Introduction
Chronic kidney disease is a global health problem.
In recent years, the incidence of chronic kidney disease has been
gradually increasing. In China, the overall prevalence rate of
chronic kidney disease is estimated to be approximately 10.8% with
a high mortality (1-3).
Uremia belongs to the end-stage of chronic renal failure, which
causes a series of clinical reactions and body system damages,
seriously affecting patients' quality of life. If treatment is not
timely, uremia caused by renal failure may aggravate the disease
and eventually lead to death (3,4). At
present, findings have shown that hemodialysis combined with
hemoperfusion has a good effect on the treatment of uremia
(5,6). Hemodialysis can remove blood urea
nitrogen (BUN), creatinine (Cr) and bilirubin. In addition, it is
mainly effective in removing internal wastes and adjusting
acid-base balance through the principle of semipermeable membrane
dialysis (7). Hemoperfusion can
adsorb inflammatory mediators, such as interleukin (IL)-1, IL-6,
IL-8, tumor necrosis factor-α and prothrombin-activating factor, to
reduce inflammatory reaction (8-10).
Hemodialysis combined with hemoperfusion can make up for each other
and play different roles, thus achieving high efficiency in
removing various toxins and maintaining water-electrolyte balance
in the body (5,7). Although blood purification technology
and drug therapy have made progress, the mortality of chronic
kidney disease remains very high (5).
MicroRNA (miRNA) is a small regulatory RNA with a
length of 19-25 nucleotides that participates in
post-transcriptional gene silencing in all eukaryotes (11). The miRNA role in a variety of kidney
diseases, including nephrotic syndrome, renal fibrosis, lupus
nephritis and acute pyelonephritis has been previously shown
(12). In addition, previous
findings have shown that miR-155 plays an important role in
inflammation, immune response and formation of hematopoietic cells
(13). It has been reported that
miR-155 expression in liver tissues of patients with chronic liver
diseases is upregulated, indicating that miR-155 may be influential
in the progression of liver diseases, and it is a potential
biomarker (14). Zhang et al
(15) suggested that serum miR-155
may be regarded as a new target for early diagnosis and
intervention of inflammatory state in uremic dialytic patients by
detecting the changes of serum miR-155 level in those treated with
alprostadil. However, clinical efficacy monitoring and the risk
factors of miR-155 were not thoroughly studied.
By monitoring the changes of miR-155 expression in
serum of uremic patients before and after treatment, the aim of the
present study was mainly to explore the clinical value of miR-155
in hemodialysis combined with hemoperfusion treatment and the risk
factors affecting their efficacy.
Subjects and methods
General information
A total of 116 uremic patients admitted to the
People's Hospital of Chengyang (Qingdao, China) were selected as
the uremia group, including 65 males and 51 females, with an
average age of 51.32±8.97 years. In addition, 127 healthy subjects
who underwent health examination during the same period were
selected as the normal group, including 69 males and 58 females,
with an average age of 50.13±9.01 years.
The study was approved by the Ethics Committee of
the People's Hospital of Chengyang (no. CYPH2017011A), and all the
patients and their families were informed prior to the study and
signed a complete informed consent form.
Inclusion criteria were as follows: Uremic patients
who met the disease diagnosis and were in relatively stable
condition; patients who showed good compliance and had complete
clinical data; patients who received routine examinations, such as
urine routine test, blood routine test, electrocardiogram; patients
with normal liver and kidney function after admission; patients who
were accompanied by their family when admitted to the hospital. All
subjects that participated in the study signed an informed consent
form.
Exclusion criteria were as follows: Patients with
liver dysfunction, severe organ lesions, history of craniocerebral
trauma, autoimmune system defects, or mental hereditary diseases;
patients who did not actively cooperate or had habits harmful to
the health such as long-term smoking and alcoholism.
Treatment plan
Patients with uremia were treated routinely after
admission; in order to avoid bad eating habits, their blood
pressure and blood sugar were controlled, and they received other
symptomatic and supportive treatment. They were treated via
hemodialysis combined with hemoperfusion. Hemodialysis was
conducted using a German Fressnius 4008S type hemodialysis machine,
and anticoagulation was conducted by carbonate dialysate and low
molecular heparin sodium, with a surface area of 1.3 m2,
ultrafiltration coefficient of 40 ml/h mmHg, blood flow of 200-250
ml/min, and dialysate flow of 500 ml/min, 4 h each time, 3 times a
week. Boxin MG 150 disposable hemoperfusion device was used, and
the perfusion device was connected in series to the front end of
the dialyzer. Two hours after treatment, the perfusion device was
taken down after its adsorption capacity was saturated,
hemodialysis was performed for 2 h separately, and joint treatment
was performed once a week. Relevant indicators were compared 12
weeks after treatment. In addition, adequate sleep, limited water,
low salt and low fat diet were ensured during the treatment of
patients.
Detection of serum miR-155
In the morning, 4 ml of fasting elbow venous blood
was collected from the subjects in the two groups after admission
as well as uremia patients after treatment, respectively. The
collected blood was placed in a centrifuge tube to collect upper
serum, centrifugation conditions were as follows: 1006.2 x g, 10
min, 10 cm (radius), 4˚C (temperature), and then it was placed in a
refrigerator at -80˚C for testing. Total RNA in serum was extracted
by TRIzol® kit (Invitrogen) according to the
manufacturer's instructions, and the template RNA was digested and
treated with DNaseI to eliminate DNA contamination. An ultraviolet
spectrophotometer (Beijing UP General Technology Co., Ltd.) was
used to measure the purity and concentration; the RNA sample was
then reverse transcribed into cDNA, and the procedure was strictly
carried out in accordance with the instructions of cDNA reverse
transcription kit (Takara). Reverse transcription-quantitative PCR
(RT-qPCR) was used for detection, and SYBR PrimeScript miRNA
RT-qPCR kit (Takara) was used for RT-qPCR in ABI Prism 7500
(Applied Biosystems). PCR reaction conditions were as follows:
Enzyme activation at 95˚C for 10 min, denaturation at 95˚C for 15
sec, annealing/extension at 60˚C for 1 min, a total of 40 cycles.
Primers for this experiment were designed by Primer Premier 5.0
(Premier), and generated by Tianjin Saier Biotechnology Co., Ltd.
U6 was used as internal reference, and the specific primer
sequences are shown in Table I. The
above system configuration was strictly in accordance with the
instructions, and the content of miR-155 was calculated by
2-ΔΔCq (16).
 | Table IPrimer sequences. |
Table I
Primer sequences.
| Genes | Upstream | Downstream |
|---|
| miR-155 |
5'-GTGCAGGGTCCGAGGT-3' |
5'-CGCTTAATGCTAATCGTGATAGG-3' |
| U6 |
5'-CTCGCTTCGGCAGCACA-3' |
5'-AACGCTTCACGAATTTGCGT-3' |
Efficacy evaluation (17,18)
Scoring for efficacy evaluation was as follows:
Marked effect: After treatment, clinical symptoms and signs of
patients significantly improved; improvement: The clinical symptoms
and signs of patients improved after relevant treatment, but these
were not significant; invalid: Patients' clinical symptoms and
signs did not change or deteriorate significantly after relevant
treatment.
Outcome measures
Clinically related indicators of uremic patients
before and after treatment were observed, including BUN, Cr,
β2-microglobulin (β2-MG), parathyroid hormone (PTH), C-reactive
protein (CRP) and IL-6. The changes of serum miR-155 level and
evaluation of the efficacy on uremic patients were observed to
analyze the risk factors affecting their efficacy.
Statistical analysis
SPSS 20.0 (IBM Corp., Armonk) was used for
statistical analysis, and GraphPad Prism 7 (San Diego Graphpad
Software Co., Ltd.) was used to draw images of the collected data.
The counting data were expressed as [n (%)], and the Chi-square
test was used for inter-group comparison. The measurement data were
expressed as mean ± standard deviation (SD), independent-samples
t-test and paired sample t-test were used for comparison between
the two groups before and after therapy, and receiver operating
characteristic curve (ROC) was used to predict and evaluate the
efficacy of uremia patients. Pearson's correlation coefficient was
used for bivariate normal distribution data, Spearman's correlation
coefficient was used to analyze the correlation between grade and
variable, and the multivariate logistic regression was used to
analyze the risk factors affecting their treatment, with
statistical significance (P<0.05).
Results
Comparison of clinical general
data
Statistical comparison of clinical general data
between the two groups is shown in Table II. There was no significant
difference with regard to sex, age, average age and body mass index
(BMI) between the uremia and normal groups (P>0.05). Hemoglobin
and blood albumin in uremia group were lower than those in normal
group (P<0.05), whereas total cholesterol, triglyceride,
low-density lipoprotein and mean arterial pressure in uremia group
were higher than those in normal group (P<0.05).
 | Table IIComparison of general clinical data
between the two groups [n (%), mean ± SD]. |
Table II
Comparison of general clinical data
between the two groups [n (%), mean ± SD].
| Clinical data | Uremia group
(n=116) | Normal group
(n=127) |
F/χ2 | P-value |
|---|
| Gender | | | 0.071 | 0.790 |
|
Male | 65 (56.03) | 69 (54.33) | | |
|
Female | 51 (43.97) | 58 (45.67) | | |
| Age, years | | | 0.078 | 0.780 |
|
<50 | 50 (43.10) | 57 (44.88) | | |
|
≥50 | 66 (56.90) | 70 (55.12) | | |
| Average age
(years) | 51.32±8.97 | 50.13±9.01 | 1.031 | 0.963 |
| BMI
(kg/m2) | 24.01±3.43 | 23.89±3.13 | 0.285 | 0.315 |
| Hemoglobin
(g/l) | 88.72±15.49 | 144.38±12.89 | 30.540 | <0.05 |
| Blood albumin
(g/l) | 36.14±5.29 | 45.21±4.45 | 14.500 | <0.05 |
| Total cholesterol
(mmol/l) | 5.08±1.09 | 4.15±1.32 | 5.956 | <0.05 |
| Triglycerides
(mmol/l) | 1.82±0.68 | 1.02±0.51 | 10.430 | <0.05 |
| Low-density
lipoprotein (mmol/l) | 3.05±0.82 | 2.31±0.87 | 6.807 | <0.05 |
| Mean arterial
pressure (mmHg) | 112.37±10.01 | 92.35±8.07 | 17.230 | <0.05 |
Evaluation of efficacy of changes in
serum miR-155 level on uremic patients
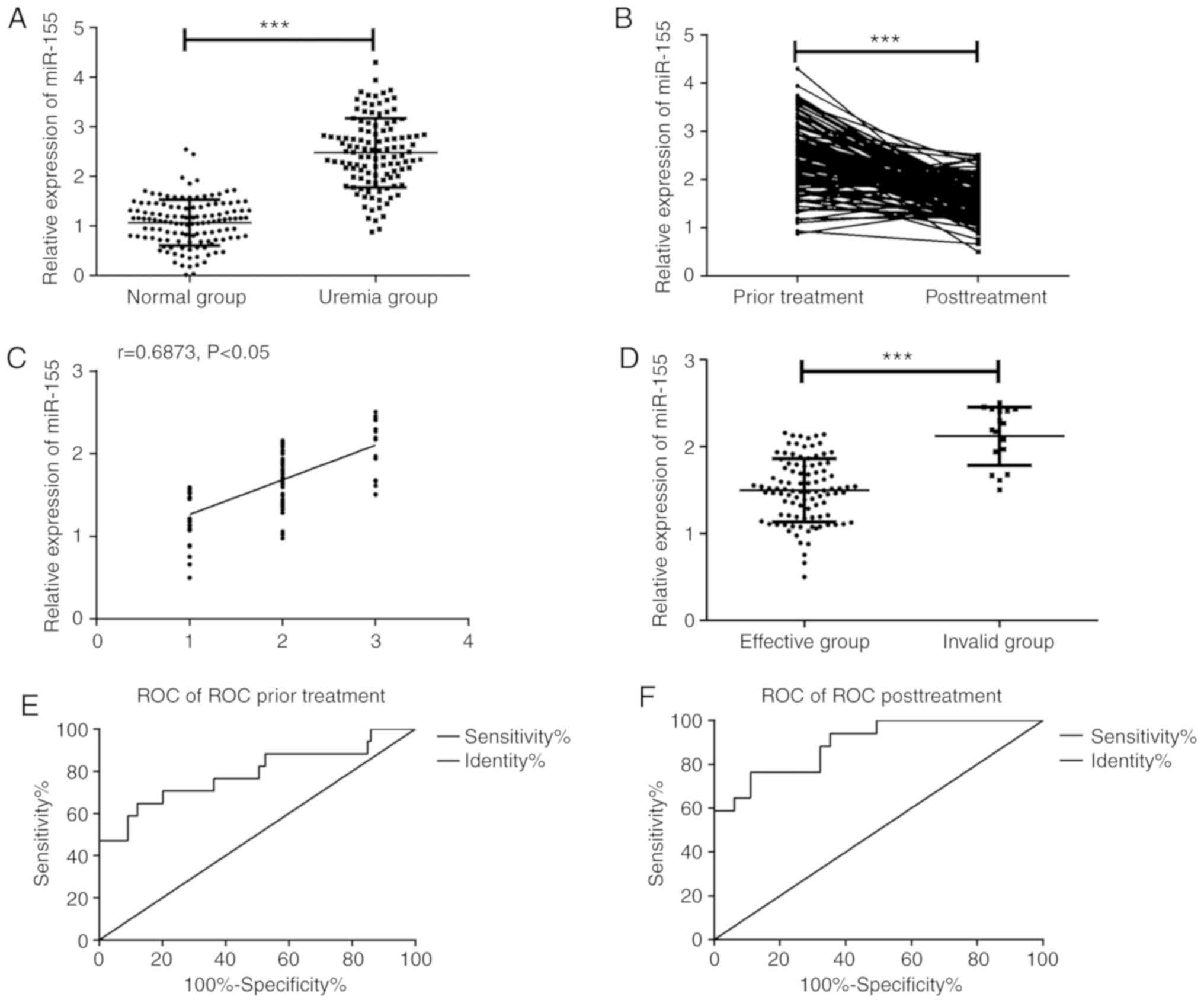
According to the detection of serum miR-155 levels
in the two groups, the serum miR-155 level in uremic patients was
significantly higher than that in the normal group (Fig. 1A, P<0.001), and that in uremic
patients after treatment was significantly lower than before
treatment (Fig. 1B, P<0.001);
there were 43 markedly effective cases, 56 improved cases and 17
invalid cases after treatment. As is evident in Fig. 1C, the miR-155 level was significantly
positively correlated with the efficacy (r=0.6873, P<0.05); the
worse the efficacy was, the higher the miR-155 level was. In
addition, according to the efficacy, patients were divided into
effective group (n=99) and invalid group (n=17); the serum miR-155
level of patients in the invalid group was significantly higher
than that in the effective group (P<0.001; Fig. 1D). ROC curve was drawn according to
miR-155 level before and after treatment; area under the curve
(AUC) of miR-155 level used for predicting efficacy of uremic
patients before treatment was 0.788, sensitivity was 64.71% and
specificity was 87.88% (Fig. 1E);
AUC of miR-155 level for evaluating efficacy of uremic patients
after treatment was 0.895, sensitivity was 76.47% and specificity
was 88.89% (Fig. 1F).
Changes of clinically related
indicators
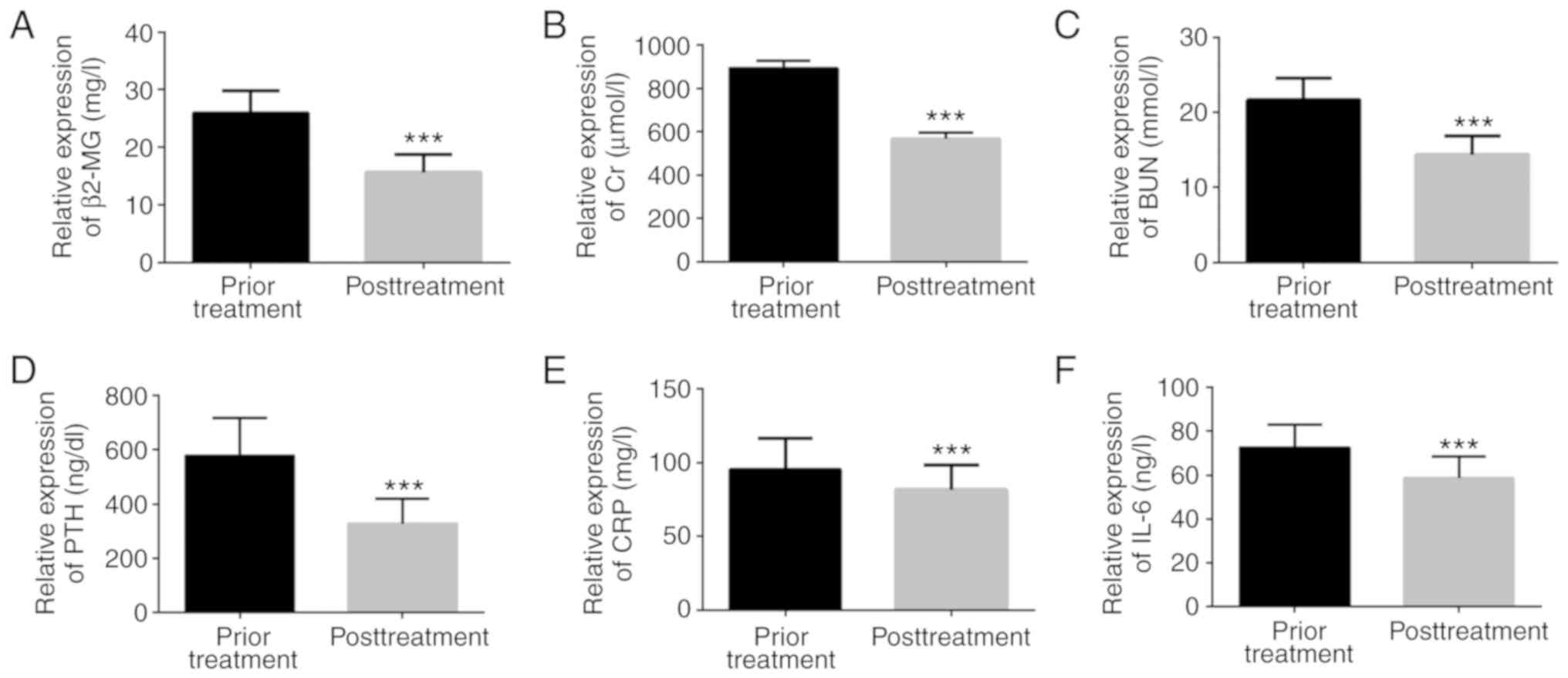
The levels of serum clinically related indicators
and inflammatory factors in uremic patients before and after
treatment were detected; β2-MG, Cr, BUN, PTH, CRP, and IL-6 levels
after treatment were significantly lower than those before
treatment, with statistically significant difference (P<0.001;
Fig. 2).
Correlation between serum miR-155
level and clinical related indicators before treatment
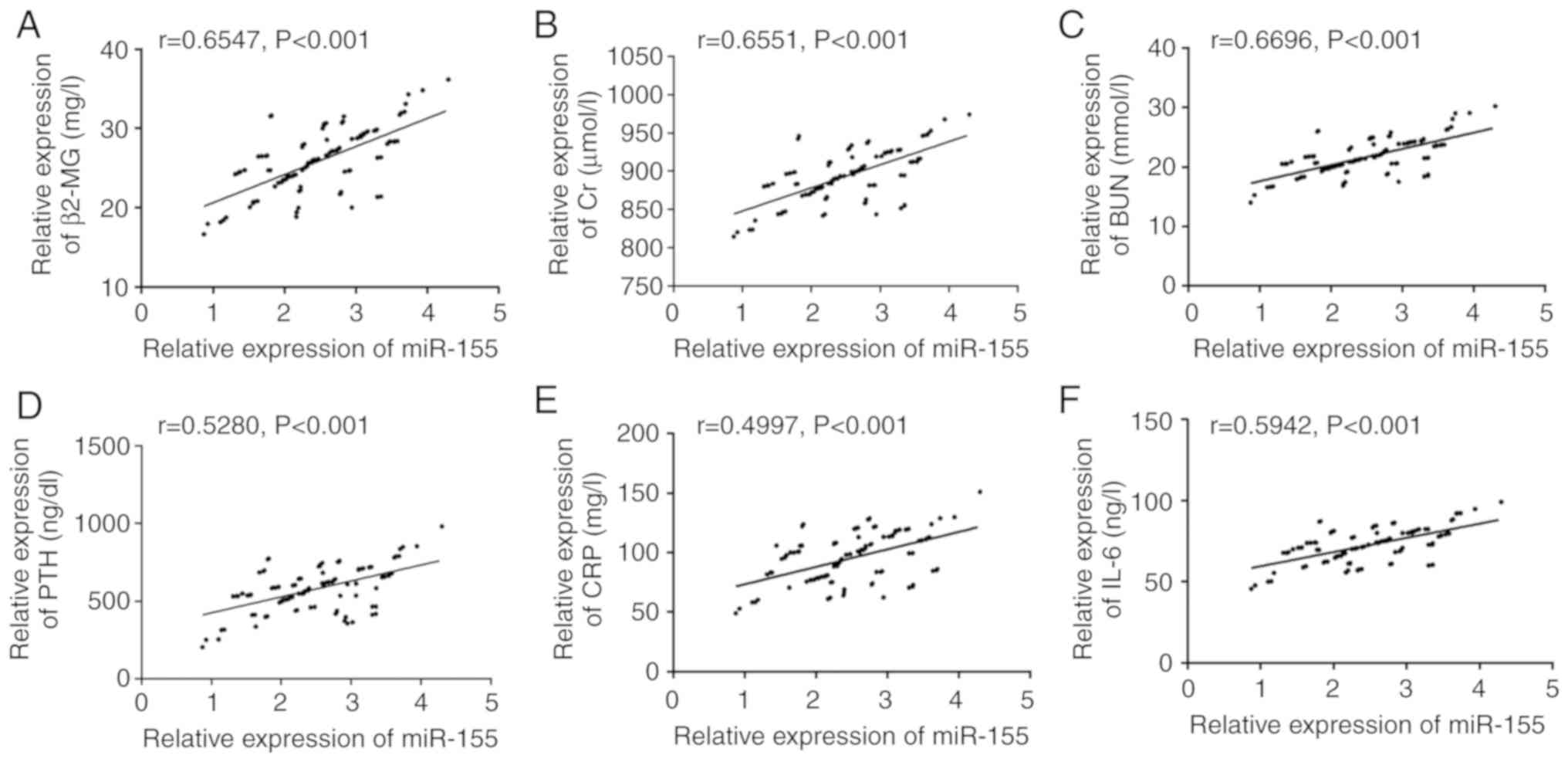
Pearson's correlation coefficient analysis showed
that prior to treatment, serum miR-155 level was significantly
positively correlated with clinically related indicators such as
β2-MG, Cr, BUN and PTH (P<0.001; Fig.
3A-D), as well as with levels of CRP and IL-6 inflammatory
factors (P<0.001; Fig. 3E and
F).
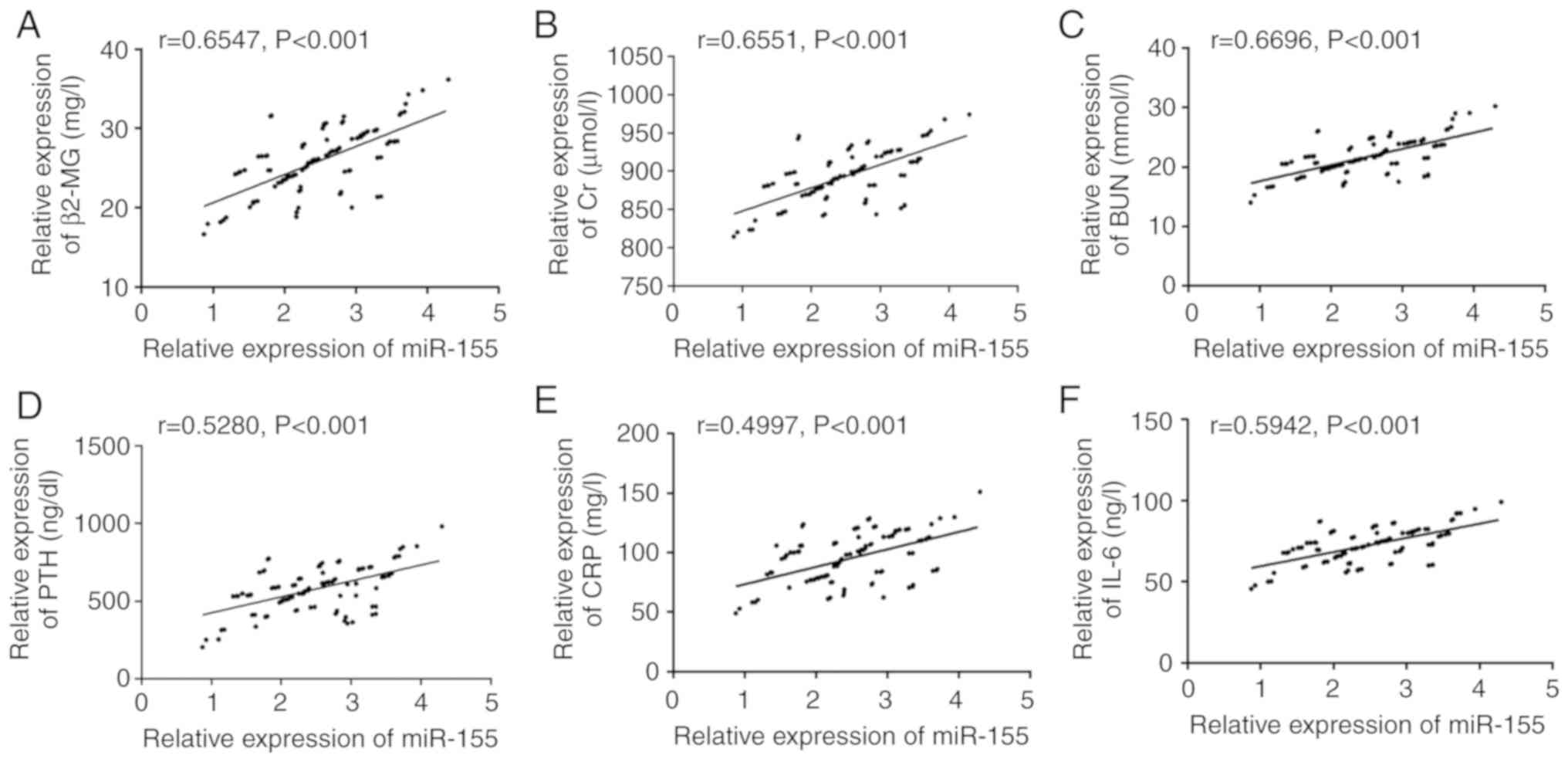 | Figure 3Correlation between serum miR-155
level and clinically related indicators before treatment. (A)
miR-155 was positively correlated with β2-MG before treatment
(r=0.6547, P<0.001). (B) Before treatment, miR-155 was
positively correlated with Cr (r=0.6551, P<0.001). (C) Before
treatment, miR-155 was positively correlated with BUN (r=0.6696,
P<0.001). (D) Before treatment, miR-155 was positively
correlated with PTH (r=0.5280, P<0.001). (E) Before treatment,
miR-155 was positively correlated with CRP (r=0.4997, P<0.001).
(F) Before treatment, miR-155 was positively correlated with IL-6
(r=0.5942, P<0.001). |
Correlation between serum miR-155
level and clinically related indicators after treatment
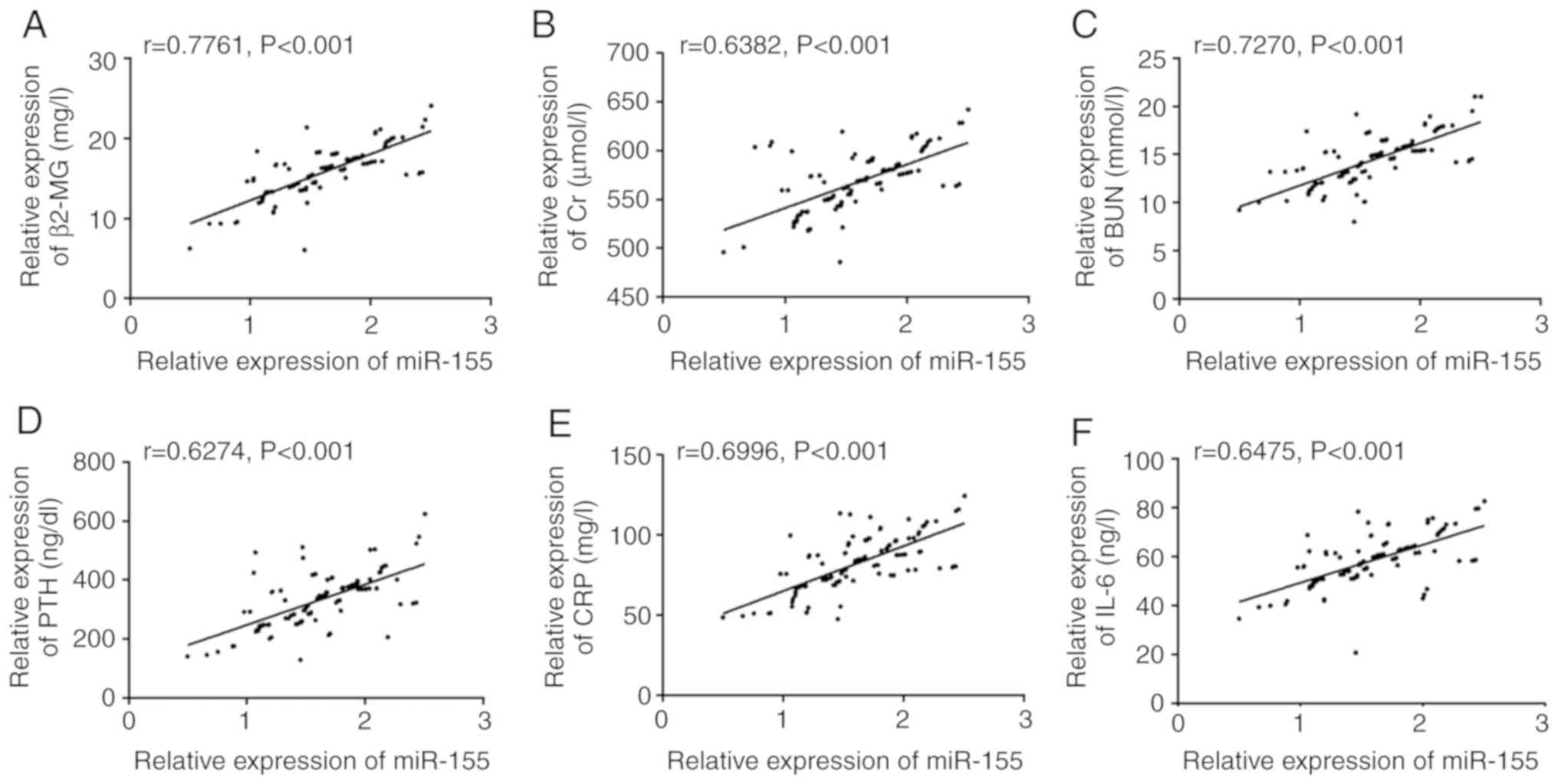
Pearson's correlation coefficient analysis revealed
that after treatment, serum miR-155 level was significantly
positively correlated with clinically related indicators such as
β2-MG, Cr, BUN and PTH (P<0.001; Fig.
4A-D), as well as with levels of CRP and IL-6 inflammatory
factors (P<0.001; Fig. 4E and
F).
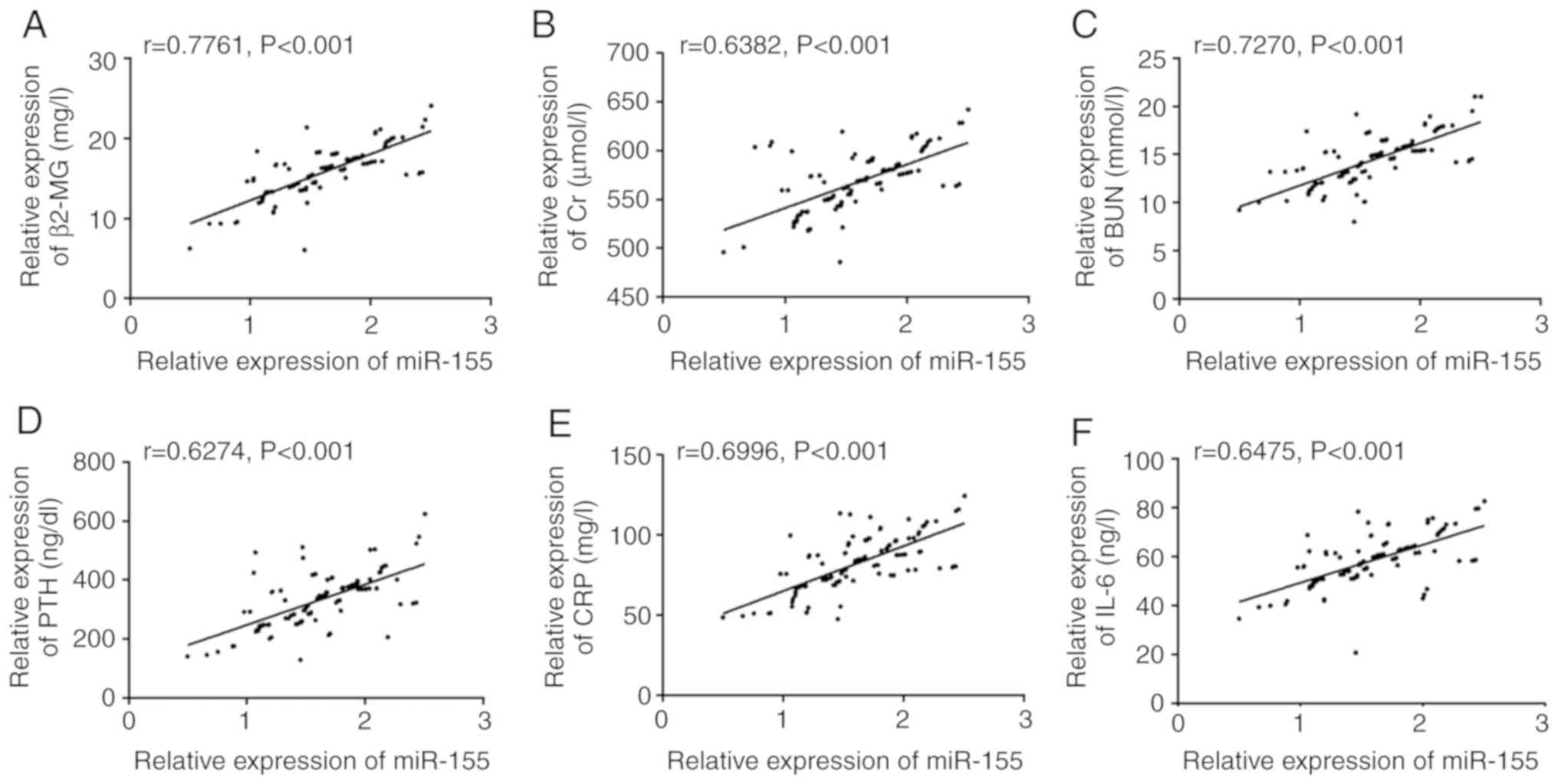 | Figure 4Correlation between serum miR-155
level and clinically related indicators after treatment. (A) After
treatment, miR-155 level was positively correlated with β2-MG
(r=0.7761, P<0.001). (B) After treatment, miR-155 level was
positively correlated with Cr (r=0.6382, P<0.001). (C) After
treatment, miR-155 level was positively correlated with BUN
(r=0.7270, P<0.001). (D) After treatment, miR-155 level was
positively correlated with PTH (r=0.6274, P<0.001). (E) After
treatment, miR-155 level was positively correlated with CRP
(r=0.6996, P<0.001). (F) After treatment, miR-155 level was
positively correlated with IL-6 (r=0.6475, P<0.001). |
Analysis on influencing factors of
efficacy
According to the efficacy, uremic patients were
divided into the effective (n=99) and invalid (n=17) groups and
were assessed via univariate analysis. There were differences in
β2-MG, Cr, BUN, PTH, CRP, IL-6, and miR-155 levels between the two
groups, as shown in Table III
(P<0.05). Results of Logistic regression analysis on risk
factors indicated that β2-MG (HR: 7.705, 95% CI: 1.380-43.030), Cr
(HR: 6.979, 95% CI: 0.921-52.906), BUN (HR: 6.869, 95% CI:
1.042-45.281), PTH (HR: 6.859, 95% CI: 1.046-44.995), CRP (HR:
7.901, 95% CI: 1.202-51.952), IL-6 (HR: 7.319, 95% CI:
1.036-51.687), and miR-155 (HR: 9.562, 95% CI: 1.520-60.163) were
all risk factors affecting their efficacy. More details are
provided in Table IV.
 | Table IIIUnivariate analysis [n (%), mean ±
SD]. |
Table III
Univariate analysis [n (%), mean ±
SD].
| Variables | Effective group
(n=99) | Invalid group
(n=17) |
t/χ2 | P-value |
|---|
| Gender | | | 0.063 | 0.802 |
|
Male | 55 (55.56) | 10 (58.82) | | |
|
Female | 44 (44.44) | 7 (41.18) | | |
| Age, years | | | 0.910 | 0.340 |
|
<50 | 45 (45.45) | 5 (29.41) | | |
|
≥50 | 54 (54.55) | 12 (70.59) | | |
| BMI
(kg/m2) | 23.93±3.09 | 24.09±3.12 | 0.401 | 0.689 |
| β2-MG (mg/l) | 15.02±2.74 | 19.30±2.70 | 12.260 | <0.05 |
| Cr (µmol/l) | 563.59±28.90 | 594.15±24.37 | 11.860 | <0.05 |
| BUN (mmol/l) | 13.82±2.23 | 17.48±1.90 | 13.810 | <0.05 |
| PTH (ng/dl) | 308.64±76.88 | 444.64±86.85 | 12.876 | <0.05 |
| CRP (mg/l) | 79.26±15.84 | 95.84±15.82 | 8.155 | <0.05 |
| IL-6 (ng/l) | 56.42±8.89 | 70.66±7.53 | 13.510 | <0.05 |
| miR-155 level | 1.55±0.42 | 1.80±0.42 | 4.635 | <0.05 |
 | Table IVMultivariate analysis. |
Table IV
Multivariate analysis.
| Variables | β | SD | χ2 | P-value | HR (95% CI) |
|---|
| β2-MG (mg/l) | 2.042 | 0.878 | 5.414 | 0.020 | 7.705
(1.380-43.030) |
| Cr (µmol/l) | 1.943 | 1.034 | 3.534 | 0.048 | 6.979
(0.921-52.906) |
| BUN (mmol/l) | 1.927 | 0.962 | 4.011 | 0.045 | 6.869
(1.042-45.281) |
| PTH (ng/dl) | 1.926 | 0.960 | 4.026 | 0.045 | 6.859
(1.046-44.995) |
| CRP (mg/l) | 2.067 | 0.961 | 4.627 | 0.031 | 7.901
(1.202-51.952) |
| IL-6 (ng/l) | 1.990 | 0.997 | 3.983 | 0.046 | 7.319
(1.036-51.687) |
| miR-155 level | 2.258 | 0.938 | 5.789 | 0.016 | 9.562
(1.520-60.163) |
Discussion
Uremia mainly results from the decline of glomerular
filtration function which causes acidolysis disorder, water
electrolyte disorder and other phenomena. It leads to the toxic
metabolites retention phenomenon, thus affecting blood, digestive
tract and nerve, resulting in severe systemic symptoms (19,20).
Recently, with the popularization and development of blood
purification technology, good news has been afforded to patients
with end-stage renal disease, and their quality of life has been
significantly improved (5,21). However, various factors in the
process of hemodialysis still seriously affect the efficacy of
maintenance hemodialysis patients, and the experiment of this study
further clarified the diagnosis and treatment experience of uremia
by analyzing the changes of miR-155 in the treatment process.
Findings have shown that triglyceride, total
cholesterol, blood glucose, and low-density lipoprotein cholesterol
increased significantly in patients with chronic kidney disease
(22). Previous results have shown
that hemoglobin and albumin in uremic patients were lower than
those in healthy individuals (15).
Those results were similar to the results of this study, showing
that the occurrence of the disease may lead to the disorder of
lipid and blood metabolism to some extent. Additionally, miR-155
upregulated significantly in clear cell renal cell carcinoma
tissues compared with corresponding normal tissues (23). The miR-155 expression in peripheral
blood mononuclear cells of patients with rheumatoid arthritis also
increased significantly, and it indicated that miR-155 had a
correlation with the activity of the disease (24). The current study examined the serum
miR-155 level of uremic patients and normal subjects, and the
results showed that the level in the former was significantly
higher than that in the latter, which was similar to the results of
Zhang et al (15). We further
observed the changes of miR-155 level before and after treatment
and found that the level of uremic patients after treatment was
significantly lower than that before treatment, suggesting that
hemodialysis combined with hemoperfusion treatment could
significantly lower miR-155 level. Nevertheless, there was still
doubt as to whether its expression was linked to the efficacy. In
addition, we found that the miR-155 level after treatment was
significantly positively correlated with the efficacy through
Spearman's correlation analysis, and that of patients in the
invalid group was significantly higher than that in the effective
group; the worse the efficacy was, the higher the miR-155 level
was. The results suggested that miR-155 may be used as a
therapeutic indicator for uremic patients. Monitoring the level of
miR-155 can reflect the state of an illness in time, which has a
certain clinical value in replacing treatment plans without delay.
Ulivi et al (25) suggested
that serum miR-20b, miR-29b, and miR-155 levels could be used as
efficacy predictors of bevacizumab in patients with metastatic
colorectal cancer, and were correlated with disease
progression-free survival and overall survival rate. In this study,
ROC curves were drawn according to miR-155 levels before and after
treatment, and it was found that those before and after treatment
could be used to predict and evaluate the efficacy of uremic
patients, and were expected to become biomarkers. Nevertheless,
more studies are needed to prove the relationship between miR-155
level and long-term survival of uremic patients. Compared with
previous studies, Liang et al (26) observed that the levels of miR-34a,
miR-205, and miR-155 in urine of patients with IgA nephropathy were
significantly lower than those of normal subjects. Then, they were
divided into complete sustained-release group and incomplete
sustained-release group according to efficacy. Their findings
indicated there was no remarkable difference in the miR-155 levels
in urine of the two groups (P>0.05). Furthermore, it has been
reported that a high miR-155 expression was an independent
predictor of lower complete-sustained release rate and shorter
overall survival in patients with acute myeloid leukemia (27). Combined with this study, it was
suggested that the miR-155 expression was different in varying
diseases and samples, its abnormal expression could be used for the
clinical monitoring of various diseases, and its detection and
prediction value in chronic kidney disease still required further
research.
β2-MG and PTH belong to macromolecular toxins; when
the human body is in an inflammatory state, it accelerates the
production and release of β2-MG, mainly through renal degradation
and re-absorption into the body (28,29).
Therefore, the concentration of β2-MG can be used to reflect the
filtration function of the kidney. Accumulation of β2-MG and
metabolic disorder of uremic patients may produce a large amount of
PTH, which is involved in the occurrence and development of renal
diseases (29,30). Cr and BUN belong to small molecular
toxins and are one of the important factors causing uremic symptoms
and complications (7,31,32).
Inflammation is a vital factor that causes the occurrence or
aggravation of various diseases, and is also crucial in the
pathogenesis of complications in uremic patients (33). IL-6 and CRP are important members of
inflammatory cytokines, have strong biological effects and can
regulate cellular immune response, and upregulate when the body is
in a pathological state (34,35). In
this study, the levels of serum clinically related indicators and
inflammatory factors in uremic patients before and after treatment
were detected, and it was found that the β2-MG, Cr, BUN, PTH, CRP,
and IL-6 levels after treatment were significantly lower than those
prior to treatment. This showed that hemodialysis combined with
hemoperfusion could effectively remove toxins and improve the
inflammatory state of uremic patients, which was consistent with
the results of previous studies (6,31,36);
hemodialysis combined with hemoperfusion had a high value in
treating uremia. The Pearson correlation coefficient analysis
revealed that before treatment, serum miR-155 level was
significantly positively correlated with clinically related
indicators of β2-MG, Cr, BUN, and PTH (P<0.001), and it was
significantly positively correlated with levels of CRP and IL-6
inflammatory factors (P<0.001). The results further verified
that miR-155 were correlated with disease-related indicators of
uremic patients, could effectively reflect their disease state, and
provided a new target for intervention or treatment thereof. At the
same time, combined with previous studies, miR-155 further
confirmed that miR-155 was able to participate in the
pathophysiological process of inflammatory state of uremic patients
by regulating the expression levels of IL-6 and CRP (15). It was reported that proteinuria ≥1.0
g/24 h, high systolic pressure, and diastolic pressure were the
risk factors affecting the improvement of blood pressure control in
patients with chronic kidney disease by logistic regression
analysis (37). Wang et al
(38) pointed out that a high level
of miR-155 was an independent risk factor for poor prognosis and
lymphocyte infiltration in non-small cell lung cancer. To the best
of our knowledge, there is currently no study on the risk factors
for efficacy of uremic patients. The present study employed
logistic regression analysis on risk factors, and the results
showed that high levels of β2-MG, Cr, BUN, PTH, CRP, IL-6, and
miR-155 were all risk factors affecting their efficacy. Close
attention should be given to the changes of the above indicators
during uremia treatment to provide some basis for changing the
treatment plans.
In this study, the changes of miR-155 expression in
serum of uremic patients before and after treatment were detected,
and the risk factors affecting their efficacy were analyzed.
However, this study has certain limitations, as it only evaluates
the efficacy based on the basic efficacy time and does not observe
the long-term effects. Moreover, due to the lack of in vitro
experiments, the mechanism of miR-155 on uremia is still at the
stage of speculation. In future research, rigorous experimental
analysis should be carried out as early as possible to obtain the
optimal experimental results against the above limitations.
To sum up, the expression level of miR-155 in serum
of uremic patients was upregulated significantly and monitoring
miR-155 can effectively reflect its efficacy and inflammatory
state.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HL conceived the study and wrote the manuscript. FQ
and FT analyzed and interpreted the patient general data. XS and AG
performed PCR. LS and JL were responsible for the analysis of the
observation indicators. All authors read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The People's Hospital of Chengyang (Qingdao, China). The patients
who participated in this research had complete clinical data. All
patients and their families were informed prior to the study and
signed a complete informed consent form.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Scherer A, Günther OP, Balshaw RF,
Hollander Z, Wilson-McManus J, Ng R, McMaster WR, McManus BM and
Keown PA: Alteration of human blood cell transcriptome in uremia.
BMC Med Genomics. 6(23)2013.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chapagain A, Caton PW, Kieswich J,
Andrikopoulos P, Nayuni N, Long JH, Harwood SM, Webster SP, Raftery
MJ, Thiemermann C, et al: Elevated hepatic 11β-hydroxysteroid
dehydrogenase type 1 induces insulin resistance in uremia. Proc
Natl Acad Sci USA. 111:3817–3822. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Shang W, Shen Y, Gao S, Feng G, Feng Y,
Wang Z and Zhang X: Comparison of HLA-A, -B and -DRB1 loci
polymorphism between kidney transplants of uremia patients and
healthy individuals in Central China. PLoS One.
11(e0165426)2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Vitetta L and Gobe G: Uremia and chronic
kidney disease: The role of the gut microflora and therapies with
pro- and prebiotics. Mol Nutr Food Res. 57:824–832. 2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lu W and Jiang GR: HD/HP versus HD trial
Group. Randomised, open-label, multicentre trial comparing
haemodialysis plus haemoperfusion versus haemodialysis alone in
adult patients with end-stage renal disease (HD/HP vs. HD): Study
protocol. BMJ Open. 8(e022169)2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Li J, Li D, Xu Y, Wang A, Xu C and Yu C:
The optimal timing of hemoperfusion component in combined
hemodialysis-hemoperfusion treatment for uremic toxins removal. Ren
Fail. 37:103–107. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Li Z, Wang G, Zhen G, Zhang Y, Liu J and
Liu S: Effects of hemodialysis combined with hemoperfusion on
severe acute pancreatitis. Turk J Gastroenterol. 29:198–202.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Wang YT, Fu JJ, Li XL, Li YR, Li CF and
Zhou CY: Effects of hemodialysis and hemoperfusion on inflammatory
factors and nuclear transcription factors in peripheral blood cell
of multiple organ dysfunction syndrome. Eur Rev Med Pharmacol Sci.
20:745–750. 2016.PubMed/NCBI
|
|
9
|
Xu X, Yu Z, Liang Y, Gao H, Liu Y and Yu
Y: Mumps caused by paraquat-induced poisoning: A case report. Exp
Ther Med. 13:401–404. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Li MQ, Shi ZX, Xu JY, Lu B, Li JQ, Xu YJ,
Wang XM, Li SM and Mo X: Hemodiafiltration combined with
resin-mediated absorption as a therapy for hyperlipidemic acute
pancreatitis. Cell Biochem Biophys. 69:699–702. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wang GK, Zhu JQ, Zhang JT, Li Q, Li Y, He
J, Qin YW and Jing Q: Circulating microRNA: A novel potential
biomarker for early diagnosis of acute myocardial infarction in
humans. Eur Heart J. 31:659–666. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mukhadi S, Hull R, Mbita Z and Dlamini Z:
The role of microRNAs in kidney disease. Noncoding RNA. 1:192–221.
2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ji H, Tian D, Zhang B, Zhang Y, Yan D and
Wu S: Overexpression of miR-155 in clear-cell renal cell carcinoma
and its oncogenic effect through targeting FOXO3a. Exp Ther Med.
13:2286–2292. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Blaya D, Aguilar-Bravo B, Hao F,
Casacuberta-Serra S, Coll M, Perea L, Vallverdú J, Graupera I, Pose
E, Llovet L, et al: Expression of microRNA-155 in inflammatory
cells modulates liver injury. Hepatology. 68:691–706.
2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zhang W, Shi L, Zhang H, Wang C, Gao S, Ma
Y, Li W and Liu J, Wang J and Liu J: Effect of alprostadil on serum
level of miRNA-155 in uremic patients. Zhong Nan Da Xue Xue Bao Yi
Xue Ban. 40:735–741. 2015.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
16
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Cai W, Chen WL and Fu HL: Effect of
Muxiang shunqi pill on digestive disorders of prephase uremia
patients and its mechanism. Zhongguo Zhong Xi Yi Jie He Za Zhi.
37:34–38. 2017.PubMed/NCBI(In Chinese).
|
|
18
|
Xue W, Zhao Y, Yuan M and Zhao Z: Chinese
herbal bath therapy for the treatment of uremic pruritus:
Meta-analysis of randomized controlled trials. BMC Complement
Altern Med. 19(103)2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lisowska-Myjak B: Uremic toxins and their
effects on multiple organ systems. Nephron Clin Pract. 128:303–311.
2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Li G, Ma H, Yin Y and Wang J: CRP, IL-2
and TNF-α level in patients with uremia receiving hemodialysis. Mol
Med Rep. 17:3350–3355. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zhang J, Yuan Y, An X, Ouyang C, Ren H,
Yang G, Yu X, Lv X, Zhang B, Wang N, et al: Comparison of combined
blood purification techniques in treatment of dialysis patients
with uraemic pruritus. Int J Clin Exp Med. 9:8563–8568. 2016.
|
|
22
|
Belarbia A, Nouira S, Sahtout W, Guedri Y
and Achour A: Metabolic syndrome and chronic kidney disease. Saudi
J Kidney Dis Transpl. 26:931–940. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Gao Y, Ma X, Yao Y, Li H, Fan Y, Zhang Y,
Zhao C, Wang L, Ma M, Lei Z and Zhang X: miR-155 regulates the
proliferation and invasion of clear cell renal cell carcinoma cells
by targeting E2F2. Oncotarget. 7:20324–30337. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kurowska-Stolarska M, Alivernini S,
Ballantine LE, Asquith DL, Millar NL, Gilchrist DS, Reilly J, Ierna
M, Fraser AR, Stolarski B, et al: MicroRNA-155 as a proinflammatory
regulator in clinical and experimental arthritis. Proc Natl Acad
Sci USA. 108:11193–11198. 2011.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ulivi P, Canale M, Passardi A, Marisi G,
Valgiusti M, Frassineti GL, Calistri D, Amadori D and Scarpi E:
Circulating plasma levels of miR-20b, miR-29b and miR-155 as
predictors of bevacizumab efficacy in patients with metastatic
colorectal cancer. Int J Mol Sci. 19(307)2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Liang S, Cai GY, Duan ZY, Liu SW, Wu J, Lv
Y, Hou K, Li ZX, Zhang XG and Chen XM: Urinary sediment miRNAs
reflect tubulointerstitial damage and therapeutic response in IgA
nephropathy. BMC Nephrol. 18(63)2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Marcucci G, Maharry KS, Metzeler KH,
Volinia S, Wu YZ, Mrózek K, Nicolet D, Kohlschmidt J, Whitman SP,
Mendler JH, et al: Clinical role of microRNAs in cytogenetically
normal acute myeloid leukemia: miR-155 upregulation independently
identifies high-risk patients. J Clin Oncol. 31:2086–2093.
2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Dung NH, Kien NT, Hai NTT, Cuong PT, Huong
NTT, Quyen DBQ, Tuan NM, Ha DM, Kien TQ, Dung NTT, et al: Measuring
serum beta2-microglobulin to predict long-term mortality in
hemodialysis patients using low-flux dialyzer reuse. Ther Clin Risk
Manag. 15:839–846. 2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Chen L, Fan D and Shi X: Comparison of the
effects of different blood purification methods on removal of
macromolecules in uremia. Chin J Primar Med Pharm. 24:1445–1449.
2017.(In Chinese).
|
|
30
|
Levine BS, Rodríguez M and Felsenfeld AJ:
Serum calcium and bone: Effect of PTH, phosphate, vitamin D and
uremia. Nefrologia. 34:658–669. 2014.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
31
|
Gao P, Ma JR, Zhao L, Pei GC, Shi GJ and
Li L: Effect of high-flux and low-flux hemodialysis on the side
metabolites and cytokines in patients with uremia. J Hainan Med
Univ. 23:61–64. 2017.
|
|
32
|
Chen Y, Duan J, Guo J, Shang E, Tang Y,
Qian Y, Tao W and Liu P: Yuanhuapine-induced intestinal and
hepatotoxicity were correlated with disturbance of amino acids,
lipids, carbohydrate metabolism and gut microflora function: A rat
urine metabonomic study. J Chromatogr B Analyt Technol Biomed Life
Sci. 1026:183–192. 2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Carrero JJ and Stenvinkel P: Inflammation
in end-stage renal disease-what have we learned in 10 years? Semin
Dial. 23:498–509. 2010.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Zhou H, Zhou D, Lu J, Wu C and Zhu Z:
Effects of pre-cardiopulmonary bypass administration of
dexmedetomidine on cardiac injuries and the inflammatory response
in valve replacement surgery with a sevoflurane postconditioning
protocol: A pilot study. J Cardiovasc Pharmacol. 74:91–97.
2019.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Shao QY, Wan C, Liu J and Zhang M: Effect
of peritoneal dialysis on inflammatory factors, nutritional index
and renal function in patients with chronic renal failure. J Hainan
Med Univ. 23:87–90. 2017.
|
|
36
|
Xiangming LI, Zhang W and Shen D: The
effect of hemodialysis filtration combined with blood perfusion in
the treatment of patients with uremic encephalopathy. Chin J
Primary Med Pharm. 23:457–459. 2016.
|
|
37
|
Wang LY, Yin DX, Zhang DL, Xu R, Cui WY
and Liu WH: Improvement and influencing factors of blood pressure
control by nephrologist referral in chronic kidney disease patients
in China: A cohort study. Int Urol Nephrol. 45:1345–1353.
2013.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Wang Y, Li J, Tong L, Zhang J, Zhai A, Xu
K, Wei L and Chu M: The prognostic value of miR-21 and miR-155 in
non-small-cell lung cancer: A meta-analysis. Jpn J Clin Oncol.
43:813–820. 2013.PubMed/NCBI View Article : Google Scholar
|