Introduction
Transient paralysis following surgical decompression
is a severe postoperative complication that may occur in patients
with chronic severe spinal cord compression (1). Spinal cord ischemia-reperfusion injury
has been confirmed as a potential etiology of the associated
neurological deterioration. Spinal cord ischemia-reperfusion injury
is defined as the sudden expansion of the compressed cord and
exposure to a rush in blood supply following decompression surgery,
which leads to disruption of the blood-brain barrier and
blood-spinal cord barrier, and may ultimately result in acute
neurologic dysfunction (2,3). The reported incidence rate of spinal
cord ischemia-reperfusion injury following cervical decompression
surgery ranges from 2-5.7%, but a higher incidence rate of 14.5%
has been reported for posterior decompressive laminectomy
procedures used for thoracic spinal stenosis (4,5).
‘White cord syndrome’, initially described by Chin et al
(2) in 2013, is an imaging feature
of spinal cord ischemia-reperfusion injury that is present on
postoperative MRI scans. ‘White cord syndrome’ refers to high
intramedullary signal changes observed on sagittal T2-weighted MRI
scans in patients with unexplained incomplete paralysis following
cervical decompression surgery (2).
In the present study, the 9th case of ‘white cord syndrome’
following cervical decompression surgery according to previous
literature, was reported.
Case report
A 51-year old male presented with the chief
complaint of numbness in the bilateral upper extremities and an
unsteady gait for 6 months. Neurological examination indicated that
muscle strength in the left upper limb was grade 4/5 from the
Medical Research Council Scale (6).
Tendon reflexes, including biceps, triceps, radial periosteal,
knees and ankles, displayed bilateral hyperreflexia. A positive
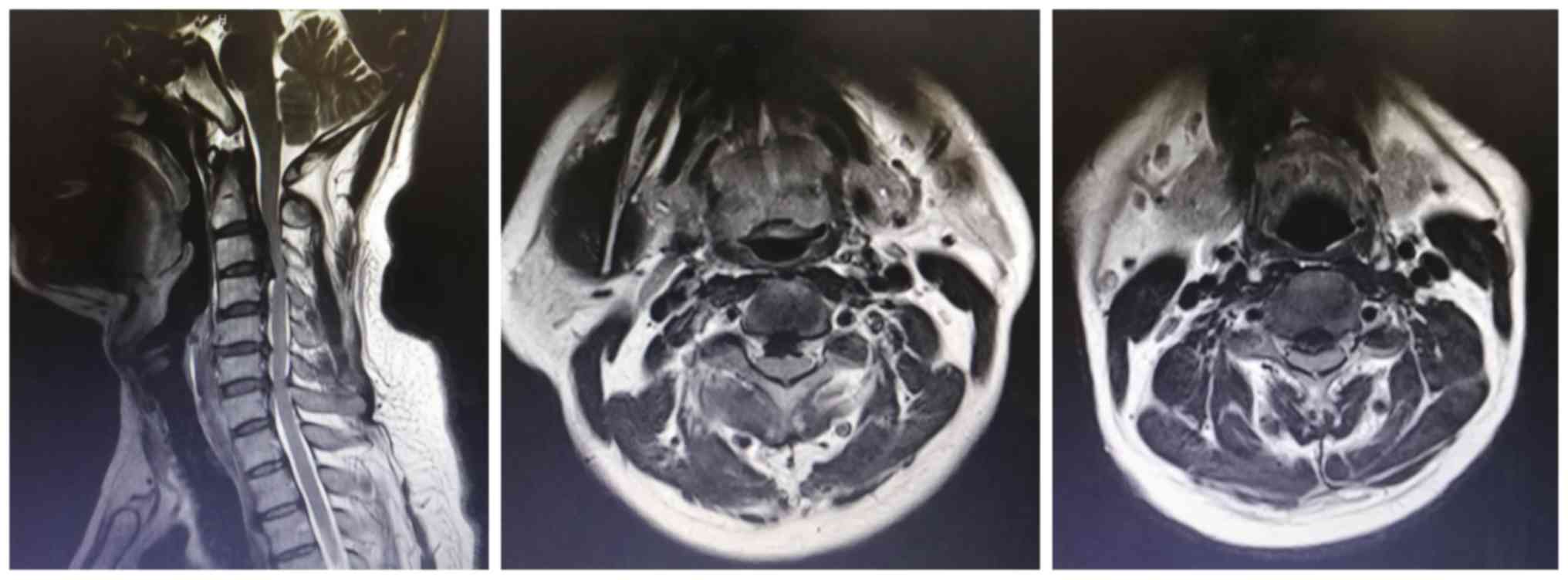
Babinski sign was also identified bilaterally. The preoperative
cervical CT and MRI scans revealed that the spinal cord was
anteriorly compressed by ossification of the posterior longitudinal
ligament (OPLL) at the C2-C4 levels, which led to severe cervical
spinal stenosis (Figs. 1 and
2). On CT, the occupying ratio
(calculated as the thickness of OPLL/the anteroposterior diameter
of the spinal canal) at the C2/3 and C3/4 levels was ~46.7 and 63%,
respectively (Fig. 1).
Due to the difficulty in operative exposure and high
risk of cerebrospinal fluid leakage by either anterior cervical
decompression and fusion (ACDF) or anterior cervical corpectomy and
fusion (ACCF) for high-level cervical spondylotic myelopathy
combined with OPLL (C2-C4), the patient underwent C3-C4 posterior
laminectomy decompression and C2-C5 fixation with pedicle screws.
Intraoperatively, sudden cord expansion occurred after the
vertebral plates were completely removed. An intravenous
methylprednisolone bolus (500 mg) was immediately administrated. On
return to the ward, the patient displayed hemiplegic paralysis and
was not able to move the left limb, displaying a muscle strength of
grade 1/5 in the lower left extremity and grade 2/5 in the upper
left extremity. Reperfusion injury following acute decompression of
the severely and chronically compressed spinal cord was highly
suspected in the patient; therefore, high-dose methylprednisolone
combined with mannitol and neurotrophic drugs were rapidly
administered intravenously. The patient received methylprednisolone
(30 mg/kg) over 15 min, followed by a 45-min rest and a 23-h
maintenance infusion (5.4 mg/kg/h), according to the National Acute
Spinal Cord Injury Study II (NASCIS-2) protocol (7). In addition, omeprazole (40 mg) was
administered to the patient prior to each dose of
methylprednisolone to prevent gastrointestinal bleeding, which may
be caused by high-dose methylprednisolone. Furthermore,
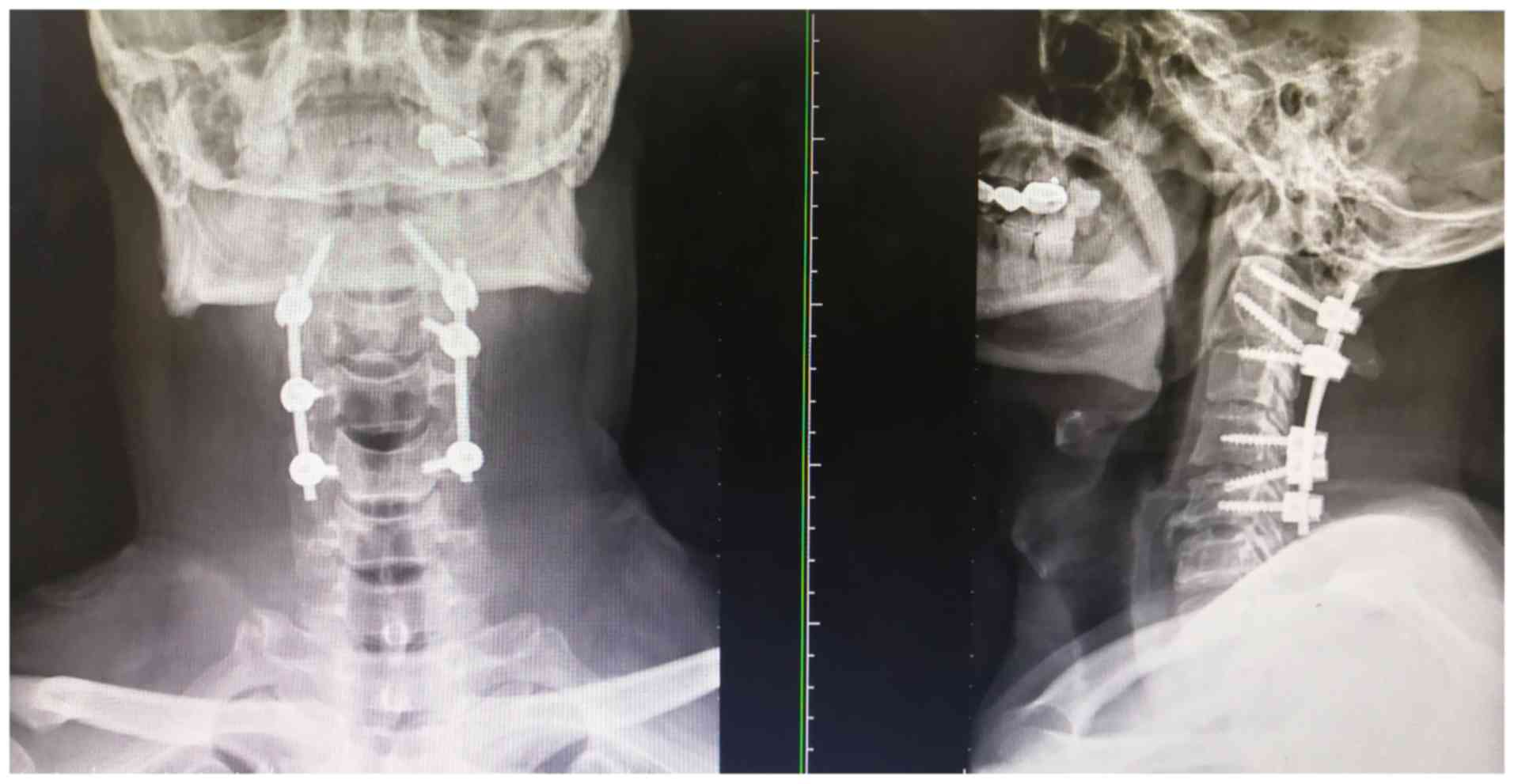
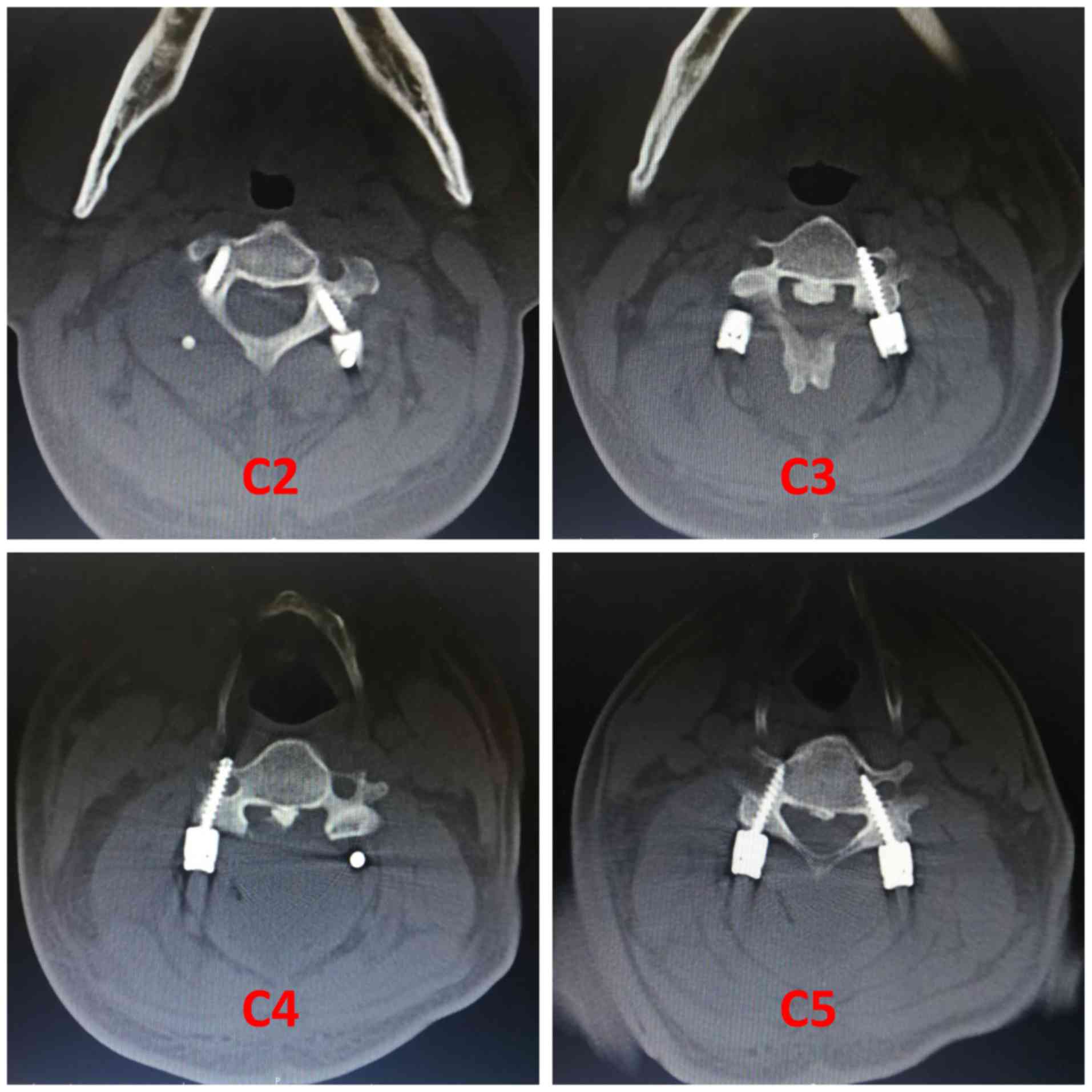
postoperative X-ray, CT and MRI scans were performed to evaluate
the spinal cord function. X-ray and CT scans displayed satisfactory
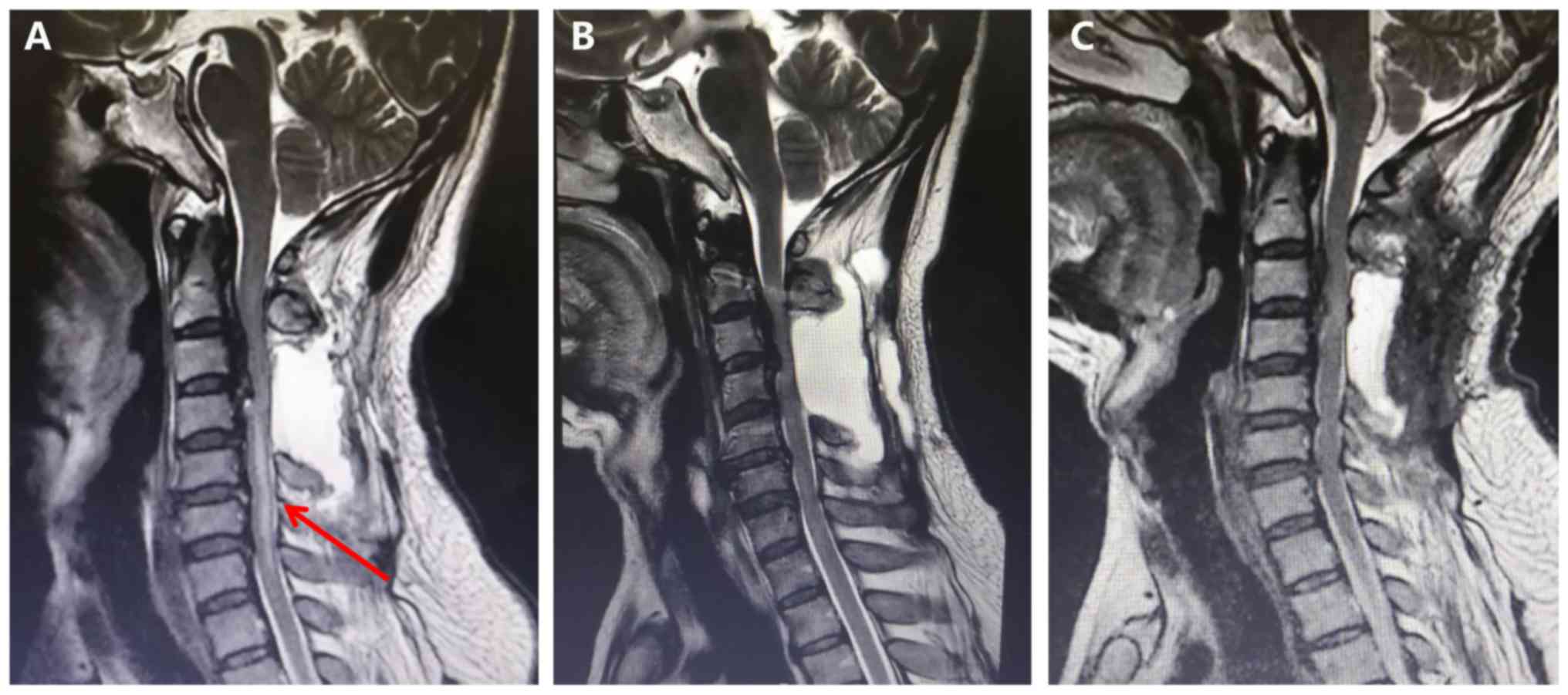
positioning of the pedicle screws (Figs. 3 and 4). However, T2-weighted MRI scans
demonstrated a signal of abnormally high intensity in the spinal
cord at the C4-C7 levels. In addition, a large-area hyperintense
signal was observed behind the epidural at the C3-C6 levels, which
indicated cerebrospinal fluid leakage (Fig. 5A). At 12 h post-methylprednisolone
treatment, the patient's muscle strength improved by one grade to
grade 2/5 in the left lower extremity and to grade 3/5 in the left
upper extremity. On postoperative day 5, the muscle strength in the
left limb recovered to grade 4/5, which was the same as the
preoperative level. Considering the patient displayed no wound
exudation, fever or dizziness, the postoperative cerebrospinal
fluid leakage was dynamically observed without treatment. At day 8
post-surgery, the patient was discharged to rehabilitation with
hyperbaric oxygen therapy.
At the 2-month follow-up, the patient's neurological
status had not deteriorated; however, the patient complained of
neck swelling and associated pain following the surgery. MRI scans
were repeatedly performed to assess the spinal cord injury and
cerebrospinal fluid leakage. The intensity of the spinal cord
signal had almost returned to normal at the C4-C7 levels (Fig. 5B); however, the area of
cerebrospinal fluid leakage had not decreased, but had expanded to
the subcutaneous tissue. The patient was readmitted for an
additional cerebrospinal fluid leakage exploration and neoplasty.
During the second surgery, an abundance of clear liquid was
released when the wound was reopened. A large crevasse was
identified on the left side of the dura, close to the pedicle at
the C4 level, and an artificial dura mater was used to repair the
crevasse (Fig. S1). At 2 weeks
post-surgery, the neck swelling and associated pain was relieved
and an MRI scan indicated that the area of cerebrospinal fluid
leakage had obviously decreased (Fig.
5C). The patient was then discharged to an inpatient
rehabilitation center for physical therapy. At the last 6-month
telephone follow-up, his neurological function was stable without
neck swelling and associated pain.
Discussion
Fixation failure, epidural hematoma, spinal cord
edema and ischemia-reperfusion injury are the major factors that
contribute to acute paralysis following spinal surgery (8). On postoperative CT and MRI scans, it
is possible to identify the position of the implant and epidural
hematomas, respectively. Spinal cord edema typically peaks at 48-72
h post-surgery and symptoms may be relieved by dehydration.
Diagnostic criteria for spinal cord ischemia-reperfusion injury
primarily include the following: Severe spinal cord compression;
surgical decompression; paralysis occurring within 3 h
post-surgery; motor and sensory dysfunction from lower to upper
limb; exclusion of other causative factors, including hematoma; and
completely or partially restored neurological function by timely
high-dose methylprednisolone combined with dehydration and
neurotrophic drugs (9,10). Zhang et al (8) reported on three cases where transient
paralysis had occurred from 30 min to 4 h post-ACCF in patients
with cervical spondylotic myelopathy. However, no hematoma was
identified in the post-operative MRI scans; therefore, spinal cord
ischemia-reperfusion injury was suspected. Following administration
of high-dose methylprednisolone combined with dehydration and
neurotrophic drugs, a full recovery was achieved in two patients.
By contrast, the neurological function of one patient was not
restored until an additional cervical posterior decompression
procedure was performed. The pathogenesis of the patients was
identical to that in the case reported by Khan et al
(11), who described a 36-year-old
male who had developed a delayed neurological deficit on day 3
post-ACDF for C5-6 cervical disc herniation.
Postoperative spinal cord ischemia-reperfusion
injury has not only been reported in cervical decompression
surgery, but also in posterior decompression for thoracic spinal
stenosis caused by ossification of the ligamentum flavum (OLF) and
OPLL. Yamazaki et al (12)
described the case of a 71-year old female who was diagnosed with
thoracic myelopathy caused by OPLL and OLF, and underwent a
thoracic posterior laminectomy at T10-T11. At 18 h post-surgery,
the patient was suddenly not able to move both lower extremities,
displaying of muscle strength of grade 0/5. Despite immediately
administering an intravenous bolus dose of methylprednisolone
sodium succinate (1 g) followed by an additional 2-h maintenance
infusion of methylprednisolone sodium succinate (1 g), the
patient's motor function did not improve. At 4 h post-paralysis,
the patient received an additional posterior instrumented fusion at
T7-L1. At 3 h after the second surgery, the patient's motor
function gradually recovered. At the final follow-up (5 years and 9
months post-surgery), the patient's neurological status was
improved and stabilized with grade 4-5/5 muscle strength in both
lower extremities. In addition, a high-intensity signal was
observed at T10-T11 on the T2-weighted MRI performed 1 week after
the second surgery and the signal intensity returned to normal when
the patient's neurological function improved. Based on this case,
it was recommended that posterior instrumented fusion should be
used to reduce postoperative paralysis when posterior decompression
for thoracic OLF and OPLL is performed. Similarly, Taher et
al (13) reported on three
cases with transient neurological deficit without spinal cord
injury following decompression for severe thoracic stenosis. The
recovery time among the patients ranged from 1-13 months.
Ischemia-reperfusion injury was regarded as the major cause of
postoperative paralysis. Furthermore, intraoperative
electrophysiological monitoring, which changed immediately once
paralysis had occurred during surgery, was recommended as a useful
tool to avoid neurological deterioration. In addition, Yang et
al (14) reported that 10
patients developed delayed neurological deficits following surgical
removal of intraspinal meningiomas (7 located in the thoracic
region and 3 located in the cervical region). The occurrence time
in those cases was 3-8 h post-surgery. Postoperative T2-weighted
MRI scans revealed high intramedullary signal changes in four
patients; however, ischemia-reperfusion injury was also considered
to be responsible for the observed deterioration.
The most widely accepted pathophysiological
mechanism underlying ‘white cord syndrome’ is the sudden expansion
of the chronically compressed cord and subsequent exposure to a
rush of blood supply following decompression surgery, which
triggers an inflammatory cascade and releases oxygen free radicals,
ultimately leading to neuronal membrane damage (15,16).
Chin et al (2) reported the
first case of ‘white cord syndrome’ in a 59-year old male with
severe C5/6 disc herniation who had undergone ACDF at the C4/5 and
C5/6 level. The patient displayed complete loss of somatosensory
evoked potentials (SSEPs) during the operation and postoperative C6
incomplete tetraplegia. A large area of high signal intensity was
identified in the spinal cord on the postoperative MRI scan, and
the term ‘white cord syndrome’ was used, referring to the
radiographic changes. Following on from the aforementioned study,
white cord syndrome after anterior or posterior cervical
decompression has received increasing attention. Antwi et al
(17) reported the case of ‘white
cord syndrome’ in a 68-year-old male who had developed acute
hemiparesis on the left side following C4-C7 posterior laminectomy
decompression in 2018. Also in 2018, Vinodh et al (3) reported similar findings in a
51-year-old female who was diagnosed with a metastatic intraspinal
tumor and presented with quadriplegia following posterior cervical
laminectomy and fusion for tumor resection. Papaioannou et
al (18) reported the case of
‘white cord syndrome’ in a 79-year old male who had undergone C4-C6
ACDF 2 years previously because of cervical spondylotic myelopathy.
The patient suffered from C6 incomplete paraplegia after the second
C3-C6 posterior decompression surgery. Papaioannou et al
(18) further indicated that
differential diagnoses of ‘white cord syndrome’ included iatrogenic
trauma leading to cerebrospinal fluid leakage, pseudo meningocele,
cerebrovascular injury and demyelinating disease. According to the
latest literature review of ‘white Cord syndrome’ by Mathkour et
al (16), there are a total of
7 cases, including 2 cases after ACDF surgery and 5 cases following
posterior cervical decompression surgery. Recently, another case of
‘white Cord syndrome’ after ACDF is reported by Jun et al
(19). Consistent with previous
cases, high intramedullary signals were also observed on the
postoperative sagittal T2-weighted MRI scan and the neurologic
deficit was reversed by immediate high-dose steroid administration
in the case reported in the present study. Furthermore, although
the patient displayed cerebrospinal fluid leakage, ‘white cord
syndrome’ was diagnosed on the basis of the observation that the
hyperintense signal in the spinal cord disappeared, although
cerebrospinal fluid leakage was still present at the 2-month
follow-up, prior to the cerebrospinal fluid leakage exploration and
neoplasty.
Ever since positive results of the NASCIS-2 protocol
were reported in 1990(7), the use
of high-dose methylprednisolone for the treatment of acute spinal
cord injury has been widely accepted worldwide. According to the
guidelines published in 2017, treatment strategy of 24-h infusion
of high-dose methylprednisolone is recommended for patients within
8 h following injury (20). To
identify the exact pathological mechanisms underlying
ischemia-reperfusion injury caused by decompression, a number of
studies established a mouse model of degenerative cervical
myelopathy (DCM). Yang et al (1) reported that surgical decompression
increased the expression of inflammatory cytokines, including TNF-α
and IL-1β, in an animal model of chronic severe spinal cord
compression. Similarly, Vidal et al (21) suggested that decompression led to a
1.5- to 2-fold increase in expression levels of inflammatory
cytokines in a mouse model of DCM. It was also reported that
delayed decompression aggravated ischemia-reperfusion injury,
resulting in decreased neurological improvement compared with
earlier intervention. In another study, perioperative
methylprednisolone treatment (30 min prior to decompression and 2
weeks after decompression at one dose of 30 mg/kg) reduced
neurological deterioration caused by ischemia-reperfusion injury
via its anti-inflammatory effect in a mouse model of DCM (22). In animal models, the levels of
inflammatory cytokines such as TNF-α and IL-1β increased when
decompression-associated spinal cord ischemia-reperfusion injury
occurred, indicating that inflammatory cytokines may be considered
as an important evaluation indicator of decompression-associated
spinal cord ischemia-reperfusion injury (1,21,22).
In the case described in the present study, signals
of abnormally high intensity in the spinal cord were detected on
the postoperative sagittal T2-weighted MRI scan once acute
paralysis had occurred, which displayed similarities to the
aforementioned cases of ‘white cord syndrome’ (2,3,17,18).
The neurological function of the patient gradually improved with
the administration of high-dose methylprednisolone therapy,
according to the NASCIS-2 protocol. Although cerebrospinal fluid
leakage occurred in the patient, transient paralysis was not
attributed to this iatrogenic injury because the muscle strength in
the left limb had recovered to normal prior to the cerebrospinal
fluid leakage exploration and neoplasty. A limitation of the
management of the case reported in the present study was that
intraoperative neurophysiological monitoring was not conducted to
evaluate SSEPs and motor-evoked potential (MEP) alterations during
the operation.
Despite the low incidence rate of ‘white cord
syndrome’, spinal surgeons should take action to reduce the risk of
this disastrous complication when performing posterior cervical
decompression surgery for chronic severe spinal cord compression.
First, preoperative remote ischemic preconditioning, consisting of
three cycles of upper right limb ischemia for 5 min with 5-min
intervals of reperfusion between each cycle, may prevent spinal
cord ischemic injury by reducing neuro-specific enolase and S-100B
expression after surgery. Enolase and S-100B are two useful
diagnostic biomarkers for spinal cord injury (4). Furthermore, intraoperative
neurophysiological monitoring is an effective tool to evaluate SSEP
and MEP alterations, and to indicate whether spinal cord injury has
occurred during surgery (23).
Finally, posterior cervical laminectomies were performed in all
reported cases of ‘white cord syndrome’ following posterior
decompression surgery (3,17,18),
including the present case report. In all cases, it may be
recommended to opt for posterior cervical laminoplasty instead of
posterior cervical laminectomy to avoid excessive expansion of the
spinal cord and to reduce the risk of ischemia-reperfusion
injury.
Cerebrospinal fluid leak, as a postoperative
complication of decompression surgery, occurred in the case
reported in the present study. Small and invisible dura defects
caused by bipolar coagulation were not identified intraoperatively
and dura repair was not performed until the second revision
surgery. Cerebrospinal fluid leak repair primarily involves primary
or delayed repair (with a non-absorbable suture or fibrin sealant)
and lumbar drainage (15-20 ml/h for 5 days) (24). Woodroffe et al (24) analyzed the clinical prognosis of 124
patients with cerebrospinal fluid leak using different treatments.
The successful repair rate was 73.4% (47/64) in the primary repair
group and 87.8% (43/49) in the lumbar drainage group. Furthermore,
39.5% of the patients who had not received primary repair and
lumbar drainage procedures were subjected to revision surgery.
Delayed repair was also associated with increased hospital stays
and higher risk of infection compared with primary repair.
Therefore, the analysis emphasized the importance of intraoperative
prompt identification and strongly recommended that primary repair
of dura defects should be combined with lumbar drainage whenever
possible. In another study, Fang et al (25) proposed two treatment strategies for
preventing cerebrospinal fluid leak: i) Direct suture with a dural
substitute material; and ii) reducing the subarachnoid fluid
pressure or increasing the epidural space pressure.
In conclusion, transient paralysis following
surgical decompression for chronic severe spinal cord compression
is a catastrophic postoperative complication. Spinal cord
ischemia-reperfusion injury, which has an imaging feature of high
intramedullary signal changes on the postoperative sagittal
T2-weighted MRI scan and therefore referred to as ‘white cord
syndrome’, has been considered as an important pathogenic factor
contributing to neurological deterioration. Regardless of its low
incidence rate, surgeons should be aware of this devastating
complication, particularly when treating long-term and severe
spinal stenosis caused by OPLL and OLF. Once transient paralysis
occurs, early diagnosis and high-dose methylprednisolone therapy
are essential to reverse the associated neurological deficits.
Supplementary Material
A large crevasse (as indicated by the
red arrow) was identified on the left side of the dura during the
second surgery.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article and its supplementary
information files.
Authors' contributions
YXL designed the study, collected clinical data and
drafted the manuscript. SSH and ZMH designed the study and
critically revised the manuscript. All of the authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the Shanghai 10th People's Hospital (SHSY-IEC-4.1/20-17/01). The
patient signed the informed consent form.
Patient consent for publication
Written informed consent for the publication of
patient data and accompanying images was obtained.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yang T, Wu L, Wang H, Fang J, Yao N and Xu
Y: Inflammation level after decompression surgery for a rat model
of chronic severe spinal cord compression and effects on
ischemia-reperfusion injury. Neurol Med Chir (Tokyo). 55:578–586.
2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chin KR, Seale J and Cumming V: ‘White
cord syndrome’ of acute tetraplegia after anterior cervical
decompression and fusion for chronic spinal cord compression: A
case report. Case Rep Orthop. 2013(697918)2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Vinodh VP, Rajapathy SK, Sellamuthu P and
Kandasamy R: White cord syndrome: A devastating complication of
spinal decompression surgery. Surg Neurol Int.
9(136)2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hu S, Dong HL, Li YZ, Luo ZJ, Sun L, Yang
QZ, Yang LF and Xiong L: Effects of remote ischemic preconditioning
on biochemical markers and neurologic outcomes in patients
undergoing elective cervical decompression surgery: A prospective
randomized controlled trial. J Neurosurg Anesthesiol. 22:46–52.
2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Young WF and Baron E: Acute neurologic
deterioration after surgical treatment for thoracic spinal
stenosis. J Clin Neurosci. 8:129–132. 2001.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Vanpee G, Hermans G, Segers J and
Gosselink R: Assessment of limb muscle strength in critically ill
patients: A systematic review. Crit Care Med. 42:701–711.
2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Bracken MB, Shepard MJ, Collins WF,
Holford TR, Young W, Baskin DS, Eisenberg HM, Flamm E, Leo-Summers
L, Maroon J, et al: A randomized, controlled trial of
methylprednisolone or naloxone in the treatment of acute
spinal-cord injury Results of the Second National acute spinal cord
injury study. N Engl J Med. 322:1405–1411. 1990.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhang JD, Xia Q, Ji N, Liu YC, Han Y and
Ning SL: Transient paralysis shortly after anterior cervical
corpectomy and fusion. Orthop Surg. 5:23–28. 2013.PubMed/NCBI View
Article : Google Scholar
|
|
9
|
Jiang X, Shi E, Nakajima Y and Sato S:
Postconditioning, a series of brief interruptions of early
reperfusion, prevents neurologic injury after spinal cord ischemia.
Ann Surg. 244:148–153. 2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Back MR, Bandyk M, Bradner M, Cuthbertson
D, Johnson BL, Shames ML and Bandyk DF: Critical analysis of
outcome determinants affecting repair of intact aneurysms involving
the visceral aorta. Ann Vasc Surg. 19:648–656. 2005.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Khan MF, Jooma R, Hashmi FA and Raghib MF:
Delayed spinal cord infarction following anterior cervical surgical
decompression. BMJ Case Rep. 2017(bcr2017219863)2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yamazaki M, Koda M, Okawa A and Aiba A:
Transient paraparesis after laminectomy for thoracic ossification
of the posterior longitudinal ligament and ossification of the
ligamentum flavum. Spinal Cord. 44:130–134. 2006.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Taher F, Lebl DR, Cammisa FP, Pinter DW,
Sun DY and Girardi FP: Transient neurological deficit following
midthoracic decompression for severe stenosis: A series of three
cases. Eur Spine J. 22:2057–2061. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yang T, Wu L, Deng X, Yang C, Zhang Y,
Zhang D and Xu Y: Delayed neurological deterioration with an
unknown cause subsequent to surgery for intraspinal meningiomas.
Oncol Lett. 9:2325–2330. 2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wiginton J IV, Brazdzionis J, Mohrdar C,
Sweiss R and Lawandy S: Spinal cord reperfusion injury: Case
report, review of the literature, and future treatment strategies.
Cureus. 11(e5279)2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Mathkour M, Werner C, Riffle J, Scullen T,
Dallapiazza RF, Dumont A and Maulucci C: Reperfusion ‘White Cord’
syndrome in cervical spondylotic myelopathy: Does mean arterial
pressure goal make a difference? Additional case and literature
review. World Neurosurg. 137:194–199. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Antwi P, Grant R, Kuzmik G and Abbed K:
‘White Cord Syndrome’ of acute hemiparesis after posterior cervical
decompression and fusion for chronic cervical stenosis. World
Neurosurg. 113:33–36. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Papaioannou I, Repantis T, Baikousis A and
Korovessis P: Late-onset ‘White Cord Syndrome’ in an elderly
patient after posterior cervical decompression and fusion: A case
report. Spinal Cord Ser Cases. 5(28)2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Jun DS, Baik JM and Lee SK: A case report:
White cord syndrome following anterior cervical discectomy and
fusion: Importance of prompt diagnosis and treatment. BMC
Musculoskelet Disord. 21(157)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Fehlings MG, Wilson JR, Tetreault LA,
Aarabi B, Anderson P, Arnold PM, Brodke DS, Burns AS, Chiba K,
Dettori JR, et al: A Clinical practice guideline for the management
of patients with acute spinal cord injury: Recommendations on the
Use of methylprednisolone sodium succinate. Global Spine J. 7 (3
Suppl):S203–S211. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Vidal PM, Karadimas SK, Ulndreaj A,
Laliberte AM, Tetreault L, Forner S, Wang J, Foltz WD and Fehlings
MG: Delayed decompression exacerbates ischemia-reperfusion injury
in cervical compressive myelopathy. J CI Insight.
2(e92512)2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Vidal PM, Ulndreaj A, Badner A, Hong J and
Fehlings MG: Methylprednisolone treatment enhances early recovery
following surgical decompression for degenerative cervical
myelopathy without compromise to the systemic immune system. J
Neuroinflammation. 15(222)2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Sutter M, Eggspuehler A, Jeszenszky D,
Kleinstueck F, Fekete TF, Haschtmann D, Porchet F and Dvorak J: The
impact and value of uni- and multimodal intraoperative
neurophysiological monitoring (IONM) on neurological complications
during spine surgery: A prospective study of 2728 patients. Eur
Spine J. 28:599–610. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Woodroffe RW, Nourski KV, Helland LC,
Walsh B, Noeller J, Kerezoudis P and Hitchon PW: Management of
iatrogenic spinal cerebrospinal fluid leaks: A cohort of 124
patients. Clin Neurol Neurosurg. 170:61–66. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Fang Z, Tian R, Jia YT, Xu TT and Liu Y:
Treatment of cerebrospinal fluid leak after spine surgery. Chin J
Traumatol. 20:81–83. 2017.PubMed/NCBI View Article : Google Scholar
|