Introduction
A previous study has reported that 20-58% of
patients with congenital scoliosis may suffer from intraspinal
abnormalities at the same time (1,2).
Intraspinal abnormalities may contribute to many problems, such as
neurological dysfunction and maldistribution of trunk muscle
strength, which may further induce neuromuscular scoliosis
(3). Neurological dysfunction
resulting from intraspinal abnormalities can lead to continuous
development of scoliosis, which eventually aggravates neurological
dysfunction. Treatment of intraspinal abnormalities, as well as
correction of scoliosis, is required for these patients. To improve
nerve function and reduce surgery-related complications, a
two-stage surgical strategy is considered typical treatment for
this disease. First, intraspinal abnormalities are treated by a
neurosurgeon. Second, corrective surgery is performed by an
orthopedic surgeon 3-6 months after the first-stage surgery. This
surgical procedure can not only avoid over-traction of the spinal
cord induced by intraspinal abnormalities during corrective
surgery, but also allows for examination of nerve function and the
identification of causes of complications during the second surgery
(4,5).
Nevertheless, there are some limitations to this
strategy: i) This procedure contains more than one surgery and
exposes the patients to the risks of multiple operations and
anesthesia; ii) the primary surgery can destroy the anatomical
markers, increasing the difficulty of the second-stage surgery;
iii) the adhesions preformed in the primary surgical site can cause
difficulties for osteotomy and hemivertebrectomy, and also
increases the risk of iatrogenic neural element injury. In
addition, scoliosis of more than 40 can still progress following
treatment of intraspinal abnormalities, which requires further
corrective surgery (6).
With the development of neuroelectrophysiological
monitoring technology, it is possible to monitor changes in nerve
function (7). To avoid the
disadvantages of two-stage surgery, single-stage surgery for
intraspinal abnormalities and scoliosis has recently been performed
in some institutions (2,6). Thus, the purpose of the present study
was to evaluate the safety and efficacy of single-stage surgical
treatment for spinal deformity and coexisting intraspinal
pathologies.
Materials and methods
Subjects
A total of 12 consecutive patients with intraspinal
abnormalities who underwent single-stage surgery between October
2016 and September 2017 at the Xuanwu Hospital of Capital Medical
University (Beijing, China) were included in the current study (7
males and 5 females). Inclusion criteria included: i) Scoliosis
with intraspinal lesions; ii) coronal Cobb angle >40 or sagittal
kyphosis deformity; and iii) single-stage surgery for
scoliosis/kyphosis deformity and intraspinal lesions. Exclusion
criteria included: i) Coronal Cobb angle <40 and no kyphosis
deformity in the sagittal plane; and ii) staged surgery for
intraspinal lesions and scoliosis. The mean age was 29.5±13.7 years
(range, 11-52 years). Progressive scoliosis was observed in all the
12 patients, and 5 of the 12 patients were diagnosed with
congenital scoliosis, including 1 wedge-shaped vertebra, 1
malsegmentation, 1 wedge-shaped vertebra combined with
malsegmentation and 2 hemivertebra with malsegmentation. In
addition, 7 patients were diagnosed with neuromuscular scoliosis.
Risser sign (8) was level 2 in 1
patient, level 3 in 2 patients and level 5 in 9 patients. Spinal
MRI scanning showed that 7 patients had tethered cord secondary to
scoliosis and 6 patients had syringomyelia. Epidermoid cyst was
observed in 2 patients and ganglioma was found in 1 patient.
Intraspinal lipoma was confirmed in 1 patient and meningioma was
observed in 1 patient. The mean coronal scoliosis Cobb angle was
65.9±13.4 (range, 48-93). The mean sagittal kyphosis angle was
71.1±19.5 (range, 44-94). No abnormality was observed in upper
extremity myodynamia or muscular tension in the 12 patients. Lower
myodynamia of the lower extremity was observed in 10 patients,
including level 0 in 4 patients, level 2 in 1 patient, level 3 in 4
patients, level 4 in 1 patient and level 5 in 2 patients. Higher
muscular tension of the lower extremity was observed in 8 patients.
Preoperative sphincter disturbances were observed in 10 patients.
The current study was approved by the ethics committee of the
Xuanwu Hospital of Capital Medical University and all the patients
or their families gave informed consent and signed a statement to
that effect.
Preoperative preparations
The general information including patient name, sex,
age and syndromes of nervous system was recorded. Preoperative and
postoperative anteroposterior and lateral full spine standing
images, CT scanning and 3D reconstruction and MRI scanning of spine
were performed to evaluate spine deformity and intraspinal
abnormalities. Ultrasound examination of urinary system was
performed to assess urinary system deformity. ECG and color Doppler
echocardiography were used to evaluate cardiac function. A
pulmonary function test (9) was
performed to evaluate the progress of ventilatory dysfunction.
Surgical procedure
The fused segments and osteotomy level were decided
according to the preoperative radiological results. Following
general anesthesia with tracheal intubation, the patient was put in
a prone position. The spinous process and vertebral plate surgical
levels were carefully explored. Vertebral deformity, fusion and
dysplasia were identified attentively and carefully handled to
avoid spinal cord injury induced by surgical instruments,
especially for patients with spinous process and vertebral plate
absence. Following localization of operative segments by
intraoperative X-ray, pedicle screws were planted into planned
segments. X-ray scanning was performed again to make sure all the
screws were in the correct position. As the spinal cord was close
to the concave side, pedicle screws on this side were carefully
inserted to protect the spinal cord. Following the planting of all
the pedicle screws, intraspinal abnormalities were handled under a
microscope. Spinal cord untethering was performed for patients with
tethered spinal cord. Lesion resection was performed for patients
with epidermoid cysts, ganglioma, intraspinal lipoma and
meningioma. No special treatment was performed for syringomyelia.
After the spinal cord was released, posterior osteotomy and
correction were performed under the microscope according to the
different spinal deformities. Usually, Schwab grade 2 osteotomy was
performed at the apical level of scoliosis or kyphosis, and one
segment above and below the apex. For patients with congenital
scoliosis or severe kyphosis, Schwab grade 3 or 4 osteotomy was
performed according to different deformities or the desired
correction. Following osteotomy, a pre-bending rod based on the
desired correction was planted. Then compression of the convex side
and distraction of the concave side were performed to correct the
deformity. The sagittal alignment of the spine should be considered
when bending the rod. Finally, mixed autogenous and allograft bone
grafting and fusion were performed. During surgery, all the
patients were under neuroelectrophysiological monitoring, including
somatosensory evoked potential, motor evoked potential and
sphincter monitoring. Following surgery, the drainage tube was
removed when the daily volume of the drainage was <20 ml, and
walking exercise under brace was allowed after the drainage tube
was removed. Exercise under brace was required for 3 months
postoperatively.
Operation effect evaluation
The operation success rate, operation time,
interoperative blood loss, fusion segments, scoliosis and kyphosis
Cobb angle, treatment of intraspinal pathology, nervous system
function and muscular strength and tension of the upper and lower
extremities were recorded. Postoperative complications, including
infection, cerebrospinal fluid leakage, spine fixation failure and
fracture of pedicle screws and rods, were reviewed. During the
follow-up time, complications such as nervous system dysfunction,
delayed infection and pseudoarthrosis were recorded.
Statistics analysis
All the data analysis was performed using SPSS 23.0
statistical software (IBM Corp.). A paired sample t-test was
performed for the data with a normal distribution. Data with a
normal distribution are presented as average value ± standard
deviation Data with a non-normal distribution are presented as the
median and interquartile range [M (P25, P75)]. P<0.05 was
considered to indicate a statistically significant difference.
Results
Changes of scoliosis and intraspinal
abnormalities
The general information of the patients is listed in
Table I. Single-stage surgery was
performed on all 12 patients with scoliosis and intraspinal
abnormalities. The surgical success rate was 100%. The average
surgical time was 451±154 min (IQR, 241-631 min) and the median
value of blood loss was 1,570.8±770.6 ml (IQR, 400-2,650 ml). The
mean length of the fused level was 11.0±2.8 cm (IQR, 7-15). The
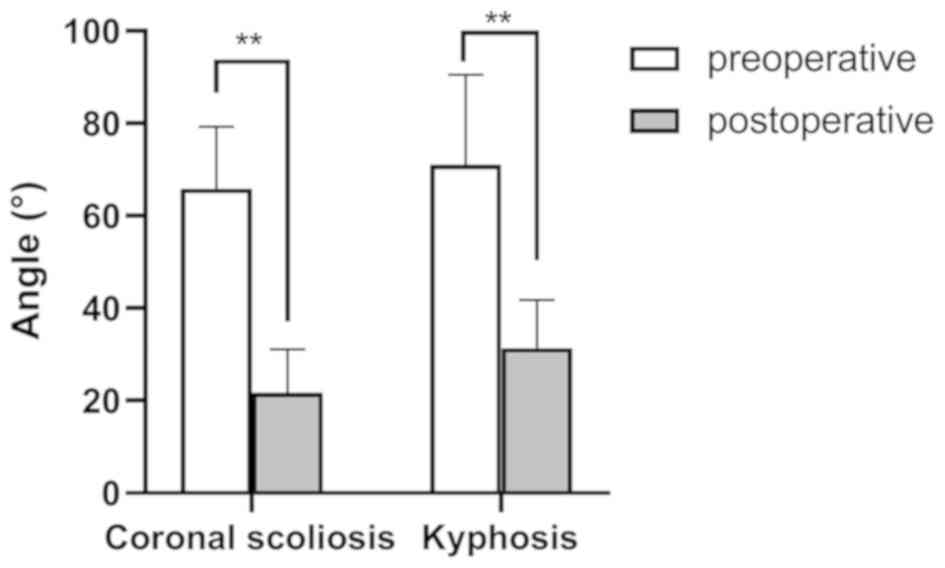
average postoperative coronal Cobb angle was 21.7±9.4 (IQR, 12-44)
and the sagittal kyphosis was 31.4±10.4 (IQR, 10-42), which were
significantly different from those before surgery (Fig. 1). The improvements in the coronal
and sagittal deformities were calculated to be 67±11 and 56±11%,
respectively, according to the data presented in Table II. For patients with hemivertebra
and dyssegmentation, further Schwab grade 3 or 4 osteotomy was
performed to release the anterior column and resect the
hemivertebra to obtain improved orthopedic effects. In addition,
coronal central sacral vertical line decreased from 19.4 (+11.3 mm)
preoperatively to 8.4 (+7.0 mm) postoperatively, and coronal
deviation was improved. Sagittal vertical axis was 25.5 (+19.3 mm)
and 29.7 (+9.1 mm) preoperatively and postoperatively,
respectively, with no significant sagittal imbalance (data not
shown).
 | Table IGeneral information of the 12
patients. |
Table I
General information of the 12
patients.
| Case no. | Sex | Age | Diagnosis | Intraspinal
pathology | Risser sign | Blood loss (ml) | Hospital stay
(days) | Follow-up
(months) |
|---|
| 01 | Male | 23 | NS | Ganglioma and
syringomyelia | 5 | 1,200 | 10 | 24 |
| 02 | Male | 40 | CS | Epidermoid cyst and
syringomyelia | 5 | 700 | 12 | 23 |
| 03 | Female | 24 | CS | Spinal cord tethering
and syringomyelia | 5 | 1,500 | 7 | 23 |
| 04 | Male | 17 | CS | Spinal cord
tethering | 3 | 2,000 | 7 | 22 |
| 05 | Male | 11 | NS | Spinal cord tethering
and syringomyelia | 2 | 400 | 6 | 22 |
| 06 | Male | 14 | NS | Spinal cord tethering
and intraspinal lipoma | 3 | 2,600 | 7 | 21 |
| 07 | Male | 28 | CS | Epidermoid cyst | 5 | 1,600 | 5 | 19 |
| 08 | Female | 50 | NS | Spinal cord tethering
and syringomyelia | 5 | 700 | 7 | 19 |
| 09 | Female | 52 | NS | Meningioma | 5 | 1,100 | 8 | 18 |
| 10 | Male | 43 | NS | Spinal cord tethering
and syringomyelia | 5 | 2,000 | 7 | 17 |
| 11 | Female | 25 | NS | Spinal cord
tethering | 5 | 2,650 | 6 | 12 |
| 12 | Female | 27 | CS | Spinal cord tethering
and diastematomyelia | 5 | 2,400 | 5 | 12 |
 | Table IIComparison of the preoperative and
postoperative parameters. |
Table II
Comparison of the preoperative and
postoperative parameters.
| | Scoliosis (˚) | | Kyphosis (˚) | | Muscle strength | Muscle tension |
|---|
| Case no. | Preoperative | Postoperative | Correction | Preoperative | Postoperative | Correction | Preoperative | Postoperative | Preoperative | Postoperative |
|---|
| 01 | 48˚ | 26˚ | 46% | 80˚ | 40˚ | 50% | 0 | 4 | High | Improved |
| 02 | - | - | - | 90˚ | 30˚ | 67% | 0 | 3 | High | Improved |
| 03 | 71˚ | 12˚ | 83% | 48˚ | 24˚ | 50% | 2 | 4 | High | Improved |
| 04 | 74˚ | 25˚ | 66% | - | - | - | 3 | 5 | High | Improved |
| 05 | 58˚ | 19˚ | 66% | 50˚ | 25˚ | 50% | 3 | 5 | Normal | - |
| 06 | 56˚ | 16˚ | 71% | 44˚ | 10˚ | 77% | 0 | 3 | High | Improved |
| 07 | - | - | - | 94˚ | 33˚ | 65% | 0 | 4 | High | Improved |
| 08 | - | - | - | 86.6˚ | 42.4˚ | 51% | 5 | 5 | High | Improved |
| 09 | 73˚ | 19˚ | 74% | - | - | - | 3 | 4 | High | Improved |
| 10 | 93˚ | 44˚ | 53% | 81˚ | 40˚ | 51% | 4 | 5 | Normal | - |
| 11 | 58˚ | 16˚ | 72% | 66˚ | 38˚ | 42% | 3 | 4 | Normal | - |
| 12 | 62˚ | 18˚ | 71% | - | - | - | 5 | 5 | Normal | - |
Radiographic images
Spinal cord untethering was performed for patients
with tethered spinal cord. Lesion resection was performed for
patients with epidermoid cyst, ganglioma, intraspinal lipoma and
meningioma. No special treatment was performed for syringomyelia.
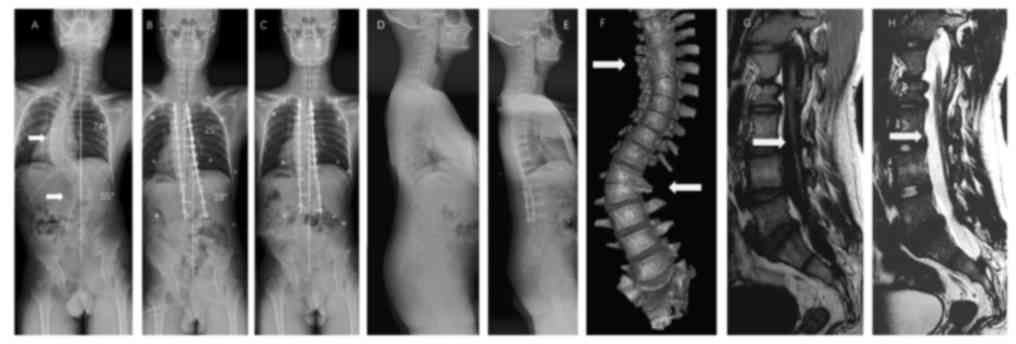
Radiographic photographs of typical case are shown in Figs. 2 and 3. Fig. 2
illustrates the case of a 17-year-old male patient with congenital
scoliosis associated with the tethered cord (case no. 4). Thoracic
curve and lumbar curve were severe, with trunk shift compensated,
shoulder and pelvic obliquity, leg length discrepancy and failure
of segmentation of T5-T7 and L1-L2 could be found preoperatively.
In the postoperative image without shoe inserts, it can be
identified that scoliosis was corrected and the shoulder obliquity
was improved, but the pelvic obliquity (the angle between the
pelvic coronal reference line and the horizontal reference line)
remained and the trunk shift (increased distance between the C7
plumb line and the center sacral vertical line) was decompensated
due to the leg length discrepancy (the difference between the
higher and lower horizontal reference line of femoral head). In the
postoperative image with shoe inserts, it can be identified that
that the leg length discrepancy and pelvic obliquity (the angle
between the pelvic coronal reference line and the horizontal
reference line decreased) were corrected and trunk shift (decreased
distance between the C7 plumb line and the center sacral vertical
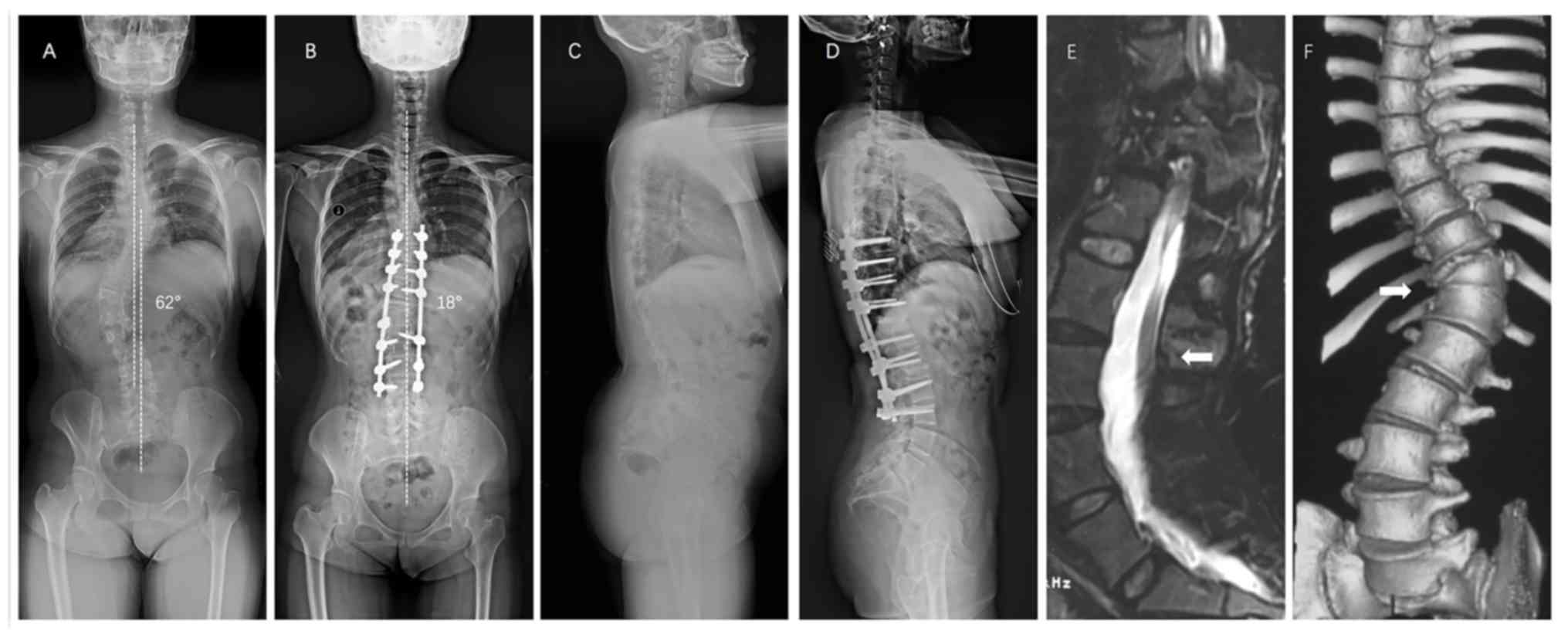
line) compensated. Fig. 3
illustrates the case of a 27-year-old female diagnosed with
congenital scoliosis and tethered spinal cord (case no. 12).
Coronal thoracic bending and lumbar bending were observed 3 years
before operation, the trunk was basically balanced by compensation,
T11 hemivertebra and T11-12 vertebral body were segmented badly
(Fig. 3A and C). Sagittal T2 WI MR before surgery
indicated spinal cord tethered (Fig.
3E). Preoperative three-dimensional reconstruction CT showed
that the T11-12 vertebral body was segmented badly, and the T11
hemivertebra was visible (Fig. 3F).
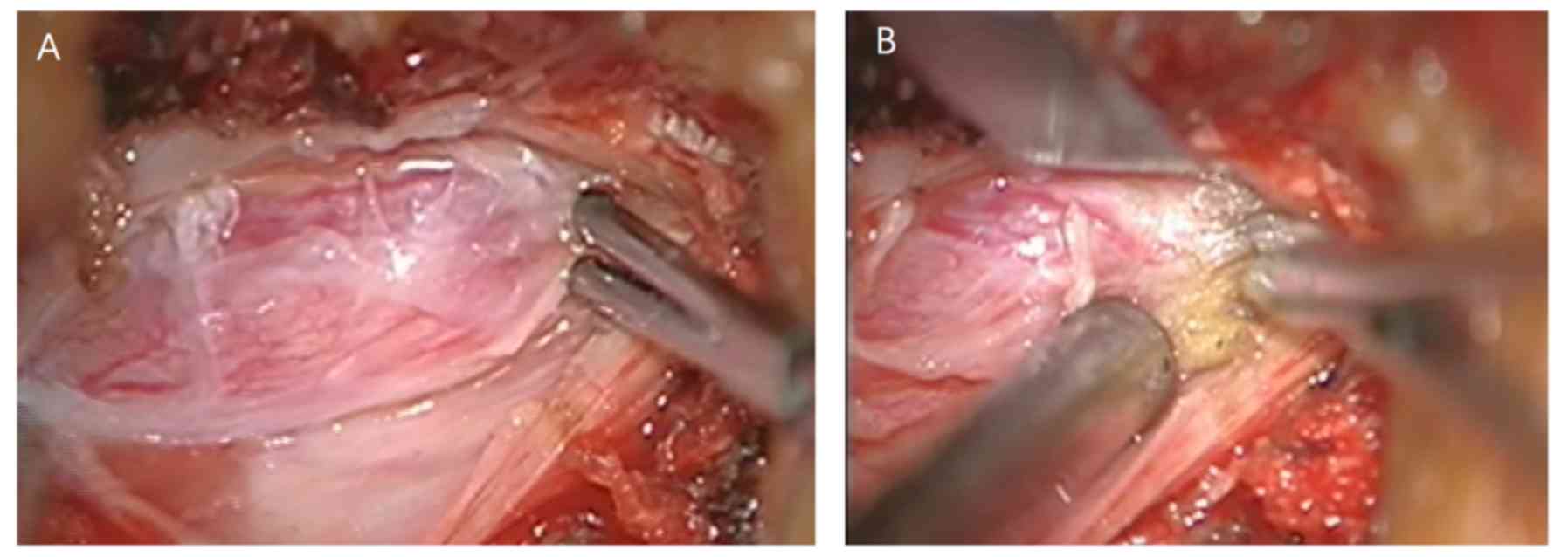
Thick terminal filaments were observed during the operation. After
electrophysiological monitoring confirmed the absence of nerves
(Fig. 4A), the terminal filaments
were cut off (Fig. 4B). The patient
was treated with spinal cord tether release, T11 hemivertebra
excision and lateral bending correction, and satisfactory results
were achieved (Fig. 3B and D).
Complications and functional recovery
following surgery
No deterioration of neurological dysfunction was
observed following surgery. The postoperative muscle strength of
the lower extremities was grade 3 in 2 patients, grade 4 in 5
patients and grade 5 in 5 patients, which were markedly improved
compared to preoperative muscle strength. Following surgery, lower
muscle tension was observed in the 8 patients with preoperative
high muscle tension. The mean stay in hospital was 7.3±2.0 days
(range, 5-12 days). No complications, such as infection,
cerebrospinal fluid leakage, fixation failure and fracture of rods
and screws, was found postoperatively. The mean follow-up time was
19.3±4.1 months (range, 12-24 months). No mortality, deterioration
of neurological dysfunction, tardive dyskinesia, pseudarthrosis and
correction loss was observed during the follow-up time.
Discussion
Coexisting intraspinal abnormalities can be found in
both congenital and neuromuscular scoliosis. Previous studies have
reported that intraspinal abnormalities can be observed on
preoperative MRI images in 20-58% patients with congenital
scoliosis, including the tethered spinal cord, syringomyelia,
intraspinal lipoma and teratoma (4,10).
Neuromuscular scoliosis induced by intraspinal abnormalities is
also common in clinical practice (4,11). For
example, cavity expansion of syringomyelia can affect both the
dorsomedial and ventromedial nerve, which further affects back
muscles that control trunk balance and finally contributes to
scoliosis (12). Spinal cord
ischemia caused by tethering can induce abnormal sensory pathways
and asymmetric paraspinal muscle strength, which finally leads to
scoliosis. Other researchers have suggested that scoliosis is one
of the clinical manifestations of intraspinal abnormalities
(4,7).
The typical treatment for these patients is
two-stage surgery. However, this surgical method is associated with
a number of limitations, including increased bleeding, increased
duration, damage to normal tissue. In order to solve its problems,
simultaneous surgical treatment in scoliosis associated with
intraspinal abnormalities has gradually come into being. When
compared to the classical surgery strategy, one-stage surgery is
safer, more effective and with fewer apparent complications. The
average surgical time, interoperative blood loss and hospital stay
time associated with this procedure are reduced compared with
traditional surgery. Better correction of scoliosis in single-stage
surgery has also been reported in several studies. In the current
study, the surgical time, blood loss and hospital stay time were
similar to those in previous studies of one-stage surgery (3,6).
Following surgery, an improvement in both scoliosis and kyphosis
was observed in all 12 patients, and no deterioration of
neurological dysfunction was observed. The muscle strength of the
lower extremities of the 10 patients and sphincter dysfunction has
been improved. No significant loss of correction was observed
during the follow-up time. Thus, one-stage surgery under
neuroelectrophysiological monitoring was recommended for patients
with intraspinal abnormalities and scoliosis.
Although spine deformity and intraspinal
abnormalities are congenital diseases, scoliosis and neurological
dysfunction appear relatively late (3). In the present study, the average age
of the 12 patients were 29.5±13.7 years, older than a mean age of
9.5 years reported by Mehta et al (6) and a mean age of 13 years reported by
Hamzaoglu et al (2). Some of
the patients did not visit the clinic once they had developed
neurological dysfunction, but came to seek medical consultations
after the deterioration of symptoms or an improvement in their
financial situation, which revealed that both clinical symptoms and
social factors can delay the seeking of medical help (3). Due to this delay in seeking medical
help and the mature skeletal development in the 12 patients in the
present study, increased stiffness was observed in these patients
compared with younger patients with scoliosis (Risser sign was
level 2 in 1 patient, level 3 in 2 patients and level 5 in 9
patients). In addition, dysplasia was common in the congenital
scoliosis patients (1 wedge-shaped vertebra, 1 malsegmentation, 1
wedge-shaped vertebra with malsegmentation and 2 hemivertebra with
malsegmentation). Thus, it was difficult to perform corrective
surgery in these patients. Osteotomy is a good choice for patients
with stiff, severe scoliosis and kyphosis (13-15).
In the current study, Schwab grade 2 osteotomy and spine release
under a microscope were performed in all 12 patients to increase
spinal flexibility and acquire better correction. For patients with
hemivertebra and malsegmentation, further Schwab grade 3 or 4
osteotomy was performed to release the front column and resect the
hemivertebra. Following surgery, scoliosis and kyphosis were
improved by 67±11 and 56±11%, respectively. Coronal correction was
better than the 27% reported by Mehta et al (6) and 23% reported by Isu et al
(16). In the present study, Schwab
grade 2 osteotomy was performed under the operating microscope to
release the spine, increase the flexibility of the spine and to
achieve improved orthopedic effects, including correcting scoliosis
and improving activity.
Scoliosis usually causes abnormalities in other
parts of the body, including unequal shoulder height and pelvic
asymmetry, which can not only change the local anatomy of the spine
but also affect the balance and symmetry of the whole body. The
pelvis, which is known as the mechanical support foundation of the
human trunk, plays an important role in spinal balance and
compensatory function (17). There
is a correlation between pelvic rotation and lumbar curvature, and
thoracic curvature; it can also be compensated for through lumbar
spine-mediated coordination (18).
Due to pelvic tilt and rotational decompensation, different degrees
of trunk deviation will occur following thoracic curvature
orthopedic internal fixation. Although pelvic reimbursement will
eventually reach a balance during follow-up, this compensation
mechanism is also constrained by spinal flexibility, and
compensation for patients with rigid scoliosis is limited (19). Correcting the lumbar curve in the
setting of pelvic obliquity may generate postoperative coronal
decompensation. In patients with pelvic obliquity in which the
spine is flexible and aligned, full correction of the curve may
lead to significant coronal decompensation, as the scoliotic curve
may be compensatory (20). If the
spine is flexible, a shoe lift may yield a considerable amount of
spinal coronal correction; however, if the spine is rigid, surgery
is probably necessary, as is a shoe insert depending on the final
standing alignment (21). Side
bending and kyphosis were serious in the patients enrolled in the
present study, which resulted in different degrees of rotation and
tilt of the pelvis. Some patients had severe lumbar bending and
pelvic tilt rotation. If lumbar bending is fused, it must be fixed
to S1 or even the pelvis. The flexibility and compensatory ability
of the waist will be completely lost, and the decompensation of the
pelvis will aggravate the trunk tilt. Therefore, for this group of
patients, we did not fully fuse lumbar bending during the
operation. Following the operation, patients were asked to wear
insoles to correct the pelvic tilt. Postoperative re-examination
showed that the lumbar curves of the patients were partially
compensated. The orthopedic effect was satisfactory and there was
no serious deviation of the trunk.
Previous studies have reported that spinal canal
lesions were mainly tethered cord, longitudinal cord, lipoma or
meningocele (22,23). However, in the present study, spinal
canal lesions also included a variety of intraspinal canal tumors.
However, this study had several limitations. First, this was a
retrospective study. Second, the sample size was relatively small.
Thus, further study of more patients and a longer follow-up time is
needed to investigate the loss of correction and compensation of
the pelvis.
In conclusion, single-stage surgery for scoliosis
combined with intraspinal abnormalities was safe and effective, and
can produce satisfactory correction of deformities and an
improvement of neurological function. No postoperative
complications were observed. The following factors are required for
single-stage surgery for scoliosis combined with intraspinal
abnormalities: i) The surgical team is experienced in dealing with
scoliosis and intraspinal scoliosis at the same time; ii) a
detailed plan is made before surgery; and, iii) interoperative
neuroelectrophysiological monitoring is available.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KW conceived, designed and analyzed the data. KW and
FS performed all the simultaneous surgical treatments in scoliosis
associated with intraspinal abnormalities. FS analyzed the data. HW
conceived and designed the research and performed the surgeries. FS
performed the research. FZJ analyzed the data and provided final
approval of the version to be published. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The current study was approved by the ethics
committee of the Xuanwu Hospital of Capital Medical University
(approval no. 2016020; V1.3, 2016-9-25; Beijing, China) and all the
patients or their families gave informed consent and signed a
statement to that effect.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Pereira EAC, Oxenham M and Lam KS:
Intraspinal anomalies in early-onset idiopathic scoliosis. Bone
Joint J. 99-B:829–833. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hamzaoglu A, Ozturk C, Tezer M, Aydogan M,
Sarier M and Talu U: Simultaneous surgical treatment in congenital
scoliosis and/or kyphosis associated with intraspinal
abnormalities. Spine (Phila Pa 1976). 32:2880–2884. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Halawi MJ, Lark RK and Fitch RD:
Neuromuscular scoliosis: Current concepts. Orthopedics.
38:e452–e456. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jankowski PP, Bastrom T, Ciacci JD, Yaszay
B, Levy ML and Newton PO: Intraspinal pathology associated with
pediatric scoliosis: A ten-year review analyzing the effect of
neurosurgery on scoliosis curve progression. Spine (Phila Pa 1976).
41:1600–1605. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Mcmaster MJ: Occult intraspinal anomalies
and congenital scoliosis. J Bone Joint Surg Am. 66:588–601.
1984.PubMed/NCBI
|
|
6
|
Mehta VA, Gottfried ON, McGirt MJ,
Gokaslan ZL, Ahn ES and Jallo GI: Safety and efficacy of concurrent
pediatric spinal cord untethering and deformity correction. J
Spinal Disord Tech. 24:401–405. 2011.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Samdani AF, Asghar J, Pahys J, D'Andrea L
and Betz RR: Concurrent spinal cord untethering and scoliosis
correction: Case report. Spine (Phila Pa 1976). 32:E832–E836.
2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Little DG and Sussman MD: The risser sign:
A critical analysis. J Pediatr Orthop. 14:569–575. 1994.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ranu H, Wilde M and Madden B: Pulmonary
function tests. Ulster Med J. 80:84–90. 2011.PubMed/NCBI
|
|
10
|
Wang Z, Liu J, Shen J, Xue X and Qiu G:
Abnormalities associated with congenital scoliosis: A retrospective
study of 226 Chinese surgical cases. Spine (Phila Pa 1976).
38:814–818. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Prahinski JR, Polly DW Jr, Mchale KA and
Ellenbogen RG: Occult intraspinal anomalies in congenital
scoliosis. J Pediatr Orthop. 20:59–63. 2000.PubMed/NCBI
|
|
12
|
Kontio K, Davidson D and Letts M:
Management of scoliosis and syringomyelia in children. J Pediatr
Orthop. 22:771–779. 2002.PubMed/NCBI
|
|
13
|
Liu ZD, Li XF, Zang WP, Wang ZY and Wu LM:
Combined pedicle subtraction osteotomy and polysegmental closing
wedge osteotomy for correction of the severe thoracolumbar kyphotic
deformity in ankylosing spondylitis. Zhonghua Wai Ke Za Zhi.
47:681–684. 2009.(In Chinese). PubMed/NCBI
|
|
14
|
Gokcen B, Yilgor C and Alanay A:
Osteotomies/spinal column resection in paediatric deformity. Eur J
Orthop Surg Traumatol. 24 (Suppl 1):S59–S68. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Holewijn RM, Schlösser TP, Bisschop A, van
der Veen AJ, Stadhouder A, van Royen BJ, Castelein RM and de
Kleuver M: How does spinal release and ponte osteotomy improve
spinal flexibility? The law of diminishing returns. Spine Deform.
3:489–495. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Isu T, Chono Y, Iwasaki Y, Koyanagi I,
Akino M, Abe H, Abumi K and Kaneda K: Scoliosis associated with
syringomyelia presenting in children. Childs Nerv Syst. 8:97–100.
1992.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Skalli W, Zeller RD, Miladi L, Bourcereau
G, Savidan M, Lavaste F and Dubousset J: Importance of pelvic
compensation in posture and motion after posterior spinal fusion
using CD instrumentation for idiopathic scoliosis. Spine (Phila Pa
1976). 31:E359–E366. 2006.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Gum JL, Asher MA, Burton DC, Lai SM and
Lambart LM: Transverse plane pelvic rotation in adolescent
idiopathic scoliosis: Primary or compensatory? Eur Spine J.
16:1579–1586. 2007.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Asher MA, Lai SM, Carlson BB, Gum JL and
Burton DC: Transverse plane pelvic rotation increase (TPPRI)
following rotationally corrective instrumentation of adolescent
idiopathic scoliosis double curves. Scoliosis. 5(18)2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Radcliff KE, Orozco F, Molby N, Chen E,
Sidhu GS, Vaccaro AR and Ong A: Is pelvic obliquity related to
degenerative scoliosis? Orthop Surg. 5:171–176. 2013.PubMed/NCBI View
Article : Google Scholar
|
|
21
|
Ames CP, Smith JS, Scheer JK, Bess S,
Bederman SS, Deviren V, Lafage V, Schwab F and Shaffrey CI: Impact
of spinopelvic alignment on decision making in deformity surgery in
adults: A review. J Neurosurg Spine. 16:547–564. 2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Herman JM, Mclone DG, Storrs BB and Dauser
RC: Analysis of 153 patients with myelomeningocele or spinal lipoma
reoperated upon for a tethered cord presentation, management and
outcome. Pediatr Neurosurg. 19:243–249. 1993.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Peng L and Xu BT: Microsurgical treatment
of complicated tethered cord resulting from mixed lipoma in a
12-year-old patient: A case report. Nan Fang Yi Ke Da Xue Xue Bao.
31:834–835. 2011.(In Chinese). PubMed/NCBI
|