Introduction
Benign prostatic hyperplasia (BPH) is a common and
frequently encountered disease in middle-aged and old males
(1). The incidence of BPH in males
is ~40% at the age of 50 and ~90% after the age of 80 years
(2,3).
The transurethral resection of the prostate (TURP)
is the gold standard of BPH surgical treatment in men with prostate
size of 30-80 ml (4). In recent
years, holmium laser, 2 µm laser and green laser have been widely
used among clinicians for their excellent coagulation hemostasis
and non-conductive properties. Two-micrometer laser is a
high-energy laser with a wavelength of 2 µm, which is close to the
maximum absorption peak of 1.94 µm of water. It can be absorbed by
the water in the tissue and produce a thermal effect, effectively
achieving the purpose of cutting and vaporizing the tissue, with
little heat loss to the surgical area (5). However, intraoperative and
postoperative bleeding is still the main complication of surgical
treatment (6). With the aging of the
population and the increase of the incidence of cardiovascular and
cerebrovascular diseases, the number of BPH patients requiring
surgical treatment while taking oral antithrombotic drugs is also
increasing year by year, further increasing the risk of
perioperative bleeding (7). However,
recent studies have found that the type of antithrombotic agents is
not a major factor in the risk of perioperative bleeding in
patients with BPH (8,9). Meskawi et al (9) treated BPH patients undergoing laser
surgery with antiplatelet agents such as clopidogrel
acetylsalicylate and anticoagulants such as warfarin, thrombin
inhibitors and rivaroxaban. However, they found no significant
difference in the effect of different antithrombotic drugs on the
risk of bleeding. So the effect of antithrombotic drugs on bleeding
risk may be related to other factors. A large number of studies
considered that antithrombotic drugs will increase the risk of
perioperative bleeding, and it is recommended to interrupt
anticoagulation preoperatively (10). However, some studies have pointed out
that the risk of cardiovascular and cerebrovascular events after
stopping antithrombotic drugs is three times higher than that of
the group that did not stop using antithrombotic drugs (11). Therefore, this study adopted the
method of systematic review to evaluate the impact of continuous
use of antithrombotic drugs on intraoperative and postoperative
bleeding risk of BPH patients, aiming to provide theoretical basis
for clinical treatment decisions.
Materials and methods
Search strategy
We searched Pubmed, Embase and Cochrane library
databases. The search terms were ‘antithrombotic or aspirin or
antiplatelet or heparin’ and ‘prostatic hyperplasia’, and limited
fields in the title and abstract. In order to increase the search
efficiency, we also excluded the studies with keywords
‘meta-analysis’, ‘review’ and ‘case report’. The time of
publication was from inception to February 28, 2019. In addition,
we searched the reference list of acquired articles manually.
Inclusion and exclusion criteria
Inclusion criteria: i) Type of study: Clinical
controlled trial. ii) Study subjects: prostate surgery patients
(including electric resection and laser surgery). iii) Intervention
measures: experimental group, perioperative continuous application
of antithrombotic drugs (including antiplatelet drugs and
anticoagulant drugs), continuous use of antithrombotic drugs was
defined as the patients did not stop using antithrombotic drugs
during the surgery. Control group, antithrombotic drugs were
discontinued preoperatively or not. The discontinued antithrombotic
drugs were defined as drugs were discontinued preoperatively for
5-10 days, and anticoagulants, including novel oral
anticoagulants-NOACs, were not used in discontinued patients during
discontinuation. The unused antithrombotic drugs were defined as
drugs were never taken or discontinued preoperatively for more than
30 days. iv) At least one outcome index was reported: incidence of
postoperative bleeding, blood transfusion rate, decreased
intraoperative hemoglobin, catheterization duration and incidence
of cardiovascular and cerebrovascular events.
Exclusion criteria: i) The studies were repeatedly
published; ii) No control group was set up in the study; iii)
Incomplete information or unable to obtain complete information of
the study.
Data extraction and quality
assessment
Study screening and data extraction were performed
independently by two reviewers. Firstly, the related studies were
selected by browsing the title and abstract of the article. After
excluding the studies that did not meet the inclusion criteria, the
full text of the studies that might meet the inclusion criteria was
searched and read, and then screened again. Two researchers
cross-checked the included studies. For the studies with
differences and difficult to reach consensus, the third researcher
was asked to decide.
The extracted data included: i) basic information of
the included studies, including author, publication time, country
or region where the study was carried out, and sample size; ii)
drugs and surgical methods; iii) anticoagulation mode and outcome
indicators; iv) study quality evaluation of the relevant
information.
Two researchers evaluated the quality of the
included studies according to the Newcastle Ottawa scale (NOS)
(12), and the third reviewer
evaluated the studies when the scores were inconsistent. The full
score of NOS score is 9, and the evaluation content includes the
selection and exposure factors of the case control study, the
comparability between groups, etc. The score of more than 6 is
divided into high-quality study.
Observed indicator
Antithrombotic agents and bleeding risk after
transurethral therapy of benign prostatic hyperplasia were
evaluated by the following observed indicator: Incidence of
postoperative bleeding, blood transfusion rate, decreased
intraoperative hemoglobin, catheterization duration and incidence
of cardiovascular and cerebrovascular events.
Statistical analysis
RevMan5.3 software was used to complete the
meta-analysis process. Mean difference (MD) and 95% confidence
interval (95% CI) was used for measurement data, odds ratio (OR)
and 95% CI was used for categorical data, and P<0.05 was
considered statistically significant. The statistical heterogeneity
among the studies was analyzed by Chi-square test, and the studies
with good homogeneity (P>0.05 and I2 <50%) were
analyzed with the fixed-effect model. If there is heterogeneity
(P<0.05 or I2 >50%), the source of heterogeneity
will be analyzed. If there is no obvious heterogeneity, the random
effect model will be used for analysis. If there is heterogeneity,
the stability and reliability of the results can be verified by
subgroup analysis or sensitivity analysis.
Results
Study selection and study
characteristics
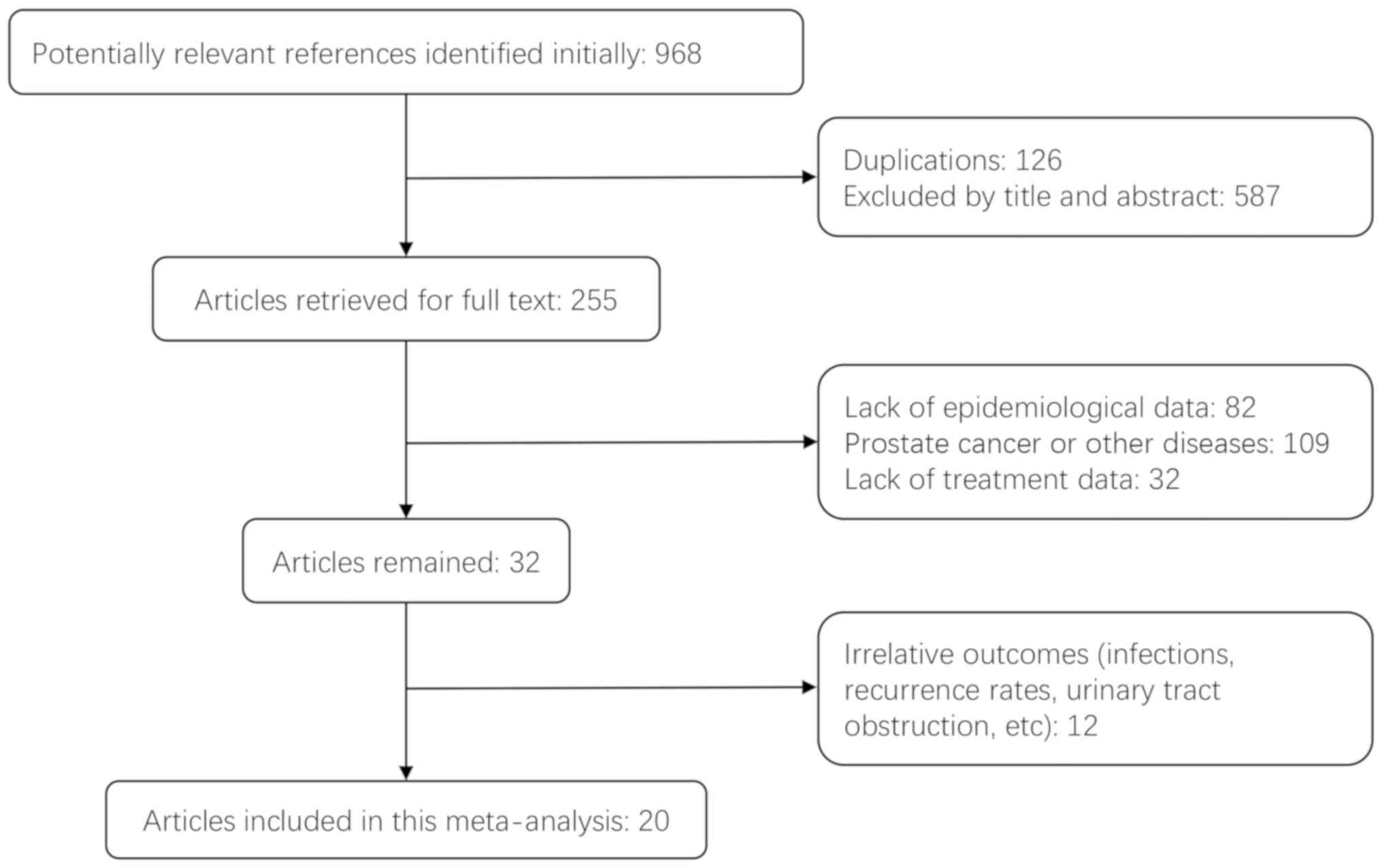
A total of 20 studies (13-32)
were included in this analysis and the study screening process is
shown in Fig. 1. Baseline data of
included studies are shown in Table
I. Among them, 8 studies (13-20)
reported TURP and 5 studies (22-30)
reported holmium laser enucleation of the prostate (HoLEP). Four
studies (27-30)
reported photoselective vaporization of the prostate (PVP). Thulium
laser vaporesection of the prostate (ThuVARP) was used as surgical
methods in 2 studies (31,32) and 1 study (21) reported thulium laser enucleation of
the prostate (ThuLEP). The quality assessment of the included
studies is shown in Table II.
 | Table IBasic characteristics of the included
studies. |
Table I
Basic characteristics of the included
studies.
| | Perioperative
anticoagulation | |
|---|
| Authors, year
(ref.) | Antithrombotic
therapy | Surgical
procedures | Persistent-usage | Heparin | Discontinued | Not taking | Outcome |
|---|
| Watson et al,
1990(13) | Aspirin | TURP | 5 | - | - | 34 | a |
| Thurston and Briant,
1993(14) | Aspirin | TURP | 14 | - | - | 111 | a |
| Ala-Opas and
Grönlund, 1996(15) | Aspirin | TURP | 40 | - | - | 42 | a |
| Nielsen et al,
2000(16) | Aspirin | TURP | 26 | - | 27 | - | b,e |
| Wenders et
al, 2012(17) | Aspirin | TURP | 42 | - | 156 | - | a,b |
| Dotan et al,
2002(18) | Anticoagulant
drugs | TURP | 20 | - | - | 20 | b |
| Taylor et
al, 2011(19) | Anticoagulant
drugs | TURP | 7 | - | 65 | 91 | a,b,e |
| Ong et al,
2015(20) | Antiplatelet
drugs | TURP | 32 | - | 69 | 166 | a,b,e |
| Carmignani et
al, 2014(21) | Antiplatelet
drugs | ThuLEP | 42 | - | - | 50 | b |
| Elzayat et
al, 2006(22) | Anticoagulant
drugs | HoLEP | 14 | 34 | 33 | - | b |
| Tyson and Lerner,
2009(23) | Anticoagulant
drugs | HoLEP | 38 | - | - | 37 | d |
| Bishop et
al, 2013(24) | Anticoagulant
drugs | HoLEP | 52 | - | 73 | - | b |
| El Tayeb et
al, 2016(25) | Anticoagulant
drugs | HoLEP | 30 | - | 86 | - | b |
| Sun et al,
2018(26) | Antiplatelet
drugs | HoLEP | 128 | - | 41 | 955 | b,c |
| Ruszat et
al, 2007(27) | Anticoagulant
drugs | PVP | 116 | - | - | 92 | d |
| Karatas et
al, 2010(28) | Anticoagulant
drugs | PVP | 9 | - | 58 | - | c,d |
| Sohn et al,
2011(29) | Anticoagulant
drugs | PVP | 30 | - | 30 | - | c |
| Knapp et al,
2017(30) | Anticoagulant
drugs | PVP | 101 | - | - | 272 | d |
| Macchione et
al, 2013(31) | Anticoagulant
drugs | ThuVARP | 41 | 35 | - | - | b,c,d |
| Sener et al,
2017(32) | Anticoagulant
drugs | ThuVARP | 56 | 47 | - | - | b,c,d |
 | Table IINOS scores of the included
studies. |
Table II
NOS scores of the included
studies.
| Authors year
(ref.) | Selection | Comparability | Exposure | Total |
|---|
| Watson et
al, 1990(13) | 3 | 1 | 2 | 6 |
| Thurston and
Briant, 1993(14) | 3 | 2 | 2 | 7 |
| Ala-Opas and
Grönlund 1996(15) | 3 | 2 | 2 | 7 |
| Nielsen et
al, 2000(16) | 2 | 1 | 1 | 4 |
| Wenders et
al, 2012(17) | 4 | 2 | 2 | 8 |
| Dotan et al,
2002(18) | 4 | 2 | 2 | 8 |
| Taylor et
al, 2011(19) | 3 | 1 | 2 | 6 |
| Ong et al,
2015(20) | 4 | 1 | 3 | 8 |
| Carmignani et
al, 2014(21) | 4 | 1 | 2 | 7 |
| Elzayat et
al, 2006(22) | 3 | 2 | 2 | 7 |
| Tyson and Lerner,
2009(23) | 4 | 2 | 2 | 8 |
| Bishop et
al, 2013(24) | 3 | 2 | 2 | 7 |
| El Tayeb et
al, 2016(25) | 4 | 1 | 2 | 7 |
| Sun et al,
2018(26) | 4 | 2 | 2 | 8 |
| Ruszat et
al, 2007(27) | 4 | 2 | 2 | 8 |
| Karatas et
al, 2010(28) | 3 | 1 | 2 | 6 |
| Sohn et al,
2011(29) | 4 | 1 | 2 | 7 |
| Knapp et al,
2017(30) | 4 | 2 | 3 | 9 |
| Macchione et
al, 2013(31) Sener et
al, | 3 | 1 | 2 | 6 |
| 2017(32) NOS, Newcastle Ottawa Scale. | 4 | 2 | 3 | 9 |
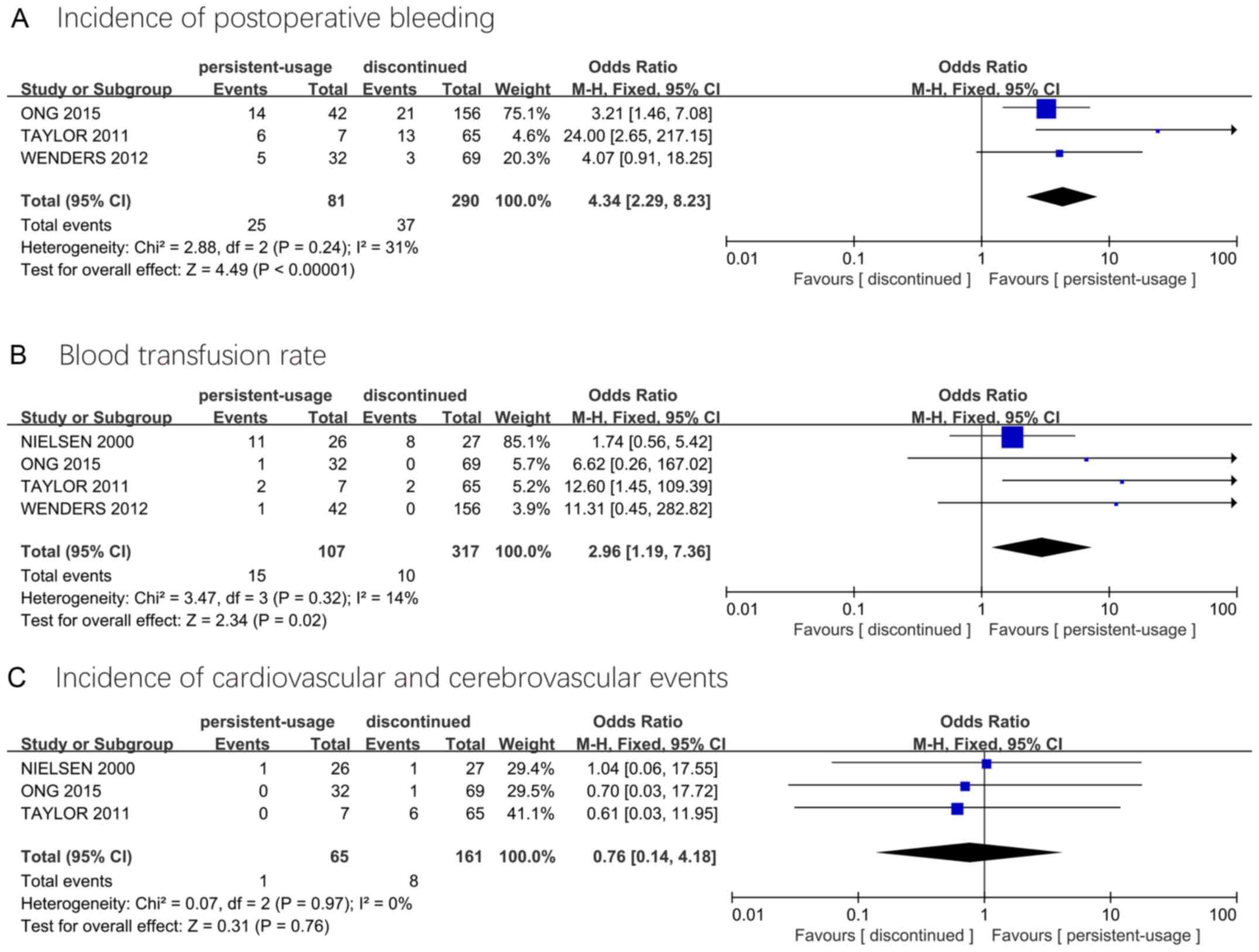
TURP: Persistent-usage group vs.
discontinued group
Three studies reported incidence of postoperative
bleeding and incidence of cardiovascular and cerebrovascular
events, and four studies reported blood transfusion rates. Compared
with the discontinued group, the persistent-usage group has a high
incidence of postoperative bleeding (OR=4.34, 95% CI=2.29-8.23) and
blood transfusion rate (2.96, 1.19-7.36), while the difference in
the incidence of cardiovascular and cerebrovascular events is not
statistically significant (0.76, 0.14-4.18) (Fig. 2).
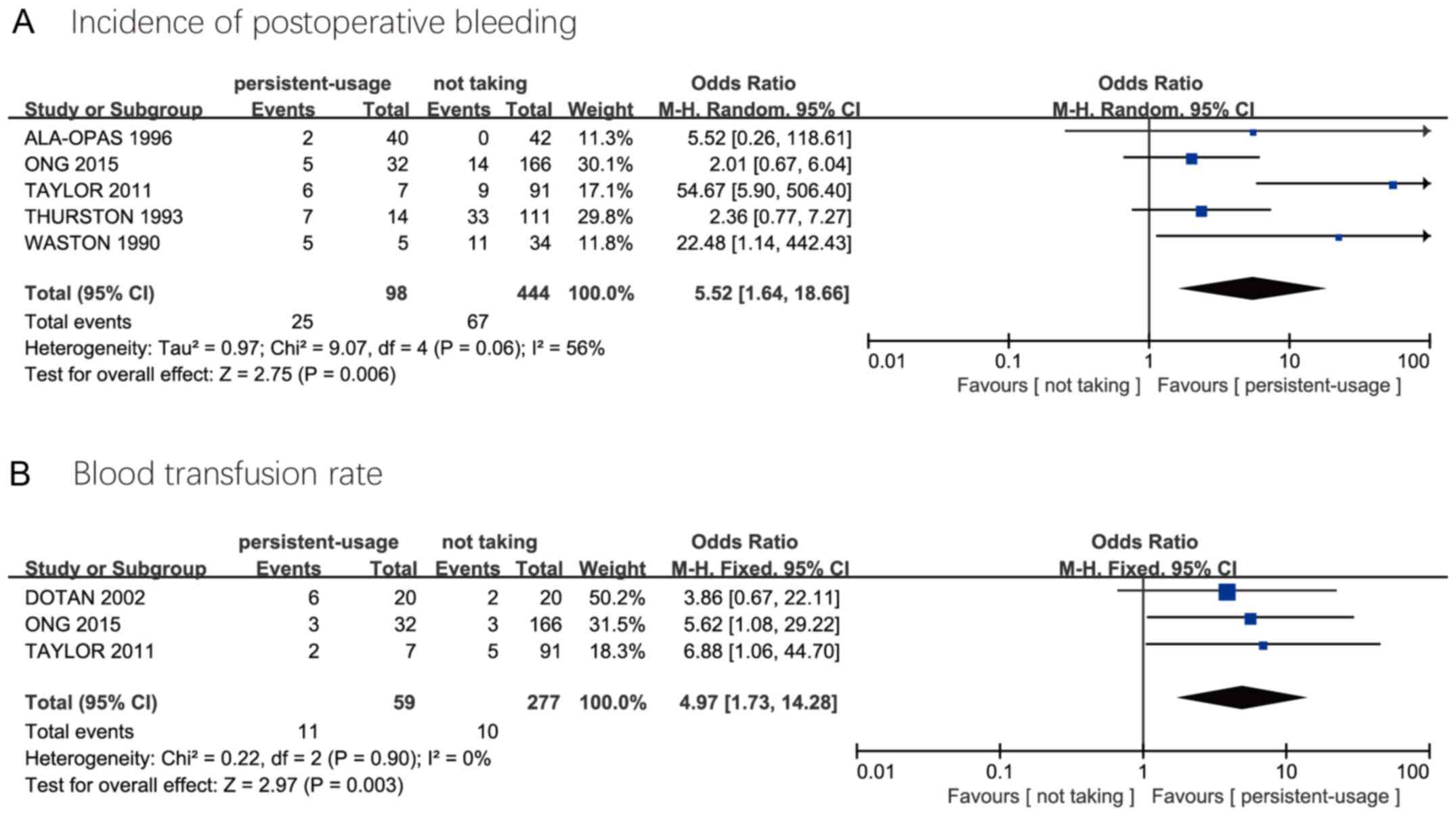
TURP: Persistent-usage group vs. not
taking group
The incidence of postoperative bleeding was reported
in four studies, with obvious heterogeneity among studies. The
random effect model was performed, and the results showed that the
incidence of postoperative bleeding was high in the
persistent-usage group (5.52, 1.64-18.66). Three studies reported
that transfusion rates were higher in the persistent-usage group
than that in not taking group (4.97, 1.73-14.28) (Fig. 3).
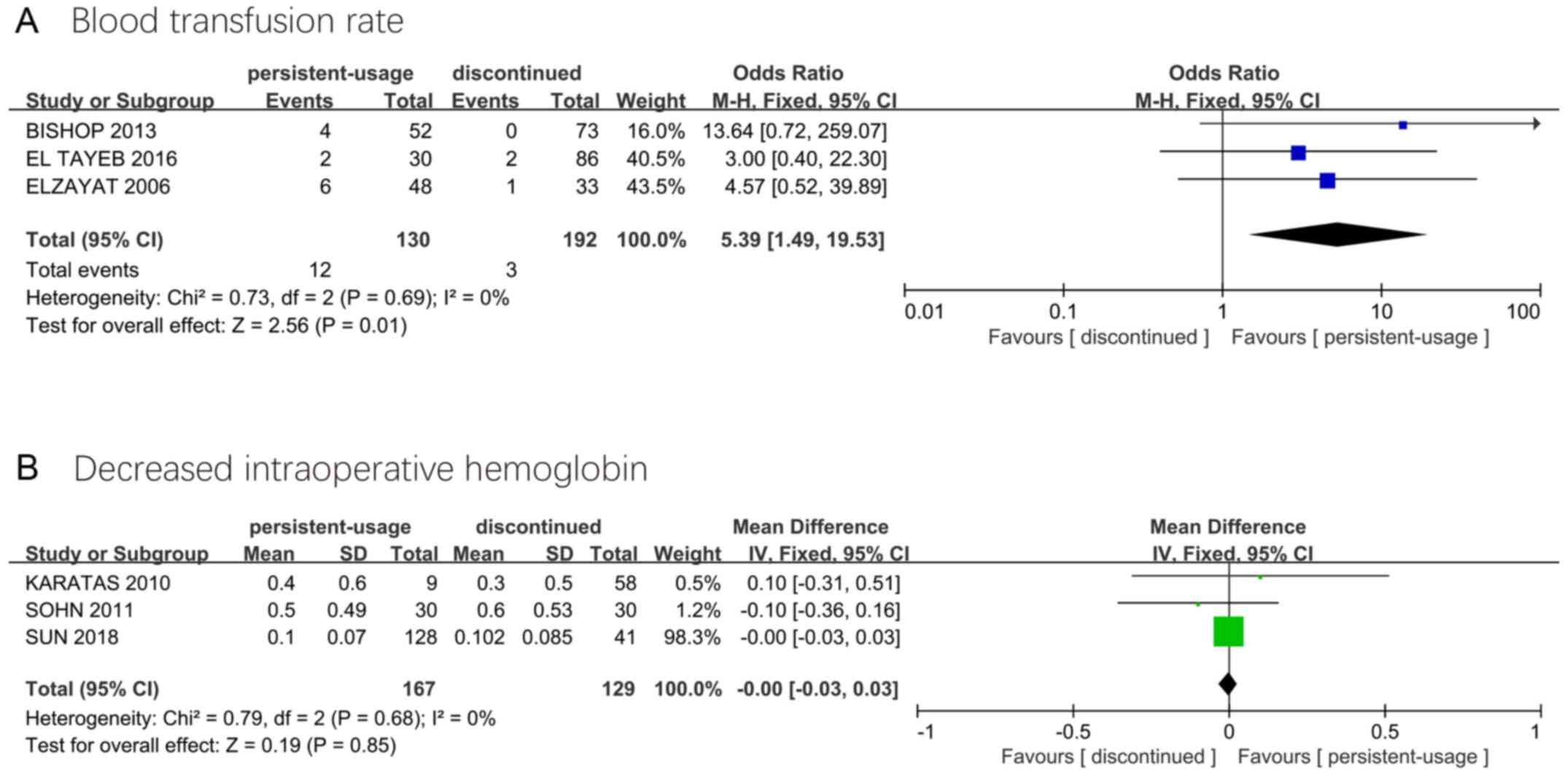
Laser surgery: Persistent-usage group
vs. discontinued group
Blood transfusion rates were reported in three
studies, and were higher in the persistent-usage group than that in
the discontinued group (5.39, 1.49-19.53). Three different studies
reported decreased intraoperative hemoglobin, with no statistically
significant difference between the groups (0.00, -0.03-0.03)
(Fig. 4).
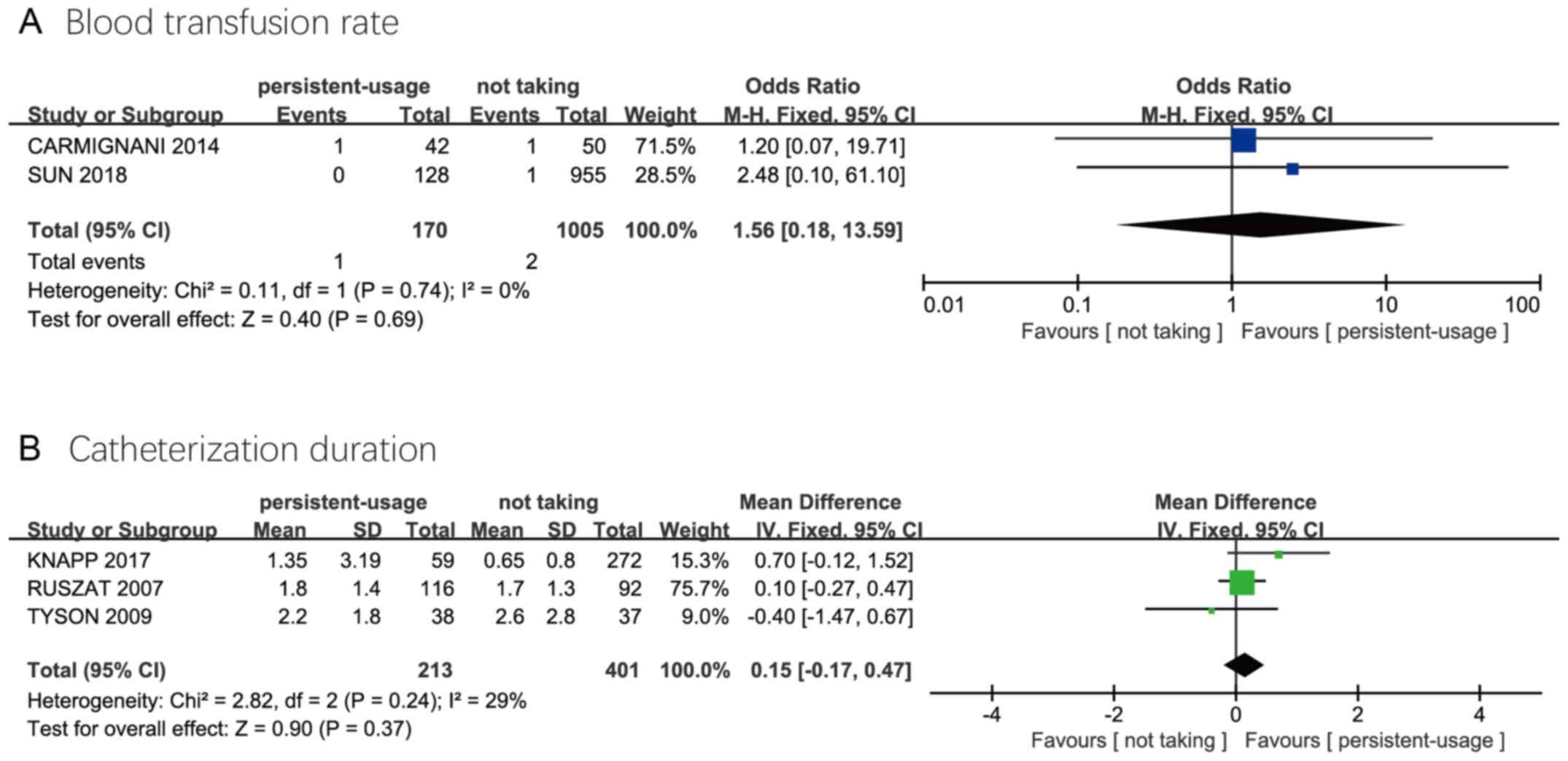
Laser surgery: Persistent-usage group
vs. not taking group
Two studies reported blood transfusion rates and
three reported catheterization duration. The results showed that
there was no significant difference in blood transfusion rate
(1.56, 0.18-13.59) and catheterization duration (0.15, -0.17-0.47)
between the two groups (Fig. 5).
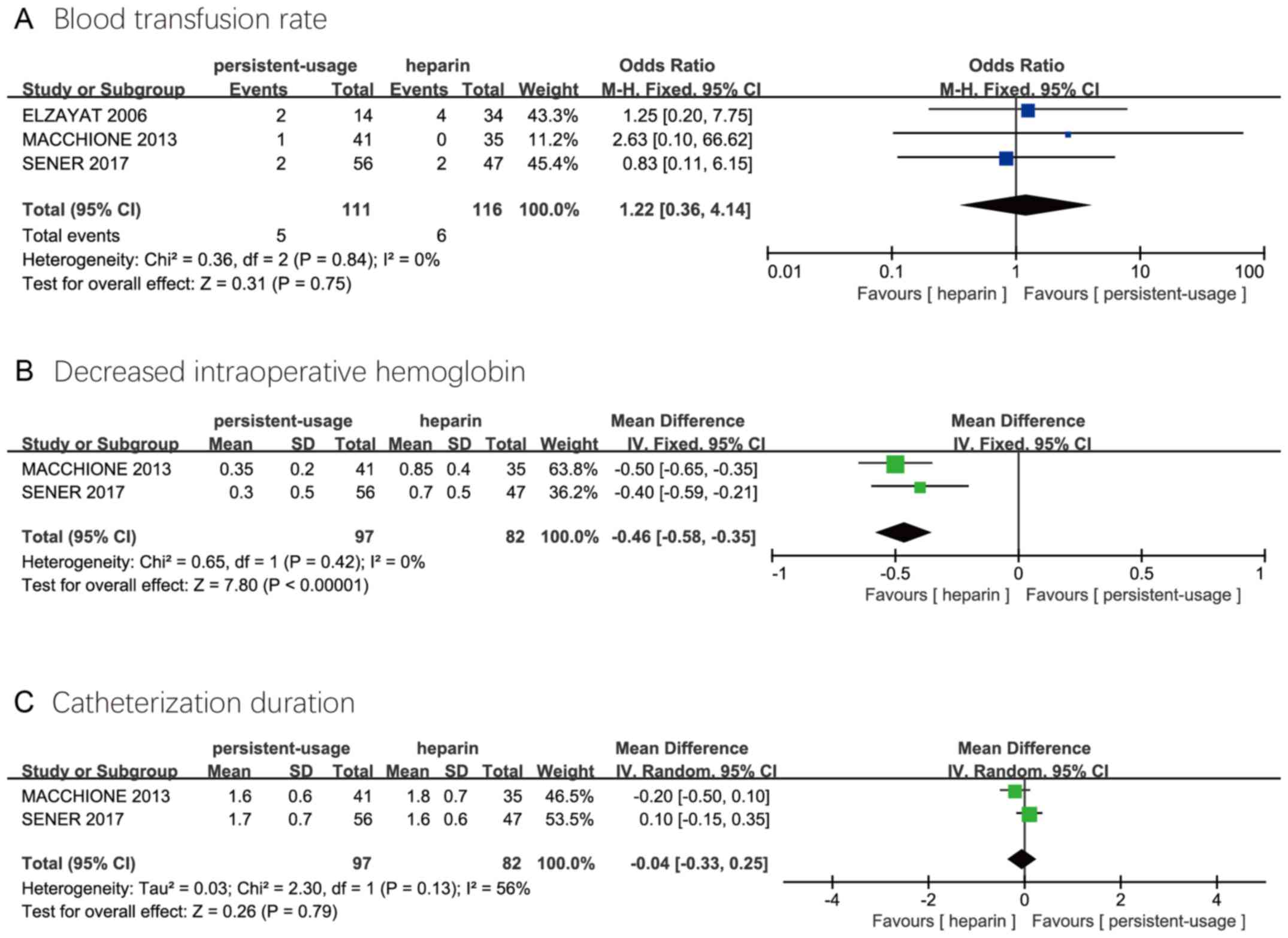
Laser surgery: Persistent-usage group
vs. heparin group
Three studies reported blood transfusion rates, and
two reported decreased intraoperative hemoglobin and
catheterization duration. Compared with the heparin group, the
persistent-usage group had a lower intraoperative decreased
intraoperative hemoglobin (-0.46, -0.58--0.35). There was no
significant difference in blood transfusion rate (1.22, 0.36-4.14)
and catheterization duration (-0.04, -0.33-0.25) (Fig. 6).
Discussion
In recent years, the number of patients requiring
oral antithrombotic drugs due to cardiovascular and cerebrovascular
diseases increased rapidly, and there was great controversy over
the perioperative anticoagulation management of these patients,
especially the intraoperative and postoperative bleeding (33). Due to the lack of high-quality RCT
studies, urologists currently have no unified consensus on the
management of antithrombotic drugs, relying only on long-term
clinical experience or existing observational studies. Although
American Urological Association and International Consultation on
Urological diseases has submitted a proposal on urology common
surgical perioperative management of antithrombotic drugs, the
number of articles in view of the prostate surgery was too small,
therefore, it is necessary to perform a meta-analysis of the
existing studies.
The meta-analysis results of TURP with or without
continuous use of antithrombotic drugs during the perioperative
period showed that continuous use of antithrombotic drugs would
increase the incidence of postoperative bleeding and increase the
possibility of blood transfusion, and the discontinuation of
antithrombotic drugs 5-10 days before surgery could reduce
postoperative bleeding complications. However, there was no
significant difference in the incidence of perioperative
cardiovascular and cerebrovascular events between the
persistent-usage group and discontinued group. Whether the
application of perioperative drugs was continuous was not random
except for the study by Nielsen et al (16), and it was determined according to the
risk of patients' cardiovascular and cerebrovascular events, which
may reduce the incidence of perioperative cardiovascular and
cerebrovascular events after drug withdrawal. In general,
continuous use of antithrombotic drugs during the perioperative
period of TURP will lead to more bleeding complications. For
patients with low risk of thrombosis who take antithrombotic drugs
for the prevention of cardiovascular and cerebrovascular diseases,
it is recommended to stop using antithrombotic drugs
preoperatively. In addition, some studies have found that the risk
of thromboembolism is related to the operative time. The risk of
thromboembolism increases with the length of surgery (34,35).
However, the included studies lacked relevant data, so large sample
studies were expected to analyze the relationship between the risk
of thromboembolism and the operative time.
In the meta-analysis of laser BPH surgery
perioperative continuous and disable or unused antithrombotic
drugs, there are three results showing the blood transfusion rate
of the persistent-usage group was higher than that of the
discontinued group. After analysis, the international normalized
ratio (INR) of the prothrombin time of patients in the study of
Bishop et al (24) is 2.61,
while the average INR of the remaining studies is less than or
equal to 2.0. Elzayat et al (22) found that high INR and early
postoperative recovery of warfarin may be the main causes of blood
transfusion, but the average blood transfusion volume in the above
studies was not large (2.5 and 3.7 units). In addition, the results
of transfusion rate and decreased intraoperative hemoglobin were
inconsistent because the studies of transfusion rate were different
from the studies included in decreased intraoperative hemoglobin.
The results of this meta-analysis showed that the continuous use of
drugs during the perioperative period of laser surgery did not
increase decreased intraoperative hemoglobin and catheterization
duration. Therefore, continuous preoperative anticoagulation is
safe and feasible for BPH patients treated with laser surgery. In
addition, some studies have found that blood transfusion rates in
patients undergoing laser surgery were lower than that in TURP,
suggesting that the risk of bleeding from laser surgery is lower
than that in TURP (36,37). This may be because the laser has a
deeper solidification depth. The solidification depth of 2 µm laser
is ~0.5-1.0 mm, while the solidification depth of TURP is ~0.29 mm
(38).
It is also controversial whether heparin should be
used during the discontinuation of antithrombotic drugs. Ong et
al (20) believed that compared
with the discontinuation of antithrombotic drugs, low molecular
weight heparin replacement during the perioperative period of TURP
would lead to higher postoperative bleeding complications (44 vs.
0%) and higher thrombotic complications (17 vs. 0%), while Dotan
et al (18) considered that
low molecular weight heparin replacement during TURP would only
slightly extend the hospital stay and not lead to the increase of
intraoperative and postoperative bleeding events. This
meta-analysis found that in the laser BPH surgery perioperative
period, there was no obvious difference in blood transfusion rate
and catheterization duration between persistent-usage and heparin
group, but heparin replacement promotes the drop in intraoperative
hemoglobin, which reduced the value of low molecular weight heparin
replacement in laser surgery. In general, the safety of low
molecular weight heparin replacement in laser surgery is similar to
that of traditional antithrombotic drugs, except for the effect on
intraoperative hemoglobin. Therefore, we believe that low molecular
weight heparin replacement should be avoided when it is not
necessary. For patients at high risk of thrombosis, the surgeon may
prescribe low molecular weight heparin in appropriate amounts.
As meta-analysis is an observational study, its
results may be affected by bias, confounding and other factors. The
limitations of this paper are as follows: i) Most of the included
studies were based on the risk of cardiovascular and
cerebrovascular disease in each patient to decide whether to stop
antithrombotic drugs, resulting in our inability to analyze the
risk of thrombosis after drug withdrawal; ii) Prostate volume,
preoperative application of 5α reductase inhibitors, preoperative
indwelling catheter have been shown to affect bleeding after
prostate surgery, this meta-analysis did not consider these
factors.
In conclusion, the discontinuation of antithrombotic
drugs during the perioperative period of TURP can reduce the risk
of postoperative bleeding; however, the risk of cardiovascular and
cerebrovascular thrombosis and embolism after discontinuation
should be carefully evaluated preoperatively. Continuous use of
antithrombotic drugs during the perioperative period of laser BPH
surgery is safe and feasible, and can be used as the preferred BPH
surgical treatment for patients with high-risk cardiovascular and
cerebrovascular diseases. There is controversy over the need for
transitional treatment during the discontinuation of antithrombotic
drugs. However, due to the limitations of the quality of the
included studies, more high-quality studies are needed to verify
the above conclusions.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
QH designed the study and wrote the manuscript. YY
and FG acquired and analyzed the data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patients consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mobley D, Feibus A and Baum N: Benign
prostatic hyperplasia and urinary symptoms: Evaluation and
treatment. Postgrad Med. 127:301–307. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kim EH, Larson JA and Andriole GL:
Management of benign prostatic hyperplasia. Annu Rev Med.
67:137–151. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Aaron L, Franco OE and Hayward SW: Review
of prostate anatomy and embryology and the etiology of benign
prostatic hyperplasia. Urol Clin North Am. 43:279–288.
2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rauch M and Strunk H: Interventional
treatment of benign prostatic hyperplasia: Embolization of the
testicular vein. Radiologe. 57:652–658. 2017.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
5
|
Bach T, Xia SJ, Yang Y, Mattioli S, Watson
GM, Gross AJ and Herrmann TR: Thulium: YAG 2 mum cw laser
prostatectomy: where do we stand? World J Urol. 28:163–168.
2010.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Nunes R, Oliveira R, Carneiro A, Neto AM,
Antunes AA, Bernardo WM and Silvinato A: Brazilian Society of
Urology. Benign prostatic hyperplasia: Laser prostatectomy (PVP).
Rev Assoc Med Bras (1992). 63:929–940. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Skagseth E Jr: Retropubic prostatectomy. A
clinical review and follow-up study. Nord Med. 77:621–624.
1967.PubMed/NCBI(In Norwegian).
|
|
8
|
Romero-Otero J, García-González L,
García-Gómez B, Justo-Quintas J, García-Rojo E, González-Padilla
DA, Sopeña-Sutil R, Duarte-Ojeda JM and Rodríguez-Antolín A:
Factors influencing intraoperative blood loss in patients
undergoing holmium laser enucleation of the prostate (HoLEP) for
benign prostatic hyperplasia: A large multicenter analysis.
Urology. 132:177–182. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Meskawi M, Hueber PA, Valdivieso R,
Karakiewicz PI, Pradere B, Misrai V, Chughtai B and Zorn KC:
Complications and functional outcomes of high-risk patient with
cardiovascular disease on antithrombotic medication treated with
the 532-nm-laser photo-vaporization Greenlight XPS-180 W for benign
prostate hyperplasia. World J Urol. 37:1671–1678. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Biondi-Zoccai GG, Lotrionte M, Agostoni P,
Abbate A, Fusaro M, Burzotta F, Testa L, Sheiban I and Sangiorgi G:
A systematic review and meta-analysis on the hazards of
discontinuing or not adhering to aspirin among 50,279 patients at
risk for coronary artery disease. Eur Heart J. 27:2667–2674.
2006.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Proietti M, Mairesse GH, Goethals P,
Scavee C, Vijgen J, Blankoff I, Vandekerckhove Y and Lip GY:
Belgian Heart Rhythm Week Investigators. Cerebrovascular disease,
associated risk factors and antithrombotic therapy in a population
screening cohort: Insights from the Belgian Heart Rhythm Week
programme. Eur J Prev Cardiol. 24:328–334. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Stang A: Critical evaluation of the
Newcastle-Ottawa scale for the assessment of the quality of
nonrandomized studies in meta-analyses. Eur J Epidemiol.
25:603–605. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Watson CJ, Deane AM, Doyle PT and Bullock
KN: Identifiable factors in post-prostatectomy haemorrhage: The
role of aspirin. Br J Urol. 66:85–87. 1990.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Thurston AV and Briant SL: Aspirin and
post-prostatectomy haemorrhage. Br J Urol. 71:574–576.
1993.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ala-Opas MY and Grönlund SS: Blood loss in
long-term aspirin users undergoing transurethral prostatectomy.
Scand J Urol Nephrol. 30:203–206. 1996.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Nielsen JD, Holm-Nielsen A, Jespersen J,
Vinther CC, Settgast IW and Gram J: The effect of low-dose
acetylsalicylic acid on bleeding after transurethral prostatectomy
- a prospective, randomized, double-blind, placebo-controlled
study. Scand J Urol Nephrol. 34:194–198. 2000.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wenders M, Wenzel O, Nitzke T and Popken
G: Perioperative platelet inhibition in transurethral
interventions: TURP/TURB. Int Braz J Urol. 38:606–610.
2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Dotan ZA, Mor Y, Leibovitch I, Varon D,
Golomb J, Duvdevani M and Ramon J: The efficacy and safety of
perioperative low molecular weight heparin substitution in patients
on chronic oral anticoagulant therapy undergoing transurethral
prostatectomy for bladder outlet obstruction. J Urol. 168:610–614.
2002.PubMed/NCBI
|
|
19
|
Taylor K, Filgate R, Guo DY and Macneil F:
A retrospective study to assess the morbidity associated with
transurethral prostatectomy in patients on antiplatelet or
anticoagulant drugs. BJU Int. 108 (Suppl 2):45–50. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ong WL, Koh TL, Fletcher J, Gruen R and
Royce P: Perioperative management of antiplatelets and
anticoagulants among patients undergoing elective transurethral
resection of the prostate - A single institution experience. J
Endourol. 29:1321–1327. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Carmignani L, Macchi A, Ratti D,
Finkelberg E, Casellato S, Bozzini G, Maruccia S, Marenghi C and
Picozzi S: Are histological findings of thulium laser
vapo-enucleation versus transurethral resection of the prostate
comparable? Pathol Oncol Res. 21:1071–1075. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Elzayat E, Habib E and Elhilali M: Holmium
laser enucleation of the prostate in patients on anticoagulant
therapy or with bleeding disorders. J Urol. 175:1428–1432.
2006.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Tyson MD and Lerner LB: Safety of holmium
laser enucleation of the prostate in anticoagulated patients. J
Endourol. 23:1343–1346. 2009.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Bishop CV, Liddell H, Ischia J, Paul E,
Appu S, Frydenberg M and Pham T: Holmium laser enucleation of the
prostate: Comparison of immediate postoperative outcomes in
patients with and without antithrombotic therapy. Curr Urol.
7:28–33. 2013.PubMed/NCBI View Article : Google Scholar
|
|
25
|
El Tayeb MM, Jacob JM, Bhojani N,
Bammerlin E and Lingeman JE: Holmium laser enucleation of the
prostate in patients requiring anticoagulation. J Endourol.
30:805–809. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Sun J, Shi A, Tong Z and Xue W: Safety and
feasibility study of holmium laser enucleation of the prostate
(HOLEP) on patients receiving dual antiplatelet therapy (DAPT).
World J Urol. 36:271–276. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ruszat R, Wyler S, Forster T, Reich O,
Stief CG, Gasser TC, Sulser T and Bachmann A: Safety and
effectiveness of photoselective vaporization of the prostate (PVP)
in patients on ongoing oral anticoagulation. Eur Urol.
51:1031–1038. 2007.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Karatas OF, Alkan E, Horasanli K, Luleci H
and Sarica K: Photoselective vaporization of the prostate in men
with a history of chronic oral anti-coagulation. Int Braz J Urol.
36:190–197. 2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Sohn JH, Choi YS, Kim SJ, Cho HJ, Hong SH,
Lee JY, Hwang TK and Kim SW: Effectiveness and safety of
photoselective vaporization of the prostate with the 120 W HPS
Greenlight laser in benign prostatic hyperplasia patients taking
oral anticoagulants. Korean J Urol. 52:178–183. 2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Knapp GL, Chalasani V and Woo HH:
Perioperative adverse events in patients on continued
anticoagulation undergoing photoselective vaporisation of the
prostate with the 180-W Greenlight lithium triborate laser. BJU
Int. 119 (Suppl 5):33–38. 2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Macchione L, Mucciardi G, Gali' A, Di
Benedetto A, Butticè S and Magno C: Efficacy and safety of prostate
vaporesection using a 120-W 2-µm continuous-wave Tm:YAG laser
(RevoLix 2) in patients on continuous oral anticoagulant or
antiplatelet therapy. Int Urol Nephrol. 45:1545–1551.
2013.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Sener TE, Butticè S, Macchione L, Netsch
C, Tanidir Y, Dragos L, Pappalardo R and Magno C: Thulium laser
vaporesection of the prostate: Can we operate without interrupting
oral antiplatelet/anticoagulant therapy? Investig Clin Urol.
58:192–199. 2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Kaciulyte J, Losco L, Maruccia M, Delia G,
Lo Torto F, Di Taranto G, Caputo GG, Berchiolli R, Ribuffo D and
Cigna E: Postsurgical antithrombotic therapy in microsurgery: Our
protocol and literature review. Eur Rev Med Pharmacol Sci.
23:4448–4457. 2019.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Ondeck NT, Bohl DD, McLynn RP, Cui JJ,
Bovonratwet P, Singh K and Grauer JN: Longer operative time is
associated with increased adverse events after anterior cervical
diskectomy and fusion: 15-minute intervals matter. Orthopedics.
41:e483–e488. 2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Catanzarite T, Saha S, Pilecki MA, Kim JY
and Milad MP: Longer operative time during benign laparoscopic and
robotic hysterectomy is associated with increased 30-day
perioperative complications. J Minim Invasive Gynecol.
22:1049–1058. 2015.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Bruyère F, Huglo D, Challacombe B, Haillot
O, Valat C and Brichart N: Blood loss comparison during
transurethral resection of prostate and high power GreenLight(™)
laser therapy using isotopic measure of red blood cells volume. J
Endourol. 25:1655–1659. 2011.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Ruszat R, Wyler SF, Seitz M, Lehmann K,
Abe C, Bonkat G, Reich O, Gasser TC and Bachmann A: Comparison of
potassium-titanyl-phosphate laser vaporization of the prostate and
transurethral resection of the prostate: update of a prospective
non-randomized two-centre study. BJU Int. 102:1432–1439.
2008.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Wendt-Nordahl G, Huckele S, Honeck P,
Alken P, Knoll T, Michel MS and Häcker A: Systematic evaluation of
a recently introduced 2-microm continuous-wave thulium laser for
vaporesection of the prostate. J Endourol. 22:1041–1045.
2008.PubMed/NCBI View Article : Google Scholar
|