Introduction
The renin-angiotensin system (RAS) is a signaling
cascade that governs the balance of water and electrolytes and the
control of systemic arterial blood pressure (ABP), thus having a
central role in the renal and cardiovascular function (1). Beyond such classical knowledge,
regarding angiotensin II (Ang II), this peptide is nowa also known
for its inflammatory effects, with their impact upon the structure
and function of the kidneys and heart (2). Chronic RAS overactivation causes
cardiovascular and renal dysfunction, which also involve the
pro-inflammatory, pro-hypertrophic, and pro-fibrotic effects of Ang
II (3). It is now well known that
arterial hypertension affects target organs (eyes, brain, heart,
kidney) (4,5), also initiating a vicious circle that
promotes the sustained increase of ABP.
There has been a recent attempt to clarify the
pathophysiological mechanisms that can be found at the basis of the
inflammatory process associated with high ABP (6). The increasing levels of certain
inflammatory cytokines, such as tumor necrosis factor-α (TNF-α) and
interleukin-6 (IL-6) and IL-1β, represent independent factors that
predict mortality for patients with chronic kidney disease (CKD).
The renal changes and the increased ABP in CKD can be related to
effects of the inflammatory cytokines and chemokines (7). Inflammatory cells are present in the
renal tissue in most kidney diseases, both in the immune-mediated
ones and in those that occur as the effect of high ABP (8). One consequence of high ABP is heart
dysfunction (9). The B-type
natriuretic peptide (BNP) is released into the circulation from
‘the stressed out myocardium’, especially from the left ventricle.
High concentrations of BNP in blood plasma can be found in patients
with a heart condition, especially in those with heart failure and
kidney failure (10). An important
marker of the heart dysfunction is the N-terminal precursor of BNP
(NT-pro-BNP).
The molecular mechanisms underlying the relationship
between inflammation and hypertension are poorly understood. Within
this context, the present study aims to address the role of the
immune system in mediating the effects of Ang II excess upon the
kidney and upon the heart. In order to achieve this, we used an
appropriate experimental model and investigated the expression of
pro-inflammatory cytokines IL-1β, IL-6 and TNF-α, and also the
blood plasma level of NT-pro-BNP as marker of cardiac
dysfunction.
Materials and methods
Experimental model of hypertension
induced by Ang II
Wistar male rats were used as the experimental
animals. They were 12 weeks old and had an average weight of 250±50
g. The animals were kept in standard cages (2 rats in each cage),
in a room with controlled temperature of 21±2˚C and with a
light/dark cycle of 12/12 h. The rats had unrestricted access to
food and water. They were allowed to accommodate for at least 4
days before the implantation of mini-pumps. Subsequently, the rats
were divided into two groups: One group of 14 rats received Ang II
and the other group of 14 rats (control) received vehicle
(isoosmotic NaCl solution). Ang II acetate (Bachem Americas, Inc.)
was administered as follows: continuously for 14 days; at a rate of
300 ng/kg/min; subcutaneously, with osmotic minipumps (Alzet, model
2001) (1 µl/h), placed in the interscapular paravertebral region
(11).
The study protocol was approved by the Ethics
Committee of the ‘Grigore T. Popa’ University of Medicine and
Pharmacy (Iasi, Romania). Regarding the use of laboratory animals
and the biological preparations and samples for scientific
research, all the procedures applied in the present study comply
with the internationally accepted rules and guidelines from: i) the
Directive 2010/63/EU of the European Parliament and of the Council
of 22 September 2010 on the protection of animals used for
scientific purposes (12); ii) the
Universities Federation for Animal Welfare; iii) the International
Association for the Study of Pain (IASP).
Animal sacrifice and kidney
harvesting
Prior to their sacrifice, the rats were anesthetized
with ketamine, administered intraperitoneally at a dose of 12.5 mg
per 100 g body weight. The ketamine solution from 5 ml vials
(ketamine 50 mg/ml) was first diluted in physiological saline (NaCl
0.9 g/dl) in a 1:4 ratio, to the final ketamine concentration of
12.5 mg/ml, and this solution was given intraperitoneally in a dose
of 1 ml per 100 g body weight. After sacrifice, the kidneys were
removed and subjected to homogenization for their further use.
Systolic ABP measurement was performed
non-invasively by tail-cuff pletysmography (BIOPAC), in the
beginning of the study, and then on days 3, 6, 9, 12 and
14(13).
Assessment of IL-1β and NT-pro-BNP in
the blood plasma
The concentrations of IL-1β and NT-pro-BNP were
assessed by ELISA, in samples of blood plasma prepared as follows.
Blood was collected from the aorta on anticoagulant (heparin),
immediately before animal sacrifice. Within 30 min after blood
sampling, the samples were centrifuged at room temperature, for 20
min at 2,000 x g . The obtained plasma was immediately stored at
-80˚C until further processing. For ELISA Quantikine®
kits were used, rat IL-1β/IL-1F2 immunoassay (R&D Systems,
Inc.) and USCN Life Science, Inc. In each case, the detailed
instructions from the producer were followed.
IL-1β, IL-6 and TNF-α assessment in
kidney homogenate
The kidney homogenate was obtained by passing the
kidney through a fine sieve, using a syringe plunger. The sieve was
washed with 2 ml of Krebs serum. The operation was repeated 3
times. After manual processing, the samples were centrifuged at
room temperature, for 20 min at 2,000 x g and stored at -80˚C until
further use.
Evaluation of gene expression for IL-6
and TNF-α
For IL-6 and TNF-α qualitative evaluation was
performed, using RT-PCR, based on the reverse transcription kit
Enhanced Avian HS-100 RT-PCR (Sigma-Aldrich; Merck KGaA). For TNF-α
the primer sequence was AAGTTCCCAAATGGGCTC, while for IL-6 the
primer sequences were TTCCCTACTTCACAAGTC and CTAGGTTTGCCGAGTAGA
(14).
Statistical analysis
The statistical interpretation of data was performed
using GraphPad Prism 5.0. The data were analyzed with Student's
t-test or analysis of variance (ANOVA) for comparison between
groups with statistical significance defined. Significance of
differences between the studied groups was determined with least
significant difference (LSD) test. A P-value ≤0.05 was considered
statistically significant (15).
Results
Arterial hypertension induced by Ang
II
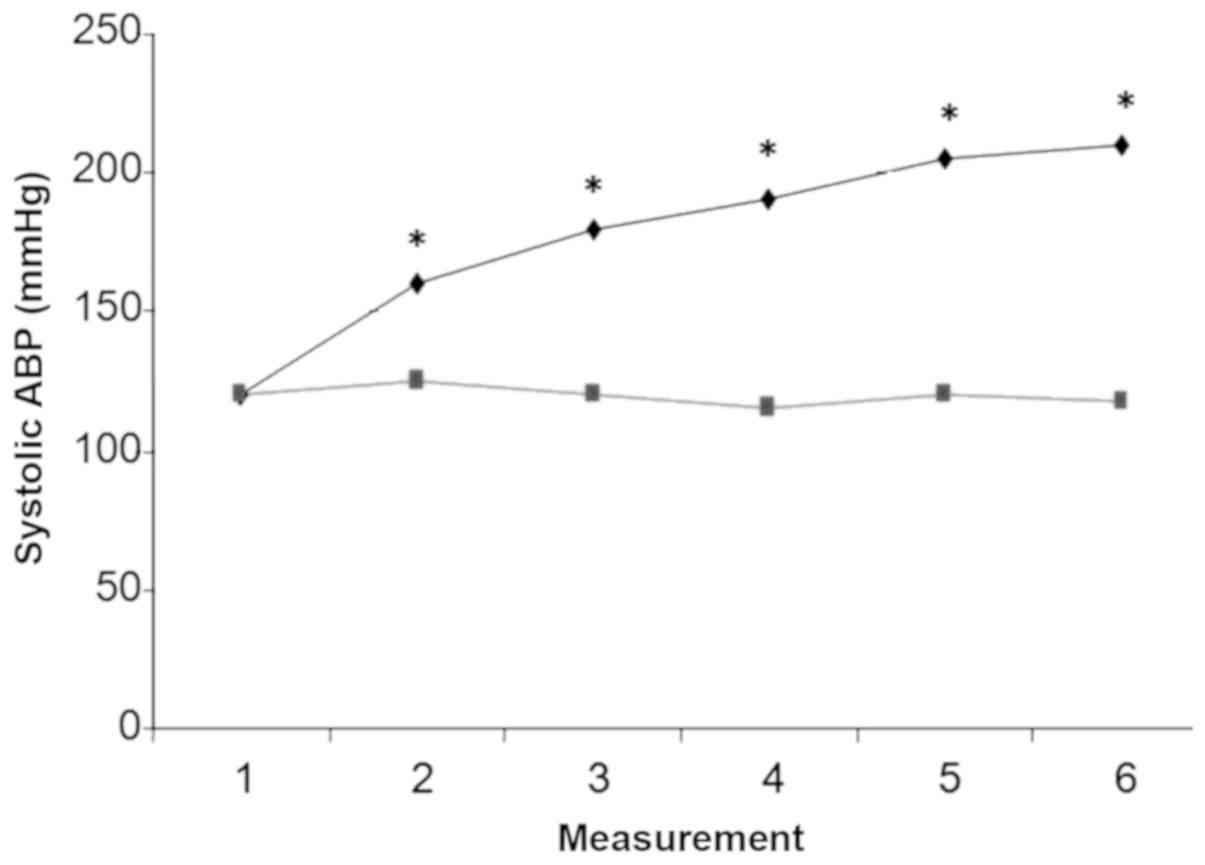
The systolic ABP was similar in the two groups of
rats before the treatment (~120 mmHg) and it increased gradually
and significantly in rats treated with Ang II, whereby on day 14 it
reached 208±2 vs. 120±5 mmHg the same day in the control group
(Fig. 1). Ang II treatment finally
raised systolic ABP above 206 mmHg in 4 rats (28.57%) and below 206
mmHg in the other 10 rats (71.43%).
Blood plasma concentration of
NT-pro-BNP
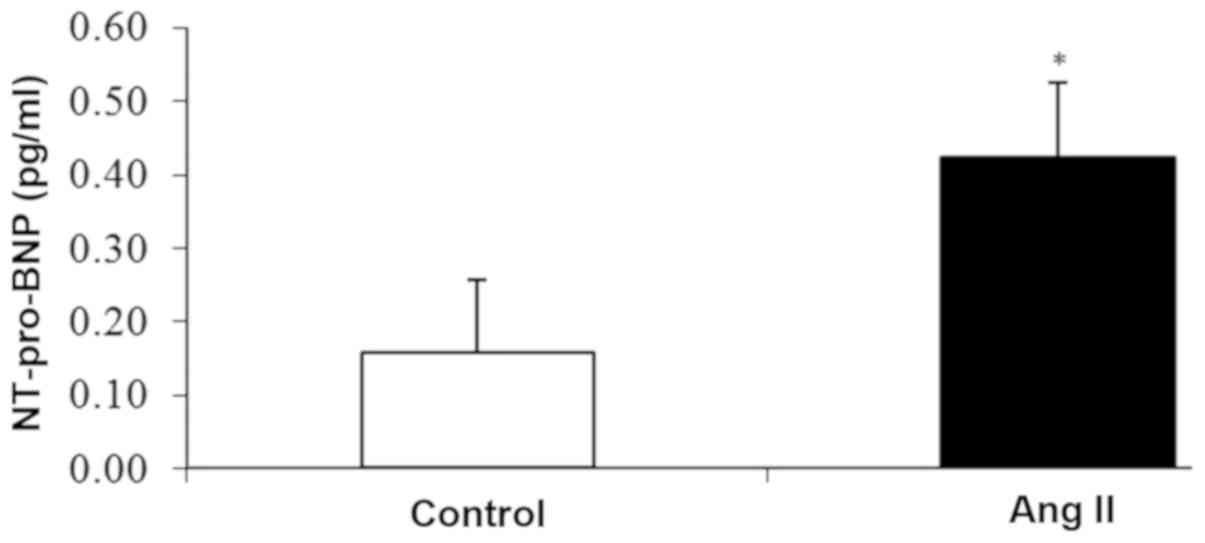
After 14 days of continuous administration of Ang
II, or of plain vehicle respectively, the blood plasma
concentration of NT-pro-BNP in rats who were given Ang II was
clearly higher (mean value 0.42 pg/ml) than in rats from the
control group (mean value 0.16 pg/ml) (Fig. 2), and the difference was
statistically significant (P=0.011).
Blood plasma concentration of
IL-1β
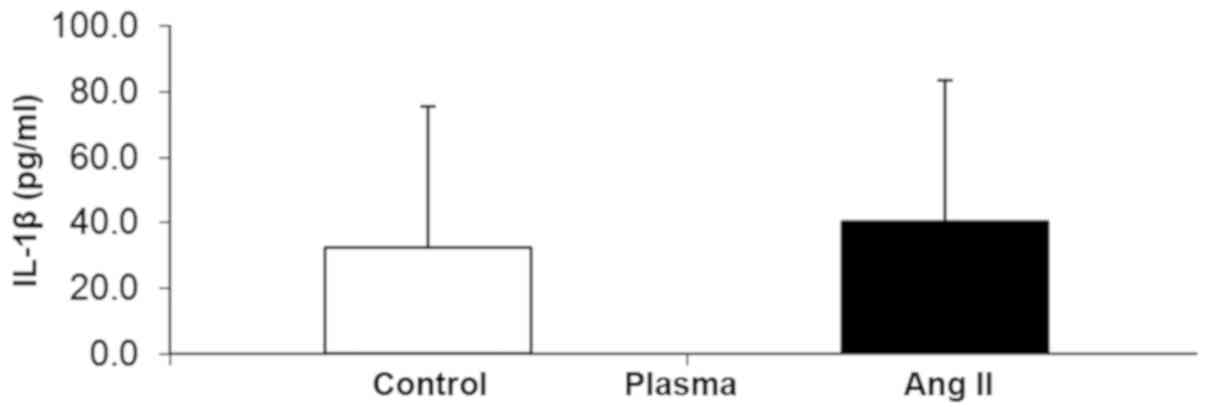
After 14 days of continuous administration of Ang
II, or of plain vehicle respectively, the blood plasma
concentration of IL-1β was somewhat higher in rats who were given
Ang II (mean value 40.4 pg/ml) than in rats from the control group
(mean value 32.43 pg/ml) (Fig. 3);
however, this difference was not statistically significant.
IL-1β concentration in the kidney
homogenate
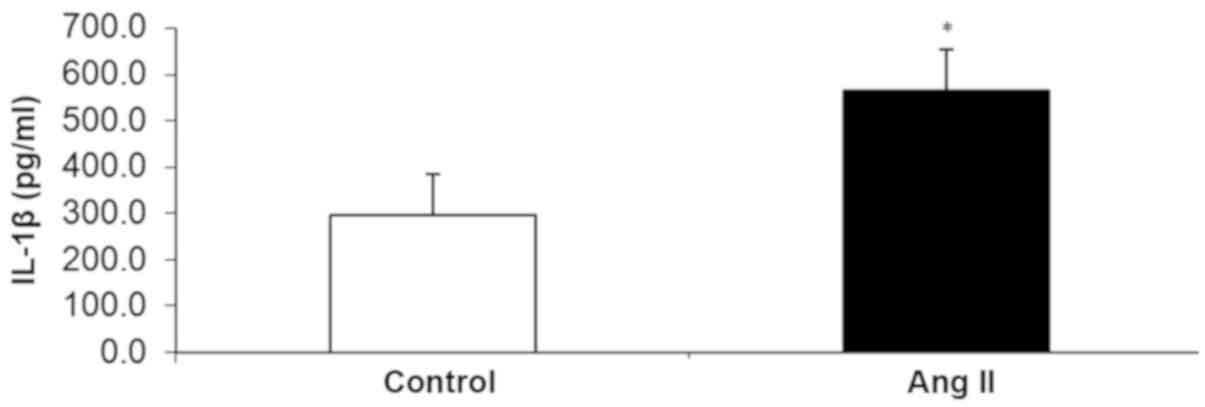
On the contrary, at the experiment end on day 14,
the IL-1β concentration in the kidney homogenate was significantly
higher (P=0.0000008) in rats treated with Ang II than in the
control group (mean values 564.3 vs. 297.49 pg/ml (Fig. 4).
Gene expression of the kidney
inflammatory markers IL-6 and TNF-α
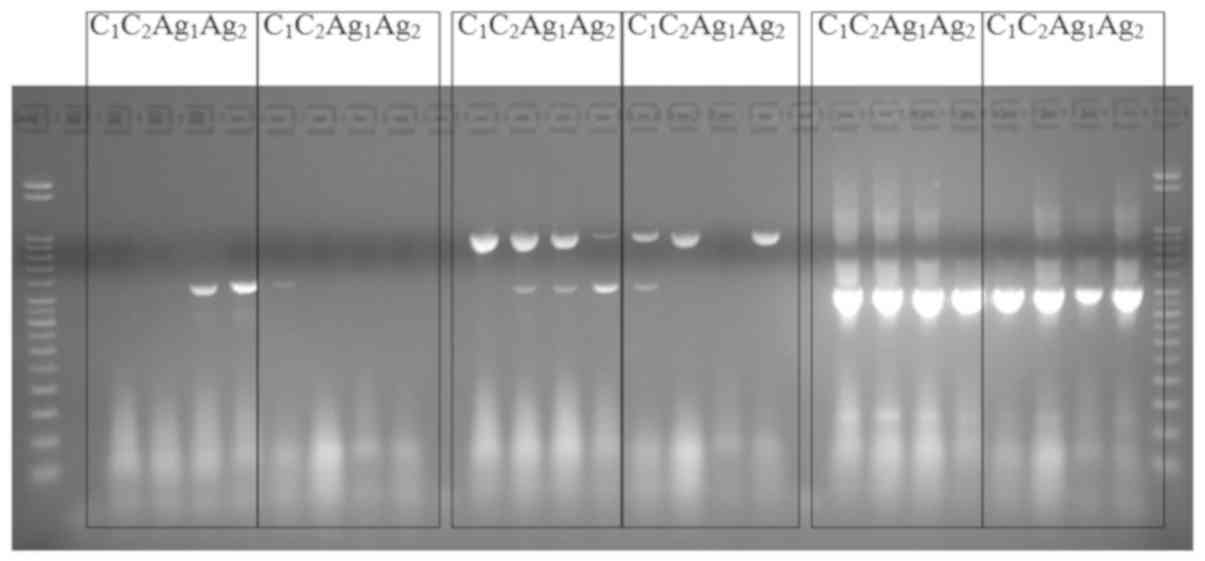
The expression of IL-6 and TNF-α was examined from a
qualitative point of view by RT-PCR, in order to evaluate the role
of Ang II as a proinflammatory molecule in kidney disease. The
expression of IL-6 and TNF-α in the kidney was increased in rats
subjected to chronic Ang II (14 days) in comparison to the control
group (Fig. 5). The bands from ~950
bp are due to genomic DNA contamination of the RNA samples. We note
that it is possible to obtain a diminution of the signal for DNA
only when the cDNA exists as a matrix.
Discussion
Cardiac muscle expansion, due to an increased
interior volume of the heart chambers and/or to an increased
myocardial transmural pressure (as occuring in heart failure,
myocardial infarction, or cardiomyopathy), causes the release of
the natriuretic peptides of cardiac origin: ANP (atrial natriuretic
peptide) and BNP (natriuretic peptide of the brain; a misnomer).
Mostly by promoting sodium and water excretion, ANP is permanently
involved in the homeostasy of the extracellular fluid volume (of
volemia actually) and its blood plasma concentration is closely
related to the left atrial pressure. BNP is released when
myocardial stress occurs and its concentration is directly related
to left ventricular pressure and volume (16).
A significant increase in systolic ABP was found in
rats treated with Ang II for 14 days (Fig. 1) and this high ABP was accompanied by
an increase in the blood plasma concentration of NT-pro-BNP
(Fig. 2). NT-pro-BNP, an established
biomarker of systolic and/or diastolic heart failure, is released
by the stressed myocardium. Such a myocardial stress, occuring in
the rats treated with Ang II, is due to the increased ABP, but is
also a direct consequence of the proinflammatory effect of Ang II
upon the ventricular myocardium.
High ABP may lead to left ventricular hypertrophy
and ultimately to heart failure. Hildebrandt et al (16) demonstrated in humans an association
between increased NT-pro-BNP in blood plasma and the high ABP
associated with left ventricular hypertrophy. On the other hand,
Jeppesen et al (17) found
that in humans an increase in blood plasma NT-pro-BNP is
accompanied by a decrease in the risk of developing hypertension,
because BNP determines the increased urinary sodium elimination,
vasodilatation, and decreased ABP (17,18).
Recent data show that BNP has an impact on the cardiac remodeling
process that occurs in hypertension, due to its anti-hypertrophic,
anti-proliferative and anti-inflammatory effects (19). In patients with CKD, left ventricular
hypertrophy occurs, with increased left ventricular volume and
pressure. Subsequent changes in myocardial structure,
calcification, fibrosis and collagen accumulation, all accompany
the ensuing systolic and diastolic cardiac dysfunction (20). Moreover, the concentration of
NT-pro-BNP in blood plasma increases in parallel with the decline
in renal function in patients subjected to dialysis (21). However, the cardiac dysfunction is
mild in rats treated with Ang II for 14 days.
IL-1β, is a well known pro-inflammatory cytokine,
released as a consequence of oxidative stress, and is involved in
the fight against infections in autoimmune and metabolic diseases.
There is an increased concentration of proinflammatory cytokines in
blood plasma of patients with cardiac dysfunction (22). IL-1β is involved in the
pathophysiology of heart failure by promoting the remodelling of
the left ventricle. Our study reveals an increase of IL-1β in Ang
II treated rats vs. control, in the kidney homogenate (Fig. 4), but not in blood plasma (Fig. 3).
In patients with CKD, left ventricular hypertrophy
and contractile myocardial dysfunction are independent predictive
factors of mortality. Blood plasma IL-1β is increased in CKD
patients (23), by a dual mechanism:
due to the increased uric acid concentration in blood serum, which
leads to increased oxidative stress, and also due to the release of
IL-1β from the myocardium in left ventricular dysfunction (24). Studies in rats with heart failure
have demonstrated an increase in proinflammatory cytokines (IL-1β,
IL-6 and TNF-α) not only in plasma but also in peripheral tissues,
associated with an increase in the concentration of all components
of RAS. In the experimental model of hypertension induced by
chronic Ang II administration, Navar et al (25) have identified new mechanisms,
involving a role for increased expression of intrarenal
angiotensinogen, which in turn is modulated by the increased
expression of TNF-α and IL-6 due to the chronic Ang II
treatment.
It is known that renal Ang II exerts proinflammatory
effects by stimulating renal infiltration with T lymphocytes and
macrophages (26). These cells,
which belong to the immune system, secrete inflammatory cytokines
such as IL-6 and TNF-α (27). We
observed increased gene expression for IL-6 and TNF-α in the kidney
homogenate from Ang II-treated rats vs. control (Fig. 5). In chronic Ang II treatment, the
elevation of intrarenal Ang II also involves IL-6, by its effect of
increasing the local gene expression for angiotensinogen; this
contributes to the increased ABP and to the renal impairment
(28).
The inflammatory effects observed in the present
study cannot be discussed in terms of their true cause, e.g. the
results themselves do not allow us to really discern whether
hypertension-related inflammation is due to hypertension itself, to
Ang II, or to both. However, we prefer the third explanation,
whereby the direct pro-inflammatory effects of Ang II are in fact
part of an aggravating positive feedback loop (6-8,11),
at least in this model of hypertension induced by Ang II. Moreover,
this should occur in any circumstance of chronic high ABP,
depending upon the degree of RAS involvement in each situation.
Obviously, the two causative and/or mediating mechanisms could be
decoupled in separate experimental models. For example in any
hypertension model where ABP still increases despite the treatment
with an antagonist of Ang II receptors. This would allow
examination of the components of the pro-inflammatory environment
which are induced by hypertension but are independent of Ang II.
Such studies are available in the wide field devoted to the use of
Ang II antagonists for the treatment of systemic arterial
hypertension.
In conclusion, chronic Ang II increases ABP and this
affects the target organs. Increased NT-pro-BNP in blood plasma
reveals dysfunction of the heart left ventricle. The mechanism of
renal impairment, in the hypertension induced by chronic Ang II,
includes immune cell infiltration of the kidney, with the secretion
of pro-inflammatory cytokines: IL-1β, IL-6 and TNF-α. Our findings
suggest that the anti-inflammatory medication, which inhibits the
immune system, might be useful to alleviate the kidney dysfunction
in hypertension.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
All authors have substantially contributed to each
of the following aspects of the article: Conception and design of
the study (mainly MAM, DMT, DEB, DNS and ILS); execution of the
experiment (mainly MAM and DMT); analysis and interpretation of the
data (mainly MAM, DMT, DNS and DCB); drafting the manuscript
(mainly MAM, DMT, ILS and DEB); revising the manuscript critically
for important intellectual content (mainly DNS, ILS, DCB and DEB).
All authors have read and approved the final version of the
manuscript. Thus, each author has participated sufficiently in the
study and takes public responsibility for appropriate portions of
the content. The authors agree to be accountable for all aspects of
the study in ensuring that questions related to the accuracy or
integrity of any part of the study are appropriately investigated
and resolved.
Ethics approval and consent to
participate
The study protocol was approved by the Ethics
Committee of the ‘Grigore T. Popa’ University of Medicine and
Pharmacy (Iasi, Romania) and fulfils all the requirements of the
guide issued by the International Society of Pain Study (IASP) and
the European Council Committee (86/609/EEC) regarding the use of
laboratory animals and biological preparations. The internationally
accepted rules on animal studies were respected.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Haulica I, Bild W and Serban DN:
Angiotensin peptides and their pleiotropic actions. J Renin
Angiotensin Aldosterone Syst. 6:121–131. 2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Benigni A, Cassis P and Remuzzi G:
Angiotensin II revisited: New roles in inflammation, immunology and
aging. EMBO Mol Med. 2:247–257. 2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ames MK, Atkins CE and Pitt B: The
renin-angiotensin-aldosterone system and its suppression. J Vet
Intern Med. 33:363–382. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Stanca HT, Suvac E, Munteanu M, Jianu DC,
Motoc AG, Roşca GC and Boruga O: Giant cell arteritis with
arteritic anterior ischemic optic neuropathy. Rom J Morphol
Embryol. 58:281–285. 2017.PubMed/NCBI
|
|
5
|
Stanca HT, Petrović Z and Munteanu M:
Transluminal Nd: YAG laser embolysis - A reasonable method to
reperfuse occluded branch retinal arteries. Vojnosanit Pregl.
71:1072–1077. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
McMaster WG, Kirabo A, Madhur MS and
Harrison DG: Inflammation, immunity, and hypertensive end-organ
damage. Circ Res. 116:1022–1033. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ruiz-Ortega M, Esteban V, Rupérez M,
Sánchez-López E, Rodríguez-Vita J, Carvajal G and Egido J: Renal
and vascular hypertension-induced inflammation: Role of angiotensin
II. Curr Opin Nephrol Hypertens. 15:159–166. 2006.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Pauletto P and Rattazzi M: Inflammation
and hypertension: The search for a link. Nephrol Dial Transplant.
21:850–853. 2006.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Savoiu Balint G, Iovanescu G, Stanca HT,
Popoiu CM, Boia E, Popovici RA and Bolintineanu SL: The protective
effect of HDL-cholesterol in patients with essential hypertension.
Rev Chim Buchar. 68:949–952. 2017.
|
|
10
|
Paget V, Legedz L, Gaudebout N, Girerd N,
Bricca G, Milon H, Vincent M and Lantelme P: N-terminal pro-brain
natriuretic peptide: A powerful predictor of mortality in
hypertension. Hypertension. 57:702–709. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Dornas WC and Silva ME: Animal models for
the study of arterial hypertension. J Biosci. 36:731–737.
2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Directive. 2010/63/eu of the European
Parliament and of the Council of 22 September 2010 on the
protection of animals used for scientific purposes. OJEU.
L276:33–79. 2010.
|
|
13
|
Buñag RD: Validation in awake rats of a
tail-cuff method for measuring systolic pressure. J Appl Physiol.
34:279–282. 1973.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Murphy PG, Grondin J, Altares M and
Richardson PM: Induction of interleukin-6 in axotomized sensory
neurons. J Neurosci. 15:5130–5138. 1995.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Winer BJ: Statistical principles in
experimental design. 2nd edition. McGraw-Hill, New York, NY,
1971.
|
|
16
|
Hildebrandt P, Boesen M, Olsen M, Wachtell
K and Groenning B: N-terminal pro brain natriuretic peptide in
arterial hypertension - a marker for left ventricular dimensions
and prognosis. Eur J Heart Fail. 6:313–317. 2004.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Jeppesen JL, Nielsen SJ, Torp-Pedersen C,
Hansen TW, Olsen MH, Berg ND, Linneberg A, Madsbad S and Fenger M:
Genetic variation in the natriuretic peptide system, circulating
natriuretic peptide levels, and blood pressure: An ambulatory blood
pressure study. Am J Hypertens. 25:1095–1100. 2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sarzani R, Spannella F, Giulietti F,
Balietti P, Cocci G and Bordicchia M: Cardiac natriuretic peptides,
hypertension and cardiovascular risk. High Blood Press Cardiovasc
Prev. 24:115–126. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Rubattu S, Forte M, Marchitti S and Volpe
M: Molecular implications of natriuretic peptides in the protection
from hypertension and target organ damage development. Int J Mol
Sci. 20:1–12. 2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Mostafa F, Sad I, Elshamaa M, Badr A,
Eldayem S, Ashmawy I and Abd Elrahim YA: Left ventricular
dysfunction by conventional and tissue Doppler echocardiography in
pediatric hemodialysis patients: Relation with plasma brain
natriuretic peptide levels. Med Sci Atheroscler Dis. 3:e18–e28.
2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Cui H, Huo G, Liu L, Fan L, Ye P, Cao J,
Bai Y, Wang F and Hu Y: Association of cardiac and renal function
with extreme N-terminal fragment pro-B-type natriuretic peptide
levels in elderly patients. BMC Cardiovasc Disord.
12(57)2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Dávila DF, Donis JH, Odreman R, Gonzalez M
and Landaeta A: Patterns of left ventricular hypertrophy in
essential hypertension: Should echocardiography guide the
pharmacological treatment? Int J Cardiol. 124:134–138.
2008.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Devereux RB, Roman MJ, Ganau A, de Simone
G, Okin PM and Kligfield P: Cardiac and arterial hypertrophy and
atherosclerosis in hypertension. Hypertension. 23:802–809.
1994.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Alberts BM, Bruce C, Basnayake K, Ghezzi
P, Davies KA and Mullen LM: Secretion of IL-1β from monocytes in
gout is redox independent. Front Immunol. 10(70)2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Navar LG, Prieto MC, Satou R and Kobori H:
Intrarenal angiotensin II and its contribution to the genesis of
chronic hypertension. Curr Opin Pharmacol. 11:180–186.
2011.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Bujak M and Frangogiannis NG: The role of
IL-1 in the pathogenesis of heart disease. Arch Immunol Ther Exp
(Warsz). 57:165–176. 2009.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Gupta J, Dominic EA, Fink JC, Ojo AO,
Barrows IR, Reilly MP, Townsend RR, Joffe MM, Rosas SE, Wolman M,
et al: CRIC Study Investigators: Association between inflammation
and cardiac geometry in chronic kidney disease: Findings from the
CRIC study. PLoS One. 10(e0124772)2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Granger JP: An emerging role for
inflammatory cytokines in hypertension. Am J Physiol Heart Circ
Physiol. 290:H923–H924. 2006.PubMed/NCBI View Article : Google Scholar
|