Introduction
Lumbar canal stenosis, a degenerative condition
commonly seen in older individuals, is characterized by
pathological spinal canal narrowing and compression of the canal
sac along with the nerve roots (1).
The usual clinical symptoms include lower backache, neurogenic
claudication, lower limb pain and decreased walking ability. The
disease not only affects daily function but also has a significant
impact on the overall quality of life (2). Initial management usually consists of
conservative measures, such as physiotherapy, steroid injections
and oral medications (2,3). However, in patients with incapacitating
pain, gradually shortened walking distances, neurological deficit
progression and failed conservative management, surgical treatment
is usually recommended (3). Studies
have indicated better clinical outcomes with surgical treatment
than with conservative management (3,4).
The primary aim of surgical treatment is to
decompress the neural structures, thereby relieving symptoms and
improving function (5). However,
conventional open surgery requires extensive dissection and
traction of paraspinal muscles that may lead to muscle ischemia and
denervation resulting in atrophy, postoperative back pain and
patient dissatisfaction (5,6). To overcome these limitations,
minimally-invasive techniques were developed. In such methods,
arthroscopes, endoscopes or microscopes are introduced through
small incisions, providing the operator with a clear working view
with limited damage to adjacent structures (6). These techniques preserve posterior
midline structures and achieve sufficient decompression by
unilateral laminotomy and bilateral decompression (ULBD). Among the
various minimally invasive methods, a biportal endoscopic approach
is an emerging technique for managing disc herniation and lumbar
canal stenosis (7). Unlike
conventional spinal endoscopy, where the working as well as the
visual channel are in a single portal, biportal endoscopic
technique utilizes two portals, of which one is the endoscopic
portal and the other is the working portal. Thus, the working
instruments may be moved independently of the visualization portal
offering a better range of motion and convenience to the operator
(7,8). The clear magnified view and free
handling of tissues allow for safe and adequate neural
decompression. Recent studies have demonstrated favorable results
with a biportal endoscopic technique for the management of lumbar
canal stenosis (7-9).
However, to date, no meta-analysis has compared outcomes of lumbar
canal stenosis decompression between biportal endoscopic and
microscopic techniques. Therefore, the purpose of the present study
was to systematically search the literature and perform a
meta-analysis of studies comparing the outcomes between biportal
endoscopic technique and microscopic technique for lumbar canal
stenosis decompression.
Data and methods
Search strategy
The present meta-analysis was performed according to
the methods described in the Preferred Reporting Items for
Systematic reviews and Meta-Analysis statement (10). A total of two authors (GZ and ZC)
independently searched the PubMed, Google Scholar, Web of Science,
Embase and the Cochrane Library databases for relevant studies
published in the English language from database inception to the
15th of December 2019. The following key words were used for the
search: ‘Lumbar canal stenosis’, ‘minimally invasive surgery’,
‘surgical decompression’, ‘endoscopy’ and ‘biportal technique’. The
references within the included articles were also searched to
identify additional relevant studies. A third reviewer (XY) was
consulted to resolve any disagreements between the two authors
performing the literature search.
Study selection
Studies were selected according to the Population,
Intervention, Comparison and Outcomes criteria (11). Studies performed on patients with
lumbar canal stenosis as the Population, comparing biportal
endoscopy as the Intervention with microscopic endoscopy for
Comparison, and assessing at least operating time or complications
as Outcomes were included. Studies were excluded if they were: i)
Single-arm studies without any comparative group, ii) studies not
reporting relevant data or iii) case series, case reports and
review articles.
Data extraction and review
Two authors (GZ and ZC) extracted data on study
design, sample size, baseline features, intervention details and
outcome variables. Any disagreements between the two authors were
resolved through discussion with the third investigator (XY). The
primary outcomes were operative time and complications. Secondary
outcomes were hospital stay, Oswestry disability index (ODI) and
pain measured on the visual analog score (VAS).
Quality assessment
The quality of studies that were not randomized
controlled trials (RCTs) was assessed using the risk of bias
assessment tool for non-randomized studies (12). Studies were rated as having a low
risk, high risk or unclear risk of bias in the following
categories: Selection of participants, confounding variables,
measurement of exposure, blinding of outcome assessment, incomplete
outcome data and selective outcome reporting. RCTs were assessed
using the Cochrane Collaboration risk assessment tool for RCTs
(13). Studies were rated as having
low risk, high risk or unclear risk of bias in terms of the
following points: Random sequence generation, allocation
concealment, blinding of participants and personnel, blinding of
outcome assessment, incomplete outcome data, selective reporting
and other biases.
Statistical analysis
Statistical analyses were performed using Review
Manager software (version 5.3; The Cochrane Collaboration). For
categorical variables, data were summarized using the
Mantel-Haenszel odds ratio (OR) with 95% CIs. Continuous data are
presented as mean differences (MDs) and 95% CI. The I2
test was used to assess statistical heterogeneity. I2
values ≥ 50% were considered to indicate significant heterogeneity
and a random-effect model was used for meta-analysis. However, if
I2 was <50%, a fixed-effects model was used.
Results
Selection of studies and bias
assessment
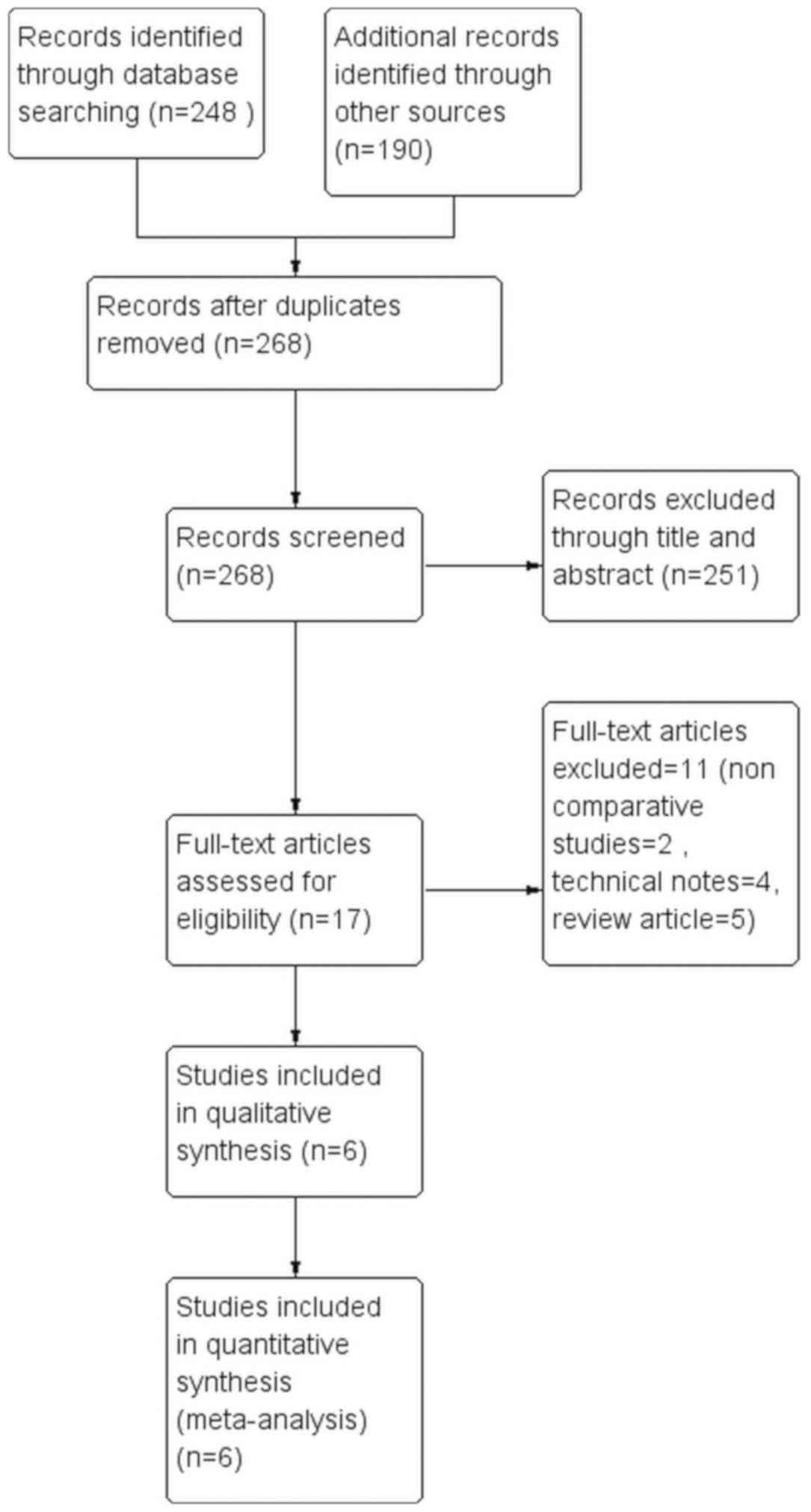
Details of the literature search for the present
review are presented in Fig. 1.
After excluding duplicates, 268 articles we screened based on the
inclusion and exclusion criteria. After excluding non-relevant
studies, 17 articles were screened by their full texts and 11
studies were excluded as they did not fulfill the inclusion
criteria. Finally, 6 trials were included in the systematic review
and meta-analysis (14-19).
The risk of bias assessment of the included studies is presented in
Table I. The overall quality of the
RCTs was moderate-to-high. For non-RCTs, there was low risk of bias
for ‘selection of participants’, ‘incomplete outcome data’ and
‘selective outcome reporting’ but a high risk of bias for ‘blinding
of outcome assessment’ owing to their study designs. The only study
that had low risk of bias for ‘confounding factors’ was that of Heo
et al (18).
 | Table IJudgement of risk of bias in included
studies. |
Table I
Judgement of risk of bias in included
studies.
| A, RCTs |
|---|
| Study | Random sequence
generation | Allocation
concealment | Blinding of
participants and personnel | Blinding of outcome
assessment | Incomplete outcome
data | Selective
reporting | Other biases | (Refs.) |
|---|
| Kang (2019) | Low risk | Unclear risk | High risk | Low risk | Low risk | Unclear risk | Low risk | (16) |
| Park (2020) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | (14) |
| B, Non-RCTs |
| Study | Selection of
participants | Confounding
variables | Measurement of
exposure | Blinding of outcome
assessment | Incomplete outcome
data | Selective reporting
outcome | | (Refs.) |
| Choi (2019) | Low risk | High risk | Unclear risk | High risk | Low risk | Low risk | | (19) |
| Heo (2018) | Low risk | Low risk | Low risk | High risk | Low risk | Low risk | | (18) |
| Heo (2019) | Low risk | High risk | Unclear risk | High risk | Low risk | Low risk | | (17) |
| Min (2019) | Low risk | Unclear risk | Low risk | High risk | Low risk | Low risk | | (15) |
Characteristics of included
studies
Details of the studies included are presented in
Table II. A total of 438 patients
with lumbar canal stenosis were analyzed in the included studies,
233 of which underwent biportal endoscopic decompressions, while
200 patients underwent microscopic decompression. All studies were
performed in Korea. With the exception of one study (19), all studies performed single-level
surgeries.
 | Table IIKey details of the studies included
in the meta-analysis. |
Table II
Key details of the studies included
in the meta-analysis.
| Study | Study type | Country | No. of levels | BESS/MD | BESS/MD (M/F) | Age, years
(BESS/MD) | Complications | Conclusion | Final follow-up
months | (Refs.) |
|---|
| Choi (2019) | Retrospective
study | Korea | BSS: Single -24
Multiple levels-11 MD: Single Multiple levels-15 | 35/30 | 14/21:17/13 | 65.4±11.8/
65.2±12.0 | BESS: Dural tear
(n=2) Root injury (n=1) MD: Dural tear (n=2) | BESS produced
clinical results not inferior to those of MD in the short-term | 6 | (19) |
| Heo (2018) | Retrospective
analysis of prospectively collected data | Korea | All single
level | 37/30 | 15/22:12/21 | 66.7±9.4/
63.4±11.1 | BESS: Durotomy
(n=1) Post-operative Hematoma (n=1) MD: Durotomy (n=2) Transient
weakness (n=1) Post-operative hematoma (n=2) | Uniportal or
biportal Endoscopic lumbar approach may be effective for the
treatment of lumbar central stenosis and an alternative to
conventional MD. | VAS Back:
BESS:1.98±0.80 MD: 2.04±0.88 VAS Leg: BESS 2.07±0.77 MD:
2.21±0.95 ODI: BESS 21.98±2.82 MD: 22.59±3.16 | (17) |
| Heo (2018) | Case control
prospective study | Korea | All single
level | 46/42 | 18/28:16/26 | 65.8±8.9/
63.6±10.5 | BESS: Durotomy
(n=1) Post-operative hematoma (n=1) MD: Durotomy (n=1)
Post-operative hematoma (n=2) | BESS is a safe and
effective treatment for lumbar spinal stenosis. Decompression rates
are similar to those of BESS and MD. | VAS Back:
BESS:1.98±0.80 MD: 2.04±0.88 VAS Leg: BESS: 2.07±0.77 MD:
2.21±0.95 ODI: BESS: 21.98±2.82 MD: 22.59±3.16 | (18) |
| Kang (2019) | Randomized
controlled trial | Korea | All single
level | 32/30 | 18/14: 14/16 | 65.1±8.6/
67.2±9.5 | BESS: Revision
(n=1) MD: Revision (n=1) | BESS resulted in
favorable clinical outcomes, less pain and a shorter hospital stay
compared to MD. | 6 | (16) |
| Min (2019) | Case control
study | Korea | All single
level | 54/35 | 27/27: 19/16 | 65.74±10.52/
66.74±7.96 | BESS: Dural tear
(n=2) Post-operative epidural hematoma (n=1) MD: Microsurgery:
Dural tear (n=1) Post-operative epidural hematoma (n=1) | Similar outcomes
with BESS and MD. However, BESS leads to less postoperative back
pain than MD and may allow early ambulation and a shorter
hospitalization period. | BESS: 27.2±5.4 MD:
31.5±7.3 | (15) |
| Park (2020) | Randomized
controlled trial | Korea | All single
level | 32/32 | 13/19:18/14 | 66.2/ 67.1 | BESS: Incidental
durotomy (n=2) Symptomatic hematoma with revision surgery (n=1) MD:
Incidental duroctomy (n=2) Symptomatic hematoma with revision
surgery (n=1) Revision surgery due to recurrent pain (n=1) | BESS is an
alternative to MD with similar clinical outcomes. | 12 | (14) |
Primary outcomes
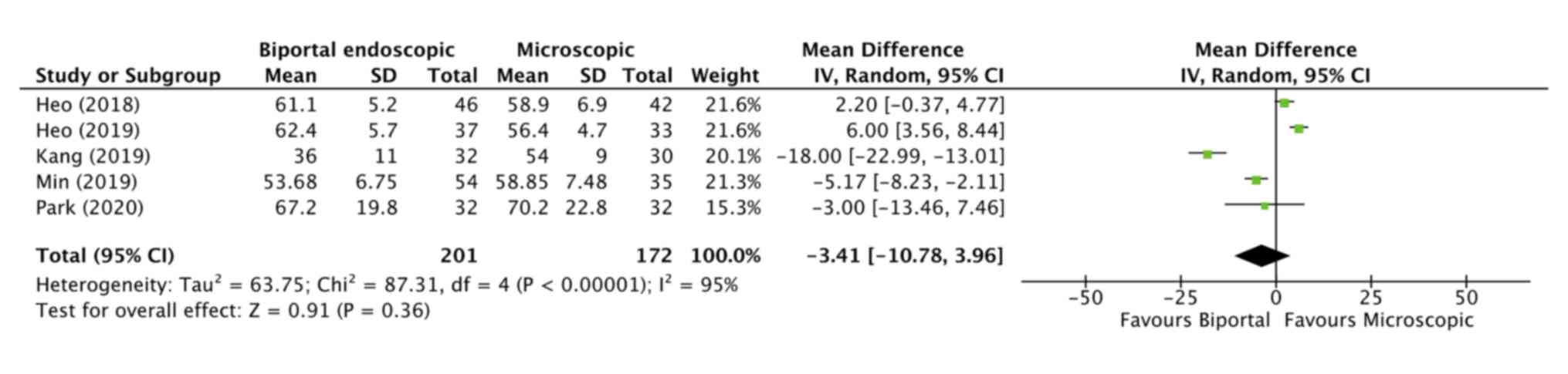
A total of 5 studies (14-18)
compared the operative time between biportal endoscopy and
microscopic endoscopy. The results of the pooled analysis
demonstrated no statistically significant differences between the
biportal endoscopic and microscopic decompression groups (MD,
-3.41; 95% CI, -10.78-3.96; P=0.36; Fig.
2).
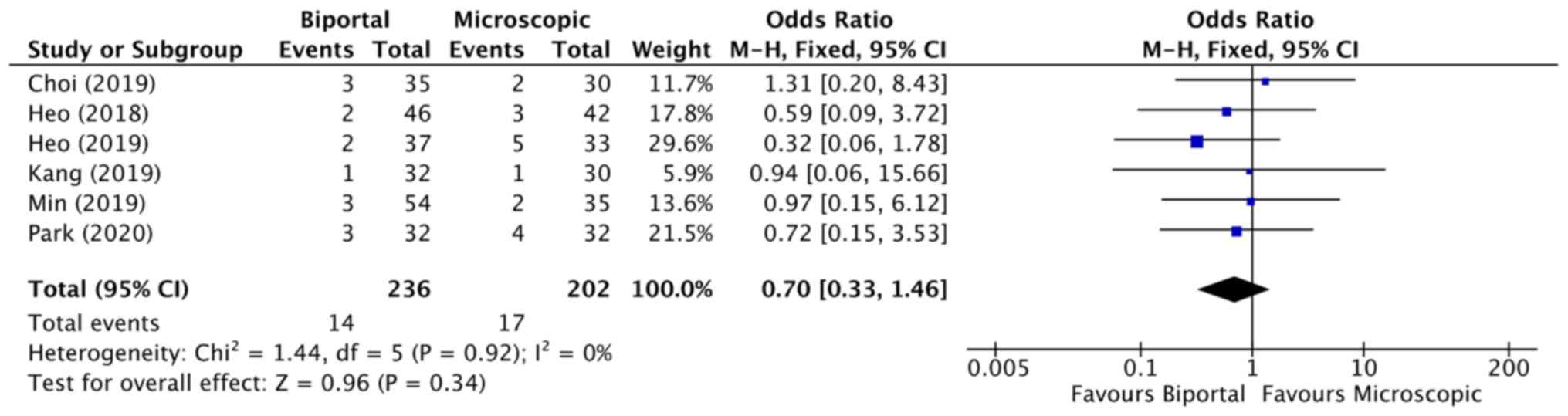
The total number of complications in each group was
pooled for meta-analysis. The results indicated no statistically
significant differences in complication rates between the two
groups (OR, 0.70; 95% CI, 0.33-1.46; P=0.34; Fig. 3). Details of complications in the
included studies are presented in Table
II.
Secondary outcomes
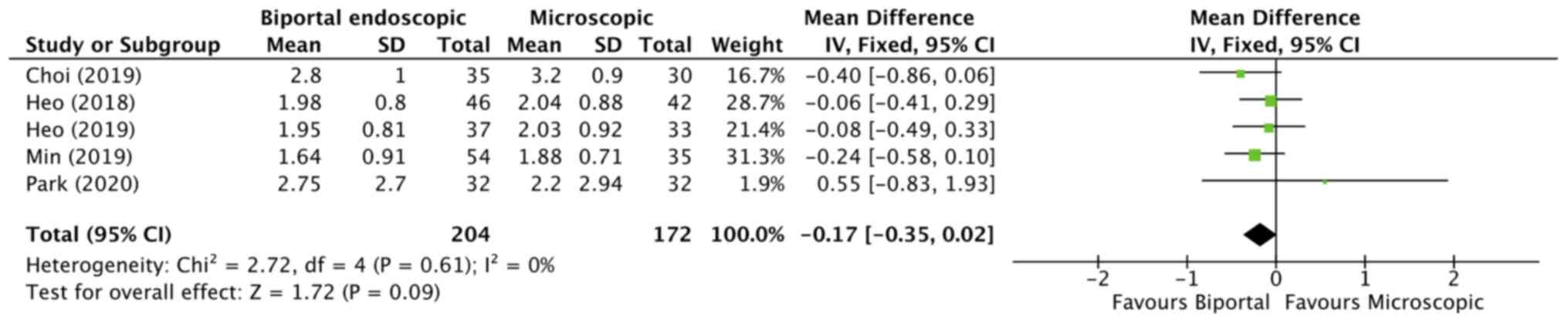
A total of 5 studies (14,15,17-19)
reported on back pain VAS scores at the final follow-ups. The
pooled analysis demonstrated no statistically significant
difference in back pain scores between the two groups (MD, -0.17;
95% CI, -0.3-0.02; P=0.09; Fig. 4).
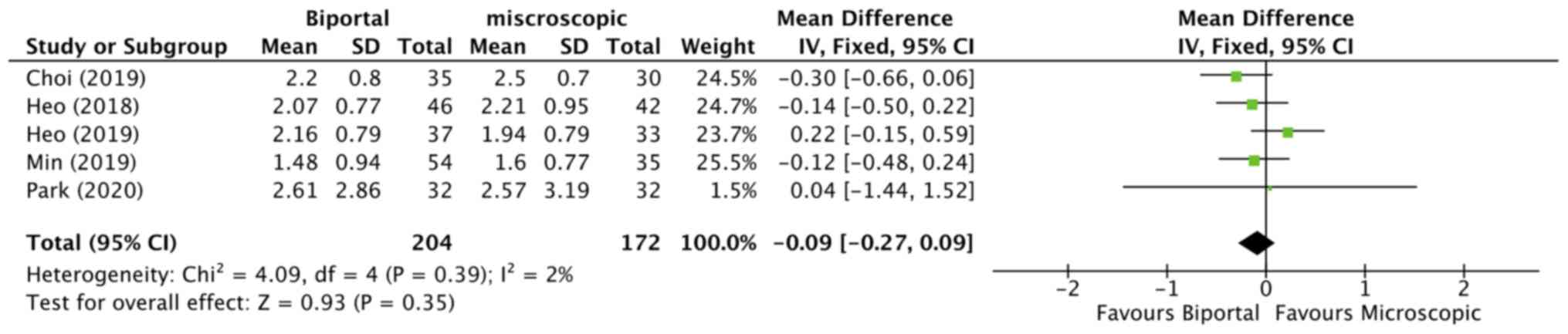
Data on leg pain VAS scores were reported by 5 studies (14,15,17-19).
The meta-analysis demonstrated no statistically significant
differences in leg pain scores between the two groups at the final
follow-ups (MD, -0.09; 95% CI, -0.27 to 0.09; P=0.35; Fig. 5).
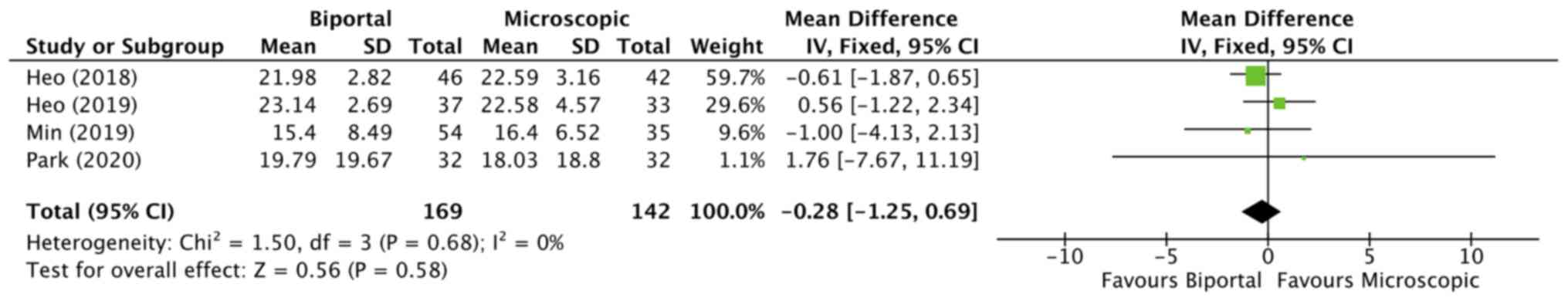
A total of 4 studies (14,15,17,18)
reported data on the ODI scores at the final follow-ups.
Meta-analysis indicated no statistically significant difference
between the biportal endoscopic decompression and microscopic
decompression groups (MD, -0.28; 95% CI, -1.25-0.69; P=0.58;
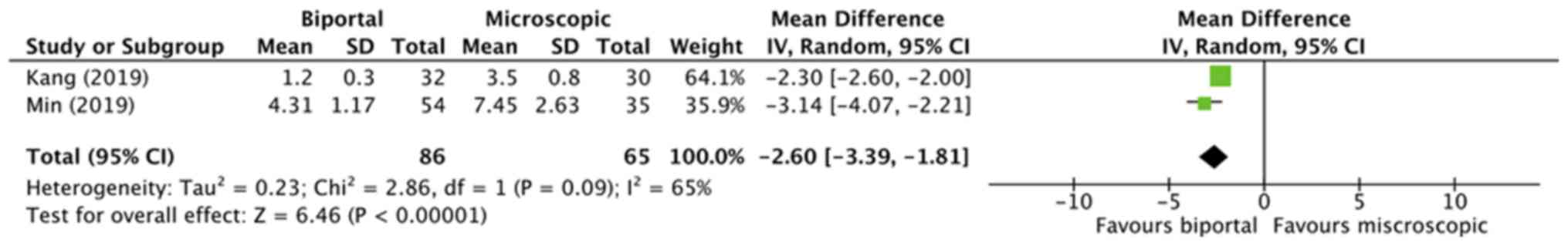
Fig. 6). Data on the length of
hospital stay were pooled from two studies (15,16). The
analysis indicated a significantly shorter length of hospital stay
in the biportal group (MD, -2.60; 95% CI, -3.39 to -1.81;
P<0.00001; Fig. 7).
Discussion
In the present meta-analysis, the comparison of the
outcomes of biportal endoscopic technique and the microscopic
technique indicated that the two techniques may be equally suitable
for managing lumbar canal stenosis. No significant difference in
operative times, complication rates, back pain and leg pain VAS
scores or ODI scores were identified between the two groups.
A number of different minimally-invasive techniques
have been reported for lumbar degenerative disease (20,21). The
advantage of minimally invasive surgery lies in the preservation of
normal anatomical structures, leading to faster post-operative
recovery (21). Several studies
comparing the microscopic ULBD technique with open surgery have
reported favorable outcomes with the former (22,23).
Trials have reported shorter operating times, reduced blood loss,
shorter hospital stay and fewer complications with ULBD technique
as compared to open surgery (22,24).
However, there are certain limitations to the microscopic
technique. First, instrument manipulation is difficult due to the
use of a single port. Second, while contralateral visualization may
be achieved, the microscope requires to be excessively tilted in
certain cases (15,25). In addition, there have been concerns
regarding inadequate exposure with the microscope, which may lead
to unsatisfactory decompression (23,26). The
technique is also associated with a steep learning curve, which may
prolong the operative time in the hands of a novice surgeon
(27).
In recent times, endoscopic decompression has been
introduced to manage patients with lumbar stenosis (28). However, the requirement for
specialized instruments and extensive training to reach surgical
competency is a disadvantage (29).
On the other hand, the instruments used in the biportal technique
are the same as those used for knee arthroscopies and conventional
spine surgeries, which may potentially reduce hospital costs
(14,30). As biportal endoscopic technique
shares the principles of arthroscopy, the learning curve is thought
to be comparable with that of microscopic methods (17). According to Heo et al
(17), around 30 operations under
supervision are required to complete the learning curve associated
with this technique. In addition, the field of view provided by the
biportal technique is wider than that of single-port endoscopes and
is comparable to the view offered by a microscope (14). The separation of viewing and working
portals in the biportal technique enable the surgeon to use both
hands freely, making instrument manipulation easier as compared to
the uniportal or microscopic technique. The contralateral
sublaminar and foraminal spaces may be visualized more
conveniently, particularly with the use of a 30˚ endoscope
(31). However, pooled analysis of 5
studies did not identify any significant differences in operating
times as compared with the biportal and the microscopic technique.
The operative time was significantly shorter with the biportal
technique as compared to microscopic technique in a study by Kang
et al (16). The authors
reported that with the biportal technique, the use of fluoroscopy
may be avoided after the preoperative level check, which saves
time. Furthermore, the clear and wide visualization provided by the
biportal technique and free movement of instruments may also
contribute to reduced operative time.
In the present analysis, no significant difference
in ODI scores and VAS scores for back pain and leg pain was
identified between the two groups. In this context, a study has
reported lower opioid use in the early postoperative period in
patients undergoing surgery with the biportal technique as compared
to the microscopic technique (31).
In addition, Choi and Kim (19)
reported a lower postoperative elevation of C-reactive protein
(CRP) in patients undergoing endoscopic procedures in comparison
with the microscopic procedures. The authors suggested that lower
CRP levels may indicate reduced muscle injury and better irrigation
with the biportal technique. On the other hand, Park et al
(14) did not obtain any
statistically significant difference in serum creatine
phosphokinase levels between the two groups. According to the
authors, even the biportal technique requires a small incision and
muscle stripping during the procedure, which is sufficient to
elevate serum creatine phosphokinase levels. While both techniques
require minimal soft-tissue dissection, there may be concerns
regarding the persistence of symptoms with minimally invasive
procedures due to inadequate decompression (15). However, the lack of differences in
VAS and ODI scores in the present analysis indicates that both the
biportal and microscopic technique result in similar outcomes.
In the present analysis, patients in the biportal
group had a significantly reduced hospital stay than those in the
microscopic technique group. However, the results must be
interpreted with caution, as only two studies reported data on the
length of hospital stay. In addition, the length of hospital stay
may be confounded by numerous other factors, including patient
co-morbidity, complications with the procedure and local hospital
protocols.
The complication rate of the biportal technique in
the present analysis was 5.9%, while that of the microscopic method
was 8.4% with no statistically significant difference. Complication
rates may be higher during the learning phase of minimally invasive
procedures and adequate supervision is highly recommended (17). Furthermore, complications are higher
when the surgical field is unclear due to bleeding (9). Bleeding with the biportal technique may
be minimized by utilizing the high magnification of the surgical
field along with continuous saline irrigation. While continuous
irrigation reduces bleeding and keeps the surgical field clean,
high-pressure irrigation is not recommended, as it may lead to
increased intracranial pressure and delay postoperative recovery
(32). A saline pressure at 30 mmHg
usually maintains a clear surgical field and causes minimal
compression of the thecal sac, avoiding potential iatrogenic damage
(32).
The limitations of the present study require to be
acknowledged. First, only 6 studies were included in the present
analysis, of which there were only two RCTs. The inherent bias of
non-RCTs may have skewed the results. Furthermore, the sample size
of the included studies was not large. In addition, there was no
consistency in the results of the included studies, indicating high
variability of the outcomes. Finally, the influence of the surgical
experience of the operators on the study outcomes cannot be
neglected. The difference in operative techniques and surgical
skills may have influenced the outcomes.
To conclude, the present study indicates that the
biportal endoscopic and microscopic techniques for lumbar canal
stenosis decompression do not differ in terms of operative time,
clinical outcomes and complications. The biportal endoscopic
technique may be considered as an alternative to the microscopic
decompression technique. However, further well-designed RCTs with
larger sample size are required to strengthen the current
evidence.
Acknowledgements
Not applicable.
Funding
This research was supported by The 6th Zhejiang
Province National Traditional Chinese Medicine Experts Academic
Experience Inheritance Project (grant no. 2018LPS07).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TC and DL designed the study. GZ, ZC and XY were
involved in the literature search and data interpretation. TC, GZ
and ZC were responsible for the data analysis. TC prepared the
manuscript. DL edited the manuscript. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hall S, Bartleson JD, Onofrio BM, Baker HL
Jr, Okazaki H and O'Duffy JD: Lumbar spinal stenosis. Clinical
features, diagnostic procedures, and results of surgical treatment
in 68 patients. Ann Intern Med. 103:271–275. 1985.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Parker SL, Godil SS, Mendenhall SK,
Zuckerman SL, Shau DN and McGirt MJ: Two-year comprehensive medical
management of degenerative lumbar spine disease (lumbar
spondylolisthesis, stenosis, or disc herniation): a value analysis
of cost, pain, disability, and quality of life: clinical article. J
Neurosurg Spine. 21:143–149. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Weinstein JN, Tosteson TD, Lurie JD,
Tosteson AN, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T,
Boden SD, et al: SPORT Investigators: Surgical versus nonsurgical
therapy for lumbar spinal stenosis. N Engl J Med. 358:794–810.
2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Malmivaara A, Slätis P, Heliövaara M,
Sainio P, Kinnunen H, Kankare J, Dalin-Hirvonen N, Seitsalo S,
Herno A, Kortekangas P, et al: Finnish Lumbar Spinal Research
Group: Surgical or nonoperative treatment for lumbar spinal
stenosis? A randomized controlled trial. Spine. 32:1–8.
2007.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ikuta K, Tono O, Tanaka T, Arima J, Nakano
S, Sasaki K and Oga M: Surgical complications of microendoscopic
procedures for lumbar spinal stenosis. Minim Invasive Neurosurg.
50:145–149. 2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Yagi M, Okada E, Ninomiya K and Kihara M:
Postoperative outcome after modified unilateral-approach
microendoscopic midline decompression for degenerative spinal
stenosis. J Neurosurg Spine. 10:293–299. 2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Eun SS, Eum JH, Lee SH and Sabal LA:
Biportal Endoscopic Lumbar Decompression for Lumbar Disk Herniation
and Spinal Canal Stenosis: A Technical Note. J Neurol Surg A Cent
Eur Neurosurg. 78:390–396. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Heo DH, Son SK, Eum JH and Park CK: Fully
endoscopic lumbar interbody fusion using a percutaneous unilateral
biportal endoscopic technique: Technical note and preliminary
clinical results. Neurosurg Focus. 43(E8)2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kim JE and Choi DJ: Unilateral biportal
endoscopic decompression by 30° endoscopy in lumbar spinal
stenosis: Technical note and preliminary report. J Orthop.
15:366–371. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Moher D, Liberati A, Tetzlaff J and Altman
DG: PRISMA Group. Preferred reporting items for systematic reviews
and meta-analyses: The PRISMA statement. PLoS Med.
6(e1000097)2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Schardt C, Adams MB, Owens T, Keitz S and
Fontelo P: Utilization of the PICO framework to improve searching
PubMed for clinical questions. BMC Med Inform Decis Mak.
7(16)2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS,
Hahn S, Jang BH and Son HJ: Testing a tool for assessing the risk
of bias for nonrandomized studies showed moderate reliability and
promising validity. J Clin Epidemiol. 66:408–414. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Higgins J, Thomas J, Chandler J, Cumpston
M, Li T, Page M and Welch V: Cochrane Handbook for Systemic Reviews
of Interventions. Version 6. Cochrane, 2019. https://doi.org/10.1002/9781119536604.
|
|
14
|
Park SM, Park J, Jang HS, Heo YW, Han H,
Kim HJ, Chang BS, Lee CK and Yeom JS: Biportal endoscopic versus
microscopic lumbar decompressive laminectomy in patients with
spinal stenosis: A randomized controlled trial. Spine J.
20:156–165. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Min W-K, Kim JE, Choi DJ, Park EJ and Heo
J: Clinical and radiological outcomes between biportal endoscopic
decompression and microscopic decompression in lumbar spinal
stenosis. J Orthop Sci, 2019.
|
|
16
|
Kang T, Park SY, Kang CH, Lee SH, Park JH
and Suh SW: Is biportal technique/endoscopic spinal surgery
satisfactory for lumbar spinal stenosis patients?: A prospective
randomized comparative study. Medicine (Baltimore).
98(e15451)2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Heo DH, Lee DC and Park CK: Comparative
analysis of three types of minimally invasive decompressive surgery
for lumbar central stenosis: Biportal endoscopy, uniportal
endoscopy, and microsurgery. Neurosurg Focus. 46(E9)2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Heo DH, Quillo-Olvera J and Park CK: Can
percutaneous biportal endoscopic surgery achieve enough canal
decompression for degenerative lumbar stenosis? Prospective
case-control study. World Neurosurg. 120:e684–e689. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Choi DJ and Kim JE: Efficacy of Biportal
Endoscopic Spine Surgery for Lumbar Spinal Stenosis. Clin Orthop
Surg. 11:82–88. 2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Storzer B and Schnake KJ: Microscopic
bilateral decompression by unilateral approach in spinal stenosis.
Eur Spine J. 25 (Suppl 2):270–271. 2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Alimi M, Hofstetter CP, Pyo SY, Paulo D
and Härtl R: Minimally invasive laminectomy for lumbar spinal
stenosis in patients with and without preoperative
spondylolisthesis: Clinical outcome and reoperation rates. J
Neurosurg Spine. 22:339–352. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Rahman M, Summers LE, Richter B, Mimran RI
and Jacob RP: Comparison of techniques for decompressive lumbar
laminectomy: The minimally invasive versus the ‘classic’ open
approach. Minim Invasive Neurosurg. 51:100–105. 2008.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Phan K and Mobbs RJ: Minimally invasive
versus open laminectomy for lumbar stenosis: A systematic review
and meta-analysis. Spine. 41:E91–E100. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Palmer S, Turner R and Palmer R: Bilateral
decompression of lumbar spinal stenosis involving a unilateral
approach with microscope and tubular retractor system. J Neurosurg.
97:213–217. 2002.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Thomé C, Zevgaridis D, Leheta O, Bäzner H,
Pöckler-Schöniger C, Wöhrle J and Schmiedek P: Outcome after
less-invasive decompression of lumbar spinal stenosis: A randomized
comparison of unilateral laminotomy, bilateral laminotomy, and
laminectomy. J Neurosurg Spine. 3:129–141. 2005.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Knotkova H, Fine PG and Portenoy RK:
Opioid rotation: The science and the limitations of the
equianalgesic dose table. J Pain Symptom Manage. 38:426–439.
2009.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Parikh K, Tomasino A, Knopman J, Boockvar
J and Härtl R: Operative results and learning curve:
Microscope-assisted tubular microsurgery for 1- and 2-level
discectomies and laminectomies. Neurosurg Focus.
25(E14)2008.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Polikandriotis JA, Hudak EM and Perry MW:
Minimally invasive surgery through endoscopic laminotomy and
foraminotomy for the treatment of lumbar spinal stenosis. J Orthop.
10:13–16. 2013.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Tenenbaum S, Arzi H, Herman A, Friedlander
A, Levinkopf M, Arnold PM and Caspi I: Percutaneous posterolateral
transforaminal endoscopic discectomy: Clinical outcome,
complications, and learning curve evaluation. Surg Technol Int.
21:278–283. 2011.PubMed/NCBI
|
|
30
|
Torudom Y and Dilokhuttakarn T: Two portal
percutaneous endoscopic decompression for lumbar spinal stenosis:
Preliminary study. Asian Spine J. 10:335–342. 2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Park SM, Kim GU, Kim HJ, Choi JH, Chang
BS, Lee CK and Yeom JS: Is the use of a unilateral biportal
endoscopic approach associated with rapid recovery after lumbar
decompressive laminectomy? A preliminary analysis of a prospective
randomized controlled trial. World Neurosurg. 128:e709–e718.
2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Choi DJ, Choi CM, Jung JT, Lee SJ and Kim
YS: Learning curve associated with complications in biportal
endoscopic spinal surgery: Challenges and strategies. Asian Spine
J. 10:624–629. 2016.PubMed/NCBI View Article : Google Scholar
|