Introduction
With the increased demand for dental implantation,
mental cosmetic surgery and orthognathic surgery, the study of the
anatomical structure of the mandible is receiving increasing
attention. The mandibular canal is an important anatomical
structure in the mandible, and its course follows a specific path.
The mental canal and the incisor nerve canal are separated from the
course of the mandibular canal at the premolar region. The mental
canal forms two backward, upward and outward foramina, which are
called the mental foramina (MFs), usually on each side of the
mandible (1). However, some studies
have found the presence of one or more accessory mental foramina
(AMFs), which are buccal foramina formed by branches of the mental
canal (2). The accessory mental
vascular bundles transmitted from the AMFs are distributed in the
skin and mucous membrane from the mouth to the middle of the lower
lip on the same side, innervating the mucous membrane and the skin
of the corner of the mouth and the cheek (3). These anatomical structures are
associated with rare and previously unexplained complications
related to implant surgery and failure. Therefore, understanding
the anatomical features of the AMFs is beneficial to avoid injury
of the submental nerve and is of great significance for mandibular
implant and alveolar surgery. Currently, there is no large-scale
study on the anatomical characteristics of AMFs in the Chinese Han
population, and research on AMFs has yet to reach a unified
conclusion. Therefore, in this study, cone beam computed tomography
(CBCT) was used to investigate the anatomical data of AMFs in the
Chinese Han population to provide information for clinical implant
surgery at the MF region and chin surgery.
Patients and methods
Patients
This study enrolled 527 patients who received
diagnostic or therapeutic CBCT at the Yantai Yuhuangding Hospital
between January and May 2017, including 256 males and 271 females,
aged between 7-88 years (age distribution shown in Table I). The inclusion criteria were as
follows: Chinese Han ethnicity; no apical lesion near the
mandibular MF; no history of mandibular fracture or orthognathic
surgery; no pathological damage to the mandible, including cysts,
tumors and unerupted teeth. The exclusion criteria were as follows:
presence of mandibular nutrient foramina, and/or discontinuous
buccal foramina of the mandibular nerve canal; unclear image at the
MF region caused by permanent plaque; and poor CBCT image quality
caused by various factors, e.g., patient movement, metal artifacts
and operation error.
 | Table IAge distribution of the patients. |
Table I
Age distribution of the patients.
| Age group
(years) | N |
|---|
| 7-18 | 85 |
| 18-40 | 167 |
| 40-60 | 201 |
| 61-88 | 74 |
The study was approved by the Ethics Committee of
The Affiliated Yantai Yuhuangding Hospital of Qingdao University
(Yantai, China). Signed informed consent was obtained from the
patients and/or their guardians.
Equipment and software
All original CBCT volume data images were collected
by professional radiologists on a Planmeca ProMax 3D Max CBCT
machine (Finland) set at 90 kV, 8 mA, 200 volume pixels and a 110
mm x 130 mm field of vision (FOV). Before scanning, all images were
set at a size of 501x501x501. After the examination, all scanned
images were transmitted to Lenovo M4650-N000 computers with
1600x900 pixel monitor resolution for 3D reconstruction and
analysis with the built-in CBCT software Planmeca Romexis
3.8.3.R.
Measurement of AMF Establishment of
the reference plane
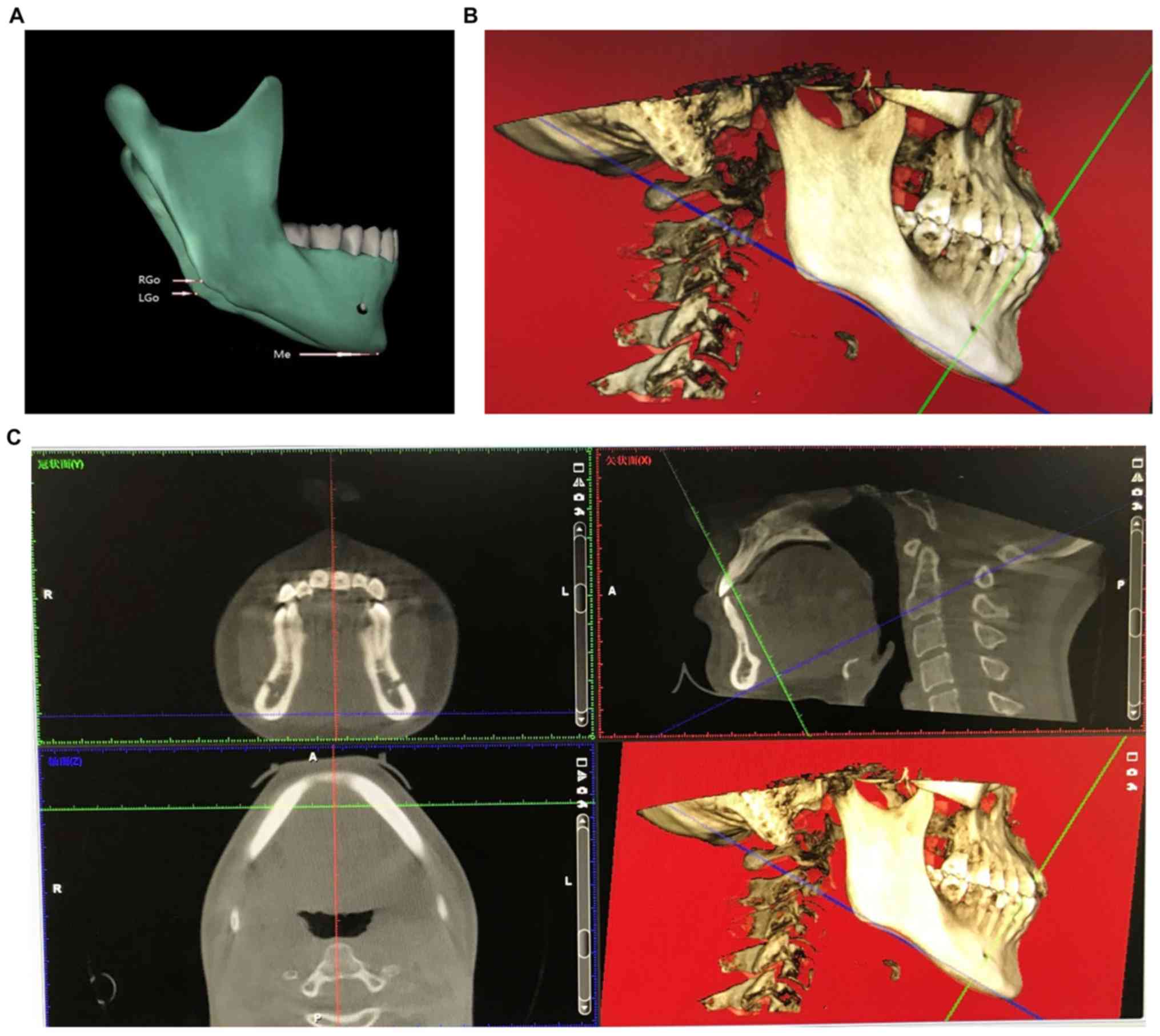
Given the potential differences in the fixed head
positions of patients during CBCT examination, there could be
forward/rearward tilt, sideward tilt and rotation in the CBCT
images; therefore, the original volume data images needed to be
processed before measurement and analysis. The horizontal plane
standard of the volume data images was adjusted to parallel to each
patient's mandibular plane. The reference plane, which was formed
by the lines connecting the menton (Me) and bilateral gonions (Go)
(Fig. 1), was used to adjust the
sagittal, coronal and axial planes of the volume data images to
correct possible oblique head positions of the patients during
image acquisition. The interval between data layers was set to 0.2
mm. The grayscale level, contrast and sharpness of the image were
adjusted to create the desired data images, and the range of
measurements was determined.
Data measurement
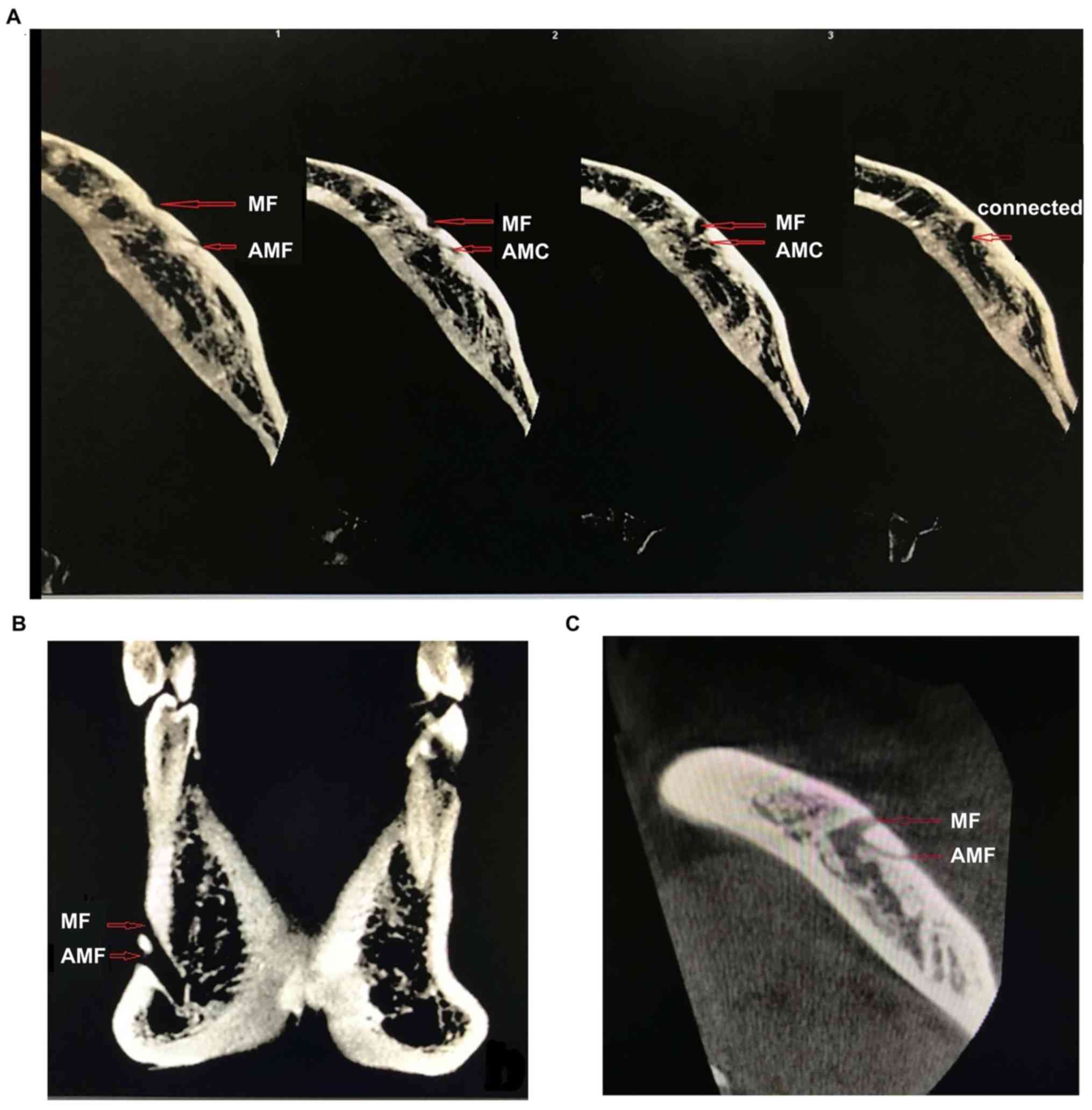
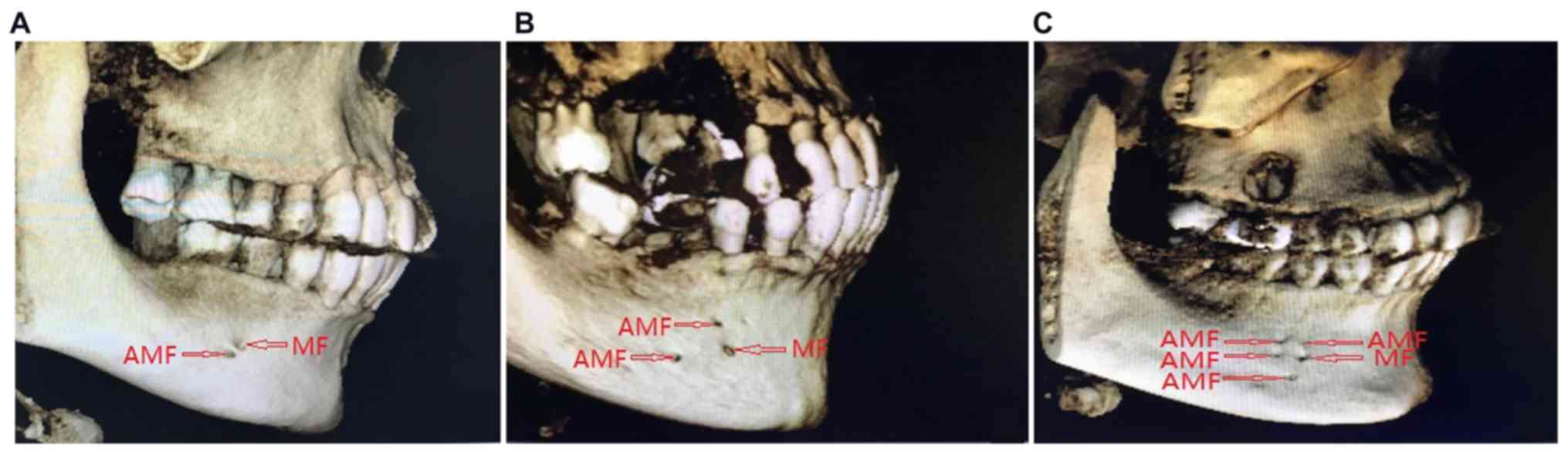
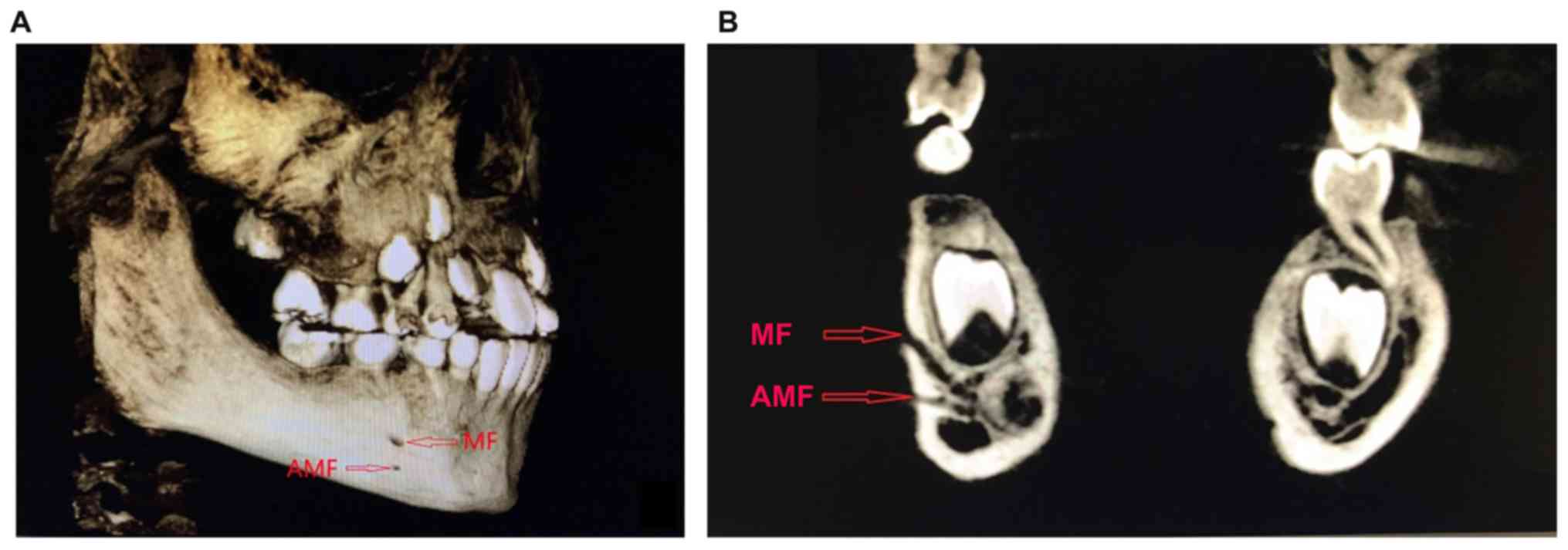
The relatively clear positions of the MFs, AMFs and
adjacent structures on the 3D reconstruction model were used as
references to make fine adjustments on the 2D CBCT images, confirm
AMFs, exclude nutrient foramina, identify the layer (Fig. 2) in which the MFs and AMFs were the
most clear on the mandibular surface and finally capture this CBCT
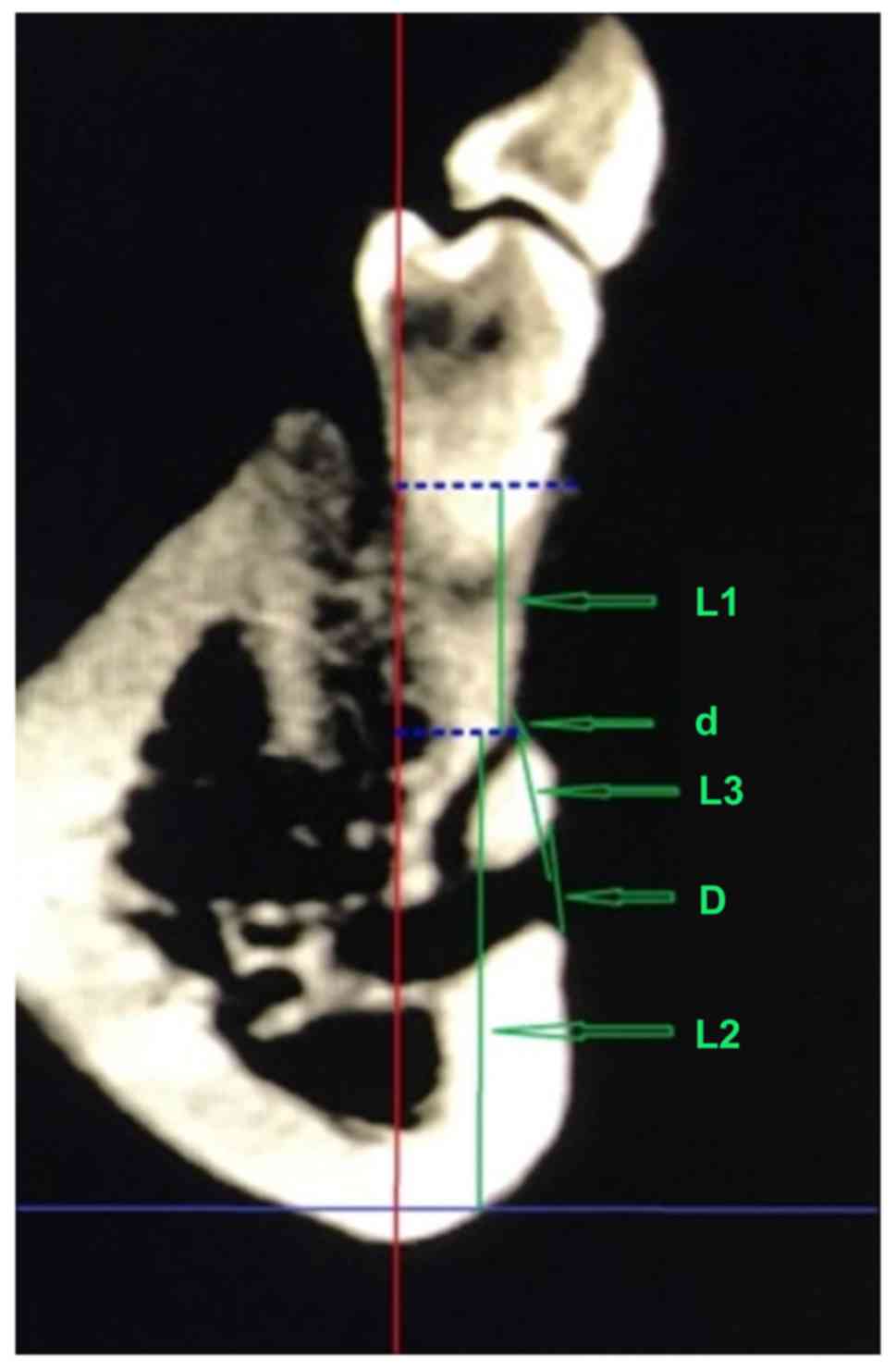
image to measure of the following data (Fig. 3): i) the diameters of the AMFs and
the ipsilateral MF, which evaluated the importance of the
neurovascular bundle in the AMFs; ii) the distances between the
centers of the AMFs and the ipsilateral MF, from the centers of the
AMFs to the alveolar ridge crest (ARC), and from the centers of the
AMFs to the mandibular plane, which were used to confirm the
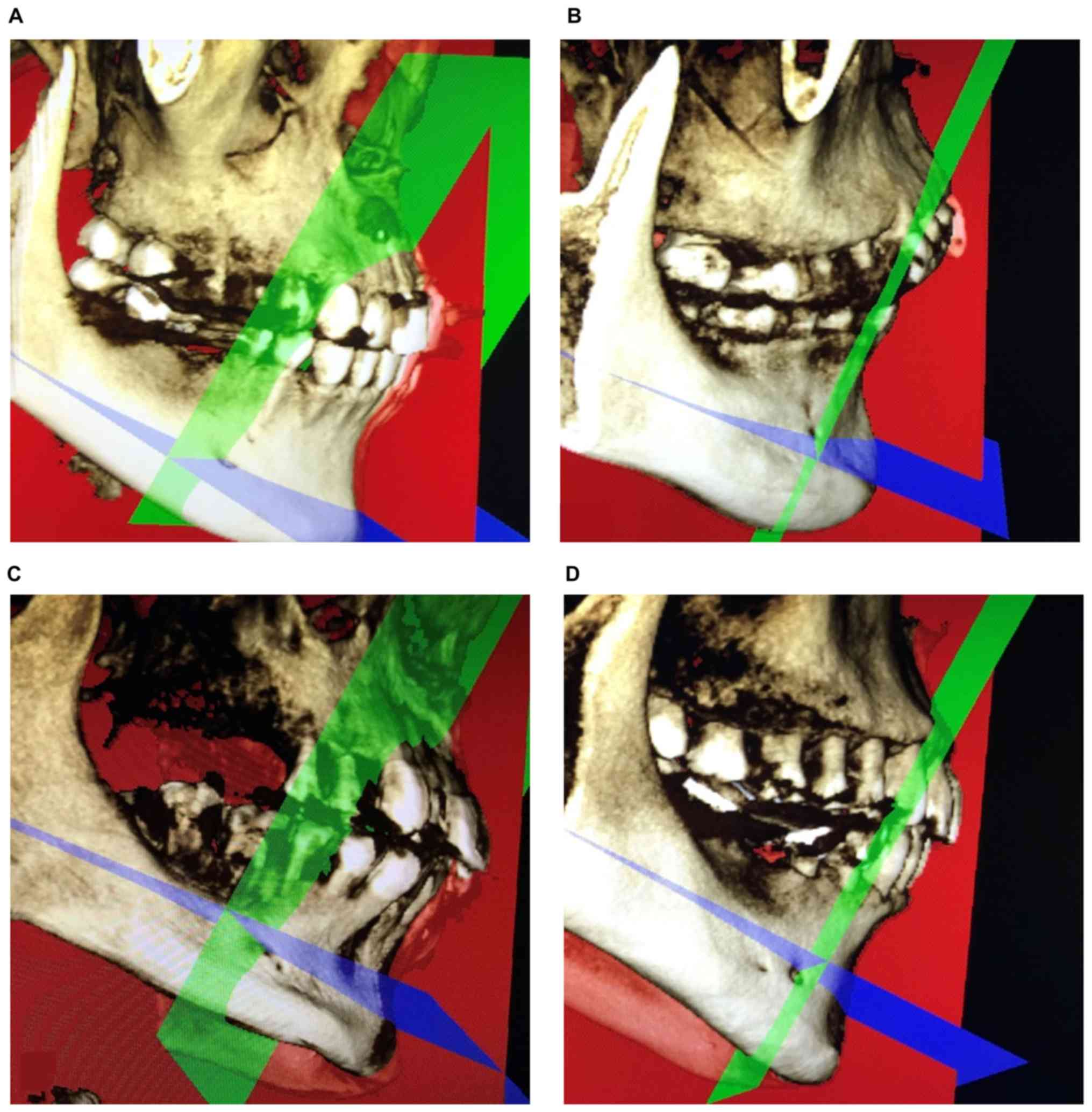
relative position of the AMFs in the mandible; iii) the positional
relationship between the AMFs and the ipsilateral MF: the tangent
of the axial plane, which was parallel to the mandibular plane and
passed through the MFs, on the buccal cortical surface of the
mandible was used as the horizontal axis. The tangent of the
coronal plane, which was vertical to the mandibular plane and
passed through the MFs, on the buccal cortical surface of the
mandible was used as the vertical axis. The two axes accurately
divided the MF region into four quadrants: the mesial-superior,
mesial-inferior, distal-superior and distal-inferior regions
(Fig. 4). These parameters
established a new partitioning for the MFs to precisely distinguish
the positional relationship between the AMFs and the ipsilateral
MF; iv) the positional relationship between the AMFs and adjacent
teeth: below the first premolar, between the first and second
premolar, below the second premolar, between the second premolar
and the first molar, and below or behind the first molar. These
indexes were used to determine the relative positions between the
AMFs and adjacent teeth. All image measurements, data records and
statistical analyses were performed by three experienced
professional dentists, and average values were calculated.
Statistical analysis
Statistical analysis was performed using SPSS 23.0
software (IBM Corp.). Measurement data are shown as the means ±
standard deviations (SDs). Comparison between left and right was
performed using a paired t-test. Correlations between the diameters
of the AMFs and the ipsilateral MF and among the diameters of the
AMFs, the ipsilateral MF and other lengths were analyzed by
Pearson's correlation. Differences with P<0.05 were considered
statistically significant.
Results
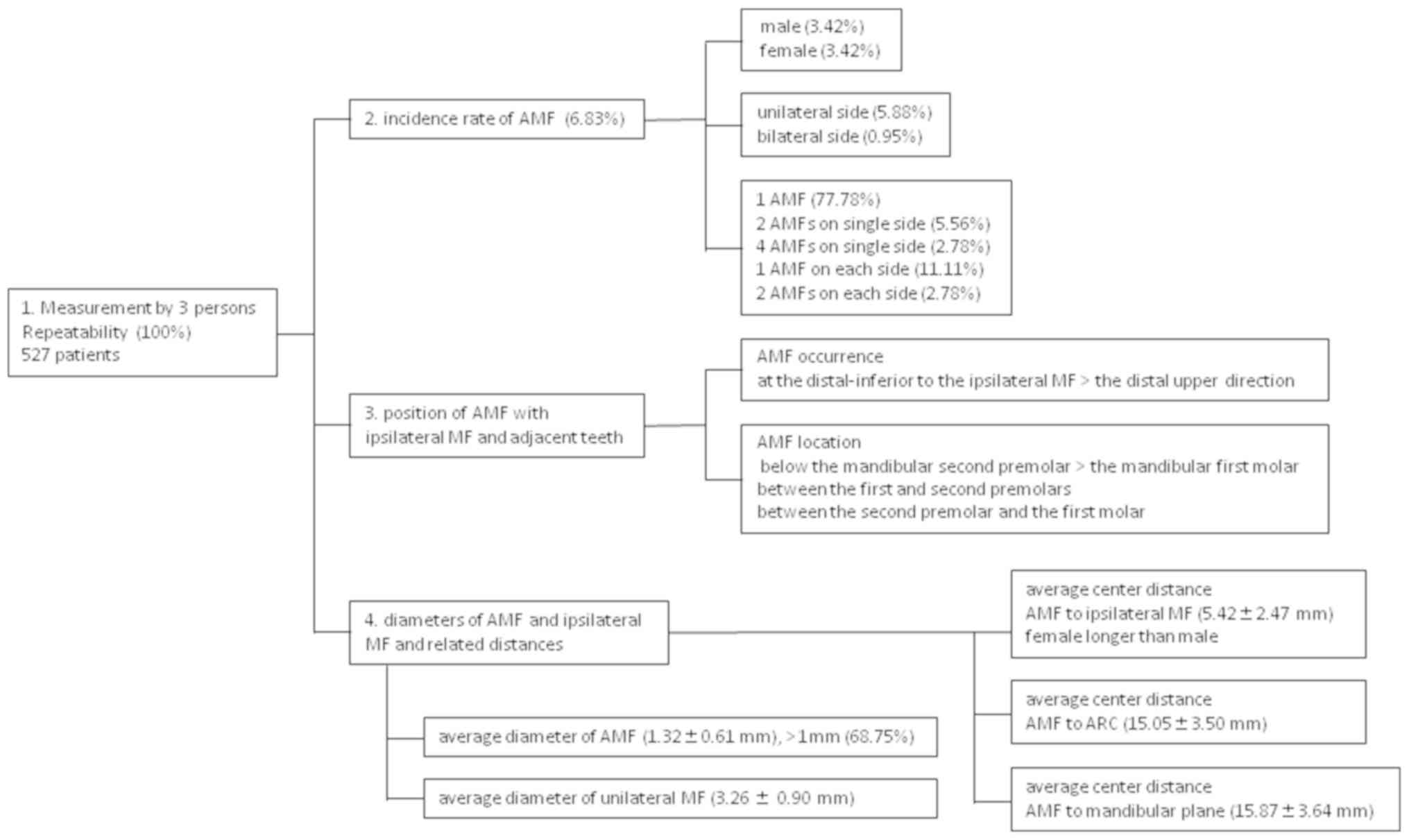
Measurement repeatability
There were 3 observers involved in this study. They
measured the diameters of the AMFs and the ipsilateral MF and the
distance between the centers of the AMFs and the ipsilateral MF.
The repeatability of the measurement of the incidence of AMFs and
of the relative position between the AMFs and the ipsilateral MF or
adjacent teeth was 100%.
Incidence of AMF
Then the incidence of AMFs among patients was
evaluated. The results showed (Table
II) that the incidence of AMFs was 6.83% (36 out of 527
patients), with 18 cases in males (3.42%) and 18 cases in females
(3.42%). There was no significant difference in AMF incidence
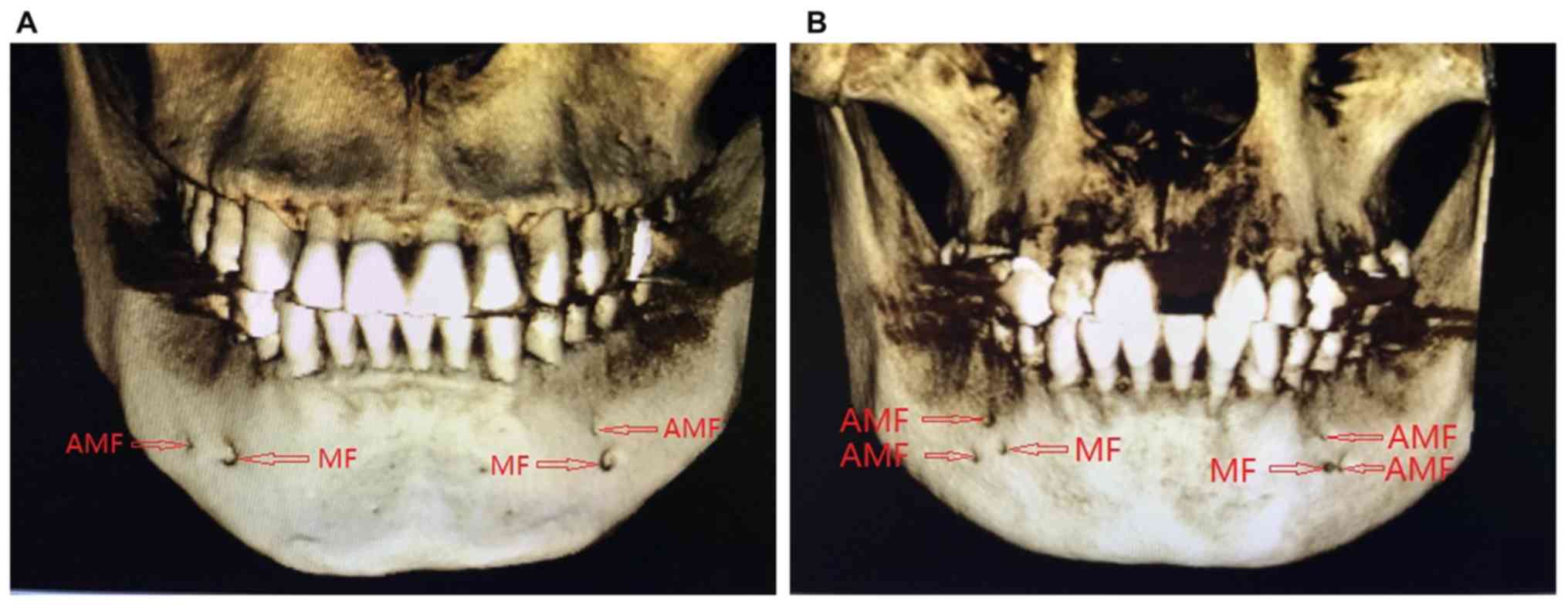
between sexes (P>0.05). AMFs occurred unilaterally in 31 cases
(5.88%) and bilaterally in 5 cases (0.95%). Among the patients
identified with AMFs, the majority (28 patients, 77.78%) had a
single AMF. For the rest, there were 2 cases (5.56%) with 2 AMFs on
one side, 1 case (2.78%) with 4 AMFs on one side (Fig. 5), 4 cases (11.11%) with 1 AMFs on
each side and 1 case (2.78%) with 2 AMFs on each side (Fig. 6). No patient was identified with 3
AMFs unilaterally.
 | Table IIFrequencies of accessary mental
foramen (AMF) (N/n%). |
Table II
Frequencies of accessary mental
foramen (AMF) (N/n%).
| Sex (N) | Single unilateral
AMF | Two unilateral
AMF | Four unilateral
AMF | Single bilateral
AMF | Double bilateral
AMF | Total |
|---|
| Male (256) | 15/5.86 | 1/0.39 | 0 | 2/0.78 | 0 | 18/7.03 |
| Female (271) | 13/4.8 | 1/0.39 | 1/0.37 | 2/0.74 | 1/0.37 | 18/6.64 |
| Total (527) | 28/5.31 | 2/0.38 | 1/0.19 | 4/0.76 | 1/0.19 | 36/6.83 |
The relative position of AMFs with
respect to ipsilateral MFs and adjacent teeth
The relative position of AMFs with respect to
ipsilateral MFs is summarized in Table
III. The relative position of AMFs with respect to adjacent
teeth is summarized in Table IV. In
this study, one case of ipsilateral AMFs was observed in an
8-year-old boy with mixed dentition, in which the AMFs were located
between the first and second deciduous molars (Fig. 7).
 | Table IIIPositions of accessary mental foramen
(AMF) relative to mental foramen (MF). |
Table III
Positions of accessary mental foramen
(AMF) relative to mental foramen (MF).
| Position | Number (n) | Percentage (%) |
|---|
|
Mesial-superior | 6 | 12.50 |
|
Mesial-inferior | 4 | 8.33 |
|
Distal-superior | 11 | 22.91 |
|
Distal-inferior | 27 | 56.25 |
 | Table IVPosition of accessary mental foramen
(AMF) relative to adjacent teeth. |
Table IV
Position of accessary mental foramen
(AMF) relative to adjacent teeth.
| Position | Number (n) | Percentage (%) |
|---|
| Below 2nd
premolar | 16 | 33.33 |
| Below 1st
molar | 12 | 25 |
| Between 1st and 2nd
premolars | 9 | 18.75 |
| Between 2nd
premolar and 1st molar | 9 | 18.75 |
| Between 1st and 2nd
primary molars | 1 | 2.08 |
| Below 1st
premolar | 1 | 2.08 |
Therefore, AMFs most frequently occurred
distal-inferior to the ipsilateral MF, followed by the
distal-superior direction. AMFs were most frequently located below
the mandibular second premolar, less frequently below the
mandibular first molar, and often between the first and second
premolars and between the second premolar and the first molar.
The diameters of AMFs and ipsilateral
MFs
The center distances, the distances from AMFs to the
ARC and to the mandibular plane were statistically analyzed
(Table V), and a correlation
analysis was performed (Table VI).
The average diameter of the 48 AMFs detected was 1.32±0.61 mm, with
33 (68.75%) larger than 1 mm. The average diameter of the
ipsilateral MFs was 3.26±0.90 mm. There was no correlation between
the diameter of the AMFs and that of the ipsilateral MFs. The
average center distance between the AMFs and the ipsilateral MFs
was 5.42±2.47 mm, ranging from 1.89 to 13.21 mm, it was not
correlated with the diameter of the AMFs and was significantly
larger in females than in males (P=0.015). The average distance
from the AMFs to the ARC was 15.05±3.50 mm and to the mandibular
plane was 15.87±3.64 mm. There was no correlation between AMF
diameter and its average distance to the ARC, to the mandibular
plane, or to the average center of the ipsilateral MFs (P>0.05).
Our summary results are presented in Fig. 8.
 | Table VGrouped comparison analysis (mean ±
SD, mm). |
Table V
Grouped comparison analysis (mean ±
SD, mm).
| | Left vs. right | Sex | |
|---|
| Group | Left (25) | Right (23) | P value | Male (21) | Female (27) | P value | Mean ± SD |
|---|
| d | 1.30±0.60 | 1.35±0.64 | 0.868 | 1.27±0.63 | 1.36±0.60 | 0.916 | 1.32±0.61 |
| D | 3.52±0.97 | 2.97±0.75 | 0.365 | 3.32±0.99 | 3.21±0.85 | 0.444 | 3.26±0.90 |
| L1 | 14.53±3.81 | 15.62±3.12 | 0.324 | 14.99±3.78 | 15.10±3.34 | 0.797 | 15.05±3.50 |
| L2 | 16.12±3.55 | 15.52±3.78 | 0.810 | 15.84±4.05 | 15.90±3.37 | 0.260 | 15.87±3.64 |
| L3 | 5.96±2.89 | 4.84±1.08 | 0.071 | 4.75±1.50 | 5.95±2.95 | 0.015 | 5.42±2.47 |
 | Table VICorrelation analysis between diameter
of accessary mental foramen (AMF) or mental foramen (MF) and each
distance. |
Table VI
Correlation analysis between diameter
of accessary mental foramen (AMF) or mental foramen (MF) and each
distance.
| Correlation | Diameter of AMF
(d) | Diameter of MF
(D) |
|---|
| Distance from the
center of AMF to alveolar ridge crest (L1) | 0.835 | 0.738 |
| Distance from the
center of AMF to mandibular plane (L2) | 0.796 | 0.627 |
| Distance from the
center of AMF to the center of ipsilateral MF (L3) | 0.735 | 0.084 |
Discussion
The physiological anatomy and clinical
significance of MF and AMF
The mandibular nerve canal is a complex pipe network
that, in most cases, opens at the MFs as a major route. AMFs are
anatomic variation of MFs (3) that
contain nerves and blood vessels. AMFs have important significance
in surgical procedures, including oral implants, apical surgery,
orthognathic surgery and tumor resection. In recent years, many
studies on AMFs have suggested that the existence of AMFs may lead
to surgical complications such as incomplete anesthesia,
intraoperative hemorrhage and inferior alveolar nerve injury
(4-6).
Boronat López and Peñarrocha Diago suggested that the presence of
AMFs might be one of the causes of local anesthesia failure, which
occurred in 10-20% of block anesthesia of the mental nerve in
patients with accessory mental nerves (7). In addition, damage of the neurovascular
bundle transmitted through AMFs during surgery may lead to
intraoperative bleeding and postoperative numbness of the lower lip
and chin (3). Therefore, it is of
great significance for clinical practice to become familiarized
with the MFs and their anatomical variation.
Current research status of AMFs
Observation method for AMFs
The most accurate and direct observation of the
anatomical structure of the MF region was made on human skull
specimens. Early studies of AMFs were carried out through skull
specimen observation (8). However,
the availability of skull specimens is very limited, and it is
difficult to acquire sufficiently large amounts of observation data
to instruct clinical practice. Therefore, imaging techniques are
typically used by researchers. As the most commonly used imaging
examination method, intraoral apex film and panoramic film benefit
from low costs but cannot accurately reflect the anatomical
structure of the oral cavity due to overlaps and distortions. AMFs
could be found only in individual case reports (9). Spiral CT and CBCT are 3D imaging
techniques that can accurately reflect the anatomical structures of
the mandible and their positional relationships. Studies have
suggested that CBCT has a higher accuracy in the observational
analysis of the MFs and the mandibular nerve anterior ring
(10-13).
The study by Imada et al on the CBCT data and panoramic
radiographs of 100 patients suggested an identification rate of 3%
for AMFs by CBCT, while no AMFs were observed on panoramic
radiographs (14). In addition,
spiral CT suffers from high amounts of radiation, complicated
operation and high economic costs, while CBCT is popular among
dentists due to its high resolution and clear images, the low
amount of radiation it produces and the ability to accurately and
clearly reflect the anatomical structure of the oral cavity. CBCT
has now become an important method for diagnosing AMFs. Therefore,
in this study, CBCT was chosen for the measurement and study of
AMFs.
Analysis of the incidence of AMFs and
related influencing factors
To date, there are no unified diagnostic criteria
for AMFs. Pancer et al proposed that AMFs must be
distinguished from the mandibular canal orifice (15). We believe that only those foramina
whose lumens are connected to the mental tube and that open on the
surface of the mandible can be defined as AMFs. Therefore, this
study adopted strict inclusion criteria to ensure the high
credibility of the data. The incidence of AMFs is inconsistent in
worldwide reports (0.88-10.66%) (3,8,16,17). The
study by Sawyer et al analyzed human skulls and suggested
that the incidence of AMFs was not the same among the populations
of different countries and regions, which was considered to be
related to ethnicity (17). The
incidence of AMFs is 1.4% in white Americans, 5.7% in African
Americans, 1.5% in Asian Indians and 9.0% in Pre-Columbian Nazca
Indians (17). Among the 527
patients in this study, the incidence of AMFs was 6.83%, which is
lower than that of Columbian Indians but higher than that of white
Americans, African Americans and Asian Indians. Hanihara and Ishida
studied 81 human populations from around the world and found that
the frequency of AMFs was the highest in middle Asian and
Subsaharan African populations, followed by European, South Asian,
East Asian, Southeast Asian, Western Australia and South American
populations (18). This study
focused on the Chinese Han population, and strict inclusion and
exclusion criteria were adopted, which excluded buccal foramina of
the branch of the mandibular nerve canal or mandibular incisor
canal and also rolled out nutrient foramina formed by the branches
of the facial artery and the submental artery transmitting through
the mandible. Our results were true and accurate and provide an
anatomical basis for the guidance of clinical operations. Naitoh
et al reported that in 157 patients, 11 had AMFs (7%), in
which 2 cases had bilateral AMFs (19). Katakami et al investigated the
CBCT data from 170 patients and found 16 cases with AMFs (10.7%),
which only included 1 case of bilateral AMFs (3). Oliveira-Santos et al studied the
CBCT data from 285 patients and identified 27 cases with AMFs
(9.4%), including 2 cases of bilateral AMFs (20). Haktanir et al examined 100
patients with multislice spiral CT and found 4% with AMFs (21), while Imada et al used CBCT to
study the same number of patients and found that the frequency of
AMFs was 3%, including 2 cases of unilateral AMFs and 1 case of
bilateral AMFs (14). In summary,
multiple studies have suggested that the incidence of AMFs is
~4-10.7%. The proportion of patients with bilateral AMFs is very
small, accounting for 7.41% of all patients with AMFs (20). Our study investigated 527 patients
and found that the frequency of AMF was 6.83%, including 5 cases of
bilateral AMFs, which constituted 13.89% of all AMFs and 0.95% of
all cases. Our result was not very consistent with the above
studies, which might be explained by differences in ethnicity,
diagnostic standards, research methods and sample sizes. In
addition, the layer thickness could reach 0.2 mm when using CBCT to
observe AMFs, while some other studies used traditional spiral CT,
which may have affected the results.
Sex differences in AMFs
Our study found no difference in the frequency of
AMFs between sexes, which is consistent with most studies worldwide
(9,16,19).
However, the study by Hanihara and Ishida on skulls suggested that
the frequency of AMFs is highest in Asian males (18). Some studies have reported that the
incidence of AMFs is higher in females than in males (22), while other studies suggest otherwise
(17,20). This variance in AMF frequency between
sexes is possibly due to the different patient ethnicities, sample
sizes and research methods.
Relative positions of AMFs with
respect to ipsilateral MFs and adjacent teeth
Internationally, there is no unified standard for
describing the relative location of AMFs with respect to
ipsilateral MFs. Our study used the tangent of the axial plane,
which was parallel to the mandibular plane and passed through the
MFs, on the buccal cortical surface of the mandible as the
horizontal axis and the tangent of the coronal plane, which was
vertical to the mandibular plane and passed through the MFs, on the
buccal cortical surface of the mandible as the vertical axis to
accurately divide the MF region into four quadrants for describing
the relative location of AMF. We believe this partition is clear
and accurate and provides a standard positioning system for
surgery, which can facilitate data comparison. Naitoh et al
found that in the Japanese population, AMFs were mostly located
distal-inferior with respect to the MFs, and the distance between
the MFs and AMFs was 6.3 mm on average (19). Katakami et al observed that 10
out of 17 AMFs (59%) were positioned in the posterior and 8 (47%)
in the inferior area relative to the MFs (3). In this study, AMFs were most frequently
positioned distal-inferior to the ipsilateral MF, accounting for
56.25% of all AMFs, followed by the distal-superior position, which
accounted for 22.91% of all AMFs. This result is consistent with
previous reports, but our partitioning of the MF region could
describe the positional relationship between AMFs and the MFs more
standardly and accurately, which can be beneficial for repeated
comparisons worldwide. The research by Kalender et al found
that in the Turkish population, AMFs were mostly positioned in an
anteroinferior position with respect to the MFs (16). Imada et al suggested that most
AMFs were located between the premolars, either superiorly or
mesially to the MFs (14). These two
reports are in disagreement with our result, which might be due to
the differences in ethnicity and diagnostic criteria.
Based on a study of 150 adult dry human mandibles,
Voljevica et al found that 60.30% of AMFs were located at
the root of the mandibular first premolar and 20.3% were located
between the mandibular first and second premolar (23). As reported by Katakami et al,
mandibular AMFs were frequently observed inferior to the root apex
of the mandibular second premolars (3). In this study, AMFs were mainly located
below the mandibular second premolars (33.33%), which is consistent
with Katakami's study, and, less frequently, inferior to the
mandibular first premolar, between the first and second premolars
and between the second premolar and the first molar, indicating the
diversity of the relative positions between AMFs and ipsilateral
teeth. In clinical practice, attention should be paid to the
presence of AMFs during implant surgery at the MF region and in
chin surgery.
Katakami et al reported that the diameter of
the mandibular AMFs was 1.2 mm (3).
Naitoh et al reported an average size of 1.5 mm for AMFs and
suggested that the frequency of AMFs was unrelated to the diameter
of the MFs after comparing the sizes of the ipsilateral and
contralateral MFs (24). The average
diameter of the AMFs measured in this study was 1.32 mm, with 33
(68.75%) larger than 1 mm. The average diameter of the ipsilateral
MF was 3.26 mm. There was no correlation between the diameter of
the AMFs and ipsilateral MFs, which agreed with the above study.
Our results showed that the size of AMFs is evidently smaller than
that of the MFs, making them easily distinguished. However, another
study (20) reported that in 37% of
the cases, the diameter of AMFs was comparable to or larger than
half of the diameter of the MFs and that the AMF/MF diameter ratio
could reach as high as 0.99, suggesting that the sizes of some AMFs
were close to that of the MFs.
The study by Naitoh et al suggested that the
average distance between AMFs and the ipsilateral MF was 6.3 mm
(19). Our result found an average
distance of 5.42 mm between the AMFs and the MFs, ranging from 1.89
to 13.21 mm, which was unrelated to the diameters of the AMFs.
These data were smaller than those in the Naitoh study but larger
than those in the study by Sisman et al (3.56 mm) (25). Clinically, 2 mm above the MF is
generally considered the safety zone for implantation. Considering
that the average distance of 5.42 mm between the AMFs and the MFs
was far beyond the 2 mm range, we suggest that this safety distance
is debatable, which is in agreement with the opinion of Al-Mahalawy
et al (26). The safety
distance should be set in consideration of the presence of AMFs.
The difference between our data and previous results can likely be
ascribed to the different imaging techniques, inclusion criteria or
other factors. As this study enrolled mainly individuals from the
Chinese Han population within Shandong Province, the results of our
survey might only apply to the population in the survey area, and a
larger sample size and survey region may be required for future
study.
Distance from the AMFs to the ARC and
mandibular plane
The ARC is the highest point of the alveolar bone
and is visible in the mouth. Measuring the distance between the
AMFs and the ARC could indirectly facilitate the determination of
the position of the MFs and AMFs for avoiding damage to blood
vessels and nerves. The mandibular plane is a standard plane
commonly used in stomatology. In this study, we used the mandibular
plane rather than the mandibular margin, which is often used in
China, as the measurement plane, which was beneficial for the
repeatability of the experiment and for making comparisons with
international data. Currently, there are few reports of
measurements of the distances from the AMFs to the ARC and
mandibular plane. This is likely due to the lack of sufficient
attention to the anatomical variations in the AMFs. Our results
showed that the average distance between the AMFs and the ARC was
15.08 mm and that between the AMF and the mandibular plane was
15.87 mm. The shortest distance between an AMF and the ARC was 6.80
mm, in which the AMF was larger than 1 mm. Therefore, during an
operation, damage should be avoided to prevent hemorrhage or
numbness. In addition, in one's lifetime, the alveolar bone is
constantly rebuilt and maintains the ability to dynamically change.
Our result could not dynamically reflect the distances between the
AMFs and the ARC, which was a limitation of this study.
In conclusion, first in regards to the confirmation
of AMFs, nutrient foramina around the MFs were excluded. An AMF was
defined as an opening of the branch of the mental canal on the
outer surface of the mandible. Second, the reference plane for
measuring AMFs was suggested to be the mandibular plane to increase
the repeatability and accuracy of the experiment. Third in regard
to the standard for determining the relative positions of the AMFs
and the MFs, the tangent of the axial plane, which was parallel to
the mandibular plane and passed through the MFs, on the buccal
cortical surface of the mandible was used as the horizontal axis.
The tangent of the coronal plane, which was vertical to the
mandibular plane and passed through the MFs, on the buccal cortical
surface of the mandible was used as the vertical axis. The two axes
accurately divided the MF region into four quadrants. This
internationally unified standard was beneficial to ensuring high
compatibility among the data.
Finally, based on our results, we propose that for
implant surgeries, the safety region of 2 mm above the MFs should
be reevaluated. If CBCT shows that an AMF is located outside the
safety range of 2 mm from the ipsilateral MF and that its diameter
is larger than 1 mm, indicating that the neurovascular bundle
through the AMF is relatively large, this area should be avoided
during operation to prevent excessive bleeding or numbness caused
by surgical trauma. On the other hand, an AMF smaller than 1 mm as
seen on CBCT indicates a smaller neurovascular bundle through the
AMF. In such cases, surgical trauma is unlikely to cause serious
consequences. Therefore, a standard safe distance of 2 mm can still
be applied. CBCT examination is recommended before the operation to
identify important anatomical structures around the MF region and
their variations and to set the safety region on an individual
basis.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LX wrote the manuscript. LX and WP were responsible
for establishing the reference plane and performing the data
measurement. HB and XH contributed to the observation index
analysis. The final version was read and adopted by all the
authors. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The Affiliated Yantai Yuhuangding Hospital of Qingdao University
(Yantai, China). Patients who participated in this study had
complete clinical data. Signed informed consent was obtained from
the patients and/or guardians for the publication of any associated
data and accompanying images.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Koutroumpas DC and Koletsi-Kounari H:
Galen on dental anatomy and physiology. J Hist Dent. 60:37–49.
2012.PubMed/NCBI
|
|
2
|
da Silva Ramos Fernandes LM, Capelozza AL
and Rubira-Bullen IR: Absence and hypoplasia of the mental foramen
detected in CBCT images: A case report. Surg Radiol Anat.
33:731–734. 2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Katakami K, Mishima A, Shiozaki K, Shimoda
S, Hamada Y and Kobayashi K: Characteristics of accessory mental
foramina observed on limited cone-beam computed tomography images.
J Endod. 34:1441–1445. 2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Muinelo-Lorenzo J, Suárez-Quintanilla JA,
Fernández-Alonso A, Varela-Mallou J and Suárez-Cunqueiro MM:
Anatomical characteristics and visibility of mental foramen and
accessory mental foramen: Panoramic radiography vs. cone beam CT.
Med Oral Patol Oral Cir Bucal. 20:e707–e714. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Torres MG, Valverde LF, Vidal MT and
Crusoé-Rebello IM: Accessory mental foramen: A rare anatomical
variation detected by cone-beam computed tomography. Imaging Sci
Dent. 45:61–65. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Cantekin K and Şekerci A: Evaluation of
the accessory mental foramen in a pediatric population using
cone-beam computed tomography. J Clin Pediatr Dent. 39:85–89.
2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Boronat López A and Peñarrocha Diago M:
Failure of locoregional anesthesia in dental practice. Review of
the literature. Med Oral Patol Oral Cir Bucal. 11:E510–E513.
2006.PubMed/NCBI
|
|
8
|
Zografos J and Mutzuri A: Incidence of
double mental foramen in a sample of Greek population.
Odontostomatol Proodos. 43:521–523. 1989.PubMed/NCBI(In Greek).
|
|
9
|
Cağirankaya LB and Kansu H: An accessory
mental foramen: A case report. J Contemp Dent Pract. 9:98–104.
2008.PubMed/NCBI
|
|
10
|
Kamburoğlu K, Kiliç C, Ozen T and Yüksel
SP: Measurements of mandibular canal region obtained by cone-beam
computed tomography: A cadaveric study. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 107:e34–e42. 2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Matherne RP, Angelopoulos C, Kulild JC and
Tira D: Use of cone-beam computed tomography to identify root canal
systems in vitro. J Endod. 34:87–89. 2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Vujanovic-Eskenazi A, Valero-James JM,
Sánchez-Garcés MA and Gay-Escoda C: A retrospective radiographic
evaluation of the anterior loop of the mental nerve: Comparison
between panoramic radiography and cone beam computerized
tomography. Med Oral Patol Oral Cir Bucal. 20:e239–e245.
2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Santana RR, Lozada J, Kleinman A, Al-Ardah
A, Herford A and Chen JW: Accuracy of cone beam computerized
tomography and a three-dimensional stereolithographic model in
identifying the anterior loop of the mental nerve: A study on
cadavers. J Oral Implantol. 38:668–676. 2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Imada TS, Fernandes LM, Centurion BS, de
Oliveira-Santos C, Honório HM and Rubira-Bullen IR: Accessory
mental foramina: Prevalence, position and diameter assessed by
cone-beam computed tomography and digital panoramic radiographs.
Clin Oral Implants Res. 25:e94–e99. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Pancer B, Garaicoa-Pazmiño C and Bashutski
JD: Accessory mandibular foramen during dental implant placement:
Case report and review of literature. Implant Dent. 23:116–124.
2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kalender A, Orhan K and Aksoy U:
Evaluation of the mental foramen and accessory mental foramen in
Turkish patients using cone-beam computed tomography images
reconstructed from a volumetric rendering program. Clin Anat.
25:584–592. 2012.PubMed/NCBI View
Article : Google Scholar
|
|
17
|
Sawyer DR, Kiely ML and Pyle MA: The
frequency of accessory mental foramina in four ethnic groups. Arch
Oral Biol. 43:417–420. 1998.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hanihara T and Ishida H: Frequency
variations of discrete cranial traits in major human populations
IV. Vessel and nerve related variations. J Anat. 199:273–287.
2001.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Naitoh M, Hiraiwa Y, Aimiya H, Gotoh K and
Ariji E: Accessory mental foramen assessment using cone-beam
computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 107:289–294. 2009.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Oliveira-Santos C, Souza PH, De Azambuja
Berti-Couto S, Stinkens L, Moyaert K, Van Assche N and Jacobs R:
Characterisation of additional mental foramina through cone beam
computed tomography. J Oral Rehabil. 38:595–600. 2011.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Haktanir A, Ilgaz K and Turhan-Haktanir N:
Evaluation of mental foramina in adult living crania with MDCT.
Surg Radiol Anat. 32:351–356. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kieser J, Kuzmanovic D, Payne A, Dennison
J and Herbison P: Patterns of emergence of the human mental nerve.
Arch Oral Biol. 47:743–747. 2002.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Voljevica A, Talović E and Hasanović A:
Morphological and morphometric analysis of the shape, position,
number and size of mental foramen on human mandibles. Acta Med
Acad. 44:31–38. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Naitoh M, Yoshida K, Nakahara K, Gotoh K
and Ariji E: Demonstration of the accessory mental foramen using
rotational panoramic radiography compared with cone-beam computed
tomography. Clin Oral Implants Res. 22:1415–1419. 2011.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Sisman Y, Sahman H, Sekerci A, Tokmak TT
and Aksu Y and E: Detection and characterization of the mandibular
accessory buccal foramen using CT. Dentomaxillofac Radiol.
41:558–563. 2012.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Al-Mahalawy H, Al-Aithan H, Al-Kari B,
Al-Jandan B and Shujaat S: Determination of the position of mental
foramen and frequency of anterior loop in Saudi population. A
retrospective CBCT study. Saudi Dent J. 29:29–35. 2017.PubMed/NCBI View Article : Google Scholar
|