Introduction
Pneumonia is a persistent and pervasive disease
(1). Despite not usually being
fatal, the effects of the disease can be severe; for example, 25%
of American pediatric patients (age, 1-6 years) hospitalized for
pneumonia were admitted to intensive care units (ICUs), with 33.3%
of pediatric ICU patients requiring mechanical ventilation in 2015
(2,3). Therefore, identifying the molecular
mechanisms mediating severe pneumonia is important to reduce the
disease burden.
MicroRNAs (miRNAs/miRs) are endogenous,
evolutionarily conserved, non-coding RNAs that are ~22 nucleotides
in length. miRNAs post-transcriptionally regulate gene expression
by targeting and binding to the 3'-untranslated region (UTR) of
target mRNAs (4-7).
In mammals, miRNAs are associated with various diseases, including
cancer (8) and viral infections
(9), and have been identified as
biomarkers for pneumonia (10).
Moreover, numerous miRNAs are involved in the progression of
pneumonia; miR-302e reduced inflammation during infantile pneumonia
via the NF-κB signaling pathway (11), miR-146a-5p regulated
lipopolysaccharide (LPS)-induced cell apoptosis and inflammation
via CC motif chemokine ligand 5 during acute pneumonia (12), and miR-370-3p modulated LPS-induced
cell apoptosis and inflammation via toll like receptor 4 during
acute pneumonia (13). It has also
been reported that miR-127 may reduce lung inflammation by
targeting immunoglobulin (Ig)G Fcγ receptor I (14). Additionally, miR-127-5p expression,
which is reduced in bronchoalveolar lavage fluid, may serve as a
biomarker for the diagnosis of the disease (15). The present study aimed to investigate
the function of miR-127-5p during severe pneumonia, as well as the
potential molecules regulated by miR-127-5p, to identify a
potential therapeutic target for severe pneumonia.
Materials and methods
Cell culture
Ana-1 murine macrophages were obtained from The Cell
Bank of Type Culture Collection of the Chinese Academy of Sciences
and cultured in RPMI-1640 medium (Gibco; Thermo Fisher Scientific,
Inc.) supplemented with 10% low endotoxin fetal calf serum
(Hyclone; GE Healthcare Life Sciences) and 1%
penicillin-streptomycin (Gibco; Thermo Fisher Scientific, Inc.) at
37˚C with 95% humidity and 5% CO2.
An in vitro model of pneumonia was induced by
treating Ana-1 murine macrophages with 0.1 µg/ml LPS
(Sigma-Aldrich; Merck KGaA) at 37˚C for 24 h (16). Subsequently, cells were randomly
divided into the following four groups: Control (treated with
saline), LPS, and/or LPS + miR-127-5p mimic and/or LPS + miR-127-5p
mimic + pcDNA3.1-TRAF1.
Cell transfection
miR-NC mimic (5'-UAGUCUCGGGAGAC UCACUACC-3') and
miR-127-5p mimic (5'-UAGUCUCGGG AGACUCGAAGUC-3') were obtained from
Guangzhou Ribobio Co., Ltd. miR-NC mimic (200 nM) or miR-127-5p
mimic (200 nM) were mixed with Lipofectamine® 2000
reagent (Invitrogen; Thermo Fisher Scientific, Inc.) and incubated
for 15 min at room temperature. Subsequently, Ana-1 murine
macrophages were seeded (1x106 cells/well) into 6-well
plates and the mimic-Lipofectamine mix was added to each well.
TRAF1 was amplified from Ana-1 murine macrophages by
PCR at thermocycling conditions of 95˚C for 15 min, followed by 30
cycles of denaturation at 98˚C for 10 sec, annealing at 55˚C for 30
sec and extension at 72˚C for 30 sec using PrimeSTAR Max DNA
Polymerase (Takara Bio, Inc.) and then cloned into pcDNA3.1 (Thermo
Fisher Scientific, Inc.) to generate pcDNA3.1 TRAF1. A total of 2
µg pcDNA3.1 TRAF1 and pcDNA3.1 (control) were transfected into
Ana-1 murine macrophages (1x105) using
Lipofectamine® 2000 reagent (Thermo Fisher Scientific,
Inc.).
Following incubation for 48 h at 37˚C, transfection
efficiency was determined by reverse transcription-quantitative PCR
(RT-qPCR). All experiments were performed 48 h
post-transfection.
ELISA
Ana-1 murine macrophages (5x105
cells/well) were plated into 24-well plates and incubated at 37˚C
with 95% humidity and 5% CO2 overnight. The protein
levels of TNF-α (cat. no. BMS607-3; Invitrogen; Thermo Fisher
Scientific, Inc.), IL-6 (cat. no. RAB0308; Sigma-Aldrich; Merck
KGaA) and IL-1β (cat. no. RAB0274; Sigma-Aldrich; Merck KGaA) in
the cell media were assessed using ELISA kits, according to the
manufacturer's protocol.
RT-qPCR
Total RNA was extracted from Ana-1 murine
macrophages using TRIzol® (Invitrogen; Thermo Fisher
Scientific, Inc.) and mirVana kits (Applied Biosystems; Thermo
Fisher Scientific, Inc.) for the detection of RNA and miRNA,
respectively, according to the manufacturer's protocol. The TaqMan
Gene Expression assay and TaqMan MicroRNA Reverse Transcription
kits (Applied Biosystems; Thermo Fisher Scientific, Inc.) were used
to reverse transcribe RNA(RT temperature protocols: (50˚C for 2
min, 95˚C for 10 min, followed with 95˚C for 15 sec and 60˚C for 1
min for 40 cycles) and miRNA (RT temperature protocols: 16˚C for 30
min, 42˚C for 30 min and 85˚C for 5 min) to cDNA, respectively,
according to the manufacturer's protocol. Subsequently, qPCR was
performed using a SYBR Green qPCR Master Mix kit (Takara
Biotechnology Co., Ltd) the StepOnePlus™ Real-Time PCR system
(Applied Biosystems; Thermo Fisher Scientific, Inc.) with the
following thermocycling conditions: initial denaturation at 95˚C
for 2 min, 35 cycles of 95˚C for 15 sec and 64˚C for 30 sec. The
kit and the system were used according to the manufacturer's
protocol. The following primer pairs were used for qPCR:
miR-127-5p, forward 5'-CT CTTCAAGCTCCAAACCAAAC-3', reverse
5'-GTATCC ACCAGAACCACCAGG-3'; IL-1β, forward 5'-GAAAGC
TCTCCACCTAATG-3', reverse 5'-GCCGTCTTTCATTACA CAGG-3'; IL-6,
forward 5'-CCAGAGATACAAAGAAATG ATGG-3', reverse
5'-ACTCCAGAAGACCAGAGGAAA-3'; TNF-α, forward
5'-TCTCATCAGTTCTATGGCCC-3', reverse 5'-GGGATGAGACAAGGTACAAC-3'; U6,
forward 5'-AT TGGAACGATACAGAGAAGATT 3', reverse 5'-GGAACGCT
TCACGAATTTG 3'; and GAPDH, forward 5'-TGATGACA TCAAGAAGGTGGTGAAG-3'
and reverse 5'-TCCTTGGA GGCCATGTGGGCCAT-3'. mRNA and miRNA
expression levels were quantified using the 2-ΔΔCq
method (17). mRNA and miRNA
expression levels were normalized to the internal reference genes
GAPDH and U6, respectively.
Western blotting
Total protein was extracted from Ana-1 murine
macrophages using RIPA buffer (Roche Diagnostics) and protein
concentrations were determined using BCA (Beyotime Institute of
Biotechnology). Proteins were then separated via 8% SDS-PAGE and
transferred to PVDF membranes (EMD Millipore), which were
subsequently blocked with 5% non-fat milk at room temperature for 1
h. The membranes were incubated at 4˚C overnight with primary
antibodies targeted against the following: GAPDH (cat no. 5174;
1:1,000), TRAF1 (cat no. 4710; 1:1,000), phosphorylated (p)-AKT
(cat no. 4060; 1:1,000), AKT (cat no. 4691; 1:1000), p-p65 (cat no.
3033; 1:1,000) and p65 (cat no. 8242; 1:1,000; all, Cell Signaling
Technology, Inc.). Following primary antibody incubation, the
membranes were incubated with an anti-rabbit horseradish
peroxidase-conjugated IgG secondary antibody (cat no. 7047;
1:2,000; Cell Signaling Technology, Inc.) at room temperature for 2
h. Protein bands were visualized using an enhanced
chemiluminescence detection system (PerkinElmer, Inc.). Protein
expression was semi-quantified using Quantity One software (version
4.62; Bio-Rad Laboratories, Inc.) with GAPDH as the loading
control.
Dual luciferase reporter assay
TargetScan (version 7.1; www.targetscan.org/vert_71) was used to predict the
binding site between miR-127-5p and the 3'-UTR of TRAF1.
The wild-type (WT) 3'-UTR of TRAF1, containing
complementary sequences for the seed sequence of miR-127-5p, was
amplified from Ana-1 murine macrophages via PCR with the
thermocycling conditions of 95˚C for 15 min, followed by 30 cycles
of denaturation at 98˚C for 10 sec, annealing at 55˚C for 30 sec
and extension at 72˚C for 30 sec via PrimeSTAR Max DNA Polymerase
(Takara Bio, Inc.) and cloned into the psi-CHECK-2 vector (Promega
Corporation). The mutant (MUT) 3'-UTR of TRAF1 was constructed
using the QuikChange II Site-Directed Mutagenesis kit (Agilent
Technologies, Inc.), according to the manufacturer's protocol.
Ana-1 murine macrophages (1x104
cells/well) were seeded into 96-well plates and transfected with
psi-CHECK-2-TRAF1-WT-3'UTR (400 ng) or psi-CHECK-2-TRAF1-MUT-3'-UTR
(400 ng) and miR-127-5p mimic (50 ng) or miR-NC mimic (50 ng) using
Lipofectamine® 2000 reagent (Invitrogen; Thermo Fisher
Scientific, Inc.). Following incubation for 48 h at 37˚C,
luciferase activities were determined using a Dual-Luciferase assay
system (Promega Corporation), according to the manufacturer's
protocol. Firefly luciferase activity was normalized to
Renilla luciferase activity.
Statistical analysis
Statistical analyses were performed using GraphPad
Prism software (version 5.04; GraphPad Software, Inc.). Data are
expressed as the mean ± standard error of the mean. Differences
between two groups were analyzed using the unpaired Student's
t-test. Differences among four groups were analyzed using one-way
ANOVA followed by Bonferroni's post hoc test. P<0.05 was
considered to indicate a statistically significant difference.
Results
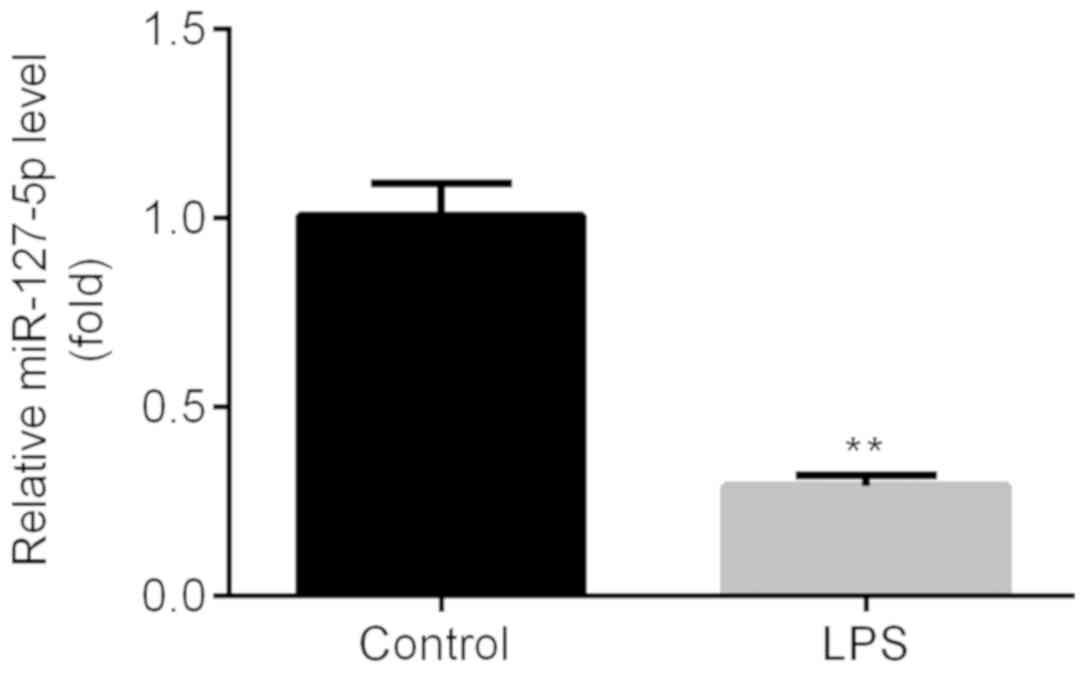
miR-127-5p expression is downregulated
during pneumonia
Once the in vitro model of pneumonia was
established using LPS, as evidenced by increased inflammatory
cytokines (data not shown), the expression of miR-127-5p in Ana-1
murine macrophages was detected by RT-qPCR. The results indicated
that miR-127-5p expression was significantly decreased in Ana-1
murine macrophages following LPS exposure compared with the control
group (Fig. 1); therefore,
LPS-treated Ana-1 murine macrophages were used for subsequent
experiments.
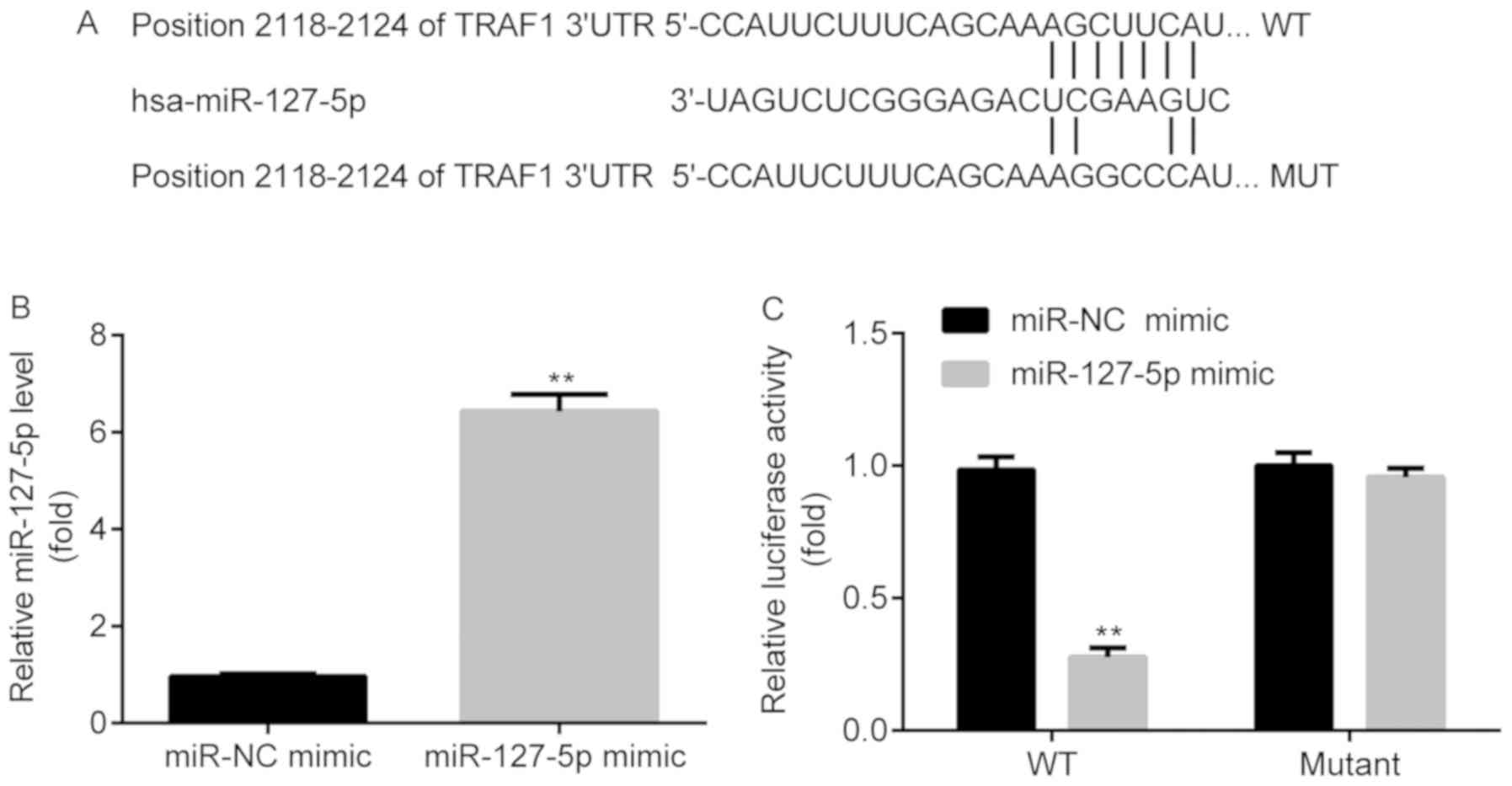
miR-127-5p targets the 3'-UTR of
TRAF1
TargetScan indicated that miR-127-5p targeted TRAF1
at the 2,118-2,124 position of the 3'-UTR (Fig. 2A). To determine whether miR-127-5p
mimic was successfully transfected into Ana-1 murine macrophages,
the expression of miR-127-5p in the miR-NC mimic and miR-127-5p
mimic groups was detected by RT-qPCR. miR-127-5p expression was
significantly increased in the miR-127-5p mimic group compared with
the miR-NC mimic group (Fig. 2B). A
dual-luciferase reporter assay was subsequently performed to
investigate the interaction between miR-127-5p and the 3'-UTR of
TRAF1. Luciferase activity was significantly reduced in the
TRAF1-WT-3'UTR + miR-127-5p mimic group compared with the
TRAF1-WT-3'UTR + miR-NC mimic group. However, no significant
difference in luciferase activity was observed between the
TRAF1-MUT-3'UTR + miR-127-5p mimic and TRAF1-MUT-3'UTR + miR-NC
mimic groups (Fig. 2C).
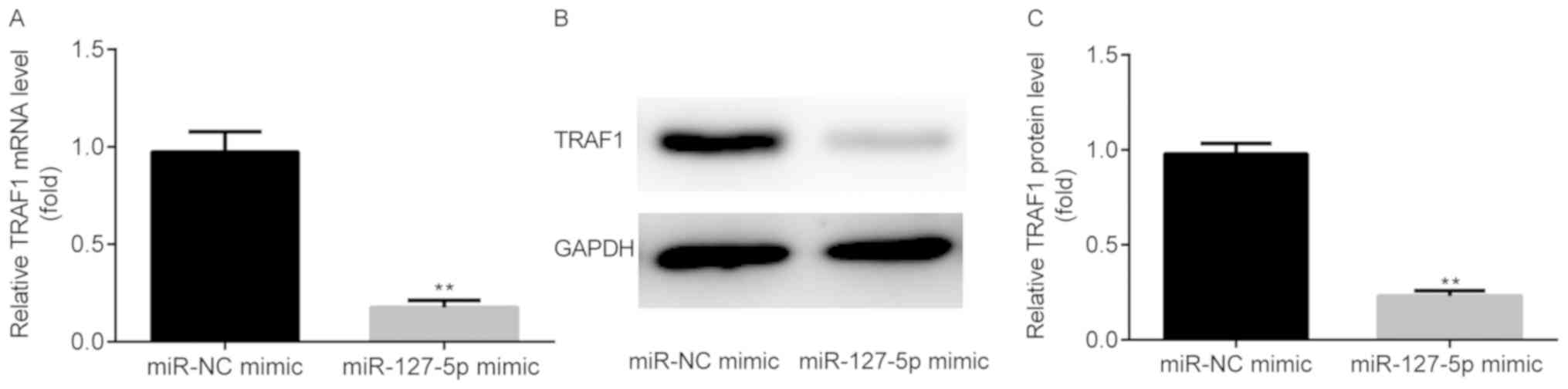
miR-127-5p inhibits TRAF1
expression
To determine whether miR-127-5p mimic could regulate
the expression of TRAF1, the mRNA and protein expression levels of
TRAF1 were detected using western blotting and RT-qPCR,
respectively. The results suggested that the mRNA (Fig. 3A) and protein (Fig. 3B and C) expression levels of TRAF1 were
significantly decreased in the miR-127-5p mimic group compared with
the miR-NC mimic group.
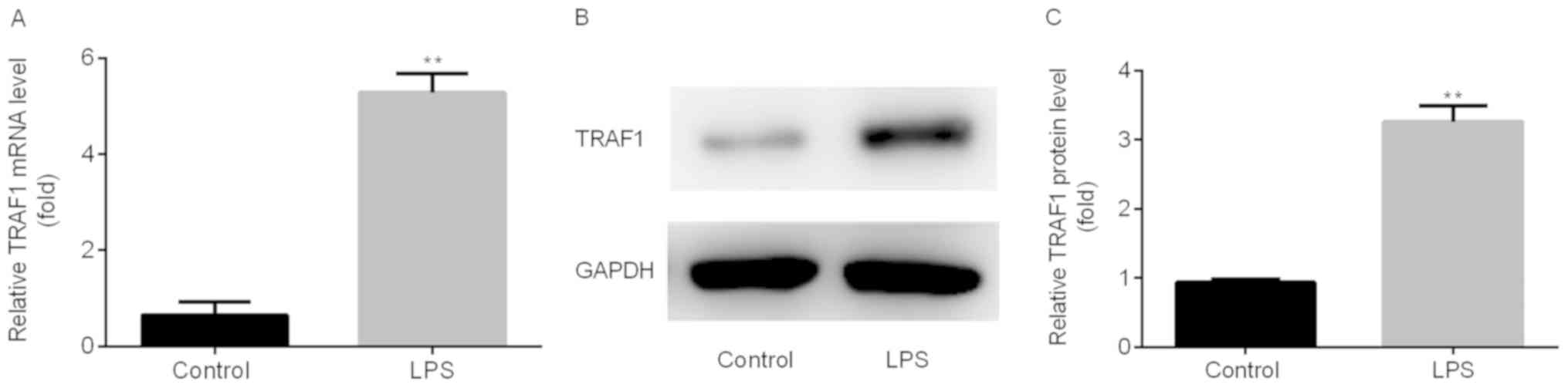
TRAF1 expression is upregulated during
pneumonia
Following the establishment of the in vitro
LPS-induced pneumonia model, the mRNA and protein expression levels
of TRAF1 were detected in Ana-1 murine macrophages using RT-qPCR
and western blotting, respectively. TRAF1 mRNA (Fig. 4A) and protein (Fig. 4B and C) expression levels were significantly
increased in Ana-1 murine macrophages following LPS treatment
compared with the control group.
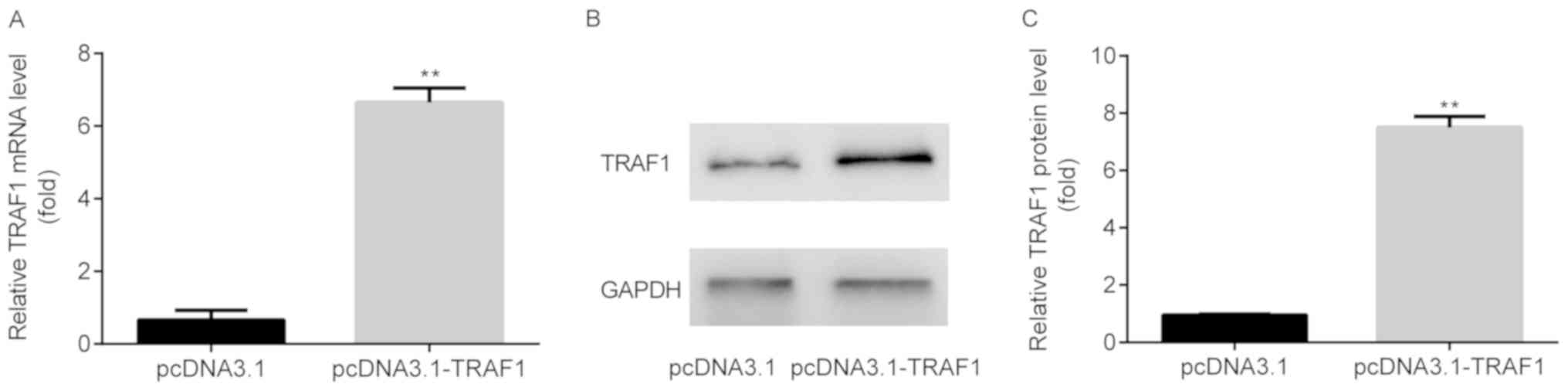
TRAF1 overexpression is induced by
pcDNA3.1-TRAF1
TRAF1 mRNA (Fig. 5A)
and protein (Fig. 5B and C) expression levels were significantly
increased in the pcDNA3.1-TRAF1 group compared with the pcDNA3.1
group.
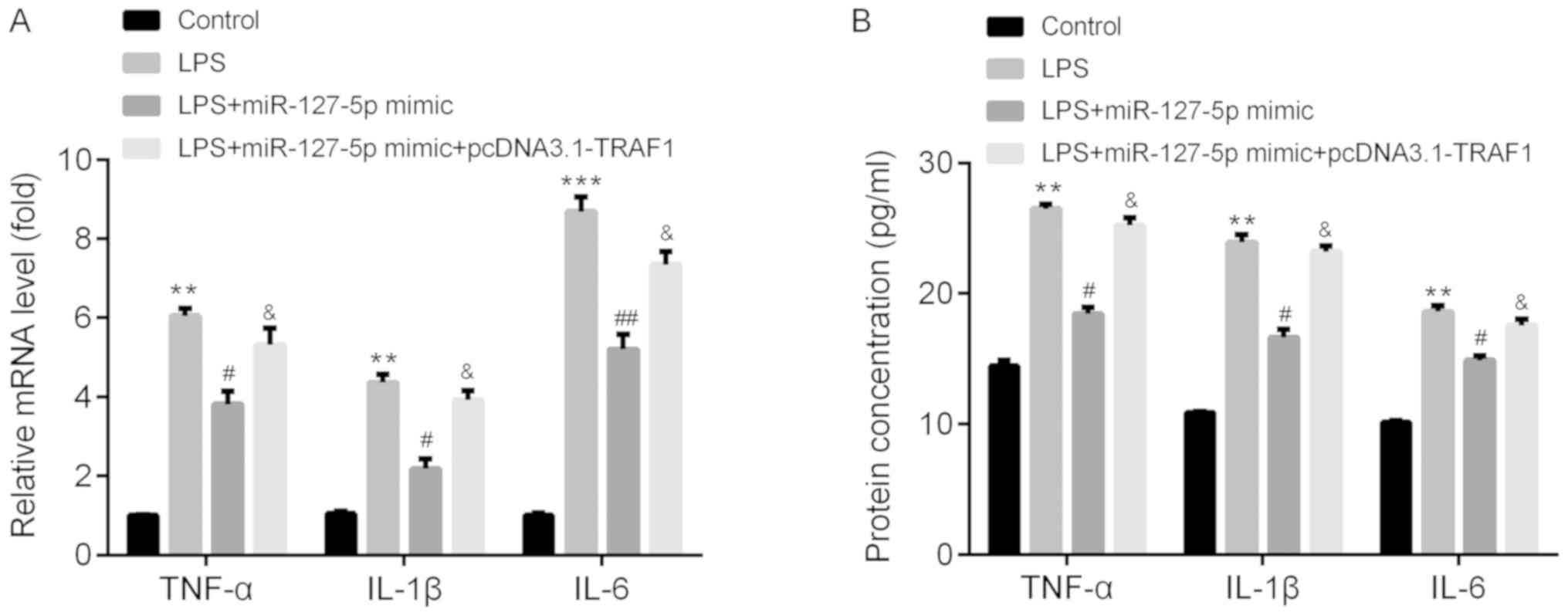
miR-127-5p mimic downregulates TNF-α,
IL-1β and IL-6 levels by targeting TRAF1
To determine the function of miR-127-5p during
pneumonia, the mRNA and protein expression levels of certain
inflammatory cytokines, including TNF-α, IL-1β and IL-6, were
detected using RT-qPCR and ELISA, respectively.
The mRNA expression levels of TNF-α, IL-1β and IL-6
were significantly increased in the LPS group compared with the
control group. Furthermore, LPS-induced effects on inflammatory
cytokine expression were significantly decreased following
transfection with the miR-127-5p mimic; however, TRAF1
overexpression reversed miR-127-5p mimic-induced effects (Fig. 6A). The protein levels of TNF-α, IL-1β
and IL-6 displayed a similar pattern to the mRNA levels in response
to LPS, miR-127-5p mimic and pcDNA3.2-TRAF1 (Fig. 6B).
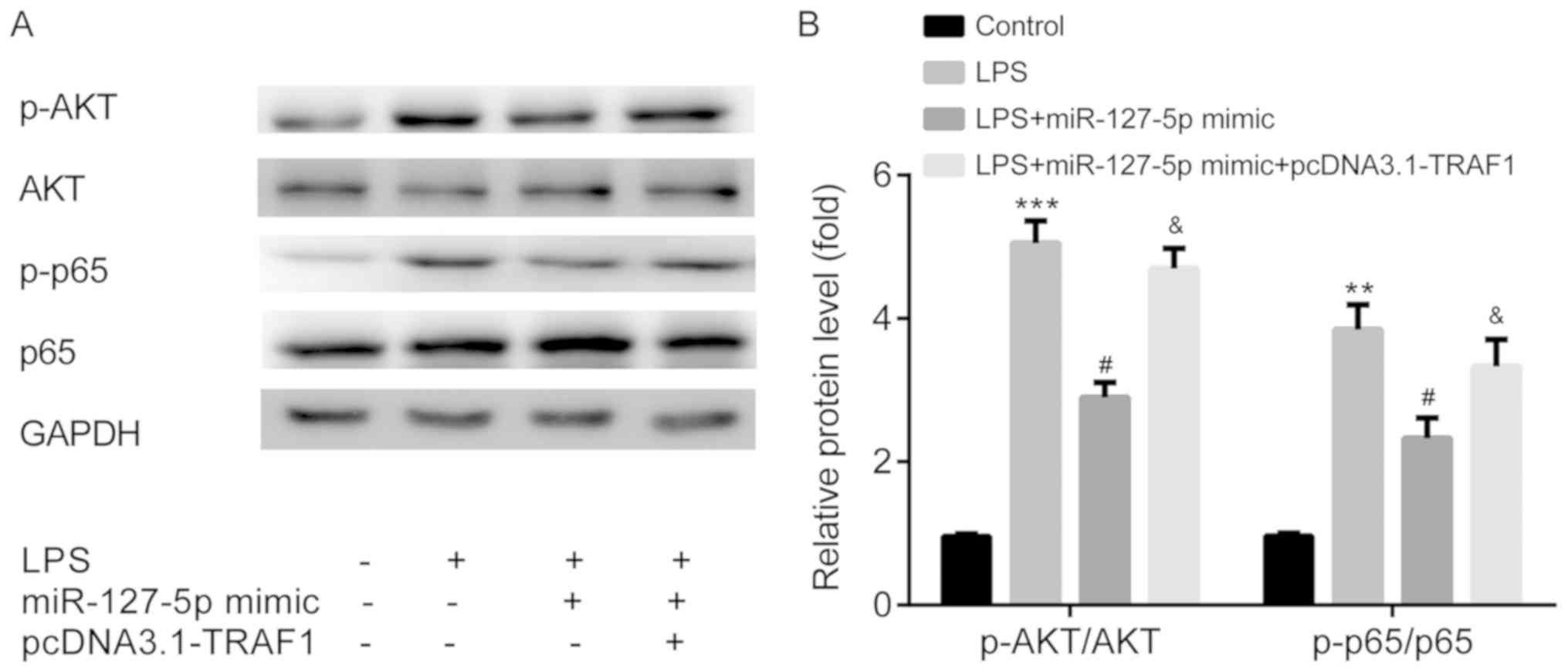
miR-127-5p mimic blocks the AKT/NF-κB
signaling pathway by targeting TRAF1
To determine the effect of miR-127-5p on the
signaling pathway involved in pneumonia, AKT phosphorylation and
NF-κB activity were measured by western blotting. The ratios of
p-AKT/AKT and p-p65/p65 expression levels were significantly
increased in the LPS group compared with the control group.
LPS-induced effects were significantly decreased by transfection
with the miR-127-5p mimic; however, treatment with miR-127-5p mimic
+ pcDNA3.1-TRAF1 did not significantly alter LPS-induced effects
(Fig. 7A and B).
Discussion
Pneumonia is a persistent and pervasive disease
(1); therefore, further
investigation into the molecules that mediate severe pneumonia is
required to identify novel therapeutics for the disease and reduce
the disease burden.
miR-127 serves a role in numerous lung diseases. For
example, miR-127 inhibits lung inflammation by targeting IgG Fcγ
receptor I (14). Additionally,
miR-127-5p, which is downregulated in bronchoalveolar lavage fluid,
serves as a novel biomarker for the diagnosis of severe pneumonia
(15). In the present study, lower
miR-127-5p expression levels were observed in the LPS group
compared with the control group, indicating the inhibitory effects
of miR-127-5p during severe pneumonia. However, to the best of our
knowledge, the molecules underlying this effect during severe
pneumonia have not been previously reported.
The present study indicated that TRAF1 was targeted
by miR-127-5p. TRAF1 is associated with a number of lung diseases,
including asthma (18), non-small
cell lung cancer (19) and lung
inflammation (20). In the present
study, higher TRAF1 expression levels were observed in the LPS
group compared with the control group. In addition, TRAF1 was
targeted by miR-127-5p and its expression was decreased by
miR-127-5p mimic, indicating the enhancing effects of TRAF1 during
severe pneumonia.
In in vitro monocyte models of pneumonia, LPS
increased the levels of TNF-α, IL-1β and IL-6 (21,22). TNF
is one of the most studied proinflammatory cytokines that displays
numerous immunomodulatory activities (23). TNF is highly active in the lung and
is therefore implicated in numerous pulmonary diseases, including
asthma, chronic bronchitis and chronic obstructive pulmonary
disease (24). Serum TNF-α and IL-6
levels have been associated with early death in patients with
community-acquired pneumonia (25).
In addition, IL-1β is a biomarker for the severity of
community-acquired pneumonia in pediatric patients (26). Consistent with the aforementioned
studies (21-26),
the present study indicated that miR-127-5p mimic reversed
LPS-induced upregulation of TNF-α, IL-1β and IL-6 levels, and TRAF1
overexpression inhibited miR-127-5p mimic-induced effects.
Collectively, these results indicated that miR-127-5p inhibited
LPS-induced inflammation by targeting TRAF1 during severe
pneumonia.
NF-κB activation is a prerequisite for the
production of a number of inflammatory cytokines, including TNF-α,
IL-1β and IL-6(27), which leads to
a more severe inflammatory reaction in stimulated macrophages
(28). AKT is an upstream activator
of the NF-κB signaling pathway (29). In the present study, miR-127-5p mimic
reversed LPS-induced activation of p-AKT and p-p65, which was
rescued by TRAF1 overexpression. Collectively, the results
indicated that miR-127-5p inhibited LPS-induced AKT/NF-κB
activation by targeting TRAF1 during severe pneumonia.
In conclusion, miR-127-5p may attenuate severe
pneumonia, by reducing LPS-induced production of TNF-α, IL-1β and
IL-6, and inactivating the AKT/NF-κB signaling pathway via TRAF1.
Therefore, the present study suggested that TRAF1 may serve as a
therapeutic target for severe pneumonia.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CC, SL, LZ, JW, JC, RY, HL, JL, and ZX carried out
the experimentations and data analyses. MC designed, conceived and
supervised the research and prepared the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mizgerd JP: Respiratory infection and the
impact of pulmonary immunity on lung health and disease. Am J
Respir Crit Care Med. 186:824–829. 2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jain S, Self WH, Wunderink RG, Fakhran S,
Balk R, Bramley AM, Reed C, Grijalva CG, Anderson EJ, Courtney DM,
et al: CDC EPIC Study Team: Community-Acquired Pneumonia Requiring
Hospitalization among U.S Adults. N Engl J Med. 373:415–427.
2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Jain S, Williams DJ, Arnold SR, Ampofo K,
Bramley AM, Reed C, Stockmann C, Anderson EJ, Grijalva CG, Self WH,
et al: CDC EPIC Study Team: Community-acquired pneumonia requiring
hospitalization among U.S children. N Engl J Med. 372:835–845.
2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bartel DP: MicroRNAs: Genomics,
biogenesis, mechanism, and function. Cell. 116:281–297.
2004.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ambros V: The functions of animal
microRNAs. Nature. 431:350–355. 2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Farh KK, Grimson A, Jan C, Lewis BP,
Johnston WK, Lim LP, Burge CB and Bartel DP: The widespread impact
of mammalian MicroRNAs on mRNA repression and evolution. Science.
310:1817–1821. 2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
He L and Hannon GJ: MicroRNAs: Small RNAs
with a big role in gene regulation. Nat Rev Genet. 5:522–531.
2004.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
He L, Thomson JM, Hemann MT,
Hernando-Monge E, Mu D, Goodson S, Powers S, Cordon-Cardo C, Lowe
SW, Hannon GJ, et al: A microRNA polycistron as a potential human
oncogene. Nature. 435:828–833. 2005.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lecellier CH, Dunoyer P, Arar K,
Lehmann-Che J, Eyquem S, Himber C, Saïb A and Voinnet O: A cellular
microRNA mediates antiviral defense in human cells. Science.
308:557–560. 2005.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Huang S, Feng C, Zhai YZ, Zhou X, Li B,
Wang LL, Chen W, Lv FQ and Li TS: Identification of miRNA
biomarkers of pneumonia using RNA-sequencing and bioinformatics
analysis. Exp Ther Med. 13:1235–1244. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Li S, Cui W, Song Q, Zhou Y and Li J:
miRNA-302e attenuates inflammation in infantile pneumonia though
the RelA/BRD4/NF-κB signaling pathway. Int J Mol Med. 44:47–56.
2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhou Z, Zhu Y, Gao G and Zhang Y: Long
noncoding RNA SNHG16 targets miR-146a-5p/CCL5 to regulate
LPS-induced WI-38 cell apoptosis and inflammation in acute
pneumonia. Life Sci. 228:189–197. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zhang Y, Zhu Y, Gao G and Zhou Z:
Knockdown XIST alleviates LPS-induced WI-38 cell apoptosis and
inflammation injury via targeting miR-370-3p/TLR4 in acute
pneumonia. Cell Biochem Funct. 37:348–358. 2019.PubMed/NCBI View
Article : Google Scholar
|
|
14
|
Xie T, Liang J, Liu N, Wang Q, Li Y, Noble
PW and Jiang D: MicroRNA-127 inhibits lung inflammation by
targeting IgG Fcγ receptor I. J Immunol. 188:2437–2444.
2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wang Z, Liu Q, Wang X, Wang Y, Zhang J,
Zhou W and Yang X: Expressions of microRNA-127-5p in
bronchoalveolar lavage fluid of patients with severe pneumonia and
its diagnostic value. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue.
29:592–595. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
16
|
Chen Y, Luo G, Yuan J, Wang Y, Yang X,
Wang X, Li G, Liu Z and Zhong N: Vitamin C mitigates oxidative
stress and tumor necrosis factor-alpha in severe community-acquired
pneumonia and LPS-induced macrophages. Mediators Inflamm.
2014(426740)2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Oyoshi MK, Bryce P, Goya S, Pichavant M,
Umetsu DT, Oettgen HC and Tsitsikov EN: TNF receptor-associated
factor 1 expressed in resident lung cells is required for the
development of allergic lung inflammation. J Immunol.
180:1878–1885. 2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wen X, Wang B, Feng T, Yuan W, Zhou J and
Fang T: TNF receptor-associated factor 1 as a biomarker for
assessment of non-small cell lung cancer metastasis and overall
survival. Clin Respir J. 12:2197–2203. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Oyoshi MK, Barthel R and Tsitsikov EN:
TRAF1 regulates recruitment of lymphocytes and, to a lesser extent,
neutrophils, myeloid dendritic cells and monocytes to the lung
airways following lipopolysaccharide inhalation. Immunology.
120:303–314. 2007.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Taganov KD, Boldin MP, Chang KJ and
Baltimore D: NF-kappaB-dependent induction of microRNA miR-146, an
inhibitor targeted to signaling proteins of innate immune
responses. Proc Natl Acad Sci USA. 103:12481–12486. 2006.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Liu Z, Yu H and Guo Q: MicroRNA-20a
promotes inflammation via the nuclear factor-κB signaling pathway
in pediatric pneumonia. Mol Med Rep. 17:612–617. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Locksley RM, Killeen N and Lenardo MJ: The
TNF and TNF receptor superfamilies: Integrating mammalian biology.
Cell. 104:487–501. 2001.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Mukhopadhyay S, Hoidal JR and Mukherjee
TK: Role of TNFalpha in pulmonary pathophysiology. Respir Res.
7(125)2006.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Bacci MR, Leme RC, Zing NP, Murad N, Adami
F, Hinnig PF, Feder D, Chagas AC and Fonseca FL: IL-6 and TNF-α
serum levels are associated with early death in community-acquired
pneumonia patients. Braz J Med Biol Res. 48:427–432.
2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Korkmaz MF, Güzel A, Açıkgöz M, Okuyucu A
and Alaçam H: Reliability of Pro-adrenomedullin and Interleukin 1β
in predicting severity of community-acquired pneumonia in pediatric
patients. Ann Clin Lab Sci. 48:81–89. 2018.PubMed/NCBI
|
|
27
|
Li Y, Reddy MA, Miao F, Shanmugam N, Yee
JK, Hawkins D, Ren B and Natarajan R: Role of the histone H3 lysine
4 methyltransferase, SET7/9, in the regulation of
NF-kappaB-dependent inflammatory genes. Relevance to diabetes and
inflammation. J Biol Chem. 283:26771–26781. 2008.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Liu SF and Malik AB: NF-κB activation as a
pathological mechanism of septic shock and inflammation. Am J
Physiol Lung Cell Mol Physiol. 290:L622–L645. 2006.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Venkatesan B, Valente AJ, Prabhu SD,
Shanmugam P, Delafontaine P and Chandrasekar B: EMMPRIN activates
multiple transcription factors in cardiomyocytes, and induces
interleukin-18 expression via Rac1-dependent PI3K/Akt/IKK/NF-kappaB
andMKK7/JNK/AP-1 signaling. J Mol Cell Cardiol. 49:655–663.
2010.PubMed/NCBI View Article : Google Scholar
|