71) | 32 (80.00) | 40 (86.96) | | |
| Cold compress after
surgery (n, %) | | | | 0.923 | 0.309 |
|
Yes | 29 (69.05) | 30 (75.00) | 36 (78.26) | | |
|
No | 13 (30.95) | 10 (25.00) | 10 (21.74) | | |
Clinical efficacy
At 24 weeks after treatment, there were 10 markedly
effective cases, 17 effective cases and 15 ineffective cases in the
conservative group; there were 16 markedly effective cases, 17
effective cases and 7 ineffective cases in the open group; and
there were 22 markedly effective cases, 16 effective cases and 8
ineffective cases in the minimally invasive group. According to the
results, there was no significant difference in efficacy among the
three groups (P>0.05; Table
II).
 | Table IIClinical efficacy (n, %). |
Table II
Clinical efficacy (n, %).
| Efficacy | Conservative group
(n=42) | Open group
(n=40) | Minimally invasive
group (n=46) | χ2 | P-value |
|---|
| Markedly
effective | 10 (23.81) | 16 (40.00) | 22 (47.83) | 5.558 | 0.062 |
| Effective | 17 (40.48) | 17 (42.50) | 16 (34.78) | 0.588 | 0.745 |
| Ineffective | 15 (37.71) | 7 (17.50) | 8 (17.39) | 5.251 | 0.072 |
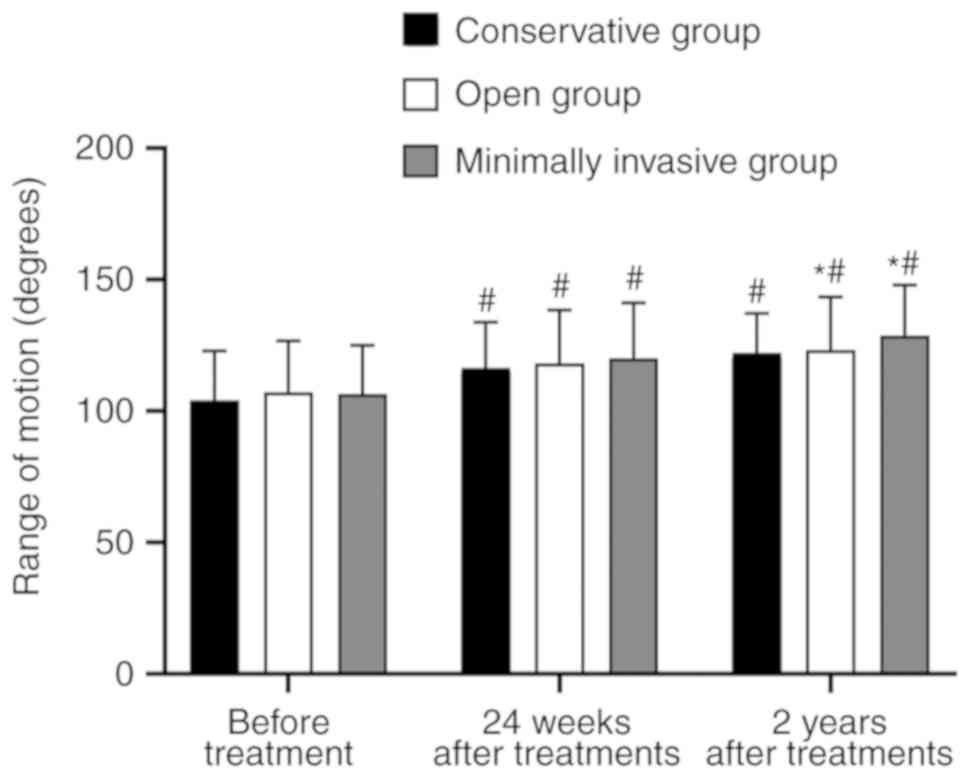
Knee joint activity
There was no significant difference in knee joint
activity among the three groups before treatment or at 24 weeks
after treatment (P>0.05). The knee joint activity of the three
groups at 24 weeks after treatment and at 2 years after treatment
was higher than that before treatment (P<0.05). There was no
significant difference between the knee joint activity at 2 years
after treatment and at 24 weeks after treatment (P>0.05). The
results of the intergroup comparison showed that there was no
significant difference in knee joint activity between the open
group and the minimally invasive group at 2 years after treatment
(P>0.05); however, both were higher than that in the
conservative group (P<0.05; Fig.
1).
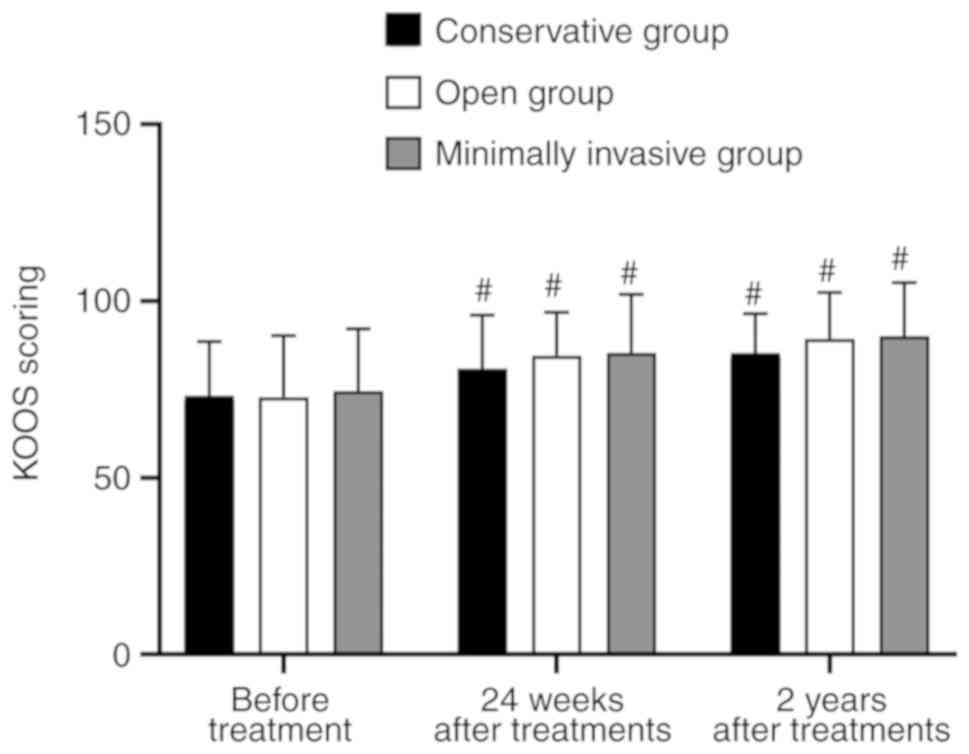
KOOS score
Before treatment, at 24 weeks after treatment and at
2 years after treatment, there was no significant difference in the
KOOS score among the three groups (P>0.05). There was no
significant difference between the KOOS scores at 24 weeks after
treatment and at 2 years after treatment (P>0.05); however, KOOS
score was higher at both time points than that before treatment
(P<0.05; Fig. 2).
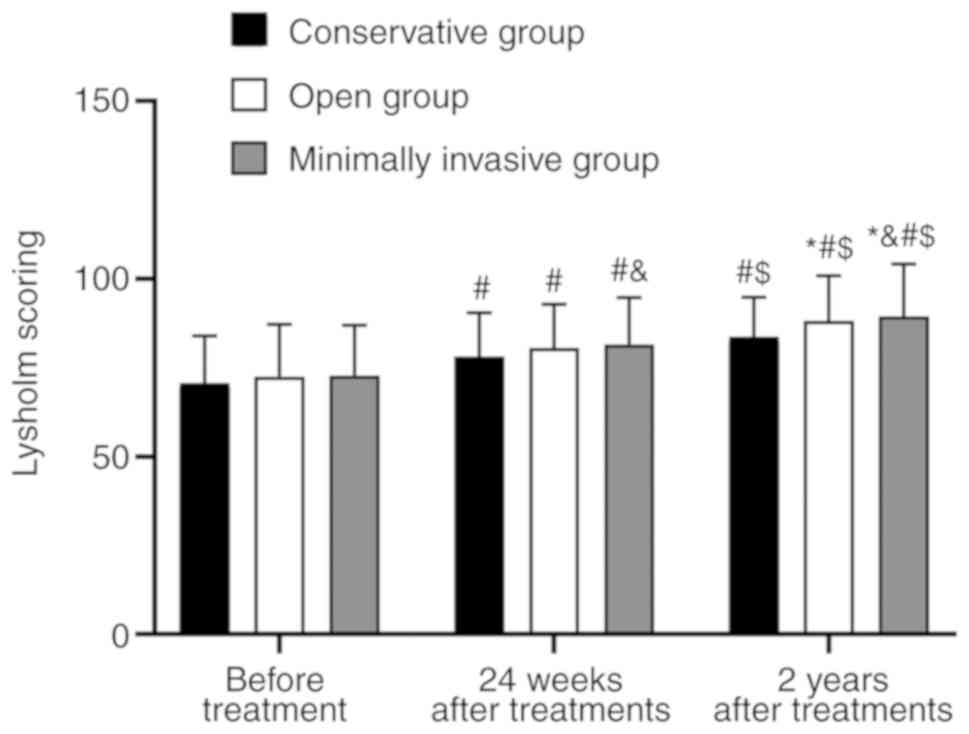
Lysholm score
There was no significant difference in the Lysholm
score among the three groups before treatment or at 24 weeks after
treatment (P>0.05). Lysholm score in the three groups at 24
weeks after treatment and at 2 years after treatment was higher
than that before treatment (P<0.05), and the score at 2 years
after treatment was higher than that at 24 weeks after treatment
(P<0.05). The results of the intergroup comparison showed that
the Lysholm score of patients in the minimally invasive group was
higher than that in the open group (P<0.05) at 24 weeks and 2
years after treatment, and in the open group was higher than that
in the conservative group (P<0.05) at 2 years after treatment
(Fig. 3).
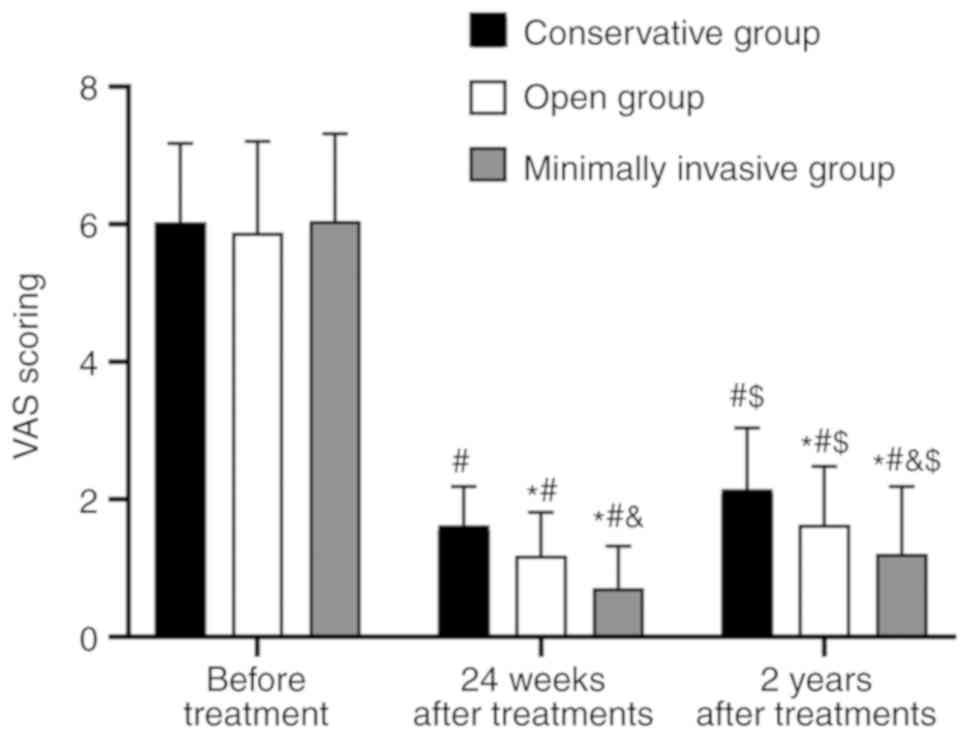
VAS score
The VAS score of patients in the three groups before
treatment showed no significant difference (P>0.05). The VAS
score of patients in the three groups at 24 weeks after treatment
and at 2 years after treatment were lower than that before
treatment (P<0.05); however, the VAS score of patients in the
three groups at 2 years after treatment were higher than that at 24
weeks after treatment (P<0.05). The results of the intergroup
comparison revealed that the VAS score of patients in the minimally
invasive group was lower than that in the open group at 24 weeks
and 2 years after treatment (P<0.05), whereas that in the open
group was lower than that in the conservative group (P<0.05;
Fig. 4).
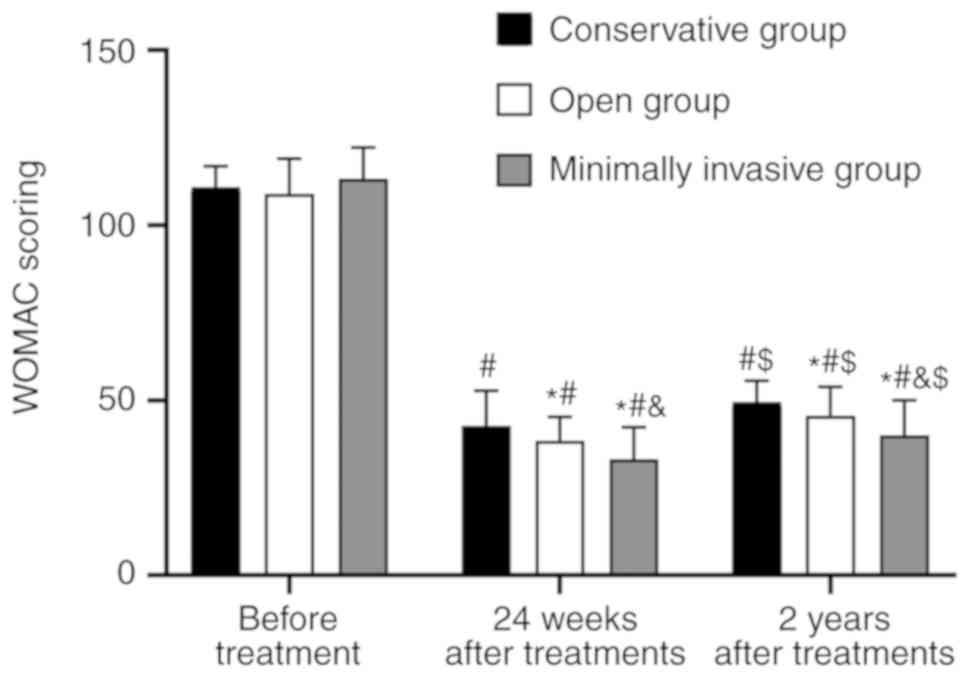
WOMAC score
There was no significant difference in the WOMAC
score among the three groups before treatment (P>0.05). At 24
weeks and 2 years after treatment, the WOMAC scores of patients in
the three groups were lower than those before treatment
(P<0.05); however, at 2 years after treatment, the WOMAC scores
of patients in the three groups were higher than those at 24 weeks
after treatment (P<0.05). Intergroup comparison between groups
showed that the WOMAC scores of patients at 24 weeks and 2 years
after treatment in the minimally invasive group were lower than
those in the open group (P<0.05) and those of the open group
were lower than those in the conservative group (P<0.05;
Fig. 5).
Postoperative pain
Both the open group and the minimally invasive group
achieved primary healing of the surgical incision after surgery; no
obvious complications, such as lower limb venous thrombosis and
incision infection occurred, and no obvious adverse reactions
occurred in the conservative group. The incidence of postoperative
pain was 52.5% (21 cases) in the open group and 26.09% (12 cases)
in the minimally invasive group, which was lower than that in the
open group (P=0.012).
Analysis of risk factors for
postoperative pain
The patients were divided into the pain group and
the painless group according to whether postoperative pain
occurred. Univariate analysis of postoperative pain showed that the
type of meniscus injury, WOMAC score, articular cartilage injury,
time of postoperative weight bearing <1 week, no postoperative
cold compress and open knee joint surgery are risk factors
affecting postoperative pain (Table
III). These factors were used to establish the logistic
multivariate analysis model, and it was revealed that WOMAC score,
articular cartilage injury, time of postoperative weight bearing
<1 week, no postoperative cold compress and open knee joint
surgery are independent risk factors causing postoperative pain
(Tables III and IV).
 | Table IIIUnivariate analysis of postoperative
pain. |
Table III
Univariate analysis of postoperative
pain.
| Variables | Pain (n=33) | Painless
(n=53) |
χ2/t | P-value |
|---|
| Sex (n, %) | | | 0.171 | 0.679 |
|
Male | 25 (75.76) | 38 (71.70) | | |
|
Female | 8 (24.24) | 15 (28.30) | | |
| Age (n, %) | | | 2.153 | 0.142 |
|
<60
years | 8 (24.24) | 21 (39.62) | | |
|
≥60
years | 25 (75.76) | 32 (60.38) | | |
| BMI | 22.32±1.64 | 22.17±1.26 | 0.634 | 0.477 |
| Type of meniscus
injury (n, %) | | | 12.156 | 0.007 |
|
Degenerative
degeneration injury | 10 (30.30) | 2 (3.77) | | |
|
Simple
horizontal tear | 4 (12.12) | 10 (18.87) | | |
|
Complex
horizontal tear | 9 (27.27) | 22 (41.51) | | |
|
Longitudinal
tear of meniscus | 10 (30.30) | 19 (35.85) | | |
| WOMAC score | 46.72±8.15 | 39.02±9.43 | 4.555 | <0.001 |
| Knee joint (n,
%) | | | 0.652 | 0.420 |
|
Left | 16 (48.48) | 21 (39.62) | | |
|
Right | 17 (51.52) | 32 (60.38) | | |
| MRI grading (n,
%) | | | 0.861 | 0.353 |
|
I | 22 (66.67) | 30 (56.6) | | |
|
II | 11 (33.33) | 23 (43.4) | | |
| Articular cartilage
injury (n, %) | | | 7.814 | 0.005 |
|
Yes | 13 (39.39) | 7 (13.21) | | |
|
No | 20 (60.61) | 46 (86.79) | | |
| Meniscectomy (n,
%) | | | 1.720 | 0.190 |
|
Yes | 25 (75.76) | 46 (86.79) | | |
|
No | 8 (24.24) | 7 (13.21) | | |
| Postoperative
weight bearing (n, %) | | | 7.727 | 0.005 |
|
<1
week | 10 (30.30) | 4 (7.55) | | |
|
≥1 week | 23 (69.70) | 49 (92.45) | | |
| Cold compress after
surgery (n, %) | | | 41.855 | <0.001 |
|
Yes | 13 (39.39) | 53 (100.00) | | |
|
No | 20 (60.61) | 0 (0.00) | | |
| Type of operation
(n, %) | | | 6.312 | 0.012 |
|
Open | 21 (63.64) | 19 (35.85) | | |
|
Minimally
invasive | 12 (36.36) | 34 (64.15) | | |
 | Table IVMultivariate analysis. |
Table IV
Multivariate analysis.
| | 95% Cl |
|---|
| Variables | B | S.E. | Wals | df | Sig. | Exp (B) | Upper limit | Lower limit |
|---|
| Type of meniscus
injury | 1.696 | 0.785 | 2.447 | 1 | 0.132 | 1.469 | 0.048 | 1.542 |
| WOMAC score | -6.072 | 1.825 | 6.438 | 1 | 0.015 | 3.125 | 1.446 | 5.738 |
| Articular cartilage
injury | -1.932 | 1.243 | 4.454 | 1 | 0.035 | 4.523 | 2.224 | 9.687 |
| Postoperative
loading | -1.065 | 1.276 | 4.764 | 1 | 0.031 | 3.152 | 1.481 | 8.637 |
| Cold compress after
surgery | 1.749 | 1.518 | 4.972 | 1 | 0.022 | 8.269 | 2.637 | 17.428 |
| Operative
methods | -1.546 | 1.075 | 3.458 | 1 | 0.041 | 5.754 | 1.973 | 12.565 |
Discussion
Meniscus injury of knee joints is one of the most
common joint diseases and one of the important causes of
osteoarthritis (10,11). Repair or resection of meniscus
through surgery is the most frequent means of meniscus injury
treatment (12). Some studies have
reported that there is no significant difference between
conservative and surgical treatment after 1 year (13,14).
Therefore, in the present study the efficacy of conservative and
surgical treatment in meniscus injury were compared, the
application value of the minimally invasive treatment in meniscus
injury surgical treatment was further analyzed and the risk factors
affecting postoperative pain were investigated in order to improve
the effectiveness of surgical treatment.
The results of the present study revealed that there
was no significant difference between the short-term efficacy (24
weeks after treatment) of the surgical treatment and that of the
conservative treatment, and there was no significant difference in
the improvement degree of KOOS, Lysholm, VAS and WOMAC scores. The
analysis of the long-term efficacy results (2 years after
treatment) manifested that the improvement of KOOS, Lysholm and
WOMAC scores of the patients who received surgical treatment was
better than that of the conservative treatment. The reason might be
that some patients had meniscus tear caused by knee joint
degeneration, cartilage damage, or synovitis. In addition, the
patients included in the present study were older and the healing
potential of meniscus was further reduced, so the long-term
efficacy of conservative treatment was lower than that of the
surgical treatment. Moreover, pain was an important criterion for
evaluating the efficacy in this study. Surgical treatment presented
more advantages in improving the pain caused by meniscus injury
(15), which also suggests that the
long-term efficacy of surgical treatment was improved. However, the
VAS score of patients treated conservatively and those treated
surgically was significantly increased after 2 years, suggesting
that the condition of patients might get worse. Thus, further
investigation is needed to determine the relevant causes, which
will be the aim of our future research. Sihvonen et al
(16) reported that after 1 year of
treatment, the efficacy of operation on patients with
osteoarthritis in meniscus tear had no difference compared with
that of the sham operation. Herrlin et al (17) and Katz et al (18) also verified that, during short-term
and medium-term follow-up, the operation treatment of patients did
not show sufficient advantages compared with non-operation
treatments, such as exercise therapy. Therefore, combined with
these aforementioned conclusions, the conservative treatment is
still preferred for patients with meniscus injury of knee
joints.
However, 30% of patients receiving conservative
treatment have failed treatment, and the conversion rate from
non-surgical to surgical treatment ranges from 0 to 35% (19). The efficacy of open surgery and
arthroscopic minimally invasive surgery in meniscus injury was
analyzed in the present study. The short-term and long-term effects
of the two methods were similar. The improvement of Lysholm, VAS
and WOMAC scores of patients who received arthroscopic surgery was
better than that of the open surgery after 2 years of treatment,
and the incidence of postoperative pain in open surgery was
significantly higher than that of arthroscopic surgery. Therefore,
overall analysis showed that arthroscopic surgery was better than
open surgery. In a report of meniscus implantation, the radial
displacement of the bone graft tunnel internal fixation pad under
arthroscopy was significantly smaller than that of the open soft
tissue internal fixation pad (20).
Gu et al (21) also claimed
that arthroscopic surgery for diffuse pigmented villonodular
synovitis of knee joints had the advantages of short operation
time, short hospital stay, less bleeding, high IKDC score and
Lysholm score after surgery. These studies suggested that
arthroscopy was more advantageous than open surgery in knee joint
surgery. Therefore, arthroscopic minimally invasive surgery can be
given priority to patients with meniscus injury who need surgical
treatment after the failure of a conservative treatment.
The risk factors of postoperative pain in patients
were analyzed. Logistic regression analysis indicated that WOMAC
score, articular cartilage injury, time of postoperative weight
bearing <1 week, no postoperative cold compress and open knee
surgery were independent risk factors affecting postoperative pain.
Degenerative meniscus injury is more common in the elderly
patients, who often suffer from different degrees of
osteoarthritis, and residual osteoarthritis is the vital
pain-related risk factor (22). Some
research reports on knee joint injury have shown that the
occurrence of cartilage injury is related to the increase of pain
frequency after anterior and posterior ligament reconstruction
(23,24). In addition, patients with higher BMI
and women are more prone to pain after anterior and posterior
ligament reconstruction (25). The
similarities and differences of these results suggest that our
research has some limitations, such as the small sample size, the
wide age range of patients, and the fact that the meniscus repair
and meniscectomy were not studied in depth. Thus, further research
is needed. In some severe trauma cases, meniscus, cruciate ligament
and lateral collateral ligament can be injured at the same time. In
these cases, it can not be determined whether the pain is caused by
meniscus injury. Therefore, our results and conclusions need more
research and further verification.
In conclusion, arthroscopic minimally invasive
treatment has a good effect on patients with meniscus injury of
knee joints who fail conservative treatment. Articular cartilage
injury, postoperative weight bearing, cold compress and type of
operation are independent risk factors that affect postoperative
pain. Clinicians should bring patient attention to the prevention
of meniscus injury and further improve the efficacy of
treatment.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JX wrote the manuscript, performed the arthroscopic
knee surgery, and interpreted and analyzed the patient data. FB
designed the study, was responsible for the conservative treatment
of the patients, performed the open knee surgery and was
responsible for the analysis and discussion of the data. Both
authors read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the Quwo County People's Hospital (Linfen, China). Patients who
participated in this research had complete clinical data. Signed
written informed consents were obtained from the patients and/or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Naimark MB, Kegel G, O'Donnell T, Lavigne
S, Heveran C and Crawford DC: Knee function assessment in patients
with meniscus injury: A preliminary study of reproducibility,
response to treatment, and correlation with patient-reported
questionnaire outcomes. Orthop J Sports Med.
2(2325967114550987)2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ebrahimi N, Jalaie S, Salsabili N, Ansari
NN and Naghdi S: Knee injury and osteoarthritis outcome score in
patients with isolated meniscus injury; validity and reliability. J
Res Med Sci. 22(55)2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Matsukura Y, Muneta T, Tsuji K, Koga H and
Sekiya I: Mesenchymal stem cells in synovial fluid increase after
meniscus injury. Orthop Relat Res. 472:1357–1364. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rai MF and McNulty AL: Meniscus beyond
mechanics: Using biology to advance our understanding of meniscus
injury and treatment. Connect Tissue Res. 58:221–224.
2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Brophy RH, Gefen AM, Matava MJ, Wright RW
and Smith MV: Understanding of meniscus injury and expectations of
meniscus surgery in patients presenting for orthopaedic care.
Arthroscopy. 31:2295–2300.e5. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Salzler MJ, Lin A, Miller CD, Herold S,
Irrgang JJ and Harner CD: Complications after arthroscopic knee
surgery. Am J Sports Med. 42:292–296. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Norton MJ and Ischy ND: Apparatus and
method for minimally invasive surgery. US Patent 9,820,771(P).
Filed on March 3, 2006; issued November 21, 2017.
|
|
8
|
Khan M, Evaniew N, Bedi A, Ayeni OR and
Bhandari M: Arthroscopic surgery for degenerative tears of the
meniscus: A systematic review and meta-analysis. CMAJ.
186:1057–1064. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Thorlund JB, Juhl CB, Roos EM and
Lohmander LS: Arthroscopic surgery for degenerative knee:
Systematic review and meta-analysis of benefits and harms. BMJ.
350(h2747)2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Meckes JK, Caramés B, Olmer M, Kiosses WB,
Grogan SP, Lotz MK and D'Lima DD: Compromised autophagy precedes
meniscus degeneration and cartilage damage in mice. Osteoarthritis
Cartilage. 25:1880–1889. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kloefkorn HE, Jacobs BY, Loye AM and Allen
KD: Spatiotemporal gait compensations following medial collateral
ligament and medial meniscus injury in the rat: Correlating gait
patterns to joint damage. Arthritis Res Ther.
17(287)2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Vaquero-Picado A and Rodríguez-Merchán EC:
Arthroscopic repair of the meniscus: Surgical management and
clinical outcomes. EFORT Open Rev. 3:584–594. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Howell R, Kumar NS, Patel N and Tom J:
Degenerative meniscus: Pathogenesis, diagnosis, and treatment
options. World J Orthop. 5:597–602. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Krause M, Freudenthaler F, Frosch KH,
Achtnich A, Petersen W and Akoto R: Operative versus conservative
treatment of anterior cruciate ligament rupture. Dtsch Arztebl Int.
115:855–862. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Filbay SR, Andersson C, Ardern C, Gauffin
H and Kvist J: Patient-reported outcome 32 to 37 years following
surgically treated or non-surgically treated acute anterior
cruciate ligament injury. Osteoarthritis Cartilage. 26 (Suppl
1):S52–S53. 2018.
|
|
16
|
Sihvonen R, Paavola M, Malmivaara A, Itälä
A, Joukainen A, Nurmi H, Kalske J and Järvinen TL: Finnish
degenerative meniscal lesion study (FIDELITY) group. Arthroscopic
partial meniscectomy versus sham surgery for a degenerative
meniscal tear. N Engl J Med. 369:2515–2524. 2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Herrlin SV, Wange PO, Lapidus G, Hållander
M, Werner S and Weidenhielm L: Is arthroscopic surgery beneficial
in treating non-traumatic, degenerative medial meniscal tears? A
five year follow-up. Knee Surg Sports Traumatol Arthrosc.
21:358–364. 2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Katz JN, Brophy RH, Chaisson CE, de Chaves
L, Cole BJ, Dahm DL, Donnell-Fink LA, Guermazi A, Haas AK, Jones
MH, et al: Surgery versus physical therapy for a meniscal tear and
osteoarthritis. N Engl J Med. 368:1675–1684. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Beaufils P, Becker R, Kopf S, Matthieu O
and Pujol N: The knee meniscus: Management of traumatic tears and
degenerative lesions. EFORT Open Rev. 2:195–203. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
De Coninck T, Huysse W, Verdonk R,
Verstraete K and Verdonk P: Open versus arthroscopic meniscus
allograft transplantation: Magnetic resonance imaging study of
meniscal radial displacement. Arthroscopy. 29:514–521.
2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gu HF, Zhang SJ, Zhao C, Chen Y and Bi Q:
A comparison of open and arthroscopic surgery for treatment of
diffuse pigmented villonodular synovitis of the knee. Knee Surg
Sports Traumatol Arthrosc. 22:2830–2836. 2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Davis TR, Brady O and Dias JJ: Excision of
the trapezium for osteoarthritis of the trapeziometacarpal joint: A
study of the benefit of ligament reconstruction or tendon
interposition. J Hand Surg Am. 29:1069–1077. 2004.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Fok AW and Yau WP: Delay in ACL
reconstruction is associated with more severe and painful meniscal
and chondral injuries. Knee Surg Sports Traumatol Arthrosc.
21:928–933. 2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Eckstein F, Cotofana S, Wirth W, Nevitt M,
John MR, Dreher D and Frobell BR: Greater rates of cartilage loss
in painful knees than in pain-free knees after adjustment for
radiographic disease stage Data from the Osteoarthritis Initiative.
Arthritis Rheumatol. 63:2257–2267. 2011.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Dunn WR, Spindler KP, Amendola A, Andrish
JT, Kaeding CC, Marx RG, McCarty EC, Parker RD, Harrell FE Jr and
An AQ: Which preoperative factors, including bone bruise, are
associated with knee pain/symptoms at index anterior cruciate
ligament reconstruction (ACLR)? A Multicenter Orthopaedic Outcomes
Network (MOON) ACLR Cohort Study. Am J Sports Med. 38:1778–1787.
2010.PubMed/NCBI View Article : Google Scholar
|